Abstract
Introduction:
Patients are at increased risk for death by suicide following a psychiatric hospitalization. There has been limited study of the association between patient engagement in follow-up care after psychiatric hospitalization and suicide risk. Understanding why psychiatric inpatients choose to engage in post-discharge care is important in developing effective suicide prevention strategies.
Materials and Methods:
The theory of planned behavior (TPB) has been widely used to understand many health behaviors including healthcare utilization. Using the TPB, we developed an interview guide that assessed psychiatric inpatients’ attitudes and beliefs about the role of post-discharge care in addressing suicide risk. We also inquired about perception of future risk for suicide after discharge. We conducted semi-structured interviews prior to discharge and administered the Columbia-Suicide Severity Rating Scale (C-SSRS). We assessed healthcare utilization at 1 and 3 mo after discharge. We coded and grouped the transcribed data according to the three domains of the TPB model: attitudes, subjective norms, and perceived behavioral control.
Results:
Sixteen individuals consented to enrollment. More than half (N = 10) believed that they were at no or low future suicide risk after discharge. Participants who felt that their future risk for suicide was low or none were significantly older (mean 59.3 yr, SD: 8.3) and reported significantly less severe suicidal ideation in the past month (mean CSSR-S 2.5, SD 2.1) compared to those participants who believed that their future risk was high (mean age 47.5, SD: 8.6; mean CSSR-S 4.7, SD 0.5, p < 0.05). However, all participants had a lifetime history of severe suicidal ideation (mean CSSR-S > 4.7). Many participants felt that peers facilitated treatment engagement. However, participants expressed a tendency to avoid treatment if they experienced unwanted side effects, encountered stigma, or experienced poor-therapeutic alliance. Five participants experienced poor continuity of care after discharge. Of these participants, four reported at the time of discharge no or low perceived future risk of suicide and three were readmitted within 90 d after discharge.
Conclusions:
Individuals may not appreciate that they are at heightened risk for suicide after hospitalization and this may negatively impact treatment engagement.
INTRODUCTION
Suicide is an important public health problem, with more than 800,000 people dying by suicide each year across the globe.1 Individuals are at particularly high risk for suicide in the year following psychiatric hospitalization,2–5 with the highest risk occurring in the first 3 mo after discharge.6 Several factors may contribute to suicide risk including psychiatric comorbidity and history of suicidal behavior.3 An important, but understudied area, includes the association between patient engagement in follow-up care and the risk for suicide risk after psychiatric hospitalization.3,4 While several studies have found that patients with a history of suicidal behavior and suicidal ideation are more likely to be non-adherent to treatment,7–9 relatively little is known about the factors that may motivate or dissuade patients from partaking in treatment. Some studies have suggested that fear of stigma, concerns about side effects of medications and poor-therapeutic alliance may contribute to treatment non-adherence.10–13 It is unclear, however, whether a similar group of factors plays a role in poor patient engagement in follow-up care after psychiatric hospitalization.
Social and behavioral theories are commonly used to understand the behaviors of individuals and to develop effective health promotion interventions.14,15 The theory of planned behavior (TPB) has been widely used to understand many health behaviors including healthcare utilization.16 The TPB emphasizes that intention plays a key role in an individual’s decision to make a behavior change.17 Intention is also directly influenced by the individual’s attitudes about the effect of the behavior, subjective norms, and the individual’s perceived ability to control his/her behavior.17 The TPB model has been proven to predict an individual’s intention to participate in health promoting behaviors.18 The TPB model has also been used in the study of help seeking behaviors among individuals with mental health disorders.13,19–22 For example, in a study of patients with and without depression, Schomerus et al23 found that attitudes about mental health treatment, as conceptualized by the TPB model, were strongly correlated with intention to seek treatment. Similarly, Stecker et al. (2012) used the TPB model in the design of an intervention which improved treatment engagement in Veterans with alcohol use disorder.24
Given that the TBP has been successfully applied to the field of mental health, the TBP may be useful in exploring the reasons why an individual with risk factors for suicide may choose to engage – or not engage – in mental health treatment after psychiatric hospitalization.25–27 Therefore, using the framework of the TBP, we designed a mixed-methods study which was aimed at understanding psychiatric inpatients’ attitudes and beliefs about suicide risk and treatment after discharge. The results of our study will help to identify potential motivational factors that may impact patient engagement in treatment after psychiatric hospitalization. This knowledge may be useful in the design of effective interventions to prevent death by suicide after psychiatric hospitalization.
METHODS
We carried out a mixed-methods study of participants who were hospitalized on a Veterans Affairs (VA) inpatient mental health unit and were deemed clinically fit to be discharged back to the outpatient setting. We conducted individual, open-ended, semi-structured interviews with participants around the time of discharge. We administered standardized assessment tools at baseline and collected data on healthcare utilization in the 3 mo following discharge. We conducted the study between January 1, 2017 and September 30, 2017.
We used convenience sampling to identify eligible participants. We recruited participants regardless of the reason for their admission because the risk for suicide after hospitalization spans across psychiatric disorders.6 We obtained signed consent from all participants. None of the participants received compensation for participation in the study. The principle investigator (NR) conducted the semi-structured interviews. The Veteran’s institutional review board of Northern New England (VINNE) and the Research and Development Committee, White River Junction Veterans Affairs Medical Center (WRJ VAMC) approved this project after full committee review.
We developed an interview guide to facilitate the semi-structured interviews. The guide was designed to elicit information which addressed the TPB domains including: attitude, subjective norm, and perceived behavioral control.17 To assess attitudes about follow-up care, the interviewer asked participants to comment on the advantages and disadvantages of follow-up care. The interviewer also asked participants to comment specifically on whether they personally believed that they were at future risk for suicide at any time after discharge. To assess subjective norms, the interviewer asked participants to comment on what role (if any) others played in their decision to engage in follow-up care. To assess perceived behavioral control, the interviewer asked participants to comment on factors that would facilitate or hinder treatment engagement.
We used an iterative approach to ensure that the interview guide adequately reflected our variables of interest. We completed two initial interviews and debriefed these results as a team. We determined that minor modifications were necessary and after incorporating these changes and piloting them in two more participants, reached consensus that the interview guide was complete. This method of reflexivity, reflection, and adaptation helped to minimize the problem of measurement bias.
Enrolled participants were interviewed in private rooms on the inpatient unit on the day before (or day of) discharge. The conversations were audio recorded and results were later transcribed. Audio recordings were complemented by observational field notes. The interviews lasted approximately 60 min.
We administered three standardized assessment tools at baseline including the Columbia-Suicide Severity Rating Scale (C-SSRS)28 (a measure of suicidal ideation and behavior), the Interpersonal Needs Questionnaire (INQ),29,30 (a measure of perceived burdensomeness and thwarted belongingness), and the Dimensions of anger reactions (DAR-7)31 (a measure of anger). These instruments are applicable to individuals with a variety of diagnostic conditions and have been found to be associated with suicide risk.29,30,32 Higher scores on each of these scales indicate more severe symptom burden.
We used the medical record to collect baseline diagnostic information (discharge diagnosis, gender and age) and to measure continuity of mental healthcare within the first 3 mo after discharge. We abstracted these data through chart review in the VA electronic medical record (VistA). Measures of post-hospitalization continuity of care included intensity of outpatient mental health treatment (total number of visits between the time of discharge and the first 3 mo after discharge), regularity of outpatient mental health treatment (number of consecutive months in the first 3 mo after discharge in which the participant had at least one mental health visit; range, zero to three), and continuity of mental health treatment across intra-organizational boundaries (whether or not the participant received any outpatient mental health treatment within the first month after discharge).33 We evaluated whether participants had lower or higher values on one or more these continuity of care measures because higher continuity of care has been associated with superior mental health outcomes.33 We defined least continuity of care as zero to two outpatient mental health visits, zero months of continuous outpatient mental health treatment and/or no outpatient mental health treatment within 1 mo of discharge.
Using Atlas.ti software (Version 7.5.16), we coded and grouped the transcribed data according to the domains of the TPB model (attitudes, subjective norms, and perceived behavioral control). Within each domain, we then sub-categorized the coded data into related sub-domains. Furthermore, we classified sub-domains based on whether the sub-domain could be considered to be a facilitator or barrier to treatment engagement. Because our interview guide included one question that did not map onto the TPB model (i.e., participant’s perceived future risk for suicide at any time after discharge), we created a separate category for this domain. We coded participant’s responses as “perceived low or no future risk” if the participant explicitly stated that he was at no future risk or he expressed that he believed it was very unlikely that his suicidal ideation would re-emerge or worsen again. Conversely, we coded participant’s responses as “perceived high future suicide risk” if the participant reported that he felt very strongly that it was likely that his suicidal ideation could worsen again in the future. We involved two analysts (NR and BS) in coding the qualitative data because this is considered a more rigorous approach to qualitative analysis and permits multiple perspectives and resolution of discrepancies through consensus.34
We used simple descriptive statistics to describe the results of scales, baseline diagnostic information, and continuity of care after discharge. For continuous measures, we used the student t-test to evaluate for significant differences between the means of participants who perceived their future risk for suicide was low or none versus high. For dichotomous outcomes, we evaluated for significant differences between proportions using the chi-squared test. We conducted these analyses using STATA version 14 (StataCorp). We considered a p-value <0.05 to be significant.
RESULTS
Among 22 eligible participants, 16 participants consented to enrollment and participated in a semi-structured interview prior to hospital discharge. As shown in Table I, all participants were men. More than half of the participants (N = 10) believed that their future risk for suicide was low or none. Participants who felt that their future risk for suicide was low or none were significantly older (mean 59.3 yr, SD: 8.3) and reported significantly less severe suicidal ideation in the past month (mean CSSR-S 2.5, SD 2.1) compared to those participants who believed that their future risk was high (mean age 47.5, SD: 8.6; mean CSSR-S 4.7, SD 0.5, p < 0.05). All participants had a lifetime history of severe suicidal ideation (mean CSSR-S > 4.7). Finally, 30% (3/10) of participants who believed that their future risk of suicide was low or none and 50% (3/6) of participants who believed that their future risk of suicide was high had a clinical alert (“flag”) in their medical record, identifying them as acutely at elevated risk for suicide. This clinical alert system is standard practice in the VA.
TABLE I.
Baseline Characteristics of Subjects Stratified by Self-reported Perception of Future Risk of Suicide
| Subject’s Self-Report Perception of Future Suicide Risk |
||
|---|---|---|
| Low Risk | High Risk | |
| Number endorsed | 10 | 6 |
| Gender, male, % (N) | 100.0 (10) | 100.0 (6) |
| Mean age, years (SD) | 59.3 (8.3) | 47.5 (8.6)** |
| Clinical history | ||
| Primary diagnosis at discharge | ||
| Major depressive disorder, % (N) | 60.0 (6) | 50.0 (3)* |
| Post-traumatic stress disorder, % (N) | 10.0 (1) | 17.0 (1)* |
| Schizoaffective disorder, % (N) | 10.0 (1) | 17.0 (1)* |
| Alcohol use disorder, % (N) | 10.0 (1) | 17.0 (1)* |
| Bipolar disorder, % (N) | 10.0 (1) | 0.0 (0)* |
| History of suicide attempt, % (N) | 40.0 (4) | 66.7 (4)* |
| History of prior hospitalization, % (N) | 80.0 (8) | 100.0 (6)* |
| Clinical alert in medical record for high suicide risk, % (N) | 30.0 (3) | 50.0 (3)* |
| Mean length of stay, days (SD) | 12.9 (10.3) | 8.8 (7.7)* |
| Results of standardized assessments at the time of discharge | ||
| Suicidal ideation – lifetime, CSSR-S mean (SD) | 4.7 (0.67) | 5.0 (0)* |
| Suicidal ideation – past month, CSSR-S mean (SD) | 2.5 (2.1) | 4.7 (0.5)** |
| Anger symptoms at discharge, DAR-7 mean (SD) | 19.9 (16.5) | 20.3 (17.4)* |
| Perceived burdensomeness at discharge, INQ-25 subscale mean (SD) | 27.9 (14.2) | 52.5 (15.9)*** |
| Thwarted belongingness at discharge, INQ-25 subscale mean (SD) | 22.4 (16.2) | 36.4 (15.1)* |
INQ-25, Interpersonal Needs Questionnaire-25; N, number; SD, standard deviation.
p > 0.05;
p < 0.05;
p < 0.01.
Figure 1 outlines how participants’ attitudes and beliefs about the role of post-discharge care in addressing their future risk for suicide mapped onto the TBP framework. Table II includes quotes that mapped onto the three TBP constructs as well as quotes that mapped onto the theme of perceived risk.
FIGURE 1.
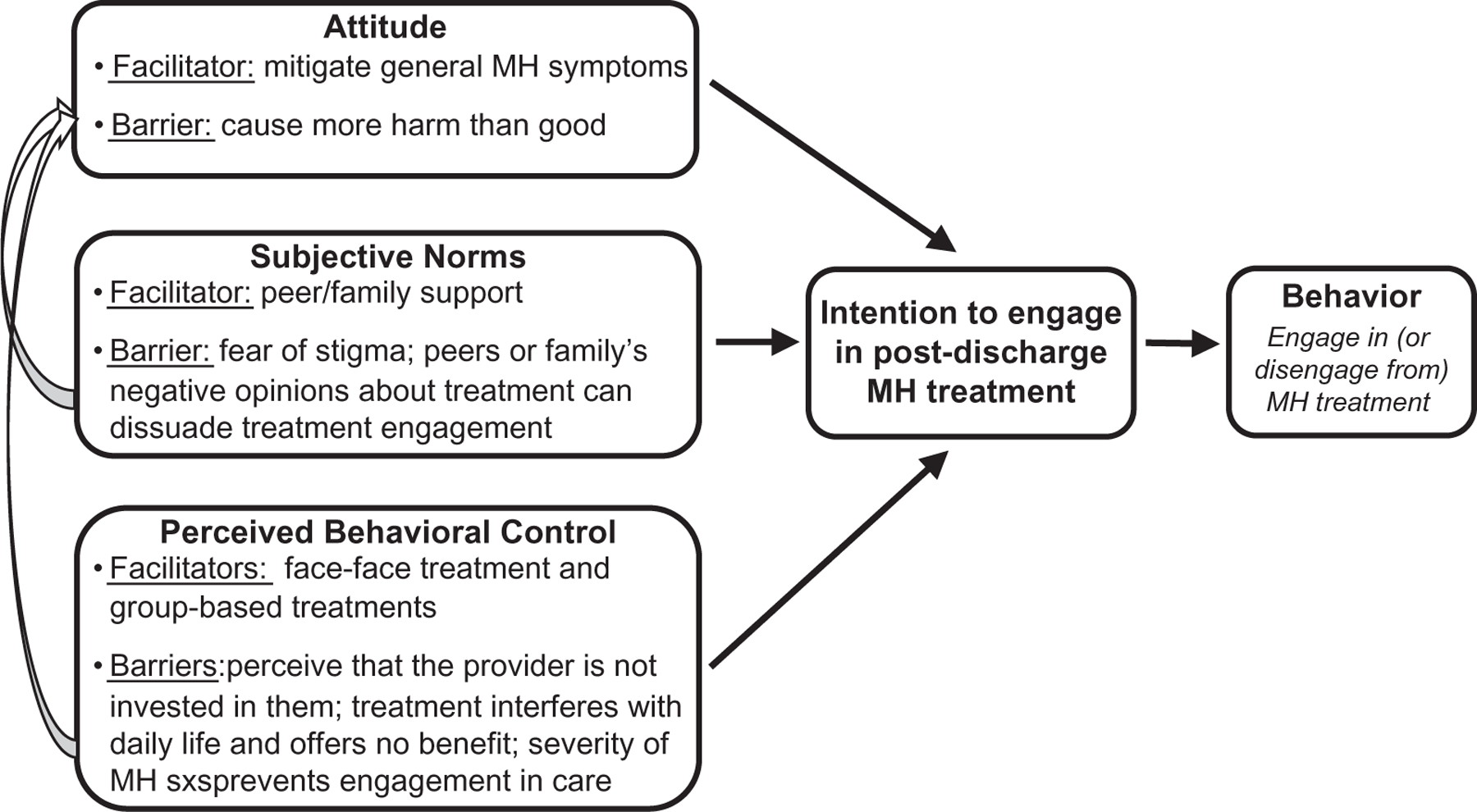
Application of the TPB framework to the evaluation of inpatient mental health patients’ attitudes and beliefs about the role of post-discharge care in addressing suicide risk. MH, mental health; Sxs, symptoms. *Figure is adapted from the TPB Model developed by Ajzen.17
TABLE II.
Attitudes and Beliefs About the Role of Follow-up Care in Addressing Suicide Risk After Hospital Discharge
| Domain | Sub-domain | Quotes from Participants |
|---|---|---|
| TPB constructs | ||
| Attitudes | Facilitator: treatment may help to mitigate general mental health symptoms | • “If my depression came back in a major way, it could help.” |
| • “I don’t fall so far.” | ||
| • “It will help me with voices.” | ||
| • “It will help me make better decisions.” | ||
| Barrier: Treatment may cause more harm than good to the individual | • “Medications come at an extremely high price. They can do great things and they can also be dangerous.” | |
| • “For short-term crisis situation, medications can be beneficial. But, side-effects don’t justify the benefits.” | ||
| • “The medications stabilized my mood, but physically screwed me up.” | ||
| Subjective norms | Facilitator: support from peers or family can facilitate engagement in care | • “We trust each other. We are brothers and sisters.” |
| • “We have a commonality and a history.” | ||
| • “My wife and daughter inspire me to come back.” | ||
| • “I am willing to do anything because my family is behind me, like my touch stone.” | ||
| • “Whole bunch of people behind me, I don’t have to carry the burden by myself.” | ||
| • “They [family] help to take the sting out of being here [hospitalized].” | ||
| Barrier: fear of being stigmatized can prevent engagement in care | • “I am embarrassed to be here [hospitalization]. I didn’t want anyone to know it. I didn’t want to seek treatment. It’s like a weakness.” | |
| • “If they [my family] shunned me, it would be hard.” | ||
| • “I don’t want to tell anyone I was here. I may scare people. My biggest concern is about being accepted.” | ||
| • “[There is a] social stigma of seeking and receiving care.” | ||
| • “People think you are crazy.” | ||
| • “We should buck up.” | ||
| Barrier: family/peers’ negative opinions about treatment can dissuade the individual from partaking in treatment | • “Based on what I have heard from other Veterans, it [lithium] makes you gain weight. It’s an extreme treatment and I am not interested in taking it.” | |
| • “I won’t do it [treatment] if I heard from other Veterans that it was a bad idea.” | ||
| Perceived behavioral control | Facilitator: face–face mental health treatment can facilitate engagement in care | • “The provider sees your emotions and can tell your affect and you won’t get that on the phone.” |
| • “The physical cues may be more important than what the person says.” | ||
| • “I want them to see my facial expressions and see my body language. They can then pick up on how I am doing.” | ||
| • “I can tell if they [the provider] are worried and that would make me worried.” | ||
| • “Body language and facial expression is very important. It’s a lot about emotions.” | ||
| Facilitator: group-based treatments can facilitate engagement in treatment | • “There is the ability to share and find out what works for others and didn’t work for me.” | |
| • “Help to develop some camaraderie with other Veterans.” | ||
| • “Its support for me and for them.” | ||
| Barrier: the perception that the provider is not invested in their personal well-being can lead the individual to disengage from care | • “I would turn it [treatment] down if they aren’t interested in fixing me.” | |
| • “I can see if they [the providers] are rolling their eyes.” | ||
| • “I am just being used as a guinea pig.” | ||
| • “I don’t want to be used as a lab rat.” | ||
| • “It’s constructive for them [providers] but not for me.” | ||
| Barrier: the perception that treatment interferes with daily life or provides no benefit can lead the individual to disengage from care | • “It gets on my nerves. It takes up time.” | |
| • “I won’t do it if I didn’t think it would help.” | ||
| • “It’s redundant and unnecessary.” | ||
| • “It’s more work than help.” | ||
| • “It’s way out of my way and more of a hassle than a help.” | ||
| • “I forget about it because it’s not important to me.” | ||
| • “It’s time-consuming. It’s disruptive to my well-being.” | ||
| Barrier: the severity of an individual’s mental health symptoms can lead the individual to disengage from care | • “Slow descent happens, it’s an avalanche and then it’s hard to seek help.” | |
| • “I deny the signs. I can’t see it or I won’t admit it.” | ||
| • “When I am really depressed, I don’t feel like doing anything.” | ||
| • “When I get sick, I isolate. I stay away from doctors.” | ||
| • “If I get so depressed that I would say it doesn’t help anyways, screw it.” | ||
| Perception of future suicide risk after discharge | ||
| Perception of future risk | Individual perceives that they are at low or no future risk for death by suicide | • “I don’t foresee that, at least not for right now. I got more ammunition to fight it [suicidal thoughts] then before coming into the hospital.” |
| • “I am extremely hopeful that it won’t happen and that is why I am here.” | ||
| • “No, I have a lot of hope for the future. This [hospitalization] was an “awesome” experience and I can hang my hat on that.” | ||
| • “No…they [suicidal thoughts] are getting shorter and I can deal with it better. I feel I am better able to manage them because I have learned the skills. Before it would have lingered. When I came in, I was incapacitated, but with these medications I have seen a positive change.” | ||
| • “I feel good and am like my old self. Being on Ground East [the inpatient mental health unit] took care of it [suicidal symptoms] and I can now live my life.” | ||
| Individual perceives that they are at high future risk for death by suicide | • “I can’t predict when it [suicidal symptoms] will happen.” | |
| • “Nothing I can do, it [suicidal symptoms] will happen in the future.” | ||
| • “First I am fine and then it [suicidal symptoms] creep back in slowly and then it gets full blown.” | ||
| • “Based on personal experience, the “on-switch” and “dimmer switch” have been turned on and you can never shut it off completely.” | ||
| • “Yes, I would be lying to myself if I denied it. My life situation is a big contribution and I have a label for it, the flag in my medical record.” | ||
| • “It’s [follow-up care] something that I need to prevent me from being suicidal” | ||
| • “I need to get on the horse. I know what I mostly what I have to do and hopefully it helps. Follow-up care is an important thing. [Otherwise] you could end up being readmitted or you could end up in a box.” | ||
Perception of Suicide Risk
Many participants did not perceive that follow-up care plays a critical role in addressing suicide risk. In fact, more than half of participants (N = 10) believed that they were at low or no future risk for suicide because the current hospitalization had completely (or nearly completely) addressed this risk. Yet, a few participants (N = 6) felt acutely aware of their risk for suicide and believed that follow-up care was necessary to mitigate this risk. Participants typically came to this conclusion because they had a history of severe suicidal ideation, had been hospitalized multiple times or had been told about the risk by their provider.
Attitudes About Post-discharge Treatment
Almost all participants (N = 15) believed that post-discharge care is important in managing general mental health symptoms such as depression. Yet, most participants (N = 12) raised concerns that in some cases, the treatment may cause more harm than good. For example, three participants suggested that behavioral interventions could “trigger” post-traumatic stress disorder symptoms. One participant mentioned, “I could be inundated with questions and get stirred up.” Eleven participants highlighted that there is a high likelihood that medications could cause substantial side effects.
Subjective Norms and Post-discharge Treatment
Many participants (N = 9) emphasized that peers were critical in supporting them through their treatment. For example, one participant described that his “vet group” was important because “we keep track of each other and that keeps us stable.” In fact, he mentioned that prior to this admission he told his “vet group” about recently purchasing a gun. The group pointed out to him that this was a warning sign for suicide and helped him to seek re admission. A few participants (N = 6) suggested that it was helpful to receive support from family. Six participants, however, raised concerns that fear of stigma prevented them from seeking treatment. In addition, four participants mentioned that if their peers or family expressed negative opinions about treatment, they would turn down the treatment.
Perceived Behavioral Control and Post-discharge Treatment – Facilitators
Fifteen participants felt more favorable about treatment when it was delivered face–face because they believed that this modality was more personal and therapeutic. Five participants described that they would be more open to group-based interventions, especially if they included Veterans. One participant was particularly interested in working with a peer support specialist, saying that it was helpful because “they can relate and they are not judging you.”
Perceived Behavioral Control and Post-discharge Treatment – Barriers
Seven participants expressed that an important barrier to engaging in treatment included the perception that the provider was not invested in their personal well-being. Participants described avoiding treatment when they felt that they were being “forced” or “pushed” into treatment to fulfill the provider’s agenda. One participant described that he would get upset if he felt that a provider was deciding the frequency of follow-up visits without considering his needs. The participant raised this concern in the context of the clinical process whereby some patients are “flagged” as high risk in the medical record and thus, require a set number of appointments. The participant reported, “I don’t like that. It feels like a ball and chain. The only goal is you want to do everything to take the red flag off my record, so I fake the funk. I say something to make it ok for them. I don’t see the team working to my advantage so I have taken things in my own hands.” Participants also believed they would turn down treatment if they perceived no benefit (N = 7) or the treatment interfered with their life (N = 7).
Finally, six participants mentioned that if their mental health symptoms became too severe, they would disengage from care. Many of these six participants were also unsure about how to handle this rapid decline in their mental health symptoms. For example, one participant mentioned, “Now I can recognize when I am headed there, but I don’t have all the tools to stop it when I am heading there.” Yet, one participant felt confident that because he had involved his family in his treatment, he would be able to get necessary care even if the severity of his symptoms precluded engagement. He stated, “It has helped to have my family look for the cues and let me know.”
Continuity of Care After Discharge
Table III outlines continuity of care in the first 3 mo after hospitalization and their in-person interview. Most of the participants who believed that their future risk for suicide was high experienced greater continuity of care after discharge. Conversely, there was more variation in the degree of continuity of care experienced by participants who believed that their future suicide risk was low or none. Finally, none of the 16 participants in this study received non-VA mental healthcare after hospital discharge.
TABLE III.
Continuity of Care Within 3 mo After Psychiatric Hospitalization Stratified by Self-reported Perception of Future Risk of Suicide
| Subject’s Self-Report Perception of Future Suicide Risk |
||
|---|---|---|
| Low Risk | High Risk | |
| Number endorsed | 10 | 6 |
| Measures of continuity of care within 3 mo of discharge, % (N) | ||
| Intensity of outpatient mental health treatment | ||
| Low intensity of outpatient MH treatment (0 – 2 MH visits) | 40.0 (4) | 16.7 (1)* |
| Medium intensity of outpatient MH treatment (3 – 4 MH visits) | 20.0 (2) | 0.0 (0)* |
| High intensity of outpatient MH treatment (5 or more MH visits) | 40.0 (4) | 83.3 (5)* |
| Regularity of outpatient mental health treatment | ||
| Zero months of continuous outpatient MH treatment after discharge | 10.0 (1) | 0.0 (0)* |
| One month of continuous outpatient MH treatment after discharge | 20.0 (2) | 16.7 (1)* |
| Two months of continuous outpatient MH treatment after discharge | 10.0 (1) | 0.0 (0)* |
| Three months of continuous outpatient MH treatment after discharge | 60.0 (6) | 83.3 (5)* |
| Continuity of mental health treatment across organizational boundaries | ||
| Received any outpatient MH treatment within 1 mo of discharge | 80.0 (8) | 100.0 (6)* |
p > 0.05.
Participants with Poor Continuity of Care
Three of the five participants who had the least continuity of care after psychiatric hospitalization were readmitted within 3 mo post-discharge. All three had reported that they felt that they were at low or no future risk for suicide. In the first case, the participant attended the first outpatient visit, but did not show up for subsequent appointments including missing a scheduled injection of a psychotropic agent. By the time, the participant re-engaged with care, his suicidal symptoms were so severe that he required readmission. In the second case, the participant received no outpatient mental health treatment due to a breakdown in communication between patient and providers. The participant was readmitted due to a worsening of his mental health symptoms. In the third case, the participant canceled the initial outpatient appointment and due to breakdowns in communication between the participant and outpatient treaters, a follow-up appointment was not rescheduled until 40 d after discharge. In the interim, the participant’s mental health symptoms worsened and he was eventually readmitted due to safety concerns.
The fourth participant initially was engaged in outpatient treatment (i.e., attending outpatient appointments) in the first month after discharge, but remained disengaged in the second and third month after discharge (i.e., no-showing or canceling appointments). This participant had reported that he believed that he was at low or no future risk for suicide. While the health status of this participant was unclear based on available medical records, there was no evidence to suggest that the participant had been readmitted to a VA facility within the first 3 mo after discharge.
The fifth participant had expressed at the time of discharge a heightened awareness of his high future risk for suicide. Accordingly, he was initially engaged in outpatient treatment in the first month after discharge, but he disengaged from care in the second and third month after discharge (i.e., no-showing or canceling appointments). Again, there was no evidence in his medical record to suggest that he had been readmitted to a VA facility within the first 3 mo after discharge.
There were no cases of psychiatric readmission or other adverse outcomes among the remaining eleven interviewed participants.
DISCUSSION
Our findings suggest that individuals who are psychiatrically discharged may be unaware of their future risk for suicide. This lack of knowledge may play a role in poor engagement in follow-up care. Concerns about the stigma from being psychiatrically hospitalized and having mental illness may serve as a barrier to treatment. When individuals experience worsening symptoms of mental illness after discharge, they may also be more likely to isolate from others including providers. Conversely, family and peers may play a critical role in helping individuals to engage in follow-up care. However, if an individual perceives that family or peers do not value treatment, the individual may turn down treatment. Individuals may also disengage from treatment if they perceive that providers are not invested in their personal well-being.
Many participants did not appreciate that they were at heightened risk for suicide after discharge. This is notable given that regardless of the reason for admission, a psychiatric hospitalization is a well-known risk factor for suicide.6 To the best of our knowledge, no prior studies have assessed psychiatric inpatients’ awareness of future suicide risk after discharge. Our findings, however, are somewhat similar to those of Qurashi et al who found that psychiatric inpatients with lower insight scores at the time of discharge were more prone to be non-compliant with medications.7 These authors did not address whether insight scores measured awareness of suicide risk.7 Several studies have proposed that patients who make a suicide attempt may experience brief catharsis after the attempt.35–37 Van Praag and Plutchik36 found that patients who were hospitalized after a suicide attempt had a significant decrease in depression within a few days of hospitalization compared to patients who were depressed, but not suicidal. While brief catharsis may explain why hospitalized patients might have poor insight into their future suicide risk, other studies have found no evidence to support this hypothesis.38,39 In our study, patients who believed that their future suicide risk was low or none reported less severe suicidal ideation in the past month compared to those participants who believed that their future suicide risk was high. Perhaps, because patients felt less suicidal recently, they concluded that their suicide risk was low or none. Patients may want to be hopeful about the future and not consider the possibility that their symptoms might worsen.
Given these findings, targeted educational interventions at the time of discharge may play an important role in suicide prevention. For example, the World Health Organization’s Brief Intervention and Contact Program (WHO BIC) is a brief education and follow-up strategy which teaches patients about their suicide risk after discharge and helps them to remain engaged in post-discharge treatment. The WHO BIC has been shown to significantly lower the odds of suicide after discharge.40
Using the TBP framework, we identified several factors that may motivate patients to engage in treatment after discharge. Similar to other studies, patients were motivated to seek out care because they believed that treatment could address their general mental health symptoms. For example, in a study of National Guard Soldiers, Stecker et al13 used the TPB framework to demonstrate that patients felt an important benefit of treatment included the ability to manage symptoms. In our study, family and peers were identified as critical factors in the decision to pursue treatment. Alonzo et al also reported that family plays an important role in keeping individuals with suicidal ideation engaged in treatment.41
We uncovered several factors that may dissuade individuals from engaging in follow-up care. Patients were more inclined to refuse care if they experienced unwanted side effects or encountered stigma. Other studies have raised similar concerns that fear of stigma and adverse side effects contribute to treatment non-adherence.10,11,42,11,13 In addition, a few patients in our study suggested that symptom severity leads to treatment non-adherence. This is somewhat similar to the findings of Carlton and Deane43 who reported that patients with more severe suicidal ideation were less likely to seek help. Akin to prior studies, we found that patients were less inclined to pursue care if they perceived no benefit from treatment or experienced poor-therapeutic alliance.44 Poor-therapeutic alliance is known to be associated with higher rates of treatment dropout.12 Finally, some patients suggested that it was important that their provider involve them more directly in treatment decisions. This aligns with available evidence supporting a role for shared decision making in mental health treatment.44
A unique strength of our study includes the fact that to the best of our knowledge, this is the first study to use the TBP to identify the attitudes and beliefs of individuals about the role of post-discharge care in mitigating future suicide risk. Given that the TPB model can predict an individual’s intention to participate in health promoting behaviors,18 it would be important to confirm our findings using a more robust study design. If the variables that we identified in our study are meaningful contributors to a patient’s decision to engage in follow-up care, this knowledge could be leveraged to design more effective post-discharge, suicide prevention interventions.
Our study has several limitations. This was a small, qualitative study limited to the Veteran population. Veterans carry unique risk factors for suicide which may influence treatment engagement. Unlike the private sector, the VA system is well resourced and this may explain why patients did not cite the lack of access to treatment as a barrier.45 Our study was comprised solely of male participants. Women have distinctive risk factors for suicide and face important challenges in accessing mental healthcare in the VA setting.46–49 Hoffmire et al50 also found that compared to nonveterans, female Veterans are at markedly higher risk for suicide than male Veterans. Our sample included a limited number of participants with co-occurring substance use disorders. Substance use disorder is an important risk factor for suicide after hospitalization and patients with substance use disorder are more likely to disengage from treatment.51,52 Our study was not designed to validate the TPB domains. It is possible that if we had used an alternative model, we would have identified different factors that influence an individual’s decision to engage in treatment. We did not use a formal scale to quantify degree of risk awareness and therefore, we may have missed nuanced differences across patients. While we collected information on treatment utilization after discharge, we were not powered to evaluate for significant differences in treatment engagement over time or adjust for confounders. We were unable to explore whether an association exists between attitudes and beliefs about follow-up care and behavior choices after discharge. Because the interviews occurred close to discharge, patients may have focused on their hope for the future and overemphasized the positive aspects of follow-up care. Yet, asking participants about their attitudes about follow-up care at a time when they are faced with similar decisions may provide better insight into their attitudes about follow-up care.
In summary, individuals who are discharged from an inpatient mental health unit may be unaware of their future risk for suicide. Larger, more robust studies are needed to confirm our findings and to evaluate whether these knowledge deficits (if present) negatively impact treatment engagement. If an individual’s decision to engage in treatment after discharge is influenced by the degree of insight they have about future suicide risk, then targeted educational interventions may be beneficial. Our results lend credence to the importance of designing prevention strategies which incorporate peers, family and provider’s investment in the patient’s care and well-being. Integrating shared decision making into discharge planning for psychiatrically hospitalized patients may also be helpful. Finally, because symptom severity may preclude individuals from participating in care, closer follow-up may be warranted.
ACKNOWLEDGEMENTS
We would like to thank the participants for taking part in this study. This material is the result of work supported with resources and use of facilities at the Veterans Affairs Medical Center, White River Junction, Vermont.
FUNDING
This work was supported by the VA National Center for Patient Safety Center of Inquiry Program (PSCI-WRJ-SHINER). Dr Riblet is the recipient of a VA New England Early Career Development Award (V1CDA-17–06). Dr Shiner is the recipient of a VA Health Services Research and Development Career Development Award (CDA11–263).
Footnotes
The views expressed in this article do not necessarily represent the views of the Department of Veterans Affairs or of the U.S. government.
REFERENCES
- 1.WHO. Preventing suicide: a global imperative 2014. Available at http://www.who.int/mental_health/suicide-prevention/world_report_2014/en/ accessed January 5, 2018.
- 2.Valenstein M, Kim HM, Ganoczy D, et al. : Higher risk periods for suicide among VA patients receiving depression treatment: prioritizing suicide prevention efforts. J Affect Disord 2009; 112: 50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bickley H, Hunt IM, Windfuhr K, Shaw J, Appleby L, Kapur N: Suicide within two weeks of discharge from psychiatric inpatient care: a case-control study. Psychiatr Serv 2013; 64: 653–9. [DOI] [PubMed] [Google Scholar]
- 4.Meehan J, Kapur N, Hunt IM, et al. : Suicide in mental health in-patients and within 3 months of discharge. Br J Psychiatry 2006; 188: 129–34. [DOI] [PubMed] [Google Scholar]
- 5.Qin P, Nordentoft M: Suicide risk in relation to psychiatric hospitalization: evidence based on longitudinal registers. Arch Gen Psychiatry 2005; 62: 427–32. [DOI] [PubMed] [Google Scholar]
- 6.Chung DT, Ryan CJ, Hadzl-Pavlovic D, Singh SP, Stanton C, Large MM: Suicide rates after discharge from psychiatric facilities: a systematic review and meta-analysis. JAMA Psychiatry 2017; 74(7): 694–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Qurashi I, Kapur N, Appleby L: A prospective study of noncompliance with medication, suicidal ideation, and suicidal behavior in recently discharged psychiatric inpatients. Arch Suicide Res 2006; 10: 61–7. [DOI] [PubMed] [Google Scholar]
- 8.Granboulan V, Roudot-Thoraval F, Lemerle S, Alvin P: Predictive factors of post-discharge follow-up care among adolescent suicide attempters. Acta Psychiatr Scand 2001; 104(1): 31–6. [DOI] [PubMed] [Google Scholar]
- 9.Costemale-Lacoste JF, Balaguer E, Boniface B, et al. : Outpatient treatment engagement after suicidal attempt: A multisite prospective study. Psychiatry Res 2017; 258: 21–3. [DOI] [PubMed] [Google Scholar]
- 10.Chapman SCE, Horne R: Medication nonadherence and psychiatry. Curr Opin Psychiatry 2013; 26: 446–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.IOM Committee on Pathophysiology and Prevention of Adolescent and Adult Suicide: Reducing suicide: a national imperative. In: Chapter 9: Barriers to Effective Treatment and Intervention, pp 1–513. Edited by Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE Washington, D. C, National Academies Press, 2002. [PubMed] [Google Scholar]
- 12.Barrett MS, Chua WJ, Crits-Christoph P, Gibbons MB, Casiano D, Thompson D: Early withdrawal from mental health treatment: implications for psychotherapy practice. Psychotherapy (Chic) 2008; 45(2): 247–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stecker T, Fortney JC, Hamilton F, Ajzen I: An assessment of beliefs about mental health care among veterans who served in Iraq. Psychiatr Serv 2007; 58: 1358–61. [DOI] [PubMed] [Google Scholar]
- 14.Fisher EB, Fitzgibbon ML, Glasgow RE, et al. : Behavior matters. Am J Prev Med 2011; 40: e15–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eccles M, Grimshaw J, Walker A, Johnston M, Pitts N: Changing the behavior of healthcare professionals: the use of theory in promoting the uptake of research findings. J Clin Epidemiol 2005; 58: 107–12. [DOI] [PubMed] [Google Scholar]
- 16.Cooke R, French DP: How well do the theory of reasoned action and theory of planned behavior predict intentions and attendance at screening programmes? A meta-analysis. Psychol Health 2008; 23: 745–65. [DOI] [PubMed] [Google Scholar]
- 17.Ajzen I: The theory of planned behavior. Organ Behav Hum Decis Process 1991; 50: 179–211. [Google Scholar]
- 18.Armitage CJ, Conner M: Efficacy of the theory of planned behaviour: a meta-analytic review. Br J Soc Psychol 2001; 40: 471–99. [DOI] [PubMed] [Google Scholar]
- 19.Mak HW, Davis JM: The application of the theory of planned behavior to help-seeking intention in a Chinese Society. Soc Psychiatry Psychiatr Epidemiol 2014; 49: 1501–15. [DOI] [PubMed] [Google Scholar]
- 20.Mo PKH, Mak WWS: Help-seeking for mental health problems among Chinese: the application and extension of the theory of planned behavior. Soc Psychiatry Psychiatr Epidemiol 2009; 44: 675–84. [DOI] [PubMed] [Google Scholar]
- 21.Stecker T, Fortney J, Hamilton F, Sherbourne CD, Ajzen I: Engagement in mental health treatment among veterans returning from Iraq. Patient Prefer Adherence 2010; 4: 45–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andrykowski MA, Burris JL: Use of formal and informal mental health resources by cancer survivors: differences between rural and nonrural survivors and a preliminary test of the theory of planned behavior. Psycho-Oncology 2010; 19: 1148–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schomerus G, Matschinger HAM: Attitudes that determine willingness to seek psychiatric help for depression: a representative population survey applying the Theory of Planned Behaviour. Psychol Med 2009; 39: 1855–66. [DOI] [PubMed] [Google Scholar]
- 24.Stecker T, McGovern MP, Herr B: An intervention to increase alcohol treatment engagement: a pilot trial. J Subs Abuse Treat 2012; 43: 161–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aldrich RS, Cerel J: The development of effective message content for suicide prevention. Crisis 2009; 30: 174–9. [DOI] [PubMed] [Google Scholar]
- 26.Kulhman STW, Walch SE, Bauer KN, Glenn AD: Intention to enact and enactment of gatekeeper behaviors for suicide prevention: an application of the theory of planned behavior. Prev Sci 2007; 18: 704–15. [DOI] [PubMed] [Google Scholar]
- 27.Gipson P, King C: Health behaviors theories and research: implications for suicidal individuals’ treatment linkage and adherence. Cogn Behav Pract 2012; 19(2): 209–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Posner K, Brown GK, Stanley B, et al. : The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry 2011; 168(12): 1266–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Van Orden KA, Cukrowicz KC, Witte TK, Joiner TE: Thwarted belongingness and perceived burdensomeness: construct validity and psychometric properties of the Interpersonal Needs Questionnaire. Psychol Assess 2012; 24(1): 197–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gutierrez PM, Pease J, Matarazzo BB, Monteith LL, Hernandez T, Osman A: Evaluating the psychometric properties of the interpersonal needs questionnaire and the acquired capability for suicide scale in military veterans. Psychol Assess 2016; 28: 1684–94. [DOI] [PubMed] [Google Scholar]
- 31.Forbes D, Hawthorne G, Elliott P, et al. : A concise measure of anger in combat-related posttraumatic stress disorder. J Trauma Stress 2004; 17(3): 249–56. [DOI] [PubMed] [Google Scholar]
- 32.Hawkins KA, Hames JL, Ribeiro JD, Silva C, Joiner TE, Cougle JR: An examination of the relationship between anger and suicide risk through the lens of the interpersonal theory of suicide. J Psychiatr Res 2014; 50: 59–65. [DOI] [PubMed] [Google Scholar]
- 33.Greenberg GA, Rosenheck RA: Continuity of care and clinical outcomes in a national health system. Psychiatr Serv 2005; 56: 427–33. [DOI] [PubMed] [Google Scholar]
- 34.Miles MB, Huberman AM: Qualitative Data Analysis: An Expanded Sourcebook, Ed 2, Thousand Oaks, Sage Publications, 1994. [Google Scholar]
- 35.Matsuishi K, Kitamura N, Sato M, et al. : Change of suicidal ideation induced by suicide attempt. Psychiatry Clin Neurosci 2005; 59: 599–604. [DOI] [PubMed] [Google Scholar]
- 36.van Praag H, Plutchik R: An empirical study on the “cathartic effect” of attempted suicide. Psychiatry Res 1985; 16(2): 123–30. [DOI] [PubMed] [Google Scholar]
- 37.Sarfati Y, Bouchaud B, Hardy-Bayle MC: Cathartic effect of suicide attempts not limited to depression: a short-term prospective study after deliberate self-poisoning. Crisis 2003; 24: 73–8. [DOI] [PubMed] [Google Scholar]
- 38.Walker RL, Joiner TEJ, Rudd MD: The course of post-crisis suicidal symptoms: how and for whom is suicide ‘cathartic’? Suicide Life Threat Behav 2001; 31: 144–52. [DOI] [PubMed] [Google Scholar]
- 39.Bronisch T: Does an attempted suicide actually have a cathartic effect? Acta Psychiatr Scand 1992; 86: 228–32. [DOI] [PubMed] [Google Scholar]
- 40.Riblet N, Shiner B, Young-Xu Y, Watts BV: Strategies to prevent death by suicide: a meta-analysis of randomized controlled trials. Br J Psychiatry 2017; 210(6): 396–402. [DOI] [PubMed] [Google Scholar]
- 41.Alonzo D, Moravec C, Kaufman B: Individuals at risk for suicide: mental health clinicians’ perspectives on barriers to and facilitators of treatment engagement. Crisis 2017; 38: 158–67. [DOI] [PubMed] [Google Scholar]
- 42.Pompili M, Serafini G, Del Casale A, et al. : Improving adherence in mood disorders: the struggle against relapse, recurrence and suicide risk. Expert Rev Neurother 2009; 9(7): 985–1004. [DOI] [PubMed] [Google Scholar]
- 43.Carlton PA, Deane FP: Impact of attitudes and suicidal ideation on adolescents’ intentions to seek professional psychological help. J Adolesc 2000; 23(1): 35–45. [DOI] [PubMed] [Google Scholar]
- 44.Dixon LB, Holoshitz Y, Nossel I: Treatment engagement of individuals experiencing mental illness: review and update. World Psychiatry 2016; 15: 13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wagner TH, Sinnott P, Siroka AM: Mental health and substance use disorder spending in the Department of Veterans Affairs, fiscal years, 2000–2007. Psychiatr Serv 2011; 62: 389–95. [DOI] [PubMed] [Google Scholar]
- 46.Tsai J, Mota NP, Pietrzak RH: U.S. female Veterans who do and do not rely on VA health care: needs and barriers to mental health treatment. Psychiatr Serv 2015; 66(11): 1200–6. [DOI] [PubMed] [Google Scholar]
- 47.Kimerling R, Pavao J, Greene L, et al. : Access to mental health care among women Veterans: is VA meeting women’s needs? Med Care 2015; 53(4 Suppl 1): S97–s104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Washington DL, Farmer MM, Mor SS, Canning M, Yano EM: Assessment of the healthcare needs and barriers to VA use experienced by women veterans: findings from the national survey of women Veterans. Med Care 2015; 53(4 Suppl 1): S23–31. [DOI] [PubMed] [Google Scholar]
- 49.Gradus JL, King MW, Galatzer-Levy I, Street AE: Gender differences in machine learning models of trauma and suicidal ideation in veterans of the Iraq and Afghanistan Wars. J Trauma Stress 2017; 30(4): 362–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hoffmire CA, Kemp JE, Bossarte RM: Changes in suicide mortality for Veterans and nonveterans by gender and history of VHA service use, 2000–2010. Psychiatr Serv 2015; 66(9): 959–65. [DOI] [PubMed] [Google Scholar]
- 51.Olfson M, Mojtabai R, Sampson NA, et al. : Dropout from outpatient mental health care in the United States. Psychiatr Serv 2009; 60(7): 898–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Olfson M, Wall M, Wang S, et al. : Short-term suicide risk after psychiatric hospital discharge. JAMA Psychiatry 2016; 73(11): 1119–26. [DOI] [PMC free article] [PubMed] [Google Scholar]


