Abstract
Objective
To develop a theoretical model to explain how parents think about the process of communicating with their affected child about the psychiatric manifestations of 22q11DS.
Methods
Semi-structured interviews were conducted with parents of children with 22q11DS, who had all received psychiatric genetic counseling. Interviews were recorded, transcribed verbatim, and analyzed concurrently with data collection, using interpretive description. Identified themes were used to inductively develop a model of how parents think about communicating with their child about psychiatric risk in 22q11DS.
Results
From interviews with 10 parents, we developed a model representing the communication of psychiatric risk in 22q11DS as a process where various dynamic contextual factors (e.g., perception of risk, desire to normalize) act as either motivators or barriers to communication. Parents described challenges with the content, process, and outcome of these conversations. Parents wanted hands on, practical, personalized, and ongoing support from health professionals around communication about these issues.
Conclusion
This model may help equip genetics professionals to support parents to communicate effectively with their children in order to improve health outcomes and family adaptation to 22q11DS.
Practice implications
Our findings may apply not only to 22q11DS, but also to other genetic conditions where psychiatric manifestations occur.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12687-021-00558-9.
Keywords: Parent/child communication, 22q11.2 deletion syndrome, Psychiatric genetic counseling, Mental illness
Introduction
When a genetic condition is diagnosed prenatally or during childhood, the information conveyed about the diagnosis is often primarily directed at parents or caregivers, who then face decisions about when and how to disclose the diagnosis to their child. Disclosure to children can be difficult (Forrest et al. 2003; Metcalfe et al. 2011; Dennis et al. 2015): parents report feeling uncertain about the words to use, how to initiate the conversation and worry about their child’s understanding (Faux et al. 2012). These challenges may be particularly acute when considering conversations about manifestations of a genetic diagnosis that are stigmatized, like psychiatric disorders (Rössler 2016).
22q11.2 deletion syndrome (22q11DS) is a genetic condition associated with a wide range of physical clinical manifestations, as well as elevated rates of psychiatric disorders, including a ~25–30% chance to develop a psychotic disorder (Murphy and Owen 2001; Vorstman et al. 2006; Niklasson et al. 2009; Stoddard et al. 2010; Monks et al. 2014; Campbell et al. 2018). For many parents of children with 22q11DS, the risk of psychiatric illness is their main concern regarding their child’s health (Hercher and Bruenner 2008; Martin et al. 2012). Psychiatric genetic counseling for these families can be helpful; parents have expressed that the analogies used by the genetic counselor are useful communication tools in explaining mental illness to their children (Carrion et al. 2021). Despite this, genetics professionals are less likely to discuss psychiatric disorders than other features of 22q11DS, in part due to the stigma that surrounds psychiatric diagnoses (Martin et al. 2012; van den Bree et al. 2013; Morris et al. 2013; Karas et al. 2014; Baughman et al. 2015; Alugo et al. 2017; Cuthbert et al. 2019). These issues may present as additional barriers to parents discussing psychiatric disorders with their child.
Within the published literature analyzing family communication about genetic risk, there are few studies evaluating parents’ experience with disclosing details of their child’s own diagnosis to the child (Metcalfe et al. 2008, 2011; Dennis et al. 2015), and aside from one as yet unpublished study (Filiaggi et al., in preparation) that used thematic analysis to examine communication about psychiatric risk in the context of 22q11DS, no other work in this specific area. In other contexts, genetic counseling has been shown to improve family communication of genetic information (Forrest et al. 2008a; Gaff and Hodgson 2014; Hodgson et al. 2016; Mendes et al. 2016); however, the role that genetic counselors can play in facilitating parent-child communication has not been widely evaluated (Dennis et al. 2015). Thus, we sought to qualitatively explore how parents think about the process of communicating with their affected child about the psychiatric manifestations of 22q11DS, and to identify how genetics professionals could help equip parents for these conversations.
Methods
Participants
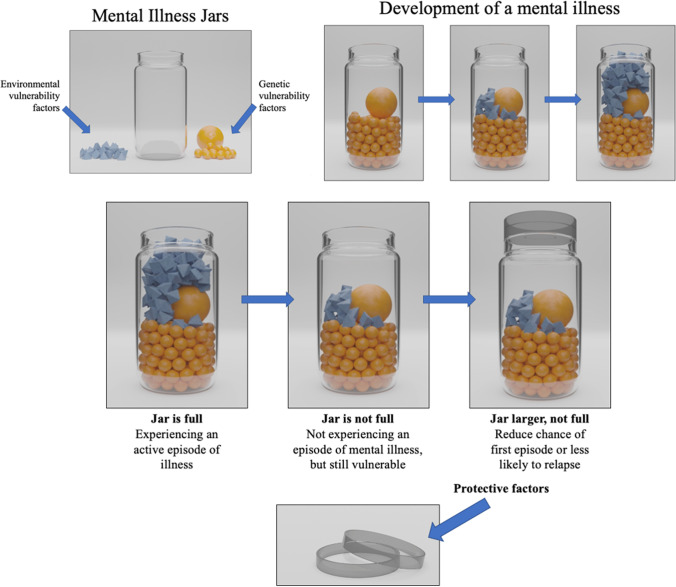
We recruited parents of children with a confirmed diagnosis of 22q11DS (i.e., by molecular/cytogenetic testing and/or clinical diagnosis by a clinical/medical geneticist) who were fluent in English and did not have a diagnosis of 22q11DS themselves. To ensure that all participants had received consistent information about the psychiatric manifestations of 22q11DS, as a foundation for the interviews, we recruited parents who had previously received psychiatric genetic counseling through (1) their participation in a previous study we conducted (Carrion et al. 2021); or (2) attending a specialist psychiatric genetic counseling clinic in Vancouver, Canada (Inglis et al. 2015). The process of psychiatric genetic counseling has been described in detail elsewhere (Inglis et al. 2015) and involves the use of a visual analogy of a “mental illness jar,” as shown in Figure 1 in the context of 22q11DS. Eligible participants were initially contacted by email, with follow-up by phone.
Fig. 1.
Mental illness jar model. Various genetic and environmental factors work together to precipitate an episode of mental illness. In the context of 22q11DS, the 22q11 deletion is discussed as a “large ball in the jar.” Protective factors, such as sleep, nutrition, exercise, and social support, are discussed as ways to make a person's mental illness jar larger, increasing its capacity to accommodate environmental stressors before becoming full. Images adapted by Ben Austin from How to Talk with Families About Genetics and Psychiatric Illness. Copyright (c) 2011 by Holly Peay and Jehannine Austin. Used with permission of the publisher, W. W. Norton & Company, Inc. All rights reserved.
Data collection
After collecting consent, interviews were conducted via BlueJeans, a secure online videoconferencing software using a semi-structured interview guide (see supplemental material), comprising questions to elicit the parents’ thoughts and experiences with communicating with their child about psychiatric risk. The initial version of the interview guide was informed by our group’s previous research and was revised over the course of the study based on preceding interviews. Demographic information was also collected to ensure that parents of children of varying ages, with and without psychiatric diagnoses, were included.
Each participant completed a single one-on-one interview (mean 65 min, range 40–96 min) with CBC (female, who was at the time an MSc genetic counseling student) between October 2020 and January 2021. Participants were aware that CBC was completing this research in partial fulfilment of the requirements of their MSc. CBC had no prior relationship with any of the participants and no personal experience with 22q11DS. Interviews were recorded, transcribed verbatim, and checked for accuracy. NVivo 12 was used to store, organize, and manage the data.
Data analysis
Transcripts were analyzed concurrently with data collection using interpretive description (Thorne 2016), which aims to understand and describe lived experience through a constructivist/inductive approach. It is an ideal methodology for understanding phenomena in a manner that informs clinical practice. To orient inquiry and make theoretical assumptions on which inductive reasoning in interpreting meaning within the data can be judged (Thorne et al. 1997), we used a family systems perspective on parenting and communication (which understands family processes and patterns as both influencing and being influenced by parent-child interaction as well as other individual and sociocultural factors) as our analytic framework (Socha and Stamp 2009; Socha 2013).
Analysis began with open coding—transcripts were analyzed line by line for basic conceptual units and to delineate the properties that characterize them (Thorne 2016). CBC and CS independently coded the first three interviews, then came together to discuss codes and develop a coding framework, which CBC subsequently applied to the remaining interviews. The coding framework was iteratively revised based on new findings from subsequent transcripts and applied to earlier interviews when relevant. Axial coding was then used to identify the main concepts from the coding framework, the conditions that give rise to them and the relationships between them. These concepts were used to inductively develop a model of the process through which parents consider communicating with their child about psychiatric risk in 22q11DS. CBC, CS, and JA met regularly to discuss concepts and theoretical linkages between them, until a cohesive theoretical model was formed. Throughout, written memos were used to capture decisions regarding the data and to record salient themes. Transcripts, codes, and memos were iteratively reviewed to discuss and resolve discrepancies. Rather than aiming for “saturation,” which has been critiqued for a variety of reasons (Vasileiou et al. 2018), we employed the concept of theoretical sufficiency, which asks whether the model constructed is adequate in terms of the use for which it was envisioned (Dey 1999). Transcripts were not returned to participants for comment, but two provided feedback on the draft theoretical model.
Results
Participants
Three eligible parents declined to participate, and ten parents (2 fathers and 8 mothers) of 9 index children agreed to participate and were interviewed. Table 1 provides self-reported demographic information for both participants and their children.
Table 1.
Demographics of parent participants and their children with 22q11DS
| Participants (n = 10) | |
| Gender | |
| Male | 2 |
| Female | 8 |
| Age (years) | |
| Mean | 44.9 |
| Range | 38-52 |
| Ancestry | |
| European | 6 |
| Middle Eastern | 1 |
| Mexican | 1 |
| Mixed | 2 |
| History of mental illness | |
| Personal | 2 |
| Personal and family | 1 |
| Family | 4 |
| Location | |
| Canada | 7 |
| United States | 3 |
| Children of participants (n=9)a | |
| Gender | |
| Male | 3 |
| Female | 6 |
| Age of (years) | |
| Mean | 13.3 |
| Range | 7-24 |
| Mental illness diagnosisb | |
| Anxiety | 5 |
| ADHD | 2 |
| Bipolar disorder with psychosis | 1 |
| Bipolar disorder | 1 |
| Depression | 1 |
| Ancestry | |
| European | 4 |
| Mixed | 5 |
aN<10 as two participants are partners (i.e., parents of the same child)
bN>9 for mental illness diagnosis for children with multiple diagnoses
Overview of the theoretical model
We developed a theoretical model of parents’ perspectives on, and experiences of, talking with their children about the psychiatric manifestations of 22q11DS (Figure 2). The parents who provided feedback on the model indicated that it comprehensively represented their experiences and perspectives and shared that the visual representation was helpful for considering and processing their own feelings about this conversation.
Fig. 2.
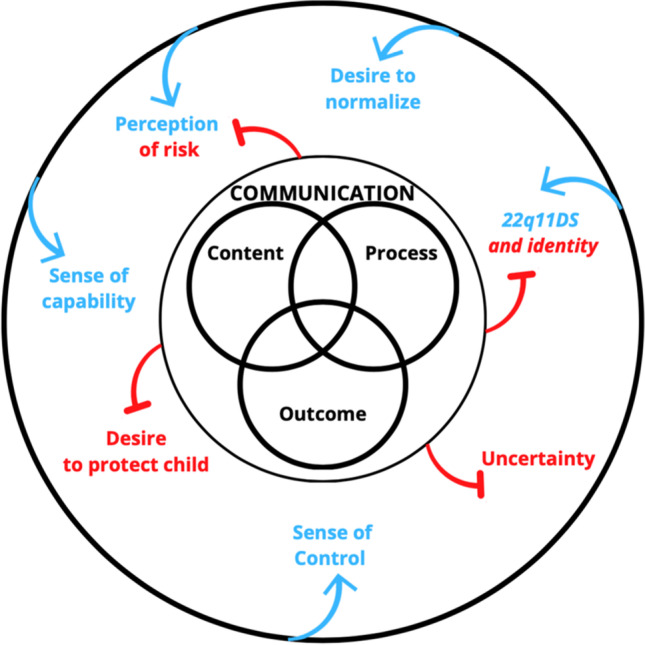
A visual representation of the process parents go through when considering and initiating a conversation about mental illness with their child. The outmost circle contains contextual factors that act as motivators or barriers to communication. Motivators are indicated by blue arrows and barriers are indicated by red inhibition arrows. Two contextual factors were perceived as either a motivator or barrier, depending on the parent, and are thus placed between a blue arrow and a red inhibition arrow. In the way that one would have to physically pass through the outermost circle to reach the inner communication circle, parents too do not engage in communication with their child without being influenced by their own unique contexts. The fluid and ongoing nature of this process is represented by the arrows extending in and out of the circles. The innermost circle represents the communication itself, comprising three intersecting components: content, process, and outcome.
Communication is represented as an ongoing, iterative process. Parents felt that there was value in communicating in “small bites” so that it would not be as much of “a shock later on when [their child] is more aware of what we’re talking about.”
“It’s a journey, it’s a process, it’s not a one-time sit down, ‘here’s your 101 on genetics and by the way you’re good, OK, woo, that’s done’…It’s going to be an ongoing thing.”
–Parent 3, father of an 11-year-old child
Context
Contextual factors had an important influence on parents’ consideration of communication—some were perceived as barriers, others as motivators and two could be perceived either way, depending on the parent.
Barrier: desire to protect child
Some parents wanted to protect their children from the knowledge that there were potential psychiatric manifestations of 22q11DS, which resulted in them not wanting to talk to their child about this topic.
“I don’t want to pre-prescribe him something that may never happen…or give him fears about something that may never happen.”
–Participant 9, mother of 9-year-old child
Other parents, though still planning to engage in these conversations, expressed that the desire to protect their child made the conversation more difficult and anxiety-provoking.
“You know, I think telling your kids that they're at risk for anything is a hard conversation. And sometimes as a parent you feel like somehow you let them down because they’re – you made them. And not so much let them down, but it’s you're worried about the repercussions. You're worried about how they're going to feel about themselves. Are they going to still have that good positive self-image.”
–Participant 4, mother of 17-year-old child
Barrier: uncertainty
All parents described “navigating the uncertainty” as a major influence on the communication process, and for some it was their biggest challenge.
“It’s not like we can have the conversation and say, “This will happen,” or, “This won’t happen.” Nothing definitive in that conversation. And at her age now, like the world is very black and white. Something is right or wrong. It’s good or bad…It’s a very binary world when you’re seven. And so, 22q it’s not so black and white.”
–Participant 10, mother of 7-year-old child
Some parents stated that they would “absolutely not” be talking to their child about the possibility of developing a mental illness because their child would not be able to understand the nuances of what being at an “increased risk” meant.
Uncertainty was a direct barrier to the communication process but also indirectly affected communication through the emotional burden it placed on parents.
“It scares me of course, it’s probably one of the more concerning things on the list of possibilities. That might be because all the physiological things probably have presented themselves by now it’s just the mental health component that we don’t know.”
–Parent 6, father of 7-year-old child
Motivator: sense of control
Parents were motivated to consider communicating with their child about mental health in order to gain a sense of control. Many parents spoke of intentionally choosing to focus “on the things that [they] could influence.”
“It’s just a matter of recognizing that it’s still your child…there’s certain things you can control and certain things you can’t and so instead of fighting against the things you can’t control, embrace what you can control and do everything you can and put all of your efforts and focus into that because that’s where you can truly make a difference.”
–Parent 6, father of 7-year-old child
Deciding to focus on things that were within one’s control (e.g., the supports their child received) was a coping mechanism for some parents. These parents believed that “knowledge is power” and that by being proactive and making their child aware of their psychiatric risk, they could better protect their mental health together.
“I feel like sometimes when we’re proactive about things, it gives you a sense of control. To sort of get ahead of it and to feel like you can lay the groundwork for something…And being proactive about things, I think has, like has helped me…because it’s where – like you feel like you have some sense of control.”
–Parent 10, mother of 7-year-old child
Motivator: desire to normalize mental health
Parents wanted to normalize the possibility of developing a mental illness in order to be “open and honest” with their child and to lessen the impact of a possible mental illness diagnosis.
“The truth is that she does have a higher risk for developing something…I think that if we can sort of instill that awareness in her, to recognize what’s happening in herself, to communicate it, to seek support, to understand that she is supported. And just normalize it so that it’s not ever something that needs to be, you know secret.”
–Parent 10, mother of a 7-year-old child
Many parents used normalization to encourage their child’s self-acceptance. Parents wanted to “take that stigma away early on” so that their child didn’t feel “unique” or “different.”
Parents tried to normalize their child’s mental illness by drawing parallels between mental illness and other aspects of 22q11DS.
“The mental health piece is just another piece to her overall health picture, I get her to the cardiologist, I get her to the ENT, I also have to get her to counseling and that kind of thing.”
–Parent 5, mother of 8-year-old child
Motivator: sense of capability
Several parents felt more equipped for these conversations due to their career (e.g., education, allied health professions, psychology) or other experience working with people with disabilities. However, even these parents articulated that despite this experience, they would have benefitted from additional support.
“I'm an educator, so I think I’m in a different boat. So if I don’t know the answers, I’m going to find the answers. I think at times it would have been nice to say these are the things that could happen instead of looking and trying to find information.”
–Parent 4, mother of a 17-year-old child
Parents also expressed that certain personality traits—such as being “adaptable,” “proactive,” or a self-described “researcher”—made them feel less overwhelmed and more capable of engaging in conversations about mental health with their child.
Barrier/motivator: perception of risk
A child’s current emotional or behavioral state affected their parent’s perception of the likelihood for them to develop a mental illness. Parents of young children who were displaying symptoms of anxiety or depression worried that their child would develop other mental illnesses.
“All the behavior manifestations she’s having now…I almost feel like it’s inevitable or like some sort of dramatic mental illness is coming if not already kind of here.”
–Participant 5, mother of 8-year-old child
Conversely, parents were somewhat reassured when their child was showing no symptoms.
“Oh my kid’s been doing well. Maybe he won’t be in that group.”
–Parent 9, mother of a 9-year-old child
Overall, parents’ perception of their child’s psychiatric risk affected the immediacy with which they wished to talk to their children about mental health. The parents who described themselves as “in denial” about the psychiatric risk viewed this conversation as a remote possibility, whereas parents that were concerned about their child’s current mental health wanted to address this possibility with their child more immediately.
Barrier/motivator: 22q11DS as a part of the child’s identity
The degree to which parents perceived 22q11DS to be a part of their child’s identity varied: some were “proud of being 22q,” others did not want to “define” their child by their genetic condition. The degree of integration of 22q11DS into a child’s identity affected whether a parent wished to connect their conversation about mental health with 22q11DS or not.
“There’s a lot of things that we’re going to probably have to connect back to her diagnosis….And in fact, I think it’s important to have conversations with her about her condition. And then the implications for like mental health.”
–Parent 10, mother of 7-year-old child
“And so that’s kind of what our mental health conversations are. I don’t know that we always connect it to 22q, because it’s – that’s real for everyone. Everyone needs sleep. Everyone needs proper food.”
–Parent 9, mother of 9-year-old child
Communication
Communication—the act of talking about psychiatric manifestations of 22q11DS—seemed to be comprised of three intersecting components: content (what to say and the words to use), process (how to have the conversation), and outcome (what to do next).
Content
Parents felt that there was a “good way” or “a better way” to have these conversations and wanted health professionals to provide more directive support or recommendations about “what words to use.” This belief that there were “better” or “right” words to use seem to originate from a desire to ensure that their child could understand the information in a constructive way.
“Like all the words that are used are just really tricky…. I really want to find some good positive language around it… It’s hard to talk about something like that without it sounding negative, “Like you’re missing chromosomes,”and like, you know, it being a syndrome. And, I don’t know, it’s – the language is just problematic for me.”
–Participant 9, mother of 9-year-old child
“I often worry that she’s just confused…and that must feel so scary to her… that’s why I’m always trying to find like the words, the right words that will enter her mind and that she can process and it’s not going to be upsetting.”
–Parent 5, mother of 8-year-old child
Process
All parents expressed thoughts about when to initiate the conversation with their child; they described thinking about their child’s developmental (not chronological) age to guide when they wanted to initiate this conversation.
“I wouldn’t say it’s so much age, as it is just like her emotional maturity level to be able to cope with what, what we’re telling her.”
– Parent 10, mother of 7-year-old child
“Yeah she’s so young. She’s eight and she’s got diagnosis of mild intellectual disability so she’s not like, her comprehension is not like an eight year old it’s probably more like six, so I don’t think she would even understand the concept of mental illness.”
– Parent 5, mother of 8-year-old child
Several parents identified that a conversation about psychiatric manifestations of 22q11DS might easily be integrated with other important conversations that parents have with their children as they approach adolescence. Parents also recognized that there might be a greater need for their child to be aware of their increased risk at this point in their lives.
“I can see getting into the high school and tween years, when emotions are higher and they’re dealing with more, that it would be more important to like connect those dots and be like, “Hey, we have to be extra careful,”you know because…kids with 22q, jars are already a little full.”
– Parent 9, mother of 9-year-old child
Outcome
To feel prepared to talk to their child about mental illness, parents needed a sense of what the outcome of the conversation would be; what next steps would need to be taken and what supports were available to their child. Ideally, these supports would be arranged prior to the conversation with their child, in order for the parent to feel at ease and more confident.
“I think being told that you could suffer from mental illness, and setting us up with someone that we could – you know, a psychiatrist, or giving us options. You know, you research this, and you say OK, your kid could suffer from this, but what do you do as a parent? Where do you go?...I think that’s the key is knowing and being set up to be successful as to what are the next steps.”
– Parent 4, mother of 17-year-old child
“Well it would just kind of take that off of my chest…Just to know that that support is there and that I can access it without feeling the need or for it to get to the point where I'm just like really struggling.”
– Parent 7, mother of 9-year-old child
Recommendations from parents for desired support
While some parents reported receiving some degree of support regarding communicating with their child about their diagnosis of 22q11DS, none had received specific support around communicating with their child about psychiatric manifestations. Parents wanted support to be practical, ongoing, personalized, and provided by someone with expertise. See Box 1.
Box 1.
Recommendations from parents for desired support
|
Hands on and practical: Health professionals should discuss the specifics of what this conversation might look like and how to go about having it. Parents expressed interest in: an educational video showing a real engagement between a parent and child; a list of examples of communication dilemmas or miscommunications between a parent and child; and including the child with 22q11DS in conversations with health professionals “I mean it’s one thing for mom and dad to say it but I think it’s more empowering if she goes and has her own conversation and has her own questions and gets her own answers. I think it gives her more control over what she wants to do and her perception of things.” – Parent 6, father of 7-year-old child | |
|
Consistent and ongoing: Parents received great support when their child was first diagnosed with 22q11DS but ongoing support as their child grew older was not readily available. Parents felt that ongoing support would allow them to be proactive in communicating with their child rather than reactive and would remove the burden of initiating contact when in need of support. “I think that there’s a real lack of support for parents to have these conversations…Because you know, you go through like counseling and support early on… but then you know you have an appointment once a year, every two years, but then it comes up to a point where, well, this is something that would be nice to be able to sort of talk through.” – Parent 3, father of 11-year-old child | |
|
Personalized: Support is most helpful when it is personalized to the parent’s context, child, and family. Many parents recalled the personalized psychiatric genetic counseling they had previously received, and wanted that same level of personalization when receiving support around communicating with their child about mental illness I think we probably like sat there forever asking like all these questions that we had. [Chuckles] And [the genetic counselors] were really great about it. They sat and answered all the questions and took time with us and that was really helpful. And you don’t find that often with doctors. Like, you know especially with specialists. You’re in and out so quickly and they have patients to see and they’re on tight schedules and, yeah. But we were able to take our time with the genetic counselor and that was really, really helpful. –Parent 10, mother of a 7-year-old child | |
|
Someone with expertise: To provide effective support around communicating with their child, health professionals must 1) be knowledgeable about 22q11DS and 2) develop and maintain a trusting relationship with the parent(s). Nearly every parent had previously interacted with a health professional that “had no clue about 22q,” which eroded parents’ trust in the health professional and their ability to provide tailored, relevant support to their child. “I know that I’m taking my daughter to somebody who understands the complexities and the multifaceted, not approach but the various things that 22q affects as opposed to just the psychological aspect.” – Parent 6, father of 7-year-old child |
Discussion and conclusion
Discussion
We developed a theoretical model that describes parents’ perspectives on the process of communicating with their child about the psychiatric manifestations of 22q11DS in which communication is an ongoing process where dynamic contextual factors act as motivators or barriers to communication.
Though we found no previously published work on this specific topic, most elements of our model are robustly supported by data from studies in related areas (as described below), and by an (as yet) unpublished thematic analysis study of communication in the context of 22q11DS (Filiaggi et al., in preparation). However, our model combines these elements together in a novel manner that describes the process of communication in families.
Our finding that parents viewed communication with their children as an ongoing iterative process is supported by other studies examining parents’ experiences of communicating with their children about a genetic condition within the family (Metcalfe et al. 2008; Rowland and Metcalfe 2013). Similarly, with regard to the contextual factors we identified: uncertainty has been cited as a barrier for parents of children with sex chromosome aneuploidies in disclosing these diagnoses to their children (Dennis et al. 2015); parents’ desire to normalize their child’s psychiatric risk is supported by several pieces of other work (Forrest et al. 2008b; Plumridge et al. 2011; Metcalfe et al. 2011; Rowland and Metcalfe 2013), as is our related finding that parents’ reluctance to talk about psychiatric risk was often driven by desire to protect their children (Gallo et al. 2005; Forrest et al. 2008b; McConkie-Rosell et al. 2009; Metcalfe et al. 2011; Wiens et al. 2013; Suwannachat et al. 2020). Several elements of our model (sense of control, sense of capability) relate to empowerment—which is a core focus of clinical genetics services that aim to facilitate family communication (Mcallister et al. 2008, 2011a, b). While other work supports the concept that current symptomology affects perception of risk (Smith et al. 2002; Stuttgen et al. 2018), our connection of this to impact communication is more novel. Similarly novel is the relationship we identified between the degree to which a condition is part of one’s identity and communication.
The three intersecting components of content, process, and outcome that comprised the act of talking about psychiatric manifestations of 22q11DS also have support in the literature. The ideal timing for talking to their children about their genetic condition is a main consideration for parents, both in our study and in the literature as a whole (Gallo et al. 2005; Metcalfe et al. 2008, 2011; Wiens et al. 2013; Dennis et al. 2015; Suwannachat et al. 2020). Parents considered both their child’s overall stage of cognitive development and their ability to comprehend the information discussed (Metcalfe et al. 2008). Klitzman et al., referring to Huntington disease risk disclosure within families, claim that decisions to disclose genetic information are influenced by life cycle and medical course (Klitzman et al. 2007). This seems to also fit with our study population in that many parents considered the teen years, a time when a child might be gaining independence but also when their chances of developing a mental illness might be more imminent, was an appropriate time to broach this topic with their child. The difficulty parents experience with the content of a conversation with their children about genetic risk is reported in other studies (Rowland and Metcalfe 2013; Suwannachat et al. 2020). Parents’ concerns about the outcome of a conversation with their child (i.e. what supports were available to their child) are also supported by other pieces of work (Vo et al. 2018; Suwannachat et al. 2020).
As in previous studies, our participants identified an overall lack of support and guidance from health professionals to aid parents in the process of communicating with their children about genetic risk (Klitzman et al. 2007; Forrest et al. 2008b; Plumridge et al. 2011; Metcalfe et al. 2011; Mendes et al. 2016), and wanted health professionals to be directive with regards to the words to use in these conversations(Dennis et al. 2015; Suwannachat et al. 2020). As other authors have pointed out (Mendes et al. 2016), it would seem concrete examples of potentially useful language might be of great benefit to parents. It has also previously been acknowledged that families would benefit from ongoing support and genetic counseling throughout their child’s life (Bassett et al. 2011; Hart et al. 2016; Rizzo et al. 2020) and that parents wished to have support from someone who was knowledgeable on the multi-faceted aspects of 22q (Hart et al. 2016; Rizzo et al. 2020).
Conclusion
We generated a theoretical model which visually represents the process a parent might go through when considering initiating a conversation about the psychiatric manifestations of 22q11DS with their child. The individual elements of our model are robustly supported by data from other studies in related areas. However, the modeling of the way the elements interact is novel and potentially useful clinically.
Practice implications
This model may help equip genetics professionals to better support families in communicating effectively about this issue with their children, in order to improve health outcomes and family adaptation to 22q11DS. Indeed, adolescents who are at risk for psychosis have reported that discussion of their risk status acted to normalize pre-psychotic experiences and self-perception, and left them feeling reassured (Welsh and Brown 2013). Specifically, this model could help health professionals to better understand the experience of parents contemplating discussing their child’s diagnosis with their child. The model may also serve to assist parents in conceptualizing their own thoughts in a way that would facilitate further communication with their child.
Psychiatric disorders are commonly associated with genetic conditions (du Souich et al. 2009); therefore, our findings may be generalizable beyond the context of 22q11DS to other genetic conditions where psychiatric manifestations occur. Although an organizing model has value in that it acts as a parsimonious explanation of parent child communication and can act as a bridge to alterations in clinical practice, it is important to also focus on intervention strategies that would be helpful and feasible from the parental perspective. The suggestions from parents provided in this study could be used to help inform clinical practice in this area.
Supplementary Information
(DOCX 27 kb)
(PDF 481 kb)
Acknowledgements
The authors wish to thank all study participants for making this work possible. We also extend our gratitude to past and present members and volunteers of the Translational Psychiatric Genetics Group and the counselors at the ADAPT clinic. JA was supported by the BC Mental Health and Substance Use services Research Institute, and the Canada Research Chairs program. The authors offer gratitude to the Coast Salish Peoples, including the xʷməθkwəy̓əm (Musqueam), Skwxwú7mesh (Squamish), and Səl̓ílwətaʔ/Selilwitulh (Tsleil-Waututh) Nations, on whose traditional, unceded and ancestral territory we have the privilege of working.
Author contribution
Courtney B. Cook: conceptualization, methodology, formal analysis, investigation, data writing—original draft, writing—review and editing, project administration, funding acquisition. Caitlin Slomp: conceptualization, methodology, formal analysis, resources, writing—review and editing, supervision. Jehannine Austin: conceptualization, methodology, formal analysis, resources, writing—review and editing, supervision.
Funding
This work has been supported by the Jane Engelberg Memorial Fellowship Student Research Award, provided by the Engelberg Foundation to the National Society of Genetic Counselors, Inc. This work was also supported by the National Society of Genetic Counselors Psychiatric Special Interest Group Grant Award. JA was supported by BC Mental Health and Substance Use Services, and the Canada Research Chairs Program.
Availability of data and material
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. The Research Ethics Board at BC Children’s and Women’s Hospital approved this study (H20-01343).
Consent to participate
Informed consent was obtained from all patients for being included in the study. All patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Alugo T, Malone H, Sheehan A, et al. Development of a 22q11DS psycho-educational programme: exploration of the views, concerns and educational needs of parents caring for children or adolescents with 22q11DS in relation to mental health issues. Child Care Health Dev. 2017;43:527–535. doi: 10.1111/cch.12457. [DOI] [PubMed] [Google Scholar]
- Bassett AS, McDonald-McGinn DM, Devriendt K, et al. Practical guidelines for managing patients with 22q11.2 deletion syndrome. J Pediatr. 2011;159:332–339.e1. doi: 10.1016/J.JPEDS.2011.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baughman ST, Morris E, Jensen K, Austin J. Disclosure of psychiatric manifestations of 22q11.2 deletion syndrome in medical genetics: a 12-year retrospective chart review. Am J Med Genet Part A. 2015;167:2350–2356. doi: 10.1002/ajmg.a.37190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell IM, Sheppard SE, Crowley TB, et al. What is new with 22q? An update from the 22q and You Center at the Children’s Hospital of Philadelphia. Am J Med Genet Part A. 2018;176:2058–2069. doi: 10.1002/ajmg.a.40637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrion P, Semaka A, Batallones R, et al (2021) Reflections of parents of children with 22q11.2 Deletion Syndrome on the experience of receiving psychiatric genetic counseling: ‘Awareness to Act.’ J Genet Couns jgc4.1460. 10.1002/jgc4.1460 [DOI] [PubMed]
- Cuthbert A, Challenger A, Hall J, Bree M van den (2019) Information and genetic counselling for psychiatric risks in children with rare genomic disorders. medRxiv 19007294. 10.1101/19007294
- Dennis A, Howell S, Cordeiro L, Tartaglia N. “How should i tell my child?” Disclosing the diagnosis of sex chromosome aneuploidies. J Genet Couns. 2015;24:88–103. doi: 10.1007/s10897-014-9741-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dey I. Grounding grounded theory: guidelines for qualitative inquiry. San Diego: Academic Press; 1999. [Google Scholar]
- du Souich C, Austin JC, Friedlander R, Boerkoel CF. A novel syndrome with psychiatric features and review of malformation syndromes with psychiatric disorders. Am J Med Genet Part A. 2009;149A:713–721. doi: 10.1002/ajmg.a.32709. [DOI] [PubMed] [Google Scholar]
- Faux D, Schoch K, Eubanks S, et al. Assessment of parental disclosure of a 22q11.2 deletion syndrome diagnosis and implications for clinicians. J Genet Couns. 2012;21:835–844. doi: 10.1007/s10897-012-9535-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrest K, Simpson S, Wilson B, et al. To tell or not to tell: barriers and facilitators in family communication about genetic risk. Clin Genet. 2003;64:317–326. doi: 10.1034/j.1399-0004.2003.00142.x. [DOI] [PubMed] [Google Scholar]
- Forrest LE, Burke J, Bacic S, Amor DJ. Increased genetic counseling support improves communication of genetic information in families. Genet Med. 2008;103(10):167–172. doi: 10.1097/gim.0b013e318164540b. [DOI] [PubMed] [Google Scholar]
- Forrest LE, Curnow L, Delatycki MB, et al. Health first, genetics second: exploring families’ experiences of communicating genetic information. Eur J Hum Genet. 2008;16:1329–1335. doi: 10.1038/ejhg.2008.104. [DOI] [PubMed] [Google Scholar]
- Gaff C, Hodgson J. A genetic counseling intervention to facilitate family communication about inherited conditions. J Genet Couns. 2014;23:814–823. doi: 10.1007/s10897-014-9696-5. [DOI] [PubMed] [Google Scholar]
- Gallo A, Angst D, Knafl K, et al. Parents sharing information with their children about genetic conditions. J Pediatr Health Care. 2005;19:267–275. doi: 10.1016/j.pedhc.2005.05.008. [DOI] [PubMed] [Google Scholar]
- Hart SJ, Schoch K, Shashi V, Callanan N. Communication of psychiatric risk in 22q11.2 deletion syndrome: a pilot project. J Genet Couns. 2016;25:6–17. doi: 10.1007/s10897-015-9910-0. [DOI] [PubMed] [Google Scholar]
- Hercher L, Bruenner G. Living with a child at risk for psychotic illness: the experience of parents coping with 22q11 deletion syndrome: An exploratory study. Am J Med Genet Part A. 2008;146A:2355–2360. doi: 10.1002/ajmg.a.32466. [DOI] [PubMed] [Google Scholar]
- Hodgson J, Metcalfe S, Gaff C, et al. Outcomes of a randomised controlled trial of a complex genetic counselling intervention to improve family communication. Eur J Hum Genet. 2016;24:356. doi: 10.1038/EJHG.2015.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inglis A, Koehn D, McGillivray B, et al. Evaluating a unique, specialist psychiatric genetic counseling clinic: uptake and impact. Clin Genet. 2015;87:218–224. doi: 10.1111/cge.12415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karas DJ, Costain G, Chow EWC, Bassett AS. Perceived burden and neuropsychiatric morbidities in adults with 22q11.2 deletion syndrome. J Intellect Disabil Res. 2014;58:198–210. doi: 10.1111/J.1365-2788.2012.01639.X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klitzman R, Thorne D, Williamson J, et al. Disclosures of Huntington disease risk within families: patterns of decision-making and implications. Am J Med Genet Part A. 2007;143A:1835–1849. doi: 10.1002/ajmg.a.31864. [DOI] [PubMed] [Google Scholar]
- Martin N, Mikhaelian M, Cytrynbaum C, et al. 22q11.2 Deletion syndrome: attitudes towards disclosing the risk of psychiatric illness. J Genet Couns. 2012;21:825–834. doi: 10.1007/s10897-012-9517-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcallister M, Payne K, Macleod R, et al. Patient empowerment in clinical genetics services. J Health Psychol. 2008;13:895–905. doi: 10.1177/1359105308095063. [DOI] [PubMed] [Google Scholar]
- McAllister M, Dunn G, Todd C. Empowerment: qualitative underpinning of a new clinical genetics-specific patient-reported outcome. Eur J Hum Genet. 2011;19:125–130. doi: 10.1038/ejhg.2010.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcallister M, Wood A, Dunn G, et al. The genetic counseling outcome scale: a new patient-reported outcome measure for clinical genetics services. Clin Genet. 2011;79:413–424. doi: 10.1111/j.1399-0004.2011.01636.x. [DOI] [PubMed] [Google Scholar]
- McConkie-Rosell A, Melvin Heise E, Spiridigliozzi GA. Genetic risk communication: experiences of adolescent girls and young women from families with fragile X syndrome. J Genet Couns. 2009;18:313–325. doi: 10.1007/s10897-009-9215-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendes Á, Paneque M, Sousa L, et al. How communication of genetic information within the family is addressed in genetic counselling: a systematic review of research evidence. Eur J Hum Genet. 2016;24:315–325. doi: 10.1038/ejhg.2015.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metcalfe A, Coad J, Plumridge GM, et al. Family communication between children and their parents about inherited genetic conditions: a meta-synthesis of the research. Eur J Hum Genet. 2008;16:1193–1200. doi: 10.1038/ejhg.2008.84. [DOI] [PubMed] [Google Scholar]
- Metcalfe A, Plumridge G, Coad J, et al. Parents and children’s communication about genetic risk: a qualitative study, learning from families experiences. Eur J Hum Genet. 2011;19:640–646. doi: 10.1038/ejhg.2010.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monks S, Niarchou M, Davies AR, et al. Further evidence for high rates of schizophrenia in 22q11.2 deletion syndrome. Schizophr Res. 2014;153:231–236. doi: 10.1016/j.schres.2014.01.020. [DOI] [PubMed] [Google Scholar]
- Morris E, Inglis A, Friedman J, Austin J. Discussing the psychiatric manifestations of 22q11.2 deletion syndrome: an exploration of clinical practice among medical geneticists. Genet Med. 2013;15:713–720. doi: 10.1038/gim.2013.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy KC, Owen MJ. Velo-cardio-facial syndrome: a model for understanding the genetics and pathogenesis of schizophrenia. Br J Psychiatry. 2001;179:397–402. doi: 10.1192/bjp.179.5.397. [DOI] [PubMed] [Google Scholar]
- Niklasson L, Rasmussen P, Óskarsdóttir S, Gillberg C. Autism, ADHD, mental retardation and behavior problems in 100 individuals with 22q11 deletion syndrome. Res Dev Disabil. 2009;30:763–773. doi: 10.1016/j.ridd.2008.10.007. [DOI] [PubMed] [Google Scholar]
- Plumridge G, Metcalfe A, Coad J. Parents’ communication with siblings of children affected by an inherited genetic condition. J Genet Couns. 2011;20:374–383. doi: 10.1007/s10897-011-9361-1. [DOI] [PubMed] [Google Scholar]
- Rizzo R, Van den Bree M, Challenger A, et al. Co-creating a knowledge base in the “22q11.2 deletion syndrome” community. J. Community Genet. 2020;11:101. doi: 10.1007/S12687-019-00425-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rössler W. The stigma of mental disorders. EMBO Rep. 2016;17:1250–1253. doi: 10.15252/embr.201643041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowland E, Metcalfe A. Communicating inherited genetic risk between parent and child: a meta-thematic synthesis. Int J Nurs Stud. 2013;50:870–880. doi: 10.1016/j.ijnurstu.2012.09.002. [DOI] [PubMed] [Google Scholar]
- Smith JA, Michie S, Stephenson M, Quarrell O. Risk perception and decision-making processes in candidates for genetic testing for Huntington’s disease: an interpretative phenomenological analysis. J Health Psychol. 2002;7:131–144. doi: 10.1177/1359105302007002398. [DOI] [PubMed] [Google Scholar]
- Socha TJ. Parents, children, and communication. New York: Routledge; 2013. [Google Scholar]
- Socha TJ, Stamp GH. Parents and children communicating with society: managing relationships outside of home. New York: Routledge; 2009. [Google Scholar]
- Stoddard J, Niendam T, Hendren R, et al. Attenuated positive symptoms of psychosis in adolescents with chromosome 22q11.2 deletion syndrome. Schizophr Res. 2010;118:118–121. doi: 10.1016/j.schres.2009.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuttgen K, Dvoskin R, Bollinger J, et al. Risk perception before and after presymptomatic genetic testing for Huntington’s disease: not always what one might expect. Mol Genet Genomic Med. 2018;6:1140–1147. doi: 10.1002/mgg3.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suwannachat S, Wattanasirichaigoon D, Arunakul J, et al. Perspectives of adults with Klinefelter syndrome, unaffected adolescent males, and parents of affected children toward diagnosis disclosure: a Thai experience. J Community Genet. 2020;11:171–181. doi: 10.1007/s12687-019-00435-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorne S. Interpretive description: qualitative research for applied practice. 2. New York: Routledge; 2016. [Google Scholar]
- Thorne S, Kirkham SR, MacDonald-Emes J. Interpretive description: a noncategorical qualitative alternative for developing nursing knowledge. Res Nurs Health. 1997;20:169–177. doi: 10.1002/(SICI)1098-240X(199704)20:2<169::AID-NUR9>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- van den Bree MBM, Miller G, Mansell E, et al. The internet is parents’ main source of information about psychiatric manifestations of 22q11.2 deletion syndrome (22q11.2DS) Eur J Med Genet. 2013;56:439–441. doi: 10.1016/J.EJMG.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasileiou K, Barnett J, Thorpe S, Young T. Characterising and justifying sample size sufficiency in interview-based studies: systematic analysis of qualitative health research over a 15-year period. BMC Med Res Methodol. 2018;18:1–18. doi: 10.1186/s12874-018-0594-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vo OK, McNeill A, Vogt KS. The psychosocial impact of 22q11 deletion syndrome on patients and families: a systematic review. Am J Med Genet Part A. 2018;176:2215–2225. doi: 10.1002/ajmg.a.38673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vorstman JAS, Morcus MEJ, Duijff SN, et al. The 22q11.2 deletion in children: high rate of autistic disorders and early onset of psychotic symptoms. J Am Acad Child Adolesc Psychiatry. 2006;45:1104–1113. doi: 10.1097/01.chi.0000228131.56956.c1. [DOI] [PubMed] [Google Scholar]
- Welsh P, Brown S. ‘I’m not insane, my mother had me tested’: the risk and benefits of being labelled ‘at-risk’ for psychosis. Health Risk Soc. 2013;15:648–662. doi: 10.1080/13698575.2013.848846. [DOI] [Google Scholar]
- Wiens ME, Wilson BJ, Honeywell C, Etchegary H. A family genetic risk communication framework: guiding tool development in genetics health services. J Community Genet. 2013;4:233–242. doi: 10.1007/s12687-012-0134-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 27 kb)
(PDF 481 kb)
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.