Abstract
Objective
To determine whether hospital adoption of a new electronic health record (EHR) developer increases patient sharing with hospitals using the same developer.
Materials and Methods
We extracted data on patients shared with other hospitals for 3076 US nonfederal acute care hospitals from the 2011 to 2016 Centers for Medicare & Medicaid Services Physician Shared Patient Patterns database. We calculated the ratio of patients shared with hospitals outside of the focal hospital’s network that use the same EHR developer as the focal hospital, and estimated difference-in-differences models to compare same-developer patient sharing among hospitals that switched to a new developer with those that did not switch developer.
Results
Switching to a new EHR developer increased the ratio of patients shared with other hospitals having the same EHR developer by 4.1–19.3%, depending on model specification. The magnitude of this effect varied by EHR developer and was increasing in developer market share.
Discussion
Consolidation in the EHR industry has led to higher patient sharing among hospitals with the same EHR developer. Contributing factors could include the growth of developer-based health information exchanges, customizable referral management systems, and provider preferences for easy and reliable data exchange. However, hospital transfers that are significantly influenced by EHR developer could lead to poor patient-provider matches.
Conclusion
Hospitals’ choice of EHR developer impacts the flow of patients across hospitals, which could have both desirable and undesirable effects on patient care. Future research should investigate whether health outcomes decline with greater same-developer patient sharing.
Keywords: health information exchange, patient sharing, electronic health record, information blocking
INTRODUCTION
With the number of state and community health information exchange (HIE) decreasing, EHR developer-based networks have become an increasingly important means of HIE.1,2 Several EHR developers have invested heavily in systems that facilitate within-developer HIE. Epic, for example, is an EHR developer with its own HIE platform named the Care Everywhere Network that allows providers to exchange information with other Epic users, subject to conditions governing data accessibility. Similarly, other major developers (Cerner, McKesson, and Athena) have their own HIE mediated exchanges that are less comprehensive than the Care Everywhere Network.3 However, the additional costs imposed by developers on providers seeking to exchange information outside of their developer’s network indicates that developer-based platforms, although valuable, might create disincentives to cross-developer exchange.4,5 In particular, over 55% of health exchange organizations reported that EHR developers engaged in information blocking.6 In response, the 21st Century Cures Act contains provisions prohibiting information blocking practices that took effect on April 5, 2021.7
The dominance of developer-based HIE platforms means that healthcare organizations might be strategic about choosing an EHR developer, as this choice could affect their quality of care and patient volume. For example, Everson and Adler-Milstein8 find less HIE in markets with low developer dominance than those with high developer dominance due to higher costs of connecting to multiple EHR developers within the area. Similarly, Castillo et al9 find the likelihood that hospitals exchange clinical care summaries increases with the percentage of hospitals in a region using the same EHR. Lin estimates that the adoption of a dominant vendor increases hospital profits by 9.2% over the adoption of a nondominant vendor.10
This study makes an important contribution to the literature as the first to examine the impact EHR developers have on patient sharing between hospitals. Prior research suggests that choice of EHR developer could be important in these situations, as lack of communication between hospitals transferring patients can lead to diagnostic errors and increase inpatient mortality, both of which are mitigated by HIE participation.11 We determine whether the use of an EHR developer is associated with an increase in patients shared across hospitals that have adopted the same developer, and whether this association varies by developer market share. To do this, we use a difference-in-differences (DD) approach to compare the change in the proportion of patients shared with other hospitals with the same EHR developer between acute care hospitals that recently switched to a new EHR developer, and hospitals that did not switch their developer. Our results have implications for policies that relate to patient sharing across providers, and information blocking practices that prohibit EHR developers and healthcare providers from limiting the exchange of electronic health information.7
MATERIALS AND METHODS
Data sources and sample
From the Centers for Medicare & Medicaid Services’ (CMS) Physician Shared Patient Patterns data, we obtained the number of patients shared among nonfederal acute care hospitals in the United States within each month from 2011 to 2016. These data include hospital identifiers, which allowed us to link to other data sources. Using the American Hospital Association (AHA) Annual Survey, we merged hospital characteristics such as healthcare network name, network ownership, and hospital referral region (HRR). To identify hospitals’ EHR developer, we used data from the CMS Promoting Interoperability (PI) programs in combination with data from the Office of the National Coordinator for Health Information Technology’s Certified Health IT Product List (CHPL; https://chpl.healthit.gov/) and the HIMSS Analytics Database.
Because our analysis focuses on patient sharing, we subset to hospitals included in the Physician Shared Patient Patterns database (97% of all nonfederal acute care hospitals). Due to concerns over their comparability to hospitals that switched EHR developer, we also excluded hospitals that did not share patients outside their healthcare network (27% of the sample) and hospitals that had not continuously adopted an EHR (23%; overlapping with the first category). The EHR adoption rate increased significantly over our study period; in 2011, 20% of hospitals did not have an EHR (by the definition provided below), but by 2016 all hospitals adopted an EHR. As a result, later years of our sample contain more observations. Overall, there are 3076 unique hospitals in our data and 13279 hospital-year observations.
Dependent variable
The dependent variable in our empirical models is “same-developer patient sharing,” defined as the ratio of patients the focal hospital has in common in a given month with hospitals outside the focal hospital’s healthcare network who use the same EHR developer as the focal hospital. In this case, the healthcare network includes the set of providers owned by or affiliated with the focal hospital’s healthcare system. The denominator of this ratio is the overall number of patients shared with hospitals outside the focal hospital’s healthcare network. For hospitals that changed EHR developers during the sample period, we used the newly adopted EHR developer as the “same developer” when computing the numerator of the patient sharing ratio.
Identification of EHR developer
To determine a hospital’s EHR, we used PI data from CMS that provides the CHPL identification number of the EHR product(s) used by the hospital for program attestation. We linked this number with CHPL data to identify the products and developers that constitute a hospital’s base EHR (as required by CMS to attest to PI). We used the HIMSS Analytics Database to identify EHR developers for hospitals that did not participate in the CMS Meaningful Use Program during the sample period. In this case, we designated adopted EHRs as those that were “live and operational” and contained at least one of the following applications: clinical data repository, clinical decision support system, or computerized practitioner order entry system.12
Analytical approach
Our base model specification is the following generalized DD model:
where is same-developer patient sharing for hospital in year , is an indicator variable for switching to a new EHR developer in the given year and is the new or existing EHR developer’s market share in the HRR, calculated as the percentage of hospitals in the HRR using the given developer in the specified year. is an indicator variable for a change to the hospital’s network affiliation or the acquisition of the hospital’s network. In addition to the base specification with hospital indicator variables (fixed effects),, and year fixed effects, , we also estimated models that include HHR-specific linear time trends, specified as , where is a fixed effect for HRR and is a linear time trend. Finally, we estimated a set of models that include the following interaction term between the indicator for switching EHR developer and the developer’s market share: . In all models, the standard errors are cluster-corrected at the hospital level and the regressions are weighted by hospital bed size to account for the importance of large hospitals in determining referral patterns.
We conducted several robustness checks to ensure that the model estimates do not represent spurious correlations. Identification of the treatment effect of switching EHR developer in the generalized DD model, , is achieved by comparing changes in same-developer patient sharing among hospitals who switched developers to changes in same-developer patient sharing among hospitals that did not switch developers over at least a 2-year period. The latter group includes hospitals that never switched developers, those that have not yet switched developers, and those that had already switched developers. Prior research shows that estimates from the generalized DD model can be biased if the treatment effect estimates are heterogeneous across time when comparing treated and control hospitals belonging to these different groups.13–15 We therefore tested for heterogeneous treatment effects and estimated the doubly robust model of Callaway and Sant’Anna (C&S)15 to correct for any potential bias (Supplementary Appendix Section SA1). We also tested another key assumption of the DD model by estimating an event study model to determine whether hospitals that switched EHR developers and those that did not had similar trends in same-developer patient sharing prior to the developer change.
One complication that arises in our data when identifying a hospital’s newly adopted EHR is that 7% of hospitals switched EHR developers more than once during the sample period. More than half of these hospitals reported switching to the prior developer, in which case we classified the hospitals as not having switched developers. For the remaining hospitals that genuinely changed developer more than once during this time period, we used the most recent EHR developer as the newly adopted developer. We estimated models using a sample that excludes hospitals that switched developers multiple times to determine whether these hospitals have an out-sized influence on our estimates.
Although we control in our models for changes in healthcare network ownership, there could be cases where a change in the hospital’s network affiliation and the EHR developer occurred simultaneously. Past research finds agglomeration of EHR developers when hospital markets become more concentrated, suggesting that the failure to separately control for network mergers could cause an upward bias on the effect of EHR developer choice on same-developer patient sharing.16 In order to test whether our models adequately control for changes in network affiliation, we estimated models using the subset of hospitals that did not change their network affiliation or remained unaffiliated.
A final potential concern is that our modeling strategy may not accurately isolate the EHR developer preferences of the focal hospital from other hospitals. This could occur if the EHR developer preferences of outside hospitals influence same-developer patient sharing by the focal hospital. For example, an outside hospital that initially had a different EHR developer than the focal hospital might switch to the same EHR developer as the focal hospital, resulting in an increase in same-developer patient sharing without any change in the focal hospital’s behavior. Likewise, an outside hospital with the same EHR developer as the focal hospital might switch to a different EHR developer. If the focal hospital were to then transfer its patients to a different outside hospital with the same EHR developer as the focal hospital, same-developer patient sharing would not change despite the action taken by the focal hospital based a preference for the same EHR developer. In order to determine whether the aforementioned scenarios lead to biased estimates in the DD model, we created an alternative outcome variable that is defined as the difference in same-developer patient sharing between the current year and past year based on the set of hospitals that used the same developer as the focal hospital in the current year (Supplementary Appendix Section SA2).
RESULTS
Trends in same-developer patient sharing and hospital characteristics
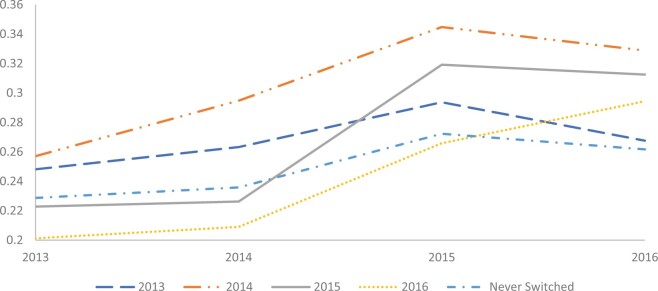
Among hospitals that never switched EHR developers, there is an upward trend in same-developer patient sharing from 2013 to 2015 and a slight decline from 2015 to 2016 (Figure 1). Hospitals that switched EHR developers at some point in the sample period generally exhibit this same trend, but patient sharing increases above trend in the year they switched developers. In the case of hospitals switching developers in 2014, the increase above trend is very slight.
Figure 1.
Proportion of patients shared across hospital systems with the same electronic health record (EHR) developer by cohort of hospitals that switched EHR developer in a given year. Sources: Centers for Medicare & Medicaid Services (CMS) referral data, CMS EHR Meaningful Use Program Data, and the Office of the National Coordinator for Health Information Technology’s Certified Health IT Product List.
We report the mean values of select hospital characteristics from the AHA Annual Survey and Information Technology Supplement for hospitals that did (N = 1021) and did not (N = 2055) switch EHR developers in Table 1. We indicate in column 2 of Table 1 whether the difference in the mean values of the given characteristic across the 2 groups of hospitals is statistically significant using a 2-sample t test. Although there are no statistically significant differences in hospital size by EHR switching status, hospitals that switched developers were less likely to be government-owned or teaching hospitals, and more likely to be nonprofit or cardiac intensive care hospitals. Hospitals that switched developers were also more likely to reside in the Northeast and less likely to be located in the Midwest and South, and they were more likely to be owned by healthcare systems. In the interoperability domain, hospitals that did not switch EHR developers were more likely to send, receive, and integrate summary of care records with other providers outside their system.
Table 1.
Characteristics of hospitals by electronic health record (EHR) developer switching status
| Switched EHR developer | Did not switch EHR developer | |
|---|---|---|
| Hospital size and status (%) | ||
| Small (<100 beds) | 35.0 | 37.1 |
| Medium (100–399 beds) | 48.8 | 46.8 |
| Large (400 or more beds) | 16.7 | 16.1 |
| Teaching | 8.4 | 10.2* |
| Government | 14.6 | 18.2* |
| Nonprofit | 76.7 | 70.9* |
| Specialty (%) | ||
| Cardiac intensive care | 44.3 | 38.9* |
| Surgical intensive care | 85.0 | 83.1 |
| Neonatal intensive care | 35.2 | 32.2 |
| Geography (%) | ||
| Urban | 68.7 | 65.7 |
| Northeast | 21.7 | 12.3* |
| West | 18.5 | 17.0 |
| Midwest | 26.5 | 32.4* |
| South | 31.5 | 37.5* |
| Business arrangement (%) | ||
| Long-term care clinic arranged within a general acute care hospital | 25.0 | 24.1 |
| Hospital itself operate subsidiary corporations | 25.0 | 24.2 |
| System owned | 74.8 | 68.6* |
| Interoperability domains (%)a | ||
| Send | 82.1 | 91.7* |
| Receive | 63.7 | 73.3* |
| Integrate | 37.5 | 45.4* |
| Find | 58.3 | 62.1 |
| N (number unique hospitals) | 1021 | 2055 |
Notes: Means are weighted by hospital bed size.
Sources: American Hospital Association Census Survey and American Hospital Association Information Technology Supplement, years 2015–2016.
The 4 domains of interoperability are: (1) send summary of care records to sources outside the hospital’s health system, (2) receive summary of care records from sources outside the hospital’s health system, (3) electronically find patient data from outside sources, and (4) integrate summary of care records from outside sources without manual input. Estimated on a sample of nonfederal acute care hospitals that adopted EHRs and shared their patients with other hospitals outside their health system.
Statistically significant from hospitals who switched EHR developer at P < .05 using 2-sample t test.
DD model estimates
Supplementary Appendix Table SA.2 contains weighted and unweighted descriptive statistics for the key variables in the DD model, computed using the estimation sample of 3154 nonfederal acute care hospitals. In total, 24.3% of hospitals in the weighted sample switched their EHR developer, and the average HRR-level market share for the focal hospital’s EHR is 33.8%.Table 2, Panel A contains estimates of the impact of switching to a new EHR developer on the proportion of patients shared with other hospitals having the same EHR developer. In our base specification containing hospital and year fixed effects, switching EHR developers is associated with a 1.0 percentage point increase in the 1 year change in same-developer patient sharing (Panel A, column 1). The weighted mean of the dependent variable is 0.24, indicating that, on average, there is a 4.1% increase in same-developer patient sharing for hospitals that switched EHR developers. The addition of HRR-specific time trends to the model (column 2) only slightly decreases the estimate of switching developers on same-developer patient sharing.
Table 2.
Effects of switching electronic health record (EHR) developer on same-developer patient sharing
| (1) | (2) | (3) | |
|---|---|---|---|
| Difference-in-differences (DD) model | DD model with HRR time trends | C&S DD | |
| Panel A | |||
| Switch | 0.010 (0.004)* | 0.008 (0.004)* | 0.047 (0.017)* |
| Panel B | |||
| Switch | 0.003 (0.007) | 0.003 (0.007) | — |
| Switch*Developer share | 0.043 (0.020)* | 0.033 (0.020) | — |
| Switched (subset = Developer share below median) | — | — | 0.046 (0.021)* |
| Switched (subset = Developer share at or above the median) | — | — | 0.057 (0.027)* |
| Year fixed effects | X | X | X |
| Hospital fixed effects | X | X | X |
| HHR linear time trends | X |
Notes: All models include controls for developer market share within the HRR and whether the hospital changed system ownership. Regressions are weighted by hospital bed size and standard errors, in parenthesis, are clustered on hospital. N (unique hospitals) = 3154 in all models.
Sources: Centers for Medicare & Medicaid Services (CMS) referral data, CMS EHR Meaningful Use Program Data, and the Office of the National Coordinator for Health Information Technology’s Certified Health IT Product List.
C&S: Calloway and Sant’Anna (2021) method.
Statistically significant from zero at P < .05.
In Table 2, Panel B, we interact the treatment variable for switching EHRs with the EHR developer’s HRR market share. The estimates from all models indicate that switching EHR developers has a bigger impact on same-developer patient sharing when that developer controls a larger share of the market. Based on the estimates in column 1, there is a small effect of switching developers on same-developer patient sharing when the EHR developer’s market share is very small. However, same-developer patient sharing increases to 4.6 percentage points after switching when the developer has a 100% market share (monopoly) in the HRR. This means that, on average, same-developer patient sharing in monopoly markets is significantly higher when a hospital switches to what becomes the monopoly developer. Given the average developer market share of 33.8%, switching EHR developer increases same-developer patient sharing by 2.5 percentage points (10.1%) in the interacted model. Adding HRR-specific linear time trends to the model reduces the magnitude and precision of the estimated coefficient on the interaction term (P = .104), but does not change the qualitative conclusions from the model.
Robustness tests
In column 3 of Table 2, we report the treatment effect of switching from the C&S doubly robust model, which is larger in magnitude than our base specification. In particular, the C&S model yields a treatment effect of switching EHR developer on same-developer patient sharing of 4.7 percentage points, or 19.3%. This suggests the conventional generalized DD model may underestimate the effect of switching EHR developer on same-developer patient sharing. Since the C&S specification is not amenable to interaction terms, we instead estimated the model separately on the subsamples of developers with less than and more than the median market share. We find that the effect of switching does increase with developer market share, but the differences are not statistically significant.
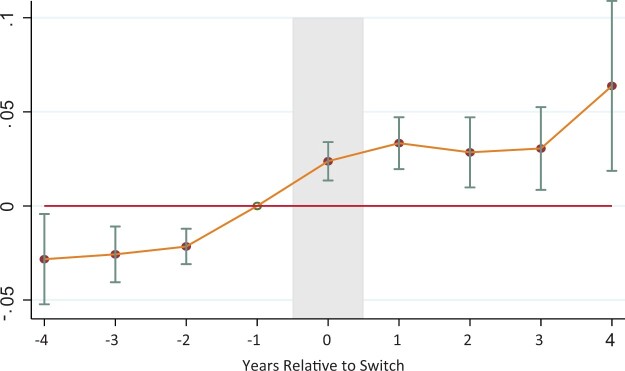
Figure 2 contains estimates from our event study model that show the treatment effect from our base specification of switching EHR developer relative to the year prior to the switch. Estimates for 2–4 years prior to the switch are not statistically different from one another, which is consistent with the parallel trend assumption of the DD model. However, these estimates are slightly lower than the year prior to the switch, suggesting a small positive effect of switching just before the year of the switch. It is possible that some hospitals utilized a new EHR during part of the calendar year prior to when they registered the new system in the CHPL, leading to a small effect in the year before the switch, or that physicians changed their behavior in anticipation of the new EHR. The small prior year effect becomes statistically insignificant when we add HRR linear time trends to the model (results not shown).
Figure 2.
Event study of treatment effects of switching EHR developer on same-developer patient sharing. Notes: Hospitals switched electronic health record (EHR) developer in Year 0. The figure shows 95% confidence intervals. Sources: Authors calculations using Centers for Medicare & Medicaid Services (CMS) referral data, CMS EHR. Meaningful Use Program Data, and the Office of the National Coordinator for Health Information Technology’s Certified Health IT Product List.
Table 3 contains estimates for other robustness checks of our main results that include subsetting the sample the hospitals that only switched developers once (column 1) and to those that did not change network affiliation (column 2). In both cases, the estimates are nearly identical to our base specification. We also present estimates corresponding to our modified dependent variable that is robust to the EHR adoption decisions of outside hospitals (column 3) and further subset these models to hospitals that did not change networks (column 4). The estimates in columns 3 and 4 are qualitatively consistent with our base specification, but larger in magnitude. Finally, we include estimates from unweighted regressions in Supplementary Appendix Table SA.3, which are very similar to the estimates using hospital bed size weights.
Table 3.
Effects of switching electronic health record (EHR) developers using alternative samples and dependent variable
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| Estimation sample | Hospitals that switched EHR developers once | Hospitals that did not change networks | All hospitals; modified dependent variable | Hospitals that did not change networks; modified dependent variable |
| Difference-in-differences (DD) model | 0.011 (0.004)* | 0.013 (0.015)* | 0.020 (0.018) | 0.01 (0.02) |
| DD model w/ HRR time trends | 0.011 (0.004)* | 0.010 (0.005)* | 0.026 (0.016)^ | 0.031 (0.021) ^ |
| N | 3035 | 2450 | 3035 | 2363 |
Notes: All models include controls for developer market share within the HRR and whether the hospital changed system ownership. Regressions are weighted by hospital bed size and standard errors, in parenthesis, are clustered on hospital.
Sources: Centers for Medicare & Medicaid Services (CMS) referral data, CMS EHR Meaningful Use Program Data, and the Office of the National Coordinator for Health Information Technology’s Certified Health IT Product List.
Statistically significant from zero at P < .05;
Statistically significant from zero at P < .10.
Differences in patient sharing across EHR developers
The EHR market has become increasingly concentrated, with the market share of the 5 largest developers currently exceeding 75% of all nonfederal acute care hospitals.17 Consolidation among EHR developers raises the prospect that 1 or 2 dominant developers could be responsible for the patient sharing concentrations we identify in our empirical analysis. We investigated this possibility by estimating the change in same-developer patient sharing for hospitals that switched to each of the 5 largest developers. In this case, the treatment group in the generalized DD model contains only those hospitals that switched to the specified developer and the control group includes all hospitals that did not change developer. The results, which are reported in Supplementary Appendix Table SA.4, indicate that hospitals switching to Cerner, Epic, and Meditech drove the increase in same-developer patient sharing identified in our main models. Hospitals switching to Meditech exhibited a 3.2 percentage point increase in the 1-year change in the percentage of patients shared with other hospitals using Meditech, while the hospitals switching to Cerner and Epic exhibited increases of 1.7 and 1.9 percentage points, respectively.
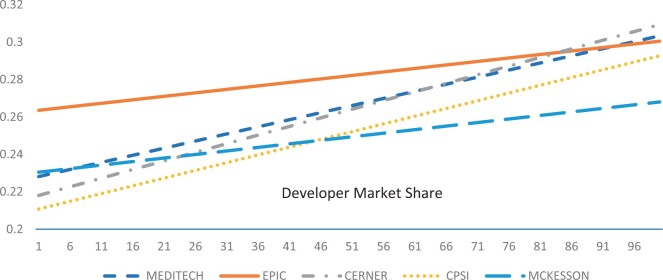
In order to determine whether the developer-specific effects varied by market share, we created linear projections of the impact of switching to the given developer on same-developer patient sharing from models with developer market share interactions (Figure 3). The magnitude of the estimated increase in same-developer patient sharing is increasing in market share for all EHR developers. However, among the three developers with statistically significant increases in the noninteracted models, the rate of same-developer patient sharing rises the most with the market share of Cerner. As a result, in highly concentrated markets, hospitals switching to Cerner are expected to increase patients shared with other hospitals using the same developer more than hospitals that switched to either Meditech or Epic.
Figure 3.
Linear projections of the effects of switching electronic health record (EHR) developer on same-developer patient sharing by developer market share. Notes: The projections are based on linear models that control for system ownership, hospital EHR developer market share, year fixed effects, and hospital fixed effects. All models are weighted by hospital bed size. Only the trend line for Cerner is statistically significant at the 10% level.
DISCUSSION
We find that the proportion of patients shared with hospitals having the same EHR developer increased over time. Consolidation in the EHR developer industry has certainly contributed to this trend, but local market conditions also play an important role. Our DD models reveal that switching to a new EHR developer increases same-developer patient sharing, and that this effect is increasing in the adopted developer’s market share.
Other findings from the literature correlate with our results. In particular, Freedman et al16 find substantial agglomeration of EHR developers, which increases as hospital markets become more competitive. It may be that the need to coordinate with other hospitals in competitive markets reinforces the desire to lower the costs of information sharing by transferring patients to hospitals using the same developer.18 Similarly, Everson and Adler-Milstein8 demonstrate that hospitals using a dominant developer engage in more HIE than those using another developer. They find that the amount of data exchange occurring among hospitals that share patients increases with the dominant developer’s market share, which could be a manifestation of lower coordination costs in markets where a single developer is dominant. Furthermore, technical barriers to exchange are lessened when exchange partners use the same developer. We find that patient sharing itself (rather than data transfer among shared patients) increases when hospitals switch to a dominant EHR developer in a market area, suggesting that market dominance leads to both an increase in shared patients as well as an increase in data sharing for each shared patient.
Our results have important implications for future policies regarding the interoperable exchange of health information. Same-developer patient sharing could benefit patients by ensuring that healthcare providers have access to accurate and timely health information. However, hospital transfers and referrals influenced more by the hospital’s EHR provider than the specific healthcare needs of the patient could result in poor patient-provider matches. There are also concerns that concentrations in patient sharing could further reduce competition in healthcare markets.19 In a perfectly interoperable environment, the referring physician’s EHR developer would not affect hospitals’ transfer or referral patterns. Our analysis cannot confirm whether technical problems associated with cross-developer exchange or efforts to block the transfer of information among hospitals and developers affect hospital patient sharing. However, we believe that both could contribute to our findings.
Recent policies could address some of these issues. To meet the requirements of the federal government’s PI programs, beginning from 2019, all hospitals have to use the 2015 Edition certified EHR.20 This edition features an application programming interface and Direct Project for secure health exchanges, which are expected to improve the exchange of health information.21,22 Furthermore, section 4004 of the 2016 Cures Act, defines practices that constitute information blocking, and establishes federal fines of up to $1 000 000 per violation.7 For example, the law specifies that “implementing health information technology in nonstandard ways that are likely to substantially increase the complexity or burden of accessing, exchanging, or using electronic health information” constitutes information blocking. Our results raise the question of whether higher patient sharing among hospitals with the same EHR developer is due, in part, to information blocking. However, further research needs to address the mechanisms underlying the concentration in patient sharing identified in this study in order to formulate regulatory policies. Finally, it is important to note that even if developer-based EHRs do not adversely influence patient sharing, under current levels of adoption, less than half of patient transitions can be supported by proprietary HIE.23 The development of open, community-based HIE is still needed to improve data transfer across swaths of the patient population.
Limitations
Our study has several limitations. First, we cannot distinguish between different types of patient sharing across hospitals. Because we consider patients shared within a 1-month period, we expect that patient sharing largely reflects intra-hospital transfers. However, it is possible that the patient may have decided to visit a different hospital in another healthcare network without a referral from any provider. In addition, provider preferences may interact with EHR design to influence patient sharing. For example, physicians may develop a preference for transferring patients to hospitals with the same EHR developer because they believe that the transmission of historical clinical information is more reliable. Certain technical characteristics of the developer-based network may reinforce this preference. Our inability to observe these and other potential mechanisms behind the change in patient sharing means that we cannot make welfare statements based on our findings. Finally, while we have controlled for the effect of simultaneous EHR adoption across hospitals in our alternative model of Table 3, we are not able to control completely for intertemporal selection effects (eg, how EHR developers might dynamically target certain markets with sales campaigns or with other promotional incentives that change over the time period).
CONCLUSIONS
We identify a systematic concentration in patient sharing between hospitals in different healthcare networks that switch to the same EHR developer. The change in transfer and referral patterns occurs immediately after the focal hospital switches EHR developers, which suggests it could be due to technical attributes of the new EHR system, rather than a shift in provider’s preferences for hospitals based on their quality of care. Future research is needed to determine whether increased patient sharing among hospitals with the same EHR developer adversely affects patient outcomes.
FUNDING
This study was conducted at the Department of Health and Human Services and Lehigh University.
The views expressed in this article are those of the authors, and no official endorsement by the Office of the National Coordinator for Health Information Technology, Agency for Healthcare Research and Quality, the Department of Health and Human Services, or Lehigh University is intended or should be inferred.
AUTHOR CONTRIBUTIONS
YP contributed to the conception, design, data acquisition, empirical analysis, and interpretation of the article. CM contributed to the design, data acquisition, interpretation, and drafted and critically revised the article. WE contributed to the design, conception, empirical analysis, interpretation, and critically revised the article. TS contributed to the conception, design, and data acquisition.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
CONFLICT OF INTEREST STATEMENT
None declared.
DATA AVAILABILITY
Data are owned by a third party. The data underlying this article were provided by the CMS, CHPL, and American Hospital Association under license. Data will be shared on request to the corresponding author with permission of the American Hospital Association.
Supplementary Material
Contributor Information
Yuriy Pylypchuk, Department of Health and Human Services, Office of the National Coordinator for Health Information Technology, Washington, District of Columbia, USA.
Chad D Meyerhoefer, College of Business, Lehigh University; Rauch Business Center, Bethlehem, Pennsylvania, USA.
William Encinosa, Department of Health and Human Services, Agency for Healthcare Research and Quality, Rockville, Maryland, USA.
Talisha Searcy, Department of Health and Human Services, Office of the National Coordinator for Health Information Technology, Washington, District of Columbia, USA.
REFERENCES
- 1. Adler-Milstein J, Lin SC, Jha AK. The number of health information exchange efforts is declining, leaving the viability of broad clinical data exchange uncertain. Health Aff (Millwood) 2016; 35 (7): 1278–85. [DOI] [PubMed] [Google Scholar]
- 2. Apathy NC, Vest JR, Adler-Milstien J, Blackburn J, Dixon BE, Harle CA. Practice and market factors associated with provider volume of health information exchange. J Am Med Inform Assoc 2021; 28 (7): ocab024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Epic’s network serves approximately 1,400 hospitals, but other developers’ platforms are more limited and less used. For example, Cerner’s system only allows lab data exchange and direct messaging, while McKesson’s platform serves only 102 hospitals (Authors’ calculations from the Definitive Healthcare database. https://www.definitivehc.com/.
- 4. Adler-Milstein J, Pfeifer E. Information blocking: is it occurring and what policy strategies can address it? Milbank Q 2017; 95 (1): 117–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Murphy K. Is $2.35 per patient a fair price for EHR interoperability? EHR Intelligence. 2015. https://ehrintelligence.com/news/is-2.35-per-patient-a-fair-price-for-ehr-interoperability Accessed June 3, 2019.
- 6. Everson J, Patel V, Adler-Milstein J. Information blocking remains prevalent at the start of 21st Century Cures Act: results from a survey of health information exchange organizations. J Am Med Inform Assoc 2021; 28 (4): 727–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.21st Century Cures Act. H.R. 34, 114th Congress. 2016. https://www.govinfo.gov/content/pkg/PLAW114publ255/pdf/PLAW-114publ255.pdf Accessed February 1, 2017.
- 8. Everson J, Adler-Milstein J. Engagement in hospital health information exchange is associated with vendor marketplace dominance. Health Aff (Millwood) 2016; 35 (7): 1286–93. [DOI] [PubMed] [Google Scholar]
- 9. Castillo A, Sirbu M, Davis AL. Vendor of choice and the effectiveness of policies to promote health information exchange. BMC Health Serv Res 2018; 18 (1): 405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lin J. Strategic complements or substitutes? The case of adopting health information technology by U.S. hospitals. SSRN Working Paper. 2019. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=309963 October 25, 2021.
- 11. Usher M, Sahni N, Herrigel D, et al. Diagnostic discordance, health information exchange, and inter-hospital transfer outcomes: a population study. J Gen Intern Med 2018; 33 (9): 1447–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.One complexity in identifying a hospital’s vendor is that some hospitals have multiple EHRs. In these cases we assigned to the hospital the EHR vendor housing the CDR, which is generally the most advanced EHR application. In this application was missing, we assigned the vendor that had CDS and/or CPOE.
- 13. Goodman-Bacon A. Difference-in-differences with variation in treatment timing. J Econom 2021; 225 (2): 254–77. [Google Scholar]
- 14. de Chaisemartin C, D’Haultfœuille X. Two-way fixed effects estimators with heterogeneous treatment effects. Am Econ Rev 2020; 110 (9): 2964–96. [Google Scholar]
- 15. Callaway B, Sant’Anna PHC. Difference-in-differences with multiple time periods. J Econom 2021; 225 (2): 200–30. [Google Scholar]
- 16. Freedman S, Haizhen L, Prince J. Does competition lead to agglomeration or dispersion in EMR vendor decisions? Rev Ind Organ 2018; 53 (1): 57–79. [Google Scholar]
- 17.Green J. Who are the largest EHR vendors. EHRinPractice. 12 Novemver 2021. https://www.ehrinpractice.com/largest-ehr-vendors.html Accessed November 20, 2021 .
- 18. Everson J, Adler-Milstein J. Sharing information electronically with other hospitals is associated with increased sharing of patients. Health Serv Res 2020; 55 (1): 128–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gaynor M, Mostashari F, Ginsburg PB. Making health care markets work: Competition policy for health care. Leonard D. Schaeffer Initiative for Innovation in Health Policy White Paper. 2017. https://www.brookings.edu/wp-content/uploads/2017/04/gaynor-et-al-final-report-v11.pdf Accessed January 17, 2020. [DOI] [PubMed]
- 20.Centers for Medicare and Medicaid Services. 2019. Certified EHR Technology. Washington, DC. https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Certification.html Accessed November 8, 2019.
- 21. Murphy K. 2015. ONC 2015 edition EHR certification builds case for APIs, FHIR. HIT Infrastructure. https://hitinfrastructure.com/news/onc-2015-edition-ehr-certification-build-case-for-apis-fhir Accessed November 8, 2019.
- 22.2015 Edition Health Information Technology (Health IT) Certification Criteria, 2015 Edition Base Electronic Health Record (EHR) Definition, and ONC Health IT Certification Program Modifications. 45 C.F.R. 170 § 170.315(h)(1) (Direct Project). 2015. https://www.federalregister.gov/documents/2015/10/16/2015-25597/2015-edition-health-information-technology-health-it-certification-criteria-2015-edition-base Accessed November 22, 2021. [PubMed]
- 23. Everson J, Cross DA. Mind the gap: the potential of alternative health information exchange. Am J Manag Care 2019; 25 (1): 32–8. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are owned by a third party. The data underlying this article were provided by the CMS, CHPL, and American Hospital Association under license. Data will be shared on request to the corresponding author with permission of the American Hospital Association.