Abstract
Background
To compare different methods of three-dimensional representations, namely 3D-Print, Virtual Reality (VR)-Glasses and 3D-Display regarding the understanding of the pathology, accuracy of details, quality of the anatomical representation and technical operability and assessment of possible change in treatment in different disciplines and levels of professional experience.
Methods
Interviews were conducted with twenty physicians from the disciplines of cardiology, oral and maxillofacial surgery, orthopedic surgery, and radiology between 2018 and 2020 at the University Hospital of Basel. They were all presented with three different three-dimensional clinical cases derived from CT data from their area of expertise, one case for each method. During this, the physicians were asked for their feedback written down on a pencil and paper questionnaire.
Results
Concerning the understanding of the pathology and quality of the anatomical representation, VR-Glasses were rated best in three out of four disciplines and two out of three levels of professional experience. Regarding the accuracy of details, 3D-Display was rated best in three out of four disciplines and all levels of professional experience. As to operability, 3D-Display was consistently rated best in all levels of professional experience and all disciplines. Possible change in treatment was reported using 3D-Print in 33%, VR-Glasses in 44%, and 3D-Display in 33% of participants. Physicians with a professional experience of more than ten years reported no change in treatment using any method.
Conclusions
3D-Print, VR-Glasses, and 3D-Displays are very well accepted, and a relevant percentage of participants with less than ten years of professional work experience could imagine a possible change in treatment using any of these three-dimensional methods. Our findings challenge scientists, technicians, and physicians to further develop these methods to improve the three-dimensional understanding of pathologies and to add value to the education of young and inexperienced physicians.
Keywords: - 3D-print, - VR-glasses, - 3D-display, - 3D-screen, - three dimensional, - education
Background
Medical imaging plays a paramount role in diagnosis, particularly volumetric computed tomography (CT) and magnetic resonance imaging (MRI) with isotropic voxels [1, 2]. Many diagnoses are made not only with interpretation of axial slices, but include medical intuition gained from 2D-Displays of volumetric data sets such as multiplanar reformatted images, maximum intensity projections, and 3D volume rendering. These are collectively defined as 3D visualizations [3]. Displays using traditional flat screens do not include information of depth [4]. For example, volume rendering has made three-dimensional visualization possible, however, adding an accurate spatial impression remains challenging.
Today’s most important available options to truly convey three-dimensional images are 3D-Printing, Virtual Reality (VR)-Glasses, and 3D-Displays. First, 3D-Printing has lately received growing attention from research [5]. Using the term “3D printing” for a search in Pubmed.gov resulted in six publications in 2000, 64 publications in 2010, and astonishing 3569 results in 2020 [5, 6]. Areas of application include anatomical models, surgical guides, prosthesis, implantable or non-implantable medical devices, printing patient-specific anatomy for visualization, micro-needle, bioprinting, and pharmacoprinting [7–18]. In contrast to other technologies, segmentation of the desired structure out of the initial dataset is necessary. Several groups of specific 3D-Printing techniques exist, comprising vat photopolymerization, material jetting, binder jetting, material extrusion, powder bed fusion, sheet lamination, and directed energy deposition [3]. Often used methods for printing are material extrusion (MEX) and vat photopolymerization (VP) [19, 20]. The most economical way is MEX. For MEX, a spool of filament such as polylactic acid (PLA) or acrylonitrile butadiene styrene (ABS) is fed through a heated nozzle [21]. The nozzle then moves along pre-programmed coordinates, extruding a layer of melted material on the build plate. Layer by layer is added to create a three-dimensional model. The second mode of presentation are VR-Glasses. VR is a computer-generated simulation of a three-dimensional environment with which a person can interact using special electronic equipment. This can be combined with a wearable headset called VR-Glasses. To achieve the effect of three-dimensionality, two screens inside the VR-Glasses show two images slightly shifted in relation to each other. This results in a stereoscopic impression similar to natural viewing, where stereoscopic viewing is achieved by perceiving images through the slightly different positions of our left and right eye. In medicine, the use of VR-Glasses has been reported in three-dimensional planning of surgeries, teaching and training, non-pharmacological pain management, and in-home therapy intervention for patients with stroke [22–32]. Only recently, VR-Glasses have become more employed in diagnostics [33, 34].
The third method, a 3D-Display, creates a realistic three-dimensional impression in contrast to the already existing three-dimensional renderings on a flat-screen. 3D-Displays use stereoscopic vision, where slightly different images are sent to each eye, leading to depth perception. There are two ways to realize this. An autostereoscopic 3D-Display works as a stand-alone screen. The second possibility are stereoscopic displays with the additional wearing of special glasses. Three-dimensional displays have seldom been used in medicine due to their higher costs compared to a normal 2D-Display and the occasional experience of visual discomfort [35]. Some applications in displaying 3D ultrasound data or intracranial MR angiography have been reported [36–38]. Lastly, augmented reality (AR) receives growing interest. AR is a blend of projected computer-generated images in a real environment e.g., in an operating theater [39]. However, AR was not assessed in this study.
3D-Printing, VR-Glasses, and 3D-Displays can enhance physicians’ understanding of pathology. However, research on the subject has mostly been restricted to limited comparison of these modalities. To our knowledge, no studies are comparing the three mentioned methods. Much uncertainty still exists about the application in different disciplines and how well received the three-dimensional representations methods are in various levels of professional experience. Furthermore, existing accounts fail to investigate if physicians state a possible change in treatment using the mentioned three-dimensional methods.
To address these research gaps, this study aims:
1. To compare the three mentioned methods of 3D representations by evaluating the understanding of the pathology, accuracy of details, quality of the anatomical representation, and technical operability and investigating how well received they are in different disciplines and different levels of professional experience.
2. To ascertain if physicians state a possible change in treatment using 3D-Print, VR-Glasses, or a 3D-Display.
Methods
Participants
Interviews were conducted with twenty-three physicians employed at the University Hospital of Basel, Switzerland. Participants were recruited from disciplines where a potential for three-dimensional representation was identified, namely cardiology, oral and maxillofacial surgery, orthopedic surgery, and radiology. The possible participants were contacted via e-mail or asked personally to participate in this study. In total, fifty-two individuals were contacted. The physicians who found the time and were willing to attend a meeting in the 3D-PrintLab were included in this study. Participation was voluntary, and everyone agreed to the use of their data. In the end, twenty-three interviews were conducted between December 2018 and March 2020. Two participants (one student and one technical adviser) failed to comply with the selection criteria (not being a physician) and were therefore excluded. One physician had to be excluded due to technical problems in demonstrating the case on the VR-Glasses. The final cohort of this study consisted of twenty participants. Five physicians from each of the following disciplines took part: Cardiology, oral and maxillofacial surgery, orthopedic surgery, and radiology. Five participants had ≤5 years of professional experience, eight 6–10 years, and seven had > 10 years of professional experience. The demographics of the final participants are shown in Table 1.
Table 1.
Demographics of the final cohort
| Variable | Number |
|---|---|
| Age (in years) | |
| 25–35 | 8 (40) |
| 36–45 | 10 (50) |
| > 45 | 2 (10) |
| Position | |
| Intern | 6 (30) |
| Attending | 1 (5) |
| Deputy senior physician | 4 (20) |
| Senior physician | 7 (35) |
| Chief physician | 2 (10) |
| Professional experience (in years) | |
| ≤ 5 | 5 (25) |
| 6–10 | 8 (40) |
| > 10 | 7 (35) |
| Gender | |
| Male | 20 (100) |
| Female | 0 (0) |
| Interest in technology | |
| None | 0 (0) |
| Medium | 7 (35) |
| Very | 13 (65) |
| Area of expertise | |
| Cardiology | 5 (25) |
| OMFS | 5 (25) |
| Orthopedic surgery | 5 (25) |
| Radiology | 5 (25) |
Data: Values are given as absolute numbers (with percentages in brackets). OMFS = Oral and maxillofacial surgery
Cases
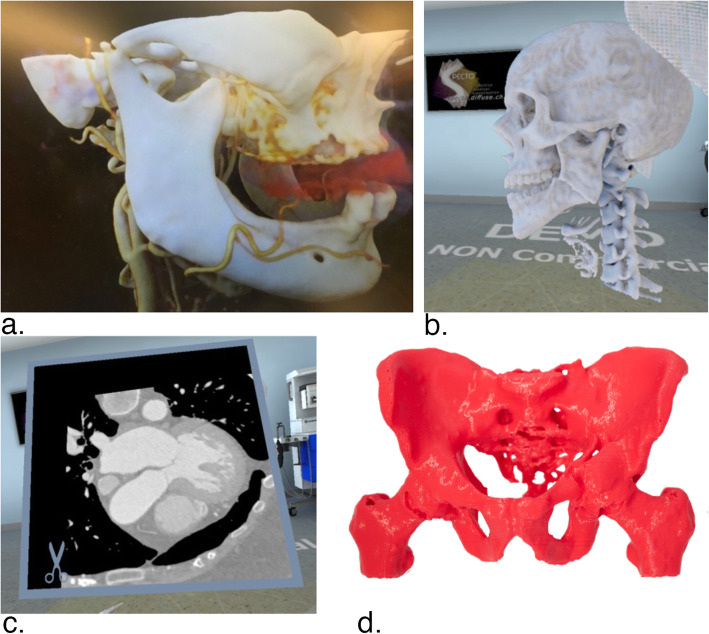
Cases were chosen from a radiologist’s daily work at the University Hospital of Basel. Pathologies needed to be well recognized with the aforementioned 3D presentation systems while being similar to allow comparability. Furthermore, the chosen cases were required to be regularly occurring pathologies. In each discipline, except radiology, three different discipline-specific cases were selected to minimize bias. Each case was produced using all three modalities. In radiology, one case from each of the three other disciplines was used. In Table 2, the nine different cases are described. The preparation of all cases presented to the participants started with exporting DICOM (Digital Imaging and Communications in Medicine) data of the CT scans from the internal university hospital servers mentioned in Table 2. After that, the preparation of each of the three modalities proceeded differently. Figure 1 shows examples of prepared cases.
Table 2.
Prepared cases
| Area of expertise | Case 1 | Case 2 | Case 3 |
|---|---|---|---|
| Cardiology | Proximal crossing of RIVA and RCX | Atypical retroaortal course of RCX with origin in the left coronary sinus | Atypical anteaortal course of left main trunk with common origin with RCA in the right coronary sinus |
| Oral and maxillofacial surgery | Dislocated right condylar fracture of the mandible | Mental mandibular fracture | Angle mandibular fracture |
| Orthopedic surgery | Transverse left acetabular fracture with contralateral pubic ramus fracture | Anterior column acetabular fracture with contralateral pubic ramus fracture | Posterior column fracture left |
Data: RIVA = Ramus interventricularis anterior, RCX = Ramus circumflexus, RCA = Arteria coronaria dextra
Fig. 1.
Examples of prepared cases. a. Dislocated right condylar fracture of the mandible on 3D-Display (picture taken through passive shutter glasses). b. Angle mandibular fracture on VR-Glasses (corresponding two-dimensional view on computer-display). c. Proximal crossing of RIVA and RCX on VR-Glasses, CT View (corresponding two-dimensional view on computer-display). d. Posterior column fracture left, 3D-printed. Data: RIVA = Ramus interventricularis anterior, RCX = Ramus circumflexus
3D-print
Exported DICOM data was segmented with 3D-Slicer (slicer.org, Version 4.10.0) [40] and final processing and integrity check was performed on Meshmixer (Autodesk, Inc., San Rafael, USA, Version 3.5.474). Slicing and printing were prepared with MakerBot Print (MakerBot Industries, New York City, USA, Version 4.6.0). Models were printed on a MEX MakerBot Replicator+ Printer (MakerBot Industries, New York City, USA) with a nozzle size of 0.4 mm, a slice thickness of 0.2 mm, and the printing material polylactic acid (PLA). Most cases were printed in 1:1 scale. However, the three orthopedic cases were printed in 0.5:1 scale due to the high print time and tall build volume needed for the 1:1 model. The time required to prepare varied between half an hour and one hour. Print duration reached from four to fifteen hours.
VR-glasses
To prepare DICOM data for VR representation specto (Diffuse Inc., Basel, Switzerland, Version 3.3.0) was used. This software uses real-time GPU volume raytracing. A three-dimensional view was created through auto-segmentation, cutting for the region of interest, and an equivalent volume rendering color look-up table (LUT). Specto then uses the Steam VR platform (Steam, Valve Corporation, Bellevue, USA, Version 1.11.11) and HTC Vive VR-Glasses (High Tech Computer Corporation, Taoyuan, Taiwan) with a resolution of 1080 × 1200 pixels per eye for representation. Two controllers were used to interact with the virtual environment, including arbitrary cutting planes, individual lightning, and the possibility of switching to a CT view. The total time needed to prepare the cases varied between half an hour and an hour and a half.
3D-display
To prepare the cases for viewing on the 3D-Display, DICOM data was imported to Cinematic Rendering Prototype (Siemens Healthineers, Erlangen, Germany, Prototype), where different tools were enabled to crop the data on the region of interest and to apply specific LUT. The three-dimensional representation was then rendered and displayed with the Syngo VectorRayCaster (Siemens Healthineers, Erlangen, Germany, Prototype) on the 3D-Display HP Zvr Virtual Reality Display (HP Inc., Palo Alto, USA, no longer in production) with a resolution of 1920 × 1080 pixels. Similar to a 3D-TV, additional glasses (passive, polarized) had to be worn. The time needed from DICOM to final representation lasted between thirty minutes and one hour.
Interviews & questionnaire
With nine cases available on all three modalities, interviews with the physicians were conducted by a 4th-year medical student. Each physician had an individual timeslot and was given a short introduction regarding methodology and the aim of the survey. The chronological order of the demonstrations followed a decreasing complexity concerning technical aspects. This approach was chosen in order to minimize the time physicians would spend in the lab in case of malfunctioning. Starting with the VR-Glasses, the participant was then presented with the first case from his discipline, followed by the presentation of the second case on the 3D-Display and a 3D-Model of the last case. While the physician was using each method, he gave oral feedback, which was written down. In the end, the physician filled out the missing information by pen. The rating scale ranged from 0 (very poor) to 10 (excellent) for the first research aim, i.e., understanding of the pathology, accuracy of details, quality of the anatomical representation, and technical operability. The accuracy of details evaluates how well details are represented e.g., the coronary arteries in the cardiology cases or the fracture gap in the maxillofacial surgery and orthopedic models. Technical operability was only assessed for VR-Glasses and 3D-Display as it concerned the user’s handling of the device used in the presentation i.e., the controllers and the mouse. Concerning the possible change in treatment, the participants were asked if in general they could imagine that the used method might lead to a change in the treatment plan. The original treatment plan was not provided, and participants were not familiar with the chosen cases. Furthermore, demographics were assessed, i.e., age, gender, discipline, years of professional experience, position within the hospital, and interest in technology. This entire procedure took around twenty minutes. For each of the disciplines the individual cases were shown. Radiologists received one case from each discipline. Cases within the discipline were randomly assigned to the participants using an alternating approach.
Statistical methods
The data acquired with the paper and pencil questionnaires was transferred to and statistically analyzed with Microsoft Excel (Microsoft Corporation, Redmond, USA, Version 16.47.1). Descriptive statistics were used for an overview of participants’ characteristics. Mean, and standard deviation (SD) were reported for normally distributed data. Absolute numbers and percentages were given for binary and categorical variables.
Ethics
A review by the institutional review board was waived. All patient data were anonymized. Furthermore, patients included in this study had already, by the time of the inclusion been treated. Therefore, this study had no impact on patients’ therapy or health.
Results
Averages
The averages including the radiologists’ feedback showed only marginal differences compared to the averages excluding the radiologists. Table 3 outlines the two averages.
Table 3.
Comparison of the averages including the radiologists’ feedback with the average excluding the radiologists’ feedback
| Variable | Average including radiologists’ feedback (n = 20) | Average excluding radiologists’ feedback (n = 15) |
|---|---|---|
| Understanding of the pathology | ||
| 3D-Print | 7.5 (2.3) | 7.6 (2.4) |
| VR-Glasses | 8.1 (2.0) | 8.0 (2.3) |
| 3D-Display | 7.6 (1.9) | 7.6 (2.0) |
| Accuracy of details | ||
| 3D-Print | 6.6 (2.3) | 6.7 (2.1) |
| VR-Glasses | 7.9 (1.5) | 8.0 (1.4) |
| 3D-Display | 8.5 (1.5) | 8.5 (1.6) |
| Quality of the anatomical representation | ||
| 3D-Print | 7.6 (2.0) | 7.7 (2.0) |
| VR-Glasses | 8.4 (1.6) | 8.4 (1.3) |
| 3D-Display | 8.3 (1.2) | 8.3 (1.2) |
| Technical operability | ||
| VR-Glasses | 7.7 (1.8) | 7.4 (1.8) |
| 3D-Display | 8.6 (1.6) | 8.4 (1.8) |
Data: The rating scale ranged from 0 (very poor) to 10 (excellent). Values are given as mean (with standard deviation (SD) in brackets)
Disciplines and levels of professional experience
Understanding of the pathology: VR-Glasses are rated best in three out of four disciplines and two out of three levels of professional experience with an average of 8.1 (SD 2.0) followed by 3D-Display with 7.6 (SD 1.9) and 3D-Print with 7.5 (SD 2.3).
Accuracy of details: 3D-Display is rated best in three out of four disciplines and in all levels of professional experience. 3D-Print is last in all disciplines and all levels of professional experience. Mean of 3D-Display is 8.5 (SD 1.5), VR-Glasses 7.9 (SD 1.5) and, 3D-Print 6.6 (SD 2.3).
Quality of the anatomical representation: VR-Glasses have the best score with 8.4 (SD 1.6), closely followed by 3D-Display with 8.3 (SD 1.2) and with some offset 3D-Print with 7.6 (SD 2.0). VR-Glasses reach the best score in three out of four disciplines and two out of three levels of professional experience.
Technical operability: 3D-Display is consistently rated best in all levels of professional experience and all disciplines with an average of 8.6 (SD 1.6). VR-Glasses rated second with 7.7 (SD 1.8). 3D-Print was not assessed.
Comparing all three methods and all research questions above, the cardiologists gave the lowest rating in all queries and modalities except in one. On the other hand, orthopedic surgeons gave the best ratings except in one case. Tables 4 and 5 show all scores stratified in disciplines and level of professional experience.
Table 4.
Comparison of 3D-Print, VR-Glasses and 3D-Display concerning disciplines
| Variable | Cardiology (n = 5) | OMFS (n = 5) | Ortho (n = 5) | Radiology (n = 5) |
|---|---|---|---|---|
| Understanding of the pathology | ||||
| 3D-Print | 5.8 (2.5) | 8.2 (1.9) | 8.8 (1.5) | 7.2 (2.1) |
| VR-Glasses | 7.2 (1.7) | 9.0 (1.5) | 7.8 (3.0) | 8.2 (0.4) |
| 3D-Display | 7.0 (2.2) | 6.6 (1.4) | 9.2 (1.2) | 7.6 (1.4) |
| Accuracy of details | ||||
| 3D-Print | 4.8 (1.7) | 7.4 (0.8) | 8.0 (2.1) | 6.2 (2.6) |
| VR-Glasses | 7.6 (1.5) | 8.0 (1.1) | 8.4 (1.5) | 7.6 (1.9) |
| 3D-Display | 7.4 (1.7) | 8.6 (1.0) | 9.4 (1.2) | 8.6 (1.2) |
| Quality of the anatomical representation | ||||
| 3D-Print | 6.4 (2.4) | 8.4 (1.0) | 8.4 (1.6) | 7.0 (1.8) |
| VR-Glasses | 7.6 (0.8) | 8.6 (1.0) | 9.0 (1.5) | 8.2 (2.1) |
| 3D-Display | 7.8 (1.3) | 8.2 (0.4) | 8.8 (1.5) | 8.2 (1.2) |
| Technical operability | ||||
| VR-Glasses | 6.0 (1.5) | 7.6 (1.4) | 9.0 (1.2) | 8.6 (1.2) |
| 3D-Display | 7.8 (2.0) | 7.8 (1.5) | 9.8 (0.4) | 9.4 (0.5) |
Data: The rating scale ranged from 0 (very poor) to 10 (excellent). Values are given as mean (with standard deviation (SD) in brackets). OMFS = Oral and maxillofacial surgery, Ortho = Orthopedic surgery
Table 5.
Comparison of 3D-Print, VR-Glasses and 3D-Display concerning professional experience (in years)
| Variable | ≤5 years (n = 5) |
6–10 years (n = 8) |
> 10 years (n = 7) |
|---|---|---|---|
| Understanding of the pathology | |||
| 3D-Print | 8.2 (1.5) | 7.0 (2.7) | 7.6 (2.3) |
| VR-Glasses | 8.6 (1.5) | 8.3 (0.8) | 7.4 (2.9) |
| 3D-Display | 8.0 (1.9) | 7.4 (1.7) | 7.6 (1.9) |
| Accuracy of details | |||
| 3D-Print | 7.0 (0.9) | 5.5 (2.4) | 7.6 (2.2) |
| VR-Glasses | 7.2 (1.9) | 8.0 (0.9) | 8.3 (1.7) |
| 3D-Display | 9.2 (0.7) | 8.1 (1.9) | 8.4 (1.2) |
| Quality of the anatomical representation | |||
| 3D-Print | 7.6 (1.0) | 6.4 (2.2) | 8.9 (1.4) |
| VR-Glasses | 7.0 (1.7) | 8.6 (1.3) | 9.0 (1.1) |
| 3D-Display | 9.0 (0.9) | 7.9 (1.1) | 8.1 (1.4) |
| Technical operability | |||
| VR-Glasses | 8.0 (1.7) | 7.5 (1.5) | 7.8 (2.1) |
| 3D-Display | 8.6 (1.4) | 9.1 (0.6) | 8.0 (2.3) |
Data: The rating scale ranged from 0 (very poor) to 10 (excellent). Values are given as mean (with standard deviation (SD) in brackets)
Change in treatment
In cardiology, two out of three participants stated a possible change in treatment when using the VR-Glasses. Furthermore, three out of five radiologists reported a possible change in treatment when using VR-Glasses. In the group with a professional experience of more than > 10 years, no change in treatment could be envisioned for any of the three methods. Table 6 shows the percentage of participants who stated a change in treatment is possible using a 3D-Print, VR-Glasses, or a 3D-Display.
Table 6.
Possible change in treatment, a. disciplines, b. professional work experience (in years)
| Disciplines | Years of experience | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Average (n = 18) | a. | Cardiology (n = 3) |
OMFS (n = 5) |
Ortho (n = 5) |
Radiology (n = 5) |
b. | ≤ 5 (n = 5) |
6–10 (n = 7) |
> 10 (n = 6) |
|
| 3D-Print | 6 (33) | 0 | 2 (40) | 2 (40) | 2 (40) | 2 (40) | 4 (57) | 0 | ||
| VR-Glasses | 8 (44) | 2 (67) | 1 (20) | 2 (40) | 3 (60) | 3 (60) | 5 (71) | 0 | ||
| 3D-Display | 6 (33) | 1 (33) | 1 (20) | 2 (40) | 2 (40) | 2 (40) | 4 (57) | 0 | ||
Data: Values are given as absolute numbers (with percentages in brackets) for binary and categorical variables. OMFS = Oral and maxillofacial surgery, Ortho = Orthopedic surgery
Discussion
Medical imaging such as computed tomography and magnetic resonance imaging plays an essential role in developing a diagnosis. These medical image datasets are acquired in three dimensions, yet they are mostly presented on a two-dimensional display. The present study was designed to compare different three-dimensional representation methods, namely 3D-Print, VR-Glasses, and 3D-Display to understand these methods better.
All three modalities were well accepted and received a high rating in understanding of the pathology, accuracy of details, quality of the anatomical representation, and operability. Furthermore, a possible change in treatment was stated using 3D-Print or 3D-Display in one-third of the cases. Using the VR-Glasses, an even higher number of physicians (44%) reported a possible change in treatment. However, this is only true in participants with less than ten years of experience. This could indicate a possible educational component that should be explored further.
Our conclusions accord to some extent with previous studies which revealed significant potential for 3D-Printing [3, 41] and VR-Glasses [22, 25]. A study by Bartella, Kamal, Scholl, et al. evaluated the use of VR-Glasses in preoperative planning in maxillofacial surgery. They presented three different cases to four participants, which had to rate them concerning, e.g., the potential for clinical use. The authors have noted the importance of VR-Glasses in preoperative planning and teaching [42]. However, the participants were only given a chance to evaluate VR-Glasses. The strength of this study is that three different methods of 3D representations were compared. Some new conclusions can therefore be drawn. First, all methods are very well accepted by physicians. Consequently, further evaluations of the function and characteristics of these modalities to gain a more profound knowledge of their use in medicine is warranted. Second, it is somewhat surprising that the cardiologist gave the lowest rating in all questions and modalities in comparing the three methods except in one. On the other hand, orthopedic surgeons gave the best ratings except in one case. A possible explanation for this might be that gross bone fractures were chosen in all three orthopedic cases. In contrast, cardiology included three delicate coronary pathologies. This might indicate a weakness of all three methods in presenting delicate, detailed structures. This holds especially true for the cinematic rendering approach of VR and 3D-Display were elaborate segmentation technology as for 3D-Printing was not available and as such could have been obscured by neighboring structures with similar voxel intensities. This is particularly the case in cardiology. Furthermore, cardiologists are generally used to angiographies while the other disciplines routinely use CT data. This might make it more difficult for cardiologists to interact with the 3D representations.
Third, many physicians with professional work experience of less than ten years stated a possible change in treatment. However, physicians with professional experience above ten years reported in no case a possible change in therapy. This result is, to some extent, not surprising. The more experienced, the less someone can benefit from new methods. Nevertheless, this result was not expected to be so clear. This, however, renders the idea of using these three-dimensional methods as teaching tools for less experienced physicians [20, 22, 30, 42]. Lastly, the averages including the radiologists’ feedback and the averages excluding their feedback differed only slightly. This could indicate a good overall acceptance by physicians who are not familiar with these new methods. Only the averages concerning technical operability were slightly higher when including the radiologists. This could be because radiologists at the University Hospital of Basel occasionally work with VR-Glasses and 3D-Displays.
The cases chosen were regularly occurring pathologies, often with a standardized treatment plan. In choosing challenging and unusual cases, a possible change in treatment could have been stated more often. This is because the optimal therapy is more difficult to derive in complex cases. The strength of 3D representations is the presentation of challenging cases. This could have had an impact especially in the group with more than ten years of work experience.
Owing to some limitations in the sampling process, in choosing and preparing the cases and technological aspects, our findings should be interpreted with caution. The main limitation is the relatively small sample size. It proved to be very difficult to recruit a sufficient number of participants. Of fifty-two possible participants contacted, only twenty-three responded, some of them only after being contacted several times. The sample size consists of twenty male physicians selected from one university hospital. These numbers could, in further studies, be increased and diversified. However, as physicians are often hardly available due to the high workload, it is challenging to acquire more participants. This could be met in expanding the range of included hospitals and transferring the test site closer to the workplace of targeted participants. Furthermore, there was some element of selection bias. Predominantly, physicians interested in new technology were more likely to self-select to participate in this study.
Cases selected were considered suitable for three-dimensional representation and from a radiologist’s daily repertoire. Therefore, these cases represent only some possibilities. Additionally, specific fields were chosen, i.e., coronary pathologies in cardiology and bone-fractures in orthopedics and oral and maxillofacial surgery. This does not represent the entire range of eventualities. It would have been interesting to place the focus on challenging and unusual cases as this is the main strength of 3D representations. However, rather general cases were chosen so the educational value in the training of young and inexperienced physicians could also be assessed. The number of cases participants tested on each modality could also be increased given that only one case per modality was shown. It would be interesting to determine whether the groups with different professional experience react differently to distinct complexities of cases. The number of three cases per specific field was not suitable as some case/modality combinations were seen more often than others. The fields chosen could also have been more diverse e.g., neurological, or abdominal pathologies would have increased the meaningfulness of this study. Lastly, by first presenting the pathology with the VR-Glasses, bias could have been introduced. However, this was minimized as cases were switched between the different methods, and participants were not informed as to why VR-Glasses were used first.
With regards to the research question concerning accuracy of details, no comparison was given such as a CT-View. This question was based on the participants clinical experience. Most physicians are familiar with interpreting CT and MRI datasets or e.g., cardiologists with a coronary angiography. This allowed the participants to compare the three-dimensional presentations with the images they were already acquainted with. Concerning the research question for possible change in treatment, the answers were based on the respective physicians’ clinical experience and their subjective decision-making. This is often the case in the day-to-day work of physicians when deciding on the personal treatment plan. An original treatment plan was not provided as this could have led to a response bias.
Technical limitations appear when rendering or segmenting the raw DICOM data. This step has a specific susceptibility to errors, and the procedure must be conducted with caution and high accuracy. Furthermore, the technical equipment showed some shortcomings. The models were printed using the MEX technology as it was widely available in the used lab. A study by Msallem et al. attested the MEX technology the highest overall precision compared to other printing technologies [43]. The layer height of 0.2 mm was rather thick and could be lowered in further studies. However, considering the chosen cases, the pathologies were adequately represented with the employed printing resolution. Any possible negative effects regarding the haptic experience were considered to be minor. The orthopedics models were printed in a 0.5:1 scale due to the high print time and tall build volume needed. This led to a decrease in details and haptic recognition. This was noted by several orthopedic surgeons who mentioned that if the models had been 1:1, a higher rating would have been achieved. The HTC Vive VR-Glasses (High Tech Computer Corporation, Taoyuan, Taiwan) that were used have a screen resolution of 1080 × 1200 pixels per eye. Newer versions of VR-Glasses hold much higher resolutions, leading to more precise representations of pathologies. This is a significant improvement that has to be accounted for in interpreting the results of this study. Moreover, the 3D-Display that was used is no longer being produced. The software used to prepare the 3D-Prints were not CE marked medical software. This is also true for the software used to prepare the DICOM data for VR representation and for representation on the 3D-Display. However, a CE marking is not thought to be necessary as this study was conducted within an experimental research context. Furthermore, the CE label does not implicate quality and is not a certification mark. Finally, some technical difficulties occurred concerning the VR-Glasses. This included and was not limited to loosen contact and the inability to render some DICOM data. This problem must be addressed technically.
Conclusions
3D-Print, VR-Glasses, and 3D-Displays are very well accepted, and a relevant percentage of physicians with less than ten years of professional work experience could imagine a possible change in treatment using any of these three-dimensional methods. These findings have important implications for further development of three-dimensional representation tools, given their high acceptance and, in our understanding, a high percentage of physicians stating a possible change in treatment. Our findings challenge scientists, technicians, and physicians to further develop these three-dimensional representation methods to improve the three-dimensional understanding of pathologies. Furthermore, possible applications in medicine must be evaluated more clearly. On the one hand, they can facilitate the day-to-day work of physicians. On the other hand, the educational value could be of importance in the training of young and inexperienced physicians.
Acknowledgements
We thank all participating physician und surgeons namely Benito Benitez, Matthias Benz, Denis Berdajs, Murat Bilici, Martin Clauss, Henrik Eckardt, Gregor Fahrni, Andreas Fischer, Emanuel Flury, Philip Haaf, Peter Kvarda, Sebastian Manneck, Simon Meyer, Mario Morgenstern, Moritz Neubauer, Maurice Pradella, Miodrag Salvic, Nicolas Schärli, Raphael Twerenbold and Matthias Ureel.
Abbreviations
- CT
Computed tomography
- MRI
Magnetic resonance imaging
- VR
Virtual Reality
- MEX
Material extrusion
- VP
Vat photopolymerization
- PLA
Polylactic acid
- ABS
Acrylonitrile butadiene styrene
- DICOM
Digital Imaging and Communications in Medicine
- LUT
Look-up-Table
- SD
Standard deviation
Authors’ contributions
JLM and PB devised the study conception and design. JLM was responsible for the data acquisition. Analysis and data interpretation was performed by JLM, PB and TH. The manuscript was drafted by JLM. Critical revision was conducted by FMT. All authors read and approved the final manuscript.
Funding
This study was partially funded by Siemens (Siemens Healthineers, Erlangen, Germany). This funding had no implications on the design of the study, collection, analysis, and interpretation of data and in writing the manuscript. No other resources financial in nature or otherwise were provided.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
PB and FMT are members of the editorial board “3D Printing in Medicine”.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fishman EK, Drebin B, Magid D, Scott WW, Ney DR, Brooker AF, et al. Volumetric rendering techniques: applications for three-dimensional imaging of the hip. Radiology. 1987;163(3):737–738. doi: 10.1148/radiology.163.3.3575725. [DOI] [PubMed] [Google Scholar]
- 2.Rubin GD. Computed tomography: revolutionizing the practice of medicine for 40 years. Radiology. 2014;273(2S):S45–S74. doi: 10.1148/radiol.14141356. [DOI] [PubMed] [Google Scholar]
- 3.Mitsouras D, Liacouras P, Imanzadeh A, Giannopoulos AA, Cai T, Kumamaru KK, George E, Wake N, Caterson EJ, Pomahac B, Ho VB, Grant GT, Rybicki FJ. Medical 3D printing for the radiologist. RadioGraphics. 2015;35(7):1965–1988. doi: 10.1148/rg.2015140320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Geng J. Three-dimensional display technologies. Adv Opt Photonics. 2013;5(4):456–535. doi: 10.1364/AOP.5.000456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chepelev L, Giannopoulos A, Tang A, Mitsouras D, Rybicki FJ. Medical 3D printing: methods to standardize terminology and report trends. 3D Print Med. 2017;3(1):4. doi: 10.1186/s41205-017-0012-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ballard DH, Trace AP, Ali S, Hodgdon T, Zygmont ME, DeBenedectis CM, et al. Clinical applications of 3D printing: primer for radiologists. Acad Radiol. 2018;25(1):52–65. doi: 10.1016/j.acra.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghosh U, Ning S, Wang Y, Kong YL. Addressing unmet clinical needs with 3D printing technologies. Adv Healthc Mater. 2018;7(17):1–24. doi: 10.1002/adhm.201800417. [DOI] [PubMed] [Google Scholar]
- 8.Tack P, Victor J, Gemmel P, Annemans L. 3D-printing techniques in a medical setting: a systematic literature review. Biomed Eng Online. 2016;15(1):1–21. doi: 10.1186/s12938-016-0236-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matai I, Kaur G, Seyedsalehi A, McClinton A, Laurencin CT. Progress in 3D bioprinting technology for tissue/organ regenerative engineering. Biomaterials. 2020;226(October 2019):119536. doi: 10.1016/j.biomaterials.2019.119536. [DOI] [PubMed] [Google Scholar]
- 10.Meyer S, Hirsch J-M, Leiggener CS, Msallem B, Sigron GR, Kunz C, Thieringer FM. Fibula graft cutting devices: are 3D-printed cutting guides more precise than a universal, reusable osteotomy jig? J Clin Med. 2020;9(12):4119. doi: 10.3390/jcm9124119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park SW, Choi JW, Koh KS, Oh TS. Mirror-imaged rapid prototype skull model and pre-molded synthetic scaffold to achieve optimal orbital cavity reconstruction. J Oral Maxillofac Surg. 2015;73(8):1540–1553. doi: 10.1016/j.joms.2015.03.025. [DOI] [PubMed] [Google Scholar]
- 12.Alturkistani R, Kavin A, Devasahayam S, Thomas R, Colombini EL, Cifuentes CA, et al. Affordable passive 3D-printed prosthesis for persons with partial hand amputation. Prosthetics Orthot Int. 2020;44(2):92–98. doi: 10.1177/0309364620905220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim T, Lee S, Kim GB, Hong D, Kwon J, Park JW, et al. Accuracy of a simplified 3D-printed implant surgical guide. J Prosthet Dent. 2020;124(2):195–201.e2. doi: 10.1016/j.prosdent.2019.06.006. [DOI] [PubMed] [Google Scholar]
- 14.Keller M, Guebeli A, Thieringer F, Honigmann P. ScienceDirect In-hospital professional production of patient-specific 3D-printed devices for hand and wrist rehabilitation Production en se ˆpital main et du poignet par impression 3D dans un ho. Hand Surg Rehabil. 2020;(xxxx). [DOI] [PubMed]
- 15.Kaae S, Lind JLM, Genina N, Sporrong SK. Unintended consequences for patients of future personalized pharmacoprinting. Int J Clin Pharm. 2018;40(2):321–324. doi: 10.1007/s11096-018-0596-x. [DOI] [PubMed] [Google Scholar]
- 16.MacLeod A, Patterson M, MacTear K, Gill HS. 3D printed locking osteosynthesis screw threads have comparable strength to machined or hand-tapped screw threads. J Orthop Res. 2020;38(7):1559–1565. doi: 10.1002/jor.24712. [DOI] [PubMed] [Google Scholar]
- 17.Economidou SN, Pere CPP, Reid A, Uddin MJ, Windmill JFC, Lamprou DA, Douroumis D. 3D printed microneedle patches using stereolithography (SLA) for intradermal insulin delivery. Mater Sci Eng C. 2019;102(April):743–755. doi: 10.1016/j.msec.2019.04.063. [DOI] [PubMed] [Google Scholar]
- 18.Forouzandeh F, Ahamed NN, Hsu MC, Walton JP, Frisina RD, Borkholder DA. A 3D-Printed Modular Microreservoir for Drug Delivery. Micromachines. 2020;11(7):648. 10.3390/mi11070648. [DOI] [PMC free article] [PubMed]
- 19.Gross BC, Erkal JL, Lockwood SY, Chen C, Spence DM. Evaluation of 3D printing and its potential impact on biotechnology and the chemical sciences. Anal Chem. 2014;86(7):3240–3253. doi: 10.1021/ac403397r. [DOI] [PubMed] [Google Scholar]
- 20.Kim GB, Lee S, Kim H, Yang DH, Kim YH, Kyung YS, Kim CS, Choi SH, Kim BJ, Ha H, Kwon SU, Kim N. Three-dimensional printing: basic principles and applications in medicine and radiology. Korean J Radiol. 2016;17(2):182–197. doi: 10.3348/kjr.2016.17.2.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hong D, Lee S, Kim GB, Lee SM, Kim N, Seo JB. Development of a CT imaging phantom of anthromorphic lung using fused deposition modeling 3D printing. Medicine (Baltimore) 2020;99(1):e18617. doi: 10.1097/MD.0000000000018617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Izard SG, Juanes Méndez JA, Palomera PR. Virtual reality educational tool for human anatomy. J Med Syst. 2017;41(5):2–7. doi: 10.1007/s10916-017-0723-6. [DOI] [PubMed] [Google Scholar]
- 23.Iannicelli AM, Vito D, Dodaro CA, De Matteo P, Nocerino R, Sepe A, et al. Does virtual reality reduce pain in pediatric patients? A systematic review. Ital J Pediatr. 2019;45(1):1–6. doi: 10.1186/s13052-019-0757-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sutherland J, Belec J, Sheikh A, Chepelev L, Althobaity W, Chow BJW, Mitsouras D, Christensen A, Rybicki FJ, la Russa DJ. Applying modern virtual and augmented reality technologies to medical images and models. J Digit Imaging. 2019;32(1):38–53. doi: 10.1007/s10278-018-0122-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim Y, Kim H, Kim YO. Virtual reality and augmented reality in plastic surgery: a review. Arch Plast Surg. 2017;44(3):179–187. doi: 10.5999/aps.2017.44.3.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ong CS, Krishnan A, Huang CY, Spevak P, Vricella L, Hibino N, Garcia JR, Gaur L. Role of virtual reality in congenital heart disease. Congenit Heart Dis. 2018;13(3):357–361. doi: 10.1111/chd.12587. [DOI] [PubMed] [Google Scholar]
- 27.Lin J, Kelleher CL, Engsberg JR. Developing home-based virtual reality therapy interventions. Games Health J. 2013;2(1):34–38. doi: 10.1089/g4h.2012.0033. [DOI] [PubMed] [Google Scholar]
- 28.Ayoub A, Pulijala Y. The application of virtual reality and augmented reality in Oral & Maxillofacial Surgery. BMC Oral Health. 2019;19(1):1–8. doi: 10.1186/s12903-019-0937-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Juhnke B, Mattson AR, Saltzman D, Azakie A, Hoggard E, Ambrose M, Iaizzo PA, Erdman A, Fischer G. Use of virtual reality for pre-surgical planning in separation of conjoined twins: a case report. Proc Inst Mech Eng Part H J Eng Med. 2019;233(12):1327–1332. doi: 10.1177/0954411919878067. [DOI] [PubMed] [Google Scholar]
- 30.Stepan K, Zeiger J, Hanchuk S, Del Signore A, Shrivastava R, Govindaraj S, et al. Immersive virtual reality as a teaching tool for neuroanatomy. Int Forum Allergy Rhinol. 2017;7(10):1006–1013. doi: 10.1002/alr.21986. [DOI] [PubMed] [Google Scholar]
- 31.Pfandler M, Lazarovici M, Stefan P, Wucherer P, Weigl M. Virtual reality-based simulators for spine surgery: a systematic review. Comput Aided Med Proced Spine J. 2017;17(9):1352–1363. doi: 10.1016/j.spinee.2017.05.016. [DOI] [PubMed] [Google Scholar]
- 32.Elsayed M, Kadom N, Ghobadi C, Strauss B, Al Dandan O, Aggarwal A, et al. Virtual and augmented reality: potential applications in radiology. Acta Radiol. 2020;61(9):1258–1265. doi: 10.1177/0284185119897362. [DOI] [PubMed] [Google Scholar]
- 33.Werner P, Rabinowitz S, Klinger E, Korczyn AD, Josman N. Use of the virtual action planning supermarket for the diagnosis of mild cognitive impairment. Dement Geriatr Cogn Disord. 2009;27(4):301–309. doi: 10.1159/000204915. [DOI] [PubMed] [Google Scholar]
- 34.King F, Jayender J, Bhagavatula SK, Shyn PB, Pieper S, Kapur T, Lasso A, Fichtinger G. An immersive virtual reality environment for diagnostic imaging. J Med Robot Res. 2016;01(01):1640003. doi: 10.1142/S2424905X16400031. [DOI] [Google Scholar]
- 35.Prajapati S, Madrigal E, Friedman MT. Acquisition, visualization, and potential applications of 3D data in anatomic pathology. Discoveries. 2016;4(4):e68. doi: 10.15190/d.2016.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beitnes JO, Klæboe LG, Karlsen JS, Urheim S. Mitral valve analysis using a novel 3D holographic display: a feasibility study of 3D ultrasound data converted to a holographic screen. Int J Cardiovasc Imaging. 2015;31(2):323–328. doi: 10.1007/s10554-014-0564-z. [DOI] [PubMed] [Google Scholar]
- 37.Abildgaard A, Witwit AK, Karlsen JS, Jacobsen EA, Tennøe B, Ringstad G, Due-Tønnessen P. An autostereoscopic 3D display can improve visualization of 3D models from intracranial MR angiography. Int J Comput Assist Radiol Surg. 2010;5(5):549–554. doi: 10.1007/s11548-010-0509-5. [DOI] [PubMed] [Google Scholar]
- 38.Ahn J, Hong J. Are three-dimensional monitors more appropriate than two-dimensional monitors in the three-dimensional analysis? J Craniofac Surg. 2017;28(1):e101–e104. doi: 10.1097/SCS.0000000000003288. [DOI] [PubMed] [Google Scholar]
- 39.Vávra P, Roman J, Zonča P, Ihnát P, Němec M, Kumar J, Habib N, el-Gendi A. Recent development of augmented reality in surgery: a review. J Healthc Eng. 2017;2017:1–9. doi: 10.1155/2017/4574172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fedorov A, Beichel R, Kalpathy-Cramer J, Finet J, Fillion-Robin J-C, Pujol S, Bauer C, Jennings D, Fennessy F, Sonka M, Buatti J, Aylward S, Miller JV, Pieper S, Kikinis R. 3D slicer as an image computing platform for the quantitative imaging network. Magn Reson Imaging. 2012;30(9):1323–1341. doi: 10.1016/j.mri.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rengier F, Mehndiratta A, Von Tengg-Kobligk H, Zechmann CM, Unterhinninghofen R, Kauczor HU, et al. 3D printing based on imaging data: review of medical applications. Int J Comput Assist Radiol Surg. 2010;5(4):335–341. doi: 10.1007/s11548-010-0476-x. [DOI] [PubMed] [Google Scholar]
- 42.Bartella AK, Kamal M, Scholl I, Schiffer S, Steegmann J, Ketelsen D, Hölzle F, Lethaus B. Virtual reality in preoperative imaging in maxillofacial surgery: implementation of “the next level”? Br J Oral Maxillofac Surg. 2019;57(7):644–648. doi: 10.1016/j.bjoms.2019.02.014. [DOI] [PubMed] [Google Scholar]
- 43.Msallem B, Sharma N, Cao S, Halbeisen FS, Hans-Florian Zeilhofer FMT. Evaluation of the Dimensional Accuracy of 3D-Printed Anatomical Mandibular Models Using. J Clin Med. 2020;9(3):817. doi: 10.3390/jcm9030817. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article.