Abstract
Background
Throughout the COVID-19 pandemic, as measures have been taken to both prevent the spread of COVID-19 and provide care to those who fall ill, healthcare workers have faced added risks to their health and wellbeing. These risks are disproportionately felt by women healthcare workers, yet health policies do not always take a gendered approach.
Objectives
The objective of this review was to identify the gendered effects of crises on women healthcare workers’ health and wellbeing, as well as to provide guidance for decision-makers on health systems policies and programs that could better support women healthcare workers.
Methods
A scoping review of published academic literature was conducted. PubMed, EMBASE, and CINAHL were searched using combinations of relevant medical subject headings and keywords. Data was extracted using a thematic coding framework. Seventy-six articles met the inclusion criteria.
Results
During disease outbreaks women healthcare workers were found to experience: a higher risk of exposure and infection; barriers to accessing personal protective equipment; increased workloads; decreased leadership and decision-making opportunities; increased caregiving responsibilities in the home when schools and childcare supports were restricted; and higher rates of mental ill-health, including depression, anxiety, and post-traumatic stress disorder. There was a lack of attention paid to gender and the health workforce during times of crisis prior to COVID-19, and there is a substantial gap in research around the experiences of women healthcare workers in low- and middle-income countries during times of crises.
Conclusion
COVID-19 provides an opportunity to develop gender-responsive crisis preparedness plans within the health sector. Without consideration of gender, crises will continue to exacerbate existing gender disparities, resulting in disproportionate negative impacts on women healthcare workers. The findings point to several important recommendations to better support women healthcare workers, including: workplace mental health support, economic assistance to counteract widening pay gaps, strategies to support their personal caregiving duties, and interventions that support and advance women's careers and increase their representation in leadership roles.
Keywords: COVID-19, Health workforce, Gender, Women, Crises
1. Introduction
Throughout the COVID-19 pandemic, as measures have been taken to both prevent the spread of COVID-19 and provide care for those who fall ill, healthcare workers have faced added risks to their health and wellbeing, including increased vulnerability to infection and stress (Daryanti Saragih et al. 2021). This is coupled with additional demands, primarily born by women, including childcare and eldercare responsibilities due to school, facility, and service interruptions (C. Wenham et al. 2020; Clare Wenham, Smith, and Morgan 2020). Globally, women make up 75% of the health and social care workforce, and in certain professions such as nursing and midwifery, the numbers are even greater (WHO 2019). As such, the impacts of crises are predominately felt by women healthcare workers. Currently, it is unclear how healthcare workers’ physical and mental health are being affected, and how this impacts the supply of healthcare workers, access to healthcare, quality of care provided, and decision-making around health systems.
We reviewed the global academic literature on workforce experiences of health crises, applying a gender-based analysis (Morgan et al. 2016) to better understand what is known about women healthcare workers’ experiences during crises. Crises included: natural disasters, such as tsunamis, wildfires, earthquakes, epidemics and pandemics (including zika, Ebola, influenza, hemorrhagic fever, and COVID-19). The objectives of the review were to: (1) Identify the gendered effects of crises on women healthcare workers’ mental and physical health, and how this affects healthcare worker supply and quality of care; (2) Investigate how measures to support healthcare workers during times of crises may differentially impact women healthcare workers; and, (3) Provide guidance to decision-makers on how broader health system policies and programs can support and empower women healthcare workers to improve health systems and outcomes.
This review's focus on peer reviewed academic literature does not preclude the importance of gray literature on this topic. Many organizations, including the World Health Organization, the International Council of Nurses, Women in Global Health, and the British Columbia Women's Health Foundation, have published important and relevant reports related to women, gender, and human resources for health, including ones that specifically focus on human resources during crises. Many of the issues discussed in this paper (inside and outside the context of crises) have been highlighted in this work, including: (1) the State of the World's Nursing Report (WHO, 2020), (2) Closing the leadership gap: gender equity and leadership in the global health and care workforce (WHO, 2021), and (3) Delivered by women, led by men: a gender and equity analysis of the global health and social workforce (WHO, 2019). Reports specifically relevant to crises include: Invisible No More: Inequities faced by women healthcare workers, especially during the COVID-19 pandemic, + recommendations for action (BCWHF, 2021), and (2) Fit for Women: Safe and Decent PPE for Women Health and Care Workers. There has also been important work that has taken an intersectional lens to health workers during times of crises, including the OECD report Contribution of migrant doctors and nurses to tackling COVID-19 crisis in OECD countries (OECD, 2020). While here we focus on research on women healthcare workers, we recognize the differences in experiences with the broad category of women and the need for research focused on the intersections of inequities. However, our aim was to start by scoping the literature on women healthcare workers and crisis broadly, which we hope can then provide grounding for more nuanced intersectional analysis.
2. Methods
A scoping review methodology was chosen, recognizing that knowledge about the experiences of women healthcare workers during times of crisis is limited. Therefore, rather than systematically analyze evidence, we aimed to gaining understanding of the breadth of the literature, and gaps therein, in order to inform further research (Munn et al. 2018).
Search strategy and inclusion criteria
PubMed, EMBASE, and CINAHL were searched using combinations of relevant medical subject headings (MeSH) and keywords. The following broad concepts were explored in the search: Human Resources, Gender, and Emergencies/Crises. Research articles and commentaries that met the following inclusion criteria were included in the study: 1) Published in English, 2) Published between 2010–2021, 3) Focused on acute and/or chronic crises, 4) Focused on human resources for health, 5) Included or focused on women, 6) Focused on the gendered effects of crises on mental and physical health, and 7) were peer reviewed. Studies were included if they reported or discussed data on the gendered effects of crises on women healthcare workers, even if this was not the primary aim of the study.
Data extraction
Data was extracted using a thematic coding framework, including the following categories: reported non-health related gendered effects, health related effects, health system effects, leadership and power in decision-making, measures to support healthcare workers, as well as the effect of these measures. In order to identify the gendered effects of crises on women healthcare workers, a gender analysis framework was applied to the data, which identifies how gender inequities manifest as inequitable: access to resources, roles, distribution of labor and practices, norms and beliefs, and decision-making power and autonomy. In addition, author, title, year published, type of article, country, methods, participants and sample size, study aim(s), type of healthcare worker, and type of crisis/emergency was also extracted. Extracted data was thematically inputted into a chart alongside each article's identifying number. Each theme was reviewed for secondary codes or sub-themes by type/level of impact (e.g. individual, household/community, health systems, in addition to measures to address), paying specific attention to similarities and differences between the articles. Secondary codes were then synthesized and condensed into a new chart. The key themes were then summarized.
Study limitations
There are a number of limitations to this review. Firstly, we did not include an independent quality assessment of the studies which were included, instead assuming the peer review process provided an element of quality control. We feel this assumption is appropriate for a scoping review which aims to understand the breadth of the literature, as opposed to analyze specific findings within it. We are therefore unable to comment on the overall quality of the included papers. We also did not conduct a search of gray literature which means some relevant research may have been missed. We also only included articles published in English.
3. Results
Search results
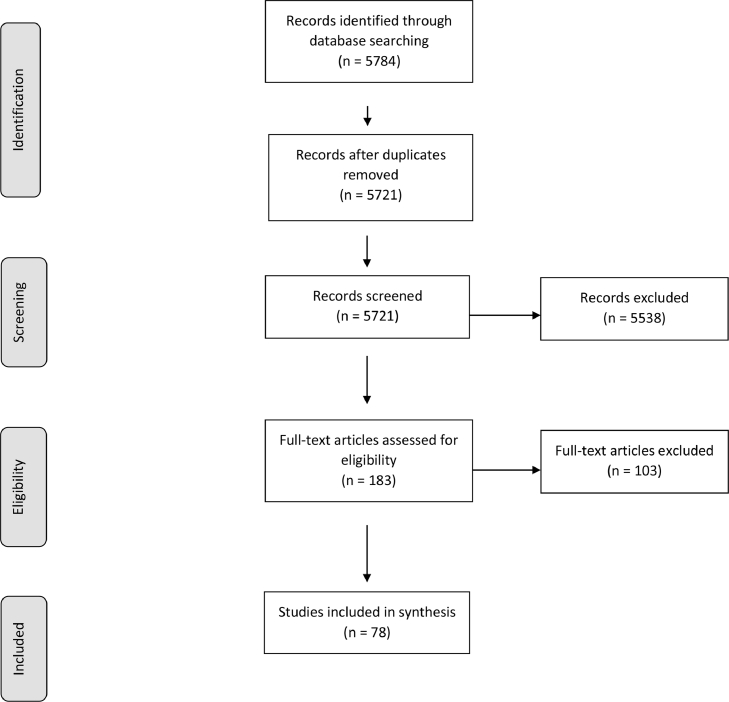
The search yielded a total of 5784 articles which were imported onto the Covidence platform and screened for duplicates; 5721 titles and abstracts were screened for eligibility, of which 5538 were excluded. Full text screening was conducted for 183 articles, where an additional 103 were excluded. Seventy-eight articles met the inclusion criteria.
Description of articles
Sixty four of the 76 articles included focused specifically on COVID-19 (Table 1). Other types of crises/emergencies included: influenza pandemic, including HIN1, seasonal flu, 1918 flu pandemic, Ebola, exanthematous diseases, and natural and manmade disasters, such as earthquakes. Sixty seven of the articles were published in 2020 (table 2).
Table 1.
Breakdown of articles by frequency of type of crisis (N=76).
| Crisis type | n (%) |
|---|---|
| Ebola | 1 (1.3%) |
| H1N1 | 1 (1.3%) |
| Seasonal flu | 1 (1.3%) |
| Spanish flu | 1 (1.3%) |
| Emergency room | 2 (2.6%) |
| Earthquake | 2 (2.6%) |
| Other | 4 (5.2%) |
| COVID-19 | 64 (84%) |
Table 2.
Breakdown of articles by year of publication (N=76).
| Year | n (%) |
|---|---|
| 2020 | 67 (88.2%) |
| 2019 | 2 (2.6%) |
| 2017 | 2 (2.6%) |
| 2015 | 1 (1.3%) |
| 2014 | 1 (1.3%) |
| 2013 | 2 (2.6%) |
| 2010 | 1 (1.3%) |
Across the articles, healthcare workers included: physicians, nurses, data-entry staff, transportation staff, patient support staff, medical students, pharmacists, physiotherapists, intensivists, administrative and clerical staff, support staff, maintenance workers, caregivers, midwives, lab staff, ophthalmologists, community health workers, emergency service employees, dentists, cardiologists, medical technicians, nursing assistants and residents, assisted living care workers, and obstetricians/gynaecologists (table 3). Not all studies distinguished by type of healthcare worker, while others included a mix of healthcare workers but did not disaggregate data by cadre.
Table 3.
Breakdown of articles by frequency of type of healthcare worker (N=76).
| Healthcare worker type | n (%) |
|---|---|
| Midwives | 1 (1.3%) |
| Community health workers | 1 (1.3%) |
| Emergency medical responders | 1 (1.3%) |
| Assistant physicians | 1 (1.3%) |
| Caregivers | 1 (1.3%) |
| Living residence workers and health aides | 2 (2.6%) |
| Emergency department staff | 3 (3.9%) |
| Hospital personnel | 3 (3.9%) |
| Medical students, nursing students, and/or residents | 3 (3.9%) |
| Nurses | 7 (9.2%) |
| Not limited to healthcare workers | 8 (10.5%) |
| Physicians | 9 (11.8%) |
| Mix of healthcare professionals | 36 (47.3%) |
Primary research studies were conducted in: Turkey, France, Saudi Arabia, Greece, Italy, Taiwan, Ireland, India, Guatemala, China, Canada, Mexico, United States, United Kingdom, Spain, Mali, Japan, Iran, Zimbabwe, Uganda, Sierra Leone, and Cambodia (table 4). Systematic reviews, literature reviews, and commentaries which were not country specific were also included.
Table 4.
Breakdown of articles by country the study was conducted in (N=76).
| Country | n (%) |
|---|---|
| Guatemala | 1 (1.3%) |
| India | 1 (1.3%) |
| Ireland | 1 (1.3%) |
| Mali | 1 (1.3%) |
| Mexico | 1 (1.3%) |
| Saudi Arabia | 1 (1.3%) |
| Taiwan | 1 (1.3%) |
| United Kingdom | 1 (1.3%) |
| Japan | 2 (2.6%) |
| Canada | 2 (2.6%) |
| France | 2 (2.6%) |
| Greece | 2 (2.6%) |
| Iran | 3 (3.9%) |
| Italy | 4 (5.2%) |
| Spain | 6 (7.9%) |
| United States of America | 7 (9.2%) |
| Turkey | 8 (10.5%) |
| China | 9 (11.8%) |
| Country comparison: Zimbabwe, Uganda, Sierra Leone, Cambodia | 1 (1.3%) |
| Not specified | 4 (5.2%) |
| N/A (Commentary, literature review) | 18 (23.6%) |
The results below are synthesized from the 76 articles. A description of the articles is provided in table 5. While we were interested in the gendered impacts of crises and emergencies on women healthcare workers, it was not always easy to disentangle a gendered impact from a non-gendered impact, particularly due to the overall gendered nature of the healthcare workforce. For example, impacts on professions such as nursing can often be assumed to be primarily affecting women, even where findings do not specifically pertain to women (Shannon et al. 2019; WHO 2019) .
Table 5.
Study Characteristics (N=76).
| Author(s) | Title | Country | Study Design | Participants | No. of participants | Aim of study | Type of emergency | |
|---|---|---|---|---|---|---|---|---|
| 1 | Ahmed & Dumanski, 2020 | Sex, gender and COVID-19: a call to action | N/A | Literature review | N/A | N/A | Outline the influence of sex and gender on the rate of infection, hospitalization, and mortality from COVID-19. | COVID-19 |
| 2 | Araç & Dönmezdil, 2020 | Investigation of mental health among hospital workers in the COVID-19 pandemic: A cross-sectional study | Turkey | Survey study (cross-sectional) | Physicians, nurses, data-entry staff, patient transportation staff, and patient support staff |
210 | Examine psychiatric disorders among healthcare professionals. |
COVID-19 |
| 3 | Azoulay et al., 2020a | Symptoms of Anxiety, Depression, and Peritraumatic Dissociation in Critical Care Clinicians Managing Patients with COVID-19. A Cross-Sectional Study | France | Survey study (cross-sectional) | ICU physicians | 1001 (34% women) | Document the prevalence of burnout syndrome amongst intensivists. | COVID-19 |
| 4 | Azoulay et al., 2020b | Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak | France | Survey study (cross-sectional) | Frontline healthcare providers, including nurses, physicians, allied professionals, physiotherapists, and psychologists | 1058 (71% women) | Assess the prevalence of symptoms of anxiety, depression, and peritraumatic dissociation. | COVID-19 |
| 5 | Bahat et al., 2020 | Evaluating the effects of the COVID‐19 pandemic on the physical and mental well‐being of obstetricians and gynecologists in Turkey | Turkey | Survey methods | Obstetricians and gynecologists | 253 (54.4% women) | Assess the general physical and mental wellbeing of obstetricians/gynecologists working in COVID‐19 hospitals. | COVID-19 |
| 6 | Balkhy et al., 2010 | Epidemiology of H1N1 (2009) influenza among healthcare workers in a tertiary care center in Saudi Arabia: a 6-month surveillance study | Saudi Arabia | Prospective cohort study | Healthcare workers, including nurses, physicians, and administrators and support staff | 526 (55.1% women) | Examine the epidemiology of H1N1 influenza among healthcare workers. | H1N1 |
| 7 | Benfante et al., 2020 | Traumatic Stress in Healthcare Workers During COVID-19 Pandemic: A Review of the Immediate Impact | N/A | Literature review | Healthcare workers, including doctors, nurses, and ancillary healthcare workers | N/A | Review studies that have explored traumatic stress in healthcare workers and associated factors between January and May 2020. | COVID-19 |
| 8 | Bennett et al., 2020 | Beyond tropes: Towards a new image of nursing in the wake of COVID‐19 | N/A | Literature review | Nurses | N/A | Evaluate the impact of COVID-19 on nurses. | COVID-19 |
| 9 | Blekas, et al., 2020 | COVID-19: PTSD symptoms in Greek health care professionals | Greece | Survey study (cross-sectional) | Healthcare professionals, including medical specialties and nursing | 270 (199 women) | Assess the emergence of posttraumatic stress symptoms in health care professionals | COVID-19 |
| 10 | Bonaccorsi, et al., 2013 | Predictive factors associated with the acceptance of pandemic and seasonal influenza vaccination in health care workers and students in Tuscany, Central Italy | Italy | Survey study (cross-sectional) | Healthcare professionals, including physicians and nurses | 2598 (1820 women) | Evaluate the opinion of healthcare workers and students regarding influenza, influenza vaccine and the factors associated with vaccination compliance | Influenza (seasonal flu) |
| 11 | Bourgeault et al., 2020 | The COVID-19 pandemic presents an opportunity to develop more sustainable health workforces | N/A | Literature review | Health workforce | N/A | Address the critically important role of health workers in their countries’ more immediate responses to COVID-19 outbreaks | COVID-19 |
| 12 | Brubaker, 2020 | Women Physicians and the COVID-19 Pandemic | N/A | Literature review | Physicians | N/A | Examine how women are impacted by the pandemic in areas at higher rates due to gender impacts. | COVID-19 |
| 13 | Carpinelli Mazzi, 2020 | Time of isolation, education and gender influence the psychological outcome during COVID‑19 lockdown in caregivers of patients with dementia | Italy | Survey study | Caregivers of people with dementia | 239 (115 women) | analyze the effects of the lockdown on the psychological outcomes in caregivers of persons with dementia. | COVID-19 |
| 14 | Chaudhary, 2020 | Women in COVID Pandemic: Beyond Morbidity and Mortality | N/A | Literature review | Healthcare providers | N/A | Examine the impact of COVID-19 on women. | COVID-19 |
| 15 | Chen, 2020 | A Large-Scale Survey on Trauma, Burnout, and Posttraumatic Growth among Nurses during the COVID-19 Pandemic | Taiwan | Survey study | Nurses | 12,596 (95.6% women) | Examine the psychological impact of COVID-19 on nurses. | COVID-19 |
| 16 | Chowdhry, 2020 | Trying To Do It All: Being a Physician-Mother during the COVID-19 Pandemic | N/A | Storytelling | N/A | N/A | Palliative women physician provides insight on the impact of being a mother physician during COVID. | COVID-19 |
| 17 | Corbett, 2020 | Anxiety and depression scores in maternity healthcare workers during the Covid-19 pandemic | Ireland | Prospective study | Maternity ward healthcare workers | 200 (175 female) | Assess anxiety and depression among healthcare workers during Covid‐19 pandemic. | COVID-19 |
| 18 | Daye et al., 2020 | Evaluation of skin problems and dermatology life quality index in health care workers who use personal protection measures during COVID-19 pandemic | Turkey | Questionnaire | Healthcare workers, including doctors and nurses | 440 | Evaluate skin problems and dermatological life quality of health care workers due to PPE. | COVID-19 |
| 19 | Demir et al., 2020 | Attitudes of Healthcare Workers Towards COVID-19 and Affecting Factors | Turkey | Cross-sectional study | Doctors, dentists, nurses, midwives, health officers and technicians | 370 (45.3% women) | Examine the attitudes of healthcare workers towards COVID-19 and the affecting factors. | COVID-19 |
| 20 | Felice et al., 2020 | Impact of COVID-19 Outbreak on Healthcare Workers in Italy: Results from a National E-Survey | Italy | Online survey | Physicians and other healthcare workers | 388 (61% women) | Assess in depth the impact of the outbreak on healthcare workers. | COVID-19 |
| 21 | García-Reyna et al., 2020 | Fear of COVID-19 Scale for Hospital Staff in Regional Hospitals in Mexico: A Brief Report | Mexico | Cross-sectional survey | Hospital personnel | 2860 (1641 women) | Identify level of fear of COVID-19 in hospital staff. | COVID-19 |
| 22 | Godderis & Rossiter, 2013 | ‘If you have a soul, you will volunteer at once’: gendered expectations of duty to care during pandemics | Canada | Historical analysis | N/A | N/A | Explore the moral and gendered dimension of pandemic risk. | 1918 flu pandemic |
| 23 | Grover et al., 2020 | “Depression, Anxiety and Stress” in a Cohort of Registered Practicing Ophthalmic Surgeons, Post Lockdown during COVID-19 Pandemic in India | India | Cross-sectional survey | Ophthalmologists | 144 (78 women) | Assess the magnitude of mental health problems among ophthalmologists in India post lockdown during the COVID-19 pandemic. | COVID-19 |
| 24 | Hacimusalar et al., 2020 | Anxiety and hopelessness levels in COVID-19 pandemic: A comparative study of healthcare professionals and other community sample in Turkey | Turkey | Online assessment | Doctors, nurses, and other healthcare workers | 2156 (52% healthcare workers) | Evaluate the factors affecting the anxiety and hopelessness levels of healthcare professionals and compare with non-healthcare professionals. | COVID-19 |
| 25 | Han et al., 2020 | Anxiety and Depression of Nurses in a North West Province in China During the Period of Novel Coronavirus Pneumonia Outbreak | China | Cross-sectional survey | Nurses | 22034 (98.6% women) | Investigate the anxiety and depression levels of frontline clinical nurses. | COVID-19 |
| 26 | Havlioğlu & Demir, 2020 | Determining the Anxiety Levels of Emergency Service Employees’ Working During the Covid-19 Pandemic | Turkey | Descriptive information form | Emergency service employees | 95 (35.8% women) | Determine the anxiety levels of emergency service employees working during the COVID-19 pandemic. | COVID-19 |
| 27 | Hernandez et al., 2020 | Adapting antenatal care in a rural LMIC during COVID‐19: A low literacy checklist to mitigate risk for community health workers | Guatemala | Piloting of an ANC protocol | Traditional birth attendants | 8 | Evaluate an ANC protocol pilot for low‐literacy community healthcare workers during the COVID‐19 pandemic. | COVID-19 |
| 28 | Huang et al., 2020 | Emotional responses and coping strategies in nurses and nursing students during COVID-19 outbreak: A comparative study | China | Online survey questionnaire | College students and first-line nurses aged 18–26 years old | 802 (74.9% women) | Investigate nurses’ emotional responses and coping styles and conduct a comparative study with nursing college students. | COVID-19 |
| 29 | Jones et al., 2020 | Collateral Damage: How COVID-19 Is Adversely Impacting Women Physicians | N/A | Commentary | Physicians | N/A | Describe how the current COVID-19 pandemic may intensify workplace inequities for women. | COVID-19 |
| 30 | Kelker et al., 2020 | Longitudinal Prospective Study of Emergency Medicine Provider Wellness Across Ten Academic and Community Hospitals During the Initial Surge of the COVID-19 Pandemic | United States | Longitudinal, descriptive, prospective cohort survey study | EM physicians and advanced practice providers | 213 | Assess the well-being, resilience, burnout, and wellness factors and needs of EM physicians and advanced practice providers (APPs) during the initial phase of the COVID-19 pandemic. | COVID-19 |
| 31 | King et al., 2020 | Reordering gender systems: can COVID-19 lead to improved gender equality and health? | Not specified | Secondary research | N/A | N/A | Discuss the impact of COVID-19 on gender in healthcare systems. | COVID-19 |
| 32 | Kuehn, 2020 | Mitigating the Psychological Harm of COVID-19 Pandemic for Clinicians | United States | Secondary research | Cardiologists | N/A | Evaluate the impact of COVID-19 on training cardiologists. | COVID-19 |
| 33 | Kurt, et al., 2020 | Levels of anxiety and depression related to covid-19 among physicians: An online cross-sectional study from Turkey | Turkey | Cross-sectional survey study | Assistant physicians taking medical specialty training | 264 | Determine anxiety and depression levels related to COVID-19 infection of assistant physicians who were taking medical specialty training in a medical faculty hospital. | COVID-19 |
| 34 | Lai et al., 2020a | Factors Associated with Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019 | China | Cross-sectional survey | Nurses and physicians | 1257 | Assess the magnitude of mental health outcomes and associated factors among health care workers treating patients exposed to COVID-19 in China. | COVID-19 |
| 35 | Lai et al., 2020b | Coronavirus Disease 2019 (COVID-2019) Infection Among Health Care Workers and Implications for Prevention Measures in a Tertiary Hospital | China | Case series | Physicians, nurses, and health care assistants | 9648 | Explore infection risk and clinical characteristics of healthcare workers healthcare workers with COVID-19 and discuss possible prevention measures. | COVID-19 |
| 36 | Li et al., 2020 | Psychological impact on women health workers involved in COVID-19 outbreak in Wuhan: A cross-sectional study | China | Cross-sectional survey | Doctors, nurses and medical technicians | 4369 | Evaluate immediate psychological impact on women healthcare workers. | COVID-19 |
| 37 | López-Atanes et al., 2020 | Are women still "the other"? Gendered mental health interventions for health care workers in Spain during COVID-19 | Spain | Secondary research | Healthcare workers | N/A | Discuss the gendered aspects of the impact of COVID-19. | COVID-19 |
| 38 | Louisias et al., 2020 | Intersectional Identity and Racial Inequality During the COVID-19 Pandemic: Perspectives of Black Physician Mothers | N/A | Commentary | Black physician mothers | N/A | Discuss the impact of the pandemic on black physician mothers. | COVID-19 |
| 39 | Luo et al., 2020 | The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - A systematic review and meta-analysis | N/A | Systematic review and meta-analysis | Healthcare workers, general population, and patients with higher COVID-19 risk | N/A | Identify the psychological and mental impact of COVID-19 among healthcare workers, general population, and patients with higher COVID-19 risk | COVID-19 |
| 40 | Makino et al., 2020 | Mental health crisis of Japanese health care workers under COVID-19 | Japan | Secondary research | Healthcare workers | N/A | Discuss the psychological impact of COVID-19 on healthcare workers. | COVID-19 |
| 41 | Mann et al., 2020 | Considerations for Pregnant Dental and Health Care Workers amid COVID-19 | United States | Secondary research | Pregnant dental and health care workers |
N/A | Present posed risks and potential effects of COVID-19 on maternal and fetal health. | COVID-19 |
| 42 | Menzel, 2015 | Nurses as scapegoats in Ebola virus disease response | Not specified | Secondary research | Nurses | N/A | Discuss the scapegoating of nurses during the Ebola epidemic. | Ebola |
| 43 | Mercer, et al., 2014 | Ready or not: does household preparedness prevent absenteeism among emergency department staff during a disaster? | United States | Survey | Emergency department staff | 399 | Determine if degree of readiness of emergency department personnel is associated with predicted likelihood of reporting for duty. | Natural disasters, terrorist events, and infectious disease outbreaks |
| 44 | Minayo & Freire, 2020 | The pandemic exacerbates health inequalities | N/A | Commentary | Nursing technicians and assistants | N/A | Discuss the impact of the pandemic on nursing technicians and assistants. | COVID-19 |
| 45 | Norton et al., 2020 | Personal protective equipment and infection prevention and control: a national survey of UK medical students and interim foundation doctors during the COVID-19 pandemic | United Kingdom | Cross-sectional study | Medical students and Year 1 doctors | 2075 | analyze self-reported adequacy of ppe and infection prevention and control training. | COVID-19 |
| 46 | Penfold & Magee, 2020 | Gender balance in an unprecedented time | N/A | Commentary | N/A | N/A | Discuss gender imbalance in health leadership. | COVID-19 |
| 47 | Reddy et al., 2020 | Management guidelines for pregnant health care workers exposed to infectious dermatoses | Not specified | Secondary research | Pregnant healthcare workers | N/A | Review infectious exanthems, transmissibility to pregnant women, and potential consequences of infection for the mother and fetus. | Exanthematous diseases & COVID-19 |
| 48 | Rivera-Izquierdo al., 2020 | Clinical Factors, Preventive Behaviours and Temporal Outcomes Associated with COVID-19 Infection in Health Professionals at a Spanish Hospital | Spain | Case series | Symptomatic health professionals, including physicians and nurses | 76 | Determine the prevalence of symptoms, main concerns as patients, preventive behaviours of healthcare professionals, and different temporal outcomes associated with the negativization of PCR results. | COVID-19 |
| 49 | Rodríguez-Rey, et al., 2020 | Working in the times of COVID-19. Psychological impact of the pandemic in frontline workers in Spain | Spain | Cross-sectional survey | Frontline workers, including healthcare workers, media professionals, grocery workers, and protective service workers | 546 (296 healthcare workers) | Evaluate the psychological impact of the COVID-19 pandemic in frontline workers. | COVID-19 |
| 50 | Rodriguez-Vega, et al., 2020 | Implementation of a Mindfulness-Based Crisis Intervention for Frontline Healthcare Workers During the COVID-19 Outbreak in a Public General Hospital in Madrid, Spain | Spain | Exploratory study | Healthcare workers, including nurses, orderlies, medical residents, physicians, cleaning staff and technicians | 150 | Describe an on-site, brief mindfulness-based crisis intervention for frontline healthcare workers. | COVID-19 |
| 51 | Romero-Blanco et al., 2020 | Sleep pattern changes in nursing students during the COVID-19 lockdown | Spain | Longitudinal observational study | Nursing students | 207 | Determine the difference in nursing students’ sleep quality before and during the COVID-19 lockdown. | COVID-19 |
| 52 | Roxby et al., 2020 | Outbreak Investigation of COVID-19 Among Residents and Staff of an Independent and Assisted Living Community for Older Adults in Seattle, Washington | United States | Symptom questionnaire for COVID-19 diagnosis | Assisted and independent living residence workers & health aides | 68% women | Conduct surveillance for SARS-CoV-2 and describe symptoms of COVID-19 among residents and staff of an independent/assisted living community. | COVID-19 |
| 53 | Ryan & Ayadi, 2020 | A call for a gender responsive, intersectional approach to address COVID-19 | N/A | Commentary | Women in general | N/A | Address health and equity issues of COVID-19 through an intersectional lens. | COVID-19 |
| 54 | Sagaon-Teyssier et al., 2020 | Assessment of mental health outcomes and associated factors among workers in community-based HIV care centers in the early stage of the COVID-19 outbreak in Mali | Mali | Self-administered questionnaire | Workers in community-based HIV care | 135 (39.5% women) | Identify individual and structural factors associated with mental health disorders in NGO healthcare workers. | COVID-19 |
| 55 | Sakuma et al., 2020 | Trajectories for Post-traumatic Stress Disorder Symptoms Among Local Disaster Recovery Workers Following the Great East Japan Earthquake: Group-based Trajectory Modeling | Japan | Questionnaire | Local municipality and hospital medical workers | 745 (59% women) | Measure PTSD symptoms post Great East Japan Earthquake of 2011. | Great East Japan Earthquake |
| 56 | Samouei et al., 2019 | Prioritization of factors related to mental health of women during an earthquake: A qualitative study | Iran | Qualitative (semi-structured interviews) | Experts in the fields of psychology, social medicine, and health management | 20 | Gather data on the views of experts regarding the mental health of women during earthquakes. | Earthquake |
| 57 | Sánchez et al., 2020 | Resilience Among Professional Health Workers in Emergency Services | Spain | Quantitative (cross-sectional) | Emergency physicians, nurses, and nursing assistants | 320 (81.87% were women) | Determine the resilience of professional health workers in emergency services and its relationships with sociodemographic and working conditions. | Focus on workers in emergency departments |
| 58 | Sandvosky et al., 2017 | Small Changes Make a Big Difference in the Fit of N95 Respirators | United States | Quality improvement test | N/A | 112 (73 women) | Investigate the equivalence in quality between HCP respirators. | General pandemics |
| 59 | Scuri et al., 2019 | Training to improve resilience and coping to monitor PTSD in rescue workers | Italy | Observational Questionnaire | Rescue workers | 52 (54% women) | Examine resilience and coping strategies of rescue workers. | Earthquake (Oct 2016, Central Italy) |
| 60 | Shaw et al., 2020 | No patient safety without health worker safety | N/A | Commentary | N/A | N/A | Highlight the intensified risks health workers undergo during times of crisis; analyze and advocate for the safety of health workers as a necessary factor for patient safety. | COVID-19 |
| 61 | Shorey & Chan, 2020 | Lessons from past epidemics and pandemics and a way forward for pregnant women, midwives and nurses during COVID-19 and beyond: A meta-synthesis | N/A | Qualitative (systematic review) | Pregnant women, midwives and nurses | 413 pregnant women, 107 midwives and nurses | Synthesize knowledge on the experiences and needs of pregnant women, midwives, and nurses of maternity units and how they were supported during past epidemics and pandemics. | Various pandemics |
| 62 | Song et al., 2020 | Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China | China | Quantitative (cross sectional questionnaire) | Doctors and nurses | 14,825 (64.3% women) | Assess the mental health of emergency department medical staff during the epidemic in China. | COVID-19 |
| 63 | St-Denis, 2020 | Sociodemographic Determinants of Occupational Risks of Exposure to COVID-19 in Canada | Canada | Literature review | Discusses occupations in relation to COVID-19 broadly | N/A | Explore the distribution of occupational exposure risks in the Canadian workforce and identify the sociodemographic characteristics associated with high or low occupational exposure risk scores. | COVID-19 |
| 64 | Sterling et al., 2020 | Experiences of Home Health Care Workers in New York City During the Coronavirus Disease 2019 Pandemic | United States | Qualitative (semi-structured interviews) | Home healthcare workers | 33 (32 women) | Understand the experiences of home health care workers caring for patients in New York City. | COVID-19 |
| 65 | Torun & Torun, 2020 | The psychological impact of the COVID-19 pandemic on medical students in Turkey | Turkey | Questionnaire | Medical students | 275 (60.7% women) | Investigate the knowledge of medical students about COVID-19, effects of traumatic situations they experienced, stress they perceived, and factors affecting them. | COVID-19 |
| 66 | Tselebis et al., 2020 | Insomnia, Perceived Stress, and Family Support among Nursing Staff during the Pandemic Crisis | Greece | Cross-sectional design | Nurses | 150 (120 women) | Investigate levels of perceived stress, insomnia, and sense of family support among nurses. | COVID-19 |
| 67 | Vahedian-Azimi et al., 2020 | Comparison of the severity of psychological distress among four groups of an Iranian population regarding COVID-19 pandemic | Iran | Quantitative (Survey) | Community population, patients with COVID-19, medical staff, and medical students | 886 (37.5% women) | Explore mental health status of four populations within Iran, including community population, patients with COVID-19, medical staff, and medical students. | COVID-19 |
| 68 | van Daalen et al., 2020 | Symptoms of a broken system: the gender gaps in COVID-19 decision-making | Not specified | Quantitative analysis | General health workers | N/A | Assess the gender gap in task forces organised to prevent, monitor and mitigate COVID-19. | COVID-19 |
| 69 | Walton, 2020 | COVID-19. The new normal for midwives, women and families | N/A | Commentary | Midwives | N/A | Give an overlay of how midwives are adjusting their practice to COVID-19. | COVID-19 |
| 70 | Wang et al., 2020 | Factors associated with post-traumatic stress disorder of nurses exposed to corona virus disease 2019 in China | China | Questionnaire | Nurses | 202 (87.6% women) | Investigate the factors potentially involved in the level of PTSD of Nurses exposed to COVID-19 in China. | COVID-19 |
| 71 | Wenham et al., 2020 | COVID-19: the gendered impacts of the outbreak | N/A | Commentary | General care workers | N/A | Describe the gap in literature on gendered effects of COVID-19. | COVID-19 |
| 72 | Wilson et al., 2020 | Caring for the carers: Ensuring the provision of quality maternity care during a global pandemic | N/A | Literature review | Maternity care providers | N/A | Overview of important considerations for supporting the emotional, mental and physical health needs of maternity care providers in the context of COVID-19. | COVID-19 |
| 73 | Witter et al., 2017 | The gendered health workforce: mixed methods analysis from four fragile and post-conflict contexts | Zimbabwe, Uganda, Sierra Leone, Cambodia | Mixed methods | General health workers | Not listed | Apply a gender analysis framework to explore access to resources, occupations, values, decision-making and power. | Crisis in post-conflict contexts |
| 74 | Zandifar et al. 2020 | Prevalence and Associated Factors of Posttraumatic Stress Symptoms and Stigma among Health Care Workers in Contact with COVID-19 Patients | Iran | Survey methods | Healthcare workers | 894 (71.4% women) | Assess the prevalence and associated factors of posttraumatic stress symptoms and stigma among health care workers. | COVID-19 |
| 75 | Zhou et al. 2020 | The prevalence and risk factors of psychological disturbances of frontline medical staff in china under the COVID-19 epidemic: Workload should be concerned | China | Survey methods | Frontline healthcare workers | 606 (81.2% women) | Investigate the prevalence and risk factors of psychological disturbances among frontline medical staff. | COVID-19 |
| 76 | Zhu et al., 2020 | COVID-19 in Wuhan: Sociodemographic characteristics and hospital support measures associated with the immediate psychological impact on healthcare workers | China | Survey methods | General health workers | 5062 (85% women) | Assess sociodemographic characteristics and hospital support measures associated with the psychological impact on healthcare workers. | COVID-19 |
4. Impacts of crises/emergencies on women healthcare workers
4.1. Exposure and risk of infection
Women often perform high contact care roles, both in the health system (such as nursing) and within homes (as caregivers), which place them at greater risk of exposure to COVID-19 (Chaudhary 2020; Hacimusalar et al. 2020; King et al. 2020). This may help to explain why they constitute the majority of healthcare workers infected with COVID-19 in countries where data is available (Ahmed and Dumanski 2020). Occupation type also intersects with gender, compounding the risk of infection. At the Tonji Hospital in Wuhan, China, for instance, nurses had a 2.7-fold risk of contracting COVID-19 compared to physicians (X. Lai et al. 2020). Home healthcare workers, most of whom are women, also face heightened risk of exposure to COVID-19, as they have extended contact with patients, frequently run errands for patients, and rely on public transportation (Sterling et al. 2020). High numbers of infections among women healthcare workers were also observed in past epidemics such as Ebola, H1N1, and the 1918 influenza (Balkhy, El-Saed, and Sallah 2010; Godderis and Rossiter 2013; Penfold and Magee 2020).
4.2. Access to and use of personal protective equipment
Insufficient access to personal protective equipment was a widespread problem, especially during the early phases of the pandemic. While women healthcare workers as a whole are affected by the lack of personal protective equipment, some are affected more than others. For example, evidence suggests that health and social care workers in community settings often have greater difficulties accessing personal protective equipment, compared to those in acute care (Penfold and Magee 2020). Additionally, many home healthcare workers in New York said that their agencies did not provide them with adequate personal protective equipment (Sterling et al. 2020).
Besides lacking personal protective equipment, women healthcare workers also reported that personal protective equipment fit poorly and that they had difficulties finding personal protective equipment of the right size (Penfold and Magee 2020). This could be due to the fact that personal protective equipment was largely designed based on the body sizes of, “white American military male recruits during the 1950s to 1970s” (Ahmed and Dumanski 2020: 982). Gender bias in the design of personal protective equipment seems to have persisted: in a study on the effect of a recent design change in a 3 M N95 respirator, women were 5.5 times more likely to fail the fit test for the new model (1870), compared to the old model (1870+). In contrast, men did not experience differences in fit between both models (Sandkovsky et al. 2017). Healthcare workers who wear head coverings, such as hijabs and turbans, may also experience difficulties with personal protective equipment fit (Bourgeault et al. 2020). Furthermore, the use of personal protective equipment can also lead to skin problems. In Turkey, women healthcare workers reported a higher prevalence of skin problems due to the use of personal protective equipment during COVID-19 compared to men (Daye, Cihan, and Durduran 2020).
Some women healthcare workers also reported receiving less information about personal protective equipment, which could reduce effective use and increase fear of infection. In a United Kingdom study of 2075 medical students and interim Foundation Year 1 doctors during COVID-19, only 41 percent of women reported receiving sufficient personal protective equipment information compared to 47 percent of men. The disparities were starker between racial and ethnic groups: only 33 percent of racial and ethnic minorities reported receiving sufficient personal protective equipment information compared to 47 percent of White participants (Norton et al. 2020). Lack of information about personal protective equipment is associated with higher levels of COVID-19-related anxiety. In the same study, both women and those without adequate personal protective equipment information were more anxious about contracting COVID-19. Participants were asked to rate whether they agreed or disagreed with the statement “I am worried that I would catch COVID-19″ on a scale of 0 to 4 (with 0 being “strongly disagree” and 4 “strongly agree”), with a higher score indicating greater anxiety about catching COVID-19. Women gave a mean score of 2.30 out of 4.0 compared to 2.11 for men. Meanwhile, those who reported receiving inadequate personal protective equipment information had a mean score of 2.32 compared to 2.17 for those who received adequate information (Norton et al. 2020).
4.3. Workload and staffing during times of crisis
Over the first year of the COVID-19 pandemic, the workload of healthcare workers increased exponentially. In a study of physicians and other healthcare workers in Italy, women were more likely to report that their workload had increased during the pandemic (mean increase, 0.38 [0.06–0.69] P=0.018) (Felice et al. 2020). Women's workload may not just increase in terms of paid work. A United States study of emergency department staff found that women were more likely to predict being absent from work during a pandemic compared to men, with higher levels of predicted absenteeism among women linked to their caregiving responsibilities at home (Mercer et al. 2014). Having to take on increased unpaid care work due to COVID-19 related childcare and school interruptions impacts women's paid work (Felice et al. 2020).
4.4. Negative effects on career and leadership potential
Women are under-represented in senior leadership positions within health systems around the world (Bennett, James, and Kelly 2020; Penfold and Magee 2020). Women's lack of participation in decision-making could lead to COVID-19 policies that do not account for women's needs, such as mandatory night shifts and work during weekends (Jones et al. 2020). Furthermore, the voices of women, especially those from low- and middle-income countries, are largely excluded from global-level responses to COVID-19, given that they constitute only 5 percent of leadership within global health organizations (Ryan and El Ayadi 2020).
The pandemic may further exacerbate women's underrepresentation in leadership and hinder their career progression. During COVID-19, women healthcare workers find it difficult to remain involved in leadership, administration, or research due to increased caregiving responsibilities (Jones et al. 2020). Some may even have to take unpaid leave to care for family members, which may widen the gender pay gap (Jones et al. 2020). Additionally, well-meaning efforts to help women healthcare workers cope during the pandemic, such as reducing their work hours and leadership roles, can further impede their career advancement (Brubaker 2020). While COVID-19 and other crises have led to more research opportunities, women healthcare workers may miss out on these opportunities due to caregiving responsibilities (Brubaker 2020).
4.5. Work-life balance and duty to provide care
Women healthcare workers with partners who are working full-time report spending a higher amount of time on unpaid care work such as cleaning, cooking, and childcare compared to their male partners (Jones et al. 2020). The burden of unpaid care work can adversely impact women's mental health. In China, women healthcare workers who were caregivers to two or more children were found to be more susceptible to stress, depression, and anxiety during COVID-19, compared to those who had one or no child (Li et al. 2020). This could be due to increased family responsibilities, unequal division of labor at home, and resulting exhaustion (Li et al. 2020; López-Atanes et al. 2020).
Women's double burden, at home and at work, can also result in guilt. During the COVID-19 pandemic, women healthcare workers in Wuhan, China, felt torn between caring for dependents and working, particularly as their work increased the risk of infection for dependents (Zhu et al. 2020). Such feelings of guilt are heightened by the duty women healthcare workers feel towards patients and to contribute to the pandemic response (Chowdhry 2020).
4.6. Economic insecurity
Women healthcare workers largely occupy the lower rungs of the health workforce and are often poorly paid and undervalued (van Daalen et al. 2020). The pandemic has exacerbated their economic insecurity, as they may be forced to take more unpaid leave to juggle caregiving responsibilities (Jones et al. 2020). Among women healthcare workers, some groups face even greater economic insecurity. For example, home healthcare workers in New York, who are predominately older women, people of color, and migrants were already earning minimum wage before the COVID-19 pandemic, with one in six living below the poverty line (Sterling et al. 2020). The pandemic has further eroded their income due to cancellations from patients who fear contracting the virus. The workers themselves were also torn between their financial need and fears for their safety when contemplating whether to continue caring for high-risk or infected patients (Sterling et al. 2020). For some, staying home was not an option because they needed to work a certain number of hours to maintain government benefits. Additionally, home healthcare workers in some parts of the United states are not designated as “essential workers”, making them ineligible for pandemic benefits such as child care and paid sick leave (Sterling et al. 2020). This example shows how certain women-dominated healthcare occupations face greater economic insecurity due to precarious employment terms and marginalized positions within the health system.
4.7. Increased mental health burden
Overall, evidence shows that women healthcare workers generally experienced a greater mental health toll during the COVID-19 pandemic, compared to healthcare workers who were men. Some of the mental health conditions covered in the literature include anxiety, depression, stress, sleep problems, burnout, trauma, and post-traumatic stress.
In most countries studied, compared to men women healthcare workers experienced greater levels of anxiety, depression, and stress during the COVID-19 pandemic. However, this trend was not seen across all countries—in some countries, there were no significant gender differences in anxiety, depression, and stress levels. For example, in a Greek study, over half of nurses reported experiencing moderate to high levels of stress during COVID-19, but there was no difference in stress levels between men and women nurses (Tselebis et al. 2020). In terms of anxiety and depression, separate studies in China, Turkey, France, and Mali during COVID-19 showed that women health workers have higher levels of depression and anxiety symptoms, compared to men (Araç and Dönmezdil 2020; Azoulay, Cariou, et al. 2020; Han et al. 2020; Kurt, Deveci, and Oguzoncul 2020; J. Lai et al. 2020; Sagaon-Teyssier et al. 2020; Zhu et al. 2020). For example, in Wuhan, China, women healthcare workers were 75 percent more likely to experience depression during COVID-19 compared to men (Zhu et al. 2020). Meanwhile, in Ireland, women healthcare workers reported higher levels of anxiety symptoms during COVID-19 compared to men, but there was no significant gender difference in depression symptoms (Corbett et al. 2020). With regards to stress, separate studies in Turkey and India found that women healthcare workers experienced greater levels of stress during COVID-19 (Grover et al. 2020; Torun and Torun 2020).
Levels of trauma, post-traumatic stress symptoms, and insomnia were also higher among women healthcare workers during the COVID-19 pandemic. In a study of 12,596 nurses in mainland China and Taiwan during COVID-19, compared to men women were 34 percent more likely to experience traumatic responses (Chen et al. 2020). Meanwhile, in Greece, women healthcare workers were four times more likely to meet the criteria for a probable diagnosis of post-traumatic stress disorder during COVID-19 compared to men (Blekas et al. 2020). With regard to insomnia, separate studies in China, Mali, and Greece showed that women healthcare workers are at a greater risk of insomnia or sleep problems during COVID-19 (Blekas et al. 2020; J. Lai et al. 2020; Sagaon-Teyssier et al. 2020). In a Mali study of workers at community-based HIV care centers during COVID-19, women workers were 53 percent more likely to experience insomnia compared to men (Sagaon-Teyssier et al. 2020).
Mental health is also impacted by the intersection of additional stratifiers and stressors, including occupation, number of dependents, age, and socioeconomic status. Nurses, for example, have been shown to have decreased resilience compared to physicians during crises. Studies suggest that this may be due to the higher autonomy and independence physicians experience in their work environments, which leads to more resilience (Sanchez-Zaballos and Mosteiro-Diaz 2020). However, this may also be due to financial differences. Similar patterns are found within midwifery (Shorey and Chan 2020). In China, nurses reported more severe symptoms of anxiety, depression, insomnia, and distress during COVID-19, compared to physicians (J. Lai et al. 2020). For example, in a Chinese study of 1257 healthcare workers during COVID-19, 7.1% of nurses reported severe symptoms of depression, compared to 4.9% of physicians (J. Lai et al. 2020). Meanwhile, in Mali, having more dependents was associated with an increased risk of depression among healthcare workers during COVID-19 (Sagaon-Teyssier et al. 2020). And in Spain, younger age was linked to increased distress among healthcare workers during COVID-19 (Rodríguez-Rey, Garrido-Hernansaiz, and Bueno-Guerra 2020). In addition, a systematic review of the psychological impact of COVID-19 found that lower socioeconomic status increased the risk of psychological impact among healthcare workers (Luo et al. 2020). Conversely, the review found that family support reduced the risk of psychological distress (Luo et al. 2020), which is consistent with findings from studies of previous epidemics (Bahat et al. 2020).
The high mental health toll among women healthcare workers can partially be explained by their fear of contracting the virus and transmitting it to family and friends (Araç and Dönmezdil 2020). This fear is heightened by their close contact with patients (Hacimusalar et al. 2020; Sterling et al. 2020), caregiving roles, and uncertainties about the virus (Araç and Dönmezdil 2020). Due to fear of transmitting the virus, women healthcare workers may avoid interacting with family and friends beyond their household, leading to isolation, which further increases their risk of mental ill-health. In China, nurses who were concerned about others contracting the disease avoided contact with social networks and experienced higher levels of anxiety and depression (Han et al. 2020). In some instances, women may not be able to avoid contact with their families, due to care responsibilities at home. This could lead to feelings of guilt for potentially placing loved ones at risk of infection (Jones et al. 2020).
Increased mental health burden among women also magnifies their risk of burnout. A study of 12,596 nurses in Taiwan and mainland China during COVID-19 found that women were 30 percent more likely to experience emotional exhaustion—a component of burnout—compared to men (Chen et al. 2020). Meanwhile, another study of 1001 intensive care unit physicians from various countries during COVID-19, also found that women experienced higher rates of severe burnout (Azoulay, De Waele, et al. 2020). The higher levels of burnout among women healthcare workers could be due to a compounding increase in unpaid care work at home, as well as fear of infection (Jones et al. 2020; López-Atanes et al. 2020; Ryan, El Ayadi, 2020). Another contributor to burnout is moral distress, which occurs when workplace constraints hinder health care workers from providing a level of care that they deem to be acceptable and ethical. In the context of COVID-19, healthcare workers may be forced to make morally fraught decisions, such as the triaging of patients, due to heavy patient load and scarce resources. In the a study of intensive care unit physicians during COVID-19, physicians’ perception of a poor ethical climate in their intensive care units was a predictor of severe burnout (Azoulay, De Waele, et al. 2020).
4.8. Recommendations to address negative impacts of crises on women healthcare workers
There are a number of measures which could be implemented to address the gendered impact of crises on women healthcare workers highlighted in the literature. These include: mental health support programs, economic support, childcare, inclusion in decision-making, and support for women's careers.
Within our scoping review, we felt it was important to extract and summarize recommendations based on the studies’ findings in order to support action against the key issues identified. However, as the scoping review did not do a formal assessment of the quality of the articles (and associated research) included, there is a need to assess the basis for these recommendations before adopting them. Those interested in adopting these recommendations can refer to back to the individual research to assess quality, including the evidence-based nature of the recommendations made.
4.9. Mental health support for healthcare workers
As women fill the majority of frontline positions within the health system, there is a need for gender-responsive interventions that specifically meet their mental health needs (Samouei et al. 2019). Evidence indicates that supporting women healthcare workers' mental health during crises is an important factor for recovering from disasters (Samouei et al. 2019). Samouei et al. identify five priorities for addressing the mental health of women healthcare workers during crises: (1) Awareness of crisis and management of adverse behavior and circumstances (emergency decision-making, self-management during disasters, logical behavioural stability); (2) Social security; (3) Tackling harmful behaviors during disasters (violence against women, stigma, exploitation of unprotected women); 4) Policies that address the status of women during disasters (mental health policies for women who are at risk, transparency in policy-making, making space for women in decision-making for policies); and 5) Establishing appropriate rules during disasters (correct implementation of said rules, allowing women to participate in rule development, input from women in disaster-related organizations, insurance for women before the disasters) (Samouei et al. 2019).
There are different avenues available for the development of mental support programs. Psychological well-being training empowers healthcare workers by providing them with tools to manage their emotions, feelings, thoughts, and behaviors (Rodriguez-Rey et al. 2020). Tele-counselling has shown promising results in improvements of mental health outcomes with healthcare workers (Shorey and Chan 2020). This method is useful during pandemic crises such as COVID-19, where social distancing is required. Short (around 5 minutes) mindfulness therapy and resilience workshops have been shown to be effective in decreasing levels of stress, anxiety, and burnout (Shorey and Chan 2020). Specialized treatments with pharmacotherapy options, such as anti-depression and anxiety medications, are also at times recommended (Arac and Donmezdil 2020). Even where support is available, healthcare workers may prioritize their work over their wellbeing, and so a proactive approach where psychologists approach the workers with their services may increase accessibility and engagement (Rodriguez-Rey, Garrido-Hernansaiz, and Bueno-Guerra 2020). National networks of psychological support with expertise in crisis intervention can be made available through human resources departments for healthcare workers (Rodriguez-Rey et al. 2020).
Technology has provided many avenues to support healthcare workers during times of need. For example, an application called PsySTART was designed to help clinicians prevent disaster induced post-tramatic stress disorder. Clinicians use the application to track factors related to post-tramatic stress disorder both during and after crises (Kuehn 2020). This information is then used to develop a personal resilience plan, as well as access local resources for support (Kuehn 2020). Similarly, the American College of Cardiology created an online Clinician Wellbeing Portal which houses resources for clinicians coping with COVID-19 stress (Kuehn 2020). The United States National Center for post-tramatic stress disorder also has an application-based post-tramatic stress disorder Coach, and the United States Department of Health and Human Services has a 24–7 Disaster Distress Helpline, which is available to any person who requires it, not just healthcare workers (Kuehn 2020). During the initial COVID-19 outbreak, China implemented psychological assistance services which included telephone, internet, and application-based counseling at the community and national level (Luo et al. 2020). Korea, Singapore, and Italy also rolled out psychological support interventions for those at high risk of being impacted by the pandemic (Luo et al. 2020).
Appropriate training is crucial for healthcare workers to reduce negative mental health impacts during crises. Literature shows that healthcare workers desire more organizational support in terms of training and education (Rodriguez-Rey et al. 2020; Scuri et al. 2019). Emotional training on coping with emergencies is also an important aspect of managing crises. Educating healthcare workers on palliative care and how to cope with grief can mitigate negative mental health impacts (Rodriguez-Rey et al. 2020). Overall, using training as a preventive measure can have a much higher impact on overall resilience than providing training during the disaster itself (Scuri et al. 2019).
4.10. Economic support
Economic support is important during times of crisis. As an example, during the COVID-19 pandemic the Society of Hospital Medicine established partnerships with businesses to provide discounted hotel rooms for healthcare workers so they could isolate without putting housemates at risk (Jones et al. 2020). Additionally, healthcare workers need to be fairly compensated, especially during crises. Those who become ill during crises require hazard pay, paid sick leave, insurance supplements, and workers compensation (Jones et al. 2020). This is even more important for women healthcare workers, as disasters will exacerbate already existing wage gaps. In the long term recovery phase, there should be salary corrections and ongoing monitoring of financial need (Jones et al. 2020).
4.11. Support for dependents
The issue of requiring support for dependents of women healthcare workers is a prevalent one (Mercer et al. 2014). As both being a woman and being responsible for dependents in a household are associated with increased absenteeism during times of disaster, hospital disaster planners should focus on providing resources for those with dependents on site, such as childcare or shelter if required (Mercer et al. 2014). If this is not possible, then there should be customized training and education for those with dependents for personal disaster planning (Mercer et al. 2014). This would entail helping healthcare workers to identify and address the potential gaps in their caretaking responsibilities, as well as providing them with tools to communicate with their families about their potential absence during a disaster (Mercer et al. 2014). This includes addressing the possibility of work and home absences due to the disaster, as well as caregiving gaps (Mercer et al. 2014).
4.12. Involving women healthcare workers in decision-making
While women healthcare workers are on the front line, they often lack representation in decision-making. It is important that women healthcare workers are involved in decision-making on such things as childcare accommodations, hazard pay, shift logistics, advancement opportunities, and hiring protocols (Jones et al. 2020). This is integral as gender gaps can be exacerbated during crises, meaning that women need the space to voice their needs in order to ensure specific and relevant resources available during times of disaster (Jones et al. 2020). Furthermore, in terms of disaster planning, including women in decision-making increases the likelihood that the needs of women will be considered. Inclusion on key task forces that address allocation of personal protective equipment, design and implementation of new processes, wellness initiatives, and emergency childcare are all opportunities for decision-making (Jones et al. 2020).
A recent study indicated that countries with women in positions of leadership had six times fewer deaths from the COVID-19 pandemic than those being led by men (van Daalen et al. 2020). Countries where women lead tend to have institutions that are more prepared for inclusive governance, which influences their response to the pandemic (van Daalen et al. 2020). As we increase women representation in leadership, there is disruption of the norm, introduction of novel opinions, higher quality of monitoring, and more effective risk management (van Daalen et al. 2020).
4.13. Supporting women's careers
During crisis, already existing gender disparities are exacerbated. It is therefore important that there is tracking of indicators of wellness, burnout, and productivity (Jones et al. 2020). There may be disproportionate derailing of women on the path to promotions during these times. This indicates a need for extending deadlines for promotions, as well as introducing new metrics to determine progress during performance review (Jones et al. 2020). Furthermore, there should be recognition of women working at higher capacity in clinical or administration areas (Jones et al. 2020). This is integral as women may be taking initiative in the workplace during times of disaster that is not in their job description and should be recognized. This recognition can provide avenues for more fair compensation and career advancement opportunities (Jones et al. 2020).
5. Discussion
5.1. Impacts of health crises on women healthcare workers
This review identified numerous impacts of health crises on women healthcare workers, as well as measures to address the challenges they face. Women healthcare workers were found to experience a higher risk of exposure and infection during disease outbreaks (Balkhy et al. 2010; Chaudhary 2020; Godderis and Rossiter 2013; Hacimusalar et al. 2020; King et al. 2020; Penfold and Magee 2020), barriers to accessing personal protective equipment (van Daalen et al. 2020; Sterling et al. 2020), increased workloads (Felice et al. 2020; Mercer et al. 2014), and decreased leadership and decision-making opportunities (Brubaker 2020; Jones et al. 2020). Women healthcare workers also experienced increased caregiving responsibilities in the home when schools and childcare supports were restricted due to health crises (Jones et al. 2020). Numerous studies also confirmed higher rates of mental health conditions among women healthcare workers, including symptoms of depression, anxiety, and post-traumatic stress disorder (Araç and Dönmezdil 2020; Azoulay, Cariou, et al. 2020; Han et al. 2020; Kurt et al. 2020; J. Lai et al. 2020; Sagaon-Teyssier et al. 2020; Zhu et al. 2020).
The high number of articles focused on mental health, particularly in comparison to physical health, is notable. The focus on mental health is positive, as normalizing mental health may lead to increased attention to mental health interventions, which have been largely stigmatized in the past. However, many interventions documented in the literature are targeted at individuals, such as workshops, training, and counselling. Such interventions place responsibility for selfcare on women healthcare workers with already increased workload and care responsibilities, who may not have the time or energy to take advantage of such opportunities. There is a need for further piloting of systemic or structural interventions that address drivers of poor mental health and build resilience across the health system.
The increased caregiving burden faced by women healthcare workers was a major theme in the literature which impacted multiple dimensions of their health, wellbeing, and livelihoods (Daryanti Saragih et al. 2021). Increased caregiving burdens, for example, were found to negatively impact mental health, risk of COVID-19 infection, income, and career advancement. Given its multidimensional impact, interventions in this area are likely to lead to substantial gains. However, as noted above, it is important that these interventions are not focused only on the individual or family, but are instead at institution and health system levels. For example, while normative change is important, such as reducing women's caregiving burden by increasing men's involvement in caregiving, this type of change takes a long time and is beyond the control of health systems actors. Instead, interventions related to easing women's burden, such as flexible working hours, subsidized childcare, on the job childcare, parental leave, and equal pay are important.
5.2. Lack of attention to gender prior to COVID-19
While our literature review included a range of health crises, such as natural disasters, and various epidemics and pandemics, the majority of the articles included were centered around the COVID-19 pandemic. This is aligned with the finding that the majority of the articles were published in 2020, despite our search extending as far back as 2010. COVID-19 can thus be viewed as a focusing event that has substantially increased the amount of published literature examining the gendered impacts of health crises on women healthcare workers.
While this presents a crucial opportunity to increase our understanding of the gender disparities that play out during health crises and how to better support women healthcare workers, it is also evidence of the lack of previous attention paid to gender and the health workforce. Given that women make up 75% of the health and social care workforce and are more likely to be on the frontlines during a crisis, lack of previous research demonstrates a significant bias within the literature and the lack of attention paid to potential gender differences. As our review excluded articles that did not disaggregate by sex or gender (i.e. reported on healthcare workers without distinguishing between men and women), we do not know how these numbers compare to the broader literature on the experiences of healthcare workers during crises in general. Any studies reporting on the experiences of healthcare workers, whether during crises or not, that do not disaggregate their data by sex or gender are ignoring the gendered nature of the health workforce (Betron et al. 2019; Boniol et al. 2019; Newman 2014). Such studies will also by default fail to consider the unique experiences of women, men or gender diverse healthcare workers, making any gender specific experiences invisible. When something is not researched or lacks data, it is deprioritized by the very fact that it “doesn't exist”. As a result, related solutions in the form of changes to policies, processes, or procedures are not developed or implemented as barriers, gaps, or inequities remain.
5.3. Increased attention to experience of women healthcare workers in high-income countries
COVID-19 has drawn attention to the gendered nature of the health workforce like never before. This increased attention may be due to the global nature of the pandemic, compared to past crises, and the fact that high-income countries were also, and initially most acutely, impacted. Of the 76 articles included in this review, the majority took place in North American and European countries, followed by Asian countries. There were only three studies from Latin American countries, three from Middle Eastern countries, and two from African countries. This highlights a significant dearth in the research examining the experiences of women healthcare workers during health crises in developing regions and countries. The lack of articles on the experiences of women healthcare workers during Ebola and Zika, which are two recent pandemics, is notable as these pandemics occurred in low- and middle-income countries where women healthcare workers were predominately affected. Lack of consideration of the experiences of women in low and middle income countries demonstrates continued inequities in global and public health research.
5.4. Understanding the causes of differential impacts
Primary research articles included in this study either centered around the experiences of women healthcare workers or reported gender-disaggregated data to enable a comparison between men and women. The presentation of gender-disaggregated data is an important first step, but the continued binary of men and women renders invisible the experiences of gender diverse people who identify differently. While we did not specifically search for studies on gender diverse health care workers, none of the studies included mentioned this population group. Moreover, most articles did not analyze the reasons behind the differential impacts of the pandemic based on gender and the intersection of different factors and stratifiers. The findings also demonstrated a substantial lack of intersectional analyses. It is important to understand how healthcare workers from racial minority backgrounds’ experiences may differ from the racial majority. And as we know that gender intersects with other social stratifiers, including race, ethnicity, age, socioeconomic status, and disability, to influence individual experiences of marginalization, it is likely that many of the issues raised in this review may be differentially and/or disproportionately experienced or felt by sub-groups of women healthcare workers. Further research is needed to better understand these dynamics.
6. Conclusion
Findings point to a number of important recommendations to better support women healthcare workers, including workplace mental health support, economic assistance to counteract widening pay gaps, and strategies to support families in their caregiving duties (Jones et al. 2020; Mann et al. 2020; Mercer et al. 2014; Samouei et al. 2019). Additionally, strategies that support and advance women's careers and increase women's representation in leadership are an important way to combat gender-blindness in healthcare systems and ensure that the needs of women healthcare workers are addressed during the COVID-19 pandemic and in future health crises (van Daalen et al. 2020; Jones et al. 2020).
Recommendations can be divided into those that address downstream impacts and those that address upstream impacts. Recommendations to address downstream impacts include access to better fitting personal protective equipment (and personal protective equipment in general), mental health services, and childcare services. Meanwhile, recommendations to address upstream impacts include integrated mental health and resilience training before a crisis occurs, closing gender wage or opportunity gaps, involving women in decision-making, as well as normative change around women's roles within the home and health system.
The increased attention to COVID-19 provides an opportunity to apply any learnings to other crises. It is important that we question why gender disparities within other crises have not received as much attention. COVID-19 also provides us with an opportunity to develop gender-responsive crisis preparedness plans within the health sector. Without consideration of gender, crises will continue to exacerbate existing gender inequities, resulting in disproportionately negative impacts on women healthcare workers. Further research is needed to better understand how to develop truly gender-responsive health systems that can withstand future health emergencies.
What is already known
-
•
Women make up the majority of the health workforce.
-
•
Healthcare workers are at high risk of experiencing negative impacts from crises such as COVID-19.
-
•
The negative impacts of COVID-19 on healthcare workers is a significant issue that needs to be addressed.
What this paper adds
-
•
Women healthcare workers are uniquely impacted by crises. These impacts include barriers to accessing personal protective equipment, decreased leadership and decision-making opportunities, increased caregiving responsibilities and higher rates of mental ill-health. A gender lens is needed to understand these impacts and why they occur.
-
•
There has been a lack of attention to gender and the health workforce during times of crises prior to COVID-19 and there is a substantial gap in research around the experiences of women healthcare workers in low- and middle-income countries during times of crisis. Increased awareness of the gendered effects of COVID-19 provides an opportunity to apply learnings to current crises responses and future prepardness efforts.
-
•
Further research is needed to better understand how to develop truly gender-responsive health systems that can withstand future health emergencies and support women healthcare workers’ health and wellbeing.
Funding statement
This scoping review was supported by the British Columbia Women's Health Foundation.(Fig. 1)
Fig. 1.
Scoping Review Search Process.
Declaration of Competing Interest
None
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ijnsa.2022.100066.
Appendix. Supplementary materials
References
- Ahmed Sofia B., Dumanski Sandra M. Sex, Gender and COVID-19: A Call to Action. Can. J. Public Health. 2020;111(6):980–983. doi: 10.17269/s41997-020-00417-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arac Songul, Donmezdil Suleyman. Investigation of Mental Health among Hospital Workers in the COVID-19 Pandemic: A Cross-Sectional Study. Sao Paulo Med. J. = Revista Paulista de Medicina. 2020;138(5):433–440. doi: 10.1590/1516-3180.2020.0272.R3.21072020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araç Songül, Dönmezdil Süleyman. Investigation of Mental Health among Hospital Workers in the COVID-19 Pandemic: A Cross-Sectional Study. Sao Paulo Med. J. 2020;138(5):433–440. doi: 10.1590/1516-3180.2020.0272.R3.21072020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azoulay Elie, Cariou Alain, Bruneel Fabrice, Demoule Alexandre, Kouatchet Achille, Reuter Danielle, Souppart Virginie, Combes Alain, Klouche Kada, Argaud Laurent, Barbier François, Jourdain Mercé, Reignier Jean, Papazian Laurent, Guidet Bertrand, Géri Guillaume, Resche-Rigon Matthieu, Guisset Olivier, Labbé Vincent, Mégarbane Bruno, Meersch Guillaume Van Der, Guitton Christophe, Friedman Diane, Pochard Frédéric, Darmon Michael, Kentish-Barnes Nancy. Symptoms of Anxiety, Depression, and Peritraumatic Dissociation in Critical Care Clinicians Managing Patients with COVID-19. A Cross-Sectional Study. Am. J. Respir. Crit. Care Med. 2020;202(10):1388–1398. doi: 10.1164/rccm.202006-2568OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azoulay Elie, De Waele Jan, Ferrer Ricard, Staudinger Thomas, Borkowska Marta, Povoa Pedro, Iliopoulou Katerina, Artigas Antonio, Schaller Stefan J., Shankar Hari Manu, Pellegrini Mariangela, Darmon Michael, Kesecioglu Jozef, Cecconi Maurizio. Symptoms of Burnout in Intensive Care Unit Specialists Facing the COVID-19 Outbreak. Ann. Intens. Care. 2020;10(1) doi: 10.1186/s13613-020-00722-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahat Pınar Yalçın, Aldıkaçtıoğlu Merve, Ayşegül Talmaç, Topbas Nura F., Ozan Selcuki, Ibrahim Karadeniz. Evaluating the Effects of the COVID - 19 Pandemic on the Physical and Mental Well - Being of Obstetricians and Gynecologists in Turkey. 2020:67–73. doi: 10.1002/ijgo.13287. August. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balkhy Hanan H., El-Saed Aiman, Sallah Mahmoud. Epidemiology of H1N1 (2009) Influenza among Healthcare Workers in a Tertiary Care Center in Saudi Arabia: A 6-Month Surveillance Study. Infect. Control Hosp. Epidemiol. 2010;31(10):1004–1010. doi: 10.1086/656241. [DOI] [PubMed] [Google Scholar]
- Bennett Clare L., James Alison H., Kelly Daniel. Beyond Tropes: Towards a New Image of Nursing in the Wake of COVID-19. J. Clin. Nurs. (John Wiley & Sons, Inc.) 2020;29(15/16):2753–2755. doi: 10.1111/jocn.15346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betron Myra, Bourgeault Ivy, Manzoor Mehr, Paulino Ema, Steege Rosalind, Thompson Kelly, Wuliji Tana. Time for Gender-Transformative Change in the Health Workforce. Lancet North Am. Ed. 2019;393(10171):e25–e26. doi: 10.1016/S0140-6736(19)30208-9. [DOI] [PubMed] [Google Scholar]
- BCWHF . British Columbia Women's Health Foundation; 2021. Invisible No More: Inequities faced by Women Healthcare workers, Especially During the COVID-19 pandemic, + Recommendations For Action.https://www.bcwomensfoundation.org/invisiblenomore/ Date Accessed: 12.20.21. [Google Scholar]
- Blekas Apostolos, Voitsidis Panteleimon, Athanasiadou Maria, Parlapani Eleni, Chatzigeorgiou Aliki F., Skoupra Marina, Syngelakis Markos, Holeva Vasiliki, Diakogiannis Ioannis. COVID-19: PTSD Symptoms in Greek Health Care Professionals. Psychological Trauma : Theory, Research, Practice and Policy. 2020;12(7):812–819. doi: 10.1037/tra0000914. [DOI] [PubMed] [Google Scholar]
- Boniol Mathieu, McIsaac Michelle, Xu Lihui, Wuliji Tana, Diallo Khassoum, Campbell Jim. World Health Organization; 2019. Gender Equity in the Health Workforce: Analysis of 104 Countries. [Google Scholar]
- Bourgeault Ivy Lynn, Maier Claudia B., Dieleman Marjolein, Ball Jane, MacKenzie Adrian, Nancarrow Susan, Nigenda Gustavo, Sidat Mohsin. The COVID-19 Pandemic Presents an Opportunity to Develop More Sustainable Health Workforces. Human Resources for Health. 2020;18(1):83. doi: 10.1186/s12960-020-00529-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brubaker Linda. Women Physicians and the COVID-19 Pandemic. JAMA. 2020;324(9):835–836. doi: 10.1001/jama.2020.14797. [DOI] [PubMed] [Google Scholar]
- Chaudhary Anurag. Women in COVID Pandemic: Beyond Morbidity and Mortality. Ind. J. Cardiovas. Dis. Women WINCARS. 2020;5(03):274–277. [Google Scholar]
- Chen Ruey, Sun Chao, Chen Jian Jun, Jen Hsiu Ju, Kang Xiao Linda, Kao Ching Chiu, Chou Kuei Ru. A Large-Scale Survey on Trauma, Burnout, and Posttraumatic Growth among Nurses during the COVID-19 Pandemic. Int. J. Ment. Health Nurs. 2020;30(1):102–116. doi: 10.1111/inm.12796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhry Shilpa Mukunda. Trying To Do It All: Being a Physician-Mother during the COVID-19 Pandemic. J. Palliat. Med. 2020;23(5):731–732. doi: 10.1089/jpm.2020.0182. [DOI] [PubMed] [Google Scholar]
- Corbett Gillian A., Milne Sarah J., Mohan Suruchi, Reagu Shuja, Farrell Tom, Lindow Stephen W., Hehir Mark P., Michael P.O’Connell. Anxiety and Depression Scores in Maternity Healthcare Workers during the Covid-19 Pandemic. Int. J. Gyn. Obs. 2020;151(2):297–298. doi: 10.1002/ijgo.13279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Daalen Kim Robin, Bajnoczki Csongor, Chowdhury Maisoon, Dada Sara, Khorsand Parnian, Socha Anna, Lal Arush, Jung Laura, Alqodmani Lujain, Torres Irene, Ouedraogo Samiratou, Mahmud Amina Jama, Dhatt Roopa, Phelan Alexandra, Rajan Dheepa. Symptoms of a Broken System: The Gender Gaps in COVID-19 Decision-Making. BMJ Global Health. 2020;5(10) doi: 10.1136/bmjgh-2020-003549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saragih Ita Daryanti, Tonapa Santo Imanuel, Saragih Ice Septriani, Advani Shailesh, Batubara Sakti Oktaria, Suarilah Ira, Lin Chia-Ju. Global Prevalence of Mental Health Problems among Healthcare Workers during the Covid-19 Pandemic: A Systematic Review and Meta-Analysis. Int. J. Nurs. Stud. 2021;121 doi: 10.1016/j.ijnurstu.2021.104002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daye Munise, Gökşin Cihan Fatma, Durduran Yasemin. Evaluation of Skin Problems and Dermatology Life Quality Index in Health Care Workers Who Use Personal Protection Measures during COVID-19 Pandemic. Dermatol. Ther. 2020;33(6) doi: 10.1111/dth.14346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felice Carla, Luca Di Tanna Gian, Zanus Giacomo, Grossi Ugo. Impact of COVID-19 Outbreak on Healthcare Workers in Italy: Results from a National E-Survey. J. Community Health. 2020;45(4):675–683. doi: 10.1007/s10900-020-00845-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godderis Rebecca, Rossiter Kate. ‘If You Have a Soul, You Will Volunteer at Once’: Gendered Expectations of Duty to Care during Pandemics. Sociol. Health Illn. 2013;35(2):304–308. doi: 10.1111/j.1467-9566.2012.01495.x. [DOI] [PubMed] [Google Scholar]
- Grover Rohini, Dua Pratham, Juneja Supreet, Chauhan Lokesh, Agarwal Pradeep, Khurana Ashi. ‘Depression, Anxiety and Stress’ in a Cohort of Registered Practicing Ophthalmic Surgeons, Post Lockdown during COVID-19 Pandemic in India. Ophthalmic Epidemiol. 2020;00(00):1–8. doi: 10.1080/09286586.2020.1846757. [DOI] [PubMed] [Google Scholar]
- Hacimusalar Yunus, Civan Kahve Aybeniz, Burak Yasar Alisan, Aydin Mehmet Sinan. Anxiety and Hopelessness Levels in COVID-19 Pandemic: A Comparative Study of Healthcare Professionals and Other Community Sample in Turkey. J. Psychiatr. Res. 2020;129:181–188. doi: 10.1016/j.jpsychires.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han Lin, Wong Frances Kam Yuet, She Dong Li M., Li Si Yan, Yang Yun Fang, Jiang Meng Yao, Ruan Yue, Su Qian, Ma Yuxia, Chung Loretta Yuet Foon. Anxiety and Depression of Nurses in a North West Province in China During the Period of Novel Coronavirus Pneumonia Outbreak. J. Nurs. Scholar. 2020 doi: 10.1111/jnu.12590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones Yemisi, Durand Vanessa, Morton Kayce, Ottolini Mary, Shaughnessy Erin, Spector Nancy D., O’Toole Jennifer. Collateral Damage: How COVID-19 Is Adversely Impacting Women Physicians. J. Hosp. Med. 2020;15(8):507–509. doi: 10.12788/jhm.3470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King Tania, Hewitt Belinda, Crammond Bradley, Sutherland Georgina, Maheen Humaira, Kavanagh Anne. Reordering Gender Systems: Can COVID-19 Lead to Improved Gender Equality and Health? Lancet (London, England) 2020;396(10244):80–81. doi: 10.1016/S0140-6736(20)31418-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuehn Bridget M. Mitigating the Psychological Harm of COVID-19 Pandemic for Clinicians. Circulation. 2020;141(21):1724–1726. doi: 10.1161/CIRCULATIONAHA.120.047747. [DOI] [PubMed] [Google Scholar]
- Kurt Osman, Deveci Suleyman Erhan, Oguzoncul Ayse Ferdane. Levels of Anxiety and Depression Related to COVID-19 among Physicians: An Online Cross-Sectional Study from Turkey. Ann. Clin. Anal. Med. 2020;11(suppl 3):0–5. [Google Scholar]
- Lai Jianbo, Ma Simeng, Wang Ying, Cai Zhongxiang, Hu Jianbo, Wei Ning, Wu Jiang, Du Hui, Chen Tingting, Li Ruiting, Tan Huawei, Kang Lijun, Yao Lihua, Huang Manli, Wang Huafen, Wang Gaohua, Liu Zhongchun, Hu Shaohua. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Network Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai Xiaoquan, Wang Minghuan, Qin Chuan, Tan Li, Ran Lusen, Chen Daiqi, Zhang Han, Shang Ke, Xia Chen, Wang Shaokang, Xu Shabei, Wang Wei. Coronavirus Disease 2019 (COVID-2019) Infection Among Health Care Workers and Implications for Prevention Measures in a Tertiary Hospital in Wuhan, China. JAMA Network Open. 2020;3(5) doi: 10.1001/jamanetworkopen.2020.9666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Guo, Miao Jinfeng, Wang Hui, Xu Shabei, Sun Wenzhe, Fan Yebin, Zhang Chenyan, Zhu Suiqiang, Zhu Zhou, Wang Wei. Psychological Impact on Women Health Workers Involved in COVID-19 Outbreak in Wuhan: A Cross-Sectional Study. J. Neurol. Neurosurg. Psychiatry. 2020;91(8):895–897. doi: 10.1136/jnnp-2020-323134. [DOI] [PubMed] [Google Scholar]
- López-Atanes Mayte, Recio-Barbero María, Sáenz-Herrero Margarita. Are Women Still ‘the Other’? Gendered Mental Health Interventions for Health Care Workers in Spain During COVID-19. Psychol. Trauma: Theory, Research, Practice, and Policy. 2020;12:243–244. doi: 10.1037/tra0000751. [DOI] [PubMed] [Google Scholar]
- Luo Min, Guo Lixia, Yu Mingzhou, Jiang Wenying, Wang Haiyan. The Psychological and Mental Impact of Coronavirus Disease 2019 (COVID-19) on Medical Staff and General Public - A Systematic Review and Meta-Analysis. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann A., Dahiya A., Souza L.C., Letra A. Considerations for Pregnant Dental and Health Care Workers amid COVID-19. JDR Clin. Transl. Res. 2020;5(4):300–306. doi: 10.1177/2380084420952747. [DOI] [PubMed] [Google Scholar]
- Mercer Mary P., Ancock Benedict, Levis Joel T., Reyes Vivian. Ready or Not: Does Household Preparedness Prevent Absenteeism among Emergency Department Staff during a Disaster? Am. J. Disast. Med. 2014;9(3):221–232. doi: 10.5055/ajdm.2014.0174. [DOI] [PubMed] [Google Scholar]
- Morgan Rosemary, George Asha, Ssali Sarah, Hawkins Kate, Molyneux Sassy, Theobald Sally. How to Do (or Not to Do)… Gender Analysis in Health Systems Research. Health Policy Plan. 2016;31(8):1069–1078. doi: 10.1093/heapol/czw037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munn Zachary, Peters Micah D.J., Stern Cindy, Tufanaru Catalin, McArthur Alexa, Aromataris Edoardo. Systematic Review or Scoping Review? Guidance for Authors When Choosing between a Systematic or Scoping Review Approach. BMC Med. Res. Method. 2018;18(1):1–7. doi: 10.1186/s12874-018-0611-x. 2018 18:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman Constance. Time to Address Gender Discrimination and Inequality in the Health Workforce. Human Resources for Health. 2014;12(1):25. doi: 10.1186/1478-4491-12-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton Emma Jane, Georgiou Ioannis, Fung Alex, Nazari Armin, Bandyopadhyay Soham, Saunders Kate E.A. Personal Protective Equipment and Infection Prevention and Control: A National Survey of UK Medical Students and Interim Foundation Doctors during the COVID-19 Pandemic. J. Public Health (Oxford, England. 2020 doi: 10.1093/pubmed/fdaa187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OECD Contribution of migrant doctors and nurses to tackling COVID-19 crisis in OECD countries. 2020 https://www.oecd.org/coronavirus/policy-responses/contribution-of-migrant-doctors-and-nurses-to-tackling-covid-19-crisis-in-oecd-countries-2f7bace2/ Date Accessed: 12.30.21. [Google Scholar]
- Penfold Rose, Magee Lucia. Gender Balance in an Unprecedented Time. Future Healthc. J. 2020;7(3):212–213. doi: 10.7861/fhj.2020-0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Rey Rocío, Garrido-Hernansaiz Helena, Bueno-Guerra Nereida. Working in the Times of Covid-19. Psychological Impact of the Pandemic in Frontline Workers in Spain. Int. J. Environ. Res. Public Health. 2020;17(21):1–23. doi: 10.3390/ijerph17218149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan Nessa E., El Ayadi Alison M. A Call for a Gender-Responsive, Intersectional Approach to Address COVID-19. Global Public Health. 2020;15(9):1404–1412. doi: 10.1080/17441692.2020.1791214. [DOI] [PubMed] [Google Scholar]
- Sagaon-Teyssier Luis, Kamissoko Aliou, Yattassaye Adam, Diallo Fodié, Rojas Castro Daniela, Delabre Rosemary, Pouradier Fabrice, Maradan Gwenaëlle, Bourrelly Michel, Cissé Mamadou, Vidal Laurent, Dembélé Keïta Bintou, Spire Bruno. Assessment of Mental Health Outcomes and Associated Factors among Workers in Community-Based HIV Care Centers in the Early Stage of the COVID-19 Outbreak in Mali. Health Policy Open. 2020;1 doi: 10.1016/j.hpopen.2020.100017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samouei Rahele, Shooshtari Shahin, Bahrami Masud, Abedi Mohammad Reza, Maracy Mohammad Reza. Prioritization of Factors Related to Mental Health of Women during an Earthquake: A Qualitative Study. World J. Emerg. Med. 2019;10(3):160–168. doi: 10.5847/wjem.j.1920-8642.2019.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez-Zaballos Marta, Mosteiro-Diaz Maria Pilar. Resilience Among Professional Health Workers in Emergency Services. J. Emerg. Nurs. 2020 doi: 10.1016/j.jen.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandkovsky Uriel, Schwedhelm Michelle, Grayer Shonelle, Adelgren Emily, Rupp Mark E. Small Changes Make a Big Difference in the Fit of N95 Respirators. Open Forum Infect. Dis. 2017;4(suppl_1) [Google Scholar]
- Scuri S., Petrelli F., Nguyen T.T.C., Grappasonni I. Training to Improve Resilience and Coping to Monitor PTSD in Rescue Workers. J. Prevent. Med. Hygiene. 2019;60(1):E58–E63. doi: 10.15167/2421-4248/jpmh2019.60.1.1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shannon Geordan, Minckas Nicole, Tan Des, Haghparast-Bidgoli Hassan, Batura Neha, Mannell Jenevieve. Feminisation of the Health Workforce and Wage Conditions of Health Professions: An Exploratory Analysis. Hum. Resour. Health. 2019;17(1) doi: 10.1186/s12960-019-0406-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shorey Shefaly, Chan Valerie. Lessons from Past Epidemics and Pandemics and a Way Forward for Pregnant Women, Midwives and Nurses during COVID-19 and beyond: A Meta-Synthesis. Midwifery. 2020;90 doi: 10.1016/j.midw.2020.102821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterling Madeline R., Tseng Emily, Poon Anthony, Cho Jacklyn, Avgar Ariel C., Kern Lisa M., Ankuda Claire K., Dell Nicola. Experiences of Home Health Care Workers in New York City During the Coronavirus Disease 2019 Pandemic: A Qualitative Analysis. JAMA Intern. Med. 2020;180(11):1453–1459. doi: 10.1001/jamainternmed.2020.3930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torun Fuat, Dilek Torun Sebahat. The Psychological Impact of the COVID-19 Pandemic on Medical Students in Turkey. Pak. J. Med. Sci. 2020;36(6) doi: 10.12669/pjms.36.6.2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tselebis Athanasios, Lekka Dimitra, Sikaras Christos, Tsomaka Effrosyni, Tassopoulos Athanasios, Ilias Ioannis, Bratis Dionisios, Pachi Argyro. “Insomnia, Perceived Stress, and Family Support among Nursing Staff during the Pandemic Crisis. Healthcare. 2020;8(4):434. doi: 10.3390/healthcare8040434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenham C., Smith J., Davies S.E., Feng H., Grépin K.A., Harman S., Herten-Crabb A., Morgan R. Women Are Most Affected by Pandemics - Lessons from Past Outbreaks. Nature. 2020;583(7815) doi: 10.1038/d41586-020-02006-z. [DOI] [PubMed] [Google Scholar]
- Wenham Clare, Smith Julia, Morgan Rosemary. COVID-19: The Gendered Impacts of the Outbreak. Lancet North Am. Ed. 2020;395(10227):846–848. doi: 10.1016/S0140-6736(20)30526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; 2019. Delivered By Women, Led by Men: A Gender and Equity Analysis of the Global Health and Social Workforce.https://www.who.int/hrh/resources/health-observer24/en/ Date Accessed: 12.20.21. [Google Scholar]
- WHO . World Health Organization; 2020. State of the World's Nursing Report.https://www.who.int/publications/i/item/9789240003279 Date Accessed: 12.30.21. [Google Scholar]
- WHO Closing the leadership gap: Gender equity and leadership in the global health and care workforce. 2021 https://www.who.int/publications-detail-redirect/9789240025905 Date Accessed: 12.30.21. [Google Scholar]
- Women in Global Health Fit for Women: Improving Personal Protective Equipment (PPE) for women health & care workers. 2021 https://www.womeningh.org/fitforwomen Date Accessed: 12.30.21. [Google Scholar]
- Zhu Zhou, Xu Shabei, Wang Hui, Liu Zheng, Wu Jianhong, Li Guo, Miao Jinfeng, Zhang Chenyan, Yang Yuan, Sun Wenzhe, Zhu Suiqiang, Fan Yebin, Chen Yuxi, Hu Junbo, Liu Jihong, Wang Wei. EClinicalMedicine COVID-19 in Wuhan : Sociodemographic Characteristics and Hospital Support Measures Associated with the Immediate Psychological Impact on Healthcare Workers. EClinicalMedicine. 2020;24 doi: 10.1016/j.eclinm.2020.100443. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.