Abstract
Introduction:
Virtual consultations (VC) have been embraced by healthcare organisations during the COVID-19 pandemic. VC allows continuation of patient care while adhering to government advised restrictions and social distancing measures. Multidisciplinary pain management programmes (PMPs) are a core element of many pain services and utilising virtual methods to deliver PMPs has allowed them to continue to provide care. This systematic review aimed to explore the content of existing virtually delivered PMPs and discuss if and how these findings can be used to guide clinical delivery.
Methods:
Eligible studies included adults (aged ⩾18 years) with persistent musculoskeletal pain and any virtually delivered intervention that was described as a PMP or that had components of PMPs. Databases were searched from inception until July 2020. We performed a content analysis comparing existing interventions with established evidence-based clinical guidelines published by the British Pain Society (BPS). Intervention reporting quality was assessed using the Template for Intervention Description and Replication (TIDieR) checklist: an established checklist developed to improve the completeness of the reporting of interventions.
Results:
Eight studies were included. One intervention included six of the seven components recommended by the BPS; none included all seven. ‘Skills training and activity management’ was present in all eight interventions; ‘education’ and ‘cognitive therapy methods’ were present in six interventions; ‘graded activation’ and ‘methods to enhance acceptance, mindfulness and psychological flexibility’ were present in four interventions; ‘physical exercise’ was present in two interventions and ‘graded exposure’ was present in one intervention. None of the studies described all 12 items of the TIDieR checklist adequately enough for replication.
Conclusion:
Published virtual PMPs partially meet established clinical guidelines. Future virtual PMPs should be based on evidence-based clinical guidelines, and more research is needed to explore the effectiveness of virtually delivered PMPs and each recommended component.
Keywords: COVID-19, chronic pain, persistent pain, pain management programme, rehabilitation, virtual consultations
Introduction
The COVID-19 pandemic has led to significant disruption of services providing multidisciplinary pain management. 1 The cessation of treatment for people with persistent pain will have consequences for service users and healthcare providers as the number of people requiring pain management services and the complexity of their problems will increase. 2 Reduced access to assessment and treatment can lead to increased severity of symptoms 2 which will add to the high prevalence of persistent pain across Europe. 3 People with persistent pain are at more risk of being critically ill with COVID-19 and are more likely to be self-isolating in order to reduce their chances of being infected. 4 Research has shown that people with persistent pain suffer greater adverse effects of ‘lockdown’. 4 This may lead to self-perceived increases in pain, greater increases in anxiety and depression, increased loneliness and reduced physical activity. 4 Consequences of reduced physical activity and greater stress increase the chance of physical deconditioning 5 and risk of sarcopenia, 6 which is associated with a number of other chronic health conditions. Reduced access to multidisciplinary pain management services is likely to increase the burden on healthcare. 6
Virtual consultations (VC) have been embraced by healthcare organisations in order to continue to provide patient care while complying with government advised social distancing measures. 7 VC is one potential way to continue to provide pain services to patients during the pandemic2,5 and has been demonstrated to be accurate, cost-effective and safe,8–12 and has high satisfaction among patients due to convenience, absence of travel time and reduced time off work. 12
Pain management programmes (PMP) consist of methods to promote behaviour change and enhance well-being. 13 They aim to enable people with persistent pain to live as normal a life as possible by improving an individual’s ability to reduce and self-manage pain-associated disability and emotional distress. 13 PMPs can be effective at reducing pain interference, 14 pain intensity,15,16 disability 16 and distress. 16 The British Pain Society (BPS) has published evidence-based clinical guidelines for PMPs in adults. 13 There is currently no guidance for delivering PMPs virtually.
A recent rapid review 17 presented a number of issues to consider when using VC to deliver group-based pain rehabilitation. These include issues with inclusion, access, participation, attrition, infrastructure, clinician training and confidence, and evaluation. Systematic reviews of the literature are important summaries of existing evidence to help inform changes to practice; to our knowledge, there are no systematic reviews discussing or evaluating virtually delivered PMPs. We therefore conducted a systematic review of the literature to identify studies reporting the use of VC in PMPs. This systematic review aims to explore the content of existing virtually delivered PMPs that include real-time delivery and discuss if and how these findings can be used to guide clinical delivery of virtual PMPs.
Methods
This review has been reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. 18 This review was submitted in July 2020 and registered with the International Prospective Register of Systematic Reviews (PROSPERO: CRD42020201593) on the 25 August 2020.
Search strategy
A list of search terms combining keywords and Medical Subject Headings (MeSH) terms was developed by the authors. Search terms related to chronic/persistent pain, pain management and telemedicine and were combined using the Boolean operators. We searched four databases: CINAHL, MEDLINE, PsycINFO and AMED which were chosen due to their widespread coverage of clinical research topics. The search was completed by one author (A.W.G.) on 21 July 2020. We also searched the reference lists of similar systematic reviews for additional articles. Supplementary Material 2 presents the search strategy for each database.
Study selection and eligibility criteria
Search results were exported into Endnote 19 and duplicates were removed. Remaining titles and abstracts were imported into Microsoft Excel for screening. Next, all titles and abstracts were screened against the eligibility criteria. One author (A.W.G.) screened 100% of the titles and abstracts, one author screened 50% (G.B.) and two authors screened 25% each (D.W. and H.P.) to ensure all titles and abstracts were independently screened by two authors. To ensure consistency, the eligibility criteria were discussed between all authors prior to starting the title and abstract screening to resolve any uncertainties. Furthermore, all authors referred to the eligibility criteria throughout and further uncertainties that arose were discussed with all authors at the nearest opportunity. Of the remaining articles, two authors (G.B. and A.W.G.) reviewed full texts and agreed on the included articles. Any ambiguities in the screening process were resolved by discussion with a third author (D.W.).
Studies of interest were those that consisted of adults (aged ⩾18 years) with persistent musculoskeletal (MSK) pain; defined as pain lasting ⩾3 months, 20 that is, experienced in bones, joints, muscles, tendons and other related soft tissues. 21 There were no restrictions to the specific conditions or origins of persistent MSK pain. Studies were included if they contained participants with persistent MSK pain, even if participants with other origins of pain were also included. We included any study with an intervention that was described as a PMP, a pain rehabilitation programme, or that had components that were consistent with PMP clinical guidelines, 13 that was delivered virtually/remotely in real time (e.g. via telemedicine). This included multi-component interventions as long as part of the intervention met this criterion. There were no limitations to study design. Studies of interest were published in peer-reviewed journals and had to be in English language. Papers reporting interventions where none of the components were aimed at active self-management of pain (such as prescription of medications/advice giving on medications) were excluded.
Data extraction
Three authors (G.B., H.P. and D.W.) independently extracted the data using a data extraction table that was created based on the data sought in this study. One author (A.W.G.) reviewed all the data extraction for accuracy. Extracted data included study design, number of participants, participant characteristics (age, sex, ethnicity and conditions/pathologies), interventions characteristics (treatment approach, specific contents, providers, dose and method of delivery/technology used) and adverse events.
Quality assessment (Template for Intervention Description and Replication)
We completed a Template for Intervention Description and Replication (TIDieR) checklist 22 for each study in order to report on the quality of the reporting of interventions. One author (G.B.) completed TIDieR checklists for all studies and a second author (A.W.G.) reviewed these for accuracy.
Data synthesis
We performed a content analysis of each intervention; comparing them with the ‘specific cognitive and behavioural methods’ components of the established BPS PMP Guidelines for adults. 13 These guidelines provide evidence-based recommendations of what PMPs delivered in healthcare settings should include. The guideline’s components include ‘graded activation’, ‘cognitive therapy methods’, ‘graded exposure’, ‘methods to enhance acceptance, mindfulness and psychological flexibility’, ‘skills training and activity management’, ‘physical exercise’ and ‘education’. Reference to the definitions used in the guidelines was referred to throughout this analysis to maximise accuracy.
Results
Study selection
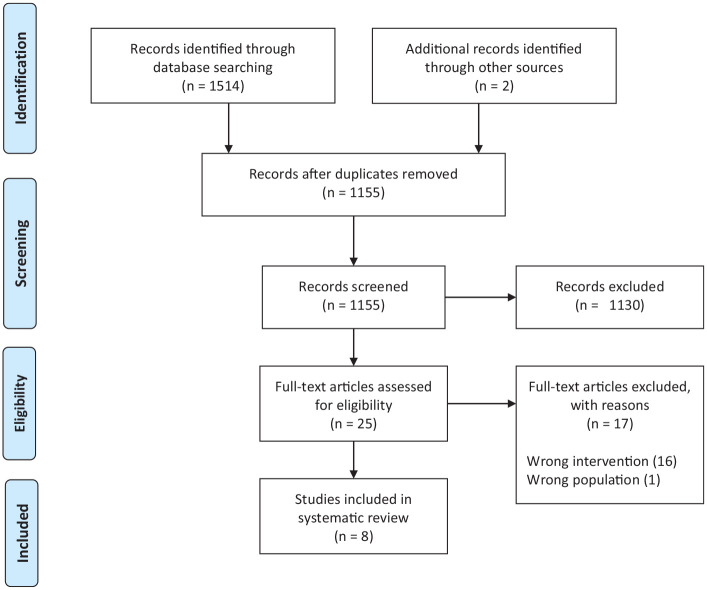
The search yielded a total of 1514 results, and 1155 unique articles were remaining after duplicates were removed. Of these, 1130 were excluded after title and abstract screening, leaving 25 articles for full-text review. After reviewing the full texts, eight were included in the systematic review.23–30 The PRISMA flow diagram is demonstrated in Figure 1.
Figure 1.
PRISMA 2009 flow diagram.
Study and participant characteristics
Of the eight included studies, one was a randomised controlled trial (RCT), 24 one was a randomised trial (no control), 23 two were non-randomised trials,25,28 one was a longitudinal case–control study, 26 one had a single-case experimental design, 27 one was a retrospective cohort analysis 29 and one was a descriptive study. 30 Participant characteristics are demonstrated in Table 1.
Table 1.
Characteristics of included studies.
| Study and design | Number of participants | Age: mean (SD) (years) | Number (%) female | Conditions/pathologies | Intervention details | Control/comparator details |
|---|---|---|---|---|---|---|
| Carmody, 2013
23
Randomised trial |
Total: 101 |
Total: 67.5 |
Total: 3 (3%) |
Not reported | Name: Telephone-delivered cognitive behavioural therapy (T-CBT) Delivery method: Telephone Individual Dose: 12 sessions over 20 weeks Schedule: Weekly – first eight sessions Fortnightly – next two sessions Monthly – final two sessions |
Type: Comparator Description: Telephone-delivered education (T-EDU) |
| Dear, 2015
24
RCT (4-arm) |
Total: 490 |
Total: 50 (13) |
Total: 375 (80%) |
Pain locations: Head/facial Neck Shoulders Upper limb Lower back Pelvic/sacrum Lower limb |
Name: The Pain Course: Internet-delivered PMP based on CBT Delivery method: Online lessons Lesson summaries Homework tasks Real-time contact: phone or email with a psychologist No tailoring Dose: Five online lessons Five lesson summaries Real time: Regular contact = 10–15 minutes weekly Optional contact = 10–15 minutes sessions Schedule: 1 week between lessons 1 and 2, and 3 and 4 2 weeks between lessons 2 and 3, and 4 and 5 |
Type: Control Description: Waiting list |
| Gardner-Nix, 2012
25
Non-randomised trial |
Total: 119 |
Total: 52 (range = 32–79) |
Total: 90 (76%) |
Back pain Fibromyalgia Facial pain Arthritis Neck pain Shoulder pain Lupus Chest pain Migraine Multiple sclerosis Neuropathy Crohn’s disease Leg pain |
Name: Mindfulness-based chronic pain management programme (MBCPM) – modified MBSR (stress reduction) Delivery method: Videoconferencing and face-to-face combination simultaneously Class-sizes of 12–22 (combined on-site and off-site) Dose: 12 sessions in 12 weeks Schedule: Weekly |
Type: Control Description: Waiting list |
| Helstrom, 2018
26
Longitudinal case–control study |
Total: 160 |
Total (all eligible participants): 76.7 (7.1) |
Total (all eligible participants): 198 (79.2%) |
High symptom chronic pain (pain interference 8+) | Name: Pain Care Management (PCM) Delivery method: Telephone Individual Tailored Dose: 20 minutes sessions Five treatment sessions in 3 months Three maintenance calls Schedule: Treatment: weeks 2, 4, 6, 9 and 12 Maintenance: weeks 16, 20 and 24 |
Type: Control Description: Symptom monitoring |
| Lafontaine, 2018
27
Single-case experimental design |
Total: 2 |
Total: 63 |
Total: 2 (100%) |
Fibromyalgia Peripheral neuropathy |
Name: CBT for chronic pain Delivery method: Videoconference Individual by a psychologist or doctoral student in psychology Tailored Dose: 10–13 1-hour sessions Schedule: Weekly |
N/A |
| Mariano, 2019
28
Non-randomised trial |
Total: 93 |
Total: 57.1 |
Total: 61 (65.6%) |
Chronic low back pain (CLBP) | Name: Group CBT teletherapy for chronic pain Delivery method: Online group CBT Individual follow-up calls Eight per group Not tailored Dose: Eight sessions Schedule: Weekly |
Type: Control Description: In person group PMP |
| Mochari-Greenberger, 2017
29
Retrospective cohort analysis |
Total: 170 |
Total: 53.3 (8.9) |
Total: 130 (76%) |
MSK pain Fibromyalgia Nerve pain Headache |
Name: AbleTo – technology-enabled telebehavioural therapy programme for chronic pain – CBT/ACT based Delivery method: Telephone or videoconference Provider: behavioural health provider and behaviour coach Individual Tailored Dose: 45 minutes sessions 15 sessions 8 weeks Schedule: Not reported |
N/A |
| Palyo, 2012
30
Descriptive study (qualitative) |
Not reported | Not reported | Not reported | Veterans with chronic pain | Name: Cognitive behavioural and physical therapy group intervention Delivery method: Videoconferencing Group-based Providers: psychologist and physical therapist Dose: 2-hour sessions 10 weeks Schedule: Not reported |
N/A |
MBSR: mindfulness-based stress reduction; ACT: acceptance and commitment therapy; SD: standard deviation; PMP: pain management programme.
Intervention characteristics
Table 1 presents intervention delivery methods, dose and schedule. All seven of the specific cognitive and behavioural methods of the BPS PMP guidelines 13 were present across the studies. The highest number of guideline contents in one study was six 24 (Table 2).
Table 2.
Studies and items of the British Pain Society PMP guidelines.
| BPS PMP content guidelines | Graded activation | Cognitive therapy methods | Graded exposure | Methods to enhance acceptance, mindfulness and psychological flexibility | Skills training and activity management (e.g. relaxation, pacing and sleep) | Physical exercise | Education (e.g. pain mechanisms/physiology, and pros and cons of medication) |
|---|---|---|---|---|---|---|---|
| Study (first author, year) | |||||||
| Carmody, 2013 | ✓ | ✓ | |||||
| Dear, 2015 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Gardner-Nix, 2014 | ✓ | ✓ | ✓ | ✓ | |||
| Helstrom, 2017 | ✓ | ✓ | ✓ | ||||
| Lafontaine, 2018 | ✓ | ✓ | ✓ | ||||
| Mariano, 2019 | ✓ | ✓ | ✓ | ✓ | |||
| Mochari-Greenberger, 2017 | ✓ | ✓ | ✓ | ✓ | |||
| Palyo, 2012 | ✓ | ✓ | ✓ | ✓ | ✓ |
BPS: British Pain Society; PMP: pain management programme.
✓ = guideline item present in intervention.
Graded activation guided by participant goals
Graded activation guided by participant goals was present in four interventions.24,26,29,30 Goal setting was used in all four of these studies and coincided with physical activity24,26,30 and self-care. 29 ‘Relapse prevention’, a strategy aimed at facilitating maintenance of change, was present in two of these studies.24,30
Cognitive therapy methods
Cognitive therapy methods were present in six studies.23,24,27–30 They were often described as teaching ways of managing or challenging negative thoughts.23,24,28,29 Others simply stated they were using ‘cognitive restructuring’ methods27,30 without further elaboration of the detail of this.
Graded exposure
Graded exposure was described in one intervention. 24 It was described as consisting of an explanation on the issues of fear and avoidance of physical activities, and instructions on gradually and safely increasing physical activities.
Methods to enhance acceptance, mindfulness and psychological flexibility
Four studies described methods of enhancing acceptance, mindfulness and psychological flexibility.24,25,28,29 Two of these studies stated using mindfulness techniques28,29; one described monitoring negative thoughts 24 and one described exploring behaviours and responses to disability. 25 There were no further explanations of these techniques.
Skills training and activity management
All eight studies included elements of skills training and activity management. Five studies included teaching of relaxation techniques24,26–28,30 to alter the adverse effects of thoughts and feelings. Another study stated teaching methods of managing negative emotions, without including specific details. 23 Six studies taught goal setting.24,26–30 Five studies taught activity management or pacing techniques24,26–28,30 to balance time spent on meaningful activity or rest. Four interventions included skills for communication and social interaction,23,27,28,30 with two studies specifically stating teaching assertiveness skills.23,30 Three studies were taught sleep management skills.25,27,28 One study was introduced to self-monitoring techniques. 26 In addition to the two mentioned above, two other studies reported teaching ‘relapse prevention’ skills.27,28 These studies did not elaborate further on specifics of this skill.
Physical exercise
Two studies included physical exercise components.25,30 One of these included stretching, strengthening and aerobic exercise 30 and the other included training in exercise. 25
Education
Six studies included education.24–28,30 Three of these studies included pain education.24,26,27 The other studies included education on nutrition, 25 weight management 28 and posture. 30
Control and comparator group characteristics
Three studies had control groups; two of these studies24,25 had waitlist controls and the other study compared online group cognitive behavioural therapy (CBT) with in-person group CBT as the control. 28 One study monitored symptoms and side effects of control participants. 26 Another study had telephone delivered pain education as their comparator to telephone delivered CBT. 23 Three studies did not have control or comparator groups due to their study design.27,29,30
Intervention reporting quality (TIDieR)
TIDieR checklist items one (brief name), two (rationale, theory or goal), three (materials), four (procedures), six (modes of delivery) and seven (locations) were adequately described in all eight intervention descriptions. Two intervention descriptions did not include sufficient information on who provided the intervention (item five).23,28 One study did not adequately describe the dose or intensity (item eight) 23 that the intervention was delivered at. Three studies did not provide information on whether the intervention was designed to be tailored or not, and under what circumstances (item nine).27,28,30 Seven studies did not mention details of any modifications (item 10) that may have happened during the study.23–26,28–30 Five studies did not report any plans to measure adherence or fidelity (item 11)24–26,28,30 and five studies did not report any actual details of adherence or fidelity (item 12).25,26,28–30
One study adequately described seven of the TIDieR items, 28 one study adequately described eight of the items, 30 three studies adequately described nine items,23,25,26 two adequately described ten items24,29 and one adequately described eleven items. 27 No studies described all 12 items adequately enough for replication (Table 3).
Table 3.
Studies and items of the TIDieR checklist.
| Study (first author, year) | Carmody, 2013 | Dear, 2015 | Gardner-Nix, 2014 | Helstrom, 2017 | Lafontaine, 2018 | Mariano, 2019 | Mochari-Greenberger, 2017 | Palyo, 2012 |
|---|---|---|---|---|---|---|---|---|
| TIDieR checklist item | ||||||||
| 1. Brief name | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 2. Why (rationale, theory, goal) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 3. Materials used in intervention (physical or informational) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 4. Procedures (activities, processes) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 5. Intervention providers | X | ✓ | ✓ | ✓ | ✓ | X | ✓ | ✓ |
| 6. Modes of delivery (e.g. face-to-face, virtual, individual or group) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 7. Location of intervention | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 8. When and how much (number of sessions, time period, schedule and dose) | X | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 9. Details of tailoring | ✓ | ✓ | ✓ | ✓ | X | X | ✓ | X |
| 10. Modifications to intervention | X | X | X | X | ✓ | X | X | X |
| 11. Planned adherence and fidelity assessment | ✓ | X | X | X | ✓ | X | X | |
| 12. Actual adherence and fidelity | ✓ | ✓ | X | X | ✓ | X | X | X |
TIDieR: Template for Intervention Description and Replication checklist.
✓ indicates item adequately reported.
X indicates item inadequately or not reported.
Adverse events
No studies formally reported any adverse events.
Discussion
To our knowledge, this is the first systematic review to assess the content of virtually delivered PMPs, or interventions including components of PMPs, in accordance with evidence-based clinical guidelines. 13 We found that all eight of the included interventions had elements of ‘skills training and activity management’. ‘Cognitive therapy methods’ and ‘education’ were each present in six studies. ‘Graded activation guided by participant goals’ and ‘methods to enhance acceptance, mindfulness and psychological flexibility’ were each present in four studies. ‘Physical exercise’ was present in two studies and ‘graded exposure’ was only present in one study. None of the included studies included all the components recommended by the BPS guidelines. 13 None of the studies adequately described all 12 TIDieR items: with details of modifications, fidelity and adherence being the items most commonly lacking. Name, rationale, theory or goal, materials, procedures, modes of delivery and location were adequately reported in all eight studies. No studies formally reported any adverse events.
None of the studies reported using clinical guidelines in their intervention design. ‘Cognitive therapy methods’ was one of the most common guideline items present across the interventions. CBT is effective (albeit effects are small or very small) at reducing pain and disability, 16 and at improving multiple psychosocial issues associated with persistent pain.16,31,32 The effectiveness of CBT delivered by videoconference for posttraumatic stress disorder is comparable with face-to-face delivery. 33 Psychotherapy methods delivered by videoconference, including CBT, can be effective for depressive symptoms 34 and may be for anxiety; 35 highly prevalent problems for people with persistent MSK pain conditions.36,37 This suggests that CBT methods delivered by videoconference may be effective for people with persistent MSK pain and should be included in virtually delivered PMPs.
Patients with persistent non-cancer pain expect explanations or improved understanding of the their pain problem. 38 Pain neuroscience education can facilitate a patient’s ability to cope with their pain, reduce kinesiophobia and decrease catastrophising. 39 The evidence for patient education delivered via real-time virtual methods is lacking but may be feasible 40 and should be considered for inclusion in virtual PMPs.
Half of the interventions included ‘methods to enhance acceptance, mindfulness and psychological flexibility’. Acceptance and mindfulness-based interventions can be effective at reducing pain and psychological problems and can improve physical and mental health-related quality of life in people with persistent pain.41,42 Studies of stand-alone virtually delivered acceptance and/or mindfulness interventions are lacking in healthcare research; this lack of supporting evidence may be a reason these treatments were not utilised across all studies.
Physical exercise was reported in two studies. Exercise alone delivered via telemedicine has been shown to be better than no intervention. 43 A combination of exercise and pain coping skills training delivered by videoconference is effective for pain and function long-term in people with chronic knee pain. 44 Exercise should be included in virtual PMP’s. All eight studies included ‘skills training’ which could be incorporated with exercise.
‘Graded exposure’ was present in only one study; this was taught during one online lesson and not practised with the participants. 24 Reasons for limited inclusion in interventions are unknown, and to our knowledge, there are no studies investigating graded exposure performed via virtual methods for any condition. Considering greater degrees of kinesiophobia are associated with higher pain levels and disability, and lower quality of life 45 and the fact that graded exposure can reduce pain-related kinesiophobia, 46 studies of virtually delivered graded exposure are required to be able to evaluate their effectiveness when working remotely with patients.
Strengths and limitations
These results must be considered in light of the study limitations. There were multiple study designs included and only two of these were randomised trials. We were therefore unable to perform formal quality assessments of the included studies due to variation in the study types as we would be unable make useful comparisons.
This systematic review was prospectively registered on the PROSPERO database, it has been reported in line with PRISMA guidelines 18 and multiple authors were involved at each stage of the review process. We compared existing interventions with established evidence-based clinical guidelines 13 and we assessed intervention reporting quality with well-known guidance, 22 strengthening our analysis. The included studies represented a broad range of chronic pain conditions, with a large number of these MSK in origin and location, although only one study solely focused on MSK pain. 28
Implications for research and clinical practice
There is a current lack of high-quality research into real-time virtually delivered PMPs. There is also limited research into real-time virtual delivery of any of the recommended components of these programmes. Future research should address these gaps in order to improve confidence in either programme or individual component effectiveness, which can subsequently be used to guide evidence-based clinical practice. Future research should focus on delivering PMPs that are in-line with established evidence-based clinical guidelines such as the BPS PMP guidelines. 13 Interventions need to be well reported to enable replication in clinical practice; the use of checklists and tools such as the TIDieR checklist 13 can aid this. Studies should also report any adverse effects of virtual PMPs as these are currently unknown, and patient safety remains of high importance. No specific guidance on clinical delivery can be made from this study. Despite the limited evidence for real-time virtual delivery of PMPs, clinical guidelines such as the BPS PMP guidelines 13 should still be used as a framework when designing virtually delivered programmes, with requirements and resources being tailored to individual context.
Conclusion
The COVID-19 pandemic has interrupted the care of people requiring multidisciplinary pain management for musculoskeletal pain. Virtually delivered PMPs have been cited as a means to continue the delivery of care for people with persistent pain. We have successfully conducted a systematic literature review of studies reporting virtually delivered PMPs. We found that few studies considered best practice guidelines, such as those offered by the BPS during the design of their programmes. Clinical interventions should be based on evidence-based clinical guidelines and future research should explore the effectiveness and acceptability of each component when delivered remotely.
Supplemental Material
Supplemental material, sj-docx-1-bjp-10.1177_20494637211023074 for What is the content of virtually delivered pain management programmes for people with persistent musculoskeletal pain? A systematic review by Gregory Booth, Deborah Williams, Hasina Patel and Anthony W Gilbert in British Journal of Pain
Supplemental material, sj-docx-2-bjp-10.1177_20494637211023074 for What is the content of virtually delivered pain management programmes for people with persistent musculoskeletal pain? A systematic review by Gregory Booth, Deborah Williams, Hasina Patel and Anthony W Gilbert in British Journal of Pain
Footnotes
Conflict of interest: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Contributorship: G.B. and A.W.G. conceptualised and designed the study. G.B. and A.W.G. developed the search strategy. A.W.G. completed the search. G.B., D.W., H.P. and A.W.G. contributed to the screening process and data extraction. G.B. conducted the content analysis. All authors contributed to interpretation of results. G.B. drafted the manuscript. D.W., H.P. and A.W.G. critically revised the manuscript. All authors approved the final version for publication.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This study was unfunded. G.B. completed this work during an ICA Pre-doctoral Clinical Academic Fellowship supported by Health Education England and the National Institute for Health Research (grant number: NIHR300342). A.W.G., Clinical Doctoral Research Fellow (ICA-CDRF-2017-03-025) is funded by Health Education England and support by the National Institute for Health Research (NIHR). The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health and Social Care.
Guarantor: G.B. is the guarantor of this study.
ORCID iDs: Gregory Booth  https://orcid.org/0000-0003-3332-1890
https://orcid.org/0000-0003-3332-1890
Deborah Williams  https://orcid.org/0000-0003-2935-0621
https://orcid.org/0000-0003-2935-0621
Supplemental material: Supplemental material for this article is available online.
References
- 1.Faculty of Pain Medicine British Pain Society. An update from the FPM and BPS to those waiting to access pain services, 2020, https://www.britishpainsociety.org/mediacentre/news/an-update-from-the-fpm-and-bps-to-those-waiting-to-access-pain-services/
- 2.Eccleston C, Blyth FM, Dear BF, et al. Managing patients with chronic pain during the COVID-19 outbreak: considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain 2020; 161(5): 889–893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Todd A, McNamara CL, Balaj M, et al. The European epidemic: pain prevalence and socioeconomic inequalities in pain across 19 European countries. Eur J Pain 2019; 23(8): 1425–1436. [DOI] [PubMed] [Google Scholar]
- 4.Fallon N, Brown C, Twiddy H, et al. Adverse effects of COVID-19-related lockdown on pain, physical activity and psychological well-being in people with chronic pain. Brit J Pain. Epub ahead of print 21 November 2020. DOI: 10.1177/2049463720973703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.El-Tallawy SN, Nalamasu R, Pergolizzi JV, et al. Pain management during the COVID-19 Pandemic. Pain and Therapy 2020; 9: 453–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kirwan R, McCullough D, Butler T, et al. Sarcopenia during COVID-19 lockdown restrictions: long-term health effects of short-term muscle loss. Geroscience 2020; 42: 1547–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gilbert AW, Billany JCT, Adam R, et al. Rapid implementation of virtual clinics due to COVID-19: report and early evaluation of a quality improvement initiative. BMJ Open Qual 2020; 9(2): e000985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cottrell MA, Galea OA, O’Leary SP, et al. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clinical Rehabilitation 2016; 31: 625–638. [DOI] [PubMed] [Google Scholar]
- 9.Cottrell MA, O’Leary SP, Swete-Kelly P, et al. Agreement between telehealth and in-person assessment of patients with chronic musculoskeletal conditions presenting to an advanced-practice physiotherapy screening clinic. Musculoskelet Sci Pract 2018; 38: 99–105. [DOI] [PubMed] [Google Scholar]
- 10.O’Brien KM, Hodder RK, Wiggers J, et al. Effectiveness of telephone-based interventions for managing osteoarthritis and spinal pain: a systematic review and meta-analysis. PeerJ 2018; 6: e5846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bradley KE, Cook C, Reinke EK, et al. Comparison of the accuracy of telehealth examination versus clinical examination in the detection of shoulder pathology. J Shoulder Elbow Surg 2020; 30: 1042–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haider Z, Aweid B, Subramanian P, et al. Telemedicine in orthopaedics and its potential applications during COVID-19 and beyond: a systematic review. J Telemed Telecare. Epub ahead of print 6 August 2020. DOI: 10.1177/1357633X20938241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.British Pain Society. Guidelines for pain management programmes for adults: an evidence-based review prepared on behalf of the British Pain Society. London: British Pain Society, 2013. [Google Scholar]
- 14.Hoffman BM, Papas RK, Chatkoff DK, et al. Meta-analysis of psychological interventions for chronic low back pain. Health Psychol 2007; 26: 1–9. [DOI] [PubMed] [Google Scholar]
- 15.van Tulder MW, Ostelo R, Vlaeyen JWS, et al. Behavioral treatment for chronic low back pain: a systematic review within the framework of the Cochrane back review group. Spine 2000; 25: 2688–2699. [DOI] [PubMed] [Google Scholar]
- 16.Williams ACC, Fisher E, Hearn L, et al. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev 2020; 8: CD007407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walumbe J, Belton J, Denneny D. Pain management programmes via video conferencing: a rapid review. Scand J Pain 2020; 21: 32–40. [DOI] [PubMed] [Google Scholar]
- 18.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 2009; 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Team TE. EndNote X9 ed. Philadelphia, PA: Clarivate, 2013. [Google Scholar]
- 20.Treede R-D, Rief W, Barke A, et al. A classification of chronic pain for ICD-11. Pain 2015; 156: 1003–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Perrot S, Cohen M, Barke A, et al. The IASP classification of chronic pain for ICD-11: chronic secondary musculoskeletal pain. Pain 2019; 160(1): 77–82. [DOI] [PubMed] [Google Scholar]
- 22.Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. Brit Med J 2014; 348: g1687. [DOI] [PubMed] [Google Scholar]
- 23.Carmody TP, Duncan CL, Huggins J, et al. Telephone-delivered cognitive-behavioral therapy for pain management among older military veterans: a randomized trial. Psychol Serv 2013; 10(3): 265–275. [DOI] [PubMed] [Google Scholar]
- 24.Dear BF, Gandy M, Karin E, et al. The Pain Course: a randomised controlled trial examining an internet-delivered pain management program when provided with different levels of clinician support. Pain 2015; 156(10): 1920–1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gardner-Nix J, Barbati J, Grummitt J, et al. Exploring the effectiveness of a mindfulness-based chronic pain management course delivered simultaneously to on-site and off-site patients using telemedicine. Mindfulness 2014; 5: 223–231. [Google Scholar]
- 26.Helstrom A, Haratz J, Chen S, et al. Telephone-based management of chronic pain in older adults in an integrated care program. Int J Geriatr Psychiatry 2018; 33(5): 779–785. [DOI] [PubMed] [Google Scholar]
- 27.Lafontaine M-F, Azzi S, Paquette D, et al. Telehealth for patients with chronic pain: exploring a successful and an unsuccessful outcome. J Tech Human Serv 2018; 36: 140–160. [Google Scholar]
- 28.Mariano TY, Wan L, Edwards RR, et al. Online group pain management for chronic pain: preliminary results of a novel treatment approach to teletherapy. J Telemed Telecare 2021; 27: 209–216. [DOI] [PubMed] [Google Scholar]
- 29.Mochari-Greenberger H, Peters A, Vue L, et al. A nationally scaled telebehavioral health program for chronic pain: characteristics, goals, and psychological outcomes. Telemed J E Health 2017; 23(8): 640–648. [DOI] [PubMed] [Google Scholar]
- 30.Palyo SA, Schopmeyer KA, McQuaid JR. Tele-pain management: use of videoconferencing technology in the delivery of an integrated cognitive-behavioral and physical therapy group intervention. Psychol Serv 2012; 9(2): 200–202. [DOI] [PubMed] [Google Scholar]
- 31.Morley S, Eccleston C, Williams A. Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain 1999; 80(1–2): 1–13. [DOI] [PubMed] [Google Scholar]
- 32.Richmond H, Hall AM, Copsey B, et al. The effectiveness of cognitive behavioural treatment for non-specific low back pain: a systematic review and meta-analysis. PLoS ONE 2015; 10(8): e0134192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Germain V, Marchand A, Bouchard S, et al. Effectiveness of cognitive behavioural therapy administered by videoconference for posttraumatic stress disorder. Cogn Behav Ther 2009; 38(1): 42–53. [DOI] [PubMed] [Google Scholar]
- 34.Berryhill MB, Culmer N, Williams N, et al. Videoconferencing psychotherapy and depression: a systematic review. Telemed J E Health 2019; 25(6): 435–446. [DOI] [PubMed] [Google Scholar]
- 35.Berryhill MB, Halli-Tierney A, Culmer N, et al. Videoconferencing psychological therapy and anxiety: a systematic review. Family Pract 2018; 36: 53–63. [DOI] [PubMed] [Google Scholar]
- 36.Stubbs B, Aluko Y, Myint PK, et al. Prevalence of depressive symptoms and anxiety in osteoarthritis: a systematic review and meta-analysis. Age Ageing 2016; 45(2): 228–235. [DOI] [PubMed] [Google Scholar]
- 37.Schmaling KB, Nounou ZA. Incident chronic spinal pain and depressive disorders: data from the national comorbidity survey. J Pain 2019; 20(4): 481–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Geurts JW, Willems PC, Lockwood C, et al. Patient expectations for management of chronic non-cancer pain: a systematic review. Health Expect 2017; 20(6): 1201–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Watson JA, Ryan CG, Cooper L, et al. Pain neuroscience education for adults with chronic musculoskeletal pain: a mixed-methods systematic review and meta-analysis. J Pain 2019; 20(10): 1140.e1–1140.e22. [DOI] [PubMed] [Google Scholar]
- 40.Warmington K, Flewelling C, Kennedy CA, et al. Telemedicine delivery of patient education in remote Ontario communities: feasibility of an Advanced Clinician Practitioner in Arthritis Care (ACPAC)-led inflammatory arthritis education program. Open Access Rheumatol 2017; 9: 11–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hilton L, Hempel S, Ewing BA, et al. Mindfulness meditation for chronic pain: systematic review and meta-analysis. Ann Behav Med 2016; 51: 199–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Veehof MM, Trompetter HR, Bohlmeijer ET, et al. Acceptance- and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cogn Behav Ther 2016; 45(1): 5–31. [DOI] [PubMed] [Google Scholar]
- 43.Adamse C, Dekker-Van Weering MG, van Etten-Jamaludin FS, et al. The effectiveness of exercise-based telemedicine on pain, physical activity and quality of life in the treatment of chronic pain: a systematic review. J Telemed Telecare 2018; 24(8): 511–526. [DOI] [PubMed] [Google Scholar]
- 44.Bennell KL, Nelligan R, Dobson F, et al. Effectiveness of an internet-delivered exercise and pain-coping skills training intervention for persons with chronic knee pain. Ann Intern Med 2017; 166: 453–462. [DOI] [PubMed] [Google Scholar]
- 45.Luque-Suarez A, Martinez-Calderon J, Falla D. Role of kinesiophobia on pain, disability and quality of life in people suffering from chronic musculoskeletal pain: a systematic review. Br J Sports Med 2019; 53(9): 554–559. [DOI] [PubMed] [Google Scholar]
- 46.Vlaeyen JWS, de Jong J, Geilen M, et al. Graded exposure in vivo in the treatment of pain-related fear: a replicated single-case experimental design in four patients with chronic low back pain. Behav Res Ther 2001; 39(2): 151–166. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-bjp-10.1177_20494637211023074 for What is the content of virtually delivered pain management programmes for people with persistent musculoskeletal pain? A systematic review by Gregory Booth, Deborah Williams, Hasina Patel and Anthony W Gilbert in British Journal of Pain
Supplemental material, sj-docx-2-bjp-10.1177_20494637211023074 for What is the content of virtually delivered pain management programmes for people with persistent musculoskeletal pain? A systematic review by Gregory Booth, Deborah Williams, Hasina Patel and Anthony W Gilbert in British Journal of Pain