Abstract
Community-acquired MRSA (CA-MRSA) is potentially a new emerging pathogen with most strains susceptible to many antimicrobials except for β-lactam antibiotics. We retrospectively reviewed MRSA isolates during a 20-month study period (January 1998 through August 1999) and investigated those that were clindamycin susceptible. Patients were not considered to harbor CA-MRSA if they had been admitted to a hospital within the preceding 2 years or if their isolate had been obtained more than 72 h after admission. There were 2,817 S. aureus isolates, with 1,071 (38%) being MRSA. Of these 1,071 isolates, 161 were clindamycin susceptible; these were recovered from 81 patients. Of these 81 patients, 20 appeared to have community-acquired strains, but only 2 could be confirmed as having CA-MRSA.
Community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) appears to be a new emerging pathogen, with recent reports coming from various areas in the United States (1, 4–7, 10), Australia (9, 12), and Canada (3). S. aureus is an important human pathogen that has been recognized for decades; however, the percentage of S. aureus isolates that are methicillin resistant has increased from 2% in 1974 to nearly 50% in 1997 in some areas (8). The emergence of CA-MRSA is a recent occurrence, raising considerable concern since this type of S. aureus would cause infections difficult to treat in the outpatient setting and would markedly increase the need for vancomycin therapy. O'Brien and colleagues related the incidence of CA-MRSA to be as high as 42% in certain rural communities in Western Australia (12). The published studies from Chicago have been based mostly in pediatric populations (5, 7), as was the recent report of the Centers for Disease Control and Prevention of four deaths due to CA-MRSA (4). The actual prevalence of CA-MRSA in communities in the United States is unknown. Interestingly, CA-MRSA isolates appear to uniquely differ from the nosocomial MRSA isolates in that they are generally more susceptible to multiple antimicrobial agents other than β-lactam antibiotics. Given their different antimicrobial susceptibility patterns, the CA-MRSA isolates may not simply be hospital strains that have been transferred into the community. Clindamycin susceptibility has been shown to have a very significant correlation with CA-MRSA (5). Our study examined whether clindamycin susceptibility could be a specific surrogate marker for CA-MRSA in patients served by our institution. Using this marker, we also assessed the number of CA-MRSA infections that may occur in our adult population cared for in the large urban area of Chicago, Ill.
Study setting.
Northwestern Memorial Hospital (NMH) is a 688-bed tertiary-care teaching facility serving an adult population. During the study period, no MRSA isolates were recovered from children.
Study design and case definition.
We retrospectively reviewed the MRSA isolates during a 20-month period (January 1998 through August 1999) and selected those that were clindamycin susceptible for further investigation. The MRSA recovered were obtained from the Sunquest laboratory information system, with duplicates removed by the computer's search function. Patients were eliminated from consideration of harboring CA-MRSA if they had been admitted to NMH within the preceding 2 years or if their isolate had been obtained more than 72 h after admission, based on information retrieved from the hospital information system. For those remaining patients with potential CA-MRSA, the medical record was reviewed to determine if there had been an admission to an outside facility or other healthcare contact within 2 years. If, after the record was reviewed, a determination could not be made, the attending physician or the patient was contacted and questioned in order to obtain that information. The Institutional Review Board of Northwestern University approved these inquiries.
Microbiology procedures.
All cultures were evaluated in the NMH microbiology laboratory. Staphylococci were identified by colonial morphology, catalase testing, tube coagulase testing, DNase reaction, mannitol fermentation, tellurite reduction, and an oxidation-fermentation test. All isolates were tested for susceptibility by the agar dilution MIC method according to the methods approved by the National Committee for Clinical Laboratory Standards (11). An MIC of ≥4 μg/ml for oxacillin determined the S. aureus isolates to be methicillin resistant.
Detection of CA-MRSA.
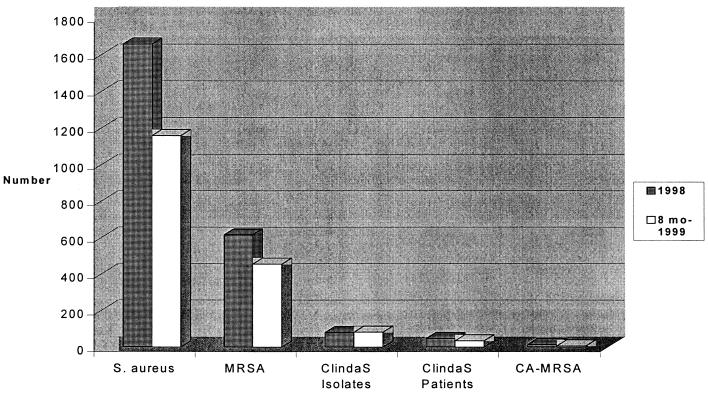
In reviewing these patients, we were unable to access only one chart. In 1998, there were a total of 1,658 S. aureus isolates recovered, with 616 being MRSA. Of these 616 isolates, the 80 (13%) that were clindamycin susceptible were recovered from 47 patients. Strains from 15 of these patients appeared potentially community acquired based on chart review. Through the first 8 months of 1999 there were 1,159 S. aureus isolates cultured, with 455 being MRSA. Of the 455 isolates, 81 (18%) were clindamycin susceptible and were recovered from 34 patients; isolates from 5 of these 34 patients appeared to be community acquired. Figure 1 shows the various proportions of S. aureus we identified by our investigation. The majority of the cases that were of potential community origin had skin or soft tissue infections.
FIG. 1.
Isolates and patients representing S. aureus in the adult population at NMH during 1998 and the first 8 months of 1999. ClindaS, MRSA isolates susceptible to clindamycin.
Of the presumed community-acquired isolates from 20 patients, all were susceptible to gentamicin, isolates from 19 were susceptible to tetracycline, and isolates from 16 were susceptible to ciprofloxacin. Despite multiple attempts, we were only able to contact 4 of the 20 patients suspected of being infected with CA-MRSA in order to confirm that there had been no admission to a healthcare facility within the prior 2 years. We found in these four cases that there had been no recent hospital admission; however, two of these four individuals were healthcare workers. Thus, only 2 of the 1,071 MRSA strains could be confirmed as CA-MRSA.
Concluding comments.
During this era of antimicrobial overuse and increasing reports of multidrug-resistant organisms, CA-MRSA has appeared as a newly emerging problem. The isolates considered as representing CA-MRSA differ from nosocomial isolates in both antimicrobial susceptibility and molecular typing patterns (4). Interestingly, two prospective studies carefully looking for patient contact with the healthcare system failed to detect significant numbers of true community-acquired MRSA in New York (United States), and London (Canada) (14, 15). Our results from Chicago, Ill., support these latest reports.
We selected clindamycin susceptibility as a surrogate to screen for CA-MRSA since this has been found as a unique marker in the published reports of CA-MRSA (5) and can be useful by narrowing the number of MRSA isolates from patients whose infection may need to be considered as community acquired. This approach should exclude the vast majority of nosocomial isolates that are typically resistant to clindamycin. While clindamycin susceptibility eliminated a large number of MRSA strains from patients that needed medical record review, it was not highly specific in that we found very few CA-MRSA in our adult population despite a fairly high number of clindamycin-susceptible isolates. The accepted mechanism for methicillin resistance is the acquisition of the mecA gene cluster, which codes for the penicillin-binding protein PBP2a. However, some CA-MRSA isolates may only have borderline resistance to methicillin and may not contain the mecA gene (2) and thus not be truly MRSA. We did not test for the mecA gene in our study, although most of our isolates were highly resistant to oxacillin (77% with an MIC of >8 μg/ml; 23% with an MIC of 8 μg/ml), strongly suggesting the presence of mecA in these strains.
A limitation to this study is its retrospective design and the fact that we were not able to speak with the majority of patients that potentially had CA-MRSA in order to confirm their lack of risk factors associated with the acquisition of MRSA. Two of the four contacted had ongoing contact with the healthcare system, thus only confirming two adults as CA-MRSA. If a patient had been admitted to a hospital within the prior 2 years, we did not include that patient since MRSA colonization has been shown to persist a long time after hospitalization: even up to 40 months in one report (13). Interestingly, if this 2-year criterion for hospital contact had been used in the Canadian study, only 2 of 331 (0.6%) newly identified patients with MRSA would have been considered as CA-MRSA (15).
Routinely reviewing patient risk factors from whom clindamycin-susceptible MRSA is recovered may be a useful tool for detecting CA-MRSA infection. However, even though using multidrug susceptibility as a surrogate for suspecting a community-acquired MRSA was a sensitive screen, it was not specific since the vast majority of even these isolates (>98%) came from patients with a demonstrated risk factor for MRSA carriage. Our data indicate that the prevalence of this unique S. aureus (CA-MRSA) is extremely low in adults served by our hospital, as opposed to what appears to be the case for children, in Chicago, but is similar to the low levels of community-acquired MRSA detected in New York and Canada (14, 15).
Acknowledgments
U.S. Public Health Service grant no. UR8/CCU515081, the Excellence in Academic Medicine program from the State of Illinois, Northwestern Memorial Hospital, and Northwestern University supported this work.
REFERENCES
- 1.Adcock P M, Pastor P, Medley F, Patterson J E, Murphy T V. Methicillin-resistant Staphylococcus aureus in two child care centers. J Infect Dis. 1998;178:577–580. doi: 10.1086/517478. [DOI] [PubMed] [Google Scholar]
- 2.Boyce J M. Are the epidemiology and microbiology of methicillin-resistant Staphylococcus aureus changing? JAMA. 1998;279:623–624. doi: 10.1001/jama.279.8.623. [DOI] [PubMed] [Google Scholar]
- 3.Embil J, Ramotar K, Romance L, Alfa M, Conly J, Taylor G, Sutherland B, Louie T, Herderson E, et al. Methicillin-resistant Staphylococcus aureus in tertiary care institutions on the Canadian prairies 1990–1992. Infect Control Hosp Epidemiol. 1994;15:646–651. doi: 10.1086/646827. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Four pediatric deaths from community-acquired methicillin-resistant Staphylococcus aureus—Minnesota and North Dakota, 1997–1999. Morb Mort Wkly Rep. 1999;48:707–710. [PubMed] [Google Scholar]
- 5.Frank A L, Marcinak J F, Mangat P D, Schreckenberger P C. Increase in community-acquired methicillin-resistant Staphylococcus aureus in children. Clin Infect Dis. 1999;29:935–936. doi: 10.1086/520463. [DOI] [PubMed] [Google Scholar]
- 6.Gorack E J, Yamada S M, Brown J D. Community-acquired methicillin-resistant Staphylococcus aureus in hospitalized adults and children without known risk factors. Clin Infect Dis. 1999;29:797–800. doi: 10.1086/520437. [DOI] [PubMed] [Google Scholar]
- 7.Herold B C, Immergluck L C, Maranan M C, Lauderdale D S, Gaskin R E, Boyle-Vavra S, Leitch C D, Daum R S. Community-acquired methicillin resistant Staphylococcus aureus in children with no identified predisposing risk. JAMA. 1998;279:593–598. doi: 10.1001/jama.279.8.593. [DOI] [PubMed] [Google Scholar]
- 8.Lowy F. Staphylococcus aureus infections. N Engl J Med. 1998;339:520–532. doi: 10.1056/NEJM199808203390806. [DOI] [PubMed] [Google Scholar]
- 9.Maguire G P, Arthur A D, Boustead P J, Dwyer B, Currie B J. Emerging epidemic of community-acquired methicillin-resistant Staphylococcus aureus infection in the Northern Territory. Med J Aust. 1996;164:721–723. doi: 10.5694/j.1326-5377.1996.tb122270.x. [DOI] [PubMed] [Google Scholar]
- 10.Moreno F, Crisp C, Jorgensen J H, Patterson J E. Methicillin-resistant Staphylococcus aureus as a community organism. Clin Infect Dis. 1995;21:1308–1312. doi: 10.1093/clinids/21.5.1308. [DOI] [PubMed] [Google Scholar]
- 11.National Committee for Clinical Laboratory Standards. Methods for dilution antimicrobial tests for bacteria that grow aerobically. Approved standard M7–A5. Wayne, Pa: National Committee for Laboratory Standards; 2000. [Google Scholar]
- 12.O'Brien F G, Pearman J W, Gracey M, Riley T V, Grubb W B. Community strain of methicillin-resistant Staphylococcus aureus involved in a hospital outbreak. J Clin Microbiol. 1999;37:2858–2862. doi: 10.1128/jcm.37.9.2858-2862.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sanford M D, Widmer A F, Bale M J, Jones R N, Wenzel R P. Efficient detection and long-term persistence of the carriage of methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 1994;19:1123–1128. doi: 10.1093/clinids/19.6.1123. [DOI] [PubMed] [Google Scholar]
- 14.Shopsin B, Mathema B, Martinez J, Ha E, Campo M L, Fierman A, Krasinski K, Kornblum J, Alcabes P, Waddington M, Riehman M, Kreiswirth B N. Prevalence of methicillin-resistant and methicillin-susceptible Staphylococcus aureus in the community. J Infect Dis. 2000;182:359–362. doi: 10.1086/315695. [DOI] [PubMed] [Google Scholar]
- 15.Warshawsky B, Hussain Z, Gregson D B, Alder R, Austin M, Bruckschwaiger D, Chagla A H, Daley J, Duhaime C, McGhie K, Pollett G, Potters H, Schiedel L. Hospital- and community-based surveillance of methicillin-resistant Staphylococcus aureus: previous hospitalization is the major risk factor. Infect Control Hosp Epidemiol. 2000;21:724–727. doi: 10.1086/501718. [DOI] [PubMed] [Google Scholar]