Abstract
Objective:
Mental health agencies provide critical safety net services for youths. No prior research has assessed the impacts of the COVID-19 pandemic on services these agencies provide or the youths they serve. This study sought to characterize mental health agency officials’ perceptions of the impacts of the pandemic on youths and challenges to providing youth services during the pandemic, and to examine associations between these challenges and impacts.
Method:
Surveys were completed by 159 state/county mental health agency officials from 46 states in September-October 2020. Respondents rated the impact of the COVID-19 pandemic on youth mental health issues, general service challenges, and tele-psychiatry service challenges across patient, provider, financing domains on 7-point scales. Multiple linear regression models estimated associations between service challenges (independent variables) and pandemic impacts (dependent variables).
Results:
Most agency officials perceived the COVID-19 pandemic as having disproportionately negative mental health impacts on socially disadvantaged youths (72% serious impact, mean= 5.85). Only 15% perceived the pandemic as having seriously negative impacts on receipt of needed youth services (mean= 4.29). Serious service challenges related to youths lacking reliable equipment/internet for tele-psychiatry services (60% serious challenge, mean= 5.47) and the inability to provide some services remotely (42% serious challenge, mean= 4.72). In regression models, the inability to provide some services remotely was significantly (p≤ .01) associated with four-of-six pandemic impacts.
Conclusions:
Mental health agency officials perceive the COVID-19 pandemic as exacerbating youth mental health disparities, but not dramatically impacting the receipt of needed services. However, some specific service challenges exist.
Keywords: Youth, mental health, mental health agencies, COVID-19 pandemic, telepsychiatry
An emerging body of evidence suggests that stressors caused by the COVID-19 pandemic are adversely impacting the mental health of many youths in the United States.1-7 For example, the proportion of emergency department visits for mental health issues nationally was 31% higher among youths ages 12-17 between March-October 2020 compared to the same prepandemic time period in 2019.1 A nationally representative survey of parents fielded in June 2020 found that 14% reported that their children’s mental health had worsened during the pandemic3 and a large survey of caregivers in Chicago, Illinois found similar results.2 The mental health impacts of the pandemic could be especially severe for youths served by public mental health agencies.
As Pinals and colleagues describe, “State behavioral health directors have faced inordinate challenges in facilitating responsive approaches to the COVID-19 crisis.” (p. 1,073) 8 Furthermore, as Goldman and colleagues note, mental health agencies are particularly vulnerable to service disruptions caused by the pandemic because they are typically under-funded and under-resourced.9 These concerns were echoed in a U.S. Government Accountability Office Report which found evidence that public mental health agencies encountered challenges to meeting service demands during the pandemic.10 These agencies also disproportionately serve youths who are low-income,11 and are thus more likely to encounter technological barriers to tele-psychiatry services.12 As such, the impacts of the pandemic on mental health agencies could contribute to pandemic-related mental health disparities between socially disadvantaged and advantaged youths13—similar to disparities observed among U.S. adults during the pandemic.14-19
The impacts of the pandemic on mental health agencies and safety net services for youths have been explored by little scholarship and virtually no empirical research. The aforementioned reviews by Pinals8 and Goldman9 do not address youth-specific issues. Surveys have assessed psychologists’ perceptions of the impacts of the COVID-19 pandemic on service delivery,20-23 however this work has largely been limited to adult-serving direct service providers in private practice. An international survey of 681 mental health professionals found that 59% identified the impact of the pandemic on youth mental health prevention, treatment, and service systems as a top research priority.24 However, data about these impacts and challenges mental health agencies have faced to providing youth services during the pandemic are lacking.
We conducted a national survey of public mental health agency officials. The study aims were to:
Describe the extent to which these officials perceive youth mental health issues as being negatively impacted by the COVID-19 pandemic;
Characterize the extent to which these officials perceive issues as challenges to providing mental health services to youths during the pandemic—including issues related to telepsychiatry services across patient, provider, and financing domains; and
Explore associations between perceptions of challenges to providing mental health services to youths during the pandemic and perceived impacts of the pandemic.
METHODS
The study was approved by the BLINED University Institutional Review Board. Between September 21, 2020 and October 30, 2020, web-based surveys were sent to 695 U.S. state and county mental health agency officials. These individuals were identified at the state-level for all 50 states and also at the county-level for 15 states that have de-centralized mental health systems (Appendix A).
The survey was created and distributed using Qualtrics, a web-based survey tool. The sample frame included agency officials in roles such as director, deputy director, children’s division director, medical director, and SAMHSA program director. Each agency official was sent a personalized e-mail with a unique survey link six times and telephone follow-up was conducted to ensure that e-mails were received.
The survey was completed by 159 respondents, 62% from state agencies and 38% from county agencies. The aggregate response rate was 23%, which is considered good for agency officals25 and notably higher than response rates of national surveys of psychologists during the pandemic.21-23 Non-response analysis revealed that there were no statistically significant differences in response rate by U.S. Census region (χ2= 2.20, df= 1, p= .53). At least one survey was completed in 46 states (92% of states responding, median respondents per state= 2). Among respondents, 30% were from the Northeast, 26% were from the South, 25% were from the Midwest, and 19% were from the West. We used Gender API—a marketing tool that uses a person’s first name to predict the probability of them identifying as female or male—to assess gender differences between respondents and non-respondents. We found no significant difference in the percentage of respondents and non-respondents who had a first name that was predicted to be female (73% vs. 68%; χ2= 1.55. df= 1, p= .21) or the average prediction probability accuracy between the two groups (98% vs. 98%, F= .917, df= 1, p= .34).
Variables
The survey focused on two domains of variables: 1) impacts of the COVID-19 pandemic on issues related to youth mental health and 2) challenges to providing mental health services to youths during the pandemic. The selection of variables, and development of survey items to assess them, was informed by practice reports about these pandemic-related issues, such as those published in the trade publication Mental Health Weekly, and general literature about barriers to providing tele-psychiatry services.26,27 The survey items (Appendix B) were reviewed by five former mental health agency officials to assess the clarity of questions. The order of items in each domain was randomized to reduce the risk of order-effect bias.28
Impacts of the COVID-19 pandemic on six issues were assessed, each on a 7-point Likert scale (1= no effect, 7= major negative impact). Challenges to providing mental health services to youths during the COVID-19 pandemic were assessed through two sets of items: one focused on general challenges and one focused on tele-psychiatry challenges. Each challenge item was assessed on a 7-point Likert scale (1= not a challenge, 7= major challenge). Challenges specifically related to tele-psychiatry services were separately assessed across patient, provider, and financing domains. Five patient challenges were assessed and summed to create a composite patient tele-psychiatry challenge score (Cronbach’s alpha= .85), eight provider challenges were assessed and summed to create a composite provider tele-psychiatry challenge score (Cronbach’s alpha= .91), and four financing challenges were assessed and summed to create a composite telepsychiatry financing challenge score (Cronbach’s alpha= .93). A composite tele-psychiatry challenge score was not calculated for a respondent if they did not respond to one or more items in the domain. Demographic characteristics related to respondents’ highest level of education, the number of years they had worked at their agency, race/ethnicity, and gender were assessed.
Analysis
Means and standard deviations were calculated for all items and composite scores. Descriptive statistics were also generated with each 7-point Likert scale item dichotomized, with responses of 6 or 7 were coded as “serious impact” or “serious challenge.” For each domain of tele-psychiatry challenge (i.e., patient, provider, financing), the mean of the mean rating for all items was calculated for each respondent. Paired sample two-tailed t-tests assessed the significance of differences in these means as well as the means of individual items. Chi-square tests were used to compare proportions. Missing data (i.e., item nonresponse) were excluded from analyses and ranged from 5% to 17% (mean 11%, median 9%).
Multiple linear regression models estimated associations between perceived challenges to providing youth mental health service during the pandemic and perceived impacts of the pandemic on youth mental health issues. Five models were run, with ratings of mental health impacts as dependent variables in separate models. We limited the variables in these analyses to instances where there was a plausible rationale for why a challenge variable might affect an impact variable. Every model adjusted for all seven general challenges and the three telepsychiatry challenge composite scores. Variables related to demographic characteristics, geographic region, and state or county agency level were not included in the models because ANOVAs and chi-square tests revealed that they were not significantly associated with perceptions of challenges or impacts. A p-value of .01 was used as the threshold for statistical significance in the models to reduce the risk of type 1 error. Assessment of multi-collinearity showed that the variance inflation factor was between 1.0 and 4.0 for all independent variables in all models, indicating the absence of multi-collinearity.29 Assessment of the normality of the data revealed that the majority of variables were skewed at a threshold ≥ .20. Thus, all variables were log transformed when entered into the regression models.
RESULTS
Nearly half of respondents (49%) had worked at their agency for ≥10 years and the modal highest level of education was master’s degree (70%) followed by doctoral degree (19%). Respondents predominantly identified as female (77%) and non-Hispanic White (73%).
Impacts of the Pandemic on Youth Mental Health Issues
The issue perceived as most serious was the COVID-19 pandemic having disproportionately negative impacts on the mental health of socially disadvantaged youths (72% serious impact, mean= 5.85 ± 1.25) (Table 1). Issues related to the pandemic having negative impacts on youth mental health in general (53% serious impact, mean= 5.48 ± 1.16) and increasing demand for youth mental health services (46% serious impact, mean= 5.16 ± 1.42) were perceived as the second and third most serious issues. The differences in mean impact ratings between these three issues were all significant at a threshold of p ≤.003. The vast majority of respondents did not perceive the pandemic as having seriously negative impacts on receipt of needed youth mental health services (15% serious impact, mean= 4.29 ± 1.16), the quality of youth mental services (12.2% serious impact, mean= 3.88 ± 1.38), or the supply of youth mental health services (15% serious impact, mean= 3.76 ± 1.44).
Table 1:
Perceptions of Impacts of the COVID-19 Pandemic on Youth Mental Health and Service Provision, State and County Mental Health Agency Officials, September 21, 2020-October 30, 2020
| Perceived Impacts | n | Meana | SD | %b |
|---|---|---|---|---|
| Disproportionately negative impacts on the mental health of socially disadvantaged youth | 149 | 5.85 | 1.25 | 72 |
| Negative impacts on the mental health of youth | 132 | 5.48 | 1.16 | 53 |
| Increased the demand for mental health services among youth | 148 | 5.16 | 1.42 | 46 |
| Prevented youth from receiving needed mental health services | 151 | 4.29 | 1.16 | 15 |
| Negatively impacted the quality of mental health services provided to youth | 147 | 3.88 | 1.38 | 12 |
| Reduced the supply of mental health services for youth | 144 | 3.76 | 1.44 | 15 |
Note: N= 159.
7-point Likert scale: 1= no effect, 7= major negative impact.
Percentage of respondents indicating 6 or 7 on scale.
Challenges to Providing Youth Mental Health Services During the Pandemic
General Service Challenges
The general service challenge perceived as most serious was the inability to provide some youths mental health services remotely during the pandemic (e.g., home and community-based programs, mobile crisis services) (42% serious challenge, mean= 4.72, ± 1.74) (Table 2). Provider staffing issues related to illness and childcare obligations was perceived as the second most serious challenge (29% serious challenge, mean= 4.25 ± 1.67). Only 11% or less of respondents indicated that facility closures (mean= 2.98 ± 1.90), redeployment of inpatient psychiatric beds for COVID-19 patients (mean= 2.60 ± 1.82), or medication supply (mean= 2.29 ± 1.45) was a serious challenge to providing youth mental health services.
Table 2:
Perceptions of General Challenges to Providing Mental Health Services to Youth During the COVID-19 Pandemic, State and County Mental Health Agency Officials, September 21, 2020- October 30, 2020
| Perceived General Challenges | n | Meana | SD | %b |
|---|---|---|---|---|
| Inability to provide some services remotely | 146 | 4.72 | 1.74 | 42 |
| Provider capacity/staffing issues because of illness and /or childcare obligations | 144 | 4.25 | 1.67 | 29 |
| Lack of personal protective equipment for providers | 145 | 3.77 | 1.85 | 20 |
| Patients missing appointments | 145 | 3.66 | 1.68 | 16 |
| Facility closures | 143 | 2.98 | 1.90 | 11 |
| Redeployment of inpatient psychiatric beds for anticipated/actual COVID-19 patients | 141 | 2.60 | 1.82 | 10 |
| Medication supply | 144 | 2.29 | 1.45 | 4 |
Note: N= 159.
7-point Likert scale: 1= not a challenge, 7= major challenge.
Percentage of respondents indicating 6 or 7 on scale.
Tele-Psychiatry Service Challenges
The tele-psychiatry service challenges perceived as most serious were in the patient domain (Figure 1). The mean rating of challenges in this domain (mean= 4.13 ±1.35) was significantly and 24% higher than the mean rating of challenges in provider domain (mean= 3.26 ± 1.42) and 32% higher than challenges in the financing domain (mean= 3.01 ± 1.64).
Figure 1:
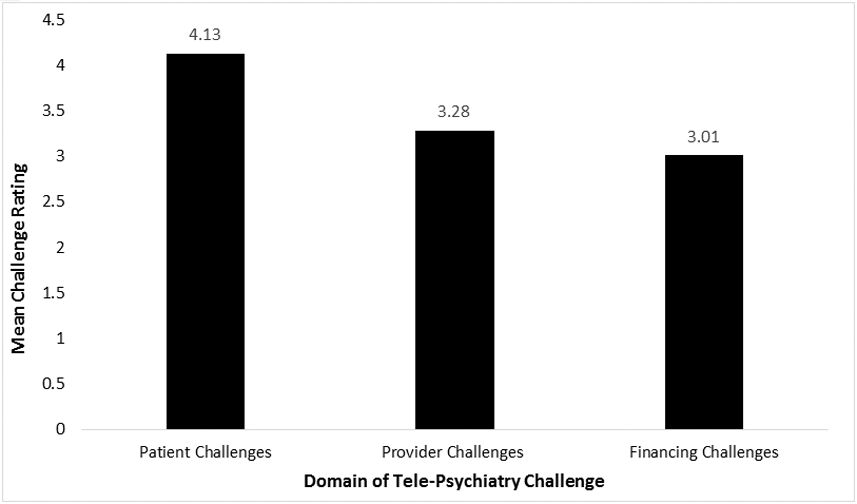
Differences in Mean Ratings of Tele-psychiatry Challenges Across Patient, Provider, and Financing Domains, State and County Mental Health Agency Officials, Fall 2020.
Note: N= 159. 7-point Likert scale: 1= not a challenge, 7= major challenge
Two specific tele-psychiatry challenges, both in the patient domain, were perceived as much more serious challenges than others (Table 3). These challenges were patients lacking reliable internet access, data on cellphone plans, or equipment (i.e., laptops, iPads) (59% serious challenge, mean= 5.47 ± 1.52) and tele-psychiatry services not being developmentally appropriate for some youths (e.g., children of certain ages, children who are non-verbal) (41% serious challenge, mean= 4.81, ± 1.81). The most serious challenges in the tele-psychiatry provider domain were lack of provider training on tele-psychiatry (18% serious challenge, mean=3.71 ± 1.77 ) and some types of therapies offered not translating to tele-psychiatry (17% serious challenge, mean= 3.68 ± 1.74). The most serious challenge in the tele-psychiatry financing domain was insufficient commercial insurance reimbursement for tele-psychiatry services (15% serious challenge, mean= 3.40 ± 1.95).
Table 3:
Perceptions of Tele-Psychiatry Challenges to Providing Mental Health Services to Youth During the COVID-19 Pandemic, State and County Mental Health Agency Officials, September 21, 2020- October 30, 2020
| Perceived Tele-Psychiatry Challenges |
n | Meana | SD | %b |
|---|---|---|---|---|
| Patient Challenges | ||||
| Lack of reliable internet access, data on cellphone plans, or equipment (i.e., laptops, iPads, smartphones) | 140 | 5.47 | 1.52 | 59 |
| Tele-psychiatry services not developmentally appropriate for some youth (e.g., age of child; child is non-verbal) | 139 | 4.81 | 1.81 | 41 |
| Youth or families not comfortable with tele-psychiatry | 140 | 3.89 | 1.67 | 19 |
| Youth or families not aware of the option for tele-psychiatry | 139 | 3.27 | 1.78 | 12 |
| Youth or families concerned about privacy issues | 138 | 3.22 | 1.76 | 12 |
| Provider Challenges | ||||
| Lack of provider training on tele-psychiatry | 140 | 3.71 | 1.77 | 18 |
| Types of therapies offered do not translate to tele-psychiatry | 139 | 3.68 | 1.74 | 17 |
| Providers not comfortable with tele-psychiatry | 141 | 3.66 | 1.55 | 11 |
| Regulations regarding billing (e.g., unable to bill for text messaging) | 137 | 3.38 | 1.93 | 18 |
| Lack of remote work policies for providers | 135 | 3.33 | 1.93 | 16 |
| Access to a HIPPA adherent platform to practice tele-psychiatry | 138 | 2.99 | 1.89 | 13 |
| Regulations do not permit flexible delivery of the service | 138 | 2.92 | 1.84 | 14 |
| Licensing challenges | 132 | 2.54 | 1.72 | 7 |
| Financing Challenges | ||||
| Lack of/insufficient private/commercial insurance reimbursement for tele-psychiatry | 132 | 3.40 | 1.95 | 15 |
| Lack of/insufficient CHIP reimbursement for tele-psychiatry | 132 | 2.92 | 1.76 | 9 |
| Limited number of tele-psychiatry services for which reimbursement is provided | 136 | 2.89 | 1.78 | 10 |
| Lack of/insufficient Medicaid reimbursement for tele-psychiatry | 135 | 2.84 | 1.74 | 7 |
Note: N= 159
7-point Likert scale: 1= not a challenge, 7= major challenge
Percentage of respondents indicating 6 or 7 on scale.
Associations between Challenges to Providing Youth Mental Health Services and Impacts
The extent to which the inability to provide some services remotely was perceived as a challenge was positively and significantly associated with the extent to which three of the five youth mental health issues were perceived as being adversely impacted by the COVID-19 pandemic (Table 4). For example, a 1% increase in the extent to which the inability to provide some services remotely was perceived as a challenge was associated with a 0.28% increase in the extent to which the pandemic was perceived as having disproportionately negative mental health impacts on socially disadvantaged youths (β= 0.28, p= .01, Model 1) and a 0.39% increase in the extent which the pandemic was perceived as adversely affecting the quality of mental health services for youths (β= 0.39, p< .0001, Model 4). None of the t tele-psychiatry challenge composite scores were significantly associated with the impact variables in the adjusted models.
Table 4:
Adjusted Associations between Perceptions of Challenges to Providing Mental Health Services to Youth and Perceptions of Impacts of the COVID-19 Pandemic on Youth , State and County Mental Health Agency Officials, September 21, 2020- October 30, 2020
| Perceived Impacts | |||||
|---|---|---|---|---|---|
| Model 1: Disproportionately negative impacts on the mental health of socially disadvantaged youth |
Model 2: Negative impacts on the mental health of youth |
Model 3: Prevented youth from receiving needed mental health services |
Model 4: Negatively impacted the quality of mental health services provided to youth |
Model 5: Reduced the supply of mental health services for youth |
|
| Perceived Challenges | β | β | β | β | β |
| Patient tele-psychiatry challenge composite score | 0.14 | 0.07 | 0.05 | −0.12 | 0.16 |
| Provider tele-psychiatry challenge composite score | −0.12 | −0.17 | −0.18 | 0.18 | −0.13 |
| Financing tele-psychiatry challenge composite score | −0.02 | 0.21 | 0.07 | 0.06 | 0.01 |
| Inability to provide some services remotely | 0.28* | 0.32 | 0.15 | 0.39** | 0.30* |
| Provider capacity/staffing issues because of illness and/or childcare obligations | 0.30* | 0.28* | 0.02 | −0.10 | 0.05 |
| Medication supply | −0.04 | −0.11 | 0.24 | 0.12 | 0.10 |
| Redeployment of inpatient psychiatric beds | −0.12 | −0.05 | −0.05 | 0.06 | −0.09 |
| Facility closures | 0.14 | 0.11 | 0.08 | −0.04 | 0.24 |
| Lack of personal protective equipment | −0.02 | −0.09 | −0.04 | 0.00 | −0.07 |
Note: N= 159.
p ≤ 0.01
p ≤ 0.001.
Adjusted R2 statistics: Model 1= 0.14, Model 2= 0.24, Model 3= 0.03, Model 4= 0.23, Model 5= 0.14.
DISCUSSION
This survey is the first national assessment of the impacts of the COVID-19 pandemic on safety net youth services provided by mental health agencies. We find that officials in these agencies perceive the pandemic having seriously adverse impacts on youth mental health, particularly among socially disadvantaged youths. However, most do not perceive the pandemic as dramatically preventing access to needed services. The primary challenges to service provision related to the inability to provide some services remotely, patients lacking sufficient technology (e.g., internet access) for tele-psychiatry services, and tele-psychiatry services not being developmentally appropriate for some youths.
The finding that the COVID-19 pandemic is perceived as having disproportionately negative impacts on the mental health of socially disadvantaged youths is consistent research about the impacts of the pandemic on adults. Surveys have observed that U.S. adults who are financially insecure, African American, and Hispanic have experienced elevated levels of stress and psychiatric morbidity because of the pandemic.14-19 Disparities in pandemic-related stress and psychiatric morbidity among adults could adversely disrupt household dynamics and subsequently contribute to disparities in pandemic-related mental health problems among youths.13,30 A key question for future research and practice is how public mental health agencies can best engage socially disadvantaged youths in care. One approach might be social marketing campaigns that reduce mental illness stigma among youths and caregivers and improve attitudes about mental health services.31 Research among U.S. adults indicates that such attitudinal barriers are major impediments to mental health treatment among racial and ethnic minorities with psychiatric disorders.32
The finding that the COVID-19 pandemic was not perceived as dramatically preventing access to youth services in public mental health systems likely reflects rapid system-wide transitions to tele-psychiatry. Recent studies indicate that mental health providers successfully transitioned to tele-psychiatry during the pandemic.20-23,33,34 Our finding that mental health agency officials do not perceive provider issues as major challenges to youth tele-psychiatry services is consistent with this literature.
However, agency officials in our survey did perceive patient issues related to lack of reliable internet access, data on cellphone plans, and equipment as major barriers to youths accessing tele-psychiatry services during the COVID-19 pandemic. These issues could contribute to disparities in the pandemic’s mental health impacts because such technological challenges are disproportionately prevalent among socially disadvantaged groups.35 For example, data from the Pew Research Center indicate that only 56% of adults with household income <$30,000 per year have broadband internet in their home and 71% have a smartphone, compared with 81% and 85%, respectively, of adults with household incomes $30,000-$99,999.12
The results of exploratory regression models highlight areas for future research. One area relates to the challenge of mental health agencies being unable to provide some services remotely. This challenge was significantly and positively associated with the extent to which the pandemic was perceived as adversely affecting three of the five youth mental health impacts assessed. Counterintuitively, this challenge was not significantly associated with the extent to which the pandemic was perceived as preventing youths from receiving needed mental health services. This could be because services that cannot be offered remotely—'home-based and community-based programs, mobile crisis, respite for caregivers” were the examples provided in the survey—might constitute a small proportion of youth mental health services offered by agencies. It should also be noted that none of the challenges assessed were significantly associated with perceptions of the pandemic preventing youths from receiving needed mental health services, and none of the models significantly explained any of its variance. Future research using administrative datasets is needed to understand the impacts of the pandemic on youth mental health service utilization in safety net settings.
Limitations
Our survey has at least five main limitations. First, although 92% of states had at least one respondent and non-response analysis revealed no statistically significant differences in the response rate by U.S. Census region or gender, it is possible that survey respondents are not fully representative of all youth-serving mental health agency officials. As previously noted, our response rate is higher than those of two national surveys of mental health service providers fielded during the pandemic, which achieved response rates of 11.8%21 and 13.6%.22,23
Second, the survey covered a wide range of topics and, with the exception of challenges related to tele-psychiatry services, assessed constructs with single Likert-scale items. Third, the regression analyses were exploratory and not hypothesis-driven. The models may have been statistically under-powered to identify all significant associations. Fourth, it should be noted that agency officials did not respond to some items, with about 10.0% of officials not responding to each item. It is likely that respondents did not respond to these items because they did not have an opinion about the issue, but the reasons are unknown. Fifth, it should be emphasized that the survey focused on the perceptions of agency officials and may not reflect the perceptions of other important stakeholders, such as patients and providers. Many challenges—such as youth privacy concerns related to tele-psychiatry encounters—may be formidable but not reflected in the survey findings because information about these challenges did not reach agency officials. There would value in future research that assesses the extent to which agency officials’ perspectives are aligned with objective measures of barriers to treatment, such as those available in health care claims databases.
CONCLUSION
Mental health agency officials perceive the COVID-19 pandemic as having serious and disproportionately negative impacts on the mental health of socially disadvantaged youths, but not dramatically preventing access to youth mental health services. The inability to provide some types of youth mental health services remotely during the pandemic is perceived as a major challenge by many agency officials, as are patient-related challenges to tele-psychiatry services for youths. However, tele-psychiatry provider and financing issues are generally not perceived as major challenges. The survey findings provide an empirical foundation to inform future research and financing, policy, and programing initiatives to support mental health agencies in their efforts to address the mental health consequences of the COVID-19 pandemic among youths.
Supplementary Material
HIGHLIGHTS.
Mental health agency officials perceive the COVID-19 pandemic as having disproportionately negative mental health impacts on socially disadvantaged youths.
Most mental health agency officials do not perceive the COVID-19 pandemic as having seriously negative impacts on the receipt of needed youth services.
Mental health agency officials perceive patient issues (e.g., lack of reliable equipment and internet) as major challenges to the provision of tele-psychiatry services to youths during the COVID-19 pandemic, but generally do not perceive provider or financing issues as major challenges to tele-psychiatry services.
Acknowledgements:
National Institute of Mental Health P50MH113662-02W1, P50MH113662-01A1
Contributor Information
Jonathan Purtle, Department of Health Management & Policy, Drexel University Dornsife School of Public Health.
Katherine L. Nelson, Department of Health Management & Policy, Drexel University Dornsife School of Public Health.
Sarah McCue Horwitz, Department of Child and Adolescent Psychiatry, New York University School of Medicine.
Lawrence A. Palinkas, Suzanne Dworak-Peck School of Social Work, University of Southern California.
Mary M. McKay, Brown School at Washington University in St. Louis.
Kimberly E. Hoagwood, Department of Child and Adolescent Psychiatry, New York University School of Medicine.
REFERENCES
- 1.Leeb RT, Bitsko RH, Radhakrishnan L, Martinez P, Njai R, Holland KM. Mental Health-Related Emergency Department Visits Among Children Aged< 18 Years During the COVID-19 Pandemic—United States, January 1–October 17, 2020. Morbidity and Mortality Weekly Report. 2020;69(45):1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raviv T, Warren CM, Washburn JJ, et al. Caregiver Perceptions of Children’s Psychological Well-being During the COVID-19 Pandemic. JAMA Network Open. 2021;4(4):e2111103–e2111103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patrick SW, Henkhaus LE, Zickafoose JS, et al. Well-being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics. 2020;146(4). [DOI] [PubMed] [Google Scholar]
- 4.Krass P, Dalton E, Doupnik SK, Esposito J. US Pediatric Emergency Department Visits for Mental Health Conditions During the COVID-19 Pandemic. JAMA Network Open. 2021;4(4):e218533–e218533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Racine N, Cooke JL, Eirich R, Korczak DJ, McArthur B, Madigan S. Child and adolescent mental illness during COVID-19: A rapid review. Psychiatry Research. 2020. doi: 10.1016/j.psychres.2020.113307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loades ME, Chatburn E, Higson-Sweeney N, et al. Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. Journal of the American Academy of Child & Adolescent Psychiatry. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Academy of Pediatrics. Interim Guidance on Supporting the Emotional and Behavioral Health Needs of Children, Adolescents, and Families During the COVID-19. Pandemic 2021. Accessed on May 26, 2021 from https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/interim-guidance-on-supporting-the-emotional-and-behavioral-health-needs-of-children-adolescents-and-families-during-the-covid-19-pandemic/. [Google Scholar]
- 8.Pinals DA, Hepburn B, Parks J, Stephenson AH. The behavioral health system and its response to COVID-19: a snapshot perspective. Psychiatric Services. 2020;71(10):1070–1074. [DOI] [PubMed] [Google Scholar]
- 9.Goldman ML, Druss BG, Horvitz-Lennon M, et al. Mental Health Policy in the Era of COVID-19. Psychiatric Services. 2020:appi. ps. 202000219. [DOI] [PubMed] [Google Scholar]
- 10.U.S. Government Accountability Office. Behavioral Health: Patient Access, Provider Claims Payment, and the Effects of the COVID-19 Pandemic. 2021. Accessed on May 26, 2021 from https://www.gao.gov/products/gao-21-437r.
- 11.Miller JE. Too Significant to Fail: The Importance of State Behavioral Health Agencies in the Daily Lives of Americans with Mental Illness, for their Families, and for their Communities. National Association of State Mental Health Program Directors; 2012. [Google Scholar]
- 12.Pew Research Center. Digital divide persists even as lower-income Americans make gains in tech adoption. 2019. Accessed on May 26, 2021 from https://pewrsr.ch/39CpmM3.
- 13.Condon EM, Dettmer AM, Gee DG, et al. Commentary: COVID-19 and mental health equity in the United States. Frontiers in Sociology. 2020;5:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shim RS. Mental health inequities in the context of COVID-19. JAMA Network Open. 2020;3(9):e2020104–e2020104. [DOI] [PubMed] [Google Scholar]
- 15.Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Low assets and financial stressors associated with higher depression during COVID-19 in a nationally representative sample of US adults. Journal of Epidemiol Community Health. 2021. 1;75(6):501–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. Morbidity and Mortality Weekly Report. 2020;69(32):1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Purtle J. COVID-19 and mental health equity in the United States. Social Psychiatry and Psychiatric Epidemiology. 2020;55(8):969–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Panchal N., Kamal R., Cox C., Garfield R. The Implications of COVID-19 for Mental Health and Substance Use. 2021. Kaiser Family Foundation. Accessed on May 26, 2021 from https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/. [Google Scholar]
- 19.Keeter S. People financially affected by COVID-19 outbreak are experiencing more psychological distress than others. 2020. Pew Research Center. Accessed on May 26, 2021 from https://www.pewresearch.org/fact-tank/2020/03/30/people-financially-affected-by-covid-19-outbreak-are-experiencing-more-psychological-distress-than-others/. [Google Scholar]
- 20.Guinart D, Marcy P, Hauser M, Dwyer M, Kane J. Mental Healthcare Providers' Attitudes Towards Telepsychiatry: A Systemwide, Multisite Survey during the COVID-19 pandemic. Psychiatr Services. 2020:1–21. [DOI] [PubMed] [Google Scholar]
- 21.Pierce BS, Perrin PB, Tyler CM, McKee GB, Watson JD. The COVID-19 telepsychology revolution: A national study of pandemic-based changes in US mental health care delivery. American Psychologist. 2021;76(1):14–25. [DOI] [PubMed] [Google Scholar]
- 22.Sammons MT, VandenBos GR, Martin JN, Elchert DM. Psychological Practice at Six Months of COVID-19: A Follow-Up to the First National Survey of Psychologists During the Pandemic. Journal of Health Service Psychology. 2020;46(4):145–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sammons MT, VandenBos GR, Martin JN. Psychological practice and the COVID-19 crisis: A rapid response survey. Journal of Health Service Psychology. 2020;46:51–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Novins DK, Stoddard J, Althoff RR, et al. Editors' Note and Special Communication: Research Priorities in Child and Adolescent Mental Health Emerging From the COVID-19 Pandemic. Journal of the American Academy of Child & Adolescent Psychiatry. 2020;60: 544–554.e8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fisher SH III, Herrick R. Old versus new: the comparative efficiency of mail and internet surveys of state legislators. State Politics & Policy Quarterly. 2013;13(2):147–163. [Google Scholar]
- 26.Chakrabarti S. Usefulness of telepsychiatry: A critical evaluation of videoconferencing-based approaches. World Journal of Psychiatry. 2015;5(3):286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cowan KE, McKean AJ, Gentry MT, Hilty DM. Barriers to use of telepsychiatry: clinicians as gatekeepers. Mayo Clinic Proceedings. 2019;94(12):2510–2523. [DOI] [PubMed] [Google Scholar]
- 28.Perreault WD. Controlling order-effect bias. The Public Opinion Quarterly. 1975;39(4):544–51. [Google Scholar]
- 29.O’brien RM. A caution regarding rules of thumb for variance inflation factors. Quality & Quantity. 2007;41(5):673–690. [Google Scholar]
- 30.Feinberg ME, Mogle AJ, Lee JK, et al. Impact of the COVID-19 Pandemic on Parent, Child, and Family Functioning. Family Process. 2021. doi: 10.1111/famp.12649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Purtle J, Nelson KL, Counts NZ, Yudell M. Population-based approaches to mental health: history, strategies, and evidence. Annual Review of Public Health. 2020;41:201–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Green JG, McLaughlin KA, Fillbrunn M, et al. Barriers to Mental Health Service Use and Predictors of Treatment Drop Out: Racial/Ethnic Variation in a Population-Based Study. Administration and Policy in Mental Health and Mental Health Services Research. 2020:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rosen CS, Morland LA, Glassman LH, et al. Virtual mental health care in the Veterans Health Administration’s immediate response to coronavirus disease-19. American Psychologist. 2021;76(1):26–38. [DOI] [PubMed] [Google Scholar]
- 34.Avalone L, Barron C, King C, et al. : Rapid Telepsychiatry Implementation During COVID-19: Increased Attendance at the Largest Health System in the United States. Psychiatric Services. 2020. DOI: 10.1176/appi.ps.202000574. [DOI] [PubMed] [Google Scholar]
- 35.Wood SM, White K, Peebles R, et al. Outcomes of a rapid adolescent telehealth scale-up during the COVID-19 pandemic. Journal of Adolescent Health. 2020;67(2):172–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


