Abstract
Introduction
An advancing healthcare system in which patients are often required to self-manage care needs across countless settings and clinicians is increasing focus on participation in care. Mismanagement of care during already risky care-transitions further increases adverse care outcomes. Understanding factors of patient participation in transitional care in an adult population can help guide ways to reduce this burden.
Methods
A systematic review of the literature guided by the PRISMA method was conducted to identify factors of patient participation in transitional care. Quantitative studies in which patient participation was measured as an outcome variable and related statistics reported, and data were collected from an adult sample, were included. Two authors independently reviewed, critiqued, and synthesized the articles, and later categorized study variables according to identified trends.
Results
Twelve studies across international and multidisciplinary backgrounds were identified. Across studies, efforts were largely based on understanding or improving patient self-management of care during transitions. The majority of studies were experimental and care interventions grounded in patient and healthcare team partnerships, delivered beyond the hospital setting. An array of measures was used to quantify patient participation. Factors of patient participation in transitional care included higher perceived levels of self-efficacy, confidence, and skills to participate in care.
Conclusion
The results of this study suggest patient participation in transitional care is largely based on perceptions of self-efficacy, confidence, and skill. Patient-centric transitional care interventions targeting these factors and delivered beyond the hospital setting may improve care outcomes. Implications and direction for further studies includes conceptual clarity, the study of a broader-reaching patient population demographic, and use of multidisciplinary interventions. Outcome variables should remain focused on patient perception of care involvement and participation and expanded to include variables such as functional abilities and social determinants of health.
Keywords: patient participation, transitional care, self-management
Introduction
Patient participation in care, a concept long been supported by The World Health Organization (WHO), refers to individuals’ involvement in the planning, organizing, and controlling of healthcare. Globally, health systems continue to deliver biopsychosocial care models rooted around patient participation in healthcare (Halabi et al., 2020). The WHO suggests healthcare should center on individual self-reliance and advises greater promotion of health literacy, individual empowerment, and participation. On a national level, government guidelines not only describe person-centeredness as a prerequisite for care but mandate it a core component of care delivery (Institute of Medicine Committee on Health Care in America, 2001). An extensive body of literature has developed describing relationships between patients and healthcare systems, including concepts such as patient participation, patient empowerment, and patient activation. However, the focus of this paper is patient participation and is defined as the patient's participation in decision-making and activities aimed at, or regarding care, through processes involving the sharing of information and the transfer of power, from the healthcare team member, to the patient (Dyrstad et al., 2015).
Numerous factors have prompted prioritizing patient participation in care. A fast-growing elderly population with numerous chronic conditions, physical disabilities, cognitive impairments, and polypharmacy have led to a need for clinical care and increased utilization across primary and secondary healthcare settings (Foss & Askautrud, 2010). Multimorbidity resulting in frequent care-transitions pose both costly and morbid outcomes (Mark et al., 2013). Patients are the only common thread weaving across the health care continuum and care management across healthcare settings becomes their responsibility. This burden is exacerbated during acute hospitalizations as shortened lengths of stay requires passive prescription of transition planning, rather than actively partnered planning to anticipate needs (Connolly et al., 2009). Consequently, numerous evidence-based care-transition programs have developed (Coleman et al., 2006; Naylor et al., 2017) and patient participation in transitional care is now recognized as a key driver of effective care management.
Although patient participation concepts are rooted in transitional care programs and highlighted in healthcare policy documents, knowledge about patient factors related to participation in care during transitions are incomplete and largely limited to the elderly population (Dyrstad et al., 2015). A comprehensive literature review of studies examining this phenomenon revealed participation in hospital discharge planning and decision-making was low, despite the use of numerous tools to increase participation and notwithstanding patients’ desire to share in the planning and managing of care. The authors recommended improvement in the quality of patient participation efforts in transitional care, though urged greater subject knowledge in the area is first required (Dyrstad et al., 2015). Knowledge gleaned from understanding factors of patient participation in transitional care may help guide quality improvement efforts and intervention development. Furthermore, requiring care from numerous professionals across various settings is not constrained to the elderly and research should not be limited to this population. Currently, there is a gap in knowledge regarding patient participation in an adult population (age 18 and older) that are not elderly. Thus, the objective of this paper is to present a systematic review of quantitative studies examining factors of adult patient participation in transitional care.
Methods
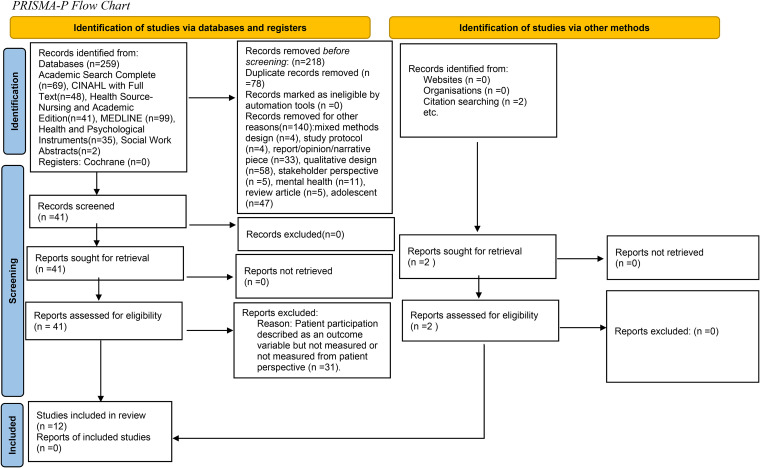
The PRISMA-P method (Page et al., 2021) guided this systematic review of quantitative studies (See Figure 1). A comprehensive review of the literature was conducted using EBSCOHost with the following databases selected: Academic Search Complete, CINAHL with Full Text, Health Source-Nursing and Academic Edition, MEDLINE, Health and Psychological Instruments, and Social Work Abstracts. A search using the terms “transitional care” AND “patient participation” was performed. Additional terms denoting the movement of patients and/or their care across the care continuum and participation in such care included: “transition of care”, “care-transition”, “discharge planning” and “patient involvement”, “patient empowerment” and “patient engagement”. Limits were set to include peer-reviewed studies of adults written in the English language and time was not limited. The examination of the retrieved articles was also competed. The initial search yielded 259 articles. Duplicates and articles that did not meet the following inclusion criteria were removed: primary quantitative study design; data collected from an adult sample; patient participation identified as an outcome variable and measured from the patient perspective; and reported related statistics. Review articles, mixed methods design studies, and studies examining patient participation in the context of psychiatric illness were excluded as this population experiences unique challenges requiring specialized treatment and services (Solomon et al., 2014). Two authors systematically critiqued each of the 12 studies using a reputable matrix (Melnyk & Fineout-Overholt, 2011). This data was used to evaluate the quality of each article and to determine themes across studies. Upon discussion, the following themes were identified: transitional care time period/foci and target timeframe, disciplinary perspective, conceptual basis of patient participation or involvement in care planning, and type of intervention and classification of outcome variable.
Figure 1.
PRISMA-P flow chart.
Any conflict that arose in the review was resolved by a third author. Reporting of the reliability and validity of measures was limited and therefore not outlined in the table. The literature search was completed July 13, 2021. This review was not registered.
Results
Twelve quantitative studies on patient participation in transitional care were analyzed for this review. Studies ranged in geographic location, timeframe, population, design, and timing (see Table 1 for details). Studies also ranged in disciplinary perspective. Six of the studies were conducted by nursing (Bull et al., 2000; Chen et al., 2018; Jangland et al., 2012; Lenaghan, 2019; Schmaderer et al., 2016; Ulin et al., 2016), followed by four by medicine (Coleman et al., 2004; Epstein-Lubow et al., 2014; Kvale et al., 2016; Noel et al., 2020) and the remaining two were implemented by occupational and physical therapy (Arnetz et al., 2010; Smith & Fields, 2020).
Table 1.
Literature Matrix.
| Author(s)/year/location | Design | Sample | Variables/concept(s) | Timing | Findings |
|---|---|---|---|---|---|
| Bull, et al. (2000), United States | Quasi-experimental-before- and-after nonequivalent control group design | N = 158 patient caregiver dyads. | CO, QO, HCU; professional-patient partnership model and patient participation. | PD | IV group felt better prepared to manage, greater continuity of information, and better health. Less days when readmitted. Caregivers received more information and greater perception of caregiving. |
| Coleman et al. (2004), United States | Quasi-experimental | N = 1,393 older adults | CO, QO, HCU; Individualized goal-setting and empowerment. | IH | No difference in HCU, IV versus CG. 75% IV reported confidence in self-management, ability to identify worsening condition, 87% understand reason for medications. |
| Arnetz et al. (2010), United States | Cross-sectional, descriptive correlational | N = 449 Myocardial Infarction (MI) patients | CO, QO, HCU; Self-efficacy. | PD | IV group reported more positive ratings of involvement and significantly associated with fewer cardiovascular symptoms 6-10 weeks. HCU (completed rehabilitation) and smoking cessation significantly less satisfied with involvement. No association between involvement and medication compliance. |
| Jangland et al. (2011), Sweden | Prospective comparative with ABA design | N = 310 surgery patients | QO, HCU; patient participation. | PD | Patients that declined to participate were significantly more likely to be admitted from the emergency department (p < .0001). Patients perceived opportunity to participate in their nursing care (p = .020) and decisions about their medical care (p = .004). Nonsignificant findings in regard to shared self-care information. |
| Epstein-Lubow, et al. (2014), United States | Descriptive correlational | N = 482 adults and caregivers | QO; Patient empowerment. | PD | Patients with family caregivers five-times more likely to complete CTI (95% CI = 4.22-7.12). Men with family caregivers were 8 times more likely to complete CTI (95%CI = 5.26-11.98). |
| Kvale et al. (2016), United States | Randomized, controlled trial | N = 79 | CO; Patient empowerment, Wagner's Chronic Care Model. | A | IV significantly higher self-reported health (p = .017), lower social role limitations (p = .014) and a trend toward greater self-efficacy (p = .07). No between group differences found in PAM score. |
| Schmaderer et al. (2016), Nebraska-United States | Cross-sectional, descriptive correlational | N = 200 adults | CO, QO, HCU; Patient Activation Model. | PD | Higher activation correlated with psychosocial factors (health literacy (p = .013), greater satisfaction with social role (p = .014) and involvement in chronic illness (p = .001). Activation also associated with higher HCU post-discharge, lower educational level, income level, less sleep and increased pain, and decreased physical functioning. |
| Ulin et al. (2016), Sweden | Controlled before and after quasi-experimental design. | N = 248 adults | CO, HCU; Person-centered, partnered planning. | PD | IV slightly non-significant higher level of dependency in ADLs. IV significantly fewer days in the hospital ready for discharge (6.77 days versus 9.22 days, p < .001) and home health notification more frequent. |
| Chen, et al. (2018), China | Two-arm single blinded randomized controlled longitudinal | N = 144 stroke survivors | CO, QO, HCU; Health Empowerment Theory. | IH | Rehospitalizations rates clinically significantly different for groups at T2 and T3. No significant differences of change in BI at T1 (p = .181) or T2 (p = .091) but significant differences between IV and CG at T3 (p = .023). Differences in the change of self-efficacy at T0, T1, T2, and T3, significant at T1 and T3. |
| Lenaghan (2019), United States | Quasi-experimental | N = 25 older adults | CO, QO; Health Belief Model and Self-efficacy. | IH | Confidence and belief subscale mean score significantly higher post-intervention (p = .001 and p < .0001). Four of the five confidence subscales, three significant: learning, following-up, giving health history(p = .005, p = .046, p = .008); all four increased in belief subscale, two significant: follow-up test results and questions about self-health (p = .0001, p = .0002). |
| Smith and Fields (2020), Australia | Non-experimental | N = 110 adults | CO; Person-centered goal setting and functional independence. | PD | A transitional care program following discharge led to clinical and significant improvements in all AusTOMs-OT scales including impairment, activity limitation, participation restriction, and wellbeing/distress. |
| Noel et al. (2020), United States | Randomized controlled trial | N = 102 adults | CO, HCU; Coleman's 4 pillars-TCM. | PD | Telehealth services that are person-centered and delivered by following discharge resulted in greater medication reconciliation rates (p = .013) and greater medication adherence. No significant differences for readmission or emergency department utilization. |
IV = intervention group; CG = control group.
Variables: CO = clinical outcomes; QO = quality outcomes; HCU = healthcare utilization.
Timing (transition period): PD = pre-discharge only; IH = inpatient to home; A = ambulatory.
Conceptual Basis
The theoretical framework differed between studies. The four studies contributed by the discipline of medicine were grounded in a medical transitional care perspective known as the Care-transition Initiative (CTI) (Coleman et al., 2004; Epstein-Lubow et al., 2014; Kvale et al., 2016; Noel et al., 2020). This conceptual framework, derived from patient and caregiver feedback of factors considered most valuable during times of care-transition, is composed of four transitional care pillars designed to mitigate quality and safety care-transition risks and support active and independent participation in care-transitions. From a nursing disciplinary perspective, each study used a different theoretical framework. Bull et al. (2000) referenced Donabedian's Quality of Care Model, while Lenaghan (2019), Chen et al. (2018), Schmaderer et al. (2016) and Ulin et al. (2016), cited the Health Belief Model, Health Empowerment Theory, Patient Activation Model, and Gothenburg Patient Centered Care model, respectively. Jangland et al. (2012) and Smith and Fields (2020) did not identify a theoretical or conceptual model.
Transition Team Member and Intervention Intensity
The intervention studies examined patient and healthcare team member partnerships in self-care planning and transition preparation, however, study designs both varied and overlapped in terms of healthcare professional, transitional care time period and setting, intervention intensity and target population. The majority of studies examining interventions intended to partner the healthcare professional and patient in a mutual, agreed-upon goal setting and coaching session, were implemented by nurses and limited to the pre-discharge time period (Bull et al., 2000; Chen et al., 2018; Coleman et al., 2004; Jangland et al., 2012; Lenaghan, 2019). Coleman et al. (2004), Lenaghan (2019) and Chen et al. (2018) implemented programs that expanded care settings and two programs were solely focused on the time period following hospital discharge with interventions delivered by physicians and occupational and physical therapists (Noel et al., 2020; Smith & Fields, 2020). Finally, the study by Kvale et al. (2016) was conducted in the ambulatory setting by a Master's degree-prepared mental health professional. The majority of interventions included coaching sessions comprised of goal setting and education, personalized health records, and telephonic and in-person support post-hospitalization. The intervention studies by Bull et al. (2000) and Jangland et al. (2012) incorporated the most passive patient participation efforts with healthcare professionals providing unidirectional self-management content.
Measuring Patient Participation
Numerous measures were used to quantify patient participation and for the purpose of this review, have been reduced to three major themes: clinical outcomes, quality outcomes, and healthcare utilization (See Table 2). A clinical outcome is used to describe or reflect how a patient feels, functions, or survives and includes biological, psychological, and social factors (Vizzotto et al., 2013). A quality outcome is used to reflect or quantify healthcare processes, outcomes, patient perceptions, and/or organizational structures associated with the capability to deliver high-quality health care (Medicaid, 2017). Healthcare utilization is the quantification or description of the use of services by persons for the purpose of preventing and curing health problems, promoting maintenance of health and well-being, or obtaining information about one's health status and prognosis (Carrasquillo, 2013). These goals include: effective, safe, well-organized, patient-centered, unbiased, and timely care. The reporting of measurement reliability and validity reporting was limited to the clinical and quality outcome domains and when described, were moderate to high (Arnetz et al., 2010; Bull et al., 2000; Jangland et al., 2012; Schmaderer et al., 2016).
Table 2.
Measures.
| Measurement type | Variable/Concept | Instrument/Measure | Article |
|---|---|---|---|
| Clinical Outcomes | Cardiovascular Symptoms |
|
Arnetz et al. (2010) |
|
|||
| Comorbidity |
|
Lenaghan (2019) | |
| Activities of Daily Living-Physical Functioning |
|
Chen et al. (2018) | |
|
|||
|
Smith and Fields (2020) | ||
| Behavioral Outcomes |
|
Kvale et al. (2016) | |
|
Arnetz et al. (2010) and Noel et al. (2020) | ||
|
Arnetz et al. (2010) | ||
| Distress and Well-Being |
|
Smith and Fields (2020) | |
|
Bull et al. (2000) | ||
|
Schmaderer et al. (2016) | ||
| Perceived Health/Perception of Health Status |
|
Bull et al. (2000); Kvale et al. (2016) | |
|
Kvale et al. (2016) | ||
|
Schmaderer et al. (2016) | ||
|
Kvale et al. (2016)— | ||
| Self-Efficacy |
|
Kvale et al. (2016) | |
|
Lenaghan (2019) | ||
|
Bull et al. (2000) | ||
|
Chen et al. (2018) | ||
|
Bull et al. (2000) | ||
|
Kvale et al. (2016); Schmaderer et al. (2016) | ||
| Health Literacy |
|
Kvale et al. (2016) | |
|
|||
|
Schmaderer et al. (2016) | ||
| Quality Outcomes | Patient Experience |
|
Coleman, et al. (2004) |
|
Bull et al. (2000) | ||
|
|||
|
|||
|
Noel et al. (2020) | ||
|
Arnetz et al. (2010) | ||
|
Ulin et al. (2016) | ||
|
Jangland et al. (2011) | ||
|
Schmaderer et al. (2016) | ||
|
Bull et al. (2000) | ||
|
|||
|
|||
| Quality Goals |
|
Arnetz et al. (2010) | |
|
Noel et al. (2020) | ||
|
Epstein-Lubow et al. (2014) | ||
| Healthcare Utilization | Readmission to the Hospital: In the 30-days following and up to 6-months following discharge |
|
Schmaderer et al. (2016) |
|
Noel et al. (2020) | ||
|
|||
|
Epstein-Lubow et al. (2014) | ||
|
Bull et al. (2000); Chen et al. (2018); Coleman et al. (2004); Noel et al. (2020) | ||
| Emergency department (ED) utilization in the 30 days or up to 6-months following discharge |
|
Bull et al. (2000) and Noel et al. (2020) | |
|
|||
|
Schmaderer et al. (2016) | ||
|
Coleman et al. (2004) | ||
| Prior Utilization: Hospital admission and observation frequency, one-year lookback from index admission |
|
Coleman et al. (2004) | |
| Primary Care Provider (PCP) Visits |
|
Kvale et al. (2016) | |
|
Noel et al. (2020) |
Clinical Outcomes
Eight of the studies examined the relationships between measures of patient participation and clinical outcome variables such as cardiovascular symptoms, activities of daily living (ADL), number of chronic conditions, perception of health status, distress and well-being, and behavioral outcomes. Two instruments were used to evaluate cardiovascular symptoms (Arnetz et al., 2010). Patients reporting angina and shortness of breath at the time of hospital discharge follow-up gave significantly lower ratings of having received meaningful discharge information and having had personal needs such as the ability to ask questions and having been treated with respect. Higher perceived care involvement was associated with systolic blood pressure control (Arnetz et al., 2010). Two studies examined patient participation and physical functioning (Chen et al., 2018; Smith & Fields, 2020). A patient-centered self-management empowerment intervention (PCSEMI) was associated with higher ADL at 3-months post-discharge (Chen et al., 2018). Likewise, an interdisciplinary care-transition program focused on physical functionality in the home following hospital discharge led to statistical and clinical improvements in patient impairment, activity limitation, and participation restriction (Smith & Fields, 2020). Finally, comorbidity was measured as a primary clinical outcome in one study (Lenaghan, 2019). A significant interaction between multimorbidity and confidence in the ability to practice self-care behaviors was found on improving patient empowerment.
The most commonly analyzed clinical outcomes were related to psychological constructs and behavioral outcomes and included perceptions of health and quality of life, self-efficacy, and distress and wellbeing. The Patient Activation Measure (PAM) was used in two studies. Higher PAM values equate to greater levels of perceived self-efficacy and mixed results were demonstrated in the studies. Schmaderer et al. (2016) determined psychological factors such as health literacy, role satisfaction, and perceived involvement in care, were predictors of higher levels of patient activation. Kvale et al. (2016) did not find patient participation interventions to increase PAM scores, however, determined those engaged in self-management transition activities demonstrated higher self-reported health, lower social role limitations and a trend toward greater self-efficacy. Similar outcomes of interventions designed to increase patient participation in transitional care were found in the studies by Chen et al. (2018) and Lenaghan (2019). Smith and Fields (2020) found that participants engaged in an interdisciplinary care-transitions program post-hospitalization maintained and/or improved levels of participation restriction and distress/well-being. Finally, in a study examining correlations of patient activation and clinical factors, those with higher activation scores experienced less difficulty with function, fewer problems with sleep and pain, and lower depression and anxiety scores (Schmaderer et al., 2016).
Quality Outcomes
Eight studies utilized quality outcomes measurements of patient participation in transitional care. Patient and healthcare team partnerships in individualized transition planning led to higher perceived health, satisfaction with planning, and a greater feeling of preparedness. Ulin et al. (2016) determined early discharge planning and communication between the hospital and community healthcare team members resulted in shorter hospital stays, while Noel et al. (2020) found statistically significant greater medication adherence and positive feedback for those participatory in a telehealth care-transitions program. In the study by Arnetz et al. (2010), an inverse relationship between patient ratings of planning inclusion and goal achievement was identified. Only two of the studies focused on caregivers and their role in patient participation (Bull et al., 2000; Epstein-Lubow et al., 2014). The latter of the two examined the correlation between bedside caregiver status during the introduction of a post-discharge care-transitions program, while Bull et al. (2000) measured actual caregiver response to caregiving. Persons with caregivers at the bedside during the time of enrollment were more likely to participate in a care-transitions program (Epstein-Lubow et al., 2014), while caregivers who participated in a person-centered care-transitions program reported receiving more hospital pre-discharge information and rated a more positive reaction to caregiving (Bull et al., 2000).
Healthcare Utilization
Healthcare utilization in the form of readmission to the acute-care hospital setting, emergency department utilization following discharge, and primary care discharge follow-up was measured as an outcome variable in seven studies. Schmaderer et al. (2016) determined lower patient activation scores were associated with higher levels of acute care utilization, while Coleman et al. (2004) and Chen et al. (2018) determined person-centered transition planning across settings resulted in lower levels of acute utilization in the time period following discharge. Like Noel et al. (2020), Bull et al. (2000) did not find a statistically significant difference in patient participation efforts and post-discharge utilization, but did identify lower readmissions. Kvale et al. (2016) examined utilization through a primary care follow-up lens and determined higher patient activation levels did not increase the likelihood of attendance, though did identify statistically significant lower perceptions of care involvement for myocardial infarction patients that completed cardiac rehabilitation post-discharge. Overall, the findings related to patient participation in transitional care and healthcare utilization are mixed, though, overall appear to point toward less utilization. While readmission to the hospital setting and emergency department utilization following acute-care discharge were frequently used as outcome measures, timeframes ranged from 30-days to 6-months post-hospitalization and data extraction procedures varied (See Table 2).
Discussion
To our knowledge, this systematic review has been the first to acknowledge factors of patient participation in transitional care include higher perceived levels of self-efficacy, confidence, health, and skills to participate in care. Efforts to increase care self-management during transition periods were shown to increase these perceptions and to decrease distress and acute care utilization. Across studies, a worldwide and multidisciplinary interest in better understanding or improving adults’ ability to participate in the self-management of care during transitions was identified. Commonly, multi-component transitional care interventions derived from patient and care team partnered planning were delivered beyond one care setting. Factors of patient participation in transitional care were found to be largely related to modifiable psychological and psychosocial patient characteristics linked to clinical outcomes, quality outcomes, and healthcare utilization. Nevertheless, study participants represented a largely narrow demographic, limited sociodemographic data were collected, and the discipline of nursing offered inconsistent theoretical support across studies. Interventions aimed at improving patient participation in transitional care were chiefly limited to one or two care settings, as opposed to a greater length of the care continuum. Although factors related to patient participation in transitional care appear primarily related to psychological and psychosocial patient factors, it is unclear from this review how these factors change across the care continuum and acuity of illness. Measurement type and measurement frequency is also unclear after the completion of this review.
The widespread international study locations found in this systematic review are an indicator that factors of patient participation in transitional care is viewed as a global priority, particularly in the elderly. For the purpose of this review, participant age was not limited to the elderly adult population, as care-transitions are noted to occur throughout the lifespan; yet, the findings from this review are similar with an average participant age of 79 years. Copious literature examining adolescents or young adults with chronic illness transitioning to adult care was found during the implementation of this study; however, literature pertaining to patient participation in transitional care in young and middle-aged adults was limited. To our knowledge, this is the first review aimed at identifying factors of patient participation in transitional care in an adult population not limited to the elderly. Accordingly, all but two of the studies expanded transitional care age parameters beyond the geriatric population. Otherwise, the majority of participants in this study were white. The United States Census Bureau notes that throughout the 2030 decade, we will see not only a considerably and slowly aging population, but one that is more racially and ethnically diverse (United States Census Bureau). Hence, there is a lack of diversity noted in the literature for patient participation in care-transitions for those who are younger and not white. Future studies should aim to included younger participants and be reflective of the diverse patient populations seen globally.
Although progress has been made on testing a number of transitional care interventions to improve care-transitions, a downward trend of readmission rates has been unevenly observed (Angraal et al., 2018; Gerhardt et al., 2013; Zuckerman et al., 2016). Among U.S. hospitals, wide variation in readmission rates is noted, as is persistently elevated rates among low-income patients and other vulnerable subgroups (Li et al., 2021). In a 2018 retrospective cohort study examining readmission to a large, rural acute tertiary and quintenary care facility, it was identified patients with ambulation difficulty, ADL deficits, difficulties completing errands, and those with a history of substance abuse treatment, experienced higher 30-day readmission rates than those without one or more of these characteristics (Mallow et al., 2020). The majority of those who were readmitted had multiple comorbidities and Medicaid as a primary insurance. In this review, collection of sociodemographic data was limited, though number and severity of chronic conditions was frequently studied. Continued study of transitional care and patient participation for people living with multiple comorbidities, functional ability, and social determinants of health is needed.
Experimental efforts to identify or improve factors of patient participation in transitional care has increased (Dyrstad et al., 2015). The results of this review highlight numerous experimental studies with increasing chronological frequency, although, a lack of randomization of study participants is noted. Several observational studies aimed at identifying factors related to patient participation in transitional care was noted in this review. This is not surprising given that a large body of both qualitative and mixed-methods research is focused on this phenomenon (Betz et al., 2013; Higgins et al., 2017; Naylor et al., 2017; Scott et al., 2017). Sample sizes identified in this review were similar to those identified in a recent systematic review of transitional care interventions on hospital readmissions with the majority of samples totaling less than 500 participants (Fønss Rasmussen et al., 2021). Future studies related to patient participation in transitional care should be designed at the randomized control trial experimental level and with adequate power to detect differences between groups.
Multidisciplinary interest in patient participation in transitional care is evident from this review. Innovative strategies to effectively manage transitional require experiential analysis and planning not only from care providers, but key stakeholders in policy positions, leadership roles, and community settings (Epping-Jordan, 2002). The discipline of social work is known for the Bridge Model of Transitional Care (Alvarez et al., 2016), while the discipline of pharmacy has long focused on mitigating medication risks during times of care-transitions (Conklin et al., 2014). Recently, multidisciplinary efforts to improve care-transitions and develop recommendations has begun (Li et al., 2021) and nursing education accreditors are recognizing both interprofessional partnerships and care that spans across settings throughout the lifespan as areas of emphasis (American Association of Colleges of Nursing, 2021). Hence, future interventions aimed at patient participation in care-transitions should be multidisciplinary in nature.
Conceptual Basis
The discipline of medicine most clearly and congruently outlined the underlying basis of their efforts to study patient participation in transitional care through the use of Coleman's CTI (Coleman et al., 2004; Epstein-Lubow et al., 2014; Kvale et al., 2016; Noel et al., 2020); although, the number and interlinking of the concepts from the original model varied. The discipline of nursing has noted a significantly growing focus on patient participation in care and a steady growth of papers on the topic; yet, many researchers are calling for greater conceptual clarification (Enderlin et al., 2013; Finset, 2017; Halabi et al., 2020; Higgins et al., 2017; Mark et al., 2013). Although several concepts on patient participation have emerged, one unifying concept has yet to be used and studied consistently (Halabi et al., 2020). Clarification and differentiation of the concepts patient participation, patient engagement, patient empowerment, and patient activation is needed. Finally, although the Transitional Care Model (TCM) (Naylor, 1990), a well-known, evidence-based model steadily demonstrated to enhance care experiences, improve health and quality of life, and to decrease unnecessary healthcare costs (Naylor et al., 2018) exists within the nursing discipline, its use was not identified in this systematic review of patient participation in transitional care. Future study should be consistent in conceptual clarity and be based on effective evidence-based models of care.
Transition Team Member and Intervention Intensity
Efforts aimed at patient participation in transitional care require a multifactorial and multidimensional approach. Though breakdowns in communication can occur at any point along the care continuum, some of the most overwhelming miscommunications during the transfer of care occur during the transition from hospital to home, where the patient often becomes solely responsible for his or her own care (McGaw et al., 2007). Evidence-based transitional care programs enlisting the expertize of a nurse or a transition coach to help guide the patient along a plan of care help mitigate barriers (Coleman et al., 2006; Naylor et al., 2017). Mary Naylor's prototype, for example, is an advanced practice nurse (APN) led, team-based, care management model designed to address amendable challenges in the current healthcare delivery system and includes components such as promoting communication and collaboration between team members and assuring coordination across settings (Naylor et al., 2017). Coleman's CTI shares similarities with the TCM and specific to both models is support of the patient to self-manage needs across the post-hospitalization continuum, as opposed to a limited time period following hospital discharge. Several of the aforementioned key components aimed at supporting patient participation in transitional care, including the delivery of transitional care services beyond an initial 24-h discharge period (Fønss Rasmussen et al., 2021; Lenaghan, 2019; Li et al., 2021). Nevertheless, a recent review examining common adaptations of these models, identified one of the most frequently cited adaptations includes termination of transitional care efforts shortly after hospital discharge (Naylor et al., 2018).
Measuring Patient Participation
Findings from this systematic review support higher PAM levels were associated with better psychological and psychosocial outcomes. Clinical factors of patient participation in transitional care included perceptions of physical functioning, distress, and wellbeing. This review also verifies patient participation in care has been credited with contributing to improved outcomes and experiences of care. Patient-centered transitional care planning grounded in patient and care team partnerships, result in greater perceived individual health and transition care planning and discharge preparation satisfaction as well as decreased, avoidable healthcare utilization. Similarly, an inverse relationship was noted between levels of patent activation and utilization. Meaning, those individuals more activated in self-management experienced less, avoidable care utilization. Thus, further warranting continued focus on patient perception of care involvement and participation.
Limitations
Several limitations to this systematic review of quantitative studies of patient participation and transitional care are noted, as were limitations within individual studies. Although subject search terms for both patient participation and transitional care were expanded to include commonly associated terminology, it is possible studies examining these phenomena were missed. This review was limited to quantitative, peer-reviewed studies, written in the English language and it is possible pertinent studies were omitted. Within the individual studies were also limitations. Participants were older, primarily white, cognitively intact, and more likely to be transitioning from the hospital setting, to home, confining generalizability. Furthermore, individuals with acute and chronic cognitive impairments, considered as some of the highest-risk, vulnerable populations, were often excluded from these studies. Otherwise not in this review was the study of caregiver inclusion in patient participation efforts during transitional care.
Implications for Practice & Research
Future studies should aim to include a broader-reaching demographic to include younger and more diverse patient populations, seen globally. Likewise, ongoing study of patient participation in transitional care should include variables such as number of chronic conditions, functional abilities, and social determinants of health. These studies should be experimental in design, at the randomized control trial level, and adequately powered to detect differences between groups. Furthermore, these studies should focus on patient perception of care involvement and participation, be conceptually clear and based on effective evidence-based models of care, and include multidisciplinary interventions. Finally, a scoping review examining patient participation in transitional care in an adult population (18 years of age and older) could be considered to examine these findings in light of a broader literature base.
Conclusions
Patient participation in transitional care is a complex phenomenon of global interest, no longer limited to the elderly, the discipline of nursing, the acute hospital setting, and signified by readmission rates alone. This systematic review of quantitative studies examining patient participation in transitional care revealed 12 studies that varied in design, location, and timeframe and overlapping themes such as transitional care time period, disciplinary perspective, conceptual basis of patient participation or involvement in care planning, and intervention type and intensity. Across studies, various measures were used to measure patient participation in transitional care and reliability and validity data was limited. Largely, patient participation in transitional care appears to be based on modifiable perceptions of self-efficacy, confidence, and skill. Identified efforts to improve patient participation in transitional care include individualized, multidisciplinary transitional care interventions targeting these characteristics and delivered beyond the hospital setting. Moving forward, these efforts should be implemented with psychological and behavioral patient perceptions in mind and aimed at seamless and patient-centric care provision. The discipline of nursing, philosophically focused on caring in the human health experience and skilled at interprofessional communication, collaboration, and organization of patient care and experience among diverse populations and across settings, remains uniquely positioned to continue in such role.
Acknowledgments
None
Footnotes
Declaration of Conflicting Interests: The Author(s) declare(s) that there is no conflict of interest.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Andrea R. Bailey https://orcid.org/0000-0001-9245-8526
Laurie Theeke https://orcid.org/0000-0002-6965-0728
Jennifer Mallow: https://orcid.org/0000-0001-8477-0405
References
- Alvarez R., Ginsburg J., Grabowski J., Post S., Rosenberg W. (2016). The social work role in reducing 30-day readmissions: The effectiveness of the bridge model of transitional care. Journal of Gerontological Social Work, 59(3), 222–227. 10.1080/01634372.2016.1195781 [DOI] [PubMed] [Google Scholar]
- American Association of Colleges of Nursing. (2021, April 7). Bold action taken to transform nursing education and strengthen the nation's healthcare workforcee [Press release] . https://www.magnetmail.net/actions/email_web_version.cfm?recipient_id=2126274304&message_id=20134553&user_id=AACN&group_id=5815322&jobid=51352653
- Angraal S., Khera R., Zhou S., Wang Y., Lin Z., Dharmarajan K., Desai N. R., Bernheim S. M., Drye E. E., Nasir K., Horwitz L. I., Krumholz H. M. (2018). Trends in 30-day readmission rates for medicare and non-medicare patients in the era of the affordable care act. American Journal of Medicine, 131(11), 1324–1331.e1314. 10.1016/j.amjmed.2018.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnetz J. E., Winblad U., Höglund A. T., Lindahl B., Spångberg K., Wallentin L., Wang Y., Ager J., Arnetz B. B. (2010). Is patient involvement during hospitalization for acute myocardial infarction associated with post-discharge treatment outcome? An exploratory study. Health Expectations: An International Journal of Public Participation in Health Care and Health Policy, 13(3), 298–311. 10.1111/j.1369-7625.2009.00588.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betz C. L., Lobo M. L., Nehring W. M., Bui K. (2013). Voices not heard: A systematic review of adolescents’ and emerging adults’ perspectives of health care transition. Nursing Outlook, 61(5), 311–336. 10.1016/j.outlook.2013.01.008 [DOI] [PubMed] [Google Scholar]
- Bull M. J., Hansen H. E., Gross C. R. (2000). A professional-patient partnership model of discharge planning with elders hospitalized with heart failure. Applied Nursing Research, 13(1), 19–28. 10.1016/s0897-1897(00)80015-4 [DOI] [PubMed] [Google Scholar]
- Carrasquillo O. (2013). Health care utilization. In Gellman M. D., Turner J. R. (Eds.), Encyclopedia of behavioral medicine (pp. 909–910). Springer New York. 10.1007/978-1-4419-1005-9_885 [DOI] [Google Scholar]
- Chen L., Chen Y., Chen X., Shen X., Wang Q., Sun C. (2018). Longitudinal study of effectiveness of a patient-centered self-management empowerment intervention during predischarge planning on stroke survivors. Worldviews on Evidence-Based Nursing, 15(3), 197–205. 10.1111/wvn.12295 [DOI] [PubMed] [Google Scholar]
- Coleman E. A., Parry C., Chalmers S., Min S.-J. (2006). The care transitions intervention: Results of a randomized controlled trial. Archives of Internal Medicine, 166(17), 1822–1828. 10.1001/archinte.166.17.1822 [DOI] [PubMed] [Google Scholar]
- Coleman E. A., Smith J. D., Frank J. C., Min S., Parry C., Kramer A. M. (2004). Preparing patients and caregivers to participate in care delivered across settings: The care transitions intervention. Journal of the American Geriatrics Society, 52(11), 1817–1825. 10.1111/j.1532-5415.2004.52504.x [DOI] [PubMed] [Google Scholar]
- Conklin J. R., Togami J. C., Burnett A., Dodd M. A., Ray G. M. (2014). Care transitions service: A pharmacy-driven program for medication reconciliation through the continuum of care. American Journal of Health-System Pharmacy, 71(10), 802–810. 10.2146/ajhp130589 [DOI] [PubMed] [Google Scholar]
- Connolly M., Grimshaw J., Dodd M., Cawthorne J., Hulme T., Everitt S., Tierney S., Deaton C. (2009). Systems and people under pressure: The discharge process in an acute hospital. Journal of Clinical Nursing, 18(4), 549–558. 10.1111/j.1365-2702.2008.02551.x [DOI] [PubMed] [Google Scholar]
- Dyrstad D. N., Testad I., Aase K., Storm M. (2015). A review of the literature on patient participation in transitions of the elderly. Cognition, Technology & Work, 17(1), 15–34. 10.1007/s10111-014-0300-4 [DOI] [Google Scholar]
- Enderlin C. A., McLeskey N., Rooker J. L., Steinhauser C., D’Avolio D., Gusewelle R., Ennen K. A. (2013). Review of current conceptual models and frameworks to guide transitions of care in older adults. Geriatric Nursing, 34(1), 47–52. 10.1016/j.gerinurse.2012.08.003 [DOI] [PubMed] [Google Scholar]
- Epping-Jordan J. (2002). Innovative care for chronic conditions: Building blocks for action: Global report. Noncommunicable Diseases and Mental Health, World Health Organization. https://search.ebscohost.com/login.aspx?direct=true&scope=site&db=nlebk&db=nlabk&AN=91361 [Google Scholar]
- Epstein-Lubow G., Baier R. R., Butterfield K., Gardner R., Babalola E., Coleman E. A., Gravenstein S. (2014). Caregiver presence and patient completion of a transitional care intervention. The American Journal of Managed Care, 20(10), e349–e444. https://pubmed.ncbi.nlm.nih.gov/25414979/ [PubMed] [Google Scholar]
- Finset A. (2017). Patient participation, engagement and activation: Increased emphasis on the role of patients in healthcare. Patient Education and Counseling, 100(7), 1245–1246. 10.1016/j.pec.2017.05.011 [DOI] [PubMed] [Google Scholar]
- Fønss Rasmussen L., Grode L. B., Lange J., Barat I., Gregersen M. (2021). Impact of transitional care interventions on hospital readmissions in older medical patients: A systematic review. BMJ open, 11(1), e040057. 10.1136/bmjopen-2020-040057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foss C., Askautrud M. (2010). Measuring the participation of elderly patients in the discharge process from hospital: A critical review of existing instruments. Scandinavian Journal of Caring Sciences, 24, 46–55. 10.1111/j.1471-6712.2010.00788.x [DOI] [PubMed] [Google Scholar]
- Gerhardt G., Yemane A., Hickman P., Oelschlaeger A., Rollins E., Brennan N. (2013). Medicare & Medicaid research review: Data shows reduction in Medicare hospital readmission rates during 2012. 3(2), E1–E11. https://www.cms.gov/mmrr/Downloads/MMRR2013_003_02_b01.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halabi I. O., Scholtes B., Voz B., Gillain N., Durieux N., Odero A., Baumann M., Ziegler O., Gagnayre R., Guillaume M., Bragard I., Pétré B. (2020). “Patient participation” and related concepts: A scoping review on their dimensional composition. Patient Education and Counseling, 103(1), 5–14. 10.1016/j.pec.2019.08.001 [DOI] [PubMed] [Google Scholar]
- Higgins T., Larson E., Schnall R. (2017). Unraveling the meaning of patient engagement: A concept analysis. Patient Education and Counseling, 100(1), 30–36. 10.1016/j.pec.2016.09.002 [DOI] [PubMed] [Google Scholar]
- doi: 10.17226/10027. Institute of Medicine Committee on Quality of Health Care in, America. (2001). In Crossing the quality chasm: A new health system for the 21st century. National Academies Press (US). [DOI] [PubMed] [Google Scholar]
- Jangland E., Carlsson M., Lundgren E., Gunningberg L. (2012). The impact of an intervention to improve patient participation in a surgical care unit: A quasi-experimental study. International Journal of Nursing Studies, 49(5), 528–538. 10.1016/j.ijnurstu.2011.10.024 [DOI] [PubMed] [Google Scholar]
- Kvale E. A., Huang C.-H. S., Meneses K. M., Demark-Wahnefried W., Bae S., Azuero C. B., Rocque G. B., Bevis K. S., Ritchie C. S. (2016). Patient-centered support in the survivorship care transition: Outcomes from the patient-owned survivorship care plan intervention. Cancer, 122(20), 3232–3242. 10.1002/cncr.30136 [DOI] [PubMed] [Google Scholar]
- Lenaghan N. A. (2019). Transitional care and empowerment of the older adult. Geriatric Nursing (New York, N.Y.), 40(2), 148–153. 10.1016/j.gerinurse.2018.07.005 [DOI] [PubMed] [Google Scholar]
- Li J., Du G., Clouser J. M., Stromberg A., Mays G., Sorra J., Brock J., Davis T., Mitchell S., Nguyen H. Q., Williams M. V. (2021). Improving evidence-based grouping of transitional care strategies in hospital implementation using statistical tools and expert review. BMC Health Services Research, 21(1), 1–20. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-020-06020-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallow J. A., Bailey A., Clark K. R., Theeke L. (2020). Assessment of readmission in a rural medical center. Online Journal of Rural Nursing and Health Care, 20(2), 241–262. 10.14574/ojrnhc.v20i2.615 [DOI] [Google Scholar]
- Mark V. P., Mary D. N., Karen B. H., Melissa O. C., Ronald B. (2013). Engaging older adults in their transitional care: What more needs to be done? Journal of Comparative Effectiveness Research, 2(5), 457–468. 10.2217/cer.13.58 [DOI] [PubMed] [Google Scholar]
- McGaw J., Conner D. A., Delate T. M., Chester E. A., Barnes C. A. (2007). A multidisciplinary approach to transition care: A patient safety innovation study. The Permanente Journal, 11(4), 4–9. 10.7812/tpp/07-012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicaid, C. G. C. F. M. A. (2017). What is a quality measure? https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/NTM-What-is-a-Quality-Measure-SubPage
- Melnyk B. M., Fineout-Overholt E. (2011). Evidence-based practice in nursing & healthcare: A guide to best practice (2nd ed.). Wolters Kluwer/Lippincott Williams & Wilkins. http://catdir.loc.gov/catdir/enhancements/fy1204/2010007467-t.html, http://catdir.loc.gov/catdir/enhancements/fy1204/2010007467-d.html, http://books.google.com.my/books?id=hHn7ESF1DJoC&lpg=PP1&dq=9781605477787&pg=PP1#v=onepage&q&f=false [Google Scholar]
- Naylor M. D. (1990). Comprehensive discharge planning for hospitalized elderly: A pilot study. Nursing Research, 39(3), 156–161. 10.1097/00006199-199005000-00007 [DOI] [PubMed] [Google Scholar]
- Naylor M. D., Hirschman K. B., Toles M. P., Jarrín O. F., Shaid E., Pauly M. V. (2018). Adaptations of the evidence-based transitional care model in the U.S. Social Science & Medicine (1982), 213, 28–36. 10.1016/j.socscimed.2018.07.023 [DOI] [PubMed] [Google Scholar]
- Naylor M. D., Shaid E. C., Carpenter D., Gass B., Levine C., Li J., Malley A., McCauley K., Nguyen H. Q., Watson H., Brock J., Mittman B., Jack B., Mitchell S., Callicoatte B., Schall J., Williams M. V. (2017). Components of comprehensive and effective transitional care. Journal of the American Geriatrics Society, 65(6), 1119–1125. 10.1111/jgs.14782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noel K., Messina C., Hou W., Schoenfeld E., Kelly G. (2020). Tele-transitions of care (TTOC): A 12-month, randomized controlled trial evaluating the use of telehealth to achieve triple aim objectives. BMC Family Practice, 21(1), 27. 10.1186/s12875-020-1094-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page M. J., McKenzie J. E., Bossuyt P. M., Boutron I., Hoffmann T. C., Mulrow C. D., Moher D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmaderer M. S., Zimmerman L., Hertzog M., Pozehl B., Paulman A. (2016). Correlates of patient activation and acute care utilization among multimorbid patients. Western Journal of Nursing Research, 38(10), 1335–1353. 10.1177/0193945916651264 [DOI] [PubMed] [Google Scholar]
- Scott A. M., Li J., Oyewole-Eletu S., Nguyen H. Q., Gass B., Hirschman K. B., Mitchell S., Hudson S. M., Williams M. V., Project A. T. (2017). Understanding facilitators and barriers to care transitions: Insights from project ACHIEVE site visits. Joint Commission Journal on Quality and Patient Safety, 43(9), 433–447. 10.1016/j.jcjq.2017.02.012 [DOI] [PubMed] [Google Scholar]
- Smith H. N., Fields S. M. (2020). Changes in older adults’ impairment, activity, participation and wellbeing as measured by the AusTOMs following participation in a transition care program. Australian Occupational Therapy Journal, 67(6), 517–527. 10.1111/1440-1630.12667 [DOI] [PubMed] [Google Scholar]
- Solomon P., Hanrahan N. P., Hurford M., DeCesaris M., Josey L. (2014). Lessons learned from implementing a pilot rct of transitional care model for individuals with serious mental illness. Archives of Psychiatric Nursing, 28(4), 250–255. 10.1016/j.apnu.2014.03.005 [DOI] [PubMed] [Google Scholar]
- Ulin K., Olsson L.-E., Wolf A., Ekman I. (2016). Person-centred care - An approach that improves the discharge process. European Journal of Cardiovascular Nursing: Journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology, 15(3), e19–e26. 10.1177/1474515115569945 [DOI] [PubMed] [Google Scholar]
- Vizzotto A. D. B., de Oliveira A. M., Elkis H., Cordeiro Q., Buchain P. C. (2013). Psychosocial characteristics. In Gellman M. D., Turner J. R. (Eds.), Encyclopedia of behavioral medicine (pp. 1578–1580). Springer New York. 10.1007/978-1-4419-1005-9_918 [DOI] [Google Scholar]
- Zuckerman R. B., Sheingold S. H., Orav E. J., Ruhter J., Epstein A. M. (2016). Readmissions, observation, and the hospital readmissions reduction program. New England Journal of Medicine, 374(16), 1543–1551. 10.1056/NEJMsa1513024 [DOI] [PubMed] [Google Scholar]