Abstract
Research question
Does the BNT162b2 COVID-19 vaccine affect sperm parameters of patients with a normal or an abnormal semen analysis?
Design
Data were collected from male patients undergoing IVF treatment after completing vaccination between February 2021 and June 2021 (post-vaccine). For comparison, records of the same patients were reviewed before the vaccination (pre-vaccine) back to January 2017. Patients with azoospermia were excluded. Sperm parameters were compared between pre- and post-vaccine groups. Each patient served as self-control.
Results
Seventy-two patients were included in the study (median interquartile range [IQR] age 35.7 [33.0–43.0] years), of whom 57 had a normal semen analysis. The time between the first vaccine and the post-vaccine sperm analysis was 71.0 (40.5–104.8) days. The sperm parameters before and after the vaccination were as follows: sperm volume before 3.0 (2.0–4.0) and after 3.0 (1.6–3.9) ml, P = 0.02; sperm concentration before 26.5 (14.0–64.7) and after 31.0 (14.2–80.0) 106/ml, P = 0.35; and total motile sperm count before 33.7 (9.0–66.0) and after 29 (6.0–97.5)106, P = 0.96. Sub-group analyses were conducted for patients with male infertility and patients with a normal semen analysis. Neither of the sub-groups showed significant changes after vaccination.
Conclusion
Sperm parameters showed no significant changes after vaccination among men with a normal and abnormal semen analysis. Therefore, the BNT162b2 vaccine does not seem to affect sperm parameters. The preliminary results are reassuring for the entire global population, currently undergoing intense vaccination campaigns against COVID-19.
KEYWORDS: BNT162b2 vaccine, COVID-19; Male fertility; SARS-CoV-2; Sperm
Introduction
A novel coronavirus emerged in December 2019 (Zhu et al., 2020), causing severe acute respiratory syndrome coronavirus 2, termed SARS-CoV-2 or coronavirus disease 2019 (COVID-19). This pandemic illness spread to millions of people worldwide, causing severe disease and widespread death, with devastating medical, economic and social consequences (Polack et al., 2020). As a result, intense international efforts were made to rapidly develop a vaccine to eliminate or mitigate the effects of COVID-19. The BNT162b2 vaccine by BioNTech and Pfizer was one of the first vaccines that received emergency use authorization by the US Food and Drug Administration and was shown to be highly effective in reducing infection rates and rates of severe illness (Dagan et al., 2021). In a large trial, the two-dose regimen of BNT162b2 was assessed and found to confer 95% protection against SARS-CoV-2 in people aged 16 years and older (Dagan et al., 2021). The vaccine's safety was assessed using self-reporting of local and systemic adverse events, the use of antipyretic or pain medication and unsolicited serious adverse events; a favourable safety profile was confirmed (Polack et al., 2020; Walsh et al., 2020). Accordingly, mass vaccination campaigns have been carried out globally with the recommendation to vaccinate the entire population from age 16 years upwards (Dagan et al., 2021).
Among the possible non-respiratory influences of COVID-19 is the effect of the virus on male fertility. Indeed, recent evidence suggests a substantial negative effect, as shown by histopathological examinations of autopsied testes after COVID-19 infection showing oedema, congestion, inflammation, thinning and injury of the seminiferous tubules (Li et al., 2020; Yang et al., 2020). Nevertheless, the vaccination pace in many countries is slower than expected, partially because of public fear of possible adverse effects and the potentially negative long-term effect of the vaccine (Lo Re et al., 2021). Despite no evidence of a negative effect on male or female fertility, as stressed by the Association of Reproductive and Clinical Scientists (Iacobucci, 2021) and the British Fertility Society (RCOG webinar series), many people are still hesitant to receive the vaccine owing to fertility concerns (Diaz et al., 2021). Hence, the aim of the present study was to investigate the effect of the BNT162b2 COVID-19 vaccine on sperm parameters among men, including men with fertility issues and impaired initial sperm parameters. The hypothesis was that the vaccine would not affect sperm quality.
Materials and methods
The present study was carried out in a large tertiary centre. The effect of BNT162b2 mRNA Covid-19 vaccine, a nucleoside-modified RNA vaccine developed by BioNTech and Pfizer, was assessed. Our medical centre is a university hospital with an IVF unit, which runs an average of 1000 fresh IVF cycles per year. Data were collected from patients in the IVF unit between 2 February and 21 June 2021, after the vaccinations became available for the population aged 16 years and older. To isolate the vaccine's effect and avoid confounding, patients with prior infection by COVID-19 were excluded from the study. Patients with azoospermia, or who had not completed two doses of vaccination, were also excluded from the study. Sperm parameters of patients who had received two doses of the BNT162b2 vaccine were collected (post-vaccine) and compared with the same patient's retrospective data before vaccination (pre-vaccine) using the hospital's electronic database. Retrospective data were collected back to 1 January 2017, before vaccination was available and before electronic data were available on our system. Only patients with two available full semen analyses before the vaccine were included; these patients were allocated to the subgroups based on these two analyses. The parameters of the most recent semen analyses were included in the study. To minimize bias, each patient served as self-control before and after vaccination. None of the patients were prescribed medications aiming to improve sperm analyses, during the study time frame.
Data obtained included patient demographics (age), indication for IVF treatment, i.e. women or male factor, unexplained infertility, fertility preservation and need for preimplantation genetic testing, sperm parameters (volume, concentration, and motility) and time since the first dose of vaccine. The second vaccine dose was given as recommended, 21 days after the first dose (Walsh et al., 2020; Dagan et al., 2021). Male factor was defined as one or more sperm abnormality (volume, concentration or motility) as per the World Health Organization criteria (Cooper et al., 2010) in at least two available semen analyses carried out at least 6 weeks apart. Semen analyses were carried out according to the World Health Organization laboratory manual and processed and examined by an experienced technician. A small drop of semen was transferred to the centre of a Makler counting chamber (Sefi Medical Instruments, Haifa, Israel) and analysed under a 400X microscope.
The primary outcome was the difference in sperm parameters between the pre- and post-vaccination groups. Sub-group analyses were conducted for patients with male infertility and patients with normal sperm analysis results undergoing IVF for indications other than male infertility. The vaccination rate among the male population undergoing IVF treatment was also assessed.
Statistical analysis
Patient characteristics are described as proportions for categorical variables, and median and interquartile range (IQR) for continuous variables. The significance of the differences between the pre- and post-vaccine groups was assessed using the Wilcoxon signed rank test. To assess the effect of the BNT162b2 vaccine based on the initial sperm parameters, sub-group analyses were carried out for patients with male infertility, as well as for patients with a normal semen analysis. A two-sided P < 0.05 indicated statistical significance. Statistical Product and Service Solutions (IBM SPSS version 25, IBM Corp, Armonk, NY) was used for data analysis.
Ethics approval
Approval was obtained from our medical center's Institutional Review Board on 12 April 2021 (reference: 0092-21-HMO), but requirement for written informed consent was waived.
Results
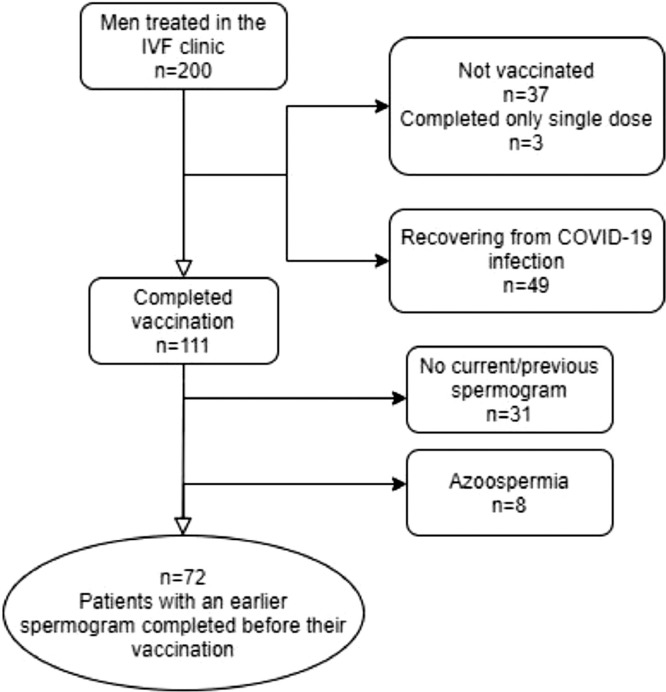
During the study period, 200 men were treated in our IVF unit. Most of them (56%) had completed the two doses of the BNT162b2 vaccine. Almost 25% (n = 49) had a prior history of SARS-CoV-2 infection, whereas 76 % (n = 151) were eligible for vaccination. In this subgroup of men who were eligible for vaccination, 74% (n = 111) had completed the two vaccine doses, 2% (n = 3) had received only one dose and 25% (n = 37) were not vaccinated for COVID-19.
A flow chart describing the study's patient inclusion protocol is presented in Figure 1 . The final cohort included a total of 72 men; their demographic data and indications for undergoing IVF are presented in Table 1 . When considering their original sperm parameters, 57 patients had a normal semen analysis, and 15 patients underwent IVF because of male factor issues. The median (interquartile range [IQR]) interval between the first vaccine dose and the second sperm analysis (post-vaccine group) was 71.0 (40.5–104.8) days.
Figure 1.
Patients included in the study.
TABLE 1.
PATIENT CHARACTERISTICS AND INDICATIONS FOR IVF
| Variables | Values |
|---|---|
| Age, years | 35.7 (33.0–43.0) |
| Time from the first vaccine dose to the second sperm analysis, days | 71.0 (40.5–104.8) |
| Time interval between the pre- and post-vaccination semen analyses, days | 244.0 (125.6–448.5) |
| Indication for IVF, n (%) | |
| Male | 15 (20.8) |
| Women | |
| Preimplantation genetic testing | 8 (11.1) |
| Low ovarian reserve | 19 (26.4) |
| Mechanical | 9 (12.5) |
| Ovulation | 2 (2.8) |
| Fertility preservation | 3 (4.2) |
| Unexplained | 16 (22.2) |
Variables are expressed as median (interquartile range) or %.
Semen analysis parameters are presented in Table 2 . Except sperm volume, none of the parameters differed significantly after vaccination resulting in a volume of (3.0 [2.0–4.0]) ml versus 3.0 [1.6–3.9], P = 0.02), a sperm concentration of (26.5 [14.0–64.7] 106/ml versus 31.0 [14.2–80.0], P = 0.35) and a total motile sperm count of 33.7 (9.0–66.0) 106 versus 29 (6.0–97.5) 106, P = 0.96), in the pre- and post-vaccination groups, respectively (median [IQR]). No significant differences were found in the sub-group analyses of patients with male infertility and with a normal semen analysis. All the sperm parameters for patients with normospermia (n = 57) and patients with male infertility (n = 15) were similar in the pre- and post-vaccinated groups (Table 2).
TABLE 2.
SPERM ANALYSIS PARAMETERS BEFORE AND AFTER BNT162B2 VACCINATION
| Variables | Pre-vaccination | Post-vaccination | P-value |
|---|---|---|---|
| All patients (n = 72) | |||
| Semen volume, ml | 3.0 (2.0–4.0) | 3.0 (1.6–3.9) | 0.02 |
| Sperm concentration, 106/ml | 26.5 (14.0–64.7) | 31.0 (14.2–80.0) | 0.35 |
| Total motile sperm count, 106 | 33.7 (9.0–66.0) | 29 (6.0–97.5) | 0.96 |
| Patients with normospermia (n = 57) | |||
| Semen volume, ml | 3.0 (2.0–4.2) | 2.7 (1.6–4.0) | 0.05 |
| Sperm concentration, 106/ml | 35.0 (20.5–75.0) | 37.0 (17.0–100.0) | 0.36 |
| Total motile sperm count, 106 | 41.9 (15.1–86.8) | 40.0 (16.0–120.) | 0.97 |
| Patients with male infertility (n = 15) | |||
| Semen volume, ml | 3.0 (2.4–4.0) | 3.0 (1.5–3.4) | 0.16 |
| Sperm concentration, 106/ml | 5.5 (2.3–25.0) | 7.0 (1.0–25.0) | 0.65 |
| Total motile sperm count, 106 | 5.0 (0.7–15.8) | 2.7 (0.9–20.7) | 0.88 |
Variables are expressed as median (interquartile range).
Discussion
The main finding of the present study is that the BNT162b2 vaccine does not affect sperm parameters. This was found to be true both for men with normospermia and for those with abnormal semen parameters.
Two recent studies showed no significant decrease in any sperm parameter after vaccination (Gonzalez et al., 2021; Lifshitz et al., 2021). Our group of patients, who are already facing fertility challenges, may be especially hesitant to receive the COVID-19 vaccine. Our results are, therefore, encouraging and may counteract the fears of many to receiving the vaccine. Moreover, given the potential negative effect of COVID-19 infection on male fertility (Li et al., 2020; Yang et al., 2020), vaccination against COVID-19 may even prevent many infertility cases. Of note, although the change in sperm volume between before and after the vaccination was statistically significant, as the median volume has not changed and as total motile sperm count did not differ between before and after the vaccination, we believe that this finding is not clinically relevant.
Our study has several limitations. The main limitation is the retrospective data collection of the sperm parameters of the pre-vaccine group. We included, however, only patients with two available full semen analyses before the vaccine, allowing for accurate pre-vaccine information. Another limitation of the study is the relatively long interval between the pre- and post-vaccination semen analyses. Although each patient had two semen analyses before vaccination, it is still possible that semen characteristics have changed over time. Additionally, the methodology in which each patient served as his own self-control strengthens the results and provides reliable answers to the questions raised regarding the effects of BNT162b2 vaccination on sperm parameters. As spermatogenesis takes approximately 3 months, our study was able to assess only the short-term effect of the vaccine; therefore, later sequalae is still possible. Moreover, data on pregnancy outcomes were not available. Nevertheless, we believe that our findings will reassure and encourage vaccination among the young population.
The BNT162b2 vaccine was launched only months ago, and worldwide vaccination is still ongoing, with health organizations strongly advocating for the public to receive the vaccine. In our study sample, only 58% of the men who applied for IVF were vaccinated against SARS-CoV-2. A much lower rate than the national average of 71–85% for the age group 20–49 years (Israel Ministry of Health), possibly owing to concerns about adverse effects of the vaccine on the fertility of young men. Furthermore, a recent study has shown that COVID-19 vaccine hesitancy is directly linked to increased internet search queries for side-effects on fertility (Diaz et al., 2021). Therefore, our results of no change in sperm parameters after vaccination among men with normal and abnormal semen analysis can reassure the young male population being vaccinated worldwide that their fears are unfounded.
Biography

Myriam Safrai obtained a BSc in Biology from the Hebrew University, graduating with excellence. She later studied medicine in the same institution and completed her residency in obstetrics and gynaecology at the Hadassah Hebrew University Medical Center. She is currently undertaking a fertility fellowship in the same institution.
Key message.
This research includes the largest cohort reported and is the first to assess the effect of the BNT162b2 vaccine on sperm parameters of men with impaired sperm parameters. The vaccine does not affect sperm parameters among men with a normal or abnormal semen analysis. This result should reduce vaccine hesitancy.
Alt-text: Unlabelled box
Declaration: The authors report no financial or commercial conflicts of interest.
References
- Cooper, T.G., Noonan, E., Von Eckardstein, S., Auger, J., Gordon Baker, H.W., Behre, H.M., Haugen, T.B., Kruger, T., Wang, C., Mbizvo, M.T., Vogelsong, K.M., 2010. World Health Organization reference values for human semen characteristics * ‡. Advanced Access publication on November 16, 231–245. https://doi.org/10.1093/humupd/dmp048 [DOI] [PubMed]
- Dagan N., Barda N., Kepten E., Miron O., Perchik S., Katz M.A., Hernán M.A., Lipsitch M., Reis B., Balicer R.D. BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. New England Journal of Medicine. 2021 doi: 10.1056/NEJMoa2101765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz P., Reddy P., Ramasahayam R., Kuchakulla M., Ramasamy R. COVID-19 vaccine hesitancy linked to increased internet search queries for side effects on fertility potential in the initial rollout phase following Emergency Use Authorization. Andrologia. 2021 doi: 10.1111/and.14156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez D.C., Nassau D.E., Khodamoradi K., Ibrahim E., Blachman-Braun R., Ory J., Ramasamy R. Sperm Parameters Before and After COVID-19 mRNA Vaccination. JAMA. 2021 doi: 10.1001/jama.2021.9976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacobucci G. Covid-19: No evidence that vaccines can affect fertility, says new guidance. BMJ (Clinical research ed.) 2021;372:n509. doi: 10.1136/bmj.n509. [DOI] [PubMed] [Google Scholar]
- Li H., Xiao X., Zhang J., Zafar M.I., Wu C., Long Y., Lu W., Pan F., Meng T., Zhao K., Zhou L., Shen S., Liu L., Liu Q., Xiong C. Impaired spermatogenesis in COVID-19 patients. EClinicalMedicine. 2020;28 doi: 10.1016/j.eclinm.2020.100604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lifshitz, D., Haas, J., Lebovitz, O., Raviv, G., Orvieto, R., Aizer, A. 2021. Does mRNA SARS-CoV-2 vaccine detrimentally affect male fertility, as reflected by semen analysis? https://doi.org/10.1016/j [DOI] [PMC free article] [PubMed]
- Lo Re V., Klungel O.H., Chan K.A., Panozzo C.A., Zhou W., Winterstein A.G. Global covid-19 vaccine rollout and safety surveillance—how to keep pace. BMJ. 2021;373:n1416. doi: 10.1136/bmj.n1416. [DOI] [PubMed] [Google Scholar]
- Polack F.P., Thomas S.J., Kitchin N., Absalon J., Gurtman A., Lockhart S., Perez J.L., Pérez Marc G., Moreira E.D., Zerbini C. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. New England Journal of Medicine. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh E.E., Frenck R.W., Jr, Falsey A.R., Kitchin N., Absalon J., Gurtman A., Lockhart S., Neuzil K., Mulligan M.J., Bailey R. Safety and immunogenicity of two RNA-based Covid-19 vaccine candidates. New England Journal of Medicine. 2020;383:2439–2450. doi: 10.1056/NEJMoa2027906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang M., Chen S., Huang B., Zhong J.M., Su H., Chen Y.J., Cao Q., Ma L., He J., Li X.F., Li X., Zhou J.J., Fan J., Luo D.J., Chang X.N., Arkun K., Zhou M., Nie X. Pathological Findings in the Testes of COVID-19 Patients: Clinical Implications. European Urology Focus. 2020;6:1124–1129. doi: 10.1016/j.euf.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P., Zhan F., Ma X., Wang D., Xu W., Wu G., Gao G.F., Tan W. A Novel Coronavirus from Patients with Pneumonia in China, 2019. New England Journal of Medicine. 2020;382:727–733. doi: 10.1056/nejmoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]