Abstract
Ethiopia has been implementing its flagship social protection programme, Productive Safety Net Programme (PSNP), since 2005, mainly in drought prone and chronically food insecure woredas. In 2011, the country also launched Community-Based Health Insurance (CBHI). However, the two large-scale social protection programmes are not integrated well. This study examines the impact of participation in the conditional cash transfer (CCT) component of the PSNP (Public Works or PW) on enrolment in the CBHI among female-headed households in Amhara region.
Data for the study generated through a cross-sectional survey collected from 365 PW-participating and non-participating female-headed households in south Gondar zone, Ebinat woreda (district). Inverse-probability-weighted regression adjustment (IPWRA) estimator is used to evaluate the impact of participating in PW component on CBHI enrolment decisions.
Enrolment in CBHI among female-headed households is 63.6%. Data also show that 61.2% of insured and 27.1% of non-insured households receive CCTs. The study finds that participating in PSNP's CCT component increases the probability of CBHI enrolment among female-headed households by 16.3 percentage points. The finding informs efforts in integrating social protection programmes among most vulnerable households in rural Ethiopia. It also gives useful insights on the role of PSNP's CCT component to achieving universal health coverage through increasing insurance enrolment among most vulnerable households in Ethiopia.
Keywords: Community-based health insurance, Conditional cash transfer, Public works, Female-headed, Ethiopia
Highlights
-
•
Integrating social protection programs helps to build inclusive social protection systems.
-
•
Conditional cash transfers (CCTs) nudge enrolment in community-based health insurance.
-
•
CCTs are vital to achieve universal health coverage among vulnerable households.
-
•
Integrated social protection programs likely to result in equity in healthcare.
1. Introduction
1.1. Background
Globally, the proportion of the population with out-of-pocket (OOP) health spending exceeding 10% of their household budget increased from 9.4% in 2000 to 12.7% in 2015. Moreover, based on the relative poverty line of 60% of median daily per capita consumption or income, the percentage of the global population impoverished by OOP health spending also rose from 1.8% to 2.5% during the same period (WHO, 2019). However, past studies present mixed results on who are the most affected by and vulnerable to the rising OOP health spending. One approach to understand this has been devoted towards analysing households according to their headship. For example, a study conducted by Pan American Health Organization (PAHO) in Bolivia, Guatemala, Nicaragua, and Peru finds mixed results on the differences in the incidence of catastrophic health spending at the 10% threshold between female- and male-headed households, but female-headed households consistently reported greater OOP health spending in absolute terms at the household level in all four countries (WHO, 2019).
Related to the links between household headship and vulnerability and poverty, the empirical evidence so far is also ambiguous. The first strand of literature shows that female-headed households tend to be poorer in Africa (Milazzo & van de Walle, 2017) and some evidence in support of this come from different African countries (Buvinić & Gupta, 1997; Quisumbing et al., 2001; Sparreboom & Albee, 2011). These empirical and review studies report that female-headed households are the majority among the poor or tend to be generally poorer than their male-headed counterparts. However, recent studies have reported the opposite. It is argued equally that Africa's female-headed households are not systematically poorer, instead they are moderately less likely to be poorer compared to male-headed households (Castañeda et al., 2018). For example, in 2016, a study by the World Bank finds lower probability of being poor for female-headed households (19%) than for male-headed households (25%) in Ethiopia. One of the underlying factors related to the mixed evidence could be due to the heterogeneity in female headships, composition of households such as the dependence ratio, and access to resources such as land. This suggests that the comparative approach based on gender of headship may not provide helpful insights as the two are different. In Ethiopia, for instance, female farmers are less educated, have lower access to resources, less likely to attend extension programmes and less likely to use agricultural inputs such as fertiliser and improved seed, resulting in lower agricultural productivity (World Bank, 2020). These problems suggest that female-headed households could be generally more vulnerable to poverty and shocks (Klasen & Lechtenfeld, 2014; Kumar & Quisumbing, 2013), hence they deserve a special attention. As a result, due to the multidimensional and overlapping nature of their vulnerability, it is important to ensure that female-headed households are protected from various shocks such as ill-health and the associated financial and economic risks. Accordingly, in this study, we asked if female-headed households targeted by the conditional cash transfer (CCT) component of the Ethiopia's Productive Safety Net Programme (PSNP) were more likely to also enrol in the community-based health insurance (CBHI) compared to non-CCT female-headed households.
This study contributes to the literature in three ways: First, it gives empirical evidence how access to one type of social protection programme could nudge to adopt multiple shields against shocks and risks among female-headed households. The evidence could give insights whether female headship is also associated with more investments in contributory risk pooling systems due to access to CCT programmes, perhaps due to lack of informal networks to rely on during health-related shocks. Second, the evidence on the access to health insurance by female-headed households would have important policy implications towards universal health coverage (UHC) due to the rising nature of female-headed households and the proportion of population headed by women in Africa (Milazzo & van de Walle, 2017). More specifically, in Ethiopia, about 27% of households were headed by females in 2016 (World Bank, 2020). Evidence on the factors leading to better access to health insurance among them may help to inform social and public health policies aimed to ensure UHC and to leave-no-one behind among vulnerable groups. Third, unlike the past phases, the current phase of the PSNP (2020–2025) uses extreme poverty and vulnerability to extreme poverty through shocks as a key targeting criterion of locations and households instead of chronic food insecurity as was the case in the previous phases. Accordingly, female-headed households are identified as one of the priority groups due to their vulnerability resulted from low education and lower access to land and financial markets (FSCD, 2020; MoA, 2020). Lack of health insurance may increase the risk of households’ vulnerability to poverty due to health shocks that erodes their abilities to earn income and pay for essential healthcare services, food, and education. This points the importance of expanding health insurance coverage to reduce vulnerability to poverty. In this regard, understanding the barriers to health insurance coverage by female-headed households is vital to inform the programme about ‘what works better to reduce vulnerability to extreme poverty’ for female-headed households.
However, due mainly to data constraint, the scope of the study is limited and does not provide a more nuanced evidence. First, this study does not differentiate between different types of female headships. Second, like any other household level studies based on a unitary household model assumption, this study does not investigate the health insurance coverage at the individual level. Enrolment in the CBHI in Ethiopia is, however, possible at the household level only. Further, it should be also noted that this study is neither a gender analysis per se to assess gender inequality nor a comparison of households headed by females and males.
1.2. Country context: poverty and the social protection landscape
In 2016, 24% of Ethiopia's population (15% in the urban areas and 26% in rural areas) were living below the national poverty line (World Bank, 2020). This suggests that majority of the poor and vulnerable households will continue to reside in rural areas unless carefully designed policies and programmes are implemented to address the fundamental causes of poverty and vulnerability to poverty. The report also indicates that due to stagnated real consumption growth between 2011 and 2016 among the poorest 10% of the population, the poor in 2016 had lower monetary living standards than the poor in 2005, and, as a result, poverty severity in rural areas was higher in 2016 than in 2005 (World Bank, 2020).
Currently, social protection is a key component of government's policy framework to reduce poverty, social and economic risks, vulnerability, and exclusion (World Bank, 2020). The country enacted its National Social Protection Policy (NSPP) in 2014 and the National Social Protection Strategy (NSPS) in 2016 to harmonise and guide the implementations of fragmented social protection programmes in the country (UNICEF, 2018). However, the social protection system in Ethiopia is not developed well. As of 2020, only 7.4% of the population were covered by at least one social protection benefit (SDG indicator 1.3.1 – Population covered by at least one social protection benefit (excluding health)), and the universal health coverage is 39%. This is lower even compared to the sub-Saharan Africa average: 13.7% of the population is covered by non-health social protection programmes and 43.8% of the population covered by a social health protection scheme (ILO, 2021).
Ethiopia's current social protection landscape constitutes a range of programmes and schemes such as the rural PSNP, healthcare fee waive scheme, private social security, CBHI, and the urban version of the PSNP. The rural PSNP — nation's flagship and poverty-targeted social protection programme, was launched in 2005 with the aim of building resilience to shocks and improve food security among beneficiary households and communities (Phases 1 through 4) and to reduce extreme poverty and vulnerability to extreme poverty (Phase 5) (FSCD, 2020; MoA, 2020). The programme has two components: The Public Works (PW) and Permanent Direct Support (PDS). The PW component helps to mitigate food insecurity risks by providing employment opportunities in various public development works to the households with able-bodied members. It is the conditional cash transfer (CCT) component of the PSNP whereby households receive payments for their labour contributions in public work activities. In contrast, the PDS is an unconditional cash transfer (UCT) for the labour-poor households such as the elderly, people with disabilities and chronic illness, and orphaned children. The PSNP (PW and PDS combined) enrols about 8% Ethiopia's population (AfDB, 2020).
The CCT is the core component of the PSNP and creates a labour market for rural and unskilled labour, primarily by involving them in labour-intensive, community-based development works. It provides cash or food to participating households mainly during the labour slack period in the woreda. The cash transfer for the PW households is made for a period of six months annually, and the daily wage rate during the fourth phase (2015–2020) was cash equivalent to the cost of buying 3 kg of cereal and 800 g of pulses (15 kg of cereals and 4 kg of pulses per month per person) in the local market (MoA, 2014). This was equivalent to Birr 49 (about USD 1.2 during data collection) per day per person in the study woreda in 2021. A recent study in four rural Amhara woredas, including the study area, also showed that the average annual cash transfer to PW households was Birr 3805 (USD 133.5 based on the exchange rate during the survey) (ISNP Evaluation Team, 2020). A PW-participating household can employ up to 5 adult household members in PW activities and work for a total of 25 days per month.
The government of Ethiopia also piloted CBHI in 13 rural woredas in 2011. CBHI was introduced in the study woreda in 2015. However, so far, the linkage between PSNP and CBHI has not been established. In this study, we aim to provide evidence on the complementarities between the two social protection programmes through investigating the impact of participation in PSNP's CCT component (PW) on enrolment decisions in CBHI among female-headed households. CBHI enrolment could be an important step towards increasing the health services utilisation among resource-poor and food insecure female-headed households and achieving the goal of UHC in the country.
2. Related literature
CCT programmes were first introduced in Latin America in mid- and late-1990s on conditions in health, nutrition, and education co-responsibilities (Fizbein & Schady, 2009; Millán et al., 2019). Ethiopia's Productive Safety Net Programme is one of earlier major CT programmes in sub-Saharan Africa (Garcia & Moore, 2012). Currently, 46 sub-Saharan Africa countries have state-sponsored social protection programmes (Handa et al., 2021). The CCTs have been studied for their impacts related to health, education, nutrition, and food security in low- and middle-income counters. But results were inconclusive.
2.1. CCT programmes and healthcare utilisation and health outcomes
The evidence on the impacts of CCT programmes on healthcare utilisation and health outcomes is mixed. The first group of studies conclude that CCTs were found to increase the maternal and child health (MCH) services utilisations (Bastagli et al., 2016; Glassman et al., 2013; Lopez-Arana et al., 2016; Zhou et al., 2020) and health and nutrition outcomes (Bastagli et al., 2016; Leroy et al., 2009; Lopez-Arana et al., 2016). Zhou et al. (2020) find positive impact of a CCT programme on the uptake of MCH services and the knowledge of mothers about MCH health issues, but not on child health outcomes (low birth weight, anaemia, stunting, and wasting) in poor areas of Western rural China. The authors argue that poor CCT implementation and low quality of rural health facilities could be possible reasons why the positive improvements in MCH services and the knowledge of mothers about MCH health issues were not translated into substantial improvements in child health outcomes. However, contrary to their finding, other review studies (Bastagli et al., 2016; Glassman et al., 2013; Leroy et al., 2009) document that CCTs significantly improve anthropometric outcomes. Further, previous studies also show that CCT programmes increased the use of maternal health services including Antenatal care (ANC) visits, skilled attendance at birth, and health facility-based delivery (Glassman et al., 2013) and use of health facilities (Bastagli et al., 2016). CCT programmes also significantly increase child immunisation rates in India (Carvalho et al., 2014), vaccination coverage against major childhood diseases in rural Nicaragua (Barham & Maluccio, 2009), and growth and development check-ups in Colombia (Lopez-Arana et al., 2016). Positive impacts of CCTs are also reported on health seeking behaviour of households for under-five children in Burkina Faso (Akresh et al., 2016) and preventive care services use in Colombia (Lopez-Arana et al., 2016). One way through which CCT programmes could facilitate health services utilisation, health, and nutrition outcomes could be through easing the liquidity constraint in the insurance demand side and increasing insurance uptake by low-socioeconomic status households.
However, past studies also show insignificant impacts of CCTs on healthcare utilisation and health outcomes. Onwuchekwa et al. (2021), through a review of eight CCTs in seven sub-Sahara African countries, implemented between 2008 and 2016, find no sufficient ground on the impacts of CCTs on health service utilisation and children's nutritional status. Further, they report that none of the reviewed studies finds significant impacts on health status based on reported illness among children and immunisation rates. Another review study by Leroy et al. (2009) also documents non-significant impact of CCTs on micronutrient status of children. In Zimbabwe, Robertson et al. (2013) also report insignificant impact of CCT on the proportion of children with a full vaccination.
2.2. CCTs and health insurance
One of the main reasons for the above mixed evidence could be differences in the beneficiaries' decisions to buy health insurance coverage for members using cash transfer. This is particularly important in the Ethiopia's PW programme case where beneficiaries can freely allocate the cash transfer received through their labour contributions. In the literature, we find studies that examined the links between CT programmes and health insurance take-up (Biosca & Brown, 2015; Bossuyt, 2017; Evans et al., 2016; Hirvonen et al., 2021; Palermo et al., 2019; Shigute et al., 2017). Pilot CCT programme in rural Tanzania significantly increased the likelihood of using government-run health insurance programme (Community Health Fund or CHF) (Evans et al., 2016). In Mexico, a study by Biosca and Brown (2015) finds that participation in Oportunidades CCT programme is positively associated with awareness of enrolment in public health insurance. Palermo et al. (2019) also find significant impacts of integrating a fee waiver for the National Health Insurance Scheme (NHIS) with Ghana's Livelihood Empowerment Against Poverty (LEAP) 1000 cash transfer programme on health insurance enrolment. The studies show that CCT programmes may be used to promote participation of the lowest socio-economic groups in health insurance systems, facilitating the UHC in developing countries.
Studies conducted by Hirvonen et al. (2021), Bossuyt (2017) and Shigute et al. (2017) in Ethiopia also provide some insights, inconsistent though, on the linkages between PSNP-participation in general and CBHI enrolment decisions. A strong association between participation in PSNP and CBHI enrolment decisions was reported by Shigute et al. (2017). Using panel data from the pilot CBHI scheme (2011–2013), they find that PSNP households were 24 percentage points more likely to enrol into CBHI. However, despite positive impacts of PSNP participation on CBHI enrolment decisions during the CBHI pilot period, Bossuyt (2017) later finds only 22% of PW households were enrolled in CBHI in 2016. Using data from four major regions in 2016, Hirvonen et al. (2021) also find limited overlap between the PSNP and the CBHI schemes in CBHI operating districts (woredas). Their study also finds 22% of enrolment in CBHI by PSNP households in CBHI operating woredas.
There are, however, some gaps in the reviewed literature linking CCT programmes and health insurance take-up that require further study. First, although CCT participating groups, in general, tend to have lower socioeconomic statuses, their vulnerabilities to poverty and shocks differ. In this regard, a disaggregated approach based on participants' vulnerability to poverty and shocks such as by household headship could inform the design of policies to leave no-one-behind in the SDGs and increase their access to social services. Second, past studies conducted in Ethiopia also considered PSNP-participating households without disaggregating based on the conditions of targeting and cash transfer to identify the linkages between PSNP and CBHI and the causal effects of benefiting from PSNP on decisions to enrol in CBHI. The PDS clients are often offered CBHI enrolment fee waiver which clearly increases their insurance membership. In this study, we analysed how participation in the CCT component of the PSNP (the PW) affects households’ decisions to enrol in the community-based and contributory health insurance programme, the CBHI, by female-headed households. The PSNP considered female-headed households as one of the groups vulnerable to extreme poverty with lower access to resources such as farmland, credit, and financial markets.
3. Methods
3.1. Study area
The study is conducted in Ebinat woreda, one of the chronically food insecure and drought prone woredas in south Gondar zone, Amhara region. In 2020, the woreda population was estimated as 181,462 people (36,200 households), residing in 29 rural and 2 urban kebeles (communities). The administrative data also indicate that the woreda has 23,168 male-headed and 13,032 female-headed households. Of them, 6,339 households (3,299 male-headed and 3,040 female-headed) receive CCTs through participating in the PWs component of the PSNP (EWAO, 2020). However, the PSNP (2015–2020) did not reach all chronically food insecure households in drought prone areas of the woreda (EWAO, 2018).
3.2. Data and sample size
Data came from a cross-sectional survey conducted in March 2021 in three rural kebeles of Ebinat woreda. The kebeles were randomly selected from three different livelihood zones (North East Weyna Dega – mixed cereal livelihood zone, Tekezie lowland – Sorghum and Goats livelihood zone, and Tana Zuria livelihood zone) – one kebele was randomly selected from each livelihood zone. Interviews were conducted with 365 female-headed households (178 beneficiary and 187 non-beneficiary). We used Cochran's (1977) formula to determine the study sample size using 5% margin of error, 95% confidence level (Z = 1.96) and proportion of P = 0.39. The proportion is calculated as the ratio between the number of female-headed households in the PW component in 2020 (3,040) and the total number of female-headed households, excluding active and potential (based on the availability of able-bodied household members) PDS households, in the district (7,828). However, when distributing the sample between treatment and comparison households, we increased the sample size for treatment group by 10 percentage points to account for potential non-response and reduced the comparison sample by 10 percentage points.
While treatment female-headed households were selected randomly from kebele PW component beneficiary list, comparison households were selected from the list of female-headed households who were shortlisted for targeting by the kebele food security task force (KFSTF) in the past two years (retargeting rounds) but were excluded due to budget constraint. We conducted household listing in kebeles where there were no lists or incomplete administrative records to select comparison households. Thus, in addition to the new household listing, our main sampling frame was the list of female-headed households obtained from the KFSTF. The female-head (as per the registry status obtained from the KFSTF and self-identified during the household listing exercise due to migration of male heads, divorce, widowhood or being not ever married) was the main respondent for the survey. Primary data were collected using interview schedule (structured questionnaire). Data collection was conducted by enumerators recruited in the study area and trained on the survey questionnaire contents and research ethics. All sampled households were successfully interviewed.
3.3. Empirical strategy
We use inverse-probability-weighted regression adjustment (IPWRA) to investigate the impact of CCT programme on CBHI enrolment decisions. Unlike alternative estimators such as propensity score matching, IPWRA is a doubly robust method, whereby both the treatment assignments and the outcome equations are estimated within the same framework. The model requires either the treatment or outcome model to be specified correctly to calculate consistent treatment effect (Robins et al., 2007; StataCorp, 2013; Wooldridge, 2010).
Following Hirano and Imbens (2001), the model specification and weights for estimating ATE using IPWRA approach is:
where Yi is the outcome variable (enrolment in CBHI), and Ti is the treatment indicator (beneficiary of PSNP's CCT programme), Zi is the vector of covariates in the outcome equation, is the sample average of Z for the sub-sample of the households that participated in CCT programme, and εi is the error term. The weights in the model are given as:
where, ω(t,x) is the weight, t represents Ti=1, x is a vector of covariates in the propensity score equation, and p(x) is the estimated propensity score. The ATE is obtained using predicted outcomes of treatment and control households as:
The propensity score are obtained from the probability of inclusion in CCT given by Pr(Ti) = f(X), where Pr(Ti) is the probability of participation and X is a vector of covariates.
On the other hand, the ATT for the IPWRA estimator can be expressed as:
where nT is the number of CCT beneficiaries (T) and ri(X) is the regression model for the CCT and non-CCT (C) households based on observed covariates X and parameters γi = (δi, φi).
Where (inverse probability weighted parameters for CCT households) is obtained from a weighted regression procedure of:
and (inverse probability weighted parameters for non-CCT households) is obtained from a weighted regression procedure of:
We used Stata's Treatment Effects command to estimate both ATE and ATT.
3.4. Covariate selection
Covariates selected for the model include those related to the head such as sex and education status and household related factors including land and livestock ownership and household size by age, household's participation in other food security related interventions, access to credit, income from non-PSNP employment sources, participation agricultural trainings, and membership in community groups. We also controlled for community characteristic such as walking distances in minutes from home to the main trading centre (access to input and output markets), main water source, main road, and the nearest health centre. These variables are assumed to be less affected by households' inclusion into the PW component to meet the unconfoundedness (ignorability) assumption.
4. Results
4.1. Descriptive statistics
Table 1 presents descriptive statistics of covariates by CBHI enrolment status. Enrolment in CBHI is 63.6% (n = 232). Households who receive conditional cash transfer benefits through PSNP's PW component constitute 48.8% of the pooled sample (61.2% among insured and 27.1% among non-insured) households. Heads have an average age of 40.29 years and 35.3% of them can read and write. Their members are also composed of 2.195 children (aged under 18 years), 2.545 adults, and 0.381 elderlies. The results also show that only one in every four households owns agricultural land and 31.5% own livestock. This is in line with the general understanding and assessment that PSNP beneficiaries tend to be landless or near landless. The data also show that 15.9% of households participate in other food security programmes (OFSP), besides the PW component and 20.8% are members in associations or groups in the village.
Table 1.
Sample characteristics.
| (1) |
(2) |
(3) |
Mean diff t-test | ||||
|---|---|---|---|---|---|---|---|
| Pooled |
Insured |
Non-insured |
|||||
| Mean | SD | Mean | SD | Mean | SD | ||
| Household is PW beneficiary | 0.488 | 0.501 | 0.612 | 0.488 | 0.271 | 0.446 | 6.80*** |
| Age of female head | 40.29 | 10.145 | 40.901 | 9.227 | 39.226 | 11.534 | 1.43 |
| No. of members by age group | |||||||
| Under 18 years old | 2.195 | 0.962 | 2.341 | 1.011 | 1.940 | 0.814 | 4.13*** |
| Between 19 and 64 years | 2.545 | 1.573 | 2.647 | 1.516 | 2.368 | 1.658 | 1.59 |
| Above 64 years | 0.381 | 0.684 | 0.315 | 0.596 | 0.496 | 0.804 | −2.27** |
| Head is literate | 0.353 | 0.479 | 0.513 | 0.501 | 0.075 | 0.265 | 10.92*** |
| Household owns farmland | 0.277 | 0.448 | 0.409 | 0.493 | 0.045 | 0.208 | 9.83*** |
| Household owns livestock | 0.315 | 0.465 | 0.466 | 0.500 | 0.053 | 0.224 | 10.82 *** |
| Household participates in one or more OFSP | 0.159 | 0.366 | 0.241 | 0.429 | 0.015 | 0.122 | 7.52*** |
| Household is a member of any associations in the Kebele | 0.208 | 0.407 | 0.289 | 0.454 | 0.068 | 0.252 | 5.98*** |
| Income from non-PSNP employment | 5512.2 | 3588.4 | 6252.8 | 4662.8 | 4978.0 | 2459.0 | 1.66 |
| Household participated in agric. trainings in the past 12 months | 0.228 | 0.420 | 0.349 | 0.478 | 0.015 | 0.122 | 10.09*** |
| Accessibilities (walking distances in minutes) | |||||||
| Home to main trading centre | 70.142 | 64.799 | 66.250 | 67.574 | 76.932 | 59.286 | −1.57 |
| Home to main water source | 27.677 | 24.986 | 26.220 | 26.137 | 30.218 | 22.710 | −1.53 |
| Home to main road | 51.458 | 57.159 | 49.560 | 59.122 | 54.767 | 53.621 | −0.86 |
| Home to the nearest health centre | 69.145 | 63.895 | 65.586 | 66.997 | 75.353 | 57.809 | −1.46 |
| Household received credit in the last 12 months |
0.348 |
0.477 |
0.504 |
0.501 |
0.075 |
0.265 |
10.70*** |
| Observations | 365 | 232 | 133 | ||||
Note: significance levels: *P<0.1, **P<0.05, ***P<0.01.
With regards to the accessibility indicators, we find that households reside 70 min walking-distance far from the man trading centre, slightly less than half an hour from the main water source, above 50 min from the main road and above 1 h from the nearest health centre. About 34.8% of households also reported that they received credit in the past 12 months.
Bivariate analyses show that insured and non-insured female-headed households vary in several of the covariates controlled for. The two groups are significantly different on their membership in the PSNP/PW component, number of under 18 and above 64 years old members, head's literacy status, land and livestock ownerships, participation OFSPs, membership in groups and associations in the Kebele, participation in agricultural trainings in the past 12 months, and access to credit in the last 12 months. However, insured and non-insured households were not significantly different with respect to the age of heads, number of adult household members aged 19–64 years, income from non-PSNP employment, and accessibility indicators (i.e., walking distances in minutes from main trading centre, nearest water source, main road, and the nearest health centre).
4.2. IPWRA estimation results
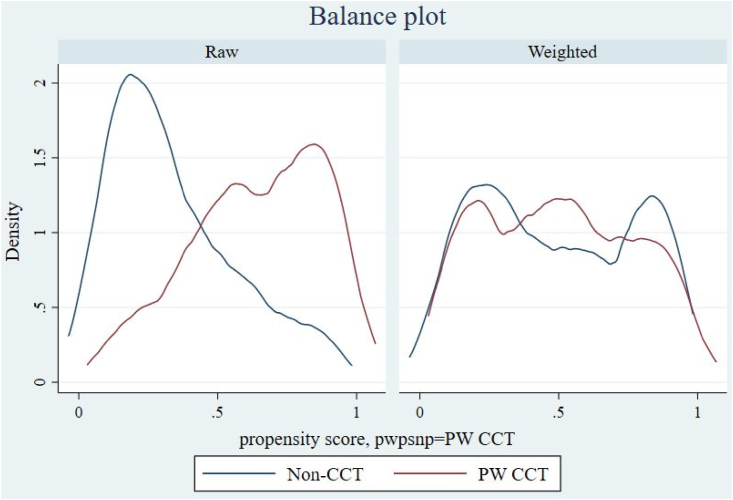
Checking for Balance – Density plots: The distribution of propensity scores is presented using Fig. 1. The density graphs show that propensity scores for insured and non-insured households were similar after weighting with clear overlap. This shows that, after weighting, households have similar chance of being included in the PSNP's conditional cash transfer programme.
Fig. 1.
Distribution of propensity scores between treatment arms before and after weighting.
Covariate Balancing: We also checked the balance between covariates between insured and non-insured households using the recommended absolute standardised mean difference (ASMD) (in covariates) method (Austin, 2009) and ratio between variances (Ali et al., 2019; Rubin, 2001). Balanced covariates between treated and non-treated households helps to create similar group of households so that differences in the outcome (CBHI uptake) can be attributed to the inclusion in the cash transfer. It also ensures the fulfilment of conditional independence assumption. The covariates said to have achieved balance if ASMD is below 0.1 (<10%) (Ali et al., 2016, 2019) and the variance ratio is closer to 1.0 (Ali et al., 2019; Rubin, 2001) or generally the variance ratios between 0.5 and 2 (Rubin, 2001). We presented the summary of covariate balance before and after weighting using Table 2. The standardised mean and proportion differences for weighted covariates are all below 0.1 and the variance ratios are mostly close to 1.0 and all are within the acceptable region. The standardised differences range between 0.001 with respect to access to credit and land ownership and 0.062 with respect to membership in local groups. On the other hand, the variance ratios range between 0.921 with respect to households' membership in local groups and 1.481 with respect to the number of adult household members aged between 19 and 64 years. Both tests suggest that covariates are balanced between insured and non-insured households on observed and controlled variables.
Table 2.
Covariate balance summary.
| Standardised differences |
Variance ratios |
|||
|---|---|---|---|---|
| Raw | Weighted | Raw | Weighted | |
| Age of female head | 0.335 | 0.056 | 1.058 | 1.024 |
| Age squared | 0.335 | 0.057 | 1.235 | 1.126 |
| No. of members by age group | ||||
| Under 18 years old | −0.041 | −0.015 | 1.384 | 1.077 |
| Between 19 and 64 years | 0.470 | 0.061 | 1.723 | 1.481 |
| Above 64 years | −0.077 | −0.002 | 1.096 | 1.160 |
| Head is literate | 0.844 | −0.006 | 1.749 | 0.997 |
| Household owns farmland | 0.215 | −0.001 | 1.241 | 0.999 |
| Household owns livestock | 0.406 | −0.028 | 1.389 | 0.978 |
| Household participates in one or more OFSP | 0.293 | 0.018 | 1.758 | 1.032 |
| Household is a member of any associations in the Kebele/ village | 0.381 | −0.062 | 1.766 | 0.921 |
| Income from non-PSNP employment (log) | −0.253 | 0.012 | 0.821 | 1.040 |
| Household participated in agricultural trainings in the past 12 months | 0.496 | 0.007 | 1.981 | 1.009 |
| Accessibilities (walking distances in minutes) | ||||
| Home to main trading centre | 0.011 | −0.009 | 1.214 | 1.023 |
| Home to main water source | 0.121 | 0.027 | 1.385 | 1.036 |
| Home to main road | 0.045 | −0.009 | 1.150 | 0.940 |
| Home to the nearest health centre | −0.008 | −0.017 | 1.171 | 1.001 |
| Household received credit in the last 12 months | 0.626 | −0.001 | 1.515 | 1.000 |
Overidentification test for covariate balance: following Imai and Ratkovic (2014), we also used the overidentification test for covariance balance to test if the covariates were balanced using tebalance overid command. We failed to reject the null hypothesis that covariates are balanced with test result of chi-square (18) = 4.663 and P = 0.999. The result of the overidentification test thus suggests that both treatment and comparison groups are balanced.
4.2.1. Impacts of PSNP's CCT component on CBHI enrolment
Table 3 presents the treatment effects of participating in CCT on the enrolment decisions in CBHI and treatment and regression adjustment equations. The average treatment effect (ATE) shows that participation in the PSNP's labour-based conditional cash transfer component leads to an increase in the probability of enrolment in CBHI by 16.3 percentage points (P < 0.01). Further, the impacts with respect to the average treatment effects on the treated (ATT) is 13.3 percentage points (P < 0.05). In non-experimental studies, it is expected that ATE and ATT differ due to potential selection bias.
Table 3.
Treatment effects of PSNP CCT (the PW) component on CBHI enrolment using IPWRA.
| (1) |
(2) |
|||
|---|---|---|---|---|
| ATE | ATT | |||
| Treatment effects of CCT | 0.163*** | [0.0676,0.257] | 0.133** | [0.0318,0.235] |
| Regression Adjustment for non-treated | ||||
| Age of female head | 0.0566** | [0.0127,0.101] | 0.102*** | [0.0466,0.157] |
| Age squared | −0.00072** | [-0.00128,-0.00016] | −0.0013*** | [-0.00199,-0.0006] |
| Number of household members | ||||
| Under 18 years old | 0.0653* | [-0.0051,0.136] | −0.00177 | [-0.086,0.0822] |
| Between 19 and 64 years | −0.0482 | [-0.121,0.0250] | −0.0357 | [-0.111,0.0391] |
| Above 64 years | 0.0739* | [-0.0116,0.159] | 0.0556 | [-0.0519,0.163] |
| Head is literate | 0.535*** | [0.331,0.739] | 0.514*** | [0.312,0.716] |
| Household owns farmland | 0.320*** | [0.151,0.489] | 0.103 | [-0.110,0.316] |
| Household owns livestock | 0.161 | [-0.0682,0.391] | 0.0750 | [-0.255,0.405] |
| Household participates in one or more OFSP | −0.0861 | [-0.387,0.215] | −0.212 | [-0.492,0.0681] |
| Household is a member of any associations in the Kebele/ village | −0.260** | [-0.483,-0.0377] | −0.294*** | [-0.515,-0.0729] |
| Income from non-PSNP employment (log) | −0.0269*** | [-0.0426,-0.0111] | −0.0446*** | [-0.0670,-0.0222] |
| Household participated in agricultural trainings in the past 12 months | −0.499*** | [-0.855,-0.143] | −0.294 | [-0.668,0.0795] |
| Home to the nearest health centre | −0.000565 | [-0.00221,0.00108] | −0.000576 | [-0.00247,0.00132] |
| Household received credit in the last 12 months | 0.248*** | [0.0728,0.424] | 0.0942 | [-0.105,0.294] |
| Constant | −0.648* | [-1.357,0.0612] | −1.125** | [-2.019,-0.230] |
| Regression Adjustment for treated | ||||
| Age of female head | 0.0528* | [-0.00801,0.114] | 0.0473** | [0.000778,0.0939] |
| Age squared | −0.000468 | [-0.00115,0.00022] | −0.000403 | [-0.00092,0.000118] |
| Number of household members | ||||
| Under 18 years old | −0.0282 | [-0.0899,0.0336] | 0.0229 | [-0.0275,0.0732] |
| Between 19 and 64 years | −0.0146 | [-0.0567,0.0275] | −0.0271 | [-0.0610,0.00683] |
| Above 64 years | −0.255*** | [-0.358,-0.152] | −0.234*** | [-0.306,-0.163] |
| Head is literate | 0.00509 | [-0.210,0.220] | 0.0604 | [-0.144,0.265] |
| Household owns farmland | 0.152* | [-0.00634,0.310] | 0.139*** | [0.0555,0.223] |
| Household owns livestock | 0.326*** | [0.130,0.522] | 0.242*** | [0.0692,0.415] |
| Household participates in one or more OFSP | −0.0759 | [-0.224,0.0726] | −0.00561 | [-0.132,0.121] |
| Household is a member of any associations in the Kebele/ village | 0.121* | [-0.0224,0.264] | 0.132* | [-0.00359,0.267] |
| Income from non-PSNP employment (log) | −0.0278*** | [-0.0478,-0.00779] | −0.0126* | [-0.0269,0.00172] |
| Household participated in agricultural trainings in the past 12 months | 0.00376 | [-0.142,0.150] | 0.0162 | [-0.113,0.145] |
| Home to the nearest health centre | −0.000399 | [-0.0015,0.00073] | −0.00007 | [-0.00092,0.00078] |
| Household received credit in the last 12 months | −0.0667 | [-0.241,0.108] | −0.0905 | [-0.276,0.0950] |
| Constant |
−0.429 |
[-1.607,0.750] |
−0.471 |
[-1.388,0.446] |
| Treatment model (Probit) | ||||
| Age of female head | −0.0176 | [-0.145,0.110] | −0.0176 | [-0.145,0.110] |
| Age squared | 0.000471 | [-0.00105,0.0020] | 0.000471 | [-0.00105,0.0020] |
| Number of household members | ||||
| Under 18 years old | −0.128 | [-0.311,0.0544] | −0.128 | [-0.311,0.0544] |
| Between 19 and 64 years | 0.121** | [0.00240,0.239] | 0.121** | [0.00240,0.239] |
| Above 64 years | −0.0398 | [-0.263,0.183] | −0.0398 | [-0.263,0.183] |
| Head is literate | 1.411*** | [0.824,1.998] | 1.411*** | [0.824,1.998] |
| Household owns farmland | −0.104 | [-0.463,0.256] | −0.104 | [-0.463,0.256] |
| Household owns livestock | −0.622** | [-1.164,-0.0796] | −0.622** | [-1.164,-0.0796] |
| Household participates in one or more OFSP | −0.612* | [-1.311,0.0876] | −0.612* | [-1.311,0.0876] |
| Household is a member of any associations in the Kebele/ village | 0.274 | [-0.230,0.778] | 0.274 | [-0.230,0.778] |
| Income from non-PSNP employment (log) | −0.0187 | [-0.0577,0.0203] | −0.0187 | [-0.0577,0.0203] |
| Household participated in agricultural trainings in the past 12 months | 0.425 | [-0.291,1.141] | 0.425 | [-0.291,1.141] |
| Accessibilities (walking distances in minutes) | ||||
| Home to main trading centre | −0.00749 | [-0.0245,0.00952] | −0.00749 | [-0.0245,0.00952] |
| Home to main water source | 0.0398*** | [0.0232,0.0564] | 0.0398*** | [0.0232,0.0564] |
| Home to main road | 0.00950 | [-0.00662,0.0256] | 0.00950 | [-0.00662,0.0256] |
| Home to the nearest health centre | −0.0113* | [-0.0242,0.00170] | −0.0113* | [-0.0242,0.00170] |
| Household received credit in the last 12 months | 0.472* | [-0.0288,0.972] | 0.472* | [-0.0288,0.972] |
| Constant |
−0.877 |
[-3.226,1.472] |
−0.877 |
[-3.226,1.472] |
| Observations | 365 | 365 | ||
95% confidence intervals in brackets; *p < 0.1, **p < 0.05, ***p < 0.01.
4.3. Predictors of inclusion in the CCT
In Table 3, the treatment model (probit regression) presents factors predicting inclusion of female-headed households into the PSNP's labour-based CCT component. Factors predicating programme inclusion include literacy status of the head, the number of adult household members, walking distance from home to the main water source, and access to credit by the household. Factors that predict exclusion from the CCT include livestock ownership, participations in one or more of other food security programmes, and distance from the nearest health centre. Characteristics that do not significantly associate with inclusion into the CCT programme among female headed households include age of the head, number of children and elderly household members, land ownership, membership in community groups, income from non-PSNP employment in the past 12 months, and participation in agricultural trainings in the past 12 months. Walking distances from home to the main trading centre and main road also do not predict inclusion into the labour-based CCT programme of the PSNP among female-headed households in the woreda.
5. Robustness check
We checked the robustness of our results to estimation approaches through running a regression adjustment (RA) treatment-effects estimator. Unlike IPWRA, RA model the outcome model only and uses contrasts of averages of treatment-specific predicted outcomes to estimate treatment effects (StataCorp, 2013). The RA estimators are consistent if the treatment is independent of the potential outcomes after conditioning on the covariates. The results are presented in Table 4. Despite slight reductions in the coefficients, our findings were robust for the change in the treatment-effects estimator.
Table 4.
Robustness check for the treatment effects of CCT on CBHI enrolment.
| (1) |
(2) |
|||
|---|---|---|---|---|
| ATE | ATT | |||
| Treatment effects of CCT | 0.156*** | [0.0672,0.245] | 0.124** | [0.0214,0.226] |
| Observations | 365 | 365 |
95% confidence intervals in brackets; *p < 0.1, **p < 0.05, ***p < 0.01.
6. Discussion
This study is the first to examine the effects of PSNP's PW component alone on CBHI enrolment decisions among female-headed households in chronically food insecure and drought prone setting in Ethiopia. The findings may contribute to better understand the complementarities between social protection programmes among the most vulnerable households. The PSNP and CBHI are the two largest social protection programmes in the country. We find that participating in PSNP's labour-based CCT component (the PW) led to increased likelihood of enrolment in CBHI. Although it is beyond the scope of this study to investigate the pathways, we hypothesise that the impact of CCT on CBHI enrolment decision could be through easing financial constraints to pay for CBHI registration and annual fees, increasing households' awareness about the benefits of health insurance, and improving households' health-seeking behaviour through information from community health extension workers, social workers, and other platforms such as behavioural change communication (BCC) sessions.
The result gives insights on how access to a poverty-targeted CCT programme (PW cash transfer) could also nudge enrolment decisions in a contributory health-targeted social protection scheme even among vulnerable groups, and its implications for an inclusive social protection system and healthcare utilisation. The rapid decline of food insecurity in Ethiopia between 2005 and 2016 but deepening of the extreme poverty for the poorest 10% led the PSNP to shift its targeting criterion in the current phase from chronic food insecurity to extreme poverty and vulnerability to extreme poverty to address the needs of the extreme poor and the most vulnerable (MoA, 2020). In this regard, female-headed households are among the specific target groups due to their vulnerability due to low human capital, lower access to land and finance, low adoption of productivity-enhancing agricultural inputs, and substantially lower wages for similar characteristics compared to their male counterparts (MoA, 2020). This suggests that due to lower income and higher financial constraints, female-headed households are vulnerable to health-related risks such as high OOP health spending as well. The PSNP also underscores that there is low health and health insurance service seeking behaviour which constrain vulnerable households' access to social services (FSCD, 2020). In this regard, our study shows that access to the PW cash transfer by female-headed households also increases the demand for health insurance. Enrolment in health insurance is more likely to reduce the financial barriers and increases their access to affordable healthcare services. The evidence also shows the potentials of PW cash transfer to establish inclusive and integrated social protection system that works for the most vulnerable groups in drought prone areas.
Our finding has also important implications towards health equity and UHC among vulnerable households in drought prone and chronically food insecure woredas in Ethiopia. The findings that low-income, food insecure, and vulnerable households such as the female-headed households likely to join CBHI through PW cash transfer is critical to improve equity in the provision of basic health care services and shield them against risks from catastrophic OOP health spending and distress productive asset sales to finance health spending. As insurance enrolment could nudge more health seeking behaviour, our findings also give insights on the potentials of PW cash transfer programme in achieving nation's UHC among vulnerable households in rural Ethiopia.
The fact that more than one in every four households in Ethiopia are headed by women also means insurance coverage against the risk of high OOP health spending among this group will have paramount implications for extreme poverty reduction. The lack of affordable quality healthcare services, often due to lower health insurance coverage, leads to poor health and impoverishment, disproportionally affecting the most vulnerable groups (ILO, 2021). For example, in 2015, 1.01% of Ethiopia's population were pushed below a relative poverty line (60% of median per capita income or consumption) due to high OOP spending on healthcare (WHO, 2019). This shows that access to health insurance among female-headed households can reduce poverty not only among the vulnerable groups but also at the national level through reducing high OOP health spending and reducing the risks of distress productive asset sales to finance healthcare services.
However, for further improvement in CBHI enrolment among female-headed households and effective utilisation of healthcare services using CBHI, gender-sensitive (of headship) social protection programmes could be designed so that PW households will receive cash transfers even when the female head is pregnant or lactating.
Our finding is consistent with conclusions from past studies such as Biosca and Brown (2015) in Mexico, Evans et al. (2016) in Tanzania, Palermo et al. (2019) in Ghana, and Shigute et al. (2017) in Ethiopia. They also find that CCT programmes in the respective study countries increase the probability of health insurance enrolment decisions among cash transfer beneficiaries. However, the extents to which CCT programmes increase enrolment in health insurance vary. For example, Evans et al. (2016) report a larger impact compared to our estimates. They find that after 2.5 years, the 2010 pilot CCT programme in rural Tanzania increased households' take-up of the government-run health insurance programme in treatment villages by 36 percentage points. In Ethiopia, Shigute et al. (2017) also find that participating in the PSNP (PW – conditional and PDS – unconditional CT components) increases the likelihood of enrolment in the pilot CBHI scheme by 24 percentage points. In Ghana, a study by Palermo et al. (2019) reports that integrating a fee waiver for the National Health Insurance Scheme (NHIS) with Livelihood Empowerment Against Poverty (LEAP) 1000 cash transfer programme increases enrolment in NHIS by 14 percentage points. This estimate is slightly lower than our finding. The study characteristics including sample sizes, types of households under consideration such as the nature of headships, the amount, frequency, and conditions of cash transfers could be among the factors for differences in the extents to which CCT programmes nudge health insurance take-up. For example, while PW households in Ethiopia are expected to contribute labour to public work activities to receive cash transfers, the conditions for the CCT programme in Tanzania include visits to health clinics by young children aged 0–5 years and by the elderly aged 60 years and above (Evans et al., 2016). This shows that while the PSNP's PW condition is directly unrelated to health-related behaviours, Tanzania's CCT programme conditions may directly increase health seeking behaviours through repeated visits to health facilities and improve households' awareness about the benefits of health insurance. However, after targeting, monthly BCC sessions are also organized for PW clients at the public work sites on various issues including health (focusing on preventive health and health seeking behaviour) and nutrition. PW clients are expected to attend six, at least 2-h, BCC sessions during the six months period of the public work which will be counted as public work activities. This may also result in health-related behavioural changes among PW households, the pathways and extents could differ though.
Our finding contrasts with other past studies in Ethiopia by Hirvonen et al. (2021) and Bossuyt (2017). They find that enrolment in CBHI by PSNP households is very limited. For example, Hirvonen et al. (2021) find that about 22% of the PSNP households are enrolled into CBHI in woredas where CBHI is operating. However, it is not clear how much of this enrolment was due to membership in PSNP, in general, and particularly in the PW component.
Important differences exist between ours and previous studies in Ethiopia. Firstly, the analyses by Shigute et al. (2017), Hirvonen et al. (2021) and Bossuyt (2017) were not disaggregated by headship of beneficiaries. As a result, their findings were less informative how female-headed PW beneficiary households make investments in health such as through buying health insurance. The evidence in this regard is very useful to inform social protection policy from a vulnerability perspective in the country. Secondly, their data, particularly for Shigute et al. (2017), came from the pilot CBHI scheme collected during 2011–2013, hence it is unlikely to give up-to-date insights on the uptake of CBHI by PSNP households. Thirdly, our study focuses on PW or the CCT beneficiary of the PSNP alone as treatments, while previous studies analyse the PSNP households without disaggregating by PSNP beneficiary types. Such approach could mask important details as PW and PDS households are different in terms of their key characteristics such as availability of able-bodied persons who could participate in the labour markets and earn additional incomes and their vulnerability to shocks. Unlike the PDS clients, PW households are often excluded from the CBHI premium fee waiver and health services fee waiver schemes and expected to be paying members of CBHI. For example, the CBHI provides premium fee waiver for the 10% of the poorest population, including PDS clients, in the woreda (Mebratie et al., 2015; Mekonen et al., 2018). Moreover, currently, a pilot programme (aimed at integrating PSNP and CBHI programmes) is also being implemented in the Amhara region to automatically enrol all PDS clients into CBHI programme and renew their insurance membership free of the registration and annual premium fees (ISNP Evaluation Team, 2020). This shows that the issue of how PSNP affects CBHI enrolment decisions among PDS clients is a lesser important policy question. What is more, including PDS clients in estimating the causal effects of PSNP on CBHI enrolment decisions is more likely to overestimate the programme impacts. On the other hand, except some of essential healthcare services such as family planning, antenatal cares, immunisation and vaccinations services, and management of new-born and childhood illness which are available free of cost to everyone at public health facilities, PW households tend to pay for all healthcare services. In this respect, our study provides new evidence that access to PW cash transfer by female-headed households could also nudge enrolment decisions to CBHI.
There are limitations to our study. We used cross-sectional data collected from a relatively small sample size, compared to some other studies and from one woreda only. Thus, the findings are not generalisable to the whole region or country. In addition, estimates may be affected by targeting biases into the PSNP's PW component based on unobservable and omitted characteristics such as kinship and network. In this regard, although other methods such as difference-in-difference could effectively reduce the risk of bias in the estimation, however, this needs baseline household data. Further, households were matched based on a small number of observable characteristics. Future research may investigate how enrolment into CBHI nudges health—seeking behaviours, reduces catastrophic out-of-pocket health spending, and investment in preventive health practices among female-headed households.
7. Conclusions
The study investigates the effects of participation in the PSNP's PW component on CBHI enrolment decisions among female-headed households in chronically food insecure and drought prone area in rural Ethiopia. We find that participation in the PW component of the PSNP increased the probability of enrolment in CBHI by 16.3 percentage points. The findings give important insights on the complementarities between social protection programmes among most vulnerable households in rural Ethiopia and the role of PSNP's CCT component on CBHI enrolment thereby in achieving UHC in the informal sectors in drought prone and chronically food insecure woredas in Ethiopia. In this regard, more work needs to be done to expand access to the CCT programme among vulnerable groups to better link the two major social protection programmes and protect such groups against shocks due to ill-health and high OOP health spending.
The study also suggests that targeting female-headed households who are identified as vulnerable to extreme poverty by the PSNP's CCT component could improve access to affordable healthcare through enrolment in community-based and contributory health insurance programme. Membership in health insurance is also more likely to avoid catastrophic OOP health spending and distress productive asset sales during members' sickness thereby contributes to reducing extreme poverty and vulnerability to extreme poverty. However, future research may explore the health seeking behaviours and individual health outcomes of enrolment in CBHI among vulnerable groups.
Ethics and consent to participate
The study was approved by the Department Research Committee (DRC) of the department of Agricultural Economics at the University of Gondar. Oral consent has been obtained from all survey respondents during interviews to participate in the study and consent was obtained from them to use their anonymised information. All methods were performed in accordance with the relevant guidelines and regulations.
Authors' contributions
ECM and ENR conceptualized the topic for this manuscript and were responsible for the research design. ECM and ENR planned and conducted the statistical analysis. ECM wrote the first draft of the manuscript. ECM, ENR, and DA contributed to interpretation of analyses and revised the manuscript. DA coordinated the data collection. All authors read and approved the final manuscript.
Funding
The data collection of the work is funded partially by the University of Gondar. Funding body did not have a role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Declaration of competing interest
The authors declare that they have no competing interests.
References
- AfDB . African Development Bank; 2020. African economic Outlook 2020: Developing Africa's workforce for the future. [Google Scholar]
- Akresh R., de Walque D., Kazianga H. In: African Successes, Volume II: Human capital. Edwards S., Johnson S., Weil D.N., editors. University of Chicago Press; 2016. Alternative cash transfer delivery mechanisms: Impacts on routine preventative health clinic visits in Burkina Faso. [Google Scholar]
- Ali M.S., Groenwold R.H., Klungel O.H. Best (but oft-forgotten) practices: Propensity score methods in clinical nutrition research. The American Journal of Clinical Nutrition. 2016;104(2):247–258. doi: 10.3945/ajcn.115.125914. [DOI] [PubMed] [Google Scholar]
- Ali M.S., Prieto-Alhambra D., Lopes L.C., Ramos D., Bispo N., Ichihara M.Y., Pescarini J.M., Williamson E., Fiaccone R.L., Barreto M.L., Smeeth L. Propensity score methods in health technology assessment: Principles, extended applications, and recent advances. Frontiers in Pharmacology. 2019;10:973. doi: 10.3389/fphar.2019.00973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin P.C. Some methods of propensity-score matching had superior performance to others: Results of an empirical investigation and Monte Carlo simulations. Biometrical Journal. 2009;51(1):171–184. doi: 10.1002/bimj.200810488. [DOI] [PubMed] [Google Scholar]
- Barham T., Maluccio J.A. Eradicating diseases: The effect of conditional cash transfers on vaccination coverage in rural Nicaragua. Journal of Health Economics. 2009;28(3):611–621. doi: 10.1016/j.jhealeco.2008.12.010. [DOI] [PubMed] [Google Scholar]
- Bastagli F., Hagen-Zanker J., Harman L., Barca V., Sturge G., Schmidt T. 2016. Cash transfers: What does the evidence say? A rigorous review of programme impact and of the role of design and implementation features. [Google Scholar]
- Biosca O., Brown H. Boosting health insurance coverage in developing countries: Do conditional cash transfer programmes matter in Mexico? Health Policy and Planning. 2015;30(2):155–162. doi: 10.1093/heapol/czt109. [DOI] [PubMed] [Google Scholar]
- Bossuyt A. Reaching the poor: Synergies and complementarities of the productive safety net programme and the community based health insurance. Social Policy and Evidence for Social Inclusion (SPESI), UNICEF Ethiopia Country Office. 2017 www.unicef.org/ethiopia/policy_evidence.html [Google Scholar]
- Buvinić M., Gupta G.R. Female-headed households and female-maintained families: Are they worth targeting to reduce poverty in developing countries? Economic Development and Cultural Change. 1997;45(2):259–280. doi: 10.1086/452273. [DOI] [Google Scholar]
- Carvalho N., Thacker N., Gupta S.S., Salomon J.A. More evidence on the impact of India's conditional cash transfer program, janani suraksha yojana: Quasi-experimental evaluation of the effects on childhood immunization and other reproductive and child health outcomes. PLoS One. 2014;9(10) doi: 10.1371/journal.pone.0109311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castañeda A., Doan D., Newhouse D., Nguyen M.C., Uematsu H., Azevedo J.P. Vol. 101. World Development; 2018. pp. 250–267. (A new Profile of the global poor). [DOI] [Google Scholar]
- Cochran W.G. Sampling Techniques. 3rd Edition. John Wiley & Sons; New York: 1977. [Google Scholar]
- Evans D.K., Holtemeyer B., Kosec K. World Bank; 2016. Cash transfers and health: Evidence from Tanzania. [Policy Research Working Paper] [Google Scholar]
- EWAO . 2018. Ebinat woreda Bureau agriculture Office report, 2017/18. Ebinat woreda, Amhara region, Ethiopia. [Google Scholar]
- EWAO . 2020. Ebinat woreda agriculture Office. Ebinat woreda, Amhara region, Ethiopia. [Google Scholar]
- Fizbein A., Schady N. The International Bank for Reconstruction and Development/The World Bank; 2009. Conditional cash transfers: Reducing Present and future poverty [A World Bank policy research report] [Google Scholar]
- FSCD . Food Security Coordination Directorate (FSCD); Addis Ababa, Ethiopia: 2020. Productive Safety Net program phase 5 (PSNP5) 2020—2025: Design document. Federal Ministry of agriculture. [Google Scholar]
- Garcia M., Moore C.M.T. In: The cash Dividend. Garcia M., Moore C.M.T., editors. The World Bank; 2012. The rise of cash transfer programs in sub-saharan Africa; pp. 31–73. [DOI] [Google Scholar]
- Glassman A., Duran D., Fleisher L., Singer D., Sturke R., Angeles G., Charles J., Emrey B., Gleason J., Mwebsa W., Saldana K., Yarrow K., Koblinsky M. Impact of conditional cash transfers on maternal and newborn health. 2013;31(4):19. [PubMed] [Google Scholar]
- Handa S., Otchere F., Sirma P. More evidence on the impact of government social protection in sub saharan Africa: Ghana, Malawi and Zimbabwe. Development Policy Review. 2021;37 doi: 10.1111/DPR.12576. [DOI] [Google Scholar]
- Hirano K., Imbens G.W. Estimation of causal effects using propensity score weighting: An application to data on right heart catheterization. Health Services & Outcomes Research Methodology. 2001;2:259–278. [Google Scholar]
- Hirvonen K., Bossuyt A., Pigois R. Evidence from the productive safety net programme in Ethiopia: Complementarities between social protection and health policies. Development Policy Review. 2021;39(4):532–547. doi: 10.1111/dpr.12516. [DOI] [Google Scholar]
- ILO . International Labour Organization; Geneva: 2021. World Social Protection Report 2020–22: Social protection at the crossroads ‒ in pursuit of a better future. [Google Scholar]
- Imai K., Ratkovic M. Covariate balancing propensity score. Journal of the Royal Statistical Society: Series B. 2014;76(1):243–263. [Google Scholar]
- ISNP Evaluation Team . UNICEF Office of Research – Innocenti; 2020. Impact evaluation of the integrated Safety Net programme in the Amhara region of Ethiopia. Final baseline report. [Google Scholar]
- Klasen S., Lechtenfeld T. World Development; 2014. A Feminization of vulnerability? Female headship, poverty, and vulnerability in Thailand and Vietnam. [Google Scholar]
- Kumar N., Quisumbing A. Gendered impacts of the 2007– 2008 food price crisis: Evidence using panel data from rural Ethiopia. Food Policy. 2013;38:11–22. [Google Scholar]
- Leroy J.L., Ruel M., Verhofstadt E. The impact of conditional cash transfer programmes on child nutrition: A review of evidence using a programme theory framework. Journal of Development Effectiveness. 2009;1(2):103–129. doi: 10.1080/19439340902924043. [DOI] [Google Scholar]
- Lopez-Arana S., Avendano M., van Lenthe F.J., Burdorf A. The impact of a conditional cash transfer programme on determinants of child health: Evidence from Colombia. Public Health Nutrition. 2016;19(14):2629–2642. doi: 10.1017/S1368980016000240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mebratie A.D., Sparrow R., Yilma Z., Alemu G., Bedi A.S. Enrollment in Ethiopia's community-based health insurance scheme. World Development. 2015;74:58–76. doi: 10.1016/j.worlddev.2015.04.011. [DOI] [PubMed] [Google Scholar]
- Mekonen A.M., Gebregziabher M.G., Teferra A.S. The effect of community based health insurance on catastrophic health expenditure in northeast Ethiopia: A cross sectional study. PLoS One. 2018;13(10) doi: 10.1371/journal.pone.0205972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milazzo A., van de Walle D. Women left behind? Poverty and headship in Africa. Demography. 2017;54(3):1119–1145. doi: 10.1007/s13524-017-0561-7. [DOI] [PubMed] [Google Scholar]
- Millán T.M., Barham T., Macours K., Maluccio J.A., Stampini M. Long-term impacts of conditional cash transfers: Review of the evidence. The World Bank Research Observer. 2019;34(1):119–159. doi: 10.1093/wbro/lky005. [DOI] [Google Scholar]
- MoA Productive safety net programme phase IV programme implementation manual. Ministry of Agriculture, Addis Ababa, Ethiopia. 2014 [Google Scholar]
- MoA . 2020. General programme implementation manual. Ministry of agriculture, Addis Ababa, Ethiopia. [Google Scholar]
- Onwuchekwa C., Verdonck K., Marchal B. Systematic review on the impact of conditional cash transfers on child health service utilisation and child health in sub-saharan Africa. Frontiers in Public Health. 2021;9:643621. doi: 10.3389/fpubh.2021.643621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palermo T.M., Valli E., Ángeles-Tagliaferro G., de Milliano M., Adamba C., Spadafora T.R., Barrington C., LEAP 1000 Evaluation Team Impact evaluation of a social protection programme paired with fee waivers on enrolment in Ghana's National Health Insurance Scheme. BMJ Open. 2019 doi: 10.1136/bmjopen-2018-028726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quisumbing A.R., Haddad L., Peña C. Are women overrepresented among the poor? An analysis of poverty in 10 developing countries. Journal of Development Economics. 2001;66(1):225–269. doi: 10.1016/S0304-3878(01)00152-3. [DOI] [Google Scholar]
- Robertson L., Mushati P., Eaton J.W., Dumba L., Mavise G., Makoni J., Schumacher C., Crea T., Monasch R., Sherr L., Garnett G.P., Nyamukapa C., Gregson S. Effects of unconditional and conditional cash transfers on child health and development in Zimbabwe: A cluster-randomised trial. The Lancet. 2013;381(9874):1283–1292. doi: 10.1016/S0140-6736(12)62168-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins J., Sued M., Lei-Gomez Q., Rotnitzky A. Comment: Performance of double-robust estimators when “inverse probability” weights are highly variable. Statistical Science. 2007;22(4):544–559. doi: 10.1214/07-STS227D. [DOI] [Google Scholar]
- Rubin D.B. Using propensity scores to help design observational studies: Application to the tobacco litigation. Health Services & Outcomes Research Methodology. 2001;2(3):169–188. [Google Scholar]
- Shigute Z., Mebratie A.D., Sparrow R., Yilma Z., Alemu G., Bedi A.S. Uptake of health insurance and the productive safety net program in rural Ethiopia. Social Science & Medicine. 2017;176:133–141. doi: 10.1016/j.socscimed.2017.01.035. [DOI] [PubMed] [Google Scholar]
- Sparreboom T., Albee A. International Labour Office; 2011. Towards decent work in sub-Saharan Africa Monitoring MDG employment indicators. [Google Scholar]
- StataCorp STATA treatment effects reference manuala: Potential Outcomes/Counterfactual Outcomes. Reealse. 2013;13 A Stata Press Publication. [Google Scholar]
- UNICEF . 2018. Social protection. Updated with national data for 2017/18 [Budget Brief] [Google Scholar]
- WHO . Global Monitoring report] Conference Edition. World Health Organization; 2019. Primary health care on the road to universal health coverage. 2019. [Google Scholar]
- Wooldridge J.M. 2nd ed. MIT Press; 2010. Econometric analysis of cross section and panel data. [Google Scholar]
- World Bank . International Bank for Reconstruction and Development/The World Bank; Washington, DC: 2020. Ethiopia poverty assessment: Harnessing continued growth for accelerated poverty reduction. [Google Scholar]
- Zhou H., Wu Y., Liu C., Sun C., Shi Y., Zhang L., Medina A., Rozelle S. Conditional cash transfers, uptake of maternal and child health services, and health outcomes in western rural China. BMC Public Health. 2020;20(1):870. doi: 10.1186/s12889-020-08996-9. [DOI] [PMC free article] [PubMed] [Google Scholar]