Abstract
Physician‒scientists have made countless discoveries, and their dwindling numbers are a significant concern. Although dermatology has become an increasingly popular destination for physician‒scientist trainees, the proportion of trainees who pursue scientific research careers after training is among the lowest of all medical specialties. To investigate this problem, we surveyed a national cohort of dermatology educators, physician‒scientist track program directors, and National Institute of Arthritis and Musculoskeletal and Skin Diseases T32 directors for opinions regarding physician‒scientist training in dermatology. On the basis of these findings and to help address the issue, we propose a training practicum and provide a resource for funding opportunities to help guide trainees and institutions interested in supporting investigative dermatologists. We also discuss the important roles of department chairs and institutions in fashioning an environment conducive to physician‒scientist training. The information and recommendations provided in this paper may help to improve the recruitment, training, development, and retention of investigative dermatologists and future leaders in this field.
Abbreviations: ABD, American Board of Dermatology; ASCI, American Society of Clinical Investigators; CDA, Career Development Award; CV, curriculum vitae; LRP, loan repayment program; MD, medical degree; MSTP, Medical Scientist Training Program; NIGMS, National Institute of General Medical Sciences; NIH, National Institutes of Health; NIAMS, National Institute of Arthritis and Musculoskeletal and Skin Diseases; PGY, postgraduate year; PSTP, physician‒scientist training program; PSW, physician‒scientist workforce; STAR, Specialty Training and Advanced Research; URM, under-represented minority
ROLES OF PHYSICIAN‒SCIENTISTS IN MEDICINE AND DERMATOLOGY
Physician‒scientists (also called clinician‒investigators) are medical doctors who harness the knowledge of physiology and disease to address questions in biology and medicine through scientific research. Physician‒scientists encompass individuals with a medical degree (MD) who may or may not also have a doctoral degree (i.e., PhD). Throughout history, physician‒scientists have been instrumental in advancing biomedical knowledge. James Shannon, the father of the modern National Institutes of Health (NIH), believed that the key driving force behind the physician‒scientist is the concept that diseases will only be cured when science provides a fundamental understanding of physiology (Goldstein and Brown, 1997). The classical role of the physician‒scientist is to make discoveries regarding human disease and to translate those discoveries to the patient bedside.
In the last century, a plethora of key discoveries were made by physician‒scientists, including up to half of Nobel Laureates in Physiology and Medicine (The Nobel Foundation, 2020) who conducted ground-breaking research encompassing basic science, disease-oriented, and patient-oriented research. Examples of their fundamental discoveries include the discovery of DNA polymerase by Arthur Kornberg, ABO blood typing by Karl Landsteiner, and inborn errors of metabolism by Archibald Garrod. From 1964 to 1972, a cohort of nine physicians trained at the NIH, all of whom were awarded Nobel Prizes for seminal discoveries, including the low-density lipoprotein receptor by Michael Brown and Joseph Goldstein, cellular oncogenes by J. Michael Bishop and Harold Varmus, G proteins and G protein‒coupled receptors by Alfred Gilman and Robert Lefkowitz (respectively), prions by Stanley Prusiner, nitric oxide signaling by Ferid Murad, and odorant receptors by Richard Axel. These examples are merely a fraction of the transformative discoveries made by physician‒scientists in recent history. In addition to important basic science discoveries, physician‒scientists have played and continue to play a vital role in clinical research and in running clinical trials.
Physician‒scientists have also played significant roles in dermatology. Nobel prize‒winning discoveries related to biochemistry, cell biology, developmental biology, and immunology have all played vital roles in our understanding of epithelial physiology and pathology. The use of phototherapy for modern-day dermatologic diseases can be traced back to Niels Ryberg Finsen, who won the Nobel Prize in 1903 for the use of electromagnetic radiation in patients with lupus vulgaris. The revolutionary treatment of melanoma using checkpoint inhibitors would not be possible without the Nobel Prize‒winning discovery of PD-1 by Tasuku Honjo. Physician‒scientists have also made important strides in understanding the molecular pathogenesis of epidermolysis bullosa, pemphigus, psoriasis, and atopic dermatitis (Rubenstein et al., 2002). Many physician‒scientists continue to work to further our understanding of dermatologic diseases and their treatments.
Despite their importance in advancing medical research, physician‒scientists represent an endangered species (Jain et al., 2019). A 2014 NIH Physician-Scientist Workforce (PSW) working group report identified a distressing trend in the PSW (Physician Scientist Workforce Working Group, 2014). Since a peak in the PSW in the late 1980s and early 1990s, PSW numbers have stagnated, with a 30% proportional decrease in R01s obtained by the PSW relative to those obtained by nonphysicians (Physician Scientist Workforce Working Group, 2014). This time period also saw a significant decline in attendance at meetings of the American Society of Clinical Investigators (ASCI) and the Association of American Physicians, two organizations dedicated to the advancement of medical knowledge through research (Erzurum, 2018; Goldstein and Brown, 1997). As the current PSW ages, inadequate numbers of new physician‒scientists enter this career path (Milewicz et al., 2015). These challenges were the impetus for the recently established Physician-Scientist Support Foundation (www.thepssf.org). To understand this decline, we must understand the modern-day training pipeline of the physician‒scientist.
THE PHYSICIAN‒SCIENTIST CAREER PATH: A LEAKY PIPELINE
In 1964, James Shannon carried out his vision of a PSW by supporting the creation of the Medical Scientist Training Program (MSTP) through the National Institute of General Medical Sciences (NIGMS). This program funded the training of a new workforce of physician‒scientists who graduate medical school with both MD and PhD degrees, a testament to their training in both clinical medicine and scientific research. There are currently 51 MSTPs in the United States that receive NIH funding through institutional T32 grants from NIGMS (National Institute of General Medical Sciences, 2021). Many schools without an MSTP also provide the opportunity for students to obtain both degrees. At any given time, there are over 5,000 students working to obtain their MD and PhD; each year, approximately 600 new MD‒PhD students matriculate, and 550 graduate (Harding et al., 2017). The typical structure of MD‒PhD programs places doctoral training between preclerkship and clerkship curricula, and students spend an average of 4 years completing their thesis research.
Upon completing medical school, MD‒PhD and MD students have the opportunity to pursue research-intensive residency programs. These research-in-residency or physician‒scientist training programs (PSTPs) have a wide variety of structures and timelines but typically involve the integration of dedicated research time into the clinical curriculum. Often, the clinical component of residency may be modified to enable more time for research. Specialties that have board-approved research tracks include anesthesiology, dermatology, internal medicine, pathology, pediatrics, and radiology. The American Board of Dermatology (ABD) typically approves the Investigative Training Track in Dermatology, often called the 2 + 2 track, allowing trainees to focus on the clinical dermatology curriculum in the first 2 years with reduced direct patient care duty in years 3 and 4 to enable additional time for dedicated research. Residents then take the board certification examination with their peers in the postgraduate year (PGY) 4, before continuing with their research and path toward independence. In other specialties such as internal medicine, the research track is tied to fellowship training and specialization. On completing postgraduate training, the physician‒scientist typically pursues a career that is a mixture of clinical practice and research.
Although many students enter the physician‒scientist career track, many do not complete the program. This so-called leaky pipeline has been of increasing concern in recent years and brings into question the value and cost effectiveness of MD‒PhD programs (Rosenberg, 2008; Whitcomb, 2007). A survey of alumni from 24 MD‒PhD programs found that only 64% of MD‒PhD graduates devote over 50% of their time to research (Brass et al., 2010). A larger analysis of MD‒PhD graduates between 1991 and 2010 found that 78% reported any amount of research engagement; this fraction differs significantly among different specialties, with only 54.1% of MD‒PhD dermatologists engaged in any amount of research (lowest among specialties) (Andriole et al., 2021). MD‒PhD neurologists had the highest level of research engagement, with 87.9% of graduates incorporating research into their careers. Among those who reported research in their careers, training in specialties such as radiation oncology, radiology, and surgery was associated with decreased time spent on research. Another survey that closed in 2015 asked what percentage of respondents engaged in ≥50% research effort; dermatology ranked 8th of 18 specialties, with 28% (Brass and Akabas, 2019). Neurology ranked the highest with 54%.
Attempts at understanding the causes of the leaky pipeline have recently been undertaken. Brown and Goldstein found that recent reductions in basic science education from the medical curriculum have resulted in a loss of conviction that progress in medicine rests on the fundamental understanding of physiology (Goldstein and Brown, 2012). They also identified the specialization of science and the financial demands of clinical medicine as two sides tugging at the physician‒scientist, forcing them to choose one or the other (Goldstein and Brown, 1997). This notion was echoed in an analysis by Harding et al. (2017) that suggested that increased training times in both science and medicine break the momentum of the physician‒scientist career path. The average physician‒scientist will not obtain their first R01 until age 44 years when their physician peers have been in the workforce for over a decade; this is 10 years greater than the average age at first R01 and first-time faculty appointment in 1980 (Milewicz et al., 2015). In a survey of MD and MD‒PhD students who expressed interest in research careers, raising children was the most frequently reported concern when it came to pursuing a career as a physician‒scientist (Kwan et al., 2017). Other challenges include lower salaries in academia than in private practice, increased pressure on clinical productivity, and decreased grant application success rates (Harding et al., 2017).
Given these challenges in the physician‒scientist’s career path and the worrying trend in PSW demographics, significant efforts must be undertaken to streamline the training process and support trainees. Several action items have been proposed, including shortening the time to an independent research position, increasing the number of physician‒scientists, and centralizing the oversight of physician‒scientist trainees at all levels (Milewicz et al., 2015). Despite these challenges, physician‒scientists continue to make important discoveries and serve as a key bridge between the clinical and scientific realms.
RECRUITING THE RIGHT CANDIDATES FOR A PHYSICIAN‒SCIENTIST CAREER PATH IN DERMATOLOGY
Recruiting the candidates for the physician‒scientist career path requires careful consideration of both the causes of the leaky pipeline and the applicant’s capacity for future success. A key issue in the leaky pipeline is the stagnant pool of qualified candidates. Whereas the number of clinicians and scientists has increased over the past 20 years plus, the number of physician‒scientists has not increased proportionally, and women and under-represented minorities (URMs) continue to be relatively lacking among physician‒scientists (Brown, 2020; Milewicz et al., 2015). Among MD‒PhD graduates, women comprise approximately a third (Association of American Medical Colleges, 2018). For URM MD‒PhD graduates, African American and Hispanic trainees comprise less than half of their proportional population representation (Association of American Medical Colleges, 2018). Historically, dermatology was a relatively more popular specialty choice for female MD‒PhD graduates since 1985, despite the low total number (Association of American Medical Colleges, 2018). Among current dermatology trainees, this balance has shifted, with female MD‒PhD graduates comprising the majority of dermatology MD‒PhD trainees (41 of 77) compared with male graduates (36 of 77), a 1.9-fold difference (Association of American Medical Colleges, 2018; Akabas and Brass, 2019). However, a lower proportion of women continue into academia, suggesting the continued presence of barriers that may preferentially affect women trainees. Our survey, which includes responses from 23 dermatology faculty members (dermatology educators, physician‒scientist track program directors, and National Institute of Arthritis and Musculoskeletal and Skin Diseases [NIAMS] T32 directors) across 17 different institutions nationwide, identified an ongoing shortfall of URMs among dermatology physician‒scientist trainees, with the majority of responders reporting that ≤10% of their trainees are URMs (Table 1). Similarly, Akabas and Brass (2019) reported that just 3.7% of URMs chose dermatology as their graduate medical education specialty.
Table 1.
Survey Questions and Responses
| Survey Responses | |||
|---|---|---|---|
| Question Number | Question | Yes | No |
| 1 | Does your program have a 2 + 2 training track? | 18 | 4 |
| Not important | Somewhat important | Important | Very important | Essential | ||
|---|---|---|---|---|---|---|
| 2 | How important are physician-scientists (MD or MD/PhD) for the future of Dermatology? | 0 | 0 | 0 | 3 | 20 |
| 3 | How important is it for your physician-scientist trainees to train with a Department of Dermatology faculty? | 9 | 8 | 2 | 2 | 2 |
| Not difficult | Somewhat difficult | Difficult | Very difficult | Extremely difficult | ||
|---|---|---|---|---|---|---|
| 4 | How difficult is it for your program to recruit the right physician–scientist (2 + 2) candidate? | 0 | 7 | 6 | 6 | 4 |
| Zero | One | Two | Three | Four | Five | ||
|---|---|---|---|---|---|---|---|
| 5 | What is the IDEAL NUMBER of physician-scientist trainees you can hire annually? | 0 | 13 | 8 | 2 | 0 | 0 |
| 6 | In the past 5 years, what was the AVERAGE NUMBER of physician-scientist trainees hired annually? | 6 | 15 | 2 | 0 | 0 | 0 |
| 7 | What is the AVERAGE NUMBER OF RESEARCH YEARS (separate from clinical dermatology) spent by your graduates to complete post-graduate training? | 0 | 2 | 8 | 7 | 3 | 0 |
| 0% | 10% | 20% | 30% | 40% | 50% | 60% | 70% | 80% | 90% | 100% | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 8 | In the past 5 years, what PERCENTAGE of your physician-scientist program graduates pursued independently funded investigation? | 2 | 0 | 3 | 2 | 0 | 5 | 3 | 1 | 2 | 2 | 1 |
| 9 | In the past 5 years, what PERCENTAGE of your physician-scientist trainees are underrepresented minorities (as defined by the NIH)? | 7 | 7 | 3 | 1 | 2 | 1 | 0 | 1 | 0 | 0 | 0 |
Abbreviations: MD, medical degree; NIAMS, National Institute of Arthritis and Musculoskeletal and Skin Diseases; NIH, National Institutes of Health.
We surveyed a national cohort of 48 dermatology educators, physician‒scientist track program directors, or NIAMS T32 directors across 33 different institutions regarding their thoughts about dermatology physician‒scientist training. We received responses from 23 dermatology faculty members across 17 different institutions. Aggregated survey questions and responses are depicted in the Table.
In addition to increasing recruitment of URM and women physician‒scientists, it will also be important to increase the involvement of URMs and women in hiring and promotion committees. This will help to identify overt and structural biases more readily within the recruitment and hiring process. Implicit bias training is also available at most institutions, and there should be mandatory training for those serving on resident recruiting/faculty hiring and promotion committees. Finally, implementing policies to better support URM and women physician‒scientists is also key. For example, women scientists in general tend to receive smaller start-up packages than men scientists (Oliveira et al., 2019). Start-up packages should not be influenced by sex or race but rather on the basis of the qualifications of the candidate. In addition, because this time in trainees’ careers typically includes family responsibilities, extending the tenure clock in these cases would also be beneficial. Other helpful suggestions for policy changes that would greatly benefit women in academic science are outlined in this commentary by Reese et al. (2021).
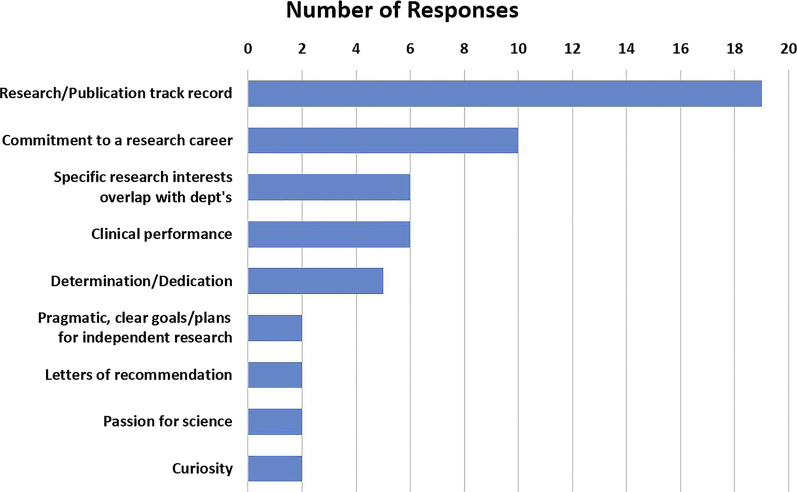
To determine the qualities of the ideal investigative dermatology trainee, we asked survey responders for their top three criteria for recruiting applicants to their PSTP (Figure 1). Most respondents reported that a strong publication record was an important criterion. Approximately half reported that commitment to a research career was a top criterion. Additional criteria included research interests that overlap with the departments’ goals and strong clinical performance. Although our survey did not directly assess this, it would be interesting to look at the correlation between these top criteria and the rate of retention and success of trainees chosen.
Figure 1.
Top criteria for recruiting applicants to a dermatology physician‒scientist training track. Aggregated open-ended survey responses from dermatology educators, physician‒scientist track program directors, and NIAMS T32 directors regarding their top three criteria for recruiting applicants to their physician‒scientist track. Only criteria with at least two responses were included. NIAMS, National Institute of Arthritis and Musculoskeletal and Skin Diseases.
Strong candidates for a career in investigative dermatology will be in high demand among other specialties as well. Our survey showed a discrepancy between the ideal number of investigative dermatology trainees that can be hired and the average number that were actually hired (Table 1): the total number of trainees that could be hired was 35, whereas the number actually hired was 19, a shortfall of 46%. It is essential that dermatology departments implement early contact with medical students to identify students who have the capacity for careers as physician‒scientists. By generating early interest, the field of dermatology will increase the likelihood of recruiting future leaders.
To spur interest in dermatology and build a pipeline among these candidates, we recommend increasing contact between faculty and students. Potential strategies may include early contact between faculty and students by teaching in medical school lectures, volunteering to interact with students, and faculty research seminars. Many schools have specialty interest groups that can help connect faculty members with interested students and showcase faculty research projects. These interactions will help to generate interest in dermatology among students and enable faculty to identify students with a passion for research. These students should be mentored throughout medical school to build their research skills and help guide them toward a career in investigative dermatology. This is also important for increasing diversity and representation in the physician‒scientist training path. Many URMs may not have had the same opportunity for or exposure to research before medical school. Early mentorship provides an opportunity to identify and train talented URMs for a career in investigative dermatology. By implementing early contact, dermatology programs can increase the numbers of physician‒scientists dedicated to a career in investigative dermatology.
The applicant’s capacity for future success is an important factor in recruiting promising candidates for a career in investigative dermatology. Applicants for this career path must have the potential to excel as both a clinician and a scientist. Clinical aptitude can be evaluated on the basis of the applicants’ medical school grades and clerkship performances. Their capacity for research can be evaluated on the basis of the productivity and quality of previous research. Additional desired qualities of the ideal applicant are professionalism, integrity, ethics, maturity, and a team spirit.
The physician‒scientist career path is suited to applicants who display significant leadership qualities and a commitment to a career in investigative dermatology. The most successful investigative dermatologists are those who will become leaders in dermatology and advance the field through impactful discoveries. They will also play significant roles in their institutions and in national organizations. Many of these candidates will also have a history of service to the communities around them. The best way to evaluate these qualities will be through scholarly work, letters of recommendation, mentors, and their interviews. These sources should be used to gauge whether an applicant has a true passion for research and the capacity to push the boundaries of our knowledge.
ROLES OF INSTITUTIONAL RESEARCH ENVIRONMENT AND MENTORSHIP IN TRAINING PHYSICIAN‒SCIENTISTS
The institutional research environment plays a significant role in training newly recruited physician‒scientists. For programs to succeed, they must provide a conducive research environment while also championing their candidates. Several factors have been proposed that may support an effective local research environment (Wang et al., 2016). In terms of personnel, programs should ensure a critical mass of both investigators and trainees: This allows for supervisor-to-peer mentorship and peer-to-peer mentorship, both of which are vital to the success of a physician‒scientist. In addition, having a dedicated team/oversight committee to advise and monitor each candidate would be helpful. Ideally, this team would include the candidate’s postdoctoral advisor, the dermatology program director, a physician‒scientist in the dermatology department, a clinician in the dermatology department, and a basic scientist from a different department. This team might meet once every 6 months or so and then more frequently later on to monitor the research progress of the candidate and guide their development into a physician‒scientist of distinction.
If possible, while the 2 + 2 fellow is still in the laboratory, it would be ideal to pair them with an MD‒PhD student in that laboratory (if there is one) so that they can collaborate on a research project. This would result in the student’s project moving forward faster and likely result in more publications. The fellow could also act as a mentor of sorts to the MD‒PhD student, introducing them to dermatology and thus enhancing the pipeline.
Another idea would be to adopt an apprentice-type approach from the very beginning of the training period. This could even potentially start as early as undergraduate or high school. This approach would be similar to the apprenticeships found in trades, where an experienced professional takes a trainee under their wing and teaches them in more of a one-on-one approach. The trainer would take a personal interest in the candidate’s training and in their scientific and career development. This person would be more involved than a typical mentor. Unfortunately, not everyone is suitable for this type of role; it requires someone who is very dedicated and deeply passionate about training the next generation of physician‒scientists. However, with the right person, this type of apprenticeship would greatly benefit the trainee as well as the program.
In addition, programs should emphasize collaboration with both basic and patient-centric scientists to promote a culture of synergy. This enables investigators and trainees across various disciplines to identify common goals, which may accelerate training and progress. Collaborations can also be encouraged with financial support: for example, University of Texas Southwestern (Dallas, TX) has implemented a Pilot Synergy Grants Program that seeks to stimulate collaborations between clinicians and basic scientists. Programs can also work toward this synergy through the restructuring of research space to avoid isolation and promote peer-to-peer contact. Finally, programs should invest in innovative research technologies that decrease benchwork time and increase productivity.
Several institutions have implemented institution-wide research training programs for physician‒scientists that incorporate both environment and mentorship. One such program, the University of California, Los Angeles Specialty Training and Advanced Research (STAR), has successfully trained physician‒scientists since its inception in 1993. An analysis of 123 University of California, Los Angeles STAR graduates from 1993‒2003 found that 80% continued toward a research career in academia or industry (Wong et al., 2016). The program accommodates trainees from a wide range of backgrounds and specialties. Trainees who are graduates of an MD‒PhD program are able to complete 2‒3 years of postdoctoral research under this program. The STAR program also enables MD-only candidates to work toward a PhD during postgraduate training. By centralizing the research-track programs, the STAR program enables significant networking within the institution and across multiple specialties. This method also enables the critical mass of trainees optimal for peer-to-peer mentorship.
Washington University in St. Louis also addresses several issues of the leaky pipeline with their Oliver Langenberg Physician Scientist Training Program (PSTP). Similar to the STAR program, the Oliver Langenberg PSTP accommodates trainees from multiple disciplines, providing expanded peer-to-peer networking. The program also allows networking opportunities with basic science departments as well as social events and seminar series for trainees in all departments. To help supplant financial concerns, the PSTP provides educational stipends during the clinical training years and a salary bonus during the research years. The program also employs structured mentorship that starts at the beginning of residency training.
The success of physician‒scientist training hinges on the marriage between excellent training and an outstanding investigational environment. In training physician‒scientists, programs must identify ways to enhance both. For programs that do not have the necessary research infrastructure to optimize physician‒scientist training, collaborations across clinical departments or with basic science departments allow for a temporary solution while the program builds within their own department. In accordance, our survey results identified that the majority of respondents felt that scientific training within the dermatology department was not important or was only somewhat important (Table 1).
CLINICAL AND INVESTIGATIVE TRAINING IN DERMATOLOGY FOR PHYSICIAN‒SCIENTISTS
The popularity of dermatology among MD‒PhD graduates has increased from just over 1% before 1975 to nearly 6% for the cohort between 2005‒2014 (Association of American Medical Colleges, 2018). However, only 48% of MD‒PhD graduates in dermatology go on to work full time in academia (Brass and Akabas, 2019). A total of 44% enter private practice, ranking dermatology as the third-highest field to funnel MD‒PhDs to private practice after family medicine and emergency medicine. Furthermore, only 28% of dermatology MD‒PhDs dedicate >50% of their time to research (Brass and Akabas, 2019; Brass et al., 2010). The poor retention of physician‒scientists within dermatology necessitates the standardization and streamlining of the research-track curriculum to maximize productivity while minimizing the total training time.
The current ABD-approved Investigative Training Track attempts to address this by condensing clinical dermatology training to 2 years, with the stipulation of 225% direct patient care time (100% in PGY2 and PGY3 and 25% in PGY4) by the time of board certification. Like many other institutions, the University of Texas Southwestern has modified its 2 + 2 physician‒scientist residency track to allow a built-in 2 + 1 mechanism in which clinical training is front loaded into the PGY2 and PGY3, with the PGY4 year comprised of 25% clinical obligations and 75% research. On completion of the PGY4, investigative residents will sit for the boards alongside their classmates before returning to the laboratory for their PGY5. Given the clinical requirements and timelines, it is important to understand that investigative residents are first and foremost dermatologists. For physician‒scientists, research questions should be guided by a deep understanding of human diseases, which requires a strong clinical background.
It is not enough to maximize only the total time residents receive for research. Given concerns about the training time to become a physician‒scientist, it is also vital to maximize research productivity and time efficiency. Unlike the clinical component, the research component of the Investigative Training Track has significant variability across institutions. Some of this variability is intrinsic to the research infrastructure and institutional funding and cannot be optimized without large-scale changes. However, variables that can be improved include mentorship and guidance on the training timeline, individual funding opportunities, and career development. In the remainder of this section, we will focus on optimizing the training timeline for residents intending to participate in the investigative track.
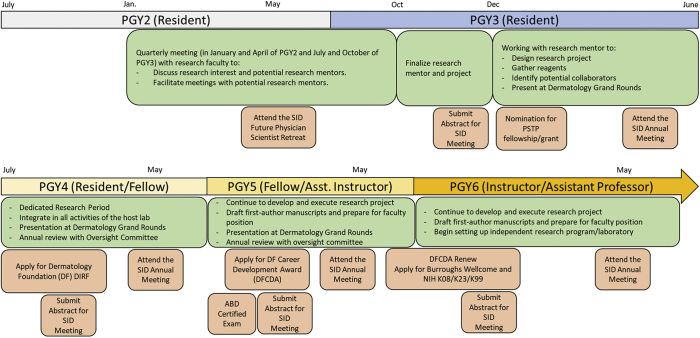
We propose a generalized research program on the basis of one utilized by our department (Figure 2 and Table 2). This program outlines the timeline of activities that should be completed to maximize efficiency during training. Typically, trainees will begin quarterly meetings with research faculty in January of their PGY2 to identify potential mentors and research projects. During the first half of the PGY3, trainees will begin finalizing mentors and projects. After approval for the ABD Investigative Training Track, PGY3 residents will begin regular meetings with their selected mentor and laboratory to design their project, gather necessary reagents, and identify potential collaborators. By the start of PGY4, trainees should be spending the majority of their professional effort in the laboratory. Our proposed practicum also includes additional details regarding transition to independence, nominations for Society for Investigative Dermatology meetings, timeframe for fellowship and grant applications, presentations at grand rounds, and annual reviews with an oversight committee. We believe that our structured practicum has contributed significantly to our ability to efficiently train physician‒scientists and maximize their productivity to speed the transition to independence.
Figure 2.
Timeline for investigative dermatology training during residency. The timeline for training begins in PGY2 and is color coded by the training period. The research practicum, including the timeframe for identifying mentors and research projects, and preparation for transition to faculty are shown in green. The orange boxes indicate the application timeframe for SID functions, funding, and board certification. ABD, American Board of Dermatology; Asst., assistant; CDA, Career Development Award; Dec, December; DF, Dermatology Foundation; DIRF, Dermatologist Investigator Research Fellowship; Exam, examination; Jan., January; NIH, National Institutes of Health; Oct, October; PGY, postgraduate year; PSTP, physician‒scientist training program; SID, Society for Investigative Dermatology.
Table 2.
Investigative Dermatology Research Practicum
| Timeline | Activity |
|---|---|
| PGY2‒PGY3 (resident) | Quarterly meeting (in January and April of PGY2 and July and October of PGY3) with the director of 2 + 2 and research faculty to discuss research interests and potential research mentors, facilitate meetings with potential research mentors, and nominate from the dermatology department to attend the SID retreat for future academicians. |
| PGY3 (resident) | 1. October–December of PGY3: finalize the selection of research mentor(s). 2. Tentative research topics/projects with research mentor(s) 3. December of PGY3: Nomination from the dermatology department for the PSTP (will need a research abstract and letter of commitment/recommendation from research mentor(s) as well as from dermatology department) |
| PGY3 (resident) | From January to July of PGY3: Regular meeting with the selected research mentor and members/trainees of his or her laboratory to facilitate: 1. Choosing and designing a mentored research project 2. Beginning to gather reagents (e.g., requesting mouse strains/plasmids from outside laboratories) and potential collaborators 3. Presentation at dermatology grand rounds (30 minutes) |
| PGY4 (resident/fellow) | 1. July of PGY4: to start full time in the selected laboratory (after 2 weeks of inpatient consult in July) to develop and execute the research projects/program. The fellow/resident needs to be fully integrated into all activities of the host laboratory/department 2. October of PGY4: to submit a dermatology DIRF application 3. Developing and submitting a first-author review manuscript with a research mentor on the basis of a literature review related to the fellow/resident’s project. This is with approval from the research mentor 4. Present at the dermatology floor work-in-progress meeting and dermatology grand rounds 5. Annual review with Oversight Committee (2 + 2 director, program director, and department chair) and research mentor to review milestones. It may be a good idea for the fellow/resident to select additional mentor(s) outside of the department to help monitor their progress |
| PGY5 (fellow/Asst instructor) | 1. Continue to execute and nucleate the research projects/program 2. Submit an abstract and attend the annual SID meeting 3. Renew the dermatology DIRF application or submit a Dermatology Foundation CDA 4. Present at the dermatology floor work-in-progress meeting and dermatology grand rounds 5. Overcoming obstacles related to projects and organizing and analyzing data 6. Developing first-author manuscripts on the basis of findings/data of the mentored project 7. Annual review with Oversight Committee and research mentor to review milestones |
| PGY6 (Asst instructor/instructor/Asst professor) | 1. Continue to execute and nucleate the research projects/program 2. Submit first-author manuscripts on the basis of findings/data of the mentored project 3. Submit an abstract and attend the annual SID meeting 4. Renew the Dermatology Foundation CDA or submit a new one 5. Submit an application for the Burroughs Wellcome Fund career award for medical scientists/K08/K23/K99 6. Present at the dermatology floor work-in-progress meeting and dermatology grand rounds 7. Annual review with Oversight Committee and research mentor to review milestones 8. Begin to set up an independent research program/laboratory |
Abbreviations: Asst, assistant; CDA, Career Development Award; DIRF, Dermatologist Investigator Research Fellowship; PGY, postgraduate year; PSTP, physician‒scientist training program; SID, Society for Investigative Dermatology.
This table shows the proposed research practicum for investigative dermatology training. The practicum outlines the recommended deadlines and goals for trainees during each training period.
One possible mechanism for further streamlining the process would be to offer promising candidates a combined internship year and dermatology residency at the same institution. This would allow the candidate more time to identify the right mentor and to formulate a research plan early, thereby giving them a head start.
Finally, with the ever-increasing efforts involving clinical research and population-based studies, programs leading to degrees such as a master of science in clinical research, epidemiology, or outcomes-based research could also be options for trainees in addition to wet-bench basic research training.
THE DEPARTMENT CHAIR’s role in developing physician‒SCIENTISTS AND TRANSITIONING TO AN INDEPENDENT CAREER
A key factor in successfully implementing the proposed timeline is the support of the department chair, who can promote the training of physician‒scientists through mentorship, monetary investment, and creation of a supportive departmental culture. Training an investigative dermatologist carries a high cost. By its nature, scientific research and discovery provide long-term and not short-term gains. Sometimes these long-term gains can be financial in the form of patentable drugs or technologies, but often, these gains are in the form of knowledge and prestige. Furthermore, a clinical dermatologist generates more revenue for the department. At its surface, the training of a physician‒scientist is not a revenue-positive endeavor. However, we argue that training investigative dermatologists is a value proposition that significantly enhances the growth of the entire field. Therefore, a successful PSTP requires the support of a department chair who will invest in fostering the development of physician‒scientists.
A key component of the leaky pipeline is the lack of a supportive environment conducive to the training and growth of the investigative dermatologist. In this situation, the departmental chair also has the ability to shape the culture of the department regarding scientific discovery and promote a climate that encourages creativity, diversity, and innovation. The department chair can encourage interaction between the scientific and clinical segments of the department and integrate the department into the heart of the institution. These interactions enable the generation of new perspectives and ideas. Collaborations also enable the translation of basic science discoveries into meaningful improvements in patient management.
The chair also plays a critical role in the physician‒scientist’s transition toward independence, serving as the gatekeeper for faculty appointments and providing access to selected award mechanisms, thereby acting as a catalyst for the trainee’s career. Physician‒scientists must optimize productivity during their research and transition years, and chairs can provide an optimal environment for the transition by securing at least 85% protected time for research by providing development monies to trainees and new faculty to financially support these commitments of professional effort. Maximizing research time enables trainees to build the body of work required to secure independent funding. The chair should consult with the trainee’s research mentor throughout the training and transitional periods. They should also advocate for the trainees by recommending faculty appointments, promotions, and merit advances. Following our proposed timeline, trainees should be promoted to junior faculty after 1‒2 years in the laboratory to help offset the opportunity cost of choosing further training over entering private practice.
Many physician‒scientists face challenges during the hiring phase. Within dermatology, faculty candidates often have less laboratory time than traditional PhD applicants, with most survey respondents reporting that their trainees undergo between 2‒3 years of postdoctorate research training (Table 1). This shorter time may not have given excellent candidates the opportunity to publish papers in high-impact journals. There has been a recent shift in dialogue regarding the importance of these objective metrics in hiring faculty members. Several articles have posited that a significant number of talented scientists are lost during the hiring phase owing to the lack of publications in high-impact journals such as Cell, Nature, and Science (Bernstein, 2014; Schmid, 2013). Similarly, many talented scientists are screened out on the basis of their curriculum vitae (CV), which is unlikely to reflect the passion, perseverance, and creativity of an individual given their particular circumstances (Schmid, 2013). Of hundreds of applicants, only a handful of the same applicants may be chosen for interviews by multiple institutions (Bernstein, 2014). This also creates an issue for departments by decreasing the chances that an applicant will choose their institution over another. Sandra Schmidt, former chair of Cell Biology at the University of Texas Southwestern, proposed four elements to better identify applicants with the potential for success in science. She proposed asking applicants about (i) their most significant scientific accomplishments as a graduate student and (ii) as a postdoctoral fellow, (iii) their overall goals and vision for a research program at the institution, and (iv) their experiences and qualifications that make them particularly well-suited to achieve these goals (Schmid, 2013). Departmental chairs should consider these factors as well as how far applicants have traveled in their careers when interviewing budding investigative dermatologists for faculty positions. Although investigative dermatology trainees may not have the same body of scholarly work as those of other candidates owing to the shortened training period, they bring a broad knowledge base that will make them invaluable members of the department. In addition, these elements will enable department chairs to look beyond the CV to identify promising candidates who will help to shape the future of dermatology.
FUNDING OPPORTUNITIES DURING THE TRAINING PERIOD AND BEYOND
The ability to acquire research funding is a critical component in the training and career of a physician‒scientist. Without funding, physician‒scientists may be pressured to increase clinical time while reducing research time. This decrease in research productivity impairs the ability to obtain future funding, starting a vicious cycle. Fortunately, many funding opportunities are available for physician‒scientists (Permar et al., 2020), including investigative dermatologists (Table 3). Several dermatology programs also hold an NIH T32 institutional training grant that provides research funding for fellows. The NIH T32 was started in 1974 under the umbrella of the Ruth L. Kirschstein National Research Service Award (NRSA) with the goal of producing a diverse pool of highly trained scientists to address the nation's biomedical, behavioral, and clinical research needs. Applications in dermatology are reviewed alongside those from the specialties of rheumatology and musculoskeletal diseases, under the auspices of the NIAMS.
Table 3.
Funding Opportunities during the Physician‒Scientist Training Period
Abbreviations: ASA, American Skin Association; HHMI, Howard Hughes Medical Institute; PGY, Postgraduate Year; URM, underrepresented minority; USA, United States of America.
A list of the various funding agencies, awards, application time, and websites is provided. General awards are available to all investigative dermatology trainees. Specialized awards are available to trainees on the basis of research topics and demographics.
Investigative dermatologists also have access to individual funding opportunities from governmental sources of funding such as the NIH and Department of Defense. Residents in the research component of their training have access to the NIH F32 postdoctoral fellowship. For trainees who are preparing to transition toward independence, the NIH/NIAMS offers the K99/R00 that funds up to 2 years of mentored research and 3 years of independent research. For MD-only or MD‒PhD trainees, the K08 and K23 awards are available for mentored research. The Department of Defense also offers periodic funding opportunities for topic-specific projects (currently lupus, melanoma, and scleroderma for the 2021 cycle). Trainees should be on the lookout for grants that designate New Investigator or New Investigator Collaboration options, which allow junior faculty to partner with more established faculty to help kick start their careers.
Among the dermatology-specific funding opportunities, the Dermatology Foundation provides multiple awards for investigative dermatologists. The Dermatologist Investigator Research Fellowship provides a 1-year stipend for trainees who will be in the research portion of their residency training. The Career Development Award (CDA) provides up to 3 years of funding for trainees who have 2‒3 years of postdoctoral research training and are looking to become independent. A recent survey of Career Development awardees found that each dollar of CDA funding through 2015 resulted in >$10 in grant support from the NIH as well as other funding sources (Boris et al., 2019), an excellent return on investment. In addition to the Dermatology Foundation, there are several other private organizations that have a long history of supporting physician‒scientists in dermatology, including the American Skin Association and the National Psoriasis Foundation (Table 3).
The Burroughs Wellcome Fund is a nonprofit medical research organization that also provides funding for the greater physician‒scientist community. Investigative dermatologists may apply for the Career Award for Medical Scientists, which helps to transition trainees from advanced postdoctoral training to early faculty. Institutions may also apply for the Physician-Scientist Institutional Award, which provides significant institutional funding for the training of MDs for a career in research. The Burroughs Wellcome Fund also provides an opportunity for postdoctoral funding for URM candidates.
The above funding opportunities represent the major funding sources for investigative dermatologists. However, additional opportunities are available depending on eligibility. The Doris Duke Foundation provides funding for physician‒scientists who are performing human-related research. The Damon Runyon Fellowship and Clinical Investigator awards are available for trainees working on cancer-related projects. L’Oreal’s For Women in Science award is a funding opportunity for women candidates. The Harold Amos Medical Faculty Development Program provides funding for the training of URM candidates and those from disadvantaged backgrounds. Funding opportunities are also available for research on specific dermatologic diseases from their respective organizations.
Finally, the NIH also offers loan repayment programs (LRPs) (Table 3) that are designed to recruit and retain highly qualified health professionals into biomedical or biobehavioral research careers. The LRP will repay up to $50,000 annually of a researcher's qualified educational debt if the trainee commits to engage in research that is relevant to the mission of the NIH. The hope is that by helping to relieve a trainee’s debt burden, this will encourage them to pursue a research career rather than a career in higher-paying private practice or industry.
Table 3 lists the numerous funding opportunities available to investigative dermatologist trainees, along with a link to the respective website. Regarding the perception that they will encounter a lifelong struggle to get their research funded, it should be noted that there are many research funding opportunities at different levels, from institutional grants to foundation grants and to federal and philanthropic grants as outlined in the table. However, the candidates have to get the right training and be creative/innovative in order to be competitive for these awards; they also need to be made aware of these various funding opportunities. This resource will help current and prospective trainees secure funding that is vital for their careers.
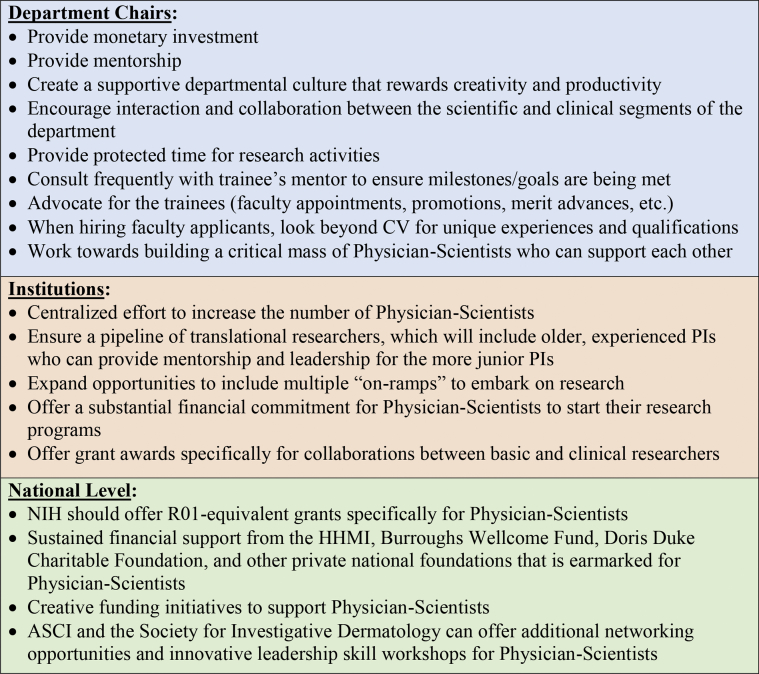
RETAINING THE PHYSICIAN‒SCIENTIST IN DERMATOLOGY
Retention of physician‒scientists is a major challenge that will require expanded efforts and innovative policies to be implemented at the departmental, institutional, and national levels (Figure 3). At the departmental level, the chair must provide protected research time; laboratory space; development monies; personnel support; and other resources, including start-up funding for trainees to smoothly transition to an independent position. A big advantage for physician‒scientists compared with their PhD colleagues is access to patients in the clinic. Thus, another helpful resource that the chair should provide is a Clinical Trial Unit to assist with the administrative burden associated with conducting research involving human subjects and clinical trials, such as developing protocols, fulfilling institutional review board requirements, overseeing patient recruitment and compliance, and others. This will greatly enable the physician‒scientist by providing a well-oiled machine with the necessary knowledge already in place to guide the researcher through the many complex regulatory steps. In addition, the chair should develop a culture within the department that values research, promotes mentorship, rewards discovery and productivity, and enhances collaboration between research faculty and clinical faculty. Finally, the chair should work toward building a critical mass of physician‒scientists, a cohort who can support each other, which includes more seasoned trailblazers who can set an example and provide guidance.
Figure 3.
Action items at different levels to support the retention of physician‒scientists in dermatology. ASCI, American Society of Clinical Investigators; CV, curriculum vitae; HHMI, Howard Hughes Medical Institute; PI, principal investigator.
Another helpful resource would be for the dermatology department to provide the candidate a start-up package that would be front loaded, meaning that it would provide resources from the start such that the candidate could immediately hire a laboratory technician during their training period to help with benchwork and mouse colony management or other technical assistance, and others. Because the candidate will still have clinical obligations, this would be very beneficial and would help them advance and move their research forward.
At the institutional level, there must be a centralized effort to increase the number of physician‒scientists, who can then provide leadership and mentorship for junior physician‒scientists, thus ensuring a pipeline of successful translational researchers (Figure 3). An excellent example of this type of initiative is at the Washington University School of Medicine in St. Louis, which recently established a Division of Physician-Scientists that directly reports to the Dean (https://physicianscientists.wustl.edu/). The goal of the division is to support physician‒scientists by providing resources, mentorships, and research and leadership programs. Other institutions should follow their lead. Institutional support should also include a significant financial commitment for physician‒scientists to start their research laboratories. This could come through special grant opportunities available only to physician‒scientists. A prime example is the University of Texas Southwestern’s Disease-Oriented Clinical Scholar program (https://www.utsouthwestern.edu/education/programs/nondegree-programs/other-programs/disease-oriented/). This award of $1 million over a 4-year period is designed to facilitate state-of-the-art research in clinical departments at the University of Texas Southwestern. Eligible applicants must be early in their career (have held the rank of Assistant Professor for <3 years) and must be nominated by a clinical department chair. Only faculty whose research is directly related to the pathophysiology or treatment of human disease are eligible for this award. This type of grant support enables the physician‒scientist to focus on establishing their research program rather than scrambling for extramural grant support at this critical time of their nascent career.
Finally, at the national level, the NIH should offer funding specifically tailored to the physician‒scientist (Figure 3). Mechanisms exist to fund physician‒scientists during the graduate and postdoctoral period, whereas transitional K awards provide mostly salary support for early-career MD‒PhDs, with very little research support. There are currently no R01-equivalent type grants. With modest pay lines for new principal investigators, receiving one’s first R01 grant is extremely competitive. Having an R01-type funding mechanism specifically for physician‒scientists would encourage patient-oriented research, making it easier for physician‒scientists to obtain independent funding and allowing them to concentrate on building their research career. In addition, continued financial support from private organizations such as the Howard Hughes Medical Institute and Burroughs Wellcome Fund that is earmarked for physician‒scientists is critical as NIH funding becomes increasingly competitive and because budgets can be uncertain. Further expanding private-sector financial support could be another route to increasing the PSW. Another national effort should fall under the auspices of the ASCI. The ASCI is a national honor society for physician‒scientists who have accomplished meritorious original, creative, and independent investigations in the clinical or allied sciences of medicine and are aged <50 years. Candidates for ACSI membership are nominated by a current ACSI member. The ASCI convenes a yearly meeting that provides an important forum for physician‒scientists to share their research, learn about cutting-edge advancements, and network. This organization, along with the Society for Investigative Dermatology and the Dermatology Foundation, can therefore play an important role in supporting physician‒scientists and nurturing their careers by providing an opportunity for them to develop their leadership skills and to pursue collaborations in translationally or clinically oriented research.
CONCLUSIONS AND PERSPECTIVES
Physician‒scientists have been a cornerstone of modern medicine, making countless scientific discoveries. Unfortunately, the PSW has stagnated since their Golden Age and the declining success of physician‒scientist training has raised significant concerns. However, the identification of underlying causes and the proposal of action items by many groups around the country suggest a promising future. To plug the leaky pipeline of physician‒scientist training, there must be a cultural shift to re-emphasize the importance of clinician-guided scientific discovery and an institutional and departmental shift to provide guidance, mentorship, financial support, and other resources for physician‒scientist trainees. Among the many barriers that we discussed, two of the most pressing are (i) recruiting qualified and capable candidates who have a true passion for and commitment to investigative dermatology and (ii) providing adequate and sustained funding at the dermatology department level to train dermatology physician‒scientist candidates as well as available funding at the department, institution, and national level to develop them into productive physician‒scientists.
The number of investigative dermatologists is dwindling. To solve this problem, we must have a centralized effort to provide dedicated funding and a commitment from the field of dermatology to invest in building a pipeline to recruit qualified and diverse candidates for a career in investigative dermatology early in their training, starting even as early as high school but certainly at all levels: high school, undergraduate, medical school, and residency. Otherwise, we are likely to lose them to other specialties or other career tracks. Identifying promising physician‒scientist trainees early in their training and providing continuous mentorship for a future career in investigative dermatology is key. These concerns have been echoed across the greater physician‒scientist community (Jain et al., 2019). This will broaden the pool of qualified applicants, enabling the identification of those with a talent for scientific discovery. The goal is to achieve a critical mass at the institution and national level to build a steady workforce of physician scientists that will continue to make impactful discoveries and revolutionize how we treat our patients. Importantly, these measures will also help in the recruitment and support for URMs and women physician‒scientists to help bring greater diversity and perspectives to this career.
As physician‒scientist training is analyzed and reworked at all levels, it will be important for dermatology to increase recruitment efforts and support for physician‒scientist trainees because investigative dermatologists play a vital role in the health and future of dermatology. To measure the success of these efforts, we must develop unified metrics that would include (i) retaining a high percentage of physician‒scientist trainees in academic positions, (ii) having physician‒scientists who are actively engaged in research/scholarly work, (iii) having sustained/continuous funding to support their research, (iv) making impactful discoveries to amplify the voice of dermatology in the medical field, and (v) successfully training the next generations of physicians and scientists. Investment in these trainees will ensure the continued development of future leaders who will push the boundaries of knowledge.
ORCIDs
Stephen Li: http://orcid.org/0000-0001-5010-771X
Kim B. Yancey: http://orcid.org/0000-0001-6101-4690
Ponciano D. Cruz Jr: http://orcid.org/0000-0002-1550-6149
Lu Q. Le: http://orcid.org/0000-0003-2817-5382
Conflict of Interest
KBY is a coprincipal investigator on the National Institute of Health T-32 Award–an award used to support trainees of the sort described in this manuscript. KBY also serves as a coprincipal investigator on a National Institute of Health‒sponsored phase I clinical trial “the Use of Autologous T Regulatory Cells in Patients with Pemphigus.” KBY has also received royalties from UpToDate for authorship of a monograph “Treatment of MMP”. The remaining authors state no conflict of interest.
Acknowledgments
We thank Renee McKay for a critical review of this manuscript. SL is supported through the Medical Scientist Training Program at The University of Texas Southwestern Medical Center (Dallas, TX) and an F30 fellowship from the National Institute on Aging of the National Institutes of Health (Bethesda, MD) (F30AG056075). LQL held a Career Award for Medical Scientists from the Burroughs Wellcome Fund and a Physician-Scientist Career Development Award from the Dermatology Foundation and is supported by funding from the National Cancer Institute of the National Institutes of Health (grant number R01 CA166593) and the United States Department of Defense. This work is funded by the Dermatology Research Training Program T32 grant T32AR065969.
Author Contributions
Conceptualization: LQL; Writing - Original Draft Preparation: SL, LQL; Writing - Review and Editing: SL, KBY, PDCJ, LQL
accepted manuscript published online 19 October 2021; corrected proof published online 2 December 2021
Footnotes
Cite this article as: JID Innovations 2022;2:100061
References
- Akabas M.H., Brass L.F. The national MD-PhD program outcomes study: outcomes variation by sex, race, and ethnicity. JCI Insight. 2019;4 doi: 10.1172/jci.insight.133010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andriole D.A., Grbic D., Yellin J., McKinney R. MD–PhD program graduates' engagement in research: results of a national study. Acad Med. 2021;96:540–548. doi: 10.1097/ACM.0000000000003516. [DOI] [PubMed] [Google Scholar]
- Association of American Medical Colleges . Association of American Medical Colleges; Washington, DC: 2018. National MD-PhD program outcomes study. [Google Scholar]
- Bernstein R. Faculty searches get a facelift. Cell. 2014;159:5–8. doi: 10.1016/j.cell.2014.09.006. [DOI] [PubMed] [Google Scholar]
- Boris C., Cotsarelis G., Fairley J.A., Wintroub B.U., Yancey K.B. A cross-sectional survey and analysis of Dermatology Foundation Career Development Award recipients. J Am Acad Dermatol. 2019;81:1093–1098. doi: 10.1016/j.jaad.2018.11.034. [DOI] [PubMed] [Google Scholar]
- Brass L.F., Akabas M.H. The national MD-PhD program outcomes study: relationships between medical specialty, training duration, research effort, and career paths. JCI Insight. 2019;4:e133009. doi: 10.1172/jci.insight.133009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brass L.F., Akabas M.H., Burnley L.D., Engman D.M., Wiley C.A., Andersen O.S. Are MD-PhD programs meeting their goals? An analysis of career choices made by graduates of 24 MD-PhD programs. Acad Med. 2010;85:692–701. doi: 10.1097/ACM.0b013e3181d3ca17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown N.J. Promoting the success of women and minority physician-scientists in academic medicine: a dean's perspective. J Clin Invest. 2020;130:6201–6203. doi: 10.1172/JCI144526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erzurum S.C. Aging and scientific medicine: 60 is the new 40. J Clin Invest. 2018;128:4204–4207. doi: 10.1172/JCI124523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein J.L., Brown M.S. The clinical investigator: bewitched, bothered, and bewildered--but still beloved. J Clin Invest. 1997;99:2803–2812. doi: 10.1172/JCI119470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein J.L., Brown M.S. History of science. A golden era of Nobel laureates. Science. 2012;338:1033–1034. doi: 10.1126/science.1231699. [DOI] [PubMed] [Google Scholar]
- Harding C.V., Akabas M.H., Andersen O.S. History and outcomes of 50 years of physician-scientist training in medical scientist training programs. Acad Med. 2017;92:1390–1398. doi: 10.1097/ACM.0000000000001779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain M.K., Cheung V.G., Utz P.J., Kobilka B.K., Yamada T., Lefkowitz R. Saving the endangered physician-scientist - A plan for accelerating medical breakthroughs. N Engl J Med. 2019;381:399–402. doi: 10.1056/NEJMp1904482. [DOI] [PubMed] [Google Scholar]
- Kwan J.M., Daye D., Schmidt M.L., Conlon C.M., Kim H., Gaonkar B., et al. Exploring intentions of physician-scientist trainees: factors influencing MD and MD/PhD interest in research careers. BMC Med Educ. 2017;17:115. doi: 10.1186/s12909-017-0954-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milewicz D.M., Lorenz R.G., Dermody T.S., Brass L.F., National Association of MD-PhD Programs Executive Committee Rescuing the physician-scientist workforce: the time for action is now. J Clin Invest. 2015;125:3742–3747. doi: 10.1172/JCI84170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of General Medical Sciences Medical Scientist Training Program (MSTP) institutions. 2021. https://www.nigms.nih.gov/training/instpredoc/pages/predocinst-MSTP.aspx (accessed July 2021)
- Oliveira D.F.M., Ma Y., Woodruff T.K., Uzzi B. Comparison of National Institutes of Health grant amounts to first-time male and female principal investigators. JAMA. 2019;321:898–900. doi: 10.1001/jama.2018.21944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Permar S.R., Ward R.A., Barrett K.J., Freel S.A., Gbadegesin R.A., Kontos C.D., et al. Addressing the physician-scientist pipeline: strategies to integrate research into clinical training programs. J Clin Invest. 2020;130:1058–1061. doi: 10.1172/JCI136181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Physician Scientist Workforce Working Group . National Institutes of Health; Bethesda, MD: 2014. Physician-scientist workforce working group report. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reese T.A., Harris-Tryon T.A., Gill J.G., Banaszynski L.A. Supporting women in academia during and after a global pandemic. Sci Adv. 2021;7 doi: 10.1126/sciadv.abg9310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg L.E. MD/PhD programs--a call for an accounting. JAMA. 2008;300:1208–1209. doi: 10.1001/jama.300.10.1208. [DOI] [PubMed] [Google Scholar]
- Rubenstein D.S., Blauvelt A., Chen S.C., Darling T.N. The future of academic dermatology in the United States: report on the resident retreat for future physician-scientists, June 15–17, 2001. J Am Acad Dermatol. 2002;47:300–303. doi: 10.1067/mjd.2002.123491. [DOI] [PubMed] [Google Scholar]
- Schmid S.L. Beyond CVs and impact factors: an employer's manifesto. Science. 2013. https://www.science.org/content/article/beyond-cvs-and-impact-factors-employers-manifesto (accessed July 7, 2020)
- The Nobel Foundation All Nobel Prizes in physiology or medicine. 2020. https://www.nobelprize.org/prizes/lists/all-nobel-laureates-in-physiology-or-medicine
- Wang K., Lee C.S., Marinkovich M.P., Chang H.Y., Oro A.E., Khavari P.A. Factors that may promote an effective local research environment. J Invest Dermatol. 2016;136:1529–1531. doi: 10.1016/j.jid.2016.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitcomb M.E. The need to restructure MD-PhD training. Acad Med. 2007;82:623–624. doi: 10.1097/ACM.0b013e318065b4ba. [DOI] [PubMed] [Google Scholar]
- Wong M.D., Guerrero L., Sallam T., Frank J.S., Fogelman A.M., Demer L.L. Outcomes of a novel training program for physician-scientists: integrating graduate degree training with specialty fellowship. J Grad Med Educ. 2016;8:85–90. doi: 10.4300/JGME-D-15-00135.1. [DOI] [PMC free article] [PubMed] [Google Scholar]