Abstract
Introduction
Previous studies have shown racial disparities in outcomes after out-of-hospital cardiac arrest. Although several treatment factors may account for these differences, there is limited information regarding differences in CPR quality and its effect on survival in underrepresented racial populations.
Methods
We conducted a secondary analysis of data from patients enrolled in the Pragmatic Airway Resuscitation Trial (PART). We calculated compliance rates with AHA 2015 high quality CPR metrics as well as compliance to intended CPR strategy (30:2 or continuous chest compression) based on the protocol in place for the first responding EMS agency. The primary analysis used general estimating equations logistic regression to examine differences between black and white patients based on EMS-assessed race after adjustment for potential confounders. Sensitivity analyses examined differences using alternate race definitions.
Results
There were 3004 patients enrolled in PART of which 1734 had >2 minutes of recorded CPR data and an EMS-assessed race (1003 white, 555 black, 176 other). Black patients had higher adjusted odds of compression rate compliance (OR: 1.36, 95% CI: 1.02-1.81) and lower adjusted odds of intended CPR strategy compliance (OR: 0.78, 95% CI: 0.63-0.98) compared to white patients. Of 974 transported to the hospital, there was no difference in compliance metric estimates based on ED-reported race.
Conclusion
Compression rate compliance was higher in black patients however compliance with intended strategy was lower based on EMS-assessed race. The remaining metrics showed no difference suggesting that CPR quality differences are not important contributors to the observed outcome disparities by race.
Keywords: racial disparities, chest compressions, emergency medicine
Introduction
Numerous studies have demonstrated the presence of racial disparities in outcomes after out-of-hospital cardiac arrest (OHCA), with explanations ranging from physiologic differences to treatment differences1–6. Black patients have worse access to quality healthcare,7 more pre-existing medical conditions,8–9 and live in greater proportions in areas of lower socioeconomic status compared to white patients.10–11 Previous studies on treatment differences by race have primarily focused on the time period prior to emergency medical services (EMS) agency arrival on scene, specifically with respect to the proportion of OHCA witnessed by bystanders, the proportion of bystander cardiopulmonary resuscitation (CPR), frequency of dispatch CPR instructions, and EMS response times4,8,12–13. Aside from a few studies that have examined differences in drug administration14, differences related to other treatments provided by EMS providers for OHCA have not been explored and these could partly explain the disparities in outcomes observed after OHCA for underrepresented racial populations.
The timely delivery of high-quality CPR by EMS professionals has been directly associated with improved patient outcomes.15 The 2015 American Heart Association (AHA) Guidelines16 recommended best practices for several CPR components, including quality guidelines for compression rate (100 to 120), depth (5cm to 6cm or 2 to 2.4 in), pre-shock pauses (<10 seconds) and compression strategy (30:2). Examining differences in compliance with these CPR quality metrics by patient race may help identify potential modifiable factors for future interventions aimed to reduce disparities.
Our study objective was to examine racial disparities in the quality of CPR performed by EMS professionals, using a dataset with high rates of EMS-assessed race and CPR quality performance measures. Our aims were to examine differences in CPR compliance status by 1) EMS-assessed race and 2) ED-reported race while examining 3) any potential interaction between patient race and neighborhood race.
Methods
Study Design
We conducted a secondary analysis of data from patients enrolled across five US cities (Birmingham, AL; Dallas-Fort Worth, TX; Milwaukee, WI; Pittsburgh, PA; Portland, OR) and their surrounding areas in the Pragmatic Airway Resuscitation Trial (PART), ClinicalTrials.gov Identifier: NCT02419573, from 2015 to 2017.17 In brief, PART aimed to assess differences in 72-hour survival for patients who suffer out-of-hospital cardiac arrest and were randomized to receive initial airway management with either a laryngeal tube or endotracheal intubation. Institutional Review Boards of participating institutions approved PART under federal Exception from Informed Consent rules (21 CFR 50.24).
Study Setting
Twenty-seven EMS agencies that varied in system structure (tiered BLS-ALS; ALS only), annual call volume, and geographical footprints from aforementioned five US communities participated in PART. These agencies differed with respect to monitor-defibrillator used: Zoll M and X series (Zoll, Inc., Chelmsford, MA) which uses an accelerometer; Philips MRX (Philips, Inc., Amsterdam, The Netherlands) which uses an accelerometer and force sensor; or Physio-Control LifePak versions 12, 15 and 1000 (Physio-Control, Inc., Redmond, WA) which uses impedance to assess CPR metrics.
Patient population
Consistent with the inclusion/exclusion criteria for the trial, we excluded patients <18 years. For purposes of this analysis, we also excluded patients with <2 minutes of CPR process data (Figure 1).
Figure 1.
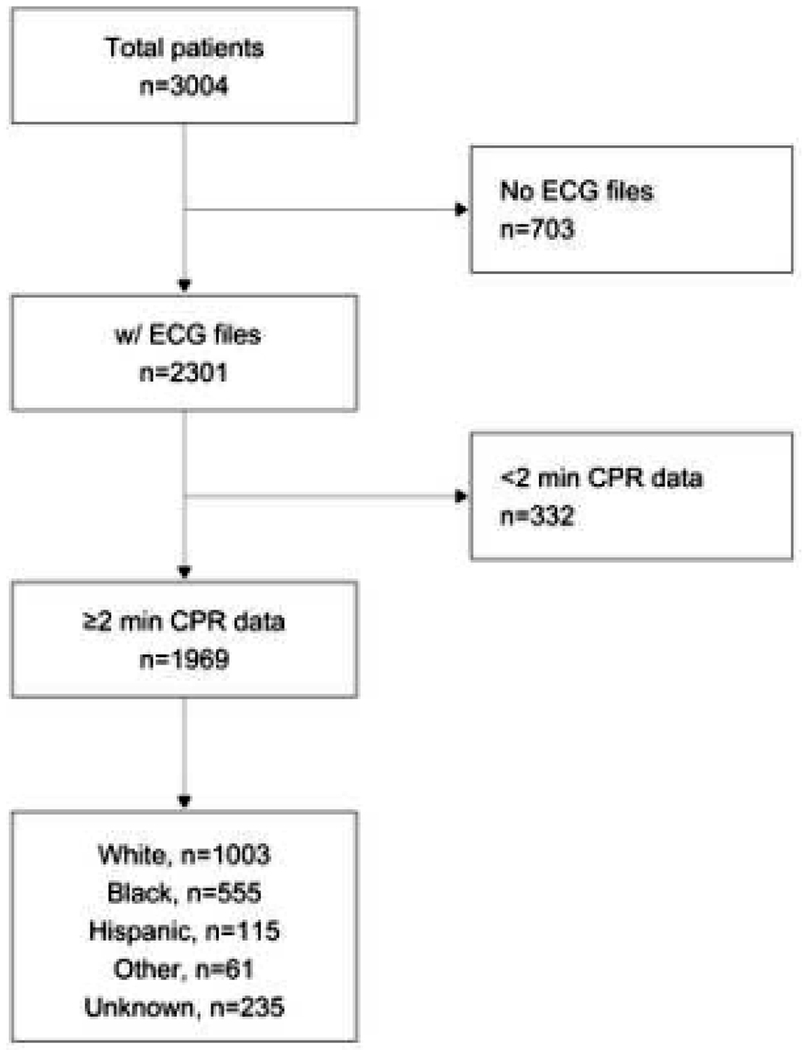
CONSORT Patient Flow Diagram
Race variables
An important challenge in OHCA disparities research is the accurate capture of patient race. As patients are unresponsive, and in most cases alone, race can often only be presumed by EMS clinicians. To account for this concern, some studies have used neighborhood level race data2,3,5 or individual reported race obtained in the ED or following admission to the hospital.
For this study, we are most interested in whether observed differences in CPR quality of care are due to inherent bias due to presumed race. Since EMS treatment is not a physiologic factor, we felt that EMS-assessed race would be of most interest. In the PART trial, race data were recorded by EMS via check boxes. Hispanic ethnicity was grouped with race; in only a few Hispanic patients was a race also checked. Because we are interested in underrepresented minorities, we focused our analysis on comparing white patients to black and separately Hispanic patients. However, we subsequently dropped Hispanic patients from the analysis because of small sample size. Thus, for the primary analysis, we examined differences between EMS-assessed white and black races. We also conducted two sensitivity analyses focusing on alternate race groups 1) differences between ED-reported white and black patients for patients transported to a hospital and 2) differences between EMS-assessed white and non-white (e.g. black, Hispanic, Asian, Native American/Pacific Islander, other, Multi-race) races.
CPR Quality variables
Using software from three different manufacturers, the lead author manually reviewed waveforms to obtain compression start and stop times as well as shock times. For quality assurance, prior to the project the lead author abstracted data from cases previously reviewed by data coordinators from other studies conducted by the Resuscitation Outcomes Consortium (ROC). In a 60 case sub-study across the five participating PART sites and three monitor-defibrillator manufacturers, 89% of all seconds had a matching compression status between the two reviews; mean (sd) CCF was comparable between the two sources - 0.86 (0.12) vs 0.85 (0.12); and the intraclass correlation of the mean CCF was 0.95.
Pre-shock times were calculated as time elapsed between end of the compression segment and the shock. In addition, compression rate and depth values over all minute epochs were obtained directly from the manufacturer’s software episode summary; median and mean values were calculated per patient across all epochs. A maximum of 20 minutes of CPR data was included. CPR data after advanced airway placement or start of mechanical compression were excluded because they represented a change in CPR strategy.
Compliance for the three standard metrics was based on AHA 2015 high quality CPR recommendations: mean compression rate 100-120, mean compression depth 5-6 cm (2-2.4 in), and mean pre-shock pause <10 seconds. Compliance to intended CPR strategy was defined as receiving CPR consistent with intended protocol of the responding EMS agency. Agencies operated under one of two CPR strategies – continuous chest compressions with asynchronous ventilations (one breath every 10 compressions) given without a pause (CCC) or a method of 30 chest compressions followed by a pause for two ventilations (30:2). Using an automated algorithm based on three metrics18,19 that describe the pattern of chest compression segments (chest compression fraction (CCF), median compression segment length and number of pauses per minute) CPR was classified as either CCC or 30:2 while some cases remained unclassified if not enough metrics were met.
Statistical analysis
We compared patient, event, EMS systems and treatment characteristics as well CPR metrics by EMS-assessed race and used regression models to assess unadjusted differences. We used general estimating equation (GEE) regression models to examine whether differences existed between white and black patients in compliance with compression rate, compression depth and pre-shock pause CPR quality recommendations after adjusting for age, sex (male; female), initial rhythm (VT/VF; PEA; Asystole; No Shock-No Strip), service level of first arriving agency (ALS; BLS) and PART site while clustering on the PART randomization cluster. We specifically did not adjust for other Utstein variables such as bystander CPR, witness status and response time because we did not feel these would be associated with the quality of CPR provided by EMS. For compliance to intended strategy, we adjusted for intended CPR strategy (CCC; 30:2) instead of site and not in addition to because of the collinearity between the two.
For the set of primary outcomes, including binary compliance metrics for compression rate; compression depth; pre-shock pause and intended strategy, we used GEE logistic regression models. For secondary outcomes, including continuous values for rate, depth and pre-shock pause, we used GEE linear regression models. For each metric, we ran two sensitivity analysis where we substituted 1) ED - reported race for those who were transported and 2) EMS-assessed non-white race for black race.
Because of previous research that showed differing proportions of bystander CPR for black individuals in predominantly white vs black neighborhoods20, we added an interaction term to check for effect modification by neighborhood level race. Essentially, this would allow us to examine if patients are treated differently in predominantly white areas than black areas. We defined neighborhood race by the percent of black residents (0%-25%; 26%-50%; 51%-75%; 76%-100%) living in the census tract where the arrest occurred.
In addition, we examined the compliance metrics by whether EMS-assessed race matched ED-reported race. Finally, we examined mean compression rate and depth by EMS-assessed race across the resuscitation effort by minute to see if CPR quality changed over time for black patients as compared to white patients. We used linear regression models with a race times resuscitation minute interaction term to assess if differences in slope existed.
Analyses were performed in R v3.5.1 (R Core Team, Vienna, Austria).
Results
Of 3004 patients enrolled in the PART trial, 703 did not have any CPR process files while 332 had a file but <2 minutes of data. Of the 1969 patients with CPR data, 1734 had a known EMS-assessed race (1003 white, 555 black, 115 Hispanic, 61 other).
Black patients compared to white patients had significantly lower unadjusted proportions of male sex, initial shockable EMS rhythm, bystander CPR, and public location of arrest (all p<0.01, Table 1). Additionally, black patients had significantly longer unadjusted times of EMS arrival (p=0.03) and lower rates of an ALS capable first arriving unit (p<0.001). Mean time from resuscitation start to patient transport or resuscitation termination did not differ between races.
Table 1:
Baseline Characteristics by EMS-assessed Race/Ethnicity
| White | Black | Hispanic | Other | |
|---|---|---|---|---|
|
| ||||
| N | 1003 | 555 | 115 | 61 |
| Sex, n (%) | ||||
| Male | 635 (63.4) | 295 (53.2) | 70 (60.9) | 42 (68.9) |
| Female | 367 (36.6) | 260 (46.8) | 45 (39.1) | 19 (31.1) |
| Age, median (IQR) | 64 (53, 76) | 62 (53, 73) | 59 (43, 72) | 64 (52, 75) |
| Initial EMS Rhythm, n (%) | ||||
| VTVF | 198 (20.0) | 76 (13.9) | 16 (13.9) | 13 (22.0) |
| Asystole | 215 (21.7) | 126 (23.0) | 27 (23.5) | 6 (10.2) |
| PEA | 551 (55.7) | 317 (57.8) | 72 (62.6) | 40 (67.8) |
| No Shock No Strip | 25 (2.5) | 29 (5.3) | 0 (0.0) | 0 (0.0) |
| Unknown | 14 (1.4) | 7 (1.3) | 0 (0.0) | 2 (3.3) |
| Witness Status, n (%) | ||||
| EMS | 81 (9.0) | 58 (11.5) | 17 (16.2) | 3 (5.4) |
| Bystander | 349 (38.6) | 186 (36.8) | 41 (39.0) | 26 (46.4) |
| Not | 475 (52.5) | 261 (51.7) | 47 (44.8) | 27 (48.2) |
| Unknown | 98 (9.8) | 50 (9.0) | 10 (8.7) | 5 (8.2) |
| Bystander CPR Status, n (%) | ||||
| Yes | 518 (53.7) | 202 (36.5) | 55 (49.1) | 30 (51.7) |
| No | 446 (46.3) | 351 (63.5) | 57 (50.9) | 28 (48.3) |
| Unknown | 39 (3.9) | 2 (0.4) | 3 (2.6) | 3 (4.9) |
| Public Location, n (%) | ||||
| Yes | 130 (13.0) | 42 (7.6) | 16 (14.0) | 6 (9.8) |
| No | 872 (87.0) | 511 (92.4) | 98 (86.0) | 55 (90.2) |
| Unknown | 1 (0.1) | 2 (0.4) | 1 (0.9) | 0 (0.0) |
| Arrival time (min), mean (sd) | 5.2 (2.3) | 5.5 (2.4) | 5.1 (2.0) | 5.5 (2.8) |
| First arriving agency service level | ||||
| BLS | 368 (36.7) | 296 (53.3) | 43 (37.4) | 20 (32.8) |
| ALS | 635 (63.3) | 259 (46.7) | 72 (62.6) | 41 (67.2) |
| Time from arrival to patient transport (min), mean (sd) | 27.5 (10.5) | 28.5 (10.6) | 27.5 (10.0) | 24.0 (6.2) |
| Time from arrival to resuscitation stop (min), mean (sd) | 30.2 (10.3) | 31.5 (8.6) | 31.1 (6.9) | 28.9 (9.0) |
NOTE – 235 patients had an unknown EMS-assessed race
CPR performance metrics by EMS-assessed race are summarized in Table 2. Black patients had lower pre-shock pause compliance (46.9% vs 63.8%, p=0.01) and intended strategy compliance (43.6% vs 54.6%, p<0.001) compared to white patients. There were no differences in rate or depth compliance measures between the two races.
Table 2:
CPR Metrics by EMS-assessed Race
| White | Black | Hispanic/Other | Black v White | |
|---|---|---|---|---|
|
| ||||
| N | 1003 | 555 | 176 | p-value |
| Compression Rate | ||||
| Mean (sd) | 112.8 (10.2) | 115.1 (13.4) | 111.1 (7.9) | <0.001 |
| Rate 100-120, n (%) | 761 (75.9) | 404 (72.8) | 150 (85.2) | 0.18 |
| Compression Depth | ||||
| Mean (sd) | 52.1 (11.2) | 50.5 (10.7) | 51.1 (9.5) | 0.01 |
| Depth 50-60mm, n (%) | 316 (35.5) | 154 (37.1) | 63 (37.5) | 0.58 |
| Pre-Shock Pause | ||||
| Mean (sd) | 10.4 (13.4) | 15.3 (17.8) | 12.3 (14.8) | 0.01 |
| <10sec, n (%) | 117 (63.6) | 38 (46.9) | 13 (59.1) | 0.01 |
| Chest Compression Fraction | ||||
| Mean (sd) | 0.86 (0.13) | 0.84 (0.15) | 0.89 (0.11) | 0.01 |
| >0.60, n (%) | 955 (95.2) | 519 (93.5) | 173 (98.3) | 0.16 |
| Compliance to intended strategy, n (%) | ||||
| Overall | 548 / 1003 (54.6) | 242 / 555 (43.6) | 91 / 176 (51.7) | <0.001 |
| CCC | 392 / 593 (66.1) | 140 / 227 (61.7) | 75 / 126 (59.5) | 0.24 |
| 30:2 | 156 / 410 (38.0) | 102 / 328 (31.1) | 16 / 50 (32.0) | 0.05 |
After adjustment for potential confounders, black patients had higher odds of compression rate compliance (OR: 1.36, 95% CI: 1.02-1.80) and lower odds of strategy compliance (OR: 0.79, 95% CI: 0.63-0.98) compared to white patients (Table 3). There were no significant differences in compression depth or pre-shock pause compliance by race. Nearly 75% of patients transported to the hospital had matching EMS-assessed and ED-reported racial categories. When considering ED-reported race (n=974), there were no differences in compliance metric estimates between races. When modeled continuously, compression depth (mm) was significantly different, β (95% CI) = −1.81 (−3.06, −0.55), for EMS-assessed black patients in comparison to white patients. No other continuous differences were detected.
Table 3:
Logistic regression estimates (OR 95%CI) for primary and sensitivity analyses
| Comparison | Black vs White | Black vs White | Black vs White | Non-White vs White |
|---|---|---|---|---|
|
| ||||
| Model Adjustment | Unadjusted | Adjusted | Adjusted | Adjusted |
|
| ||||
| Race Definition | EMS-assessed | EMS-assessed | ED-reported | EMS-assessed |
| Rate Compliance | 0.85 (0.67, 1.08) | 1.36 (1.02, 1.80) | 0.85 (0.57, 1.26) | 1.36 (1.05, 1.76) |
| Depth Compliance | 1.07 (0.84, 1.36) | 1.01 (0.78, 1.31) | 1.40 (0.95, 2.05) | 1.02 (0.81, 1.29) |
| Pre-Shock Compliance | 0.51 (0.30, 0.86) | 0.84 (0.44, 1.61) | 1.06 (0.48, 2.37) | 0.90 (0.50, 1.60) |
| Strategy Compliance | 0.64 (0.52, 0.79) | 0.79 (0.63, 0.98) | 1.07 (0.94, 1.22) | 0.78 (0.64, 0.96) |
NOTE: Adjusted models for rate, depth and pre-shock compliance include sex, age, initial EMS rhythm, ALS first on scene and site; Adjusted models for strategy compliance include sex, age, initial EMS rhythm, ALS first on scene and intended CPR strategy
Results when comparing EMS-assessed white patients to non-white patients were consistent though slightly attenuated from the white vs black comparisons. Rate compliance was significantly higher in non-whites (OR: 1.34, 95%CI: 1.04-1.74) and strategy compliance was lower in non-whites (OR: 0.78, 95%CI: 0.64-0.95).
In an interaction analysis with EMS-assessed race, neighborhood race modified the association with strategy compliance (Q4 OR: 1.34, 95% CI: 0.59-3.08 vs Q1 OR: 0.62, 95% CI: 0.43-0.89; interaction p-value<0.01). There was no significant interaction between EMS-assessed race and neighborhood race for the three other metrics of interest.
Compression depth compliance was significantly higher (interaction p-value <0.001; Supplemental Table 1) for black patients than white patients when EMS-assessed race matched ED-reported race (OR: 1.45, 95%CI: 0.96 −2.17) compared to when there was a mismatch (OR: 0.40, 95%CI: 0.16, 0.98).
Mean compression rate across resuscitation minute differed by race (white β: 0.13, 95%CI: 0.05-0.21 vs black β: 0.36, 95%CI: 0.28-0.44); interaction p-value <0.01) while depth did not vary by race across resuscitation minute (Supplemental Figure 1).
Intended CPR strategy, racial distribution and metric compliance all varied across PART site (Supplemental Table 2).
Discussion
This study suggests that although there are some differences in individual CPR performance metrics, the conflicting results do not suggest racial disparities in overall CPR quality. While we were unable to find differences in adjusted compression depth or pre-shock pause compliance, black patients had higher compliance with compression rate but lower compliance with intended compression strategy. Similar to the known inverse relationship between compression depth and rate, these findings might simply suggest a tradeoff – improved care in one area such as rate may lead to worse performance in another such as CPR strategy regardless of race.
This tradeoff could be important with respect to survival differences between black and white patients. In this study, 59% of black patients were treated by agencies with 30:2 as their intended strategy. Our previous research showed that a higher rate of noncompliance to 30:2 is associated with lower survival19 while several studies have shown higher compliance to rate is associated with improved survival.16 Along with no differences in depth or pre-shock pause compliance, these counteracting effects could be a major reason why we observed no survival difference between white and black patients in this cohort.21
An important driver of outcome in almost all clinical trials conducted by the ROC, the parent network of PART, has been site.22–24 This finding was evident in this study as compliance with the four CPR metrics varied by site (Supplemental Table 1). In the unadjusted analysis, compression rate compliance was lower for black patients than white, however, it was significantly higher once we adjusted for potential confounders including site. This was primarily due to one site which had both the lowest compliance and highest percentage of black patients. Because the site accounted for a large proportion of black patients in the study, compliance for black patients has a greater impact than that for white patients. Adjusting for site accounts for this and helps explain the findings in the adjusted analyses.
For those 974 patients admitted to the ED, nearly 75% had matching EMS-assessed and ED-reported race. The estimates using ED-reported race were not significant, most likely due to the smaller sample size. An interesting observation is seen when examining those with matching EMS-assessed and ED-reported race against those that have a mismatch. For those with matching race, black patients had higher odds of compliant depth, OR (95%CI) = 1.45 (0.96, 2.17) while for those with nonmatching race, black patients have lower odds of compliant depth, OR (95%CI) = 0.40 (0.16, 0.98). It could be that quality depth begets higher rates of ROSC and hence an increased opportunity to confirm race in the field; alternatively, this could be related to a data entry error or simply represent a random finding.
Similar with prior studies that showed bystander CPR proportions for black patients differ based on neighborhood,12 we found that the association between compression rate and EMS-assessed race was modified by neighborhood level race. This suggests that rate compliance was higher for black patients living in predominantly black areas and lower for black patients living in predominantly white areas. However, this individual finding is difficult to interpret since neighborhood did not modify the association with the three other metrics.
When comparing EMS-assessed white patients to non-white patients, results were consistent - higher odds of compression rate compliance and lower odds of strategy compliance for non-white compared to white. This is not surprising since black patients accounted for over 75% of non-white patients in this population.
While we were unable to determine if the EMS treatment rate varied by race in the PART trial, we were able to examine whether CPR varied over time. We found no difference in length of resuscitation by race in patients who were transported or who were pronounced dead at the scene. However, we did find a race difference in compression rate across resuscitation minute. Mean compression rate for black patients increased by 3.6 per 10 minutes compared to white patients who increased by 1.8 per 10 minutes. In addition, mean compression rates for minutes 16-19 were all >120 for black patients. Compression depth, although not significant over minute does appear to have an inverse trend compared to rate. This tradeoff could be explained by changes in chest stiffness over resuscitation minute. While previous studies have explored stiffness by sex25, more studies are needed to address this finding.
This study has several strengths with the first being the geographically diverse sites from across the US. In addition, the amount of available EMS-assessed race was high (89%) as was the agreement between EMS-assessed race and ED-reported race (Kappa = 0.88 (0.86, 0.90)).21 Limitations include the proportion of patients with missing CPR data (34%) or missing compression depth (18%) in those with available CPR data; the proportion of unclassified care (29.7%) via the algorithm; the lack of racial diversity in three of the study sites; the race of responding EMS providers and the overall importance of site in the dataset.
We acknowledge that findings of this study are limited by its observational design. Racial disparities in health care persist and we hope that this as well as another PART manuscript related to the impact of race on resuscitation quality can serve as a framework to guide future research in this year. Important areas for investigation include impact of the race of the responding EMS clinician on resuscitation outcomes and quality metrics as well as the impact of manual vs. mechanical CPR on outcomes according to race.
Conclusion
Compression rate compliance was higher in black patients however compliance with intended strategy was lower based on EMS-assessed race. The remaining metrics showed no difference suggesting that CPR quality disparities are not important contributors to the observed outcome disparities by race.
Supplementary Material
Acknowledgements
This study was supported by grant 5R21HL145423-02 from National Heart Lung and Blood Institute. The Resuscitation Outcomes Consortium institutions participating in the studies were supported by a series of cooperative agreements from the NHLBI, including 5U01 HL077863 (University of Washington Data Coordinating Center), HL077866 (Medical College of Wisconsin), HL077871 (University of Pittsburgh), HL077873 (Oregon Health and Science University), HL077881 (University of Alabama at Birmingham), and HL077887 (University of Texas Southwestern Medical Center/Dallas). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung and Blood Institute or the National Institutes of Health. The NHLBI did not have any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflicts of Interest:
Robert Schmicker, Audrey Blewer, Josh Lupton, Henry Wang, Elisabete Aramendi, Mohamed Hagahmed Owen Traynor, Riccardo Colella and Mohamud Daya reported no conflicts.
Tom Aufderheide is the site Principal Investigator of the Milwaukee site for the ROC grant.
Ahamed Idris has research grants from the National Institutes of Health and the Center for Disease Control and Prevention. He is an unpaid volunteer of the American Heart Association National Emergency Cardiovascular Care Committee and an unpaid volunteer of the Clinical Advisory Board for Stryker Belfast, Northern Ireland.
Appendix Figure 1.
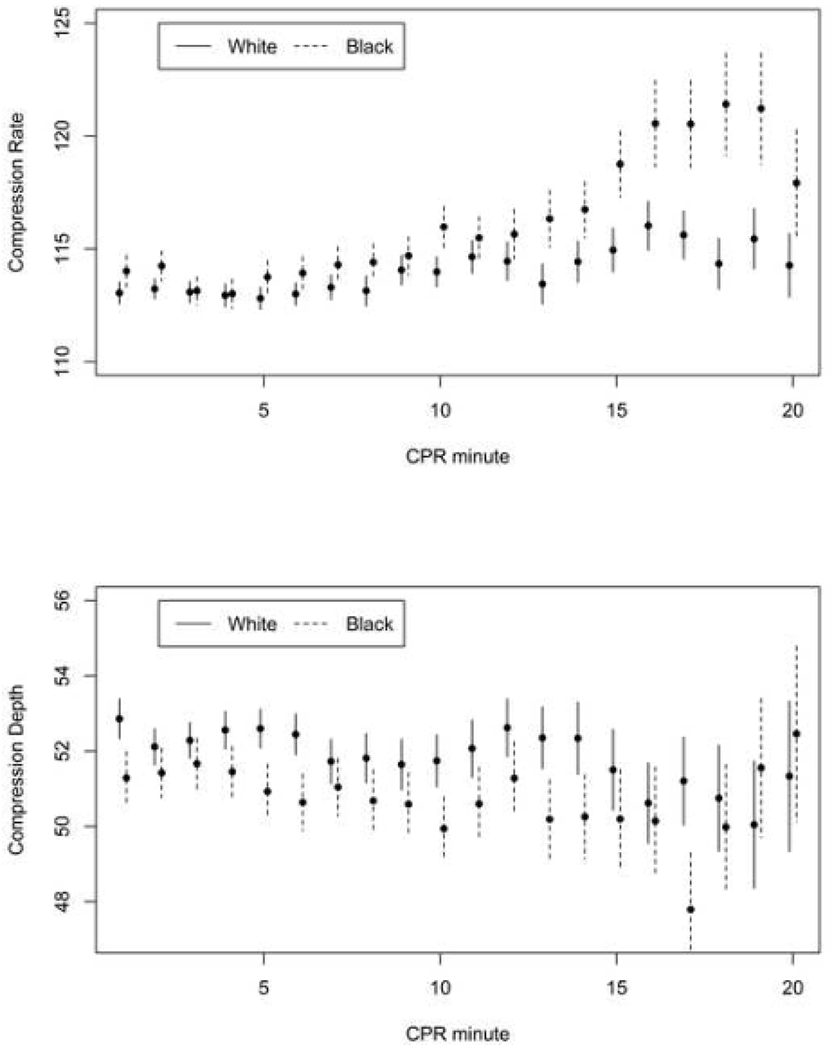
Mean compression rate and depth over first 10 minutes of CPR by EMS-assessed race
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Access to data and data analysis
Robert Schmicker had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Reinier K, Rusinaru C, Chugh SS. Race, ethnicity, and the risk of sudden death. Trends Cardiovasc Med. 2019;29(2):120–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Starks MA, Schmicker RH, Peterson ED, et al. Association of Neighborhood Demographics With Out-of-Hospital Cardiac Arrest Treatment and Outcomes: Where You Live May Matter. JAMA Cardiol. 2017. Oct 1;2(10):1110–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan PS, McNally B, Vellano K, et al. Association of Neighborhood Race and Income With Survival After Out-of-Hospital Cardiac Arrest. J Am Heart Assoc. 2020. Feb 18;9(4):e014178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shah KS, Shah AS, Bhopal R. Systematic review and meta-analysis of out-of-hospital cardiac arrest and race or ethnicity: black US populations fare worse. Eur J Prev Cardiol. 2014. May;21(5):619–38. [DOI] [PubMed] [Google Scholar]
- 5.Galea S, Blaney S, Nandi A, et al. Explaining racial disparities in incidence of and survival from out-of-hospital cardiac arrest. Am J Epidemiol. 2007. Sep 1;166(5):534–43. [DOI] [PubMed] [Google Scholar]
- 6.Zhao D, Post WS, Blasco-Colmenares E, et al. Racial Differences in Sudden Cardiac Death. Circulation. 2019. Apr 2;139(14):1688–1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lewey J, Choudhry NK. The current state of ethnic and racial disparities in cardiovascular care: lessons from the past and opportunities for the future. Curr Cardiol Rep. 2014;16(10):530. [DOI] [PubMed] [Google Scholar]
- 8.Reinier K, Nichols GA, Huertas-Vazquez A, et al. Distinctive Clinical Profile of Blacks Versus Whites Presenting With Sudden Cardiac Arrest. Circulation. 2015. Aug 4;132(5):380–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Henderson SO, Haiman CA, Wilkens LR, et al. Established risk factors account for most of the racial differences in cardiovascular disease mortality. PLoS One. 2007. Apr 18;2(4):e377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann N Y Acad Sci. 2010;1186:69–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Williams DR, Priest N, Anderson NB. Understanding associations among race, socioeconomic status, and health: Patterns and prospects. Health Psychol. 2016;35(4):407–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.York Cornwell E, Currit A. Racial and Social Disparities in Bystander Support During Medical Emergencies on US Streets. Am J Public Health. 2016. Jun;106(6):1049–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amen A, Karabon P, Bartram C, et al. Disparity in Receipt and Utilization of Telecommunicator CPR Instruction. Prehosp Emerg Care. 2020. Jul-Aug;24(4):544–549. [DOI] [PubMed] [Google Scholar]
- 14.Wilde ET, Robbins LS, Pressley JC. Racial differences in out-of-hospital cardiac arrest survival and treatment. Emerg Med J. 2012. May;29(5):415–9. [DOI] [PubMed] [Google Scholar]
- 15.Meaney PA, Bobrow BJ, Mancini ME, et al. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation. 2013. Jul 23;128(4):417–35. >Erratum in: Circulation. 2013 Aug 20;128(8):e120. Erratum in: Circulation. 2013 Nov 12;128(20):e408. [DOI] [PubMed] [Google Scholar]
- 16.Kleinman ME, Brennan EE, Goldberger ZD, et al. Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015. Nov 3;132(18 Suppl 2):S414–35. [DOI] [PubMed] [Google Scholar]
- 17.Wang HE, Prince DK, Stephens SW, et al. Design and implementation of the Resuscitation Outcomes Consortium Pragmatic Airway Resuscitation Trial (PART). Resuscitation. 2016. Apr;101:57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang HE, Schmicker RH, Herren H, et al. Classification of cardiopulmonary resuscitation chest compression patterns: manual versus automated approaches. Acad Emerg Med. 2015. Feb;22(2):204–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schmicker RH, Nichol G, Kudenchuk P, et al. CPR compression strategy 30:2 is difficult to adhere to, but has better survival than continuous chest compressions when done correctly. Resuscitation. 2021. Jun 5;165:31–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iwashyna TJ, Christakis NA, Becker LB. Neighborhoods matter: A population-based study of provision of cardiopulmonary resuscitation. Annals of Emergency Medicine. Volume 34, Issue 4, Part 1, October 1999, Pages 459–468. [DOI] [PubMed] [Google Scholar]
- 21.Lupton JR, Schmicker RH, Aufderheide TP, et al. Racial disparities in out-of-hospital cardiac arrest interventions and survival in the Pragmatic Airway Resuscitation Trial. Resuscitation. 2020. Oct;155:152–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008. Sep 24;300(12):1423–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Daya MR, Schmicker RH, Zive DM, et al. Out-of-hospital cardiac arrest survival improving over time: Results from the Resuscitation Outcomes Consortium (ROC). Resuscitation. 2015. Jun;91:108–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zive DM, Schmicker R, Daya M, et al. Survival and variability over time from out of hospital cardiac arrest across large geographically diverse communities participating in the Resuscitation Outcomes Consortium. Resuscitation. 2018. Oct;131:74–82. [DOI] [PubMed] [Google Scholar]
- 25.Russell JK, González-Otero DM, Leturiondo M, et al. Chest stiffness dynamics in extended continuous compressions cardiopulmonary resuscitation. Resuscitation. 2021. May;162:198–204. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


