Abstract
ABP 710 (AVSOLA®) is a biosimilar to infliximab reference product (RP), a monoclonal antibody targeting tumor necrosis factor alpha (TNFα). It is approved in the USA and Canada for all the same indications as infliximab RP. Approval of ABP 710 was based on the totality of evidence (TOE) generated using a stepwise approach to assess its similarity with infliximab RP with regard to analytical (structural and functional) characteristics, pharmacokinetic parameters, and clinical efficacy and safety. ABP 710 was shown to be analytically similar to infliximab RP including in amino acid sequence, primary peptide structure, and glycan mapping and purity. ABP 710 was also demonstrated to be similar to infliximab RP with regard to functional characterization including in vitro binding, effector functions, and signaling pathways important for the mechanisms of action for clinical efficacy in multiple indications of immune-mediated inflammatory disorders including inflammatory bowel disease (IBD), especially binding to both soluble and membrane-bound TNFα. Pharmacokinetic similarity of ABP 710 with infliximab RP was demonstrated in healthy volunteers following a single 5 mg/kg intravenous dose. Comparative clinical efficacy of ABP 710 with infliximab RP was demonstrated in patients with rheumatoid arthritis. Safety and immunogenicity were also demonstrated to be similar for both ABP 710 and the RP. Overall, the TOE supported the conclusion that ABP 710 is highly similar to infliximab RP and supported scientific justification for extrapolation to all approved indications of infliximab RP, including IBD.
Keywords: ABP 710, Biosimilar, Inflammatory bowel disease, Infliximab, Infliximab biosimilar
Key Summary Points
| ABP 710 (AVSOLA®) is a biosimilar to infliximab reference product (RP) and is approved in the USA and Canada for all the same indications as infliximab RP. |
| ABP 710 was demonstrated to be similar to infliximab RP with regard to analytical (structural and functional) characteristics, clinical pharmacokinetics in healthy volunteers, and clinical efficacy, safety, and immunogenicity in patients with rheumatoid arthritis. |
| Infliximab RP is a highly efficacious treatment for inflammatory bowel disease (IBD) and infliximab biosimilars are expected to provide additional treatment options with the potential to improve patient outcomes. |
| The totality of evidence for ABP 710 supports the scientific justification for extrapolation of indications to IBD. |
Introduction
ABP 710 (AVSOLA®; Amgen Inc., Thousand Oaks, CA, USA) is a biosimilar to infliximab reference product (RP) [1, 2]. ABP 710 is approved in the USA and Canada for all the same indications as infliximab RP including adult and pediatric Crohn’s disease (CD), adult and pediatric ulcerative colitis (UC), rheumatoid arthritis (RA), ankylosing spondylitis (AS), psoriatic arthritis (PsA), and plaque psoriasis (PsO) [3, 4]. Infliximab RP (Remicade®) is a tumor necrosis factor alpha-targeting monoclonal antibody (mAb, anti-TNFα) used to treat immune-mediated inflammatory disorders (IMIDs) [1, 2]. Such IMIDs include disease states that are clinically diverse and defined by the organ system(s) impacted by immune dysregulation. Infliximab RP was the first biological therapy to be approved for the treatment of inflammatory bowel disease (IBD) and was the first biologic agent that demonstrated efficacy in RA, AS, and PsA. Anti-TNFα therapeutics such as infliximab RP have radically changed the therapeutic approach for treating IMIDs beyond just mitigation of symptoms by driving suppression and control of the chronic inflammation which would otherwise cause irreversible damage and disability.
IMIDs are seemingly unrelated diseases linked by the common pathway of chronic inflammatory response which includes overproduction of pro-inflammatory cytokines including TNFα [5]. UC is an IBD in which mucosal inflammation is localized to the large intestine and rectum, whereas in CD transmural inflammation can affect any part of the gastrointestinal tract in a discontinuous manner, with predilection for the terminal ileum and the colon. Overall, IBD is a chronic and debilitating disease that decreases life expectancy [6], especially when diagnosed at a young age. Infliximab is highly efficacious in the treatment of IBD including CD with fistulizing disease, and in treating UC in adults and children by inducing and maintaining remission [7]. To date, infliximab RP is still perceived as the most efficacious agent to induce and maintain clinical remission and endoscopic healing when used as combination therapy (SONIC Study), as the most effective agent in UC (as evidenced from network meta-analysis), and as the only biologic with demonstrated efficacy in prospective studies in patients with perianal CD [8]. Furthermore, efficacy of infliximab RP has been demonstrated in patients with steroid-refractory acute, severe UC [9]. Since its first approval in 1998, millions of patients have benefitted from the use of infliximab RP to treat IMIDs. The safety and tolerability of infliximab RP and infliximab biosimilars in clinical trials have been favorable, with integrated safety data indicating that adverse events (AEs) such as serious infections are rare, and results on malignancy still being contentiously discussed.
While biologics such as infliximab RP have revolutionized the treatment of IMIDs [10, 11], access to such treatments has been limited; infliximab biosimilars are expected to provide additional treatment options with the potential to improve patient outcomes. Unlike small-molecule generic products which are chemically identical to the corresponding reference product (RP), biosimilars are biologics with complex structures that fold into unique three-dimensional structures, and are similar, but not identical, to the RP. The rationale behind the idea of biosimilars comes from the understanding that this category of products would provide alternative treatment options by improving access to biologics [12]. Several infliximab biosimilars are currently available: Remsima® (CT-P13; Celltrion, South Korea), Inflectra™ (CT-P13; Pfizer, USA); Infimab (BOW015; Reliance Life Sciences, India), Reneflexis® (SB2; Samsung Bioepis Co. Ltd/Merck Sharp & Dohme Corp; USA), and Avsola® (ABP 710; Amgen, Inc.; USA).
Approval of ABP 710 was based on the totality of evidence (TOE) which supports the similarity of ABP 710 with infliximab RP [3, 4, 13]. The TOE is generated to meet the criteria for the development and approval of biosimilars as required by regulatory agencies around the world. The US Food and Drug Administration (FDA) defines a biosimilar as a biologic agent that is highly similar (not withstanding minor differences in clinically inactive components) to an already approved originator biologic or RP with no clinically meaningful differences in terms of safety, purity, and potency [14]. The European Medicines Agency (EMA), an early pioneer in the development of regulatory guidance for biosimilar development and approval, as well as other regulatory authorities worldwide, also provide a similar definition for biosimilars and their guidelines consistently reflect similar requirements for the development and approval of biosimilars [15–18]. Here we present a review of the TOE that resulted in the approval of ABP 710 as a biosimilar to infliximab RP and which supports justification for extrapolation to all indications of the RP including IBD.
All studies discussed in this article are based on previously conducted studies; no new studies with human participants or animals were performed by any of the authors.
Development of ABP 710
The development of ABP 710 as a proposed biosimilar was informed by the stepwise, TOE-based guidance from both the FDA and the EMA [14, 19, 20]. The resulting ABP 710 TOE used to demonstrate biosimilarity comprised similarity studies that began with analytical characterization using state-of-the-art techniques to assess structural and functional attributes followed by non-clinical assessments including the mechanisms of action (MoA). The next step in the TOE-based development was the pharmacokinetic (PK) evaluation in healthy volunteers and then a comparative clinical study in patients with RA to confirm that there are no clinically meaningful differences in efficacy, safety, and immunogenicity.
Analytical Characterization
As recommended by regulatory guidelines, the RP for these studies was sourced from local jurisdictions including from the USA and EU such that comparisons could be made to assess the similarity of ABP 710 with the US and EU RP, as well as ensure similarity of the two sources of RP. This allowed for the establishment of the scientific bridge which then allowed the use of a single source for the RP in the comparative clinical study. It is also important to note that while infliximab RP was developed using an SP2/0 murine cell line, ABP 710 was developed using a Chinese hamster ovary (CHO) cell line [21]. CHO cell lines are now generally regarded as the state-of-the-art choice with benefits supporting both development and manufacturing [22]. Among the benefits of a CHO cell line for development is a potential for decreased immunogenicity. SP2/0 cells generate mAbs that present with glycoforms with terminal galactose-alpha-1,3-galactose (α-Gal) and N-glycolylneuraminic acid (NGNA) [23] but CHO cells do not. Since a large proportion of the human population has been reported to have pre-existing antibodies with reactivity against α-Gal and NGNA, this could increase the risk of reaction to the α-Gal and NGNA glycans formed on antibodies in an SP2/0 murine cell line compared to a CHO cell line [24].
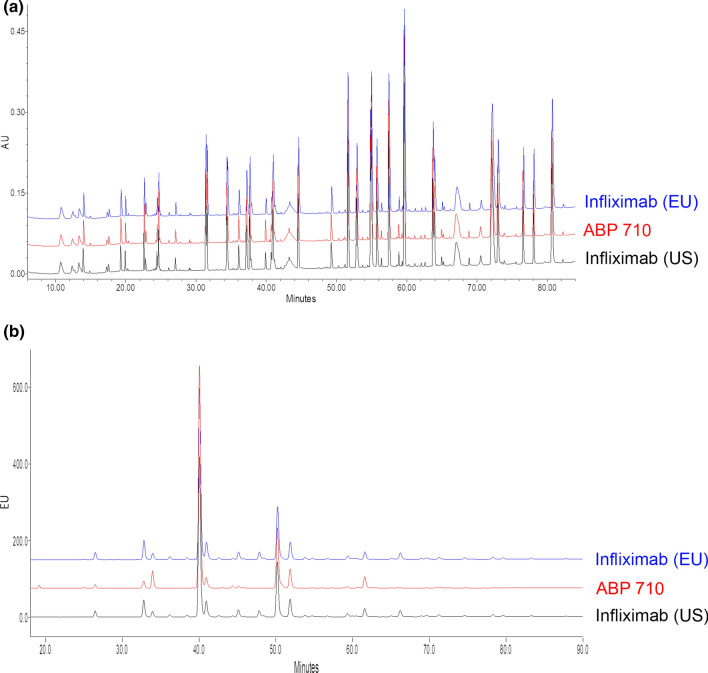
As pointed out by Duivelshof et al. [25], there is an increasing importance of comprehensive analytical platforms for extensive characterization and then integration of these results to improve the design and analysis of clinical studies with the aim of increasing the power to support similarity [26, 27]. To assess the analytical similarity of ABP 710 with infliximab RP, detailed identification and comparisons of critical quality attributes (CQAs) were used to evaluate similarity in biochemical and biophysical attributes. ABP 710 was demonstrated to be analytically similar to infliximab RP from both sources for assessments which included primary structure (intact molecular mass, reduced and deglycosylated molecular mass, amino acid sequence, and post-translational modifications [PTMs] including glycan structure), higher-order structure, particles and aggregates, product-related substances and impurities, and general properties including those of the finished drug product [21]. The overlays of the peptide and glycan maps depicted in Fig. 1 confirm similarity of ABP 710 with the RP. The minor differences observed in physiochemical attributes and in some PTMs, such as the glycan profile and charge variants, were consistent with expectations due to the change in cell line from Sp2/0 for the RP to CHO for ABP 710. For example, ABP 710 does not contain α-galactosylation and NGNA sialyation residues. This is as expected owing to the use of the CHO cell line, while such residues are detectable albeit in low levels in infliximab RP. These differences did not impact clinical efficacy and safety [28]. Comprehensive biological characterization was used to verify that these mostly minor differences did not translate into functional differences; this was further confirmed on the basis of results from clinical evaluation (discussed below).
Fig. 1.
a Reduced tryptic peptide map; b HILIC glycan map of ABP 710 and infliximab reference product (RP) sourced from the EU and US. Reproduced from Saleem et al. [21]. https://www.creativecommons.org/licenses/by/4.0/. HILIC hydrophilic interaction chromatography
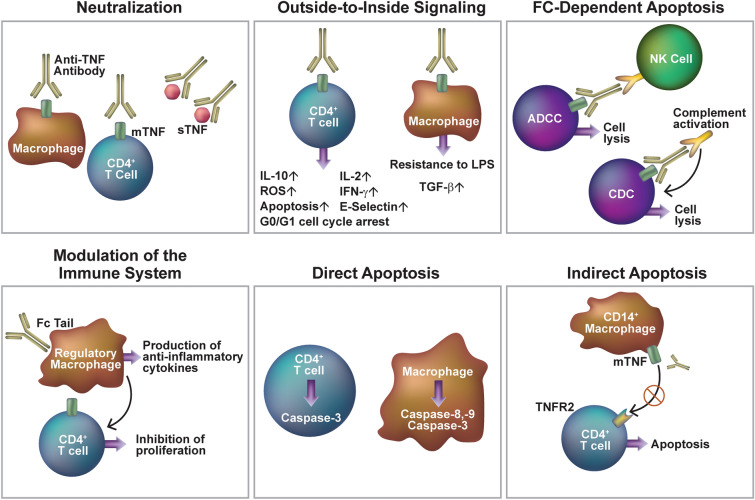
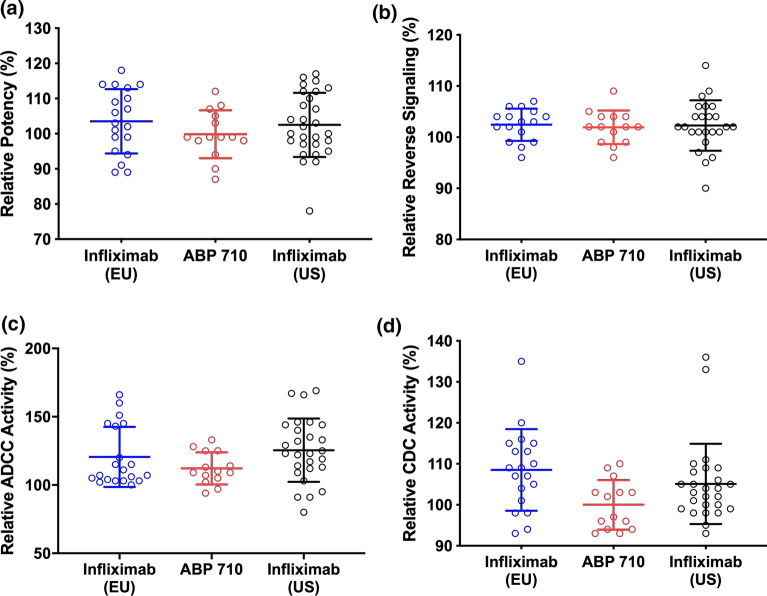
The biological activity of ABP 710 was demonstrated to be functionally similar to infliximab RP on the basis of assessments focused on the biological properties mediated by target and receptor binding to suppress ongoing inflammation. This MoA involves the inhibition of binding of both the membrane-bound TNFα (mbTNFα) and soluble TNFα (sTNFα) [29, 30] and subsequent neutralization of pro-inflammatory biological activity (Fig. 2). Neutralization also occurs through downstream effector functions including antibody-dependent cell-mediated cytotoxicity (ADCC) and complement-dependent cytotoxicity (CDC) through the Fc-containing portion of the antibody, apoptosis through reverse signaling in mbTNFα-expressing cells, and antibody-dependent cellular phagocytosis (ADCP) with mbTNFα-expressing cells. For infliximab RP, Fc-mediated effector functions are considered to be CQAs [31] and any differences in afucosylated glycan levels can potentially impact ADCC which is considered to be one of the known TNFα MoAs [32]. Furthermore, ABP 710 was shown to be similar to infliximab RP with regard to in vitro binding to FcRn and FcγRIIIa. Figure 3a demonstrates similarity of ABP 710 with infliximab RP for potency to inhibit sTNFα-induced apoptosis. Figure 3b depicts the similarity of the induction of apoptosis as measured through direct activation of an mbTNFα-specific reverse signaling pathway downstream of binding to mbTNFα which leads to apoptosis. Figure 3c, d demonstrate the similarity of ABP 710 with infliximab RP for in vitro effector function activities including ADCC and CDC. These functional assessments reflect on the key MoAs as they relate to activity in the treatment of IMIDs in general, and also reflect on the biological functions underlying efficacy in all indications for which infliximab RP is approved and which are complex and may not be the same for each indication [21, 33–35]. With the confirmation of similarity in analytical (structural and functional) characteristics, the development of ABP 710 advanced to the evaluation of clinical PK/pharmacodynamics (PD).
Fig. 2.
Mechanism of action of anti-tumor necrosis factor antibodies in inflammatory bowel disease. Schematic illustration of different modes of action of anti-TNF antibodies in inflammatory bowel diseases. Modified from Billmeier et al. [30]. https://www.creativecommons.org/licenses/by-nc/4.0/. Fc fragment crystallizable region of the antibody, IL interleukin, IFN interferon, LPS lipopolysaccharide, ROS reactive oxygen species, TGF transforming growth factor, TNF tumor necrosis factor, mTNF membrane-bound TNF, sTNF soluble TNF, TNFR TNF receptor, NK cell natural killer cell, ADCC antibody-dependent cellular cytotoxicity, CDC complement-dependent cytotoxicity
Fig. 3.
Functional assessment of Fab-mediated activities for ABP 710 and infliximab reference product (RP) sourced from the EU and US. a Inhibition of sTNFα-induced apoptosis in U937 (potency); b Reverse signaling developed as a measure of apoptosis; c NK92 ADCC activity; d CDC activity. Individual data points, the mean, and ± one standard deviation are shown. Reproduced from Saleem et al. [21]. https://www.creativecommons.org/licenses/by/4.0/. ADCC antibody-dependent cellular cytotoxicity, CDC complement-dependent cytotoxicity, Fab antigen-binding fragment of antibody, sTNF soluble TNF
PK/PD Assessment
As the next step in biosimilar development, PK/PD assessments are important not only to establish drug exposure and PK and PD similarity between the biosimilar and the RP but also to understand the comparative safety and immunogenicity of the proposed biosimilar and its RP. Additionally, to support extrapolation of indications, an understanding of PK and MoA is imperative. The clinical PK/PD of ABP 710 was evaluated in healthy volunteers; this patient population is considered to comprise a homogeneous immune-competent population which permits a rigorous comparison of the proposed biosimilar and the RP, thereby providing results without the influence of confounding factors. Once again, to satisfy the regulatory requirement for establishing a scientific bridge, for this study the RP was sourced from the USA and EU. A randomized, single-blind, single-dose, study (5 mg/kg; n = 50 per treatment group) demonstrated the PK similarity of ABP 710 with infliximab RP (see Fig. 4); all PK parameters including AUCmax, AUCinf, Cmax, Tmax, and T1/2 were similar [36]. Using an average bioequivalence approach, all 90% confidence intervals for the ratios of least-squares geometric means (GMs) of AUCinf, Cmax, and AUClast were found to be fully contained within the prespecified standard PK equivalence criteria range of 0.80–1.25 for which bioequivalence was evaluated. Safety and immunogenicity were also found to be comparable with similar incidence of treatment-related AEs (ABP 710, 83.7%; RP US, 86.0%; RP EU, 83.7%), similar incidence of rate of binding ADAs through the end of the study—day 57 (ABP 710, 39.6%; RP US, 32.0%; RP EU, 27.1%), and similar incidence of neutralizing ADAs (ABP 710, 12.5%; RP US, 10.0%; RP EU, 18.8%) in ABP 710 compared with the RP in this study.
Fig. 4.
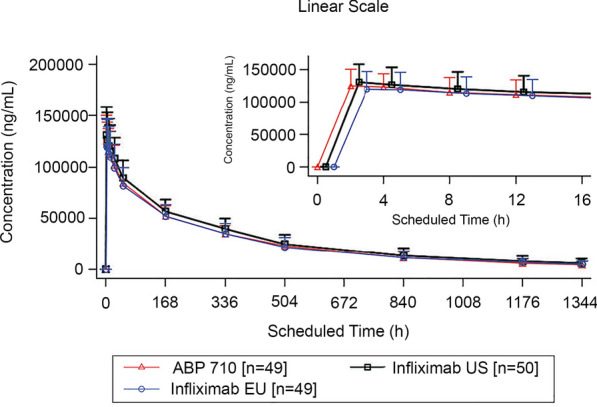
Pharmacokinetics (mean serum concentrations* vs. time profiles) of ABP 710 and infliximab reference product (RP) dosed at 5 mg/kg i.v. in healthy volunteers. Reproduced from Chow et al. [36]. https://www.creativecommons.org/licenses/by-nc/4.0/. *Concentration values below the limit of quantification are presented as 0 and included as such in the calculation of means (± SD)
Clinical Evaluation
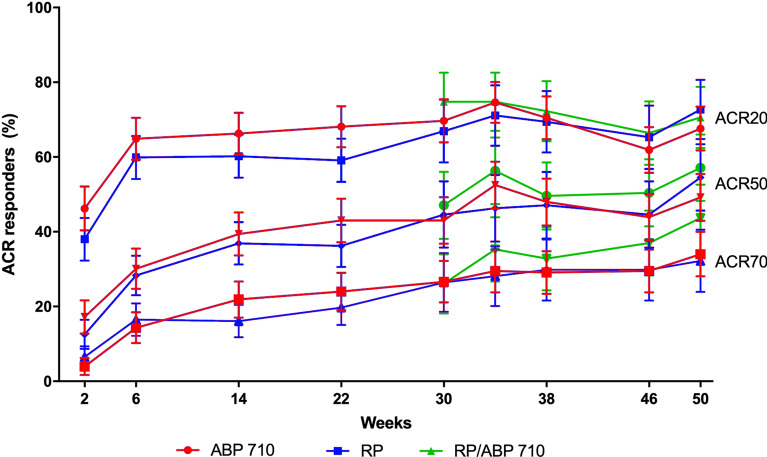
The final step in the development of a proposed biosimilar is a comparative clinical trial conducted in a representative indication ideally using sensitive endpoints to assess for clinically meaningful differences. Similarity of ABP 710 with infliximab RP with respect to efficacy, safety, and immunogenicity in patients with moderate to severe RA was demonstrated in a randomized, double-blind, active-controlled, multiple-dose, comparative, 50-week clinical equivalence study in patients with moderate to severe active RA with inadequate response to methotrexate (MTX) [28]. Patients (n = 279 for each treatment group) were randomized to receive 3-mg/kg infusions of ABP 710 or RP at predetermined intervals based on initial randomization and then following re-randomization at week 22. At week 22, patients receiving ABP 710 continued to receive ABP 710 while those in the RP arm were re-randomized in a 1:1 ratio to either receive ABP 710 or the RP for the remainder of the study. Overall results demonstrated that there were no clinically meaningful differences between ABP 710 and infliximab RP. The estimated response difference (RD) of achieving a 20% improvement from baseline in the American College of Rheumatology core set of measurements (ACR20) at week 22, the primary endpoint, was 9.37% with 90% CI 2.67%, 15.96%. While the lower (non-inferiority) bound was not exceeded, the upper (non-superiority) bound exceeded the pre-specified margin by 0.96%, and post hoc analyses were consistent with both non-inferiority and non-superiority. When covariates identified to be predictive of ACR20 by a stratified conditional logistic regression were used to adjust for the impact of random imbalance between the two treatment arms in baseline demographic and disease characteristics, the resulting estimates of RD of ACR20 at week 22 and the associated 90% CIs were narrowed such that both the lower and upper bounds were contained within the prespecified equivalence margin. Further, additional efficacy endpoints including changes from baseline in Disease Activity Score 28-joint count-CRP (DAS28-CRP) and the RD for ACR20, ACR50, and ACR70 (20%, 50%, 70% improvement in ACR core set of measurements) response rates across time, and hybrid ACR evaluations also support the conclusion that there are no clinically meaningful differences. See Fig. 5 for ACR20, ACR50, and ACR70 across time. Of note, trough serum concentrations were similar between groups across the entire study, indicating that exposure was similar between treatment groups.
Fig. 5.
Percentage of patients achieving ACR20, ACR50, and ACR70 by study week, ± 95% CI. Reproduced from Genovese et al. [28]. https://www.creativecommons.org/licenses/by/4.0/. ACR20, ACR50, and ACR70 are the 20%, 50%, and 70% improvement, respectively, from baseline in the American College of Rheumatology core set of measurements. CI confidence interval, RP reference product
Overall safety and immunogenicity were similar between treatment groups and were not impacted by the single transition from infliximab RP to ABP 710 (referred to as RP/ABP 710; see Table 1). AEs were similar between treatment groups. The highest subject incidence rates of AEs were infections and infestations and were similar in the two groups. Overall, safety events were consistent with the known safety profile of infliximab with no new or unexpected safety signals. Binding ADA incidence at week 22 of patients with a negative or no result before week 22, ADA results by week 50 and post week 22 of patients with a negative or no result before week 22, and ADA results by week 50 are also shown in Table 1.
Table 1.
Safety and immunogenicity of ABP 710 and infliximab reference product (RP) in patients with rheumatoid arthritis (RA). Modified from Genovese et al. [28]. https://www.creativecommons.org/licenses/by/4.0/
| Safety | Through week 22 | Post week 22 (after single transition) | |||
|---|---|---|---|---|---|
| ABP 710 | RP | ABP 710/ABP 710 | RP/RP | RP/ABP 710 | |
| Any AE, n (%) | 144 (51.8) | 138 (49.6) | 130 (53.9) | 69 (57.0) | 69 (58.0) |
| Any grade ≥ 3 AE, n (%) | 12 (4.3) | 14 (5.0) | 18 (7.5) | 7 (5.8) | 5 (4.2) |
| Any AE with outcome of death, n (%) | 1 (0.4) | 1 (0.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Any AE leading to infusion delay/not administered, n (%) | 30 (10.8) | 30 (10.8) | 19 (7.9) | 11 (9.1) | 8 (6.7) |
| Infusion reactions including hypersensitivity, n (%) | 22 (7.9) | 37 (13.3) | 20 (8.3) | 12 (9.9) | 7 (5.9) |
| Upper respiratory tract infection, n (%) | 17 (6.1) | 18 (6.5) | 23 (9.5) | 9 (7.4) | 14 (11.8) |
| Hematological reaction, n (%) | 11 (4.0) | 5 (1.8) | 10 (4.1) | 6 (5.0) | 8 (6.7) |
| Hepatotoxicity, n (%) | 9 (3.2) | 9 (3.2) | 11 (4.6) | 4 (3.3) | 0 (0.0) |
| Serious infections, n (%) | 2 (0.7) | 4 (1.4) | 5 (2.1) | 1 (0.8) | 3 (2.5) |
| Malignancies, n (%) | 2 (0.7) | 2 (0.7) | 2 (0.8) | 0 (0.0) | 0 (0.0) |
| Immunogenicity | Antibody positive by week 22 with a negative or no result at baseline | Antibody positive post week 22 with a negative or no result at week 22 (after single transition) | |||
|---|---|---|---|---|---|
| ABP 710 | RP | ABP 710/ABP 710 | RP/RP | RP/ABP 710 | |
| Number of patients | 261 | 264 | 96 | 45 | 45 |
| Binding antibody, n (%) | 149 (57.1) | 160 (60.6) | 29 (30.2) | 19 (42.2) | 18 (40.0) |
| Neutralizing antibody, n (%) | 47 (18.0) | 55 (20.8) | 3 (3.1) | 1 (2.2) | 2 (4.4) |
AE adverse event
Extrapolation
Extrapolation is a concept that is unique to biosimilars and allows for approval and use of the proposed biosimilar in indications that the RP is approved for even though the proposed biosimilar has not been clinically evaluated in these patient populations. Approval for use in multiple indications via extrapolation supports the abbreviated pathway for biosimilars development and approval. Per FDA guidance, extrapolation is based on all available data, the previous finding of safety and efficacy for the approved indications for the RP, and knowledge and consideration of various scientific factors for each indication. It is important to note that extrapolation is based on the TOE that supports similarity between the proposed biosimilar and its RP and not just on the similarity of clinical efficacy in the evaluated representative indication. This scientific justification supports extrapolation when the purported MoA for the additional indications is the same as that for the indication evaluated in the comparative clinical trial of the proposed biosimilar. It is also important to note that approval for use based on extrapolation is limited to indications that are not protected by regulatory exclusivities.
It is particularly important to assess similarity of proposed biosimilars within all relevant MoAs to support justification for extrapolated indications. As an anti-TNFα therapeutic, infliximab RP is efficacious in the mitigation of ongoing inflammation in a variety of IMIDs that are otherwise seemingly unrelated diseases other than being linked by the common pathway of chronic inflammatory response which includes overproduction of pro-inflammatory cytokines including TNF [5]. Neutralization of TNFα happens through a process that includes binding to and neutralization of sTNFα and mbTNFα and mediation of downstream Fc-mediated effector functions (Fig. 2). The binding and neutralizing activities of sTNFα are critical for efficacy in all IMIDs while the relative importance of other MoAs has been suggested for particular IMIDs [32]. For example, binding to mbTNFα by anti-TNFα antibodies can induce reverse signaling in some mbTNFα-expressing cell types which results in Fc-dependent apoptosis [37] through ADCC and CDC which may be involved in clinical efficacy in IBD [30, 38–40].
Also important for extrapolated indications is confirmation of similarity of mechanisms underlying variability in PK and with regard to different patient populations, and in patients across time for long-term treatment. The latter is especially important in patients with IBD where both high inter-individual variability in efficacy and waning efficacy over time can occur. The PK of intravenously dosed infliximab RP is well characterized and typical of a mAb, with clearance from circulation occurring by catabolism through interaction with Brambell (FcRB) or neonatal Fc (FcRn) receptors [41, 42]; catabolism is increased in high inflammatory states [43]. Proteolytic catabolism occurs through Fc gamma receptors (FcγRs) and antibody salvage and recirculation are mediated by FcRn [41, 42]. Polymorphisms in FcγRs may impact the PK of infliximab RP [44]. Therefore, similarity of ABP 710 with the RP in these mechanisms of action provides as highlighted here support for the approval of use in IBD as an extrapolated indication.
Discussion
In this review we have described the TOE that supported the approval of ABP 710 as a biosimilar to infliximab RP. ABP 710 has been shown to be analytically similar to infliximab RP with regard to primary structure, higher-order structure, potency, general properties, and biological activities. Importantly, ABP 710 is similar to infliximab RP with regard to Fc-mediated binding and effector function, as well as MoAs including binding to sTNFα, binding to mbTNFα, inhibition of sTNFα-induced apoptosis, and reverse signaling via induction of apoptosis in mbTNFα-expressing cells. Clinical PK along with safety and tolerability has also been demonstrated to be similar between ABP 710 and infliximab RP in healthy subjects. Further, in a comparative clinical study, no clinically meaningful differences in efficacy, safety, and immunogenicity were observed in patients with moderate-to-severe RA. Furthermore, results of MoA studies supported extrapolation to additional indications including IBD. Use of infliximab biosimilars has become increasingly well established since the approval of CT-P13 in 2016 and the availability of additional infliximab biosimilars since then. ABP 710 offers another treatment alternative among infliximab biosimilars.
The approval of infliximab biosimilars, including ABP 710 for use in IBD, is based on extrapolation. Therefore, it is important to evaluate the real-world use of these products in the IBD patient population. These data would allow one to build confidence in the use of biosimilars in extrapolated indications. As ABP 710 was recently approved by the FDA, there is relatively limited real-world data of its use in IBD. However, with the availability of several infliximab biosimilars there is an abundance of real-world evidence of use of these products in IBD. These include the NOR-SWITCH and DANBIO studies, as well as several systematic reviews and meta-analyses [45–48]. The data reported in these real-world studies provide insight into the effectiveness and safety of infliximab biosimilars in all indications for which these products are approved, including IBD.
Even with additional treatment options, successful long-term treatment for patients with IBD remains a challenge because the known underlying complexities of IBD including host genetics, immune function, gut microbiome, and environmental factors can be confounding for tracking therapeutic benefit and for which the influence of precision medicine may offer new opportunities. Currently, artificial intelligence, machine learning, and systems biology are being applied to IBD research to potentially enable patient stratification based on disease subtypes and severity, progression of disease, and treatment response [49]. Particularly important for long-term infliximab RP treatment is the prediction of response and dose to manage developing ADAs, which may be associated with increased rates of clearance, decreased efficacy, and increased risk of infusion-related reactions. Population PK and PK/PD modeling for infliximab RP have identified body weight and baseline infliximab RP clearance as early predictors of ADA formation; both these factors are measurable at baseline and early in treatment and are useful early predictors of ADA formation [50].
Conclusion
The TOE for ABP 710 which includes analytical (structural and functional) characteristics, clinical PK in healthy volunteers, and efficacy, safety, and immunogenicity in patients with RA confirms that ABP 710 is similar to infliximab RP and supports justification for extrapolation to all indications of the RP including IBD. Among the armamentarium of infliximab biosimilars, ABP 710 provides an additional treatment option for patients with IBD.
Acknowledgements
Funding
This work as well as the journal’s Rapid Service and Open Access Fees were funded by Amgen Inc., Thousand Oaks, CA, USA.
Medical Writing, Editorial, and Other Assistance
Medical writing assistance was provided by Sonya G. Lehto, PhD, Amgen, Inc. Assistance with editing, graphics, and submission was provided by Innovation Communications Group, New York, NY and paid for by Amgen Inc.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, contributed to the concept for the review and take responsibility for the integrity of the article. The first draft of the manuscript was written by Sonya G. Lehto, and all authors commented on previous versions of the manuscript and have read and approved the final manuscript.
Author Contributions
All authors provided input, reviewed, and approved the final manuscript.
Disclosures
Walter Reinisch, Stanley Cohen, Majed Khraishi, and Jean-Frederic Colombel have participated as investigators for Amgen Inc. for studies discussed in this review. Monica Ramchandani was an employee of Amgen at the time of this work; she is a current stockholder of Amgen Inc. Jennifer Liu, Vincent Chow, and Janet Franklin are employees and stockholders of Amgen Inc.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
References
- 1.Remicade® (infliximab). Full prescribing information. Horsham: Janssen Biotech, Inc.; 2020.
- 2.Remicade® (infliximab). Summary of product characteristics. Leiden: Janssen Biologics B.V.; 2020.
- 3.AVSOLA® (infliximab-axxq) for injection, for intravenous use. Full prescribing information. Thousand Oaks: Amgen Inc.; 2021.
- 4.PrAVSOLA™ (infliximab for injection). Product monograph. Mississauga: Amgen Canada Inc.; 2020.
- 5.Smolen JS, Emery P. Infliximab: 12 years of experience. Arth Res Ther. 2011;13:S2. doi: 10.1186/1478-6354-13-S1-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jess T, Frisch M, Simonsen J. Trends in overall and cause-specific mortality among patients with inflammatory disease from 1982. Clin Gastroenterol Hepatol. 2013;11:43–48. doi: 10.1016/j.cgh.2012.09.026. [DOI] [PubMed] [Google Scholar]
- 7.Roumeguère P, Bouchard D, Pigot F, et al. Combined approach with infliximab, surgery, and methotrexate in severe fistulizing anoperineal Crohn's disease: results from a prospective study. Inflamm Bowel Dis. 2011;17:69–76. doi: 10.1002/ibd.21405. [DOI] [PubMed] [Google Scholar]
- 8.Lin Z, Bai Y, Zheng P. Meta-analysis: efficacy and safety of combination therapy of infliximab and immunosuppressives for Crohn’s disease. Eur J Gastroenterol Hepatol. 2011;23:1100–1110. doi: 10.1097/MEG.0b013e32834b9544. [DOI] [PubMed] [Google Scholar]
- 9.Laharie D, Bourreille A, Branche J, et al. Evolution of endoscopic lesions in steroid-refractory acute severe ulcerative colitis responding to infliximab or cyclosporine. Clin Gastroenterol Hepatol. 2021;19:1180–1188. doi: 10.1016/j.cgh.2020.08.001. [DOI] [PubMed] [Google Scholar]
- 10.Kuek A, Hazleman BL, Östör AJ. Immune-mediated inflammatory diseases (IMIDs) and biologic therapy: a medical revolution. Postgrad Med J. 2007;83:251–260. doi: 10.1136/pgmj.2006.052688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.D’Haens GR, van Deventer S. 25 years of anti-TNF treatment for inflammatory bowel disease: lessons from the past and a look to the future. Gut. 2021;70:1396–1405. doi: 10.1136/gutjnl-2019-320022. [DOI] [PubMed] [Google Scholar]
- 12.Kim H, Alten R, Avedano L, et al. The future of biosimilars: maximizing benefits across immune-mediated inflammatory diseases. Drugs. 2020;80:99–113. doi: 10.1007/s40265-020-01256-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.US Food and Drug Administration. Drug Approval Package: AVSOLA. Jan 2021. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2019/761086Orig1s000TOC.cfm. Accessed 28 Sept 2021.
- 14.US Food and Drug Administration. Guidance document. Scientific considerations in demonstrating biosimilarity to a reference product (final guidance). 2015. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/scientific-considerations-demonstrating-biosimilarity-reference-product. Accessed 9 Apr 2020.
- 15.European Medicines Agency (EMA). Guideline on similar biological medicinal products. 2014. https://www.ema.europa.eu/en/similar-biological-medicinal-products. Accessed 16 Apr 2021.
- 16.WHO 2009 World Health Organization (WHO). Guidelines on evaluation of similar Biotherapeutic Products (SBPs), Annex 2, Technical Report Series No. 977, 2009. https://www.who.int/biologicals/publications/trs/areas/biological_therapeutics/TRS_977_Annex_2.pdf?ua=1. Accessed 16 Apr 2021.
- 17.Ministry of Health Labour and Welfare (MHLW). Interim translation. Guidelines for the quality, safety and efficacy assurance of follow-on biologics. No 0304004. MHLW; Tokyo, Japan (2009). http://www.pmda.go.jp/files/000153851.pdf. Accessed 3 June 2021.
- 18.Health Canada. Guidance document: Information and submission requirements for biosimilar biologic drugs. 2016. https://www.canada.ca/en/health-canada/services/drugs-health-products/biologics-radiopharmaceuticals-genetic-therapies/applications-submissions/guidance-documents/information-submission-requirements-biosimilar-biologic-drugs-1.html. Accessed 16 Apr 2021.
- 19.U.S. Food & Drug Administration. Development of therapeutic protein biosimilars: comparative analytical assessment and other quality-related considerations. Guidance for industry. Draft guidance. May 2019. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/development-therapeutic-protein-biosimilars-comparative-analytical-assessment-and-other-quality. Accessed 28 Sept 2021.
- 20.European Medicines Agency. Guideline on similar biological medicinal products containing biotechnology-derived proteins as active substance: quality issues (revision 1). May 2014. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-similar-biological-medicinal-products-containing-biotechnology-derived-proteins-active_en-0.pdf. Accessed 28 Sept 2021.
- 21.Saleem R, Cantin G, Wikström M, et al. Analytical and functional similarity assessment of ABP 710, a biosimilar to infliximab reference product. Pharm Res. 2020;37:114. doi: 10.1007/s11095-020-02816-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee JS, Park JH, Ha TK, et al. Revealing key determinants of clonal variation in transgene expression in recombinant CHO cells using targeted genome editing. ACS Synth Biol. 2018;7:2867–2878. doi: 10.1021/acssynbio.8b00290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Raju TS. Glycosylation variations with expression systems and their impact on biological activity of therapeutic immunoglobulins. BioProcess Int. 2003;April:44–53. [Google Scholar]
- 24.Ghaderi D, Taylor RE, Padler-Karavani V, Diaz S, Varki A. Implications of the presence of N-glycolylneuraminic acid in recombinant therapeutic glycoproteins. Nat Biotechnol. 2010;28:863–867. doi: 10.1038/nbt.1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Duivelshof BL, Jiskoot W, Beck A, Veuthey J-L, Guillarme D, D’Atri V. Glycosylation of biosimilars: recent advances in analytical characterization and clinical implications. Anal Chim Acta. 2019;1089:1–18. doi: 10.1016/j.aca.2019.08.044. [DOI] [PubMed] [Google Scholar]
- 26.Rogers RS, Nightlinger NS, Livingston B, Campbell P, Bailey R, Balland A. Development of a quantitative mass spectrometry multi-attribute method for characterization, quality control testing and disposition of biologics. MAbs. 2015;7:881–890. doi: 10.1080/19420862.2015.1069454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zeng D, Pan J, Hu K, Chi E, Lin DY. Improving the power to establish clinical similarity in a phase 3 efficacy trial by incorporating prior evidence of analytical and pharmacokinetic similarity. J Biopharm Stat. 2018;28:320–332. doi: 10.1080/10543406.2017.1397012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Genovese MC, Sanchez-Burson J, Oh MS, Balazs E. Comparative clinical efficacy and safety of the proposed biosimilar ABP 710 with infliximab reference product in patients with rheumatoid arthritis. Arthritis Res Ther. 2020;22:60. doi: 10.1186/s13075-020-2142-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grell M, Douni E, Wajant H, et al. The transmembrane form of tumor-necrosis-factor is the prime activating ligand of the 80 kDa tumor-necrosis-factor receptor. Cell. 1995;83:793–802. doi: 10.1016/0092-8674(95)90192-2. [DOI] [PubMed] [Google Scholar]
- 30.Billmeier U, Dieterich W, Neurath M, Atreya R. Molecular mechanism of action of anti-tumor necrosis factor antibodies in inflammatory bowel diseases. World J Gastroenterol. 2016;22:9300–9313. doi: 10.3748/wjg.v22.i42.9300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reusch D, Tejada ML. Fc glycans of therapeutic antibodies as critical quality attributes. Glycobiology. 2015;25:1325–1334. doi: 10.1093/glycob/cwv065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Horiuchi T, Mitoma H, Harashima S-I, Tsukamoto H, Shimoda T. Transmembrane TNF-α: structure, function and interaction with anti-TNF agents. Rheumatology. 2010;49:1215–1228. doi: 10.1093/rheumatology/keq031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vande Casteele N, Sandborn WJ. IBD: indication extrapolation for anti-TNF biosimilars. Nat Rev Gastroenterol Hepatol. 2015;12:373–374. doi: 10.1038/nrgastro.2015.104. [DOI] [PubMed] [Google Scholar]
- 34.Ben-Horin S, Vande Casteele N, Schreiber S, Lakatos PL. Biosimilars in inflammatory bowel disease: facts and fears of extrapolation. Clin Gastroenterol Hepatol. 2016;14:1685–1696. doi: 10.1016/j.cgh.2016.05.023. [DOI] [PubMed] [Google Scholar]
- 35.Vos AC, Wildenberg ME, Duijvestein M, Verhaar AP, van den Brink G, Hommes DW. Anti-tumor necrosis factor-α antibodies induce regulatory macrophages in an Fc region-dependent manner. Gastroenterology. 2011;140:221–230. doi: 10.1053/j.gastro.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 36.Chow V, Oh M, Gessner MA, Fanjiang G. Pharmacokinetic similarity of ABP 710, a proposed biosimilar to infliximab: results from a randomized, single-blind, single-dose, parallel-group study in healthy subjects. Clin Pharmacol Drug Dev. 2020;9(2):246–255. doi: 10.1002/cpdd.738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mitoma H, Horiuchi T, Tsukamoto H, et al. Mechanisms for cytotoxic effects of anti-tumor necrosis factor agents on transmembrane tumor necrosis factor α-expressing cells: comparison among infliximab, etanercept, and adalimumab. Arthritis Rheum. 2008;58:1248–1257. doi: 10.1002/art.23447. [DOI] [PubMed] [Google Scholar]
- 38.Peake STC, Bernardo D, Mann ER, Al-Hassi HO, Knight SC, Hart AL. Mechanisms of action of anti-tumor necrosis factor α agents in Crohn's disease. Inflamm Bowel Dis. 2013;19:1546–1555. doi: 10.1097/MIB.0b013e318281333b. [DOI] [PubMed] [Google Scholar]
- 39.Levin AD, Wildenberg ME, van den Brink GR. Mechanism of action of anti-TNF therapy in inflammatory bowel disease. J Crohns Colitis. 2016;10:989–997. doi: 10.1093/ecco-jcc/jjw053. [DOI] [PubMed] [Google Scholar]
- 40.Chang S, Hanauer S. Extrapolation and interchangeability of infliximab and adalimumab in inflammatory bowel disease. Curr Treat Options Gastroenterol. 2017;15:53–70. doi: 10.1007/s11938-017-0122-6. [DOI] [PubMed] [Google Scholar]
- 41.Wang W, Wang EQ, Balthasar JP. Monoclonal antibody pharmacokinetics and pharmacodynamics. Clin Pharmacol Ther. 2008;84:548–558. doi: 10.1038/clpt.2008.170. [DOI] [PubMed] [Google Scholar]
- 42.Ordas I, Mould DR, Feagan BG, Sandborn WJ. Anti-TNF monoclonal antibodies in inflammatory bowel disease: pharmacokinetics-based dosing paradigms. Clin Pharmacol Ther. 2012;91:635–646. doi: 10.1038/clpt.2011.328. [DOI] [PubMed] [Google Scholar]
- 43.Fasanmade AA, Adedokun OJ, Ford J, et al. Population pharmacokinetic analysis of infliximab in patients with ulcerative colitis. Eur J Clin Pharmacol. 2009;65:1211–1228. doi: 10.1007/s00228-009-0718-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Billiet T, Dreesen E, Cleynen I, et al. A genetic variation in the neonatal Fc-receptor affects anti-TNF drug concentrations in inflammatory bowel disease. Am J Gastroenterol. 2016;111:1438–1445. doi: 10.1038/ajg.2016.306. [DOI] [PubMed] [Google Scholar]
- 45.Jørgensen KK, Olsen IC, Goll GL, NOR-SWITCH Study Group et al. Switching from originator infliximab to biosimilar CT-P13 compared with maintained treatment with originator infliximab (NOR-SWITCH): a 52-week, randomized, double-blind, non-inferiority trial. Lancet. 2017;389:2304–2316. doi: 10.1016/S0140-6736(17)30068-5. [DOI] [PubMed] [Google Scholar]
- 46.Glintborg B, Loft AG, Omerovic E, et al. To switch or not to switch: results of a nationwide guideline of mandatory switching from originator to biosimilar etanercept. One-year treatment outcomes in 2061 patients with inflammatory arthritis from the DANBIO registry. Ann Rheum Dis. 2019;78:192–200. doi: 10.1136/annrheumdis-2018-213474. [DOI] [PubMed] [Google Scholar]
- 47.Høivik ML, Buer LC, Cvancarova M, et al. Switching from originator to biosimilar infliximab—real world data of a prospective 18 months follow-up of a single-centre IBD population. Scand J Gastroenterol. 2018;53:692–699. doi: 10.1080/00365521.2018.1463391. [DOI] [PubMed] [Google Scholar]
- 48.Argüelles-Arias F, Guerra Veloz MF, Perea Amarillo R, et al. Switching from reference infliximab to CT-P13 in patients with inflammatory bowel disease: 12 months results. Eur J Gastroenterol Hepatol. 2017;29:1290–1295. doi: 10.1097/MEG.0000000000000953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Seyed Tabib NS, Madgwick M, Sudhakar P, Verstockt B, Korcsmaros T, Vermeire S. Big data in IBD: big progress for clinical practice. Gut. 2020;69:1520–1532. doi: 10.1136/gutjnl-2019-320065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Eser A, Reinisch W, Schreiber S, Ahmad D, Boulos S, Mould DR. Increased induction infliximab clearance predicts early antidrug antibody detection. J Clin Pharmacol. 2021;61:224–233. doi: 10.1002/jcph.1732. [DOI] [PMC free article] [PubMed] [Google Scholar]