Abstract
The novel coronavirus disease 2019 (COVID-19) caused by the new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has spread at a very fast rate, overwhelming and disrupting healthcare systems around the world since its outbreak in December 2019 in China. As of October 2021, the total number of COVID-19 cases exceeds 240,000,000, and the total number of deaths is close to 5,000,000. In the situation of widespread SARS-CoV-2 infection, restrictions on the medical system due to shifts in medical care to accommodate the pandemic will occur, and its impact on surgical and endoscopic treatment for colorectal cancer is inevitable. Therefore, it is necessary to satisfy all of the following requirements: patient safety, prevention of exposure of healthcare workers including surgeons, prevention of nosocomial infection, and a decision on how to treat the primary disease. Surgical triage is also required, based on comprehensive consideration of the patient's condition, the severity of the disease, the SARS-CoV-2 infection situation in the region, and the medical supply system at each facility, including medical resources, human resources, and the availability of medical equipment. Understanding the diagnostic and treatment environment that the COVID-19 pandemic has dramatically changed is important in providing appropriate surgical care to patients who require surgery while taking utmost care to prevent the spread of COVID-19.
Keywords: colorectal cancer, COVID-19, pandemic, surgery
Introduction
In December 2019, the first case of a new type of infection caused by the new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was reported in Wuhan, China[1]. Symptoms of the novel coronavirus disease 2019 (COVID-19) caused by this novel virus include fever, cough, malaise, and dyspnea[2]. SARS-CoV-2 infections have spread at a very fast rate, overwhelming and disrupting healthcare systems around the world. Consequently, the COVID-19 pandemic was declared by the World Health Organization (WHO) in March 2020 (Figure 1)[3]. Lockdowns and states of emergency were declared in many parts of the world, restricting movement and travel. In January 2020, the first case was reported in Japan. In February 2020, 10 positive cases were confirmed on board the Diamond Princess, which arrived at the port of Yokohama, which eventually led to an outbreak that spread to 696 people[4]. On April 7, 2020, an emergency declaration was issued for Tokyo, Kanagawa, Saitama, Chiba, Osaka, and Hyogo, which was later extended to all prefectures on April 16, 2020. The number of infected people has repeatedly increased and decreased. As of October 2021, there is still no sign of an end to the pandemic (Figure 2).
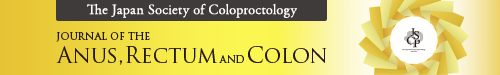
Figure 1.
Trend of COVID-19-infected patients worldwide. Daily cases (A), total cases (B), daily deaths (C), and total deaths (D) are shown. Ordinate: number of cases; abscissa: time series. Data from Johns Hopkins University are available at https://github.com/CSSEGISandData/COVID-19.
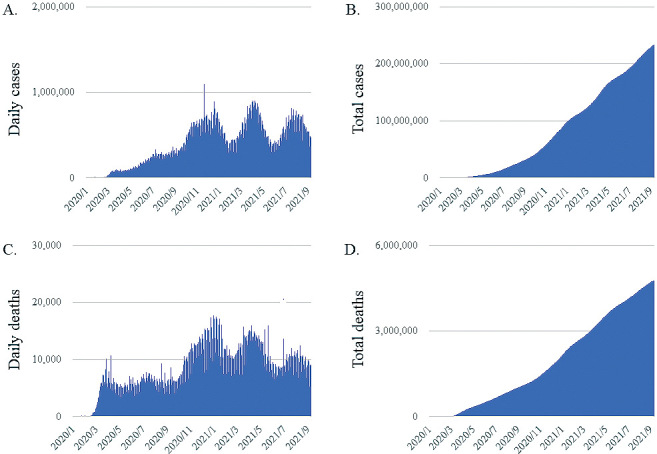
Figure 2.
Trend of COVID-19-infected patients in Japan. Daily cases (A), total cases (B), daily deaths (C), and total deaths (D) are shown. Ordinate: number of cases; abscissa: time series. Data from the Ministry of Health, Labor, and Welfare are available at https://www.mhlw.go.jp/stf/covid-19/open-data.html.
Screening for Colorectal Cancer during the COVID-19 Pandemic
The basic routes of transmission of SARS-CoV-2 are droplet and contact transmission, but recently, the WHO and the Centers for Disease Control and Prevention (CDC) have also mentioned the possibility of airborne transmission[5]. It has been reported that SARS-CoV-2 can survive in the air for several hours, and exposure to highly contaminated aerosol for a certain period of time in a closed space such as an endoscopy room may result in transmission of the virus by aerosol to the person performing the examination, at a high frequency[6]. Although the risk of SARS-CoV-2 infection in upper gastrointestinal endoscopy has been reported, the possibility of viral shedding from feces has also been pointed out, as has the potential risk of infection in colonoscopy[7]. The Japan Gastroenterological Endoscopy Society recommends that the following examinations should be considered for postponement under a declared state of emergency for COVID-19: (1) gastrointestinal endoscopy for screening and surveillance of asymptomatic patients, (2) examinations within 3 years of endoscopic resection of colorectal polyps that are judged to be intact, and (3) gastrointestinal endoscopy for follow-up purposes in which the results do not significantly affect the treatment plan, for example, follow-up examination after endoscopic submucosal dissection with low risk of recurrence[8]. The Japan Gastroenterological Endoscopy Society also lists cases that should not be postponed even under a declared state of emergency, i.e., (1) endoscopy in cases of gastrointestinal bleeding or when gastrointestinal bleeding is suspected, (2) when malignant disease is strongly suspected, (3) gastrointestinal endoscopy as a staging test prior to chemotherapy or surgery, (4) when the endoscopic examination and treatment will change the response to and management of the disease, and (5) when the person in charge of each facility deems it necessary. However, even in the case of nonurgent endoscopic examinations, it cannot be denied that a prolonged suspension may cause serious disadvantages to patients. Therefore, in the absence of a declaration of emergency, it is recommended that regular endoscopic examinations, including those for asymptomatic patients who are not clinically suspected of having COVID-19, should be performed as usual, provided that appropriate triage and reliable infection prevention measures, similar to the New York Society for Gastrointestinal Endoscopy (NYSGE) guidelines, are implemented[9].
Due to the COVID-19 pandemic, only 23.6% of people in Japan were screened in April and May 2020 compared with the previous year (Figure 3)[10]. A study in the United Kingdom reported a 30% decrease in the rate of visits to primary healthcare facilities and a decrease in the number of patients diagnosed with colorectal cancer because screening tests including colonoscopy and CT scans could no longer be performed, due to their restriction to only urgent cases, which had many effects on the healthcare system[11]. From April to May 2020, a survey of 252 centers in 55 countries reported an 85% reduction in the number of lower endoscopies as an effect of the COVID-19 pandemic[12]. The results of a systematic review show that, in general, colorectal cancer screening has decreased by 28%-100% in different countries and at different times after the onset of the COVID-19 pandemic and that completion of colonoscopies requiring examination showed a decrease of 65.7%. There has also been a decrease of 44.6%-79% in surveillance colonoscopy and a 43% decline in referrals to colonoscopy[13].
Figure 3.
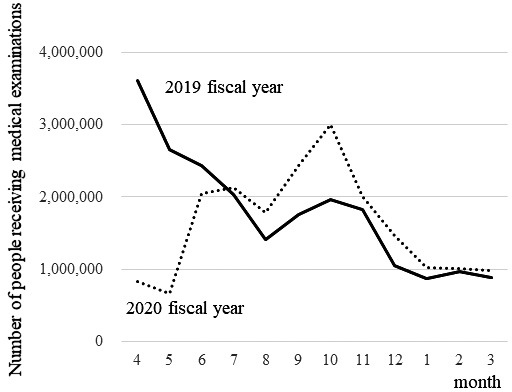
Trend of number of people receiving medical examinations in Japan. Ordinate: number of cases; abscissa: time series. Data from the Japan Society of Health Evaluation and Promotion are available at https://jhep.jp/jhep/top/index.jsp.
When performing gastrointestinal endoscopy, it is advisable to wear personal protective equipment (PPE), including a mask with a face shield (or a mask and goggles), gloves, a cap, and a gown with long sleeves, and change them for each patient whenever possible[14]. After the examination and treatment are completed, the examiner should then wash themselves from fingers to elbows. As for masks, surgical masks are recommended as the standard protective equipment, but since there may be asymptomatic infected patients, the use of N95 masks should be considered even for low-risk patients, considering the situation of infection spread in the region. For high-risk patients, the use of N95 masks is recommended for reliable infection protection. Infection protection measures should be implemented to the maximum extent possible according to the availability of medical resources such as PPE at each facility.
Gastrointestinal endoscopy is recommended only in urgent cases for patients with positive polymerase chain reaction (PCR) or antigen tests for SARS-CoV-2 infection and patients clinically suspicious for COVID-19[15,16]. In symptomatic patients with confirmed SARS-CoV-2 infection, after 10 days since the onset of symptoms and 72 h since the symptoms have abated, or when negative results of two PCR tests are confirmed at intervals of 24 h or more after the symptoms have abated even if 10 days have not passed, they are considered to be cured and can undergo endoscopy as usual[17]. Even when performing gastrointestinal endoscopy on asymptomatic patients not clinically suspected of having COVID-19, the possibility of SARS-CoV-2 positivity should be fully understood, and endoscopy should be performed with reliable infection control measures[18].
A cohort study from the United States evaluated time to colonoscopy and risk and progression of colorectal cancer at diagnosis in patients with positive fecal occult blood. The study found that patients who underwent colonoscopy more than 10 months after a positive fecal occult blood result had a higher frequency of colorectal cancer detection and a higher proportion of advanced disease at diagnosis[19]. Hence, even under a COVID-19 pandemic, patients with a positive result for fecal occult blood should undergo colonoscopy as soon as possible. While the risk of infection in gastrointestinal endoscopy must be taken into account, we must always consider that many patients can be saved by gastrointestinal endoscopy. In the current situation where the battle against COVID-19 will be long, continuing gastrointestinal endoscopy as usual is also required. In addition, although the vaccine is expected to be effective, it is necessary to continue to take reliable infection control measures, mainly the use of PPE, in gastrointestinal endoscopy.
Surgery during the COVID-19 Pandemic
A review of postoperative mortality in 1128 patients with COVID-19 at 235 centers in 24 countries found that the 30-day postoperative mortality rate was 23.8% (268/1128) with respiratory complications occurring in 577 patients (51.2%) and leading to a high mortality rate. This tendency was more pronounced in men over 70 years of age[20]. Since surgery under general anesthesia in COVID-19-infected patients increases the risk of death due to worsening pneumonia, it is better to postpone nonurgent surgery and consider nonsurgical treatment[21-23]. In the American Society of Anesthesiologists (ASA) and Anesthesia Patient Safety Foundation (APSF) Joint Statement, the following recommendations are made regarding the delay of surgery for patients after COVID-19 infection: (1) 4 weeks for an asymptomatic patient or recovery from only mild, nonrespiratory symptoms; (2) 6 weeks for a symptomatic patient (e.g., cough, dyspnea) who did not require hospitalization; (3) 8-10 weeks for a symptomatic patient who is diabetic, immunocompromised, or hospitalized; and (4) 12 weeks for a patient who was admitted to an intensive care unit due to COVID-19 infection[24]. According to a report reviewing postoperative mortality in 3127 previously infected COVID-19 patients and 137,104 previously uninfected patients in 116 countries, the odds ratios (95% confidence intervals) for mortality at 0-2 weeks, 3-4 weeks, and 5-6 weeks after diagnosis of COVID-19 were 4.1 (3.3-4.8), 3.9 (2.6-5.1), and 3.6 (2.0-5.2), respectively, indicating that the mortality rate after 7 weeks was similar to that of patients without prior infection[25]. Furthermore, even after the seventh week post diagnosis, patients with persistent symptoms had a higher mortality rate than those with improving symptoms or asymptomatic patients. Therefore, they reported that surgery should be postponed until at least 7 weeks after diagnosis in patients with a history of COVID-19 infection, and further postponement should be considered in case of symptomatic disease. In the situation of widespread SARS-CoV-2 infection, restrictions on the medical system due to medical shifts to accommodate it will occur, and its impact on surgical treatment is inevitable. Therefore, it is necessary to satisfy all of the following requirements: patient safety, prevention of SARS-CoV-2 exposure of healthcare workers including surgeons, and prevention of nosocomial infection, as well as the decision to treat the primary disease. Surgical triage is required based on comprehensive consideration of the patient's condition, the severity of the disease, the SARS-CoV-2 infection situation in the region, and the medical supply system at each facility, including medical resources, human resources, and the availability of medical equipment. In April 2020, the Japanese Surgical Society recommended that scheduled surgery for nonfatal and nonurgent diseases should be postponed when the medical emergency system is in a tight situation, that surgery for nonfatal but potentially serious diseases should be also postponed if possible, and that surgery should be performed with adequate infection control measures for potentially fatal diseases[26]. In this context, it is also necessary to consider alternative treatments in case of postponement or cancellation of surgery. According to the St. Louis University Elective Surgery Acuity Scale (ESAS)-based surgical triage recommended by the American College of Surgeons (ACS), cancers are classified into two categories. Some low-grade cancers are classified as nonfatal but potentially life-threatening or serious, and surgery for them should be postponed if possible. On the other hand, most cancers are considered potentially fatal if not operated on within a few months, and surgery for them should be performed carefully with adequate infection control measures[27]. Within the first wave of SARS-CoV-2 infection in Japan, the Japanese Society of Anesthesiologists reported that the number of surgeries from the fourth week of April to the fourth week of June decreased to about 80% of the previous year's number nationwide[28]. Detailed data will be reported in the future.
Patients with symptoms suggestive of COVID-19 should be screened by interview 24-48 h prior to surgery, and delaying surgery until 2 weeks after symptoms have improved should be considered. However, because asymptomatic patients can spread COVID-19, it is important to determine the COVID-19 status of patients undergoing surgery[29,30]. Genetic tests (nucleic acid tests) including the reverse transcription polymerase reaction (RT-PCR) and loop-mediated isothermal amplification methods and antigen tests are used to check for SARS-CoV-2 infection. Antigen tests have two types : a qualitative test using a simple kit and a quantitative test using a chemiluminescent enzyme immunoassay. Nucleic acid tests have the highest detection sensitivity, but the procedures are complicated and time-consuming. The antigen test takes less time to obtain results but is less sensitive because it cannot detect a low viral load. If emergency surgery is required and the possibility of SARS-CoV-2 infection cannot be ruled out, it is necessary to test for SARS-CoV-2 infection first, wait for the results, and confirm the presence of pneumonia by chest CT. However, the target patients for PCR testing should be determined in consideration of the prevalence of COVID-19 in each region, the number of tests that can be performed, and the time required to obtain the results.
Aerosols are produced by medical procedures such as endotracheal intubation and extubation, tracheostomy, mask ventilation, bronchoscopy, thoracic drainage, gastrointestinal surgery, and laparoscopic abdominal surgery as well as gastrointestinal endoscopy. All healthcare professionals, especially surgeons and anesthesiologists, should be aware of the high risk of SARS-CoV-2 infection by contaminated aerosols generated by these procedures and should take optimal precautions against exposure to aerosols, as they do during endoscopy. Healthcare professionals should wear PPE to protect themselves when performing surgery or other procedures on patients with confirmed or suspected COVID-19 infection. In situations where the risk of infection from aerosols is high, it is recommended that a higher level of protection be provided by wearing an N95 mask[31]. Tracheal intubation is a high-risk procedure that generates aerosols, and the anesthesiologist should wear enhanced droplet/airborne PPE, avoid conscious intubation, obtain sufficient muscle relaxation to avoid inducing the cough reflex, and ensure that the patient's exhaled air does not leak into the air[32]. Nucleic acid tests may detect SARS-CoV-2 RNA in COVID-19-infected patients for a long time. However, since replication-competent viruses are no longer detected 10 days after the onset of symptoms, the Centers for Disease Control and Prevention (CDC) recommends that isolation and other infection control measures be discontinued after 10 days of symptom onset, 24 h after fever resolution, and when symptoms such as cough and respiratory distress improve[33].
Adverse reactions such as fever often occur 2-3 days after coronavirus vaccination. In addition, there is concern that immunosuppression associated with anesthesia and surgery may suppress antibody production induced by the vaccine. To differentiate these adverse reactions from postoperative inflammation, it is recommended to leave a gap between the vaccination date and the surgery date for elective surgery[34].
Therapeutic Strategies for Colorectal Cancer during the COVID-19 Pandemic
According to the ACS COVID-19 Guidelines for Triage of Colorectal Cancer Patients, it is recommended that treatment for early-stage colorectal cancers be delayed for 3 months when there are few COVID-19 patients, hospital resources are not exhausted, the institution still has ICU ventilator capacity, and the COVID-19 trajectory is not in a phase of rapid escalation. Similar to the recommendation in the United States, the Japan Society of Clinical Oncology suggests that postponing surgery for 3 months is an option for early-stage colorectal cancer when part of a polyp has become cancerous[35]. Additionally, postponement of surgery should be considered for patients with Stage 0-I colorectal cancer when the medical supply system is in a tight situation or when resources such as intensive care unit beds and ventilators are insufficient. However, if delaying surgery for 3 months would adversely affect oncologic outcomes, they suggest that curative resection should be performed without postponement.
In the treatment of resectable Stage II-III colorectal cancer, surgery should be performed carefully with appropriate infection prevention measures, even if the patient is asymptomatic. However, in the case of confirmed COVID-19 cases or suspected cases, or when the medical supply system becomes tight, alternative treatments such as neoadjuvant chemotherapy (NAC) for 2-3 months should be considered, and surgery should be performed carefully with appropriate infection control measures only when it is unavoidable[35]. A strong association between chemotherapy in the past 14 days and severe COVID-19 has been reported, and immunosuppressed status should be taken into account more carefully during the COVID-19 pandemic. Regarding 5-fluorouracil (5-FU) regimens, such as FOLFOXIRI, which frequently cause neutropenia, the dosage and number of concomitant drugs should be considered[36]. Therefore, for NAC regimens, oral chemotherapy is recommended over continuous intravenous 5-FU, which requires the construction of a CV port, to reduce the patient's contact with the hospital and chemotherapy unit, minimizing the risk of infection[37]. Because of the increased risk of toxicity, FOLFOXIRI should be used only when the patient's condition is deteriorating. Based on the above, the National Comprehensive Cancer Network suggests capecitabine or CAPOX as candidates for NAC regimens[38]. It has also been reported that postoperative adjuvant chemotherapy for high-risk Stage II and Stage III patients is not actively recommended, but it may be necessary to shorten the administration period or consider switching to oral chemotherapy[36]. For advanced rectal cancer, neoadjuvant chemoradiotherapy (NACRT), which is the standard in Europe and the United States, is not actively performed in Japan at present. In facilities where surgery is usually performed without NACRT, curative surgery should be performed with appropriate infection prevention measures if the impact of COVID-19 is minimal. In Europe, during the COVID-19 pandemic, short-course radiation therapy (5 Gy × 5 sessions) is recommended to reduce the risk of infection in patients with T3N0 rectal cancer less than 12 cm from the anal canal. For patients with T3-4 and/or N + rectal cancer less than 12 cm from the anal verge, total neoadjuvant therapy is strongly recommended[36,39].
Although the effects of specific aerosols of SARS-CoV-2 are still unclear, a recent study reported that surgeons are less exposed to surgical smoke in laparoscopic surgery than in open surgery[40,41]. The association between surgical smoke and viruses has been widely reported for HPV and HBV. Although SARS-CoV-2 has been found in blood and stool, it has not yet been identified within surgical smoke, but the risk of infection cannot be ruled out and should be noted. In the COVID-19 pandemic, the use of more complex endoscopic systems with ULPA filters, which are capable of removing 99.9% of particles larger than 0.12 um in diameter, has been recommended. The possibility of infection due to intra-abdominal gas leakage around the trocar cannot be ruled out, and further studies are warranted[42,43]. Transanal total mesorectal excision (TaTME) should be avoided during the COVID-19 pandemic because it is associated with high-flow insufflation and clearly increases the exposure to surgical smoke[40].
The Japan Surgical Society recommends that emergency surgery be performed only on patients who have no option of choosing nonoperative treatment[44]. In the case of colorectal cancer ileus, which can be fatal if not operated within a few days, that is, if there is no other treatment such as stent insertion or ileus tube insertion, and frequent blood transfusion is required due to bleeding from the tumor, or if perforation or sepsis occurs, SARS-CoV-2-positive patients or suspected COVID-19 patients are also indicated for emergency surgery[39]. In an emergency surgery, the medical personnel should take adequate infection prevention measures, including full PPE. If bowel decompression can be achieved by stenting or transanal ileus tube insertion, it is possible to perform the surgery on a standby basis. However, care must be taken to prevent infection in SARS-CoV-2-infected or suspected cases, because fluoroscopic endoscopy is required for these procedures. Regarding laparoscopic surgery in emergency surgery, the risk of infection due to aerosol generation cannot be denied at present, and only cases with an extremely low possibility of infection should be subjected to laparoscopic surgery[45].
Conclusions
The COVID-19 pandemic has dramatically changed the diagnostic and treatment environment for colorectal cancer. Although one cohort study in Japan reported that significantly fewer patients were diagnosed with Stage I gastric and colorectal cancers during the COVID-19 pandemic, its impact on colorectal cancer has not been fully studied[46]. In order to provide appropriate surgical care to patients who require surgery, while taking the utmost care to prevent the spread of COVID-19 infection, the Clinical Study Group of Osaka University is currently collecting data retrospectively at multiple institutions and analyzing the effect of the COVID-19 pandemic on the diagnostic and treatment environment for colorectal cancer. It will be important to understand the change in consultation behavior caused by COVID-19.
Conflicts of Interest
There are no conflicts of interest.
Author Contributions
All authors made substantial contributions to the study and met all four criteria for authorship.
References
- 1.Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020 Mar; 579(7798): 270-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020 Feb; 395(10223): 514-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization [Internet]. WHO Director-General's opening remarks at the Member States information session on COVID-19 - 11 March 2021. 2021 Mar 11. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-member-states-information-session-on-covid-19---11-march-2021
- 4.Wang C, Horby PW, Hayden FG, et al. A novel coronavirus outbreak of global health concern. Lancet. 2020 Feb; 395(10223): 470-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu IT, Li Y, Wong TW, et al. Evidence of airborne transmission of the severe acute respiratory syndrome virus. N Engl J Med. 2004 Apr; 350(17): 1731-9. [DOI] [PubMed] [Google Scholar]
- 6.van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020 Apr; 382(16): 1564-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gu J, Han B, Wang J. COVID-19: gastrointestinal manifestations and potential fecal-oral transmission. Gastroenterology. 2020 May; 158(6): 1518-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Japan Gastroenterological Endoscopy Society [Internet]. Q&A on gastrointestinal endoscopy for new coronavirus infections. 2021 Jun 15. Available from: https://www.jges.net/medical/covid-19-qa#cq3
- 9.New York Society for Gastrointestinal Endoscopy [Internet]. New York Society for Gastrointestinal Endoscopy Guidelines for Endoscopy Units during the COVID-19 Pandemic. 2020 Mar 16. Available from: https://www.nysge.org/Files/NYSGE%20Guidelines%20for%20Endoscopy%20Units%20During%20the%20COVID-19%20Pandemic.pdf
- 10.Japan Society of Health Evaluation and Promotion [Internet]. Results of a fact-finding survey on the trend of health checkup recipients and the impact on health checkup institutions due to the spread of new coronavirus infection. 2021 Jun 30. Available from: https://jhep.jp/jhep/sisetu/pdf/coronavirus_25.pdf
- 11.Morris EJA, Goldacre R, Spata E, et al. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: a population-based study. Lancet Gastroenterol Hepatol. 2021 Mar; 6(3): 199-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parasa S, Reddy N, Faigel DO, et al. Global impact of the COVID-19 pandemic on endoscopy: an international survey of 252 centers from 55 countries. Gastroenterology. 2020 Oct; 159(4): 1579-81.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mazidimoradi A, Tiznobaik A, Salehiniya H. Impact of the COVID-19 pandemic on colorectal cancer screening: a systematic review. J Gastrointest Cancer. 2021 Aug: 1-15. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Niikura R, Fujishiro M, Nakai Y, et al. International observational survey of the effectiveness of personal protective equipment during endoscopic procedures performed in patients with COVID-19. Digestion. 2021 Feb; 102(6): 845-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang J, Du G. COVID-19 may transmit through aerosol. Ir J Med Sci. 2020 Nov; 189(4): 1143-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 Apr; 382(18): 1708-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walsh KA, Spillane S, Comber L, et al. The duration of infectiousness of individuals infected with SARS-CoV-2. J Infect. 2020 Dec; 81(6): 847-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhu J, Ji P, Pang J, et al. Clinical characteristics of 3062 COVID-19 patients: a meta-analysis. J Med Virol. 2020 Oct; 92(10): 1902-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Corley DA, Jensen CD, Quinn VP, et al. Association between time to colonoscopy after a positive fecal test result and risk of colorectal cancer and cancer stage at diagnosis. Jama. 2017 Apr; 317(16): 1631-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.COVIDSurg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020 Jul; 396(10243): 27-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aminian A, Safari S, Razeghian-Jahromi A, et al. COVID-19 outbreak and surgical practice: unexpected fatality in perioperative period. Ann Surg. 2020 Jul; 272(1): e27-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Knisely A, Zhou ZN, Wu J, et al. Perioperative morbidity and mortality of patients with COVID-19 who undergo urgent and emergent surgical procedures. Ann Surg. 2021 Jan; 273(1): 34-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020 Mar; 21(3): 335-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.ASA and APSF [Internet]. ASA and APSF Joint Statement on Elective Surgery and Anesthesia for Patients after COVID-19 Infection. 2021 Mar 9. Available from: https://www.asahq.org/about-asa/newsroom/news-releases/2021/03/asa-and-apsf-joint-statement-on-elective-surgery-and-anesthesia-for-patients-after-covid-19-infection-rv
- 25.Lobo D, Devys JM. Timing of surgery following SARS-CoV-2 infection: an international prospective cohort study. Anaesthesia. 2021 Jul. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mori M, Ikeda N, Taketomi A, et al. COVID-19: clinical issues from the Japan Surgical Society. Surg Today. 2020 Aug; 50(8): 794-808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.American College of Surgeons [Internet]. COVID-19: Guidance for Triage of Non-Emergent Surgical Procedures. 2020 Mar 17. Available from: https://www.facs.org/%20covid-19/clinical-guidance/triage
- 28.Japanese Society of Anesthesiologists [Internet]. Our response to the new coronavirus infection (COVID-19). 2021 Sep 21. Available from: https://anesth.or.jp/
- 29.Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020 Mar; 382(10): 970-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Suehiro K. Preoperative assessment for scheduling surgery during the coronavirus disease pandemic. J Anesth. 2021 Jun; 35(3): 378-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020 May; 67(5): 568-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zuo MZ, Huang YG, Ma WH, et al. Expert recommendations for tracheal intubation in critically ill patients with novel coronavirus Disease 2019. Chin Med Sci J. 2020 Feb; 35(2): 105-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention [Internet]. Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic. 2021 Sep 10. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhcp%2Fdisposition-hospitalized-patients.html
- 34.Centers for Disease Control and Prevention [Internet]. Interim Clinical Considerations for Use of COVID-19 Vaccines Currently Approved or Authorized in the United States. 2021 Nov 3. Available from: https://www.cdc.gov/vaccines/covid-19/clinical-considerations/covid-19-vaccines-us.html
- 35.Japan Society of Clinical Oncology [Internet]. New Coronavirus Infection (COVID-19) and Cancer Treatment. 2021 Feb 2. Available from: http://www.jsco.or.jp/jpn/index/page/id/2333
- 36.Lou E, Beg S, Bergsland E, et al. Modifying practices in GI oncology in the face of COVID-19: recommendations from expert oncologists on minimizing patient risk. JCO Oncol Pract. 2020 Jul; 16(7): 383-8. [DOI] [PubMed] [Google Scholar]
- 37.National Comprehensive Cancer Network [Internet]. COVID-19 Resources. 2021 Jan 28. Available from: https://www.nccn.org/covid-19
- 38.Liu F, Yang L, Wu Y, et al. CapOX as neoadjuvant chemotherapy for locally advanced operable colon cancer patients: a prospective single-arm phase II trial. Chin J Cancer Res. 2016 Dec; 28(6): 589-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Di Marzo F, Fiori E, Sartelli M, et al. SARS-CoV-2 pandemic: implications in the management of patients with colorectal cancer. New Microbiol. 2020 Oct; 43(4): 156-60. [PubMed] [Google Scholar]
- 40.Wexner SD, Cortés-Guiral D, Gilshtein H, et al. COVID-19: impact on colorectal surgery. Colorectal Dis. 2020 Jun; 22(6): 635-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pavan N, Crestani A, Abrate A, et al. Risk of virus contamination through surgical smoke during minimally invasive surgery: a systematic review of the literature on a neglected issue revived in the COVID-19 pandemic era. Eur Urol Focus. 2020 Sep; 6(5): 1058-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kameyama H, Otani T, Yamazaki T, et al. Comparison of surgical smoke between open surgery and laparoscopic surgery for colorectal disease in the COVID-19 era. Surg Endosc. 2021 Feb: 1-8. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dalli J, Khan MF, Nolan K, et al. Laparoscopic pneumoperitoneum escape and contamination during surgery using the airseal insufflation system - a video vignette. Colorectal Dis. 2020 Sep; 22(9): 1029-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Japan Surgical Society [Internet]. 2020 Apr 10. Recommendations for surgical procedures in patients with positive or suspected novel coronaviruses. Available from: https://www.jssoc.or.jp/aboutus/coronavirus/info20200402.html
- 45.Zheng MH, Boni L, Fingerhut A. Minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann Surg. 2020 Jul; 272(1): e5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kuzuu K, Misawa N, Ashikari K, et al. Gastrointestinal cancer stage at diagnosis before and during the COVID-19 pandemic in Japan. JAMA Netw Open. 2021 Sep; 4(9): e2126334. [DOI] [PMC free article] [PubMed] [Google Scholar]