Abstract
Objetive
We conducted a randomized double blind clinical trial, to compare the effectiveness of McKenzie exercises and electroanalgesia via an e-Health program versus a home rehabilitation program on functionality, pain, fear of movement and quality of life in patients with non-specific chronic low back pain.
Methods
Seventy-four participants with non-specific chronic low back pain were randomized to either the e- Health program group (n = 39) or the home rehabilitation program group (n = 35). The interventions consisted of the e-Health program group performing McKenzie exercises and received transcutaneous electrical nerve stimulation, while the home rehabilitation group attended an information session to explain the exercises, which they then performed at home with printed instructions. Both groups performed 3 weekly sessions for 8 weeks. The following were analyzed main measures: pain, disability, fear of movement, quality of life, trunk muscle endurance and trunk anteflexion motion were assessed at baseline and at 2 months.
Results
Independent samples Student’s t-tests showed that although the patients who followed the e-Health program showed significantly greater improvement than those who followed the home disability rehabilitation program in terms of intensity of pain, lumbar flexion mobility (P < 0.001), and the following dimensions of quality of life (P < 0.005), both groups improved significantly in the immediate post-treatment follow up compared with baseline scores.
Conclusions
Patients with chronic low back pain who followed an unsupervised home intervention supported by an individualized video exercise program showed greater post-treatment improvement than those who followed the same program with printed instructions.
Keywords: Chronic low back pain, general, telemedicine, home rehabilitation, McKenzie exercises, transcutaneous electrical nerve stimulation, randomized controlled trial
Introduction
Low back pain (LBP) is the main cause of activity limitation and absence from work in most countries. It is associated with a considerable economic burden,1,2 and has been considered the main contributor to years lived with disability. 3
Although nonspecific LBP has no known pathoanatomical cause, treatment focuses on reducing pain and its consequences. Spinal instability has been an important clinical factor in back pain. Different studies have shown that people with back pain appear to have different recognition patterns for the control of deep lumbar stabilizing muscles.4,5 Given the relationship between alterated neuromuscular function and LBP, there is clearly a need for reeducation exercises to correct lumbo-pelvic stabilization, as well as other treatments that improve pain.6,7
Studies and clinical practice guidelines recommend several possible interventions for the treatment and management of LBP, ranging from active participation through exercise to passive methods such as electroanalgesia.8,9 Evidence has shown that transcutaneous electrical nerve stimulation (TENS) is a cost-effective intervention that activates both central and peripheral mechanisms to reduce hyperalgesia.10,11 Facci et al. 12 found that applying 30 min of TENS current at a comfortable intensity, adjusted according to each patient's sensitivity, reduced pain intensity, improved disability, and reduced drug use in patients with nonspecific chronic low back pain. Furthermore, others studies has obtained beneficial results of TENS current in the control of non-radicular pain with respect to a control group or to other more conventional treatments in patients with chronic low back pain. 13 Regarding functional disability, the TENS current has also shown positive results in a short period of time, on the other hand, in follow-ups longer than 6 weeks the evidence is limited. 14
Clinical practice guidelines recommend self-care exercises as a key strategy in the treatment of patients with chronic LBP, and prioritize primary care triage for the management of patients with LBP. Triage consists of classifying patients according to their signs and symptoms in order to prescribe certain exercises, give advice to patients who remain active, and provide information on effective self-care options.15,16 The McKenzie Method is a widely-used, comprehensive approach to chronic LBP that includes both an evaluation and intervention component. The evaluation component of the McKenzie Method classifies patients with LBP into subgroups, each with a specific management approach. 17 There is also evidence that home rehabilitation programs with good compliance are moderately effective in reducing pain and improving function in chronic LBP, and also reduce healthcare costs. 18 Recent evidence has shown that a McKenzie therapy program based on telerehabilitation obtained clinical results comparable to traditional McKenzie therapy performed under supervision, and could reduce the healthcare burden of LBP. 19
Currently, digital health systems are considered a promising innovation to solve the demand for health resources as a consequence of the aging of the population and the scarce material and human resources available to health institutions.20,21 In chronic disease such as low back pain, the telemedicine can be an effective alternative of intervention for patients can manage different components of their health such as functional independence, self-care, and self-maintenance of their disease.22–24 In addition to being a scalable, universally accessible and low-cost approach within the multidisciplinary treatment of low back pain. 25
The objective of this study was to compare the effectiveness of an e-health program versus home rehabilitation based on McKenzie exercises and TENS treatment to reduce disability, pain, fear of movement, and improve quality of life and spinal mobility in patients with chronic LBP.
Methods
Study design and study setting
We conducted a double blind randomized controlled comparative trial with a 6-month follow-up period between January 2018 and December 2020. The study protocol was approved by the Human Research Ethics Committee of the “Hospital Complex Torrecárdenas of Almeria, University Hospital Complex of Granada and Hospital Virgen Macarena of Sevilla – Andalusian Health Service” (CFS/apg), and registered on clinicaltrials.gov (protocol number NCT03469024)
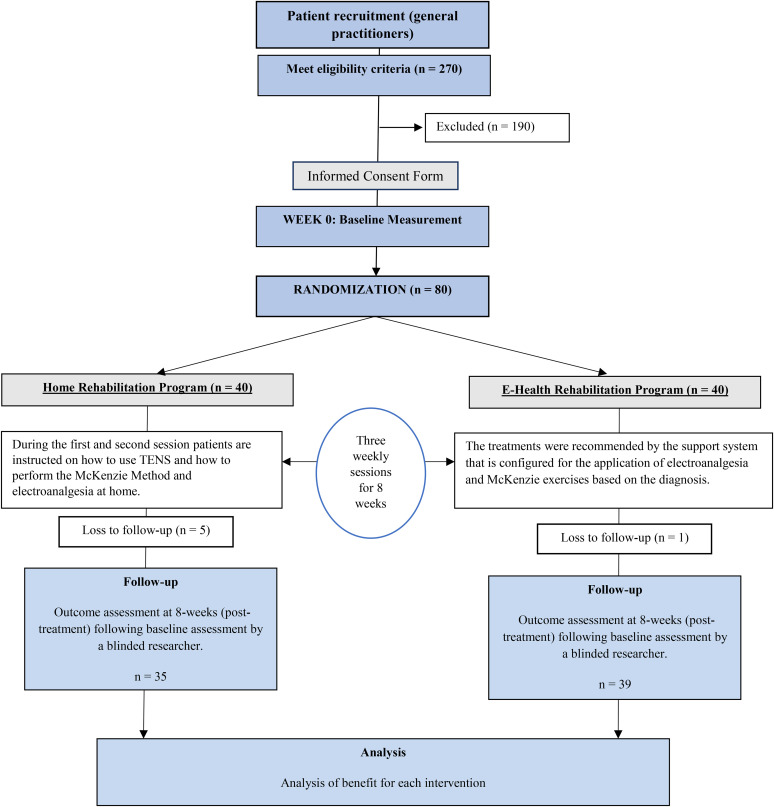
Two hundred and seventy patients with nonspecific chronic LBP treated in the outpatient physiotherapy departments of 3 Andalusian Health Service hospitals were selected to participate in this trial. After referral by a general practitioner, patients were interviewed by phone to determine whether they met the inclusion or exclusion criteria. After telephone and face-to-face screening, only 80 of the patients that had agreed to participate were eligible for the study. All patients provided written informed consent to participate in the study. (Figure 1) shows a brief outline of the design of the trial.
Figure 1.
Brief outline of the design of the trial.
Participants
Patients with non-specific LBP for at least 3 months, who were aged between 30 and 67 years, had a disability score of 4 or more on the Roland Morris Disability Questionnaire (RMQ) for LBP, and were not receiving any other physiotherapy treatment were eligible for inclusion. Exclusion criteria were: contraindication for McKenzie exercises or TENS such as fracture, infection, cancer, or cauda equina syndrome; presence of clinical signs or symptoms of radiculopathy; known medical diagnosis of spondylolisthesis, spinal stenosis, inflammatory or metabolic disease, fibromyalgia, presence of central or peripheral system pathology (i.e, stroke, peripheral nerve, etc.) or history of spinal surgery; and no corticosteroids or other drug therapy in the preceding 2 weeks.
Sample size
The sample size was based on the estimates established by Willian. 26 The calculations have been based on the detection of differences of 2.5 points in the RMQ score (minimum clinically important difference), 27 assuming a standard deviation of 2.5 points, a 2-tailed test, an alpha (α) of 0.05, and a target power (beta) of 85%. The estimated sample size was 80 subjects (40 per group).
Randomization
After a baseline examination, patients were randomly assigned to follow a telemedicine program that included TENS and McKenzie Method exercises, or the same program with no online support. Allocation was concealed using a computer-generated randomized table of numbers (software Epidat 4.2) created prior to the start of data collection by a researcher not involved in either recruitment or treatment. Index cards sequentially numbered according to the random assignment were printed, folded, and placed in sealed opaque envelopes. A third therapist, blinded to baseline examination findings, opened the envelope, assigned the patient to the corresponding study group, and booked their first treatment session. Patients were assessed by 2 blinded physical therapists associated with Almeria University who had more than 10 years’ experience in the clinical management of patients with chronic LBP.
Outcomes measures
All data were gathered before the first treatment session (baseline) and immediately after the final treatment session by a physical therapist blinded to the patient's treatment allocation. Patients provided demographic and clinical information and completed a number of self-administered questionnaires: the Roland Morris Disability Questionnaire, 28 the SF-36 Health Questionnaire,29,30 the Oswestry Disability Index, 31 the Visual Analog Scale, 32 the Tampa Scale for Kinesiophobia, 33 the McQuade test, 34 Spinal movement was assessed using the Fingertip-to-Floor Distance test. 35
Adherence to treatment was evaluated on the basis of diary entries made by patients in the Home rehabilitation group, and according to the number of logins and time spent on the online program by patients in the E-health group.
The main independent variable was the Roland Morris Disability Questionnaire – a 24-item patient-reported disability measure with a score ranging from 0 = no disability to 24 = severe disability. 28 SF-36 Health Questionnaire scores range from 0% to 100% and indicate the self-perceived health-related quality of life.29,30 The Oswestry disability index evaluates limitations in activities of daily living in 10 dimensions, each scored on a 6-point scale (0–5 points). The total score is expressed as a percentage that classifies individuals as minimally disabled (0%–10%), moderately disabled (20%–40%), severely disabled (40%–60%), crippled (60–80%), or bedbound (80%–100%). 31 The visual analogue scale for pain intensity ranges from 0 = no pain to 10 = worst imaginable pain. 32 The Tampa Scale of Kinesiophobia is a 17-item questionnaire that rates the respondent's fear of movement or recurrent lesion. Each item is scored on a 4-point Likert scale, ranging from “completely disagree” to “completely agree”. 33 The McQuade test measures the isometric resistance of abdominal muscles in seconds. 34 Lumbar mobility in flexion was determined by measuring the distance from the tip of the third finger to the floor with a tape measure. 35
Both the outcome assessor and statistician were blinded to the entire study. The outcome assessor was not involved in treatment and did not attempt to guess the participant's group. The computerized outcome measures received by the statistician did not contain any information identifying patients as belonging to either group.
Intervention
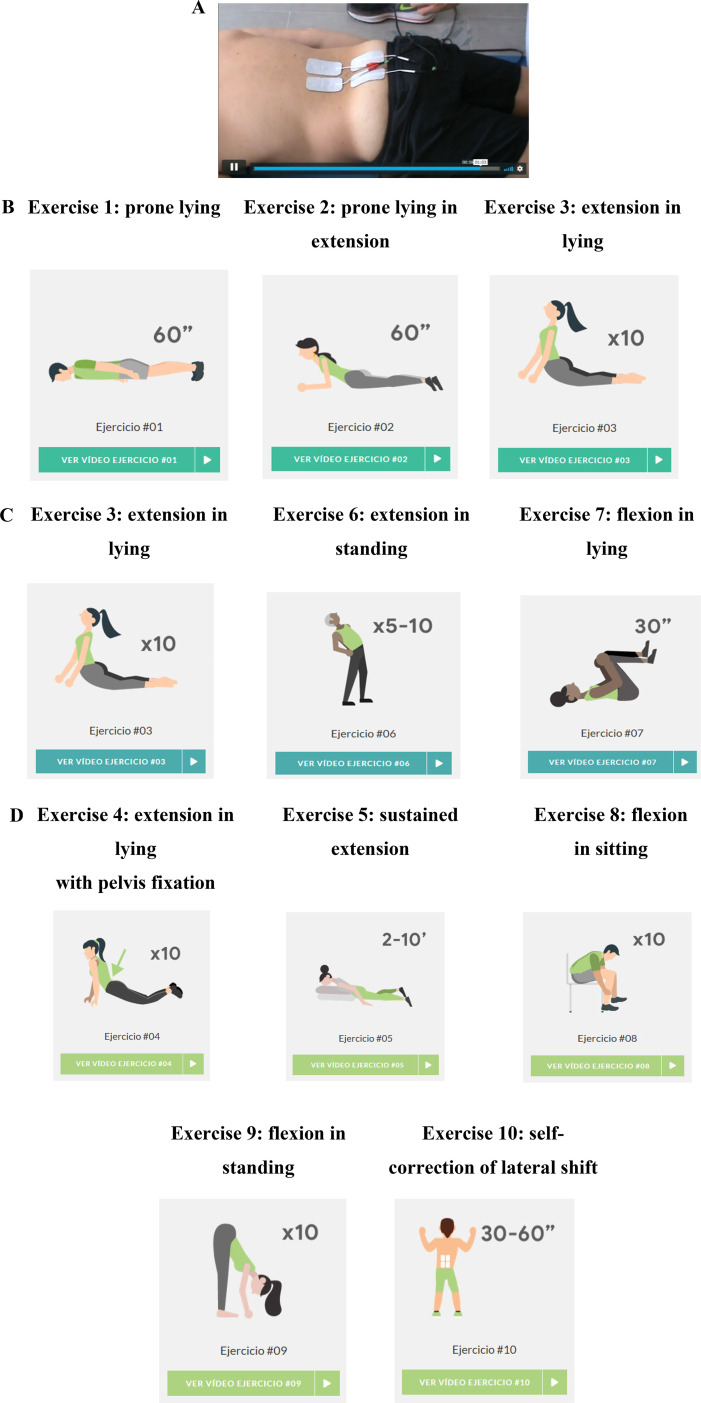
The McKenzie treatment was planned individually after the pretreatment physical assessment and before randomization; therefore, patients in each group were divided into 3 subgroups (postural, dysfunction and derangement) according to the McKenzie therapeutic classification, which divides them according to symptoms and their frequency of appearance; limitation of mobility; results of dynamic tests and persistence of symptoms when mechanical loading (static or dynamic) is withdrawn. All patients were treated by 2 physical therapists with more than 10 years of clinical experience with patients, and with at least 5 years certified application of the McKenzie Method after completing their physical therapy degree. Both groups performed 3 sessions weekly for 8 weeks. The protocol was as follows (Figure 2).
Figure 2.
Protocol of mcKenzie exercise and transcutaneous electrical nerve stimulation. (A) Transcutaneous electrical nerve stimulation (80 Hz/200 µs) applied directly in the lumbar area by four electrodes (5 × 9 cm) at the paravertebral level bilateral. (B) Patients with Postural Syndrome: Exercises 1, 2 and 3. (C) Patients with Dysfunction Syndrome: Exercises 3, 6 and 7. (D) Patients with Derangement Syndrome (DS): Exercises 1 to 10 (according to type of derangement syndrome).
Home rehabilitation program group
This consisted of an unsupervised home rehabilitation program with no online support. During first and second 60 min session, a therapist taught the patients how to use a portable low-frequency, high intensity TENS (80 Hz/200 µs) device applied directly to the lumbar region by means of 4 electrodes (5 × 9 cm) placed bilaterally at the paravertebral level, and how to perform their exercises, which were individualized according to the diagnosis and mechanical therapy of the McKenzie Method. The patient continued the protocol at home until completing the 24 sessions.
Each subgroup of patients performed the following exercises simultaneously with TENS:
Patients with Postural Syndrome: exercises 1, 2 and 3 (posture correction and prophylaxis).
Patients with Dysfunction Syndrome: exercises 3, 6 and 7.
- Patients with Derangement Syndrome (DS):
- □ DS 1: exercises 1–4 and 6, with prone extension.
- □ DS 2: the exercises begins in the prone position and the patients continue with protocol DS1 and exercise 5.
- □ DS 3: DS1 protocol, exercise 7 and rotation maintained for 2 min.
- □ DS 4: exercise 7, exercise 2 and 3, and DS 1 protocol.
- □ DS 5: exercise 7 and 8, and exercise 1–3.
- □ DS 6: DS4 protocol, followed by the DS1 and DS3 protocol.
- □ DS 7: exercises 7–10.
A booklet and laminated cards with detailed photographs of each exercise prescribed were provided.
E-Health program group
This is an internet-based system for the treatment of chronic LBP, accredited as a healthcare website. The system registers the subjects and provides individualized treatment of electroanalgesia and exercise using the McKenzie Method. Patients access the platform on a computer or mobile device and watch electroanalgesia and exercise videos with a duration of 1 to 3 min depending on the time of completion. The videos are preceded by an explanatory image and audio instructions during playback. The number of exercises and treatment are recommended by the system from the database that is configured to accommodate the application of electroanalgesia and McKenzie exercises, depending on the diagnosis made according to the McKenzie Method, programs of 3 to 9 exercises can be established.
In the first 5 sessions, the patient receives instructions on how the app works and records his or her data. He then continues the treatment at home until 24 sessions have been completed.
Both the app and the booklet given to the control group included information on the specific characteristics of the diagnosed syndrome and explained the benefits of these exercises for chronic low back pain.
Statistical analysis
Data were analyzed with SPSS© version 21.0, using intention-to-treat analysis. When post-intervention data were missing, baseline scores were used. The analysis of the data from the outcome measures was performed by the statistician who remained blinded to group allocation until the analysis was completed. The sample was size was calculated before the start of the study. The primary outcome measure was the change in the RMQ score at the end of the 8-week study period (post-treatment follow-up after the last session).
The data were tested for normality using the Kolmogorov-Smirnov test. The independent samples t-test was used to compare the effect of treatment (E-health vs. Home rehabilitation). The paired t-test was used to compare variables before (baseline) and after (post-treatment) treatment in each group. The confidence interval was established at 95%, and the significance level at 0.05. Effect size was tested using Cohen's d. An effect size < 0.2 indicates a negligible difference, between ≥0.2 and ≤0.5 a small difference, between ≥0.5 and ≤0.8 a moderate difference, and ≥0.8 a large difference.
Results
Two hundred seventy consecutive patients were screened for eligibility. Eighty patients (mean ± SD age: 47.96 ± 12.85) satisfied all the eligibility criteria, agreed to participate, and were randomized to the E-Health (telemedicine) (n = 40) or Home rehabilitation (n = 40) program; 6 participants dropped out before completion due to inability to comply with required study visits; change of residence and illness due to Covid-19. The reasons for ineligibility and withdrawal are shown in (Figure 1). A summary of demographic characteristics for the 74 enrolled subjects is shown in (Table 1). There were no significant differences between the baseline data of both groups (p > 0.05).
Table 1.
Baseline demographic data of patients.
| Parameters | Baseline | Pre | |
|---|---|---|---|
| E-health program (n = 39) | Home program (n = 35) | P Value | |
| Gender (m/f) | 17/22 | 14/21 | 0.543 |
| Age (y) (Mean ± SD) | 41.9 ± 9.4 | 54.6 ± 12.9 | 0.097 |
| Level of studies | |||
| Primary | 5 | 7 | |
| High school or institute | 15 | 11 | |
| University studies | 19 | 17 | |
| McKenzie classification | |||
| Postural Syndrome | 0 | 0 | |
| Dysfunction Syndrome | 9 | 11 | |
| Derangement Syndrome | 30 | 24 | |
p-value of 0.05.
Table 2 shows the mean outcomes by group at all time points and inter-group differences with a 95% confidence interval (CI). The results showed that although the patients who received telemedicine (E-health group) showed significantly greater improvement than those who following the Home rehabilitation program in most outcomes, both groups improved significantly in the immediate post-treatment follow-up compared with baseline scores: E-health group (score changes for Roland Morris: 7.4; Oswestry: 11.4; Visual analog scale: 4.5; Tampa Scale for Kinesiophobia: 10; McQuade Test: 17.1; Lumbar mobility flexion: 11.6; Physical function: 16.6; Physical role: 30.7; Bodily pain: 12.6; General Health: 16.7; Vitality: 21.5; Social functioning: 8.3; Emotional role: 23.3; and Mental health: 22.2) and Home rehabilitation group (score changes for Roland Morris: 1.9; Oswestry: 5.1; Visual analog scale: 2.2; Tampa Scale for Kinesiophobia: 4.4; McQuade Test: 17.7; Lumbar mobility flexion: 1.7; Physical function: 9.2; Physical role: 18.2; Bodily pain: 15.6; General Health: 5; Vitality: 3.3; Social functioning: 3.2; Emotional role: 8.9; and Mental health: 5.7).
Table 2.
Outcome measures for subjects by groups and time.
| Outcome/group | e-health program (n = 39) | Home rehabilitation program (n = 35) | Inter-group difference in score change | P Value | Cohen’s d |
|---|---|---|---|---|---|
| RMD (0–24) | |||||
| Baseline | 9.92 ± 4.35 | 9 ± 3.98 | 0.92 (−1.01, 2.86) | 0.346 | |
| Post-treatment | 2.49 ± 2.19 | 7.03 ± 4.59 | −4.54 (−6.18, −2.90) | 0.001 a | 1.16 |
| ODI (0–50) | |||||
| Baseline | 17.53 ± 11.91 | 21.80 ± 11.63 | −4.26 (−9.73, 1.21) | 0.125 | |
| Post-treatment | 6.10 ± 5.76 | 16.71 ± 10.07 | −10.61 (−14.36, −6.85) | 0.001 a | 1.16 |
| VAS (0–10 points) | |||||
| Baseline | 6.72 ± 1.29 | 6.71 ± 1.15 | 0.00 (−0.56, 0.57) | 0.990 | |
| Post-treatment | 2.20 ± 1.39 | 4.48 ± 2.03 | −2.28 (−3.08, −1.48) | 0.001 a | 1.14 |
| TSK (17–68) | |||||
| Baseline | 37.64 ± 8.07 | 34.40 ± 8.73 | 3.24 (−0.65, 7.13) | 0.101 | |
| Post-treatment | 27.59 ± 6.68 | 30.00 ± 8.02 | −2.41 (−5.82, 0.99) | 0.163 | 0.28 |
| Quality of life SF-36/group (0–100) | |||||
| Physical function | |||||
| Baseline | 76.41 ± 16.58 | 72.14 ± 11.39 | 4.27 (−2.40, 10.94) | 0.206 | |
| Post-treatment | 93.08 ± 8.71 | 81.43 ± 12.28 | 11.64 (6.75, 16.54) | 0.001 a | 0.95 |
| Physical role | |||||
| Baseline | 58.72 ± 21.29 | 59.57 ± 18.60 | −0.85 (−10.17, 8.46) | 0.856 | |
| Post-treatment | 89.48 ± 17.00 | 77.86 ± 16.90 | 11.63 (3.76, 19.50) | 0.004 a | 0.56 |
| Body pain | |||||
| Baseline | 59.83 ± 19.84 | 53.21 ± 14.93 | 6.62 (−1.59, 14.83) | 0.113 | |
| Post-treatment | 72.45 ± 17.97 | 68.78 ± 13.38 | 3.66 (−3.75, 11.07) | 0.328 | 0.18 |
| General health | |||||
| Baseline | 65.89 ± 17.01 | 63.28 ± 14.85 | 2.61 (−4.83, 10.05) | 0.486 | |
| Post-treatment | 67.41 ± 17.86 | 68.28 ± 15.24 | −0.87 (−8.61, 6.86) | 0.822 | 0.04 |
| Vitality | |||||
| Baseline | 61.28 ± 14.35 | 67.28 ± 13.79 | −6.00 (−12.54, 0.53) | 0.071 | |
| Post-treatment | 82.82 ± 12.24 | 70.57 ± 12.59 | 12.25 (6.49, 18.01) | 0.001 a | 0.81 |
| Social functioning | |||||
| Baseline | 78.51 ± 22.60 | 71.78 ± 16.69 | 6.73 (−2.57, 16.02) | 0.154 | |
| Post-treatment | 86.86 ± 19.23 | 75.00 ± 17.41 | 11.86 (3.32, 20.39) | 0.007 a | 0.52 |
| Emotional role | |||||
| Baseline | 71.54 ± 26.85 | 76.72 ± 24.94 | −5.17 (−17.23, 6.88) | 0.395 | |
| Post-treatment | 94.88 ± 12.17 | 85.71 ± 23.27 | 9.16 (0.68, 17.64) | 0.035 a | 0.45 |
| Mental health | |||||
| Baseline | 71.43 ± 13.85 | 74.63 ± 11.43 | −3.19 (−9.12, 2.73) | 0.286 | |
| Post-treatment | 93.64 ± 7.98 | 80.34 ± 10.59 | 13.29 (8.97, 17.62) | 0.001 a | 1.22 |
| Physical measurements | |||||
| McQuade test (s) | |||||
| Baseline | 46.28 ± 13.82 | 42.71 ± 11.14 | 3.57 (−2.29, 9.43) | 0.229 | |
| Post-treatment | 63.38 ± 17.58 | 60.48 ± 9.12 | 2.89 (−3.70, 9.50) | 0.384 | 0.15 |
| Lumbar flexion mobility (cm) | |||||
| Baseline | 19.15 ± 13.83 | 16.36 ± 8.28 | 2.78 (−1.53, 7.09) | 0.203 | |
| Post-treatment | 7.55 ± 4.98 | 12.40 ± 7.74 | −4.86 (−7.84, −1.87) | 0.002 a | 0.66 |
Values are expressed as mean ± standard deviation for baseline and immediate post-treatment and as mean (95% confidence interval) for inter-group change scores. Abbreviations: ODI = Oswestry Disability Index; RMD = Roland-Morris Low Back and Disability Questionnaire; TSK = Tampa Scale for Kinesiophobia; VAS = Visual Analogue Scale.
The outcome measures with statistically significant differences between groups according to the Student’s t-tests were: disability (Roland Morris and Oswestry), intensity of pain, lumbar flexion mobility (p < 0.001), and the following dimensions of the SF-36: physical function, physical role, vitality, social functioning, emotional role, and mental health (p < 0.005).
However, the Student’s t-test analysis found no significant inter-group differences in the Tampa Scale for Kinesiophobia (p < 0.163), or the McQuade test (p < 0.384); patients in both groups experienced similar improvements in fear of movement and isometric resistance of abdominal muscles: E-health group (Kinesiophobia: p < 0.001; McQuade: p < 0.001) and Home rehabilitation group (Kinesiophobia: p < 0.001; McQuade: p < 0.001).
Discussion
Although the main findings of our study revealed significant inter-group differences, and the e-health intervention appeared to be the more favorable method of treatment, post-treatment improvements were observed in all outcomes in both the E-health group and the Home rehabilitation group.
The intra-group comparison of participants in the E-health and Home program groups in the post-treatment period (2 months from the start of treatment / after the last session) revealed that exercise therapy based on the McKenzie Method combined with TENS performed at home without or with the help of a tablet or mobile phone application had a significant effect on disability, pain intensity, isometric resistance of the abdominal muscles, lumbar anteflexion mobility, and quality of life. These findings are consistent with previous studies in the use of the McKenzie protocol,19,36–38 and in transcutaneous electrical nerve stimulation,39,40 although few authors have used both therapies simultaneously. 41 In Deyo et al. 41 transcutaneous electrical nerve stimulation was no more effective than placebo, and added no apparent benefit to exercise alone.
The positive results observed in both study groups could also be due to good compliance with both interventions, irrespective of the use of online support. Various studies have shown that treatment compliance determines the effectiveness of home exercise programs.42–44 We believe that the performance of simple, easily mastered exercises individualized to each patient that gave perceptible benefits might have boosted our patient's confidence in the treatment prescribed, and improved the rate of compliance – a finding that has also been reported in other studies. 45
Our results indicated that the rehabilitation program with online support (E-health group) provided greater improvement in disability, pain, physical function, vitality, and mental health than the same program without online support (Home group) (Cohen’s d ≥ 0.8); the remaining outcome measures showed small or moderate effect size. The differences could be due to the help and motivation in performing the exercises and placing the electrodes that the telemedicine group received from the online program. There is evidence that interventions in patients with chronic musculoskeletal disease performed online (telehealth) through video and audio materials can be as effective as those based on traditional printed instructions. 46 The audiovisual instructions helped patients understand the exercises and perform them correctly, and this could have improved compliance, self-control and symptoms, and helped them achieve their targets.47–49
This leads us to believe that the support of an online platform during the home program increased patient motivation and interest in the intervention, making it more effective in the short and medium term than the same home physiotherapy program performed without online support.
One of the limitations of our study is that follow-up was only performed in the short term, so we cannot be sure that our results would be maintained in the long-term, and more extensive longitudinal studies are needed. Although studies have shown that telehealth outcomes are comparable to face-to-face programs, and online applications can improve home treatment for people with chronic illnesses,50,51 evidence also suggests that outcomes and patient satisfaction improve with a program that combines telehealth and traditional healthcare. 52
Our conclusions suggest that unsupervised interventions at home supported by simple online health technologies based on individualized exercise videos may be more beneficial in improving symptoms in patients with non-specific chronic LBP than traditional home programs based on printed instructions. However, high-quality randomized trials with long-term follow-up that explicitly address the same type of home rehabilitation program are needed.
Acknowledgements
We thank, above all, our study participants for their time, dedication, and enthusiasm. We would also like to thank the clinicians, research staff, and Almeria University for making this study possible.
Footnotes
Contributorship: ICLP: authoring of first draft of the manuscript, study design, manuscript editing, supervision, and project administration. EAS, GAMP, MFS, HGL and AMCS: Conceptualization, methodology, writing, reviewing and editing. MEAF: Conceptualization, methodology, investigation, formal analysis, writing, reviewing and editing, and visualization. All authors read and approved the final manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Andalusian Health Service, Junta de Andalucía (grant number PC-0185-2017, PC-0253-2017 and PC-0536-2017, PI18/00562 Proyecto E-CEPEDOL). This study was funded by a research grant (PI18/00562 Proyecto E-CEPEDOL co-funded by FEDER – European Regional Development Fund/European Social Fund “A way to make Europe”/“Investing in your future”) from the Carlos III Health Institute and 3 grants from the Andalusian Health Service, Junta de Andalucía (PC-0185-2017, PC-0253-2017 and PC-0536-2017). The funders did not take part in the design of the study, its implementation, analysis, data interpretation an/or the presentation of results.
Ethical approval: The Human Research Ethics committee of the “Hospital Complex Torrecárdenas of Almeria, University Hospital Complex of Granada and Hospital Virgen Macarena of Sevilla – Andalusian Health Service” (CFS/apg), and registered on clinicaltrials.gov (protocol number NCT03469024).
Guarantor: The Carlos III Health Institute.
Informed consent: Not applicable, because this article does not contain any studies with human or animal subjects.
ORCID iD: Héctor García-López https://orcid.org/0000-0003-3160-7692
Trial registration: Not applicable, because this article does not contain any clinical trials.
References
- 1.Kent PMKJ. The epidemiology of low back pain in primary care. Chiropractice and Osteopathy 2005; 26: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schaafsma FG, Whelan K, van der Beek AJet al. et al. Physical conditioning as part of a return to work strategy to reduce sickness absence for workers with back pain. Cochrane Database Syst Rev 2013; 8: CD001822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoy D, March L, Brooks P, et al. The global burden of low back pain: estimates from the global burden of disease 2010 study. Ann Rheum Dis 2014; 73: 968–974. [DOI] [PubMed] [Google Scholar]
- 4.Hu H, Zheng Y, Wang X, et al. Correlations between lumbar neuromuscular function and pain, lumbar disability in patients with nonspecific low back pain. Medicine (Baltimore) 2017; 96: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Panjabi MM. Clinical spinal instability and low back pain. J Electromyogr Kinesiol 2003; 13: 371–379. PubMed PMID: 12832167. [DOI] [PubMed] [Google Scholar]
- 6.Coghlan S, Crowe L, McCarthypersson Uet al. et al. Neuromuscular electrical stimulation training results in enhanced activation of spinal stabilizing muscles during spinal loading and improvements in pain ratings. Conf Proc IEEE Eng Med Biol Soc 2011; 2011: 76225. [DOI] [PubMed] [Google Scholar]
- 7.Airaksinen O, Brox JI, Cedraschi C. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J 2006; 15(Suppl 2): S192–S300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Almeida M, Saragiotto B, Maher CG. Primary care management of non-specific low back pain: key messages from recent clinical guidelines. Med J Aust 2018; 209: 235–235. e1. [DOI] [PubMed] [Google Scholar]
- 9.van Middelkoop M, Rubinstein SM, Kuijpers T, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. Eur Spine J 2011; 20: 19–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Köke AJ, Schouten JS, Lamerichs-Geelen MJet al. et al. Pain reducing effect of three types of transcutaneous electrical nerve stimulation in patients with chronic pain: a randomized crossover trial. Pain 2004; 108: 36–42. [DOI] [PubMed] [Google Scholar]
- 11.Gibson W, Wand BM, Meads Cet al. et al. Transcutaneous electrical nerve stimulation (TENS) for chronic pain – an overview of cochrane reviews. Cochrane Database Syst Rev 2019; 4: CD011890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Facci LM, Nowotny JP, Tormem Fet al. et al. Effects of transcutaneous electrical nerve stimulation (TENS) and interferential currents (IFC) in patients with non-specific chronic low back pain: randomized clinical trial. Sao Paulo Med J 2011; 129: 206–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buchmuller A, Navez M, Milletre-Bernardin Met al. et al. Value of TENS for relief of chronic low back pain with or without radicular pain. Eur J Pain 2012; 16: 656–665. [DOI] [PubMed] [Google Scholar]
- 14.Wu LC, Weng PW, Chen CHet al. et al. Literature review and meta-analysis of transcutaneous nerve stimulation in treating chronic back pain. Reg Anesth Pain Med 2017; 43: 425–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chou R, Qaseem A, Snow Vet al. et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American college of physicians and the American pain society. Ann Intern Med 2007;147:478–491. PubMed PMID: 17909209. [DOI] [PubMed] [Google Scholar]
- 16.Delitto A, George SZ, Van Dillen Let al. Low back pain. J Orthop Sports Phys Ther 2012; 42: A1–57. Epub 2012 Mar 30. PubMed PMID: 22466247; PubMed Central PMCID: PMC4893951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.May S, Donelson R. Evidence-informed management of chronic low back pain with the McKenzie method. Spine J 2008; 8: 134–141. Review. PubMed PMID: 18164461. [DOI] [PubMed] [Google Scholar]
- 18.Beinart NA, Goodchild CE, Weinman JAet al. et al. Individual and intervention-related factors associated with adherence to home exercise in chronic low back pain: a systematic review. Spine J 2013; 13: 1940–1950. Epub 2013 Oct 26. Review. PubMed PMID: 24169445. [DOI] [PubMed] [Google Scholar]
- 19.Mbada CE, Olaoye MI, Dada OOet al. Comparative efficacy of clinic-based and telerehabilitation application of mckenzie therapy in chronic low-back pain. Int J Telerehabil 2019; 11: 41–58. eCollection 2019 Spring. PubMed PMID: 31341546; PubMed Central PMCID: PMC6597146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Darkins A, Kendall S, Edmonson Eet al. et al. Reduced cost and mortality using home telehealth to promote self-management of complex chronic conditions: a retrospective matched cohort study of 4,999 veteran patients. Telemed J E Health 2015; 21: 70–76. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization (WHO). Guideline: recommendations on digital interventions for health system strengthening. Geneva, Switzerland: World Health Organization, 2019. [PubMed] [Google Scholar]
- 22.van Gemert-Pijnen JE, Wynchank S, Covvey HDet al. et al. Improving the credibility of electronic health technologies. Bull World Health Organ 2012; 90: 323–323A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tabacof L, Baker TS, Durbin JRet al. et al. Telehealth Treatment for Non-Specific Low Back Pain: A Review of the Current State in Mobile Health. PM R. 2021.
- 24.Fatoye F, Gebrye T, Dada O. The clinical and cost-effectiveness of telerehabilitation for peorple with nonspecific chronic low back pain: randomized controlled trial. JMIR Mhealth UHealth 2020; 8: e15375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lewkowicz D, Slosarek T, Wernicke Set al. et al. Digital therapeutic care and decision support interventions for people with low back pain: systematic review. JMIR Rehabil Assist Technol 2021; 8: e26612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Willan AR. Analysis, sample size, and power for estimating incremental net health benefit from clinical trial data. Control Clin Trials 2001; 22: 228–237. [DOI] [PubMed] [Google Scholar]
- 27.Ostelo RW, de Vet HC. Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol 2005; 19: 593–607. [DOI] [PubMed] [Google Scholar]
- 28.Kovacs FM, Llobera J, Gil del Real MTet al. et al. Validation of the Spanish version of the Roland-Morris questionnaire. Spine (Phila Pa 1976) 2002; 27: 538–542. [DOI] [PubMed] [Google Scholar]
- 29.Ware JE. SF-36 health survey update. Spine (Phila Pa 1976) 2000; 25: 3130–3139. [DOI] [PubMed] [Google Scholar]
- 30.Alonso J, Prieto L, Antó JM. The Spanish version of the SF-36 health survey (the SF-36 health questionnaire): an instrument for measuring clinical results. Med Clin (Barc) 1995; 104: 771–776. [PubMed] [Google Scholar]
- 31.Muller U, Duetz MS, Roeder C, et al. Condition-specific outcome measures for low back pain. Part I: validation. Eur Spine J 2004; 13: 301–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Crichton N. Visual analogue scale (VAS). J Clin Nurs 2001; 10: 706–706. [Google Scholar]
- 33.Miller RP, Kori S, Todd D. The Tampa scale: a measure of Kinesiophobia. Clin J Pain 1991; 7: 51–52. [Google Scholar]
- 34.McGuill SM, Childs A, Liebenson C. Endurace times for low back stabilization exercises: clinical targets for testing and training from a normal database. Arch Phys Med Rehabil 1999; 80: 941–944. [DOI] [PubMed] [Google Scholar]
- 35.Frost M, Sutckey S, Samelley LAet al. et al. Reliability of measuring trunk motions in centimetres. Phys Ther 1982; 62: 1431–1438. [DOI] [PubMed] [Google Scholar]
- 36.Clare HA, Adams R, Maher CG. A systematic review of efficacy of McKenzie therapy for spinal pain. Aust J Physiother 2004; 50: 209–216. [DOI] [PubMed] [Google Scholar]
- 37.Busanich BM, Verscheure SD. Does McKenzie therapy improve outcomes for back pain? J Athl Train 2006; 41: 117–119. [PMC free article] [PubMed] [Google Scholar]
- 38.Garcia AN, Costa Lda C, da Silva TMet al. et al. Effectiveness of back school versus McKenzie exercises in patients with chronic nonspecific low back pain: a randomized controlled trial. Phys Ther 2013; 93: 729–747. [DOI] [PubMed] [Google Scholar]
- 39.Machado LA, Kamper SJ, Herbert RDet al. et al. Analgesic effects of treatments for non-specific low back pain: a meta-analysis of placebo-controlled randomized trials. Rheumatology (Oxford) 2009; 48: 520–527. Epub 2008 Dec 24. PMID: 19109315. [DOI] [PubMed] [Google Scholar]
- 40.Claydon LS, Chesterton LS, Barlas Pet al. et al. Dose-specific effects of transcutaneous electrical nerve stimulation (TENS) on experimental pain: a systematic review. Clin J Pain 2011; 27: 635–647. [DOI] [PubMed] [Google Scholar]
- 41.Deyo RA, Walsh NE, Martin DCet al. et al. A controlled trial of transcutaneous electrical nerve stimulation (TENS) and exercise for chronic low back pain. N Engl J Med 1990; 322: 1627–1634. [DOI] [PubMed] [Google Scholar]
- 42.Jack K, McLean SM, Moffett JKet al. et al. Barriers to treatment adherence in physiotherapy outpatient clinics: a systematic review. Man Ther 2010; 15: 220–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Saner J, Bergman EM, de Bie RAet al. et al. Low back pain patients’ perspectives on long-term adherence to home-based exercise programmes in physiotherapy. Musculoskelet Sci Pract 2018; 38: 77–82. [DOI] [PubMed] [Google Scholar]
- 44.Jordan JL, Holden MA, Mason EEet al. et al. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev 2010; 2010: CD005956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Van Dillen LR, Norton BJ, Sahrmann SAet al. Efficacy of classification-specific treatment and adherence on outcomes in people with chronic low back pain. A one-year follow-up, prospective, randomized, controlled clinical trial. Man Ther 2016; 24: 52–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lambert TE, Harvey LA, Avdalis Cet al. An app with remote support achieves better adherence to home exercise programs than paper handouts in people with musculoskeletal conditions: a randomised trial. J Physiother 2017; 63: 161–167. [DOI] [PubMed] [Google Scholar]
- 47.Ouegnin A, Valdes K. Client preferences and perceptions regarding a written home exercise program or video self-modeling: a cross-sectional study. J Hand Ther 2020; 33: 67–72. [DOI] [PubMed] [Google Scholar]
- 48.Lysack C, Dama M, Neufeld Set al. et al. A compliance and satisfaction with home exercise: a comparison of computer-assisted video instruction and routine rehabilitation practice. J Allied Health 2005; 34: 76–82. [PubMed] [Google Scholar]
- 49.Lindberg B, Nilsson C, Zotterman Det al. et al. Using information and communication technology in home care for communication between patients, family members, and healthcare professionals: a systematic review. Int J Telemed Appl 2013; 2013: 461829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Palacín-Marín F, Esteban-Moreno B, Olea Net al. et al. Agreement between telerehabilitation and face-to-face clinical outcome assessments for low back pain in primary care. Spine (Phila Pa 1976) 2013; 38: 947–952. [DOI] [PubMed] [Google Scholar]
- 51.Cottrell MA, O’Leary SP, Raymer Met al. et al. Does telerehabilitation result in inferior clinical outcomes compared with in-person care for the management of chronic musculoskeletal spinal conditions in the tertiary hospital setting? A non-randomised pilot clinical trial. J Telemed Telecare 2019: 1357633X19887265. [DOI] [PubMed] [Google Scholar]
- 52.Cottrell MA, Galea OA, O’Leary SPet al. et al. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clin Rehabil 2017; 31: 625–638. [DOI] [PubMed] [Google Scholar]