Highlights
-
•
The use of clinical prediction models (CPMs) to personalise interventions varies.
-
•
We reviewed 32 CPM-guided lifestyle interventions to prevent cardiovascular disease.
-
•
CPMs were mainly used to determine the intervention’s type, rarely its intensity.
-
•
CPMs were supplemented with univariable risk factors, relative risk estimates, etc.
-
•
Often reporting lacked detail and designs were unfit to assess the CPM’s impact.
Keywords: Cardiovascular diseases/prevention and control; Behavioral medicine; Decision support techniques; Models, cardiovascular; Patient-specific modeling
Abstract
This study aimed to systematically review the use of clinical prediction models (CPMs) in personalised lifestyle interventions for the prevention of cardiovascular disease. We searched PubMed and PsycInfo for articles describing relevant studies published up to August 1, 2021. These were supplemented with items retrieved via screening references of citations and cited by references. In total, 32 studies were included. Nineteen different CPMs were used to guide the intervention. Most frequently, a version of the Framingham risk score was used. The CPM was used to inform the intensity of the intervention in five studies (16 %), and the intervention’s type in 31 studies (97 %). The CPM was supplemented with relative risk estimates for additional risk factors in three studies (9 %), and relative risk estimates for intervention effects in four (13 %). In addition to the estimated risk, the personalisation was determined using criteria based on univariable risk factors in 18 studies (56 %), a lifestyle score in three (9 %), and a physical examination index in one (3 %). We noted insufficient detail in reporting regarding the CPM’s use in 20 studies (63 %). In 15 studies (47 %), the primary outcome was a CPM estimate. A statistically significant effect favouring the intervention to the comparator arm was reported in four out of eight analyses (50 %), and a statistically significant improvement compared to baseline in five out of seven analyses (71 %). Due to the design of the included studies, the effect of the use of CPMs is still unclear. Therefore, we see a need for future research.
1. Introduction
Cardiovascular disease (CVD) was the cause of an estimated 17.80 million deaths worldwide in 2017, according to the global burden of disease report published in 2018 (Roth et al., 2018). In comparison, the total number of deaths due to neoplasms (mainly cancer) was estimated at 9.56 million. Moreover, two CVDs, coronary artery disease and stroke, ranked respectively first and third in terms of estimated years of life lost (Roth et al., 2018).
An association between lifestyle, i.e. behavioural patterns, and CVD has been reported in several previous studies. For example, not smoking, increased fruit and vegetable intake, and increased leisure-time physical activity have been linked to less risk in meta-analyses (Aune et al., 2018, He et al., 2007, Sattelmair et al., 2011). Moreover, adhering to a healthy lifestyle, i.e. combining different health behaviours, has been reported to be associated with an estimated CVD risk reduction of 66 % (95 % CI: 59 – 72 %) via meta-analysis (Barbaresko et al., 2018).
Clinical prediction models (CPMs) estimate a diagnostic or prognostic clinical outcome based on relevant variables, such as patient characteristics, disease indicators, and treatment domains (Steyerberg, 2019). Due to the joint effects of separate risk factors, estimation of CVD risk using CPMs is deemed preferable to univariable approaches (Alderman, 1993, Jackson et al., 2005).
Well-validated CPMs have been endorsed by clinical guidelines. Examples are the systematic coronary risk evaluation (SCORE) estimator (Conroy et al., 2003, Piepoli et al., 2016, Systematic Coronary Risk Evaluation 2 Working Group and European Society of Cardiology Cardiovascular Risk Collaboration, 2021, Visseren et al., 2021) in Europe, the Framingham risk score (FRS) pooled cohort equations (PCE) (Arnett et al., 2019, Goff et al., 2014) in the United States of America, the QRISK estimator (Hippisley-Cox et al., 2008, Hippisley-Cox et al., 2017, National Institute for Health and Care Excellence, 2014) in the United Kingdom, and PREDICT in New Zealand (New Zealand Ministry of Health, 2018, Pylypchuk et al., 2018).
In addition to risk assessment and communication of this risk to the patient, these CPMs may be used to suggest an action to reduce CVD risk. After all, knowing the risk estimate does not change it, changing behaviours or medications do. Contrary to a one size fits all approach, the intervention may differ based on the CPM’s estimate, i.e. CPMs may be used to personalise the intervention.
A CPM may inform the intervention in a quantitative manner. People with a higher estimated risk may receive more intensive lifestyle support. For example, higher risk estimates may be linked to higher follow-up frequencies.
Additionally, one can imagine a CPM informs the intervention in a qualitative manner. For example, the CPM’s estimate for a particular participant may be adjusted to reflect hypothetical intervention effects. Those with the largest expected risk reductions may be given priority, if the patient and guiding physician are in accordance.
In this review, we focus on the use of CPMs to personalise lifestyle interventions for CVD prevention by suggesting an action. We aim to systematically review the literature to provide an overview of studies with such interventions, and analyse how CPMs are currently being used.
2. Methods
2.1. Study protocol registration
The study protocol was not registered.
2.2. Search strategy
We conducted a number of scoping searches for publications up to August 1, 2021 matching our inclusion criteria in the PubMed database and in the American Psychological Association PsycInfo database. We constructed search strings using various terms to capture three main concepts: CVD, a lifestyle-oriented prevention strategy, and prediction modelling. Table A1 in appendix A presents the search strings that led to at least one retained publication after screening based on title and abstract, which was conducted by a single reviewer (AB). The database searches were supplemented with items retrieved via non-systematic screening of references and cited by references. One reviewer (AB) did an initial screening based on full-text. If a publication was considered suitable to be included or when there were doubts whether to include or exclude a publication, a minimum of two reviewers read independently the full-text (AB, BS, IB). A final decision was made based on agreement between at least two reviewers. References of publications excluded based on full-text are provided in appendix B.
2.3. Eligibility criteria
The intervention described in the study had to focus on lifestyle change as a means for CVD prevention, and comprise a risk estimate of a CPM used as part of the intervention. Studies that used a risk estimate of a CPM exclusively as an eligibility criterion or to communicate risk were excluded. Studies that targeted specific patient populations other than people with CVD, such as people with diabetes, were excluded as well. All studies selected had to be described in a full-text publication in English. Finally, if multiple publications were derived from one unique intervention, we included only the main publication.
2.4. Data extraction and synthesis
Data extraction and synthesis was performed jointly by two reviewers (AB, IB).
The study name, citation, and region were extracted, and the study design was noted.
The following sample characteristics were extracted: the total number of participants at baseline, the type of population targeted, what age criterion for eligibility was applied, whether an inclusion criterion based on CVD risk was applied, and whether an exclusion criterion based on a history of CVD was applied. We summarised the lifestyle intervention described in the study, as well as the comparator, if the study was a randomised controlled trial (RCT). We classified the lifestyle intervention domains as related to smoking, physical activity, nutrition, alcohol intake, psychological well-being, medication adherence, or other. Moreover, we noted whether medications were treatment options, including those via referral.
In addition, we extracted what CPM was used in the intervention, noted which data elements, if any, were used to supplement the CPM estimate, and classified whether the suggested action based on the CPM was to determine the lifestyle intervention’s intensity and / or its type. The lifestyle intervention’s intensity refers to quantitative differences, for example, a higher follow-up frequency for those at higher risk. The lifestyle intervention’s type refers to qualitative suggestions, such as indicating which lifestyle domain is associated with most gains in terms of risk reduction. Note that we are considering suggestions based on the CPM. These are not necessarily carried forward in the actual treatment plan, for example, if smoking cessation would be preferable according the CPM, but the participant does not wish to quit smoking. Furthermore, we indicated whether reporting lacked detail concerning the description of the CPM and its use. Arguments are provided in appendix C.
Lastly, we extracted the length of follow-up, classified the primary outcome(s) as related to mortality, morbidity, CPM estimate, biomarkers (blood pressure, lipids, other), anthropometrics, lifestyle (smoking, physical activity, nutrition, other), medications, or other, and noted the results.
Frequencies and proportions were tabulated when appropriate to provide an overview.
2.5. Reporting
Reporting followed guidance provided by the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement (Page et al., 2021). The completed checklist for abstracts and main text are provided in appendix D.
3. Results
3.1. Search results
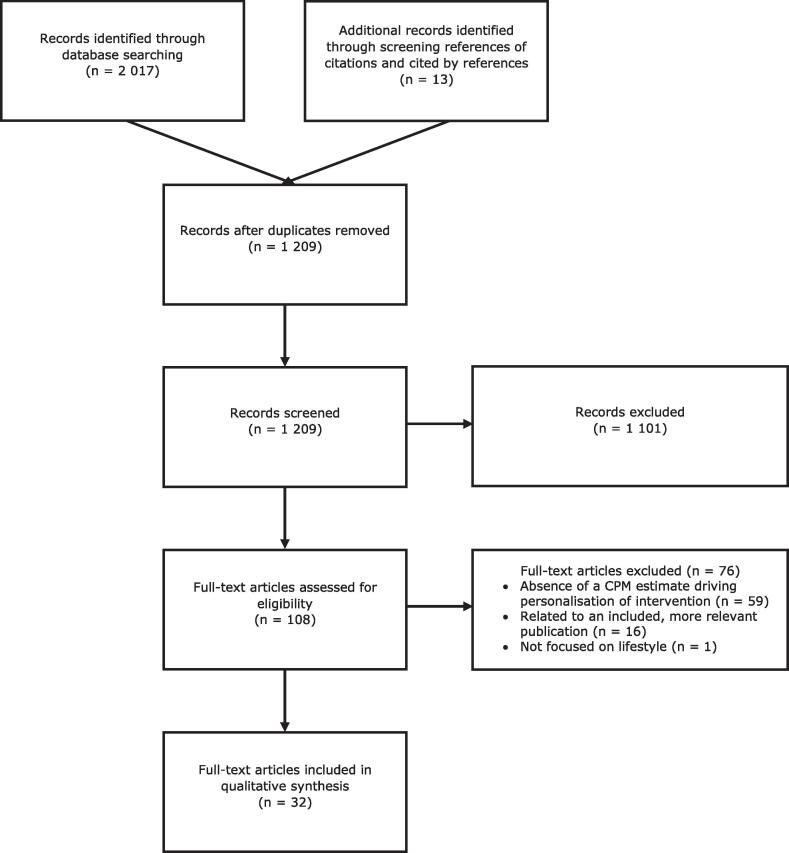
Fig. 1 presents an overview of the selection process, based on the preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow-diagram template (Liberati et al., 2009). There were 2 017 items identified via database searches, and 13 by screening references of citations and cited by references. In total, there were 1 209 unique items screened. There were 1 101 items excluded based on title and abstract, and 108 were selected for a more in-depth assessment. Based on full-text, we excluded an additional 76 items: 59 due to the absence of a CPM estimate linked to a suggested action in the intervention, 16 due to their relation with an included, more relevant publication, and one which was not focused on lifestyle (references are provided in appendix B). This final selection led to a total of 32 included publications.
Fig. 1.
PRISMA flow-diagram.
3.2. Data extraction and synthesis
Table 1 provides the following information per study: study name (if any), citation, region, study design, participants, a description of the intervention and comparator (if the study design was a RCT), a description of aspects concerning the CPM used in the intervention, and a summary regarding the primary outcome(s). Publications are listed chronologically, ranging from 1994 to 2020. Seventeen (53 %) studies were located in Europe, ten (31 %) in North America, three (9 %) in Oceania, and two (6 %) in Asia. Regarding the study design, 20 out of 32 studies (63 %) were RCTs and 12 (38 %) were single-arm studies.
Table 1.
Synthesis: study name (if any), citation, region, study design, participants, intervention and comparator (if RCT), CPM, supplement, and use of CPM, primary outcome(s).
| Study name (if any) | Citation | Region | Study design | Participants | Intervention and comparator (if RCT) | CPM, supplement, and use of CPM | Primary outcome(s) | |
|---|---|---|---|---|---|---|---|---|
| 1. | British FHS | (Wood et al., 1994) | UK | RCT |
|
|
|
|
| 2. | – | (Ketola et al., 2001) | FI | RCT |
|
|
|
|
| 3. | – | (Edelman et al., 2006) | USA | RCT |
|
|
|
|
| 4. | Hartslag Limburg | (Harting et al., 2006) | NL | RCT |
|
|
|
|
| 5. | Simon Fraser heart health report card system | (Wister et al., 2007) | CA | RCT |
|
|
|
|
| 6. | ARRIBA-Herz | (Krones et al., 2008) | DE | RCT |
|
|
|
|
| 7. | Inter99 study | (Jørgensen et al., 2014) | DK | RCT |
|
|
|
|
| 8. | Healthy hearts | (Richardson et al., 2008) | UK | Single-arm study |
|
|
|
|
| 9. | REACH OUT | (Benner et al., 2008) | EU | RCT |
|
|
|
|
| 10. | IMPALA | (Koelewijn-van Loon et al., 2009) | NL | RCT |
|
|
|
|
| 11. | COHRT | (Nolan et al., 2011) | CA | RCT |
|
|
|
|
| 12. | HAPPY / MyCLIC: NL | (Hofstra et al., 2011, Yousuf et al., 2019) | NL | Single-arm study |
|
|
|
|
| 13. | Heart to heart | (Sheridan et al., 2011) | USA | RCT |
|
|
|
|
| 14. | Fremantle primary prevention study | (Brett et al., 2012) | AU | RCT |
|
|
|
|
| 15. | PreCardio | (Claes et al., 2013) | BE | RCT |
|
|
|
|
| 16. | ANCHOR | (Cox et al., 2013) | CA | Single-arm study |
|
|
|
|
| 17. | Heart to health | (Keyserling et al., 2014) | USA | RCT |
|
|
|
|
| 18. | My family medical history and me (pilot) | (Imes et al., 2015) | USA | Single arm study (pilot) |
|
|
|
|
| 19. | Protecting healthy hearts program / GARDIAN | (Carrington and Stewart, 2015) | AU | Single-arm study |
|
|
|
|
| 20. | – | (Abbas et al., 2015) | UK | Single-arm study |
|
|
|
|
| 21. | IEHPS (pilot) | (Liu et al., 2015) | CN | RCT (pilot) |
|
|
|
|
| 22. | INTEGRATE (pilot) | (van den Brekel-Dijkstra et al., 2016) | NL | Single-arm study (pilot) |
|
|
|
|
| 23. | – | (Siren et al., 2016) | FI | Single-arm study |
|
|
|
|
| 24. | CHARLAR | (Krantz et al., 2017) | USA | Single-arm study |
|
|
|
|
| 25. | DECADE | (Tinsel et al., 2018) | DE | RCT (pilot) |
|
|
|
|
| 26. | ACTIVATE | (Oddone et al., 2018) | USA | RCT |
|
|
|
|
| 27. | HAPPY / MyCLIC: AZM | (Yousuf et al., 2019) | NL | Single-arm study |
|
|
|
|
| 28. | HAPPY / MyCLIC: London | (Khanji et al., 2019, Yousuf et al., 2019) | UK | RCT |
|
|
|
|
| 29. | – | (Kavita et al., 2020)* | IN | Single-arm study |
|
|
|
|
| 30. | INTEGRATE | (Stol et al., 2020) | NL | RCT |
|
|
|
|
| 31. | CONNECT | (Redfern et al., 2020) | AU | RCT |
|
|
|
|
| 32. | – | (Kwon et al., 2020) | USA | Single-arm study |
|
|
|
|
ACTIVATE = a coaching by telephone intervention for veterans and care team engagement; ANCHOR = a novel approach to cardiovascular health by optimizing risk management; ARRIBA-Herz = Aufgabe gemeinsam definieren, Risiko subjektiv, Risiko objektiv, Information über Präventionsmöglichkeiten, Bewertung der Präventionsmöglichkeiten und Absprache über weiteres Vorgehen – Herz (define task together, subjective risk, objective risk, information about prevention options and agreement on further action - heart); ATP = adult treatment panel; AU = Australia; AZM = Academisch Ziekenhuis Maastricht (Maastricht University Medical Centre +); BE = Belgium; BMI = body mass index; CA = Canada; CHARLAR = community heart health actions for Latinos at risk; CMD = cardiometabolic disease; CN = China; COHRT = community outreach heart health and risk reduction trial; CONNECT = consumer navigation of electronic cardiovascular tools; CPM = clinical prediction model; CVD = cardiovascular disease; DE = Deutschland (Germany); DECADE = decision-aid, action planning, and follow-up support for patients to reduce the 10-year risk of CVD; DK = Denmark; EU = European Union; FHS = family heart study; FI = Finland; FRS = Framingham risk score; GARDIAN = green, amber, red delineation of risk and need; GP = general practitioner; HAPPY = heart attack prevention program for you; ICVD = ischemic cardiovascular disease; IEHPS = individualised electronic healthcare prescription software; IHD = ischemic heart disease; IMPALA = improving patient adherence to lifestyle advice; IN = India; MyCLIC = my cardiac lifestyle intervention coach; NL = Netherlands; PCE = pooled cohort equations; PROCAM = prospective cardiovascular Münster study; RCT = randomised controlled trial; REACH OUT = risk evaluation and communication health outcomes and utilization trial; SCORE = systematic coronary risk evaluation; SMS = short message service; TAU = Treatment as usual; UK = United Kingdom; UKPDS = United Kingdom prospective diabetes study; USA = United States of America; WHO / ISH = World Health Organization / International Society of Hypertension.
* This publication described two studies, the second did not satisfy our eligibility criteria, and was consequently not included.
Table 2, Table 3, Table 4 summarise different aspects of the studies. Table 2 presents an overview of the participants targeted by the studies, intervention domains possible to select, and the use of decision-aids. The total number of participants of the reviewed studies ranged from 15 to 59 616. Most studies targeted primary care patients (50 %), the general population (13 %), or groups based on the participant’s occupation (13 %). In the majority of the studies (72 %), an eligibility criterion based on age (excluding specifying an age ≥ 18 years) was applied. Furthermore, in 59 % of the studies, potential participants were included if they had a high CVD risk. Additionally, in half of the studies (50 %), potential participants with known CVD were excluded. Most studies included multiple intervention domains, and smoking cessation, physical activity, and nutrition were included in more than 90 % of studies. About one-third of the interventions included alcohol intake, psychological well-being, and / or medication adherence. Less frequently, other domains, such as sleep or goal setting, were considered. In the majority of the interventions (72 %), medications were considered. Decision-aids were used in six interventions (19 %).
Table 2.
Summary of study participants, intervention domains, and decision-aids.
| n (%) | |||
|---|---|---|---|
| Participants | Target population | Primary care patients | 16 (50 %) |
| General population | 4 (13 %) | ||
| Based on occupation | 4 (13 %) | ||
| Other | 8 (25 %) | ||
| Eligibility criteria | Age | 23 (72 %) | |
| Inclusion based on CVD risk | 19 (59 %) | ||
| Exclusion based on CVD | 16 (50 %) | ||
| Intervention domains | Lifestyle | Smoking | 30 (94 %) |
| Physical activity | 30 (94 %) | ||
| Nutrition | 31 (97 %) | ||
| Alcohol intake | 10 (31 %) | ||
| Psychological well-being | 10 (31 %) | ||
| Medication adherence | 9 (28 %) | ||
| Other | 5 (16 %) | ||
| Medications | 23 (72 %) | ||
| Decision-aids | 6 (19 %) | ||
| Total number of studies | 32 (100 %) |
CVD = cardiovascular disease.
Table 3.
Breakdown of the CPMs used in each study, how they were supplemented and used, and whether reporting was lacking detail.
| n (%) | ||
|---|---|---|
| Name | British FHS risk score (Thompson et al., 1996) | 1 (3 %) |
| Copenhagen risk score (Thomsen et al., 2001) | 1 (3%) | |
| CPM for CMD (Alssema et al., 2012) | 1 (3 %) | |
| CPM for ICVD (Wu et al., 2006) | 1 (3%) | |
| FRS Anderson (Anderson et al., 1991) | 5 (16 %) | |
| FRS Anderson (modified) (New Zealand Guidelines Group, 2003) | 1 (3 %) | |
| FRS ATP III (National Cholesterol Education Program Expert Panel, 2002) | 5 (16 %) | |
| FRS Wilson (Wilson et al., 1998) | 3 (9 %) | |
| FRS PCE (Goff et al., 2014) | 1 (3 %) | |
| Healthy heart score (Chiuve et al., 2014) | 1 (3 %) | |
| Know your number (Hu and Root, 2005) | 1 (3 %) | |
| MyHealtheVet’s health age (Martin and Sartori, 2014) | 1 (3 %) | |
| North Karelia risk score (modified) (Suomen Sydäntautiliitto et al., 1986) | 2 (6 %) | |
| SCORE (Conroy et al., 2003) | 4 (13 %) | |
| SCORE (modified) (Van der Kalken and Kraaijenhagen, 2007) | 1 (3 %) | |
| PROCAM (Assmann et al., 2002) | 2 (6 %) | |
| QRISK2 (Hippisley-Cox et al., 2008) | 2 (6 %) | |
| UKPDS (Stevens et al., 2001) | 1 (3 %) | |
| WHO / ISH (World Health Organization, 2007) | 1 (3 %) | |
| Supplement | Univariable risk factors | 18 (56 %) |
| Relative risk estimates for additional risk factor (s) | 3 (9 %) | |
| Relative risk estimates for intervention effect (s) | 4 (13 %) | |
| Lifestyle score | 3 (9 %) | |
| Physical examination index | 1 (3 %) | |
| Use | Determine intervention intensity | 5 (16 %) |
| Determine intervention type | 31 (97 %) | |
| Insufficient detail in reporting | 20 (63 %) | |
| Total number of studies | 32 (100 %) |
ATP = adult treatment panel; CMD = cardiometabolic disease; CPM = clinical prediction model; FHS = family heart study; FRS = Framingham risk score; ICVD = ischemic cardiovascular disease; PCE = pooled cohort equations; PROCAM = prospective cardiovascular Münster study; SCORE = systematic coronary risk evaluation; UKPDS = United Kingdom prospective diabetes study; WHO / ISH = World Health Organization / International Society of Hypertension.
Table 4.
Summary of reported statistically significant effects in favour of the intervention concerning the primary outcomes.
| Intervention versus comparator | Comparison to baseline | |||
|---|---|---|---|---|
| n (%) | n (%) | |||
| Mortality / morbidity | 0 / 1 (0 %) | – | ||
| CPM estimate | 4 / 8 (50 %) | 5 / 7 (71 %) | ||
| Biomarkers | Blood pressure | 1 / 2 (50 %) | 1 / 1 (100 %) | |
| Lipids | 0 / 2 (0 %) | 1 / 1 (100 %) | ||
| Other | Glucose | 0 / 1 (0 %) | 0 / 1 (0 %) | |
| Carotid-femur pulse wave velocity | 0 / 1 (0 %) | – | ||
| Anthropometrics | 1 / 2 (50 %) | 0 / 1 (0 %) | ||
| Lifestyle | Smoking | 1 / 1 (100 %) | 1 / 2 (50 %) | |
| Physical activity | 1 / 1 (100 %) | 1 / 1 (100 %) | ||
| Nutrition | 1 / 1 (100 %) | 1 / 1 (100 %) | ||
| Other | Medication adherence | 0 / 1 (0 %) | – | |
| Patient activation | 3 / 3 (100 %) | – | ||
| Medications | 1 / 1 (100 %) | – | ||
| Other | Detection CMD | 1 / 1 (100 %) | – | |
| Decisional regret | 1 / 1 (100 %) | – |
CMD = cardiometabolic disease; CPM = clinical prediction model.
Table 3 presents a breakdown of the CPMs used in the studies, as well as how they were used to personalise the interventions, and whether and how supplementary sources were used in the personalisation. Fifteen studies (47 %) reported using a version of the FRS (Anderson et al., 1991, Goff et al., 2014, National Cholesterol Education Program Expert Panel, 2002, New Zealand Guidelines Group, 2003, Wilson et al., 1998), while a version of the SCORE estimator (Conroy et al., 2003, Van der Kalken and Kraaijenhagen, 2007) was used in five (16 %). The North Karelia risk score (modified) (Suomen Sydäntautiliitto et al., 1986), prospective cardiovascular Münster study (PROCAM) estimator (Assmann et al., 2002), and QRISK2 (Hippisley-Cox et al., 2008) were each used twice (6 %). The other CPMs were used only in one study each (3 %). The CPM was most often, in 18 interventions (56 %), supplemented with univariable risk factors. For example, part of the intervention described by Abbas et al. (2015) consisted of a referral to a weight management specialist only if the participant had a CPM estimate ≥ 10 % as well as a BMI ≥ 28. Three studies (9%) reported applying relative risk estimates to the risk estimated by the CPM to account for additional risk factors not included in the CPM. For example, Cox et al. (2013) reported multiplying the CPM’s estimate by two if the participant had relatives with premature CVD. Four studies (13 %) reported using relative risk estimates from literature to calculate the expected reduction in risk. For example, in the decision-aid included as a supplementary material by Krones et al. (2008), a relative risk reduction of approximately 35 % for quitting smoking was reported. The lifestyle score was used in three related interventions (9 %), part of the heart attack prevention program for you (HAPPY) / my cardiac lifestyle intervention coach (MyCLIC). Reporting lacked detail to understand thoroughly how this lifestyle score was constructed and used. Lastly, the use of a physical examination index was reported once (3 %), by Liu et al. (2015). No definition was provided. Regarding the use of the CPM, we categorised five (16 %) interventions as using the CPM in a quantitative manner to determine the intervention’s intensity, and 31 (97 %) in a qualitative manner to determine the intervention’s type. Finally, we deemed reporting concerning the use of the CPM lacked detail in 20 studies (63 %) (argumentation provided in appendix C).
Table 4 summarises the effectiveness of the interventions as reported by the studies by focusing on the primary outcomes and whether the improvement effected by the intervention was statistically significant. In RCTs, the outcome measures in the intervention arm were compared against the control arm (with the exception of analyses by Keyserling et al., 2014, Stol et al., 2020), whilst in single-arm studies the outcome measures at follow-up were compared against baseline. Various outcome measures were investigated in the reviewed studies. Ten studies (31 %) did not specify a primary outcome. A composite measure concerning mortality and morbidity, i.e. lethal and non-lethal ischemic heart disease events, was reported as a primary outcome in one study. No statistically significant difference between intervention and comparator was found. The most common primary outcome was risk estimated by a CPM. Regarding this outcome, four out of eight studies (50 %) in which the intervention condition and comparator condition were contrasted reported a statistically significant difference in favour of the intervention. These four do not include the mixed results described by Wister et al. (2007). The authors reported a statistically significant difference between the intervention and comparator in the primary prevention group, yet not in the secondary prevention group. Further, five out of seven studies (71 %) in which the comparison regarding risk estimated by a CPM was made to baseline reported a statistically significant improvement. These five do not include the results described by Siren et al. (2016) and by Stol et al. (2020). In the former publication, a statistically significant effect was found in only one of the two CPMs used, noting that the non-significant effect had a p-value of 0.060. In the latter publication, a statistically significant effect was found only after adjusting for aging. Other primary outcomes were biomarkers, anthropometrics, and lifestyle behaviours affecting risk, namely smoking, physical activity, nutrition, medication adherence, and patient activation. In general, the effectiveness of the interventions in terms of statistical significance concerning these outcomes was mixed. Finally, one RCT reported an increase in prescriptions of cardiometabolic medications and an improved detection of cardiometabolic disease, and one RCT reported a statistically significant reduction in decisional regret, contrasting the intervention condition to the comparator condition.
4. Discussion
We systematically reviewed existing literature concerning the use of CPMs to personalise lifestyle interventions for the prevention of CVD. Thirty-two studies were included, of which 20 were RCTs (63 %) and 12 were single-arm studies (38 %). Nineteen different CPMs were employed. Notably, in 15 out of 32 interventions (47 %), a version of the FRS was used. Most often, in 18 out of 32 interventions (56 %), the CPM estimates were supplemented with univariable risk factor values. Multiplying the CPM estimate by relative risk estimates of risk factors not included in the model was applied in three studies (9 %), and by relative risk factor estimates of intervention effects in four studies (13 %). Additionally, in three studies (9 %), the CPM estimate was supplemented with a lifestyle score, and in one study (3 %), with a physical examination index. The CPM estimate was used to determine the intervention’s intensity in just five out of 32 studies (16 %). In most studies, 31 out of 32 (97 %), the CPM estimate was used to inform the type of the intervention. Reporting regarding the use of the CPM was deemed lacking detail in 20 out of 32 studies (63 %). No studies were found in which the usage of the CPM was the only experimental variable that varied, therefore, it is inconclusive what effect the CPM in the intervention had. The most commonly used primary outcome were CPM estimates. In four out of eight (50 %) of the analyses comparing the intervention condition and comparator condition, a statistically significant effect in favour of the intervention was reported. Moreover, in five out of seven (71 %) of the analyses with a comparison to baseline, a statistically significant improvement was found.
Considering a quantitative suggestion based on a CPM estimate, both CPMs based on causal or non-causal associations may be used. Remarkably, only a few interventions used the information provided by the CPM estimate in this manner.
Considering the route from a CPM estimate to a suggested qualitative action, different approaches are possible. The CPM estimate may be combined with univariable risk factors to inform the decision. One must be cautious when applying a univariable risk factor cut-off value when a multivariable estimate indicates the individual has a high risk, in order not to exclude those at high risk by having moderately elevated values on multiple risk factors (Alderman, 1993, Jackson et al., 2005). However, at times, it is advised to combine information from a CPM estimate and univariable risk factors, for example, when considering the initiation of antihypertensive medications (e.g., Arnett et al., 2019). Furthermore, when CPMs are used to predict a hypothetical intervention effect to inform the treatment plan, a foundation in causal inference is necessitated (Hernán et al., 2019). A CPM may be combined with relative risk reduction estimates from RCTs, as described by Harrell and Lazzeroni (2017). To derive causal CPMs based on observational data, other techniques have been developed (Lin et al., 2021, Shalit et al., 2017). Additionally, suggested actions may be based on combining non-causal CPMs and decision-curve analyses (Vickers and Elkin, 2006). van der Leeuw and colleagues advocate for using a CPM and accompanying decision-curve analysis for contrasting expected treatment benefits and harms of medications to tailor CVD prevention treatment (van der Leeuw et al., 2014). With the exception of supplementing the CPM estimate with univariable risk factors, these techniques were rarely used in the included studies.
It is worth noting that the information provided by the CPM may be incorporated into a decision-aid. A Cochrane review reported strong evidence indicating that patients using a decision-aid were more knowledgeable of their options and which option they preferred (Stacey et al., 2017). Just six (19 %) of the interventions included used a decision-aid.
Importantly, cultivating a healthy lifestyle is a process. It is likely that the effects of lifestyle interventions diminish over time without sustained efforts. Harting et al. (2006), for example, reported a waning in the decrease of fat intake at 18 months compared to 4 months. Recurrence of unhealthy behaviours should be anticipated in lifestyle interventions, since the patterns are not forgotten, but rather inhibited (Bouton, 2014). A healthy lifestyle is not an end-point you achieve, but a process with ups and downs, requiring continuous efforts. Providing intermediate feedback of the effect of the participant’s behavioural changes on the CPM-based estimated risk may aid the participant to understand this dynamic. This was done in the publications by Edelman et al., 2006, Wister et al., 2007, Khanji et al., 2019, Redfern et al., 2020, and Kwon et al. (2020).
Unfortunately, in none of the studies, the use of a CPM was the only experimental variable that varied. Therefore, it is inconclusive what the effect of the CPM or differential use of the CPM is. Impact studies are needed (Moons et al., 2009). These should not only address a comparison of an intervention condition with a CPM to a comparator condition without a CPM, but also the manner in which a CPM estimate is translated to a suggested action.
Our review was hindered by insufficient detail in reporting concerning the CPM, possibly because the study did not focus on the implementation of the CPM. For example, Ketola et al. (2001) wrote regarding the modified North Karelia risk score “the use of this score assists the staff in recognising, informing and treating high-risk patients” and “an individual multifactorial intervention programme was tailored for each patient according to the risk factor status and needs of the patients”. While this indicates the CPM estimate was used to inform the intervention, it is not clear how. More recently, two extensions to guidelines regarding studies using artificial intelligence have been published: standard protocol items: recommendations for interventional trials - artificial intelligence (SPIRIT-AI) (Cruz Rivera et al., 2020) and consolidated standards of reporting trials – artificial intelligence (CONSORT-AI) (Liu et al., 2020). Whereas the included CPMs may not be considered artificial intelligence, these guidelines do provide guidance to report the application of the CPM in more detail.
Furthermore, it is likely that the listed studies are not exhaustive. Only two databases were searched (PubMed and PsycInfo). However, considering the broadness of these databases, we deem the selected studies do provide a sufficient indication of the usage of CPMs in this type of intervention.
In addition, we acknowledge that statistical significance is likely not the most relevant criterion to determine the intervention’s effectiveness. It has been criticised by statisticians for dichotomising research results based on arbitrary thresholds (Amrhein et al., 2019), and statistically significant effects might fall short from being clinically significant. Moreover, cost-effectiveness is disregarded (van Giessen et al., 2017). Nonetheless, we discussed statistical significance, since we considered the included studies too heterogeneous for meta-analysis, and most often statistical significance played a part in the publication to interpret whether the intervention was effective.
Further, we did not complete a risk of bias assessment. Although this would provide more insight into the primary outcome results, our main aim was to provide an overview of the use of CPMs. A risk of bias assessment would not provide any added value concerning this objective.
Future research on the topic is needed to build better tools and assess their effectiveness, not only in terms of statistical significance, but also examining clinical significance, generalisability, and cost-effectiveness. A well-validated CPM, appropriate to the specific context, may be used as a foundation. Impact analyses are desired, investigating the potential added value of using a CPM versus not using a CPM, and to compare different methods concerning translating a CPM estimate to a suggested action. Furthermore, future research may address conveying the information in an informative and practical manner to the clinician and patient, taking into account the patient’s values. This may encompass the development or fine-tuning of suitable decision-aids. In addition, different channels for the implementation of these tools, such as electronic health records or digital e-coaches hosted in wearable devices or smartphones, may be explored in future studies.
In conclusion, this study presented an overview of the use of CPMs to personalise lifestyle interventions for CVD prevention. Due to the design of the included studies, it is inconclusive what the optimal use of CPMs may be. Therefore we believe there is a need for further research to explore the full potential of using CPMs to personalise lifestyle interventions for the prevention of CVD.
Funding
This research received funding from the Netherlands Organisation for Scientific Research (NWO): Coronary ARtery disease: Risk estimations and Interventions for prevention and EaRly detection (CARRIER): project nr. 628.011.212.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2021.101672.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Abbas S.Z., Pollard T.M., Wynn P., Learmonth A., Joyce K., Bambra C. The effectiveness of using the workplace to identify and address modifiable health risk factors in deprived populations. Occup. Environ. Med. 2015;72(9):664–669. doi: 10.1136/oemed-2014-102743. [DOI] [PubMed] [Google Scholar]
- Alderman M.H. Blood pressure management: Individualized treatment based on absolute risk and the potential for benefit. Ann. Intern. Med. 1993;119(4):329. doi: 10.7326/0003-4819-119-4-199308150-00013. [DOI] [PubMed] [Google Scholar]
- Alssema M., Newson R.S., Bakker S.J.L., Stehouwer C.D.A., Heymans M.W., Nijpels G., Hillege H.L., Hofman A., Witteman J.C.M., Gansevoort R.T., Dekker J.M. One risk assessment tool for cardiovascular disease, type 2 diabetes, and chronic kidney disease. Diab. Care. 2012;35(4):741–748. doi: 10.2337/dc11-1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amrhein V., Greenland S., McShane B. Scientists rise up against statistical significance. Nature. 2019;567(7748):305–307. doi: 10.1038/d41586-019-00857-9. [DOI] [PubMed] [Google Scholar]
- Anderson K.M., Odell P.M., Wilson P.W.F., Kannel W.B. Cardiovascular disease risk profiles. Am. Heart J. 1991;121(1):293–298. doi: 10.1016/0002-8703(91)90861-B. [DOI] [PubMed] [Google Scholar]
- Arnett D.K., Blumenthal R.S., Albert M.A., Buroker A.B., Goldberger Z.D., Hahn E.J., Himmelfarb C.D., Khera A., Lloyd-Jones D., McEvoy J.W., Michos E.D., Miedema M.D., Muñoz D., Smith S.C., Virani S.S., Williams K.A., Yeboah J., Ziaeian B. 2019 ACC/AHA guideline on the primary Prevention of cardiovascular disease. J. Am. Coll. Cardiol. 2019;74(10):e177–e232. doi: 10.1016/j.jacc.2019.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assmann G., Cullen P., Schulte H. Simple scoring scheme for calculating the risk of acute coronary events based on the 10-year follow-up of the Prospective Cardiovascular Münster (PROCAM) study. Circulation. 2002;105(3):310–315. doi: 10.1161/hc0302.102575. [DOI] [PubMed] [Google Scholar]
- Aune D., Schlesinger S., Norat T., Riboli E. Tobacco smoking and the risk of sudden cardiac death: A systematic review and meta-analysis of prospective studies. Eur. J. Epidemiol. 2018;33(6):509–521. doi: 10.1007/s10654-017-0351-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badenbroek I.F., Stol D.M., Nielen M.M., Hollander M., Kraaijenhagen R.A., de Wit G.A., Schellevis F.G., de Wit N.J. Design of the INTEGRATE study: Effectiveness and cost-effectiveness of a cardiometabolic risk assessment and treatment program integrated in primary care. BioMed. Central Family Pract. 2014;15(1):90. doi: 10.1186/1471-2296-15-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badenbroek I.F., Stol D.M., Nielen M.M., Hollander M., Kraaijenhagen R.A., de Wit G.A., Schellevis F.G., de Wit N.J. Erratum to: Design of the INTEGRATE study: Effectiveness and cost-effectiveness of a cardiometabolic risk assessment and treatment program integrated in primary care. BioMed. Central Family Pract. 2016;17(1):42. doi: 10.1186/s12875-016-0438-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbaresko J., Rienks J., Nöthlings U. Lifestyle indices and cardiovascular disease risk: A meta-analysis. Am. J. Prev. Med. 2018;55(4):555–564. doi: 10.1016/j.amepre.2018.04.046. [DOI] [PubMed] [Google Scholar]
- Benner J.S., Cherry S.B., Erhardt L., Fernandes M., Flammer M., Gaciong Z., Girerd X., Johnson E.S., García-Puig J., Sturkenboom M.C.J.M., Sun W. Rationale, design, and methods for the risk evaluation and communication health outcomes and utilization trial (REACH OUT) Contemporary Clin. Trials. 2007;28(5):662–673. doi: 10.1016/j.cct.2007.03.004. [DOI] [PubMed] [Google Scholar]
- Benner, J. S., Erhardt, L., Flammer, M., Moller, R. A., Rajicic, N., Changela, K., Yunis, C., Cherry, S. B., Gaciong, Z., Johnson, E. S., Sturkenboom, M. C. J. M., García-Puig, J., Girerd, X., on behalf of the REACH OUT Investigators, 2008. A novel programme to evaluate and communicate 10-year risk of CHD reduces predicted risk and improves patients’ modifiable risk factor profile. Int. J. Clin. Pract. 62(10), 1484–1498. https://doi.org/10.1111/j.1742-1241.2008.01872.x. [DOI] [PMC free article] [PubMed]
- Bouton M.E. Why behavior change is difficult to sustain. Prev. Med. 2014;68:29–36. doi: 10.1016/j.ypmed.2014.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brett T., Arnold-Reed D., Phan C., Cadden F., Walker W., Manea-Walley W., Mora N., Young J., Bulsara M. The Fremantle primary prevention study: A multicentre randomised trial of absolute cardiovascular risk reduction. Br. J. Gen. Pract. 2012;62(594):e22–e28. doi: 10.3399/bjgp12X616337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrington M.J., Jennings G.L., Clark R.A., Stewart S. Assessing cardiovascular risk in regional areas: The Healthy Hearts – Beyond City Limits program. BioMed Central Health Serv. Res. 2012;12(1):296. doi: 10.1186/1472-6963-12-296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrington M.J., Stewart S. Cardiovascular disease prevention via a nurse-facilitated intervention clinic in a regional setting: The Protecting Healthy Hearts Program. Eur. J. Cardiovasc. Nurs. 2015;14(4):352–361. doi: 10.1177/1474515114537022. [DOI] [PubMed] [Google Scholar]
- Chiuve S.E., Cook N.R., Shay C.M., Rexrode K.M., Albert C.M., Manson J.E., Willett W.C., Rimm E.B. Lifestyle-based prediction model for the prevention of CVD: The Healthy Heart Score. J. Am. Heart Assoc. 2014;3(6) doi: 10.1161/JAHA.114.000954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claes N., Jacobs N., Clays E., Schrooten W., De Bourdeaudhuij I. Comparing the effectiveness of two cardiovascular prevention programmes for highly educated professionals in general practice: A randomised clinical trial. BioMed Central Cardiovasc. Disord. 2013;13(1):38. doi: 10.1186/1471-2261-13-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy R.M., Pyörälä K., Fitzgerald A.P., Sans S., Menotti A., De Backer G., De Bacquer D., Ducimetière P., Jousilahti P., Keil U., Njølstad I., Oganov R.G., Thomsen T., Tunstall-Pedoe H., Tverdal A., Wedel H., Whincup P., Wilhelmsen L., Graham I.M. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur. Heart J. 2003;24(11):987–1003. doi: 10.1016/S0195-668X(03)00114-3. [DOI] [PubMed] [Google Scholar]
- Cox J.L., Carr B., Vallis T.M., Szpilfogel C., O’Neill B.J. A novel approach to cardiovascular health by optimizing risk management (ANCHOR): A primary prevention initiative examining the impact of health risk factor assessment and management on cardiac wellness. Can. J. Cardiol. 2011;27(6):809–817. doi: 10.1016/j.cjca.2011.04.013. [DOI] [PubMed] [Google Scholar]
- Cox J.L., Vallis T.M., Pfammatter A., Szpilfogel C., Carr B., O’Neill B.J. A novel approach to cardiovascular health by optimizing risk management (ANCHOR): Behavioural modification in primary care effectively reduces global risk. Can. J. Cardiol. 2013;29(11):1400–1407. doi: 10.1016/j.cjca.2013.03.007. [DOI] [PubMed] [Google Scholar]
- Cruz Rivera S., Liu X., Chan A.-W., Denniston A.K., Calvert M.J., Ashrafian H., Beam A.L., Collins G.S., Darzi A., Deeks J.J., ElZarrad M.K., Espinoza C., Esteva A., Faes L., Ferrante di Ruffano L., Fletcher J., Golub R., Harvey H., Haug C., Holmes C., Jonas A., Keane P.A., Kelly C.J., Lee A.Y., Lee C.S., Manna E., Matcham J., McCradden M., Moher D., Monteiro J., Mulrow C., Oakden-Rayner L., Paltoo D., Panico M.B., Price G., Rowley S., Savage R., Sarkar R., Vollmer S.J., Yau C. Guidelines for clinical trial protocols for interventions involving artificial intelligence: The SPIRIT-AI extension. Lancet Digital Health. 2020;2(10):e549–e560. doi: 10.1016/S2589-7500(20)30219-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelman D., Oddone E.Z., Liebowitz R.S., Yancy W.S., Olsen M.K., Jeffreys A.S., Moon S.D., Harris A.C., Smith L.L., Quillian-Wolever R.E., Gaudet T.W. A multidimensional integrative medicine intervention to improve cardiovascular risk. J. Gen. Intern. Med. 2006;21(7):728–734. doi: 10.1111/j.1525-1497.2006.00495.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood D.A., Kinmonth A.L., Davies G.A., Yarwood J., Thompson S.G., Pyke S.D.M., Kok Y., Cramb R., Le Guen C., Marteau T.M., Durrington P.N. Randomised controlled trial evaluating cardiovascular screening and intervention in general practice: Principal results of British Family Heart Study. Br. Med. J. 1994;308(6924):313–320. doi: 10.1136/bmj.308.6924.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goff D.C., Lloyd-Jones D.M., Bennett G., Coady S., D’Agostino R.B., Gibbons R., Greenland P., Lackland D.T., Levy D., O’Donnell C.J., Robinson J.G., Schwartz J.S., Shero S.T., Smith S.C., Sorlie P., Stone N.J., Wilson P.W.F. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014;129(25 suppl 2):S49–S73. doi: 10.1161/01.cir.0000437741.48606.98. [DOI] [PubMed] [Google Scholar]
- Harrell, F. Jr., Lazzeroni, L., 2017, July 17. EHRs and RCTs: Outcome prediction vs. Optimal treatment selection. Statistical Thinking. https://www.fharrell.com/post/ehrs-rcts/.
- Harting J., van Assema P., van Limpt P., Gorgels T., van Ree J., Ruland E., Vermeer F., de Vries N.K. Cardiovascular prevention in the Hartslag Limburg project: Effects of a high-risk approach on behavioral risk factors in a general practice population. Prev. Med. 2006;43(5):372–378. doi: 10.1016/j.ypmed.2006.06.016. [DOI] [PubMed] [Google Scholar]
- He F.J., Nowson C.A., Lucas M., MacGregor G.A. Increased consumption of fruit and vegetables is related to a reduced risk of coronary heart disease: Meta-analysis of cohort studies. J. Hum. Hypertens. 2007;21(9):717–728. doi: 10.1038/sj.jhh.1002212. [DOI] [PubMed] [Google Scholar]
- Hernán M.A., Hsu J., Healy B. A second chance to get causal inference right: A classification of data science tasks. Chance. 2019;32(1):42–49. doi: 10.1080/09332480.2019.1579578. [DOI] [Google Scholar]
- Hippisley-Cox J., Coupland C., Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: Prospective cohort study. Br. Med. J. 2017;j2099 doi: 10.1136/bmj.j2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hippisley-Cox J., Coupland C., Vinogradova Y., Robson J., Minhas R., Sheikh A., Brindle P. Predicting cardiovascular risk in England and Wales: Prospective derivation and validation of QRISK2. Br. Med. J. 2008;336(7659):1475–1482. doi: 10.1136/bmj.39609.449676.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofstra L., Laufer E., Dijk F., van Dieijen M., Wellens H.J.J., Narula J. Mass screening and intervention by mass communication: The HAPPY program. Global Heart. 2011;6(4):221–222. doi: 10.1016/j.gheart.2011.08.005. [DOI] [PubMed] [Google Scholar]
- Hu G., Root M.M. Building prediction models for coronary heart disease by synthesizing multiple longitudinal research findings. Eur. J. Cardiovasc. Prev. Rehab. 2005;12(5):459–464. doi: 10.1097/01.hjr.0000173109.14228.71. [DOI] [PubMed] [Google Scholar]
- Imes C.C., Lewis F.M., Austin M.A., Dougherty C.M. My Family Medical History and Me: Feasibility results of a cardiovascular risk reduction intervention. Public Health Nurs. 2015;32(3):246–255. doi: 10.1111/phn.2015.32.issue-310.1111/phn.12130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson R., Lawes C., Bennett D., Milne R., Rodgers A. Treatment with drugs to lower blood pressure and blood cholesterol based on an individual’s absolute cardiovascular risk. Lancet. 2005;365(9457):434–441. doi: 10.1016/S0140-6736(05)70240-3. [DOI] [PubMed] [Google Scholar]
- Jørgensen T., Borch-Johnsen K., Thomsen T.F., Ibsen H., Glümer C., Pisinger C. A randomized non-pharmacological intervention study for prevention of ischaemic heart disease: Baseline results Inter99 (1) Eur. J. Cardiovasc. Prev. Rehab. 2003;10(5):377–386. doi: 10.1097/01.hjr.0000096541.30533.82. [DOI] [PubMed] [Google Scholar]
- Jørgensen T., Jacobsen R.K., Toft U., Aadahl M., Glumer C., Pisinger C. Effect of screening and lifestyle counselling on incidence of ischaemic heart disease in general population: Inter99 randomised trial. Br. Med. J. 2014;348(jun09 2):g3617. doi: 10.1136/bmj.g3617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavita, Thakur J.S., Vijayvergiya R., Ghai S. Task shifting of cardiovascular risk assessment and communication by nurses for primary and secondary prevention of cardiovascular diseases in a tertiary health care setting of Northern India. BioMed Central Health Serv. Res. 2020;20(1) doi: 10.1186/s12913-019-4864-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavita, Thakur, J. S., Vijayvergiya, R., Ghai, S., Agnihotri, M., 2018. Rationale and design of cardiovascular diseases (CVD) risk assessment and communication by nurses for primary and secondary preventation of CVDs in India. Nurs. Midwifery Res. J. https://doi.org/10.33698/NRF0232.
- Ketola E., Mäkelä M., Klockars M. Individualised multifactorial lifestyle intervention trial for high-risk cardiovascular patients in primary care. Br. J. Gen. Pract. 2001;51:291–294. [PMC free article] [PubMed] [Google Scholar]
- Keyserling T.C., Sheridan S.L., Draeger L.B., Finkelstein E.A., Gizlice Z., Kruger E., Johnston L.F., Sloane P.D., Samuel-Hodge C., Evenson K.R., Gross M.D., Donahue K.E., Pignone M.P., Vu M.B., Steinbacher E.A., Weiner B.J., Bangdiwala S.I., Ammerman A.S. A comparison of live counseling with a web-based lifestyle and medication intervention to reduce coronary heart disease risk: A randomized clinical trial. J. Am. Med. Assoc.: Internal Med. 2014;174(7):1144–1157. doi: 10.1001/jamainternmed.2014.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanji M.Y., Balawon A., Boubertakh R., Hofstra L., Narula J., Hunink M., Pugliese F., Petersen S.E. Personalized e-Coaching in cardiovascular risk reduction: A randomized controlled trial. Ann. Glob. Health. 2019;85(1):107. doi: 10.5334/aogh.2496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koelewijn-van Loon M.S., van der Weijden T., van Steenkiste B., Ronda G., Winkens B., Severens J.L., Wensing M., Elwyn G., Grol R. Involving patients in cardiovascular risk management with nurse-led clinics: A cluster randomized controlled trial. Can. Med. Assoc. J. 2009;181(12):E267–E274. doi: 10.1503/cmaj.081591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koelewijn-van Loon M.S., van Steenkiste B., Ronda G., Wensing M., Stoffers H.E., Elwyn G., Grol R., van der Weijden T. Improving patient adherence to lifestyle advice (IMPALA): A cluster-randomised controlled trial on the implementation of a nurse-led intervention for cardiovascular risk management in primary care (protocol) BioMed Central Health Serv. Res. 2008;8(1):9. doi: 10.1186/1472-6963-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krantz M.J., Beaty B., Coronel-Mockler S., Leeman-Castillo B., Fletcher K., Estacio R.O. Reduction in cardiovascular risk among Latino participants in a community-based intervention linked with clinical care. Am. J. Prev. Med. 2017;53(2):e71–e75. doi: 10.1016/j.amepre.2017.04.012. [DOI] [PubMed] [Google Scholar]
- Krones T., Keller H., Sönnichsen A., Sadowski E.-M., Baum E., Wegscheider K., Rochon J., Donner-Banzhoff N. Absolute cardiovascular disease risk and shared decision making in primary care: A randomized controlled trial. Ann. Family Med. 2008;6(3):218–227. doi: 10.1370/afm.854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon B.C., VanDam C., Chiuve S.E., Choi H.W., Entler P., Tan P.-N., Huh-Yoo J. Improving heart disease risk through quality-focused diet logging: Pre-post study of a diet quality tracking app. J. Med. Internet Res. MHealth UHealth. 2020;8(12):e21733. doi: 10.2196/21733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009;62(10):e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- Lin L., Sperrin M., Jenkins D.A., Martin G.P., Peek N. A scoping review of causal methods enabling predictions under hypothetical interventions. Diagnos. Prognos. Res. 2021;5(1):3. doi: 10.1186/s41512-021-00092-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Rivera S.C., Moher D., Calvert M.J., Denniston A.K. Reporting guidelines for clinical trial reports for interventions involving artificial intelligence: The CONSORT-AI extension. Br. Med. J. 2020;m3164 doi: 10.1136/bmj.m3164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z., Chen S., Zhang G., Lin A. Mobile phone-based lifestyle intervention for reducing overall cardiovascular disease risk in Guangzhou, China: A pilot study. Int. J. Environ. Res. Public Health. 2015;12(12):15993–16004. doi: 10.3390/ijerph121215037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin, H. L., Sartori, J., 2014. What’s your health age? A health risk assessment for veterans (http://hdl.handle.net/10713/5714). University of Maryland Baltimore.
- Moons K.G.M., Altman D.G., Vergouwe Y., Royston P. Prognosis and prognostic research: Application and impact of prognostic models in clinical practice. Br. Med. J. 2009;338(jun04 2):b606. doi: 10.1136/bmj.b606. [DOI] [PubMed] [Google Scholar]
- National Cholesterol Education Program Expert Panel Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III): Final report. Circulation. 2002;17:3144–3421. [PubMed] [Google Scholar]
- National Health Services Health Check Programme, 2009. Putting prevention first: NHS health check: Vascular risk assessment and management: Best practice guidance. Central Office of Information.
- National Institute for Health and Care Excellence, 2014. Cardiovascular disease: Risk assessment and reduction, including lipid modification (NICE Guideline CG181). www.nice.org.uk/guidance/cg181. [PubMed]
- New Zealand Guidelines Group, 2003. The assessment and management of cardiovascular risk. New Zealand Guidelines Group.
- New Zealand Ministry of Health, 2018. Cardiovascular disease risk assessment and management for primary care. https://www.health.govt.nz/system/files/documents/publications/cvd-risk-assessment-and-management-for-primary-care-v2.pdf.
- Nolan R.P., Upshur R.E.G., Lynn H., Crichton T., Rukholm E., Stewart D.E., Alter D.A., Chessex C., Harvey P.J., Grace S.L., Picard L., Michel I., Angus J., Corace K., Barry-Bianchi S.M., Chen M.H. Therapeutic benefit of preventive telehealth counseling in the community outreach heart health and risk reduction trial. Am. J. Cardiol. 2011;107(5):690–696. doi: 10.1016/j.amjcard.2010.10.050. [DOI] [PubMed] [Google Scholar]
- Oddone E.Z., Gierisch J.M., Sanders L.L., Fagerlin A., Sparks J., McCant F., May C., Olsen M.K., Damschroder L.J. A coaching by telephone intervention on engaging patients to address modifiable cardiovascular risk factors: A randomized controlled trial. J. Gen. Intern. Med. 2018;33(9):1487–1494. doi: 10.1007/s11606-018-4398-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … et al., 2021. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Brit. Med. J. n71. https://doi.org/10.1136/bmj.n71. [DOI] [PMC free article] [PubMed]
- Piepoli M.F., Hoes A.W., Agewall S., Albus C., Brotons C., Catapano A.L., Cooney M.-T., Corrà U., Cosyns B., Deaton C., Graham I., Hall M.S., Hobbs F.D.R., Løchen M.-L., Löllgen H., Marques-Vidal P., Perk J., Prescott E., Redon J., Richter D.J., Sattar N., Smulders Y., Tiberi M., van der Worp H.B., van Dis I., Verschuren W.M.M. 2016 European guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2016;37(29):2315–2381. doi: 10.1093/eurheartj/ehw106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pylypchuk R., Wells S., Kerr A., Poppe K., Riddell T., Harwood M., Exeter D., Mehta S., Grey C., Wu B.P., Metcalf P., Warren J., Harrison J., Marshall R., Jackson R. Cardiovascular disease risk prediction equations in 400 000 primary care patients in New Zealand: A derivation and validation study. Lancet. 2018;391(10133):1897–1907. doi: 10.1016/S0140-6736(18)30664-0. [DOI] [PubMed] [Google Scholar]
- Redfern J., Coorey G., Mulley J., Scaria A., Neubeck L., Hafiz N., Pitt C., Weir K., Forbes J., Parker S., Bampi F., Coenen A., Enright G., Wong A., Nguyen T., Harris M., Zwar N., Chow C.K., Rodgers A., Heeley E., Panaretto K., Lau A., Hayman N., Usherwood T., Peiris D. A digital health intervention for cardiovascular disease management in primary care (CONNECT) randomized controlled trial. npj Digital Med. 2020;3(1) doi: 10.1038/s41746-020-00325-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson G., van Woerden H.C., Morgan L., Edwards R., Harries M., Hancock E., Sroczynsk S., Bowley M. Healthy Hearts – A community-based primary prevention programme to reduce coronary heart disease. BioMed Central Cardiovasc. Disord. 2008;8(1):18. doi: 10.1186/1471-2261-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth G.A., Abate D., Abate K.H., Abay S.M., Abbafati C., Abbasi N., Abbastabar H., Abd-Allah F., Abdela J., Abdelalim A., Abdollahpour I., Abdulkader R.S., Abebe H.T., Abebe M., Abebe Z., Abejie A.N., Abera S.F., Abil O.Z., Abraha H.N., Abrham A.R., Abu-Raddad L.J., Accrombessi M.M.K., Acharya D., Adamu A.A., Adebayo O.M., Adedoyin R.A., Adekanmbi V., Adetokunboh O.O., Adhena B.M., Adib M.G., Admasie A., Afshin A., Agarwal G., Agesa K.M., Agrawal A., Agrawal S., Ahmadi A., Ahmadi M., Ahmed M.B., Ahmed S., Aichour A.N., Aichour I., Aichour M.T.E., Akbari M.E., Akinyemi R.O., Akseer N., Al-Aly Z., Al-Eyadhy A., Al-Raddadi R.M., Alahdab F., Alam K., Alam T., Alebel A., Alene K.A., Alijanzadeh M., Alizadeh-Navaei R., Aljunid S.M., Alkerwi A., Alla F., Allebeck P., Alonso J., Altirkawi K., Alvis-Guzman N., Amare A.T., Aminde L.N., Amini E., Ammar W., Amoako Y.A., Anber N.H., Andrei C.L., Androudi S., Animut M.D., Anjomshoa M., Ansari H., Ansha M.G., Antonio C.A.T., Anwari P., Aremu O., Ärnlöv J., Arora A., Arora M., Artaman A.l., Aryal K.K., Asayesh H., Asfaw E.T., Ataro Z., Atique S., Atre S.R., Ausloos M., Avokpaho E.F.G.A., Awasthi A., Quintanilla B.P.A., Ayele Y., Ayer R., Azzopardi P.S., Babazadeh A., Bacha U., Badali H., Badawi A., Bali A.G., Ballesteros K.E., Banach M., Banerjee K., Bannick M.S., Banoub J.A.M., Barboza M.A., Barker-Collo S.L., Bärnighausen T.W., Barquera S., Barrero L.H., Bassat Q., Basu S., Baune B.T., Baynes H.W., Bazargan-Hejazi S., Bedi N., Beghi E., Behzadifar M., Behzadifar M., Béjot Y., Bekele B.B., Belachew A.B., Belay E., Belay Y.A., Bell M.L., Bello A.K., Bennett D.A., Bensenor I.M., Berman A.E., Bernabe E., Bernstein R.S., Bertolacci G.J., Beuran M., Beyranvand T., Bhalla A., Bhattarai S., Bhaumik S., Bhutta Z.A., Biadgo B., Biehl M.H., Bijani A., Bikbov B., Bilano V., Bililign N., Bin Sayeed M.S., Bisanzio D., Biswas T., Blacker B.F., Basara B.B., Borschmann R., Bosetti C., Bozorgmehr K., Brady O.J., Brant L.C., Brayne C., Brazinova A., Breitborde N.J.K., Brenner H., Briant P.S., Britton G., Brugha T., Busse R., Butt Z.A., Callender C.S.K.H., Campos-Nonato I.R., Campuzano Rincon J.C., Cano J., Car M., Cárdenas R., Carreras G., Carrero J.J., Carter A., Carvalho F., Castañeda-Orjuela C.A., Castillo Rivas J., Castle C.D., Castro C., Castro F., Catalá-López F., Cerin E., Chaiah Y., Chang J.-C., Charlson F.J., Chaturvedi P., Chiang P.-C., Chimed-Ochir O., Chisumpa V.H., Chitheer A., Chowdhury R., Christensen H., Christopher D.J., Chung S.-C., Cicuttini F.M., Ciobanu L.G., Cirillo M., Cohen A.J., Cooper L.T., Cortesi P.A., Cortinovis M., Cousin E., Cowie B.C., Criqui M.H., Cromwell E.A., Crowe C.S., Crump J.A., Cunningham M., Daba A.K., Dadi A.F., Dandona L., Dandona R., Dang A.K., Dargan P.I., Daryani A., Das S.K., Gupta R.D., Neves J.D., Dasa T.T., Dash A.P., Davis A.C., Davis Weaver N., Davitoiu D.V., Davletov K., De La Hoz F.P., De Neve J.-W., Degefa M.G., Degenhardt L., Degfie T.T., Deiparine S., Demoz G.T., Demtsu B.B., Denova-Gutiérrez E., Deribe K., Dervenis N., Des Jarlais D.C., Dessie G.A., Dey S., Dharmaratne S.D., Dicker D., Dinberu M.T., Ding E.L., Dirac M.A., Djalalinia S., Dokova K., Doku D.T., Donnelly C.A., Dorsey E.R., Doshi P.P., Douwes-Schultz D., Doyle K.E., Driscoll T.R., Dubey M., Dubljanin E., Duken E.E., Duncan B.B., Duraes A.R., Ebrahimi H., Ebrahimpour S., Edessa D., Edvardsson D., Eggen A.E., El Bcheraoui C., El Sayed Zaki M., El-Khatib Z., Elkout H., Ellingsen C.L., Endres M., Endries A.Y., Er B., Erskine H.E., Eshrati B., Eskandarieh S., Esmaeili R., Esteghamati A., Fakhar M., Fakhim H., Faramarzi M., Fareed M., Farhadi F., Farinha C.S.E.s., Faro A., Farvid M.S., Farzadfar F., Farzaei M.H., Feigin V.L., Feigl A.B., Fentahun N., Fereshtehnejad S.-M., Fernandes E., Fernandes J.C., Ferrari A.J., Feyissa G.T., Filip I., Finegold S., Fischer F., Fitzmaurice C., Foigt N.A., Foreman K.J., Fornari C., Frank T.D., Fukumoto T., Fuller J.E., Fullman N., Fürst T., Furtado J.M., Futran N.D., Gallus S., Garcia-Basteiro A.L., Garcia-Gordillo M.A., Gardner W.M., Gebre A.K., Gebrehiwot T.T., Gebremedhin A.T., Gebremichael B., Gebremichael T.G., Gelano T.F., Geleijnse J.M., Genova-Maleras R., Geramo Y.C.D., Gething P.W., Gezae K.E., Ghadami M.R., Ghadimi R., Ghasemi Falavarjani K., Ghasemi-Kasman M., Ghimire M., Gibney K.B., Gill P.S., Gill T.K., Gillum R.F., Ginawi I.A., Giroud M., Giussani G., Goenka S., Goldberg E.M., Goli S., Gómez-Dantés H., Gona P.N., Gopalani S.V., Gorman T.M., Goto A., Goulart A.C., Gnedovskaya E.V., Grada A., Grosso G., Gugnani H.C., Guimaraes A.L.S., Guo Y., Gupta P.C., Gupta R., Gupta R., Gupta T., Gutiérrez R.A., Gyawali B., Haagsma J.A., Hafezi-Nejad N., Hagos T.B., Hailegiyorgis T.T., Hailu G.B., Haj-Mirzaian A., Haj-Mirzaian A., Hamadeh R.R., Hamidi S., Handal A.J., Hankey G.J., Harb H.L., Harikrishnan S., Haro J.M., Hasan M., Hassankhani H., Hassen H.Y., Havmoeller R., Hay R.J., Hay S.I., He Y., Hedayatizadeh-Omran A., Hegazy M.I., Heibati B., Heidari M., Hendrie D., Henok A., Henry N.J., Herteliu C., Heydarpour F., Heydarpour P., Heydarpour S., Hibstu D.T., Hoek H.W., Hole M.K., Homaie Rad E., Hoogar P., Hosgood H.D., Hosseini S.M., Hosseinzadeh M., Hostiuc M., Hostiuc S., Hotez P.J., Hoy D.G., Hsiao T., Hu G., Huang J.J., Husseini A., Hussen M.M., Hutfless S., Idrisov B., Ilesanmi O.S., Iqbal U., Irvani S.S.N., Irvine C.M.S., Islam N., Islam S.M.S., Islami F., Jacobsen K.H., Jahangiry L., Jahanmehr N., Jain S.K., Jakovljevic M., Jalu M.T., James S.L., Javanbakht M., Jayatilleke A.U., Jeemon P., Jenkins K.J., Jha R.P., Jha V., Johnson C.O., Johnson S.C., Jonas J.B., Joshi A., Jozwiak J.J., Jungari S.B., Jürisson M., Kabir Z., Kadel R., Kahsay A., Kalani R., Karami M., Karami Matin B., Karch A., Karema C., Karimi-Sari H., Kasaeian A., Kassa D.H., Kassa G.M., Kassa T.D., Kassebaum N.J., Katikireddi S.V., Kaul A., Kazemi Z., Karyani A.K., Kazi D.S., Kefale A.T., Keiyoro P.N., Kemp G.R., Kengne A.P., Keren A., Kesavachandran C.N., Khader Y.S., Khafaei B., Khafaie M.A., Khajavi A., Khalid N., Khalil I.A., Khan E.A., Khan M.S., Khan M.A., Khang Y.-H., Khater M.M., Khoja A.T., Khosravi A., Khosravi M.H., Khubchandani J., Kiadaliri A.A., Kibret G.D., Kidanemariam Z.T., Kiirithio D.N., Kim D., Kim Y.-E., Kim Y.J., Kimokoti R.W., Kinfu Y., Kisa A., Kissimova-Skarbek K., Kivimäki M., Knudsen A.K.S., Kocarnik J.M., Kochhar S., Kokubo Y., Kolola T., Kopec J.A., Koul P.A., Koyanagi A.i., Kravchenko M.A., Krishan K., Kuate Defo B., Kucuk Bicer B., Kumar G.A., Kumar M., Kumar P., Kutz M.J., Kuzin I., Kyu H.H., Lad D.P., Lad S.D., Lafranconi A., Lal D.K., Lalloo R., Lallukka T., Lam J.O., Lami F.H., Lansingh V.C., Lansky S., Larson H.J., Latifi A., Lau K.-M., Lazarus J.V., Lebedev G., Lee P.H., Leigh J., Leili M., Leshargie C.T., Li S., Li Y., Liang J., Lim L.-L., Lim S.S., Limenih M.A., Linn S., Liu S., Liu Y., Lodha R., Lonsdale C., Lopez A.D., Lorkowski S., Lotufo P.A., Lozano R., Lunevicius R., Ma S., Macarayan E.R.K., Mackay M.T., MacLachlan J.H., Maddison E.R., Madotto F., Magdy Abd El Razek H., Magdy Abd El Razek M., Maghavani D.P., Majdan M., Majdzadeh R., Majeed A., Malekzadeh R., Malta D.C., Manda A.-L., Mandarano-Filho L.G., Manguerra H., Mansournia M.A., Mapoma C.C., Marami D., Maravilla J.C., Marcenes W., Marczak L., Marks A., Marks G.B., Martinez G., Martins-Melo F.R., Martopullo I., März W., Marzan M.B., Masci J.R., Massenburg B.B., Mathur M.R., Mathur P., Matzopoulos R., Maulik P.K., Mazidi M., McAlinden C., McGrath J.J., McKee M., McMahon B.J., Mehata S., Mehndiratta M.M., Mehrotra R., Mehta K.M., Mehta V., Mekonnen T.C., Melese A., Melku M., Memiah P.T.N., Memish Z.A., Mendoza W., Mengistu D.T., Mengistu G., Mensah G.A., Mereta S.T., Meretoja A., Meretoja T.J., Mestrovic T., Mezgebe H.B., Miazgowski B., Miazgowski T., Millear A.I., Miller T.R., Miller-Petrie M.K., Mini G.K., Mirabi P., Mirarefin M., Mirica A., Mirrakhimov E.M., Misganaw A.T., Mitiku H., Moazen B., Mohammad K.A., Mohammadi M., Mohammadifard N., Mohammed M.A., Mohammed S., Mohan V., Mokdad A.H., Molokhia M., Monasta L., Moradi G., Moradi-Lakeh M., Moradinazar M., Moraga P., Morawska L., Moreno Velásquez I., Morgado-Da-Costa J., Morrison S.D., Moschos M.M., Mouodi S., Mousavi S.M., Muchie K.F., Mueller U.O., Mukhopadhyay S., Muller K., Mumford J.E., Musa J., Musa K.I., Mustafa G., Muthupandian S., Nachega J.B., Nagel G., Naheed A., Nahvijou A., Naik G., Nair S., Najafi F., Naldi L., Nam H.S., Nangia V., Nansseu J.R., Nascimento B.R., Natarajan G., Neamati N., Negoi I., Negoi R.I., Neupane S., Newton C.R.J., Ngalesoni F.N., Ngunjiri J.W., Nguyen A.Q., Nguyen G., Nguyen H.T., Nguyen H.T., Nguyen L.H., Nguyen M., Nguyen T.H., Nichols E., Ningrum D.N.A., Nirayo Y.L., Nixon M.R., Nolutshungu N., Nomura S., Norheim O.F., Noroozi M., Norrving B.o., Noubiap J.J., Nouri H.R., Nourollahpour Shiadeh M., Nowroozi M.R., Nyasulu P.S., Odell C.M., Ofori-Asenso R., Ogbo F.A., Oh I.-H., Oladimeji O., Olagunju A.T., Olivares P.R., Olsen H.E., Olusanya B.O., Olusanya J.O., Ong K.L., Ong S.K.S., Oren E., Orpana H.M., Ortiz A., Ortiz J.R., Otstavnov S.S., Øverland S., Owolabi M.O., Özdemir R., P A M., Pacella R., Pakhale S., Pakhare A.P., Pakpour A.H., Pana A., Panda-Jonas S., Pandian J.D., Parisi A., Park E.-K., Parry C.D.H., Parsian H., Patel S., Pati S., Patton G.C., Paturi V.R., Paulson K.R., Pereira A., Pereira D.M., Perico N., Pesudovs K., Petzold M., Phillips M.R., Piel F.B., Pigott D.M., Pillay J.D., Pirsaheb M., Pishgar F., Polinder S., Postma M.J., Pourshams A., Poustchi H., Pujar A., Prakash S., Prasad N., Purcell C.A., Qorbani M., Quintana H., Quistberg D.A., Rade K.W., Radfar A., Rafay A., Rafiei A., Rahim F., Rahimi K., Rahimi-Movaghar A., Rahman M., Rahman M.H.U., Rahman M.A., Rai R.K., Rajsic S., Ram U., Ranabhat C.L., Ranjan P., Rao P.C., Rawaf D.L., Rawaf S., Razo-García C., Reddy K.S., Reiner R.C., Reitsma M.B., Remuzzi G., Renzaho A.M.N., Resnikoff S., Rezaei S., Rezaeian S., Rezai M.S., Riahi S.M., Ribeiro A.L.P., Rios-Blancas M.J., Roba K.T., Roberts N.L.S., Robinson S.R., Roever L., Ronfani L., Roshandel G., Rostami A., Rothenbacher D., Roy A., Rubagotti E., Sachdev P.S., Saddik B., Sadeghi E., Safari H., Safdarian M., Safi S., Safiri S., Sagar R., Sahebkar A., Sahraian M.A., Salam N., Salama J.S., Salamati P., Saldanha R.D.F., Saleem Z., Salimi Y., Salvi S.S., Salz I., Sambala E.Z., Samy A.M., Sanabria J., Sanchez-Niño M.D., Santomauro D.F., Santos I.S., Santos J.V., Milicevic M.M.S., Sao Jose B.P., Sarker A.R., Sarmiento-Suárez R., Sarrafzadegan N., Sartorius B., Sarvi S., Sathian B., Satpathy M., Sawant A.R., Sawhney M., Saxena S., Sayyah M., Schaeffner E., Schmidt M.I., Schneider I.J.C., Schöttker B., Schutte A.E., Schwebel D.C., Schwendicke F., Scott J.G., Sekerija M., Sepanlou S.G., Serván-Mori E., Seyedmousavi S., Shabaninejad H., Shackelford K.A., Shafieesabet A., Shahbazi M., Shaheen A.A., Shaikh M.A., Shams-Beyranvand M., Shamsi M., Shamsizadeh M., Sharafi K., Sharif M., Sharif-Alhoseini M., Sharma R., She J., Sheikh A., Shi P., Shiferaw M.S., Shigematsu M., Shiri R., Shirkoohi R., Shiue I., Shokraneh F., Shrime M.G., Si S.i., Siabani S., Siddiqi T.J., Sigfusdottir I.D., Sigurvinsdottir R., Silberberg D.H., Silva D.A.S., Silva J.P., Silva N.T.D., Silveira D.G.A., Singh J.A., Singh N.P., Singh P.K., Singh V., Sinha D.N., Sliwa K., Smith M., Sobaih B.H., Sobhani S., Sobngwi E., Soneji S.S., Soofi M., Sorensen R.J.D., Soriano J.B., Soyiri I.N., Sposato L.A., Sreeramareddy C.T., Srinivasan V., Stanaway J.D., Starodubov V.I., Stathopoulou V., Stein D.J., Steiner C., Stewart L.G., Stokes M.A., Subart M.L., Sudaryanto A., Sufiyan M.B., Sur P.J., Sutradhar I., Sykes B.L., Sylaja P.N., Sylte D.O., Szoeke C.E.I., Tabarés-Seisdedos R., Tabuchi T., Tadakamadla S.K., Takahashi K., Tandon N., Tassew S.G., Taveira N., Tehrani-Banihashemi A., Tekalign T.G., Tekle M.G., Temsah M.-H., Temsah O., Terkawi A.S., Teshale M.Y., Tessema B., Tessema G.A., Thankappan K.R., Thirunavukkarasu S., Thomas N., Thrift A.G., Thurston G.D., Tilahun B., To Q.G., Tobe-Gai R., Tonelli M., Topor-Madry R., Torre A.E., Tortajada-Girbés M., Touvier M., Tovani-Palone M.R., Tran B.X., Tran K.B., Tripathi S., Troeger C.E., Truelsen T.C., Truong N.T., Tsadik A.G., Tsoi D., Tudor Car L., Tuzcu E.M., Tyrovolas S., Ukwaja K.N., Ullah I., Undurraga E.A., Updike R.L., Usman M.S., Uthman O.A., Uzun S.B., Vaduganathan M., Vaezi A., Vaidya G., Valdez P.R., Varavikova E., Vasankari T.J., Venketasubramanian N., Villafaina S., Violante F.S., Vladimirov S.K., Vlassov V., Vollset S.E., Vos T., Wagner G.R., Wagnew F.S., Waheed Y., Wallin M.T., Walson J.L., Wang Y., Wang Y.-P., Wassie M.M., Weiderpass E., Weintraub R.G., Weldegebreal F., Weldegwergs K.G., Werdecker A., Werkneh A.A., West T.E., Westerman R., Whiteford H.A., Widecka J., Wilner L.B., Wilson S., Winkler A.S., Wiysonge C.S., Wolfe C.D.A., Wu S., Wu Y.-C., Wyper G.M.A., Xavier D., Xu G., Yadgir S., Yadollahpour A., Yahyazadeh Jabbari S.H., Yakob B., Yan L.L., Yano Y., Yaseri M., Yasin Y.J., Yentür G.K., Yeshaneh A., Yimer E.M., Yip P., Yirsaw B.D., Yisma E., Yonemoto N., Yonga G., Yoon S.-J., Yotebieng M., Younis M.Z., Yousefifard M., Yu C., Zadnik V., Zaidi Z., Zaman S.B., Zamani M., Zare Z., Zeleke A.J., Zenebe Z.M., Zhang A.L., Zhang K., Zhou M., Zodpey S., Zuhlke L.J., Naghavi M., Murray C.J.L. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sattelmair J., Pertman J., Ding E.L., Kohl H.W., Haskell W., Lee I.-M. Dose response between physical activity and risk of coronary heart disease: A meta-analysis. Circulation. 2011;124(7):789–795. doi: 10.1161/CIRCULATIONAHA.110.010710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shalit, U., Johansson, F. D., Sontag, D., 2017. Estimating individual treatment effect: Generalization bounds and algorithms. ArXiv:1606.03976 [Cs, Stat]. http://arxiv.org/abs/1606.03976.
- Sheridan S.L., Draeger L.B., Pignone M.P., Keyserling T.C., Simpson R.J., Rimer B., Bangdiwala S.I., Cai J., Gizlice Z. A randomized trial of an intervention to improve use and adherence to effective coronary heart disease prevention strategies. BioMed Central Health Serv. Res. 2011;11(1):331. doi: 10.1186/1472-6963-11-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siren R., Eriksson J.G., Vanhanen H. Observed changes in cardiovascular risk factors among high-risk middle-aged men who received lifestyle counselling: A 5-year follow-up. Scand. J. Prim. Health Care. 2016;34(4):336–342. doi: 10.1080/02813432.2016.1248649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stacey D., Légaré F., Lewis K., Barry M.J., Bennett C.L., Eden K.B., Holmes-Rovner M., Llewellyn-Thomas H., Lyddiatt A., Thomson R., Trevena L. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst. Rev. 2017;2017(4) doi: 10.1002/14651858.CD001431.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens R.J., Kothari V., Adler A.I., Stratton I.M., Holman R.R. The UKPDS risk engine: A model for the risk of coronary heart disease in Type II diabetes (UKPDS 56) Clin. Sci. 2001;101(6):671–679. doi: 10.1042/cs1010671. [DOI] [PubMed] [Google Scholar]
- Steyerberg E.W. Clinical prediction models: A practical approach to development, validation, and updating. Springer International Publishing. 2019 doi: 10.1007/978-3-030-16399-0. [DOI] [Google Scholar]
- Stol D.M., Badenbroek I.F., Hollander M., Nielen M.M.J., Kraaijenhagen R.A., Schellevis F.G., de Wit N.J. Effectiveness of a stepwise cardiometabolic disease prevention program: Results of a randomized controlled trial in primary care. Prev. Med. 2020;132:105984. doi: 10.1016/j.ypmed.2020.105984. [DOI] [PubMed] [Google Scholar]
- Suomen Sydäntautiliitto, Lääkintöhallitus, Kansanterveyslaitos, Suomen Kardiologinen Seura, 1986. Pohjois-Karjala-projektin riskipistetaulukko. (In Finnish.). In: Sepelvaltimotaudin ehkäisyn suuntaviivat -kirjassa. Keski-Pohjanmaan Kirjapaino Oy.
- Systematic Coronary Risk Evaluation 2 Working Group and European Society of Cardiology Cardiovascular Risk Collaboration, 2021. SCORE2 risk prediction algorithms: New models to estimate 10-year risk of cardiovascular disease in Europe. Eur. Heart J. 42(25), 2439–2454. https://doi.org/10.1093/eurheartj/ehab309. [DOI] [PMC free article] [PubMed]
- Thompson S.G., Pyke S.D.M., Wood D.A. Using a coronary risk score for screening and intervention in general practice. Eur. J. Cardiovasc. Prev. Rehab. 1996;3(3):301–306. doi: 10.1177/174182679600300307. [DOI] [PubMed] [Google Scholar]
- Thomsen T.F., Davidsen M., Ibsen H., Jorgensen T., Jensen G., Borch-Johnsen K. A new method for CHD prediction and prevention based on regional risk scores and randomized clinical trials; PRECARD and the Copenhagen risk score. Eur. J. Cardiovasc. Prev. Rehab. 2001;8(5):291–297. doi: 10.1177/174182670100800508. [DOI] [PubMed] [Google Scholar]
- Tinsel I., Siegel A., Schmoor C., Poguntke I., Maun A., Niebling W. Encouraging self-management in cardiovascular disease prevention: A randomized controlled study of a structured advice and patient activation intervention in primary care. Deutsches Aerzteblatt Int. 2018;113:469–476. doi: 10.3238/arztebl.2018.0469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Brekel-Dijkstra K., Rengers A.H., Niessen M.A.J., de Wit N.J., Kraaijenhagen R.A. Personalized prevention approach with use of a web-based cardiovascular risk assessment with tailored lifestyle follow-up in primary care practice – A pilot study. Eur. J. Prev. Cardiol. 2016;23(5):544–551. doi: 10.1177/2047487315591441. [DOI] [PubMed] [Google Scholar]
- Van der Kalken, C. K., Kraaijenhagen, R. A., 2007. Computer installation for establishing a diagnosis (Patent No. P217247PCTIIL). www.preventionkompas.nl.
- van der Leeuw J., Ridker P.M., van der Graaf Y., Visseren F.L.J. Personalized cardiovascular disease prevention by applying individualized prediction of treatment effects. Eur. Heart J. 2014;35(13):837–843. doi: 10.1093/eurheartj/ehu004. [DOI] [PubMed] [Google Scholar]
- van Giessen A., Peters J., Wilcher B., Hyde C., Moons C., de Wit A., Koffijberg E. Systematic review of health economic impact evaluations of risk prediction models: Stop developing, start evaluating. Value Health. 2017;20(4):718–726. doi: 10.1016/j.jval.2017.01.001. [DOI] [PubMed] [Google Scholar]
- Vickers A.J., Elkin E.B. Decision curve analysis: A novel method for evaluating prediction models. Med. Decis. Making. 2006;26(6):565–574. doi: 10.1177/0272989X06295361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visseren, F. L. J., Mach, F., Smulders, Y. M., Carballo, D., Koskinas, K. C., Bäck, M., Benetos, A., Biffi, A., Boavida, J.-M., Capodanno, D., Cosyns, B., Crawford, C., Davos, C. H., Desormais, I., Di Angelantonio, E., Franco, O. H., Halvorsen, S., Hobbs, F. D. R., Hollander, M., et al., 2021. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J., 42(34), 3227–3337. https://doi.org/10.1093/eurheartj/ehab484. [DOI] [PubMed]
- Wilson P.W.F., D’Agostino R.B., Levy D., Belanger A.M., Silbershatz H., Kannel W.B. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–1847. doi: 10.1161/01.CIR.97.18.1837. [DOI] [PubMed] [Google Scholar]
- Wister A., Loewen N., Kennedy-Symonds H., McGowan B., McCoy B., Singer J. One-year follow-up of a therapeutic lifestyle intervention targeting cardiovascular disease risk. Can. Med. Assoc. J. 2007;177(8):859–865. doi: 10.1503/cmaj.061059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood D., De Backer G., Faergeman O., Graham I., Mancia G., Pyörälä K. Prevention of coronary heart disease in clinical practice: Recommendations of the Second Joint Task Force of European and other Societies on coronary prevention. Eur. Heart J. 1998;19:1434–1503. doi: 10.1016/s0021-9150(98)90209-x. [DOI] [PubMed] [Google Scholar]
- World Health Organization (Ed.), 2007. Prevention of cardiovascular disease: Guidelines for assessment and management of cardiovascular risk. World Health Organization.
- Wu Y., Liu X., Li X., Li Y., Zhao L., Chen Z., Li Y., Rao X., Zhou B., Detrano R., Liu K. Estimation of 10-year risk of fatal and nonfatal ischemic cardiovascular diseases in Chinese adults. Circulation. 2006;114(21):2217–2225. doi: 10.1161/CIRCULATIONAHA.105.607499. [DOI] [PubMed] [Google Scholar]
- Yousuf H., Reintjens R., Slipszenko E., Blok S., Somsen G.A., Tulevski I.I., Hofstra L. Effectiveness of web-based personalised e-Coaching lifestyle interventions. Netherlands Heart J. 2019;27(1):24–29. doi: 10.1007/s12471-018-1200-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.