Abstract
Objective
This study aimed to understand the association between primary care physician (PCP) proficiency with the electronic health record (EHR) system and time spent interacting with the EHR.
Materials and Methods
We examined the use of EHR proficiency tools among PCPs at one large academic health system using EHR-derived measures of clinician EHR proficiency and efficiency. Our main predictors were the use of EHR proficiency tools and our outcomes focused on 4 measures assessing time spent in the EHR: (1) total time spent interacting with the EHR, (2) time spent outside scheduled clinical hours, (3) time spent documenting, and (4) time spent on inbox management. We conducted multivariable quantile regression models with fixed effects for physician-level factors and time in order to identify factors that were independently associated with time spent in the EHR.
Results
Across 441 primary care physicians, we found mixed associations between certain EHR proficiency behaviors and time spent in the EHR. Across EHR activities studied, QuickActions, SmartPhrases, and documentation length were positively associated with increased time spent in the EHR. Models also showed a greater amount of help from team members in note writing was associated with less time spent in the EHR and documenting.
Discussion
Examining the prevalence of EHR proficiency behaviors may suggest targeted areas for initial and ongoing EHR training. Although documentation behaviors are key areas for training, team-based models for documentation and inbox management require further study.
Conclusions
A nuanced association exists between physician EHR proficiency and time spent in the EHR.
Keywords: EHR use, EHR optimization, primary care physicians, documentation burden
INTRODUCTION
Researchers have increasingly reported on the association between the burden imposed by the use of electronic health record (EHR) systems and physician burnout.1–5 EHR-related burden stems from many factors, such as usability issues, systems implementation issues (eg, lack of sufficient EHR support, training), and documentation burden from the payer and quality reporting requirements.1,6 Consequently, EHR vendors, federal agencies, and healthcare organizations are exploring solutions to reduce clinicians’ EHR-related burden.3,7–11
Physicians spend an estimated 50% of their time on EHR tasks,12–15 which include documentation, inbox management, and chart review.15–21 However, physician-level factors, such as specialty, may influence differences in EHR-related burden.17,21–24 For instance, primary care physicians (PCPs) spent more time in the EHR when compared with specialists.17,25,26 This EHR burden is likely to grow over time, as patient complexity (eg, comorbidities, aging of the population) increases and new payment models are developed.27–31 Thus, additional information will be needed to identify how PCPs’ EHR use patterns may be adapted to increase efficiency.
Improving EHR proficiency skills, through optimal use of EHR proficiency and efficiency tools to facilitate workflow, has been suggested as a path to reducing time spent in the EHR.32–36 A 2020 single-center study found that self-reported after-hours time spent in the EHR was positively associated with EHR-derived measures of after-hours use.37 However, self-reported EHR proficiency showed mixed associations with after-hours EHR use.37 EHR proficiency scores, as calculated by the EHR vendor, were negatively correlated with EHR-derived measures of time spent in the EHR after-hours.37 These EHR proficiency scores are challenging to interpret, in part, due to the scores’ proprietary calculations.37,38 To improve our understanding of what drives clinicians’ time spent in the EHR, there is a need to parse out which specific EHR proficiency tools and EHR efficiency behaviors affect time spent in the EHR.
To address this gap, our study utilizes EHR-derived measures to assess whether the use of EHR proficiency tools and EHR efficiency behaviors were associated with reduced time interacting with the EHR. Findings may guide healthcare organization leaders in identifying key training areas to emphasize during onboarding of new physicians, post-onboarding support, refresher training, and EHR optimization efforts.
MATERIALS AND METHODS
Setting and sample
Study data focused on one academic health system in North Central Florida that offers multiple services, such as primary care, to patients throughout the state. This health system spans 2 metropolitan areas and utilizes Epic as its EHR provider (Epic Systems, Verona, WI).
The sample included all physicians (ie, attending physicians, residents/fellows), who practiced in ambulatory primary care during the study period, November 2019 to October 2020 inclusive. We defined primary care to include those in general internal medicine, general pediatrics, and family medicine. We focused on primary care due to the known substantial documentation burden,14,17 an established driver of time spent in the EHR.16,18,19,21,39–42 We excluded all physicians practicing in other settings and other clinician types (eg, nurse practitioners).
Data
Our data source was Epic Signal, an analytical platform developed by Epic that computes and stores EHR use measures for ambulatory clinicians.8,43 Health system clients can use these measures to assess the impact of interventions (eg, training) on the use of proficiency tools and time spent in the EHR. Since healthcare organizations have access to these measures and resulting dashboards for their internal use, we restricted all measures for this study to only those that healthcare organizations could access. The Institutional Review Boards at the University of Florida and the University of Alabama at Birmingham approved the study protocol.
Measures
The EHR automatically collected multiple data points for each clinician that uses the EHR system. These variables include the amount of time spent interacting with the EHR, amount of time on specific EHR activities, use of EHR tools (eg, macros), and patient workload (eg, average number of appointments per day). Most measures were non-negative continuous variables and a few were reported as dichotomous variables (eg, any use of chart search features). All EHR use measures were reported on a clinician-week level.
Outcome measures
We used 4 variables to measure time spent in the EHR. First, we assessed the overall time spent in the EHR, which is defined as the mean number of minutes spent per day. Second, we examined time spent outside scheduled hours, which is defined as the mean number of minutes spent in the EHR outside of scheduled appointments per day. This definition considers any EHR activity recorded more than 30 minutes before the first scheduled appointment or more than 30 minutes after the final appointment ended to be “outside of scheduled hours.” Although alternate options were considered to assess after-hours EHR use (eg, time outside of 7:00 AM to 7:00 PM), studies have raised questions about the heterogeneity and validity of time intervals used.43,44 Other measures (eg, time outside scheduled days) were not feasible given the academic setting (ie, many physicians in the study spent half of the day in clinic and the other half on educational, research, or administrative duties). Third, we reviewed time spent in the EHR writing notes per day, which is defined as the mean number of minutes spent writing notes. Lastly, we studied time spent on inbox management per day, which is defined as the mean number of minutes spent on the In Basket interface. These 4 outcome variables were selected due to their documented association with physician burnout.1
Independent variables
Our main independent variables were the use of EHR proficiency tools and EHR efficiency behaviors provided by the data source. We considered EHR proficiency tools to be any EHR tool implemented to improve a clinician’s productivity. These included the Chart Search feature, QuickActions (ie, macroed workflows), NoteSpeed buttons (ie, shortcuts to pulling in SmartPhrases), NoteWriter macros, QuickFilters (ie, applies pre-specified search criteria when reviewing information), SmartPhrases (ie, personal documentation templates), and bookmarked orders. We considered EHR efficiency behaviors to be measures describing how fast a clinician completed tasks. These included documentation length, signing visits on the same day, writing notes manually, volume of completed messages, time spent per message, and turnaround times for messages. We selected these variables as we hypothesized they may be associated with time spent in the EHR. Other proficiency-related variables, such as creating diagnosis and level of service speed buttons, were not analyzed because it was unclear how they might affect time spent in the EHR, had significant missing data, or were not calculated at the clinician-level.
Additional covariates
We included other variables known to influence EHR use patterns, such as patient load (number of appointments each day, proportion of the 7-day week with appointments, proportion of new patient visits),18,39,45,46 patient complexity (proxied by average patient age and average problem list length),47,48 having assistance on EHR tasks from support staff,49–51 and use of the EHR on mobile devices.52,53 New patient visits were defined as those with Current Procedural Terminology codes 99201 through 99205. At the study site, these billing codes are used for both patients who are new to the organization and those who have not been seen in over 3 years.
Analytic approach
We summarized the sample’s characteristics using median, interquartile range (IQR), and range for continuous variables and percentages for categorical variables. Since all outcomes of interest had a skewed distribution, rather than using traditional methods (eg, linear regression), we chose a multivariable quantile regression approach, allowing us to estimate the differential effect of model covariates across the various quantiles of the outcome distribution.54,55 For the analyses, we used the 10th, 25th, 50th, 75th, and 90th quantiles. We controlled for physician-level factors (in light of the limited demographic variables offered by the data source) and weekly variations in EHR use by including physician-level and time fixed effects. Since our study period overlapped with the coronavirus pandemic, we controlled for pandemic-related effects on EHR use (eg, switching to telemedicine) by including a dichotomous variable that represents whether a given week occurred during or after the state’s governor issued the executive order to cease elective services.56 We used complete case analysis to address missing data for variables of interest. Multicollinearity analysis was conducted to test for high correlations between predictors. A P-value of <.05 was interpreted as significant. All analyses were calculated using Stata SE 16.0 (Stata-Corp, LP, College Station, TX, USA), using the “xtqreg” commands.57
RESULTS
Sample characteristics
Our sample consisted of 441 primary care physicians. Over half of the physicians were female (54.2%), and the plurality of physicians practiced general internal medicine (38.8%). The median total time spent on various EHR activities is listed in Table 1 and the usage level of each of the proficiency tools studied is listed in Supplementary Table S1.
Table 1.
Sample characteristics (n = 441)
| Variables | ||
|---|---|---|
| EHR use measures (in minutes/day) | Median (IQR) | Range |
| Total time in EHR | 70.5 (106.5) | 0.6–417.2 |
| Total time in EHR outside scheduled hours | 40.9 (43.8) | 0.0–278.7 |
| Time spent in EHR documenting | 22.8 (46.2) | 0.2–143.5 |
| Time spent in In Basket | 5.9 (13.5) | 0.1–70.7 |
| Physician demographics, n (%) | ||
| Sex | ||
| Male | 196 (44.4%) | — |
| Female | 239 (54.2%) | — |
| Unknown | 6 (1.4%) | — |
| Primary care specialty | ||
| Family medicine | 139 (31.5%) | — |
| General internal medicine | 171 (38.8%) | — |
| General pediatrics | 131 (29.7%) | — |
| Patient load | ||
| Proportion of new patient visits | 0.0 (0.0) | 0–1 |
| Number of appointments in a day | 5.0 (7.5) | 1–30 |
| Number of problems in problem lists | 10.1 (8.7) | 0.9–34.9 |
| Patient age (in years) | 48.6 (47.9) | 2–76 |
| Proportion of week with appointments | 0.3 (0.4) | 0.1–1 |
EHR, electronic health records; IQR, interquartile range.
Total time interacting with the EHR
After controlling for other factors, increased availability of NoteSpeed buttons was associated with less time spent in the EHR per day at the 50th (β: −2.00, P < .01), 75th (β: −2.54, P < .01), and 90th quantiles (β: −3.02, P < .05). Conversely, as the number of QuickActions available increased, greater time was spent in the EHR per day at the 10th (β: 1.01, P < .01), 25th (β: .97, P < .001), 50th (β: .93, P < .001), 75th (β: .88, P < .001), and 90th quantiles (β: .84, P < .05). As the number of SmartPhrases created by the physician increased, greater time was spent in the EHR per day at the 10th (β: .15, P < .05), 25th (β: .15, P < .01), 50th (β: .16, P < .001), 75th (β: .16, P < .001), and 90th quantiles (β: .17, P < .01). Use of NoteWriter macros, QuickFilters, proportion of notes written manually, and In Basket turnaround time had no association with time spent interacting with the EHR. Further details are reported in Table 2.
Table 2.
Adjusted beta coefficient estimates of factors associated with total EHR use (in minutes/day) (n = 431)a,b
| Variables | 10th quantile | 25th quantile | 50th quantile | 75th quantile | 90th quantile |
|---|---|---|---|---|---|
| Patient load | |||||
| Proportion of new patient visits | −0.06 | 0.64 | 1.46 | 2.36 | 3.19 |
| Number of appointments in a day | 0.30 | 0.49** | 0.71*** | 0.95*** | 1.17*** |
| Proportion of week with scheduled appointments | 141.12 | 133.14*** | 123.79*** | 113.51*** | 104.12*** |
| Patient complexity | |||||
| Patient age | 0.11 | 0.13 | 0.15* | 0.16 | 0.18 |
| Number of problems on problem list | −0.11 | −0.08 | −0.05 | −0.02 | 0.01 |
| EHR proficiency and efficiency behaviors | |||||
| Chart search feature used | |||||
| No | Ref | Ref | Ref | Ref | Ref |
| Yes | 3.86 | 3.55* | 3.19** | 2.79* | 2.42 |
| Number of QuickActions | 1.01** | 0.97*** | 0.93*** | 0.88*** | 0.84* |
| Number of NoteSpeed buttons | −1.11 | −1.52 | −2.00** | −2.54** | −3.02* |
| Number of NoteWriter macros | 0.24 | 0.19 | 0.14 | 0.07 | 0.02 |
| Number of QuickFilters | 0.48 | 0.36 | 0.22 | 0.06 | −0.08 |
| Number of SmartPhrases created | 0.15* | 0.15** | 0.16*** | 0.16*** | 0.17** |
| Number of order bookmarks created | 0.01 | 0.04 | 0.07** | 0.11** | 0.14** |
| Proportion of orders used from bookmarks without additional changes | 11.70** | 10.58*** | 9.27*** | 7.82** | 6.50 |
| Documentation length per appointment | 0.002*** | 0.002*** | 0.002*** | 0.002*** | 0.002*** |
| Proportion of visits closed same day | 0.08 | 2.99 | 6.40*** | 10.14*** | 13.56*** |
| Proportion of note written manually | 6.04 | 7.22 | 8.60 | 10.12 | 11.51 |
| Number of completed In Basket messages | 0.76 | 0.86** | 0.98*** | 1.11*** | 1.23** |
| Seconds spent per message | 0.01 | 0.05 | 0.09*** | 0.13*** | 0.17*** |
| In Basket turnaround | −0.002 | 0.01 | 0.03 | 0.05 | 0.07 |
| Team-based care behaviors | |||||
| Proportion of note written by team members | −16.10* | −19.36*** | −23.78*** | −28.34*** | −32.50*** |
| Proportion of medications orders prepared by team members | −0.93 | −0.95 | −0.96 | −0.98 | −1.00 |
| Proportion of non-medications orders prepared by team members | 1.26 | 0.08 | −1.29 | −2.81* | −4.20** |
| Mobile device EHR behaviors | |||||
| Placed orders | |||||
| No | Ref | Ref | Ref | Ref | Ref |
| Yes | −3.83 | −3.95 | −4.10 | −4.26 | −4.41 |
| Wrote notes | |||||
| No | Ref | Ref | Ref | Ref | Ref |
| Yes | 0.89 | 0.87 | 0.84 | 0.81 | 0.78 |
| In Basket management | |||||
| No | Ref | Ref | Ref | Ref | Ref |
| Yes | 0.57 | 0.49 | 0.40 | 0.29 | 0.20 |
| COVID-related effects | |||||
| Onset of COVID | |||||
| Pre | Ref | Ref | Ref | Ref | Ref |
| Post | −6.32*** | −6.85*** | −7.48*** | −8.17*** | −8.80*** |
EHR, electronic health records.
Fixed effects on time and physician-level factors.
Multicollinearity analysis revealed high correlations between some predictors. Consequently, percent of orders placed from bookmarks and level of service entered using speed buttons were removed from the model.
P < .05, **P < .01, ***P < .001.
As the proportion of notes written by other team members increased, less time was spent in the EHR per day at the 10th (β: −16.10, P < .05), 25th (β: −19.36, P < .001), 50th (β: −23.78, P < .001), 75th (β: −28.34, P < .001), and 90th quantiles (β: −32.50, P < .001). As the proportion of non-medication orders (eg, referrals) prepared by team members for the physician to sign increased, less time was spent in the EHR per day at the 75th (β: −2.81, P < .05) and 90th quantiles (β: −4.20, P < .01) (Table 2).
Time in EHR outside scheduled appointment hours
After controlling for other factors, none of the studied proficiency behaviors were associated with less time spent in the EHR outside scheduled hours per day. However, as the number of QuickActions available increased, greater time was spent in the EHR outside scheduled hours per day at the 25th (β: .48, P < .01), 50th (β: .54, P < .001), 75th (β: .60, P < .01), and 90th quantiles (β: .66, P < .05). As the number of SmartPhrases created by the physician increased, greater time was spent in the EHR outside scheduled hours per day at the 25th (β: .08, P < .05) and 50th quantiles (β: .08, P < .01). Use of the Chart Search function, NoteSpeed buttons, NoteWriter macros, QuickFilters, order bookmarks, proportion of notes written manually, completed message volume, and In Basket turnaround had no association with time spent in the EHR outside scheduled clinic hours. Further details are reported in Table 3.
Table 3.
Adjusted beta coefficient estimates of factors associated with total after-hours EHR use (in minutes/day) (n = 390)a,b
| Variables | 10th quantile | 25th quantile | 50th quantile | 75th quantile | 90th quantile |
|---|---|---|---|---|---|
| Patient load | |||||
| Proportion of new patient visits | −11.18 | −10.81 | −10.34 | −9.77 | −9.23 |
| Number of appointments in a day | 0.03 | 0.04 | 0.06 | 0.08 | 0.10 |
| Proportion of week with scheduled appointments | 29.64*** | 20.45*** | 8.47** | −5.73 | −19.14** |
| Patient complexity | |||||
| Patient age | 0.07 | 0.05 | 0.01 | −0.03 | −0.08 |
| Number of problems on problem list | 0.05 | 0.11 | 0.19 | 0.29 | 0.38 |
| EHR proficiency and efficiency behaviors | |||||
| Chart search feature used | |||||
| No | Ref | Ref | Ref | Ref | Ref |
| Yes | 1.89 | 1.85 | 1.79 | 1.72 | 1.65 |
| Number of QuickActions | 0.44 | 0.48** | 0.54*** | 0.60** | 0.66* |
| Number of NoteSpeed buttons | −1.20 | −1.10 | −0.97 | −0.82 | −0.68 |
| Number of NoteWriter macros | 0.11 | 0.09 | 0.05 | 0.02 | −0.02 |
| Number of QuickFilters | 0.13 | 0.43 | 0.83 | 1.29 | 1.74 |
| Number of SmartPhrases created | 0.08 | 0.08* | 0.08** | 0.08 | 0.08 |
| Number of order bookmarks created | −0.02 | −0.02 | −0.02 | −0.02 | −0.02 |
| Proportion of orders used from bookmarks without additional changes | 5.97 | 4.87 | 3.44 | 1.74 | 0.13 |
| Documentation length per appointment | 0.001*** | 0.001*** | 0.001*** | 0.002*** | 0.002*** |
| Proportion of visits closed same day | 7.03* | 7.91*** | 9.06*** | 10.43*** | 11.72** |
| Proportion of note written manually | 1.21 | 3.91 | 7.42 | 11.58 | 15.51 |
| Number of completed In Basket messages | 0.01 | 0.03 | 0.06 | 0.09 | 0.12 |
| Seconds spent per message | 0.01 | 0.02 | 0.04* | 0.06* | 0.08 |
| In Basket turnaround | 0.04 | 0.03 | 0.01 | −0.003 | −0.02 |
| Team-based care behaviors | |||||
| Proportion of note written by team members | −4.35 | −3.57 | −2.55 | −1.34 | −0.21 |
| Proportion of medications orders prepared by team members | −1.03 | −0.62 | −0.08 | 0.55 | 1.15 |
| Proportion of non-medications orders prepared by team members | 3.81* | 3.36* | 2.77** | 2.07 | 1.41 |
| Mobile device EHR behaviors | |||||
| Placed orders | |||||
| No | Ref | Ref | Ref | Ref | Ref |
| Yes | 2.30 | −0.02 | −3.05 | −6.63 | −10.02 |
| Wrote notes | |||||
| No | Ref | Ref | Ref | Ref | Ref |
| Yes | 1.54 | 0.84 | −0.06 | −1.14 | −2.16 |
| In Basket management | |||||
| No | Ref | Ref | Ref | Ref | Ref |
| Yes | −2.12 | −2.35* | −2.65** | −3.01* | −3.34 |
| COVID-related effects | |||||
| Onset of COVID | |||||
| Pre | Ref | Ref | Ref | Ref | Ref |
| Post | −0.50 | −1.35 | −2.47*** | −3.79*** | −5.04** |
EHR, electronic health record.
Fixed effects on time and physician-level factors.
Multicollinearity analysis revealed high correlations between some predictors. Consequently, percent of orders placed from bookmarks and level of service entered using speed buttons were removed from the model.
P < .05, **P < .01, ***P < 0.001.
Time spent writing notes
After controlling for other factors, none of the studied proficiency behaviors were associated with less time spent writing notes per day. As the number of QuickActions available increased, greater time was spent writing notes per day (β: .40, P < .05). As the number of SmartPhrases created by the physician increased, greater time was spent writing notes per day at the 50th (β: .12, P < .05) and 75th quantiles (β: .14, P < .05). As the proportion of the note written manually increased, greater time was spent writing notes per day at the 25th (β: 13.98, P < .05), 50th (β: 16.91, P < .01), 75th (β: 2.31, P < .01), and 90th quantiles (β: 23.52, P < .05). Chart Search, NoteSpeed buttons, NoteWriter macros, QuickFilters, and order bookmarks had no association with time spent writing notes. Further details are reported in Table 4.
Table 4.
Adjusted beta coefficient estimates of factors associated with time spent documenting (in minutes/day, n = 432)a,b
| Variables | 10th quantile | 25th quantile | 50th quantile | 75th quantile | 90th quantile |
|---|---|---|---|---|---|
| Patient load | |||||
| Proportion of new patient visits | 1.40 | 1.49 | 1.60 | 1.73 | 1.85 |
| Number of appointments in a day | 0.14 | 0.26 | 0.41** | 0.58** | 0.75* |
| Proportion of week with scheduled appointments | 64.78*** | 60.07*** | 54.18*** | 47.34*** | 40.88*** |
| Patient complexity | |||||
| Patient age | 0.03 | 0.02 | 0.004 | −0.01 | −0.03 |
| Number of problems on problem list | −0.07 | −0.06 | −0.03 | −0.01 | 0.02 |
| EHR proficiency and efficiency behaviors | |||||
| Chart search feature used | |||||
| No | Ref | Ref | Ref | Ref | Ref |
| Yes | 0.13 | 0.33 | 0.59 | 0.88 | 1.16 |
| Number of QuickActions | 0.28 | 0.33 | 0.40* | 0.49 | 0.56 |
| Number of NoteSpeed buttons | −1.02 | −1.09 | −1.18 | −1.28 | −1.38 |
| Number of NoteWriter macros | 0.18 | 0.16 | 0.15 | 0.13 | 0.12 |
| Number of QuickFilters | 0.68 | 0.67 | 0.65 | 0.62 | 0.60 |
| Number of SmartPhrases created | 0.09 | 0.10 | 0.12* | 0.14* | 0.16 |
| Number of order bookmarks created | 0.01 | 0.02 | 0.04 | 0.06 | 0.07 |
| Proportion of orders used from bookmarks without additional changes | 6.51 | 5.41 | 4.04 | 2.46 | 0.96 |
| Documentation length per appointment | 0.001 | 0.001*** | 0.001*** | 0.002*** | 0.002** |
| Proportion of visits closed same day | 1.39 | 2.43 | 3.73 | 5.25* | 6.67 |
| Proportion of note written manually | 11.64 | 13.98* | 16.91** | 20.31** | 23.52* |
| Team-based care behaviors | |||||
| Proportion of note written by team members | −19.10** | −21.90*** | −25.40*** | −29.46*** | −33.30*** |
| Proportion of medications orders prepared by team members | 0.23 | 0.10 | −0.06 | −0.25 | −0.42 |
| Proportion of non-medications orders prepared by team members | 0.62 | 0.36 | 0.03 | −0.34 | −0.70 |
| Mobile device EHR behaviors | |||||
| Placed orders | |||||
| No | Ref | Ref | Ref | Ref | Ref |
| Yes | −0.76 | −0.98 | −1.27 | −1.60 | −0.42 |
| Wrote notes | |||||
| No | Ref | Ref | Ref | Ref | Ref |
| Yes | 0.37 | 0.40 | 0.44 | 0.49 | 0.54 |
| COVID-related effects | |||||
| Onset of COVID | |||||
| Pre | Ref | Ref | Ref | Ref | Ref |
| Post | −3.79* | −4.40*** | −5.17*** | −6.05*** | −6.89*** |
Fixed effects on time and physician-level factors.
Multicollinearity analysis revealed high correlations between some predictors. Consequently, percent of orders placed from bookmarks and level of service entered using speed buttons were removed from the model.
P < .05, **P < .01, ***P < .001.
As the proportion of the note written by other team members increased, less time was spent writing notes per day at the 10th (β: −19.10, P < .01), 25th (β: −21.90, P < .001), 50th (β: −25.40, P < .001), 75th (β: −29.46, P < .001), and 90th quantiles (β: −33.30, P < .001) (Table 4).
Time spent in In Basket
After controlling for other factors, no proficiency behavior was associated with time spent in the In Basket per day (Supplementary Table S2).
DISCUSSION
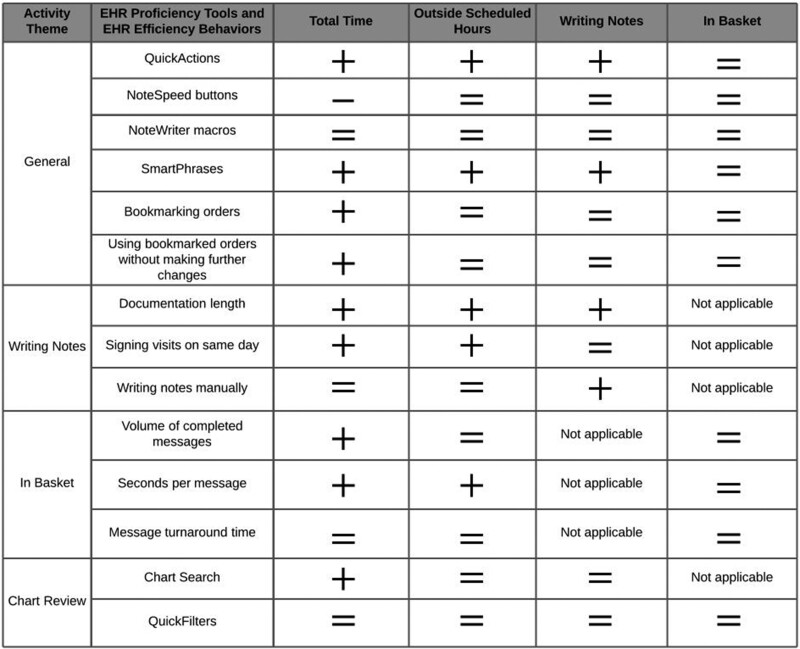
This cross-sectional study assessed the association between EHR proficiency tools and efficiency behaviors and time spent in the EHR among PCPs at one academic health system. To our knowledge, this is the first study to report on individual EHR proficiency behaviors, as opposed to vendor-derived EHR proficiency composite scores. Overall, we found a nuanced association between EHR proficiency measures and time spent in the EHR. Certain individual EHR proficiency behaviors were associated with time spent in the EHR (Figure 1).
Figure 1.
Summary of predictors’ association with time spent throughout the electronic health records system at the 50th quantile. Plus signs represent a positive association. Minus signs represent a negative association. Equal signs represent a null association.
Our study builds on a 2020 study that found EHR vendor-derived proficiency composite scores were not associated with time spent interacting with the EHR during after-hours.37 Although we found many EHR proficiency behaviors were not associated with time spent in the EHR outside scheduled hours, we found several that showed a surprising positive association (eg, QuickActions, SmartPhrases). Across 14 EHR proficiency and efficiency behaviors that we studied, only one (NoteSpeed buttons) was associated with reduced time spent interacting with the EHR. These findings may, in part, suggest issues in feature design or use. Furthermore, the findings could indicate that PCPs who spent more time in the EHR may be more likely to use these EHR features as well as create longer notes. Indeed, prior studies found the use of documentation tools (eg, structured templates) were associated with longer notes.58–61 Alternatively, the findings may suggest that such features may only be truly useful for limited types of clinical encounters. The present results also highlight the need for future qualitative research on the reasons for use or non-use of documentation support tools, as different interventions may be required based on the predominant reasons discovered (eg, lack of awareness vs. lack of utility). These studies could also identify types of clinical encounters when certain tools may be more useful. Examining between-physician and within-physician variability in use of the tools may also elucidate their association with other EHR-related behaviors.
We found that PCPs who had greater support from their care team in writing notes (eg, scribes) spent less total time interacting with the EHR per day and less time in documentation-specific activities per day. These findings suggest that PCPs may experience reductions in EHR-related burden and documentation burden by decentralizing documentation responsibilities. These findings were consistent with other studies’ findings.49–51 Healthcare organizations could implement various team-based documentation models by utilizing nursing staff,62,63 medical assistants,58,63,64 medical students,65–67 third-party scribing companies,64,66 or internally developed scribing programs to assist with this role.63,68 However, it is unclear which group will yield the most benefit. For instance, scribes have high turnover (1–2 years) but require at least 6 months of training to maximize productivity.64 Meanwhile, there are mixed perceptions regarding the delegation of clerical tasks to nursing staff.62,69 With the federal 2019 Patients Over Paperwork elimination of requirements to re-document trainees’ notes,70 researchers have found promising results from incorporating clinical documentation training and responsibilities into medical students’ clerkships.65,67 Although the care team can offload some documentation burden from physicians, healthcare organizations could amplify these benefits by enabling patients to assist in documentation tasks. For instance, offering patients structured pre-visit questionnaires through the patient portal may allow for the PCP to obtain history information that may integrate with the EHR’s existing tools to auto-populate in the note. In general pediatrics, the Bright Futures questionnaire is used to assess developmental milestones and to screen for at-risk behaviors, such as tobacco use.71 Healthcare organizations that convert these paper screening tools into electronic forms in the patient portals may enable PCPs to immediately import information directly into the note using the existing integration between patient portals and EHRs. However, additional research should assess the feasibility of implementing pre-visit questionnaires and its impact on physicians’ documentation burden.
Another key finding was that PCPs who manually wrote a greater proportion of their notes spent more time in the EHR writing notes per day. Consequently, interventions targeting this specific efficiency behavior may reduce documentation burden. In our sample, use of some documentation-related proficiency tools (eg, use of macros) were recorded for less than half of studied physicians. Together, these findings suggest targeted approaches for training initiatives to improve EHR proficiency. Indeed, researchers have highlighted the need for both initial and ongoing training on EHR workflows and proficiency tools, especially as EHR interfaces are continually updated.35,72–74 Clinicians may benefit from practicing new EHR skills in a training environment as scenario-based training and simulations have been shown to improve educational outcomes with EHR use.75–77 Furthermore, if EHR features are impacted by EHR updates, healthcare organizations could consider re-training or dissemination of impacts to features (eg, icon moved to new location) to sustain feature use. Lastly, ease of set-up and use may influence physicians’ adoption of features. For instance, voice dictation may require considerable time for set-up.78 With physicians reporting limited time for documentation,79,80 EHR features that are perceived as cumbersome to set up may lead to lower adoption rates. Future research assessing the use of EHR features should measure perceived ease of set-up and use.
Furthermore, our In Basket model revealed no association across many predictors, suggesting the proficiency tools, as designed or implemented, may not be as helpful during inbox management. This finding may also suggest that interventions outside of EHR proficiency tools may be more beneficial. Notably, the data source contained no variables to capture the use of team-based models in the In Basket (eg, shared inbox among team members, active triage by support staff). Further research should assess for other unmeasured proficiency behaviors, such as message batching,81 and examine the impact of team-based models on time spent managing messages. Other informatics-based interventions may include the use of machine learning to flag certain messages for review based on analysis of message content.82
Notable limitations are as follows: first, this was a single-center study, which may limit generalizability to nonacademic organizations and those using other EHR products. Physicians in our sample had less clinical load due to concurrent teaching, research, or administrative responsibilities, which may influence their extent of interactions with the EHR. Second, we were precluded from assessing time spent in more granular units due to how EHR measures were reported by the vendor. Third, we were unable to control for practice-level differences, as some physicians practiced in multiple clinics. Fourth, we were unable to obtain information on how many scheduled appointments were canceled or whether the problem list length is calculated before or after the appointment. Future studies should use additional datasets to explore how these nuances may affect time spent in the EHR. Other variables that may affect EHR use patterns, but were not reported by our data source, include medication list length and whether visits were for wellness checks, follow-up of chronic care, or for a sick visit. Additional research should examine EHR proficiency tool use and time spent in the EHR for specific visit types. Lastly, the use of EHR logs and derived measures may underestimate EHR and documentation burden among clinicians because the measures may not capture care activities done outside the EHR (eg, patient emails to institutional email accounts).15
CONCLUSION
Among PCPs, mixed associations were found between certain EHR proficiency behaviors and the relative amount of time spent interacting with the EHR, suggesting targets for future training. Additionally, support from other members of the care team was an important determinant of PCPs’ time spent in the EHR. Future research is needed to elucidate reasons for non-use of specific documentation support tools and test team-based models for their impact on EHR-related burden.
FUNDING
We acknowledge the University of Florida Integrated Data Repository (IDR) and the UF Health Office of the Chief Data Officer for providing the analytic data set for this project. Additionally, the research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under University of Florida Clinical and Translational Science Awards UL1TR000064 and UL1TR001427.
The content of this publication is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
AUTHOR CONTRIBUTIONS
This work represents the original research of the authors. This work has not been previously published. OTN, KT, NCA, LJM, and SSF conceptualized the study. OTN analyzed the data. All authors interpreted the data. OTN drafted the manuscript. All authors provided critical revisions to the manuscript and approved the submission.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
We thank Joel Traylor and Cara McDonnell for assisting with familiarizing us with the data source and pulling the data for this study’s analysis. We also would like to thank the peer reviewers for strengthening this manuscript.
CONFLICT OF INTEREST STATEMENT
None declared.
DATA AVAILABILITY
The data underlying this article will be shared on reasonable request to the corresponding author.
Contributor Information
Oliver T Nguyen, Department of Health Services Administration, University of Alabama at Birmingham, Birmingham, Alabama, USA; Department of Community Health and Family Medicine, University of Florida, Gainesville, Florida, USA.
Kea Turner, Department of Health Outcomes and Behavior, Moffitt Cancer Center, Tampa, Florida, USA; Department of Oncological Sciences, University of South Florida, Tampa, Florida, USA.
Nate C Apathy, Leonard Davis Institute of Health Economics, University of Pennsylvania, Philadelphia, Pennsylvania, USA.
Tanja Magoc, Clinical and Translational Science Institute, University of Florida, Gainesville, Florida, USA.
Karim Hanna, Department of Family Medicine, Morsani College of Medicine, University of South Florida, Tampa, Florida, USA.
Lisa J Merlo, Department of Psychiatry, University of Florida, Gainesville, Florida, USA.
Christopher A Harle, Clinical and Translational Science Institute, University of Florida, Gainesville, Florida, USA; Department of Health Outcomes and Biomedical Informatics, University of Florida, Gainesville, Florida, USA.
Lindsay A Thompson, Department of Health Outcomes and Biomedical Informatics, University of Florida, Gainesville, Florida, USA; Department of Pediatrics, University of Florida, Gainesville, Florida, USA.
Eta S Berner, Department of Health Services Administration, University of Alabama at Birmingham, Birmingham, Alabama, USA.
Sue S Feldman, Department of Health Services Administration, University of Alabama at Birmingham, Birmingham, Alabama, USA.
REFERENCES
- 1. Nguyen OT, Jenkins NJ, Khanna N, et al. A systematic review of contributing factors of and solutions to electronic health record-related impacts on physician well-being. J Am Med Inform Assoc 2021; 28 (5): 974–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Moy AJ, Schwartz JM, Chen R, et al. Measurement of clinical documentation burden among physicians and nurses using electronic health records: a scoping review. J Am Med Inform Assoc 2021; 28 (5): 998–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Thomas Craig KJ, Willis VC, Gruen D, et al. The burden of the digital environment: a systematic review on organization-directed workplace interventions to mitigate physician burnout. J Am Med Inform Assoc 2021; 28 (5): 985–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yan Q, Jiang Z, Harbin Z, et al. Exploring the relationship between electronic health records and provider burnout: a systematic review. J Am Med Inform Assoc 2021; 28 (5): 1009–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wu DTY, Xu C, Kim A, et al. A scoping review of health information technology in clinician burnout. Appl Clin Inform 2021; 12 (3): 597–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Erickson SM, Rockwern B, Koltov M, et al. ; Medical Practice and Quality Committee of the American College of Physicians. Putting patients first by reducing administrative tasks in health care: a position paper of the American College of Physicians. Ann Intern Med 2017; 166 (9): 659–61. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Medicare & Medicaid Services. Patients Over Paperwork. https://www.cms.gov/About-CMS/story-page/patients-over-paperwork Accessed September 10, 2020.
- 8. Cohen GR, Boi J, Johnson C, et al. Measuring time clinicians spend using EHRs in the inpatient setting: a national, mixed-methods study. J Am Med Inform Assoc 2021; 28 (8): 1676–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Office of the National Coordinator for Health Information Technology. Strategy on Reducing Regulatory and Administrative Burden Relating to the Use of Health IT and EHRs. https://www.healthit.gov/sites/default/files/page/2020-02/BurdenReport_0.pdf Accessed January 23, 2021.
- 10. Chen L, Guo U, Illipparambil LC, et al. Racing against the clock: internal medicine residents’ time spent on electronic health records. J Grad Med Educ 2016; 8 (1): 39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Office of the National Coordinator for Health Information Technology. 2020-2025 Federal Health IT Strategic Plan. https://www.healthit.gov/sites/default/files/page/2020-10/Federal%20Health%20IT%20Strategic%20Plan_2020_2025.pdf Accessed September 27, 2020.
- 12. Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J Am Med Inform Assoc 2014; 21 (e1): e100–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc 2016; 91 (7): 836–48. [DOI] [PubMed] [Google Scholar]
- 14. Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med 2017; 15 (5): 419–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Goldstein IH, Hribar MR, Reznick LG, et al. Analysis of total time requirements of electronic health record use by ophthalmologists using secondary EHR data. AMIA Annu Symp Proc 2018; 2018: 490–7. [PMC free article] [PubMed] [Google Scholar]
- 16. Overhage JM, McCallie D Jr. Physician time spent using the electronic health record during outpatient encounters: a descriptive study. Ann Intern Med 2020; 172 (3): 169–74. [DOI] [PubMed] [Google Scholar]
- 17. Rotenstein LS, Holmgren AJ, Downing NL, et al. Differences in total and after-hours electronic health record time across ambulatory specialties. JAMA Intern Med 2021; 181 (6): 863–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tran B, Lenhart A, Ross R, et al. Burnout and EHR use among academic primary care physicians with varied clinical workloads. AMIA Jt Summits Transl Sci Proc 2019; 2019: 136–44. [PMC free article] [PubMed] [Google Scholar]
- 19. Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med 2016; 165 (11): 753–60. [DOI] [PubMed] [Google Scholar]
- 20. Kannampallil TG, Denton CA, Shapiro JS, et al. Efficiency of emergency physicians: insights from an observational study using EHR log files. Appl Clin Inform 2018; 09 (01): 99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Melnick ER, Ong SY, Fong A, et al. Characterizing physician EHR use with vendor derived data: a feasibility study and cross-sectional analysis. J Am Med Inform Assoc 2021; 28 (7): 1383–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gupta K, Murray SG, Sarkar U, et al. Differences in ambulatory EHR use patterns for male vs. female physicians. https://catalyst.nejm.org/ambulatory-ehr-patterns-physician-gender/ Accessed November 26, 2019.
- 23. Attipoe S, Huang Y, Schweikhart S, et al. Factors associated with electronic health record usage among primary care physicians after hours: retrospective cohort study. JMIR Hum Factors 2019; 6 (3): e13779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rotenstein LS, Jay Holmgren A, Lance Downing N, et al. Differences in clinician electronic health record use across adult and pediatric primary care specialties. JAMA Netw Open 2021; 4 (7): e2116375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kokkonen EWJ, Davis SA, Lin H-C, et al. Use of electronic medical records differs by specialty and office settings. J Am Med Inform Assoc 2013; 20 (e1): e33–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hilliard RW, Haskell J, Gardner RL. Are specific elements of electronic health record use associated with clinician burnout more than others? J Am Med Inform Assoc 2020; 27 (9): 1401–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Beasley JW, Hankey TH, Erickson R, et al. How many problems do family physicians manage at each encounter? A WReN study. Ann Fam Med 2004; 2 (5): 405–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Abbo ED, Zhang Q, Zelder M, et al. The increasing number of clinical items addressed during the time of adult primary care visits. J Gen Intern Med 2008; 23 (12): 2058–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Okunogbe A, Meredith LS, Chang ET, et al. Care coordination and provider stress in primary care management of high-risk patients. J Gen Intern Med 2018; 33 (1): 65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Friedman A, Howard J, Shaw EK, et al. Facilitators and barriers to care coordination in patient-centered medical homes (PCMHs) from coordinators’ perspectives. J Am Board Fam Med 2016; 29 (1): 90–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hsiao C-J, King J, Hing E, et al. The role of health information technology in care coordination in the United States. Med Care 2015; 53 (2): 184–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Longhurst CA, Davis T, Maneker A, et al. ; Arch Collaborative. Local investment in training drives electronic health record user satisfaction. Appl Clin Inform 2019; 10 (2): 331–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lourie EM, Utidjian LH, Ricci MF, et al. Reducing electronic health record-related burnout in providers through a personalized efficiency improvement program. J Am Med Inform Assoc 2021; 28 (5): 931–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Office of Inspector General. Training deficiencies with VA’s new electronic health record system at the Mann-Grandstaff VA Medical Center in Spokane, Washington. 2021. https://www.va.gov/oig/pubs/VAOIG-20-01930-183.pdf Accessed July 13, 2021.
- 35. Stroup K, Sanders B, Bernstein B, et al. A new EHR training curriculum and assessment for pediatric residents. Appl Clin Inform 2017; 8 (4): 994–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Stevens LA, DiAngi YT, Schremp JD, et al. Designing an individualized EHR learning plan for providers. Appl Clin Inform 2017; 8 (3): 924–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Adler-Milstein J, Zhao W, Willard-Grace R, et al. Electronic health records and burnout: Time spent on the electronic health record after hours and message volume associated with exhaustion but not with cynicism among primary care clinicians. J Am Med Inform Assoc 2020; 27 (4): 531–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hron JD, Lourie E. Have you got the time? Challenges using vendor electronic health record metrics of provider efficiency. J Am Med Inform Assoc 2020; 27 (4): 644–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Murphy DR, Meyer AND, Russo E, et al. The burden of inbox notifications in commercial electronic health records. JAMA Intern Med 2016; 176 (4): 559–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Melnick ER, Dyrbye LN, Sinsky CA, et al. The association between perceived electronic health record usability and professional burnout among US physicians. Mayo Clin Proc 2019; 95 (3): 476–87. [DOI] [PubMed] [Google Scholar]
- 41. Butler RJ, Johnson WG. Rating the digital help: electronic medical records, software providers, and physicians. Int J Health Econ Manag 2016; 16 (3): 269–83. [DOI] [PubMed] [Google Scholar]
- 42. Melnick ER, Sinsky CA, Dyrbye LN, et al. Association of perceived electronic health record usability with patient interactions and work-life integration among US physicians. JAMA Netw Open 2020; 3 (6): e207374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Baxter SL, Apathy NC, Cross DA, et al. Measures of electronic health record use in outpatient settings across vendors. J Am Med Inform Assoc 2021; 28 (5): 955–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Sinsky CA, Rule A, Cohen G, et al. Metrics for assessing physician activity using electronic health record log data. J Am Med Inform Assoc 2020; 27 (4): 639–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Tai-Seale M, Olson CW, Li J, et al. Electronic health record logs indicate that physicians split time evenly between seeing patients and desktop medicine health. Health Aff (Millwood) 2017; 36 (4): 655–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Saag HS, Shah K, Jones SA, et al. Pajama time: working after work in the electronic health record. J Gen Intern Med 2019; 34 (9): 1695–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Krauss JC, Boonstra PS, Vantsevich AV, et al. Is the problem list in the eye of the beholder? An exploration of consistency across physicians. J Am Med Inform Assoc 2016; 23 (5): 859–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Grant RW, Ashburner JM, Hong CS, et al. Defining patient complexity from the primary care physician’s perspective: a cohort study. Ann Intern Med 2011; 155 (12): 797–804. [DOI] [PubMed] [Google Scholar]
- 49. Reuben DB, Knudsen J, Senelick W, et al. The effect of a physician partner program on physician efficiency and patient satisfaction. JAMA Intern Med 2014; 174 (7): 1190–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Gidwani R, Nguyen C, Kofoed A, et al. Impact of scribes on physician satisfaction, patient satisfaction, and charting efficiency: a randomized controlled trial. Ann Fam Med 2017; 15 (5): 427–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Contratto E, Romp K, Estrada CA, et al. Physician order entry clerical support improves physician satisfaction and productivity. South Med J 2017; 110 (5): 363–8. [DOI] [PubMed] [Google Scholar]
- 52. Lee Y, Park YR, Kim J, et al. Usage pattern differences and similarities of mobile electronic medical records among health care providers. JMIR Mhealth Uhealth 2017; 5 (12): e178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Soh JY, Jung S-H, Cha WC, et al. Variability in doctors’ usage paths of mobile electronic health records across specialties: comprehensive analysis of log data. JMIR Mhealth Uhealth 2019; 7 (1): e12041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Buchinsky M. Recent advances in quantile regression models: a practical guideline for empirical research. J Hum Resour 1998; 33 (1): 88–126. [Google Scholar]
- 55. Machado JAF, Santos Silva JMC. Quantiles via moments. J Econom 2019; 213 (1): 145–73. [Google Scholar]
- 56.The State of Florida. Executive Order Number 20-72 (Emergency Management - COVID-19 - Non-essential Elective Medical Procedures). 2020. https://www.flgov.com/wp-content/uploads/orders/2020/EO_20-72.pdf Accessed July 21, 2021.
- 57.Santos Silver JMC. Quantile Regression: Basics and Recent Advances. 2019.https://www.stata.com/meeting/uk19/slides/uk19_santos.pdf Accessed July 23, 2021.
- 58. Misra-Hebert AD, Amah L, Rabovsky A, et al. Medical scribes: how do their notes stack up? J Fam Pract 2016; 65 (3): 155–9. [PubMed] [Google Scholar]
- 59. Neri PM, Volk LA, Samaha S, et al. Relationship between documentation method and quality of chronic disease visit notes. Appl Clin Inform 2014; 5 (2): 480–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Blackley SV, Schubert VD, Goss FR, et al. Physician use of speech recognition versus typing in clinical documentation: a controlled observational study. Int J Med Inform 2020; 141: 104178. [DOI] [PubMed] [Google Scholar]
- 61. Colicchio TK, Dissanayake PI, Cimino JJ. Physicians’ perceptions about narrative note sections format and content: a multi-specialty survey. Int J Med Inform 2021; 151: 104475. [DOI] [PubMed] [Google Scholar]
- 62. Funk KA, Davis M. Enhancing the role of the nurse in primary care: the RN ‘Co-Visit’ model. J Gen Intern Med 2015; 30 (12): 1871–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Corby S, Ash JS, Mohan V, et al. A qualitative study of provider burnout: do medical scribes hinder or help? JAMIA Open 2021; 4 (3): ooab047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Ash JS, Corby S, Mohan V, et al. Safe use of the EHR by medical scribes: a qualitative study. J Am Med Inform Assoc 2021; 28 (2): 294–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Gagliardi JP, Bonanno B, McPeek Hinz ER, et al. Implementation of changes to medical student documentation at Duke University Health System: balancing education with service. Acad Med 2021; 96 (6): 900–5. [DOI] [PubMed] [Google Scholar]
- 66. Shultz CG, Holmstrom HL. The use of medical scribes in health care settings: a systematic review and future directions. J Am Board Fam Med 2015; 28 (3): 371–81. [DOI] [PubMed] [Google Scholar]
- 67. Bachrach L, Fadadu RP, Sharp M, et al. Pediatric workplace learning opportunities for medical students: is scribing a win-win? Acad Pediatr 2021; 21 (3): 580–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Lin S, Duong A, Nguyen C, et al. Five years’ experience with a medical scribe fellowship: shaping future health professions students while addressing provider burnout. Acad Med 2021; 96 (5): 671–9. [DOI] [PubMed] [Google Scholar]
- 69. Gesner E, Gazarian P, Dykes P. The burden and burnout in documenting patient care: an integrative literature review. Stud Health Technol Inform 2019; 264: 1194–8. [DOI] [PubMed] [Google Scholar]
- 70.Centers for Medicare & Medicaid Services. Final Policy, Payment, and Quality Provisions Changes to the Medicare Physician Fee Schedule for Calendar Year 2019. https://www.cms.gov/newsroom/fact-sheets/final-policy-payment-and-quality-provisions-changes-medicare-physician-fee-schedule-calendar-year Accessed September 9, 2021.
- 71.American Academy of Pediatrics. Bright Futures Tool and Resource Kit. https://brightfutures.aap.org/materials-and-tools/tool-and-resource-kit/Pages/default.aspx Accessed July 26, 2021.
- 72. Laramee AS, Bosek M, Shaner-McRae H, et al. A comparison of nurse attitudes before implementation and 6 and 18 months after implementation of an electronic health record. Comput Inform Nurs 2012; 30 (10): 521–30. [DOI] [PubMed] [Google Scholar]
- 73. Kaelber D, Greco P, Cebul RD. Evaluation of a commercial electronic medical record (EMR) by primary care physicians 5 years after implementation. AMIA Annu Symp Proc 2005; 1002. [PMC free article] [PubMed] [Google Scholar]
- 74. Barr JA. Invest in EHR Training to Increase Efficiency, Improve Physician Well-Being. https://www.aappublications.org/news/2020/12/01/hit120120?utm_source=TrendMD&utm_medium=TrendMD&utm_campaign=AAPNews_TrendMD_0 Accessed March 17, 2021.
- 75. Reis ZSN, Maia TA, Marcolino MS, et al. Is there evidence of cost benefits of electronic medical records, standards, or interoperability in hospital information systems? Overview of systematic reviews. JMIR Med Inform 2017; 5 (3): e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Vuk J, Anders ME, Mercado CC, et al. Impact of simulation training on self-efficacy of outpatient health care providers to use electronic health records. Int J Med Inform 2015; 84 (6): 423–9. [DOI] [PubMed] [Google Scholar]
- 77. March CA, Scholl G, Dversdal RK, et al. Use of electronic health record simulation to understand the accuracy of intern progress notes. J Grad Med Educ 2016; 8 (2): 237–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Johnson M, Lapkin S, Long V, et al. A systematic review of speech recognition technology in health care. BMC Med Inform Decis Mak 2014; 14: 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Gardner RL, Cooper E, Haskell J, et al. Physician stress and burnout: the impact of health information technology. J Am Med Inform Assoc 2019; 26 (2): 106–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Olson K, Sinsky C, Rinne ST, et al. Cross-sectional survey of workplace stressors associated with physician burnout measured by the Mini-Z and the Maslach Burnout Inventory. Stress Health 2019; 35 (2): 157–75. [DOI] [PubMed] [Google Scholar]
- 81. Akbar F, Mark G, Prausnitz S, et al. Physician stress during electronic health record inbox work: in situ measurement with wearable sensors. JMIR Med Inform 2021; 9 (4): e24014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Lowres N, Duckworth A, Redfern J, et al. Use of a machine learning program to correctly triage incoming text messaging replies from a cardiovascular text-based secondary prevention program: feasibility study. JMIR Mhealth Uhealth 2020; 8 (6): e19200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.