Abstract
This study investigates whether the illness perception mediates the relationship between psychological hardiness and the health status of Covid-19 survived patients. In a cross-sectional study, 205 Covid-19 were selected by purposive sampling from Qom (the first coronavirus epidemiological site in Iran) and responded to Abridged Hardiness Scale (AHS) and Brief Illness Perception Questionnaire (Brief IPQ) and Patient Health Questionnaire (PHQ-9). Results: The results of correlation showed that the relationship between AHS scores with PHQ-9 (P<0.01) and Brief IPQ (P<0.01) was negative and significant. The relationship between Brief IPQ and PHQ-9 scores was also positive and significant (P<0.01). The proposed mediating model had a relatively good fit. However, a better fit was achieved by releasing several covariance errors and explained 47% of the PHQ-9 scores (χ2/df=2.46, RMSEA=0.075, CFI=0.950, PCFI=0.689, IFI=0.953, GFI=0.964). The Bootstrap analysis showed that Brief IPQ scores significantly mediated the relationship between AHS and PHQ-9 scores (95% CI: -0.073 to -0.002). The findings suggest a more negative perception of perceptions Covid-19 disease is associated with lower levels of patient health. As a mediating variable, it prevents the positive effects of psychological hardiness on improving patients’ health. The application of these findings has been discussed.
Keywords: coronavirus, covid-19, psychological hardiness, illness perception, health status
Introduction
Coronavirus is a family of viruses that causes severe respiratory symptoms. The previous viruses of this family, i.e., SARS and MERS-CoV, spread in 2004 and 2012, respectively. As a new coronavirus was discovered in December 2019, it was called the Covid-19. This virus was first found in Wuhan-China and caused a pandemic. Accordingly, the World Health Organization (WHO) declared a public health emergency on January 31, 2020.1
Convincing evidence suggests that the incidence of infectious diseases such as SARS, Mers, and type A influenza associated with mental health problems in among public,2,3 patients4,5 and family members of patients.6 Lee, Kang, Cho, Kim, and Park5 conducted a study to investigate the effect of Covid-19 on emotional indicators (e.g., anxiety, depression, anger, and happiness) and cognitive indicators (e.g., social risk judgment and life satisfaction) on the active users of a social network. This study indicated that negative indicators such as anxiety, depression, anger, and sensitivity to social risks increased, and positive indicators such as happiness and life satisfaction declined among these people.
Implementing health policies such as quarantine, despite the positive consequences, have negative psychological effects on society. On the other hand, low predictability, high prevalence, and long incubation period affect patients’ mental health emotionally and cognitively.7 Stress caused by a disease such as Covid-19 does not affect everyone equally, and this issue is due to a variety of factors, including psychosocial hardiness. Kobasa, Maddi, and Zola8 argued that the hardiness personality trait positively correlates with physical and mental health. Hardiness is the most important source of stress-relieving effects and strengthens the immune system. Kobasa et al.8 considered the three components of control, commitment, and challenge effective in reducing stress. Under stressful conditions, people who feel more “in control” of what is happening in their lives are healthier than those who feel weak in the face of external forces. Moreover, those who feel “committed” to their life problems are healthier than those who feel alienated. On the other hand, those who see change as a “challenge” are healthier than those who consider changing a threat.9
Indeed, these patients have been faced with secondary side effects, such as limitations in social life, jobless and financial problems, and dozens of other consequences that will ultimately negatively affect their quality of life. To improve the quality of life of these patients, it is important to adapt to the existing situations. One of the important psychological variables that effectively adapt to the disease is the individual’s perception of the illness. Illness perception means the organized cognitive representation of the patient of his illness. As patients actively process their disease, they make cognitive representations that threaten their health, which determines how patients respond to these factors, determine patients’ adaptation to the illness and its symptoms. They are associated with several significant consequences, such as adherence to the treatment process and improving performance.10 On the other hand, the findings show that negative illness perception is one of the most important predictors of fatigue, anxiety, and depression.11 Therefore, it is assumed that the illness perception can affect the relationship between psychological hardiness and the health of Covid-19 survived patients. The question of the present study is whether the individual’s illness perception can play a mediating role in the positive relationship between psychological hardiness and health status of patients recovered from COVID-19?
Materials and Methods
Participants
The present study is fundamental in terms of purpose and descriptive-cross-sectional based on the method. In this study, psychological hardiness, patient health, and illness perception are the exogenous, endogenous, and mediator variables. The study’s statistical population included Covid-19 survived patients in Qom, who were purposively selected from April 1 to 13, 2020. This city is located in central Iran, and the first cases of Covid-19 were reported there. Mueller’s (1996) method was used to determine the sample size for the structural equation modeling based on the expected average effect size, the statistical power of 0.80, and 95% confidence level, during which it was determined that the proposed model with 41 free parameters in measurement model, 3 latent variables and 39 indicators requires 205 samples with less than 10% of missing data.
According to the expert physician, the inclusion criteria were definite infection with Covid-19, living in Qom province, and being over 18 years old. The exclusion criteria were inadequate completion of tests, being under 18 years of age, and the inconclusive diagnosis of coronavirus. These patients were selected by purposive sampling. First, the list of all patients who had a positive coronavirus disease (COVID-19) test results by transcription-polymerase chain reaction (RT-PCR) testing and chest CT scanning and referred to all hospitals in Qom was received from the Headquarters of Administrating coronavirus (located in Qom University of Medical Sciences). Then, to prevent the virus’s spread and cut off the transmission chain, questionnaires were sent electronically through cyberspace (WhatsApp and Telegram messengers) to the selected participants. The links of the posted questionnaires to smartphones were completed by 205 patients and returned to the researcher’s email address. In case of ethical considerations, this study has no intervention or biological sampling from a human. This was a questionnaire-based study; however, all procedures performed in this study were by the ethical standards of the Institutional and/or National Research Committee and with the 2007 Helsinki declaration and its later amendments or comparable ethical standards.12 The tools used in the research are as follows:
Measures
Abridged Hardiness Scale (AHS): The AHS was developed by Kobasa (1982) to measure hardiness. The test consists of 20 four-choice questions (never, rarely, sometimes, and often) and includes three components: commitment, control, and challenge. The minimum and maximum scores in this test are 0 to 60, respectively, and the high score indicates more and higher hardiness. Using Cronbach’s alpha method Kobasa13 reported the reliability of this test as 0.81. Using Cronbach’s alpha method, Zare and Aminpour14 reported the internal consistency reliability for the whole test as 0.91. Using the Varimax rotation, they obtained three main factors from the Persian version of AHS, which was similar to the theoretical concepts proposed by Kobasa.13 In the present study, the internal consistency of AHS was calculated by Cronbach’s alpha coefficient as 0.921.
Brief Illness Perception Questionnaire (Brief IPQ): This questionnaire was designed and validated by Broadbent, Petrie, Main, and Weinman.15 It consists of 9 items. Questions include the consequences, timeline, personal control, treatment control, identity, illness concern, illness comprehension, emotional response, and causal representation. Sample items are ” How much do you think your treatment can help your illness?” and ” How concerned are you about your illness?” The total range of the first eight questions is between 0 and 80, and getting higher scores means a more profound understanding or more significant impact of the illness. Question 9 is an open-answer item and questions the three main causes of the disease respectively.QuestionGiven that the purpose of the present study was not to investigate the cause of the disease, this question is omitted. Cronbach’s alpha for this questionnaire was 0.80, and the retest reliability coefficient for different questions was from 0.42 to 0.75 after six weeks of interval. In Iran, Bazzazian, and Basharat,16 the calculated reliability coefficient was 0.33. In the present study, using Cronbach’s alpha coefficient, the internal consistency of Brief IPQ was 0.68.
Patient Health Questionnaire (PHQ-9): This questionnaire is a multi-objective tool consisting of 9 questions with a 4-point Likert scale (from 0 to 3) for screening, diagnosis, follow-up, and measurement of depression severity. The PHQ-9 includes the DSM-IV Depression Diagnostic Index along with the main symptoms of depression. Acquiring higher scores on PHQ-9 means more depression. In Iran, PHQ-9 has shown acceptable validity and reliability in clinical settings.17 In the present study, using Cronbach’s alpha coefficient, the internal consistency of PHQ-9 is calculated as 0.83.
In the present study, Pearson product-moment correlation coefficient and structural equation modeling technique were used to analyze the data. SPSS and AMOS software version 22 were used in the statistical analyses. The Bootstrap analysis was used for the significance test of indirect paths in Preacher and Hayes’ Macro program.18
Results
Two hundred and five patients improved from coronavirus participated in the study. Table 1 shows the descriptive characteristics of the demographic variables of these patients. The mean age of the participants was 41.15 ± 12.07, ranging from 18 to 85 years. The mean length of hospital stay was 10.76 ± 10.26 days, with a minimum of 1 and a maximum of 45 days. The mean number of patients’ family members with coronavirus infection was 1.62 ± 1.01, with a minimum of 1 and a maximum of 7 subjects in the family (Table 1).
Table 1. Demographic characteristics of Covid-19 survived patients (n = 205).
| characteristics | Frequency | Percent | |
|---|---|---|---|
| Sex | Male | 128 | 62.4 |
| Female | 77 | 37.6 | |
| Age | <30 | 30 | 14.6 |
| 30-40 | 82 | 40 | |
| 41-50 | 51 | 24.9 | |
| >50 | 42 | 20.5 | |
| Educational level | Less than diploma | 41 | 20 |
| Diploma | 57 | 27.8 | |
| Bachelor | 57 | 27.8 | |
| Higher Bachelor | 50 | 24.5 | |
| Duration of hospital stay (in days) | 1 | 55 | 26.8 |
| 2-10 | 55 | 26.8 | |
| 11-20 | 60 | 29.3 | |
| >20 | 35 | 17.1 | |
| Number of infected people in family | 1 | 129 | 62.9 |
| 2 | 46 | 22.4 | |
| >2 | 30 | 14.6 |
Before analyzing the data, the Mahalanobis distance index was evaluated to assess the absence of multivariate outlier data. According to this index, there was no outlier data. In examining the univariate normality, the distribution status of the observed variables in the model, i.e., the components of the leading research variables, was analyzed using the skewness and kurtosis indices in Table 2. According to Kline,19 the absolute value of skewness less than 3 and the total value of kurtosis value less than 10 indicate the absence of a data problem in univariate normality.
Table 2. Descriptive indicators of illness perception scores, patient health, and psychological hardiness in various dimensions (n = 205).
| characteristics | Mean ± SD | Min-Max | Skewness | Kurtosis |
|---|---|---|---|---|
| Hardiness | 33.42±13.65 | 1-59 | -0.137 | -0.739 |
| Commitment | 15.03±6.17 | 1-27 | -0.108 | -0.674 |
| Control | 12.02±5.57 | 0-21 | -0.203 | -0.924 |
| Challenge | 6.36±3.93 | 0-12 | -0.078 | -0.1.220 |
| Illness perception | 41.82±14.89 | 0-77 | -0.112 | -0.172 |
| Patient Health | 9.67±5.70 | 0-27 | 0.724 | 0.062 |
Table 2, which shows the skewness and kurtosis indices of the research variables in the structural model. The absolute value of skewness is not greater than 3 for any of the variables. Similarly, the absolute value of kurtosis is not greater than 10 for any of the variables. Therefore, according to Kline,19 the administration of this analysis is flawless in terms of univariate normality. Table 3 shows the Pearson correlation between illness perception, patient health, and psychological hardiness scores in various dimensions.
Table 3. Correlation coefficient between illness perception, patient health and psychological hardiness and its dimensions in Covid-19 survived patients (n = 205).
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. Hardiness | 1 | |||||
| 2. Commitment | 0.892** | 1 | ||||
| 3. Control | 0.916** | 0.725** | 1 | |||
| 4. Challenge | 0.769** | 0.498** | 0.624** | 1 | ||
| 5. Illness perception | -0.148* | -0.219** | -0.079 | -0.055 | 1 | |
| 6. Patient Health | -0.418** | -0.529** | -0.280** | -0.223** | 0.290** | 1 |
**P<0.01, *P<0.05
According to the results of Table 3, there is a significant and positive relationship between psychological hardiness and sub-components of commitment, control, and challenge (P<0.01). There is a significant negative relationship between psychological hardiness and patient health (P<0.01) and illness perception (P<0.05).
The maximum likelihood method was used to evaluate the structural model and fitting it to the collected data. In this study, Mardia’s normalized multivariate kurtosis value was used to check multivariate normality. This value was 10.66 in the present study, which is less than 15 and is calculated by the p (p + 2) formula. In this formula, p is equal to the number of latent variables in the model, 3 in this study.20 To determine the fitting of the proposed research model, the indicators suggested by Meyers, Gamst, and Guarino21(p559) were used, the values of which are reported in Table 4. By testing this model, it was decided to answer whether the structural relationship between psychological hardiness and patient health fits through the mediating role of illness perception of Covid-19 survived patients?
Table 4. Fit indices of the primary and modified model.
| Models | χ2 | df | P-value | χ2/df | RMSEA | PNFI | CFI | PCFI | IFI | GFI |
| Primary model | 609.13 | 169 | 0.0001 | 3.640 | 0.095 | 0.570 | 0.807 | 0.629 | 0.811 | 0.881 |
| Improved model | 380.16 | 154 | 0.0001 | 2.469 | 0.075 | 0.629 | 0.950 | 0.689 | 0.953 | 0.964 |
*Abbreviations; CFA: Confirmatory Factor Analysis; CMIN/DF: Chi-square/degree-of-freedom ratio; RMSEA: Root Mean Square Error of Approximation; PCFI: Parsimonious Comparative Fit Index; GFI: Goodness of Fit Index; PNFI: Parsimonious Normed Fit Index; IFI: Incremental Fit Index; CFI: Comparative Fit Index. Fit indices: PNFI, PCFI (>.5), CFI, IFI, GFI (>.9), RMSEA (<0.05 good,0.05-0.08 accept, 0.08-0.1 marginal), CMIN/DF (< 3 good, <5 acceptable).
Before examining the structural coefficients, the fit of the original model was evaluated. The initial/original model fit was assessed based on the introduced fitness indicators21(p559) Although the values of some fitness indicators indicate the acceptable fit of the originally proposed model with the data, to enhance the proposed model’s fit, another analysis of the data was performed by releasing several covariance errors and the final/improved model was presented (Figure 1). The fit indices of these patterns are shown in Table 4.
Figure 1. Standard coefficients of the proposed model of the relationship between structural hardiness and patient health through mediation of illness perception in Covid-19 survived patients.
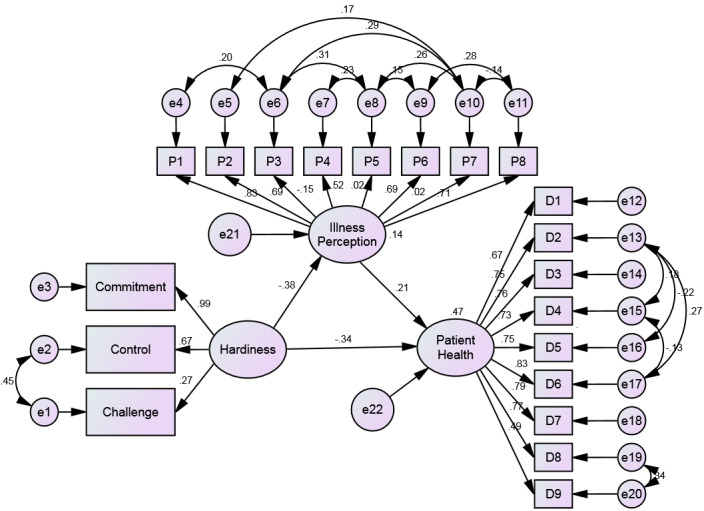
Table 3 shows that the proposed model has a relatively good fit, but a better fit was achieved by releasing several covariance errors (modified/improved model). The R2 index demonstrates the amount of explained variance by the latent endogenous variable. The coefficient of determination of patients’ health variables is 0.471, which shows that exogenous and mediator variables, i.e., psychological hardiness and illness perception respectively, can predict 47% of the changes in the health status of Covid-19 survived patients, which this value is mediocre. Table 5 shows the standard coefficients of the paths, and Figure 1 also illustrates the improved/modified model.
Table 5. Standardized Path Coefficients of the Improved/Modified model.
| Path | Estimate | S.E. | C.R. | P-value |
|---|---|---|---|---|
| Hardiness → Illness Perception | -0.380 | 0.217 | -4.932 | < 0.001 |
| Illness Perception → Patient Health | 0.213 | 0.032 | 2.632 | 0.008 |
| Hardiness → Patient Health | -0.339 | 0.087 | -4.416 | < 0.001 |
The direct relationship between the research variables in the proposed model shows that, in general, all the path coefficients between the variables are statistically significant. In the improved/modified research model, the relationship between psychological hardiness and patient health and illness perception was negative and significant (P<0.001). The relationship between patients’ health and illness perception was positive and significant (P<0.05). Therefore, according to the standard coefficients and critical values presented in Table 5, all direct paths in the structural model are significant (P<0.001).
Then, to determine the significance of the mediating relationship and the indirect effect of the exogenous variable on the endogenous variable through the mediator variable, the Bootstrap analysis was used in Preacher and Hayes’ Macro program18 in SPSS-22 software. 95% confidence intervals and 5000 Bootstrap re-samplings were considered. The lower bound of the confidence interval for illness perception as the mediator variable between psychological hardiness and patient health is (-0.073), and the upper bound is (-0.002) (95% CI: -0.073 to -0.002). Given that zero is outside of this interval and it is statistically significant (Standardized β= -0.0034, SE= 0.018, P<0.001), the illness perception mediates the relationships between psychological hardiness and patient health.
Discussion
This study aimed to determine the mediating role of illness perception in the relationship between psychological hardiness and health status of Covid-19 survived patients in Qom city. The study’s first results showed an inverse relationship between psychological hardiness and the health status of Covid-19 survived patients. This reverse relationship means that patients with poorer scores on psychological hardiness reported higher scores on depression and vice versa. As psychological hardiness is a source of resilience to stressful life events, irresistible people are the ones who can control life events, change the stressors, be committed to the activities they undertake, and expect this change to be an exciting challenge for further growth.22,23 Therefore, psychological hardiness plays an effective role in people’s mental health.
The second study result showed that illness perception has a positive and direct statistical effect on the health status of patients. That is, with increasing illness perception, the rate of depression increases in participants. In explaining this relationship, it should be noted that the illness perception in individuals is based on getting information from different sources and the patient’s beliefs. Individual’s Interpretation, perception, and experience of illness and his/her emotional and behavioral responses to the disease determine his/her coping strategy and quality of life.24,25 During the daily pandemic, people receive stressful news through the media, such as an increase in the number of deaths, the unknown nature of the virus, and the lack of specific treatment, which led to a negative illness perception. Previous researches have also consistently identified the role of illness perception as a cognitive factor that can significantly impair a person’s ability to manage a disease.26,27 These results are consistent with the third finding of the study, which shows that the relationship between psychological hardiness and illness perception is reversed, i.e., increasing negative illness perception reduces the criteria of psychological hardiness.
The model-fitting results in this study show that illness perception plays a mediating role in the relationship between hardiness and a patient’s health. When illness perception was introduced as a mediating variable to the structural model, it played a destructive role and reduced the relationship between psychological hardiness and patient health. In other words, this mediating variable significantly prevents the positive effects of hardiness on improving patients’ health in the present study. This result suggests that the task of mental health professionals to intervene in patients with Covid-19 is to reveal to them that anxiety and stress caused by coronavirus reduce psychological hardiness and decrease patients’ ability to cope with the effects of the disease. To minimize the negative impact of the illness perception and increase the positive impact of hardiness on the health of patients, it is also important for health psychologist to modify their perception of Covid-19 disease, especially in terms of duration and control that a person can have to protect him/herself and educate patients to control their emotional coronavirus responses.
In performing the present study, there are limitations, such as restricting the sample to the Qom city, which makes the generalization of the results challenging. Furthermore, the present study’s design is descriptive and correlational, and the measurements are solely based on self-report questionnaire tools that prevent causal inferences and comprehensive assessments.
Conclusion
The findings of this study emphasize the need to increase public awareness through the media to improve Covid-19 perception, resolve suspicions about coronavirus, and clarify false information. On the other hand, due to the direct connection of the medical personnel with the affected people, the medical staff knowledge of the patient’s psychological condition can be effective in reducing the psychological effects of this disease because it was found that the decline in patients’ hardiness was associated with their health deterioration.
References
- 1. Zulkifli NA, Sivapatham S, Guan NC. Brief Psychotic Disorder in Relation to Coronavirus, COVID-19 Outbreaks: A Case Report. Malaysian Journal of Psychiatry. 2020;29(1).
- 2. Ko CH, Yen CF, Yen JY, Yang MJ. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry Clin Neurosci. 2006;60(4):397-403. doi:10.1111/j.1440-1819.2006.01522.x [DOI] [PubMed]
- 3. Taha S, Matheson K, Cronin T, Anisman H. Intolerance of uncertainty, appraisals, coping, and anxiety: The case of the 2009 H1N1 pandemic. Br J Health Psychol. 2014;19(3):592-605. doi:10.1111/bjhp.12058 [DOI] [PubMed]
- 4. Wang Y, Xu B, Zhao G, Cao R, He X, Fu S. Is quarantine related to immediate negative psychological consequences during the 2009 H1N1 epidemic? General Hospital Psychiatry. 2011;33(1):75-77. doi:10.1016/j.genhosppsych.2010.11.001 [DOI] [PubMed]
- 5. Lee SM, Kang WS, Cho AR, Kim T, Park JK. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Comprehensive Psychiatry. 2018;87:123-127. doi:10.1016/j.comppsych.2018.10.003 [DOI] [PMC free article] [PubMed]
- 6. Elizarrarás-Rivas J, Vargas-Mendoza JE, Mayoral-García M, et al. Psychological response of family members of patients hospitalised for influenza A/H1N1 in Oaxaca, Mexico. BMC Psychiatry. 2010;10(1):104. doi:10.1186/1471-244x-10-104 [DOI] [PMC free article] [PubMed]
- 7. Li S, Wang Y, Xue J, Zhao N, Zhu T. The impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo users. IJERPH. 2020;17(6):2032. doi:10.3390/ijerph17062032 [DOI] [PMC free article] [PubMed]
- 8. Kobasa SC, Maddi SR, Zola MA. Type A and hardiness. J Behav Med. 1983;6(1):41-51. doi:10.1007/bf00845275 [DOI] [PubMed]
- 9. Ghafourian-Boroujerdnia M, Shiravi Z, Hamid N, Hemmati AA, Kooti W. The Relationship of Hardiness and Immune System Cells. Journal of Isfahan Medical School. 2014;31(260).
- 10. Petrie KJ, Jago LA, Devcich DA. The role of illness perceptions in patients with medical conditions. Current Opinion in Psychiatry. 2007;20(2):163-167. doi:10.1097/yco.0b013e328014a871 [DOI] [PubMed]
- 11. Moss-Morris R, Chalder T. Illness perceptions and levels of disability in patients with chronic fatigue syndrome and rheumatoid arthritis. Journal of Psychosomatic Research. 2003;55(4):305-308. doi:10.1016/s0022-3999(03)00013-8 [DOI] [PubMed]
- 12. Goodyear MDE, Krleza-Jeric K, Lemmens T. The Declaration of Helsinki. BMJ (Clinical research ed). 2007;335(7621):624-625. doi:10.1136/bmj.39339.610000.be [DOI] [PMC free article] [PubMed]
- 13. Kobasa SC. The hardy personality: Toward a social psychology of stress and health. Social psychology of health and illness. 1982;4:3-32.
- 14. Zare H, Aminpour H. Psychological tests. Tehran, Aeezh. Published 2011. http://opac.nlai.ir/opac-prod/bibliographic/2537151
- 15. Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. Journal of Psychosomatic Research. 2006;60(6):631-637. doi:10.1016/j.jpsychores.2005.10.020 [DOI] [PubMed]
- 16. Bazzazian S, Besharat MA. Attachment styles, illness perception and quality of life in patients with type I diabetes. J Contemporary. 2010;5(1):3-11. doi:10.1016/j.sbspro.2010.07.217
- 17. Ardestani MS, Ashtiani RD, Rezaei Z, Vasegh S, Gudarzi SS. Validation of Persian version of PHQ-9 for diagnosis of major depressive episode in psychiatric wards in IRAN. International Journal of Applied Behavioral Sciences. 2019;5(2):1-8. doi:10.22037/ijabs.v5i2.21094
- 18. Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879-891. doi:10.3758/brm.40.3.879 [DOI] [PubMed]
- 19. Kline R. Data Preparation and Psychometrics Review. Principles and Practice of Structural Equation Modeling. 4th ed. Guilford; 2016:64-96.
- 20. Teo T, Noyes J. Explaining the intention to use technology among pre-service teachers: a multi-group analysis of the Unified Theory of Acceptance and Use of Technology. Interactive Learning Environments. 2014;22(1):51-66. doi:10.1080/10494820.2011.641674
- 21. Meyers LS, Gamst G, Guarino AJ. Applied Multivariate Research: Design and Interpretation. Sage publications; 2006.
- 22. Kobasa SC. tressful life events, personality, and health: an inquiry into hardiness. Journal of Personality and Social Psychology. 1979;37(1):1. doi:10.1007/bf00845275 [DOI] [PubMed]
- 23. Tadayon M, Dabirizadeh S, Zarea K, Behroozi N, Haghighizadeh MH. Investigating the relationship between psychological hardiness and resilience with depression in women with breast cancer. The Gulf Journal of Oncology. 2018;1(28):23-30. [PubMed]
- 24. Karabulutlu Y, Okanli A. The evaluation of illness perceptions in hemodialysis patients. Journal of Anatolia Nursing and Health. 2011;14:25-30. doi:10.29252/ijn.30.108.60
- 25. Uysal Y, Akpinar E. Illness perception and depression of type 2 diabetic patients. Cukurova Medical Journal. 2013;38(1):31-40.
- 26. Vaughan R, Morrison L, Miller E. The illness representations of multiple sclerosis and their relations to outcome. British journal of health psychology. 2003;8(3):287-301. doi:10.1348/135910703322370860 [DOI] [PubMed]
- 27. Cooper A, Lloyd G, Weinman J, Jackson G. Why patients do not attend cardiac rehabilitation: role of intentions and illness beliefs. Heart. 1999;82(2):234-236. doi:10.1136/hrt.82.2.234 [DOI] [PMC free article] [PubMed]


