Abstract
Background
There is widespread concern regarding how the COVID-19 pandemic has affected mental health. Emerging meta-analyses suggest that the impact on anxiety/depression may have been transient, but much of the included literature has major methodological limitations. Addressing this topic rigorously requires longitudinal data of sufficient scope and scale, controlling for contextual variables, with baseline data immediately pre-pandemic.
Aims
To analyse self-report of symptom frequency from two largely UK-based longitudinal cohorts: Cohort 1 (N = 10,475, two time-points: winter pre-pandemic to UK first winter resurgence), and Cohort 2 (N = 10,391, two time-points, peak first wave to UK first winter resurgence).
Method
Multinomial logistic regression applied at the item level identified sub-populations with greater probability of change in mental health symptoms. Permutation analyses characterised changes in symptom frequency distributions. Cross group differences in symptom stability were evaluated via entropy of response transitions.
Results
Anxiety was the most affected aspect of mental health. The profiles of change in mood symptoms was less favourable for females and older adults. Those with pre-existing psychiatric diagnoses showed substantially higher probability of very frequent symptoms pre-pandemic and elevated risk of transitioning to the highest levels of symptoms during the pandemic. Elevated mental health symptoms were evident across intra-COVID timepoints in Cohort 2.
Conclusions
These findings suggest that mental health has been negatively affected by the pandemic, including in a sustained fashion beyond the first UK lockdown into the first winter resurgence. Women, and older adults, were more affected relative to their own baselines. Those with diagnoses of psychiatric conditions were more likely to experience transition to the highest levels of symptom frequency.
Keywords: SARS-CoV-2, COVID, Well-being, Anxiety, Depression, Sleep, Fatigue, Insomnia
1. Introduction
The COVID-19 pandemic has led to profound changes in society and the ways that people live their lives. There are major concerns about the potential negative impact of the pandemic (including lockdown) on common mental health symptoms, both at the level of the general population, and in terms of vulnerable groups: such as individuals with pre-existing conditions, or from particular age groups [[1], [2], [3]]. Across the range of mental health domains, anxiety and depressive symptoms are particularly pertinent at the global public health level, due to their high prevalence and burden ranking amongst the highest of all mental disorders (and brain disorders more widely), and direct contextual relevance to the pandemic. Access to clinical support for people with these conditions has been severely disrupted [4]. Some studies suggest the negative impact of the pandemic on mood/anxiety may have been transient in the UK and elsewhere e.g. [5]; and this is also suggested by emerging meta-analyses e.g. [6]. However, addressing the impact of the pandemic on common mental health symptoms based on the current literature is challenging. The unexpected nature of the pandemic means that much of the longitudinal research has been hindered by inherent design limitations. Studies have commonly lacked true baseline data collected immediately before the pandemic (instead relying on historical data; e.g. several years out-of-date); fail to control for seasonal variation in mood; have under-recruited minority and other vulnerable groups; and have analysed a relatively narrow set of contextual variables [6]. Additionally, in our recent cross-sectional work, conducted at very-large scale, specific aspects of depression/anxiety symptoms were found to have been impacted in different ways in different sub-populations [3]. It therefore appears important to consider item-level data, rather than composite symptom scores. Achieving this in a rigorous way requires more complex statistical approaches and larger sample sizes, due to the (often overlooked) fact that mental health item responses are typically on an ordinal non-linear scale, with implications for transition probabilities from different start points.
Here, we leveraged a longitudinal platform collecting data from large numbers of individuals in the UK, instigated as a collaboration with BBC2 Horizon. There were two cohorts: Cohort 1, who provided baseline data in the period immediately prior to the emergence of the pandemic in the UK (December 2019–February 2020) then again at the time of first UK (winter) resurgence (December-2020 to January 2021); and Cohort 2, who instead provided baseline data during the period of the first UK lockdown (May 2020), and likewise during the first UK resurgence (December-2020 to January 2021). This allowed examination not only of lasting pandemic-related changes in mental health symptoms over a 1-year timescale as a function of rich contextual variables (Cohort 1), but also whether there was habituation of such effects (Cohort 2). Based on the existing literature and data, we hypothesised that: the COVID-19 pandemic (1) resulted in an initial global increase in anxiety across the general population relative to the pre-pandemic baseline (i.e., as measured in Cohort 1) (2) the magnitude of mental health changes would be larger in specific subgroups of participants (e.g. older people, females, people in certain work and home contexts, and those reporting pre-existing mental disorder(s)); and (3) that exacerbation of anxiety would reduce over time (e.g., across timepoints in Cohort 2). To test these hypotheses, we first examined global changes in the self-reported frequency of item-level mood and anxiety symptoms in both cohorts. We then applied multinomial logistic regression to identify which amongst a broad set of population variables were longitudinally predictive of the probability of increase vs. decrease in symptom frequency across time. Finally, we implemented an innovative nonparametric permutation-based approach to explore in detail the nature of changes in reported mental health symptoms (transitions) for both clinical and non-clinical subgroups – specifically exploring the range and predictability of mental health state transitions between different groups.
2. Method
2.1. Data collection
Data collection was conducted in the period of December 2019 through January 2021 as part of a broader citizen science study. Recruitment was via articles describing the study placed on the BBC2 Horizon, BBC Homepage, BBC News homepage and circulated on mobile news meta-apps. These were made prominent in the public eye through two promotional drives, one at the beginning of January 2020 and the other at the beginning of May 2020, producing two large peaks in recruitment in these times points just prior to the emergence of the COVID-19 pandemic in the UK (Cohort 1) and during the first UK lockdown (Cohort 2). The cross-sectional aspect of the study was originally designed to map dimensions of cognition, personality and mood across the broadest possible cross section of the UK general public. With the emergence of the pandemic, we applied for an ethics amendment to include additional follow up timepoints as well as questionnaires on COVID-19 illness [3], cross sectional analyses of which have been reported previously [3,7].
The baseline recruitment materials did not mention COVID-19, thereby mitigating topic-specific selection bias at enrolment. On navigating to the study specific URL, participants conducted an online survey, programmed in HTML5 with JavaScript, hosted on our Cognitron platform (https://gbit.cognitron.co.uk), which supports a diversity of bespoke online studies, and is accessible via practically any mainstream device that has a browser (e.g. smartphones, tablets and personal computers). On completion of the first timepoint, participants were given the option to sign up for future research studies. In order to collect follow up data, emails were sent to all participants who were 16 or over who had signed up During late December 2020-early January 2021, inviting them to take part in a follow up assessment. The current study includes data for all participants who completed the survey at both timepoints. Cross sectional differences between baselines are reported elsewhere [3,7].
2.2. Questionnaire items
Sections included (a) demographics, comprising age in years, sex, handedness, education level, work arrangements, country of residence and first language; (b) self-report of pre-existing diagnosed psychiatric conditions selected via checkbox; (c) five items from the NHS Mood and Anxiety Self-Assessment, corresponding to the first item of the Generalized Anxiety Disorder Assessment (GAD) [8] and four items from the Patient Health Questionnaire (PHQ) [9]. Questions were of the form ‘how often in the past month have you suffered from’ followed by the following items:
-
1.
‘Feeling nervous, anxious or on edge?’
-
2.
‘Feeling down or depressed’
-
3.
‘Feeling tired or having little energy’
-
4.
‘Trouble concentrating on things, such as reading the newspaper or watching television’
-
5.
‘Not being able to get to sleep or stay asleep?’
Participants answered by selecting from a pre-specified set of items pertaining to symptom frequency - specifically: ‘0-Never’, ‘1-Almost never’, ‘2-One or twice a week’, ‘3-Several times a week’, ‘4-Daily’, ‘5-Hourly’, ‘6-More often’. The question pertaining to sleep had a maximum level ‘4-Daily’. Additional mood self-assessment items were collected from the GAD-7 and are available for the mid-lockdown and resurgence timepoints; however, they are not reported here as were not collected at the pre-pandemic timepoint. Response times were collected for all questionnaire items, but these are not analysed here. Participants were able to navigate back and forwards on the questionnaire to change responses if they felt they had made an error, with this behaviour also recorded. Our rationale for using brief versions of symptom rating instruments was to enable maximum participation.
2.3. Data processing and analysis
Data curation, preprocessing, and statistical analyses were conducted in MATLAB R2020a. Preprocessing steps comprised (1) casewise removal of any participants who had missing data for the analysed questions and (2) binning of participants into age decades, with those above the age of 70 collapsed into a single category due to lower subject numbers in the 80+ range. A categorical approach was applied to age data to account for non-linear associations. Outcome measures of interest were responses to the mood self-assessment items. A combination of MATLAB native t-tests and multinomial logistic regression functions was applied in the analyses, alongside custom permutation modelling functions. Details of permutation testing and Entropy analyses are described in the Supplementary Methods.
2.4. Ethics & consent
This study and its procedures complied with the ethical standards and with the Helsinki Declaration of 1975, as revised in 2008. All procedures were approved by the Imperial College Research Ethics Committee (17IC4009). All participants provided informed consent prior to completing the survey. Individuals did not receive payment or other financial-related contributions for taking part.
3. Results
3.1. Study participants
An overview of the characteristics of all study participants is provided in Supplementary Table S1. Within both cohorts, participants included a broad demographic range including minority and vulnerable groups. The two cohorts explored in this study were defined a priori from the dataset based on recruitment date. Participants in Cohort 1 were first tested during the period of time just prior to the pandemic reaching the UK (December 2019–February 2020). Participants in Cohort 2 were first tested around the middle of the first national lockdown in the UK (April 2020–June 2020). Of the 49,103 from Cohort 1 and 46,338 of Cohort 2 who signed up to be recontacted about future studies, 10,475 and 10,391 respectively completed the follow up timepoint in response to a single follow up email, sent in batches during late December 2020 and early January 2021, i.e., at the peak of the winter resurgence. Regarding sampling bias, after transforming response items to a numeric scale (0–6), t-tests of baseline data indicated that those participants who were retained at follow-up showed negligible effect size differences (<0.1SDs for all questions) in mental health measures as compared to those who were not retained at follow up (Supplementary Table S2).
3.2. Change in mental health self-assessment scores over time
In order to explore whether frequency of in mental health symptoms had a prevalent direction of change from the months prior to the pandemic escalating in the UK to winter resurgence one year later (Cohort 1), or between the peak of the first wave and winter resurgence (Cohort 2) we subtracted reported symptom frequency (Supplementary Table S3a-e) quantified on a scale of 0–5 (0 = never 5 = hourly), for timepoint 2 minus timepoint 1, separately for the two cohorts.
Calculating Pearson's r for the item level scores within each timepoint showed medium to large correlations (r ~ = 4 to 7) within baseline and follow up timepoints, and across timepoints (Table 1 ). Notably, the correlations across items in their changes across time were in the small to medium effect size range (r ~ = 2 to 4). Together, this variability supported conducting the main analyses at the item as opposed to composite score level.
Table 1.
Pearson's correlation coefficients for item scores across timepoints, across items at baseline and follow up, and across items for change between baseline and follow up.
| Baseline vs follow up |
Anxiety |
Depression |
Low energy |
Concentration |
Insomnia |
|
|---|---|---|---|---|---|---|
| 0.63 | 0.62 | 0.62 | 0.58 | 0.60 | ||
| Baseline | Anxiety | |||||
| Depression | 0.65 | |||||
| Low energy | 0.50 | 0.60 | ||||
| Concentration | 0.54 | 0.55 | 0.55 | |||
| Insomnia | 0.39 | 0.41 | 0.43 | 0.40 | ||
| Follow up | Anxiety | |||||
| Depression | 0.66 | |||||
| Low energy | 0.54 | 0.65 | ||||
| Concentration | 0.54 | 0.62 | 0.62 | |||
| Insomnia | 0.41 | 0.45 | 0.47 | 0.46 | ||
| Follow up - baseline | Anxiety | |||||
| Depression | 0.36 | |||||
| Low energy | 0.22 | 0.39 | ||||
| Concentration | 0.27 | 0.33 | 0.35 | |||
| Insomnia | 0.20 | 0.22 | 0.25 | 0.25 |
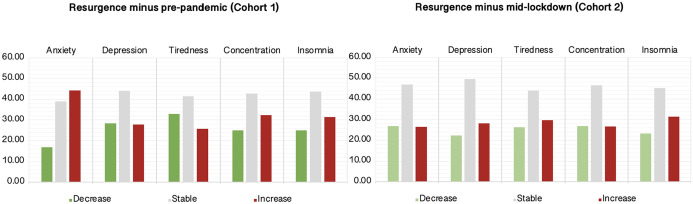
T-tests against zero (Table S4) showed significant changes in mood measures for both Cohorts. The largest change was anxiety in Cohort 1 (t = 36.82 p < 0.0001). Approximately 44% of participants showed increased anxiety vs. <17% decreased (Fig. 1 ). By contrast, Cohort 2 did not show a statistically significant change in anxiety levels. Cohort 1 also showed a significant net increase in trouble concentrating (t = 11.29 p < 0.0001) with 32% reporting an increase vs. 25% a decrease, but no significant difference for Cohort 2. Interestingly, Cohort 1 showed worsening of insomnia (t = 9.29 p < 0.0001, increase = ~31% decrease = ~25%) but decreased incidence of tiredness (t = −9.46 p < 0.0001, increase = ~26% decrease = ~33%) whereas Cohort 2 showed significant net increases for both insomnia (t = 10.98 p < 0.0001, increase = ~32% decrease = ~23%) and tiredness (t = 5.36 p < 0.0001, increase = ~30% decrease = ~26%). Only Cohort 2 showed a significant increase in depression (t = 8.49 p < 0.0001, increase = ~28% decrease = ~22%). Combined with previously reported elevation in anxiety levels for Cohort 2 vs Cohort 1 at baseline when controlling for detailed sociodemographic variables [3], these results demonstrate a significant and sustained increase in symptoms of anxiety, and a smaller magnitude increase in low mood during the pandemic.
Fig. 1.
Percent population exhibiting longitudinally increased, decreased or stable symptom frequency.
Anxiety appeared most affected during the pandemic, with >44% of participants in Cohort 1 reporting increased frequency from pre-pandemic to mid resurgence one year later. Problems with concentration and insomnia showed smaller but statistically significant increases for Cohort 1. Anxiety did not increase from mid lockdown to resurgence in Cohort 2, however small increases were evident in depression, tiredness and insomnia.
3.3. Identifying population variables that predict probability of symptom change
Next, we aimed to identify population variables that were associated with the reported changes in mental health symptoms (i.e. anxiety, depression, tiredness, concentration, and insomnia, as described above). We used multinomial logistic regression, where participants were classified according to whether their self-reported symptom severity increased, decreased or remained stable. The predictors used were: age-decade (16–19, 20–29, 30–39… 70+); sex (male, female or other), handedness (left, right or ambidextrous); education level (no school, primary/elementary, secondary, university degree or PhD); work arrangements (furloughed, healthcare worker with coronavirus patients, other healthcare worker, retail/ job involving interaction with public, working from home, office/lab/other workplace, other); report of a diagnosed neurological condition; and report of a diagnosed psychiatric condition. Full results are reported in the supplement (Supplementary Table S5a-e). Age; sex and pre-pandemic diagnosed psychiatric conditions were consistently identified for all five items as being significant predictors of the probability of change in mood between the pre-pandemic and mid-resurgence timepoints. Therefore, these population variables were investigated in greater detail below.
3.4. Further analysis of change in mood symptom frequency distributions within select sub-populations
Response options on the mood self-assessment scale constitute a non-linear ordinal scale; therefore, differences across populations in the probability of change across time can be hard to interpret if the baseline distributions for those populations also differ. That is, a change from ‘never’ to ‘almost never’ is not equivalent in importance or scale to a change from ‘daily’ to ‘hourly’ frequency whilst floor and ceiling effects are also a consideration. Consequently, we examined differences in the probability distributions of mood self-assessment scores for the age, sex and pre-existing conditions in more detail.
3.5. Age group
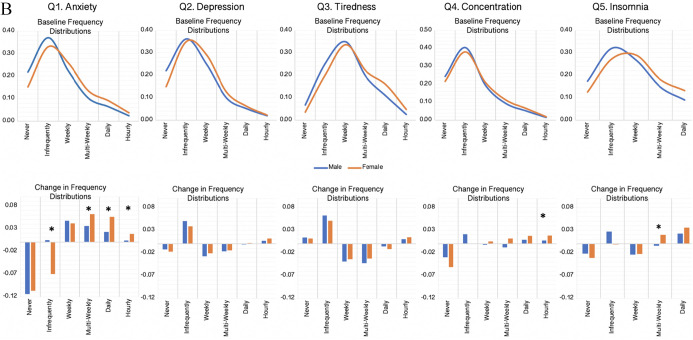
We first examined differences in item-level symptom scores as a function of age decade (Supplementary Table S6a & Fig. 2 , PANEL A). Permutation testing (Supplemental Methods), where the age-group labels were randomly reassigned 10,000 times, showed significant differences in the baseline symptom frequencies across age decades for the five items (all p < 0.001 two tailed & Bonferroni corrected) and in both cohorts. Plotting the distributions showed a clear pattern of results whereby symptoms were substantially more likely to be reported as frequent by people of younger age (Fig. 2 , PANEL A).
Fig. 2.
Cohort 1 symptom frequency measures across timepoints as a function of age (Panel A) and gender (Panel B).
Top. Proportion of participants in Cohort 1 reporting symptoms at each frequency within separate age decades at timepoint 1. Note that older adults are substantially less likely to report high frequency of symptoms across all five questions. Bottom. Absolute change in frequency for timepoint 2 - timepoint 1. Overall change in anxiety, depression and tiredness differed significantly across age groups (p < 0.001 Bonferroni corrected). Stars indicate significant cross-group differences at the item-response level at the threshold of p < 0.05 2-tailed and Bonferroni corrected.
Top. Proportion of male and female participants in Cohort 1 reporting symptoms at each frequency at timepoint 1. Note that females are slightly more likely to report high frequency of symptoms across all five questions (all p < 0.001 Bonferroni corrected). Bottom. Absolute change in frequency for timepoint 2 - timepoint 1. Insomnia was threshold level at p ~ =0.1. Stars indicate significant between-sex differences at the item-response level at the threshold of p < 0.05 2-tailed and Bonferroni corrected for those conditions where the set level distributions differ significantly.
Permutation testing when contrasting resurgence minus baseline in Cohort 1 (Supplementary Table S6b) showed significant differences in the overall change in symptom frequency distributions for anxiety, depression and tiredness (all 2-tailed p < 0.001 Bonferroni corrected) but not concentration or insomnia (p = 0.910 & p = 0.350 Bonferroni corrected). At a finer grain (Fig. 2 , PANEL A), a higher proportion of older adults switched from the ‘never anxious’ category and a higher proportion switched to the multiple-times per week category, whereas younger adults were more likely to switch to the ‘anxious every day category’. Older adults showed higher probability of switching out of the ‘never depressed’ category whereas younger adults were more likely to switch out of the weekly and multi-weekly depressed categories. People of middle working age were more likely to switch into the ‘almost never’ tired category with reductions seen at higher frequency categories.
Contrasting resurgence minus baseline in Cohort 2 in the same manner (Supplementary Table S6b) showed significant differences in overall change in frequency distributions for tiredness (p < 0.01) and insomnia (p < 0.001) only. People of middle working age were significantly more likely to shift from the ‘never’ category for insomnia and to the higher frequency categories, e.g., ‘daily’.
3.6. Sex
Next, we examined differences in symptom frequencies as a function of male vs female sex (Supplementary Table S7a & Fig. 2 PANEL B). Individuals indicating ‘other’ were excluded from statistical analysis due to being low frequency and forming a non-significant predictor in the multinomial logistic regression analyses. Permutation testing, showed significant differences in the baseline symptom frequencies across sexes for all five symptom types (p < 0.001 two tailed & Bonferroni corrected) and in both cohorts with the exception of concentration, which was non significant in Cohort 2 (p = 0.181 two tailed and Bonferroni corrected). Plotting the distributions showed a clear pattern of results whereby symptoms were more likely to be reported as frequent by females than males (Fig. 2 PANEL B).
Permutation testing when contrasting resurgence minus baseline in Cohort 1 (Supplementary Table S7b) showed significant differences in the overall change in symptom frequency distributions for anxiety and concentration only (p < 0.001 and p = 0.04 two-tailed & Bonferroni corrected). At a finer grain (Fig. 2 PANEL B), a higher proportion of females transitioned from the ‘almost never’ anxiety category and into the three higher frequency anxiety categories. Females also were more likely to transition into the highest frequency category for problems concentrating. There were no other significant differences in the response category permutation analyses and no significant differences in the set level analysis for Cohort 2 (Supplementary Table S7b).
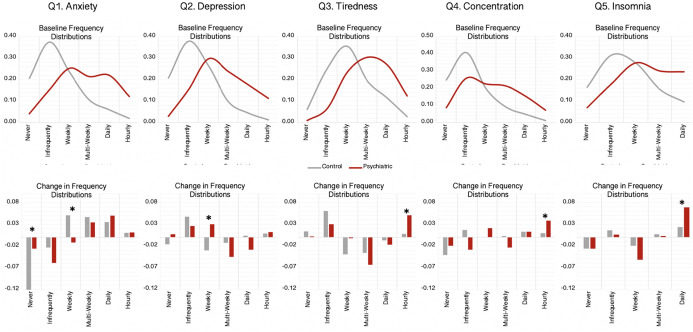
3.7. Pre-existing psychiatric conditions
We examined the relationship between having a pre-existing psychiatric condition and change in symptom frequencies (Supplementary Table S8a). Permutation testing showed significant differences in the baseline symptom frequencies across psychiatric and non-psychiatric sub-groups for the five items and in both cohorts (all p < 0.001 two tailed & Bonferroni corrected). Plotting the distributions showed a clear pattern of results whereby symptoms were substantially more likely to be reported as frequent by people with pre-existing psychiatric conditions (Fig. 3 TOP).
Fig. 3.
Cohort 1 symptom frequency at baseline and across timepoints for people with vs. without preexisting psychiatric conditions.
Top. Proportion of participants in Cohort 1 reporting symptoms at each frequency separately for those with vs. without pre-existing psychiatric conditions. Note that people with pre-existing psychiatric conditions are substantially more likely to report high frequency of symptoms across all five questions (all p < 0.001 Bonferroni corrected). Bottom. Absolute change in frequency for timepoint 2 - timepoint 1. Stars indicate significant cross-group differences at the item-response level at the threshold of p < 0.05 2-tailed and Bonferroni corrected.
Permutation testing when contrasting resurgence minus baseline in Cohort 1 (Supplementary Table S8b) showed significant differences in the overall change in symptom frequency distributions for anxiety, depression, tiredness and concentration but not insomnia (p < 0.001, p = 0.002, p = 0.010, p = 0.030 & p = 1.005 two-tailed Bonferroni corrected). At a finer grain (Fig. 3 BOTTOM), a higher proportion of the non-psychiatric group transitioned from the never anxious category and to the weekly category. More psychiatric patients transitioned to the weekly depressed category, with reductions in the daily frequency category. The psychiatric group were significantly more likely to transition into the highest symptom frequency category for tiredness, concentration and insomnia. Permutation testing when contrasting resurgence minus baseline in Cohort 2 (Supplementary Table S8b) showed significant differences in the overall change in anxiety symptom frequency only (p = 0.005 two-tailed Bonferroni corrected). This reflected higher probability of the psychiatric subgroup transitioning from the daily and to the multi-weekly category.
3.8. Contrasting entropy estimates of mood stability in control vs psychiatric groups
A salient feature of the above results was that people reporting psychiatric conditions appeared more likely to change states across timepoints. Plotting the transition probabilities in matrix form also indicated that they were more likely to transition to a broader range of end points given their start points than people without psychiatric conditions (Fig. 4 & Table S9). The statistical significance of this symptom variability was analysed by estimating the Shannon entropy of each group's transition matrix and comparing it to the permutation null distribution, calculated by permuting group labels between individuals who had the same responses at the first timepoint (Supplemental Methods). The psychiatric sub-group had significantly more variable trajectories across timepoints 1 and 2 for the depression and concentration questions in both cohorts, and for the insomnia question in Cohort 2. Trends in the same direction for the anxiety question did not stand up to Bonferroni correction for multiple comparisons.
Fig. 4.
Transition graphs for controls vs psychiatric groups in Cohorts 1 and 2.
Left. heat maps of transition matrices, separately for each questionnaire item, for controls and people reporting diagnosed psychiatric conditions in Cohort 1 (baseline pre-pandemic) and Cohort 2 (baseline mid first lockdown). Rows are symptom frequencies at baseline and columns are symptom frequencies at follow up. Color intensity is joint probability, where the cells of each matrix sum to 1. Right. Difference in Shannon entropy for patient minus control transition matrices with observed non-permuted value indicated by the red line (test) and null distributions, calculated from 10,000 permutations where baseline frequencies are matched, indicated in blue. People with psychiatric conditions showed greater variability in their change in symptom frequency across timepoints than controls for depression and concentration in both cohorts, and for insomnia in Cohort 2.
4. Discussion
This study examined changes in mental health during the pandemic longitudinally, including whether previously reported early-pandemic elevation in symptoms [3] were sustained over time. The analytic approach first determined whether particular aspects of mental health had been more affected than others. Intersecting questionnaire item responses with population variables identified the most prominent sociodemographic features associated with the scale of pandemic impact. Permutation analysis of symptom frequency distributions then disambiguated the underlying nature of those associations. Finally, analysis of transition probability matrices provided further insight into the relative stability of symptom states in people with a history of mental health diagnoses, versus those without.
The results confirmed some but not all of our hypotheses. Most notably, analysis of Cohort 1, i.e., pre-pandemic to peak resurgence one year later, confirmed that the greatest increase in overall symptom frequency was for anxiety, with smaller but still statistically significant changes in other aspects of mental health, i.e. tiredness, concentration and insomnia. A particularly pronounced impact on anxiety accords with previous UK cross sectional and longitudinal studies [3,10,11], but extends to demonstrate a sustained effect relative to a baseline immediately preceding the pandemic and controlling for any seasonal variation in mood. Importantly, and contrary to our and others [5] expectations, we found little evidence for habituation to the pandemic conditions over the examined timeframes. More specifically, in addition to baseline mental health symptoms differing between Cohort 1 and 2, which demonstrated the previously reported early change between pre-pandemic and first lockdown [3], changes herein were observed in Cohort 1 over a 1-year timeframe, indicating a longer-term pandemic impact. The fact that symptom frequencies were similar across timepoints in Cohort 2 provides little evidence of habituation. These results converge in supporting both immediate and sustained negative impact of the pandemic on some mental health symptoms.
In concordance with our hypotheses, the relatively subtle global changes in depression, concentration, tiredness and insomnia symptom frequency belied more substantial changes in specific sub-populations. Specifically, the multinomial regression analysis indicated that older adults, women and people reporting previously diagnosed psychiatric conditions were more likely to report increased frequency across multiple symptom types. Notably though, the detailed analysis of change in frequency distributions showed a more complicated dynamic, highlighting the need for caution when interpreting such findings, here and in the broader literature.
More specifically, when analysing age, older adults showed a greater increase in mean symptom frequency than younger adults relative to their respective baselines. However, when the frequency distributions were examined in detail it was notable that younger adults already had substantially higher symptom frequency endorsement prior to the pandemic and that older adults were more likely to be close to the floor of the frequency scale. Indeed, with anxiety, younger and older adults had similar probabilities of increased symptom frequency, but younger adults were more likely to transition to lower frequency. Furthermore, older adults showed greater increases in the lower range of the frequency scale, i.e., to multi-weekly anxiety, whereas younger adults were more likely to transition to daily anxiety. This pattern of results highlights the importance of focusing mental health research and interventions towards both ends of the lifespan.
In terms of differential impact of the pandemic across men and women, we found that on average anxiety and problems concentrating were more likely to increase in frequency for women than men during the pandemic. Detailed analysis of the change in frequency distributions showed that women were also more likely to transition to the highest frequency categories for anxiety. Notably, in contrast to the age differences discussed above, this was from a higher pre-pandemic baseline, with a slightly higher frequency of symptoms evident for females in all five items prior to the pandemic emerging.
As expected, people who reported pre-existing psychiatric conditions differed from those without such diagnoses in their probabilities of reporting changes in their symptom frequency during the pandemic for all five symptom domains. Examination of frequency distributions showed that those with pre-existing mental health conditions differed substantially to controls in pre-pandemic baseline distributions, being much more likely to report the higher frequencies of symptoms and unlikely to report the lowest frequency symptoms. Furthermore, whilst those without mental health diagnoses were more likely to transition to moderate frequency symptoms, those with diagnoses were more likely to transition into the highest frequency category for items including tiredness and insomnia.
The entropy analysis provided further insights into how these sub-populations differed with respect to the distributions of change trajectories, that is, as opposed to change in overall symptom frequency distributions. When controlling for baseline symptom frequencies, it was clear that people with diagnosed mental disorders were more likely to change across time and that the changes were distributed across a wider range of start to end frequencies. These differences in the nature of change across time were evident in both cohorts, highlighting that the higher level of fluctuation in symptoms during the pandemic appeared to be sustained rather than transient. This observation speaks to the potential value of future work using frequent brief assessments of symptoms to better characterise vulnerable populations in terms of the fluctuations and dynamics of symptoms across time, both in relation to the pandemic, and in general. This accords with broader developments in psychiatric practice, supporting the use of evidence-based digital monitoring tools [12]. The results of the current study, where a remotely delivered mental health assessment comprising five items provided robust and informative associations, highlights the potential for more frequent monitoring using such approaches, as such a brief scale can be completed in minimal time.
While many people in this study experienced exacerbation of mental health symptoms during the pandemic, it is important to note that a significant proportion of people did not. Indeed, many individuals reported symptom score improvement during the pandemic. This highlights the cardinal importance of following up these current findings to explore risk and resilience markers [13] as well as exploring how environmental changes could impact symptoms for the better, depending on a person's demographic and other characteristics. This will form the basis of future analyses.
Several limitations should be noted. This study did not use a random sampling strategy: COVID-19 mental health studies with random sampling strategies have been published but typically rely on old historical baseline data and lack contextual measures. Furthermore, random sampling still requires participants to choose to respond, and our follow up cohort compares favourably to others in terms of both inclusivity and to its own baseline in terms of minimal quantifiable bias with respect to self-assessment scores. Here, mean age and educational achievement were higher than would be expected for the 16+ population within the UK. Furthermore, Cohort 1 and Cohort 2 were closely matched in age, first language employment and education status, but differed in representation of minority groups (88% vs 93% minority ethnic) and sexes (6:4 vs 4:6 male vs female). Nonetheless, the sample sizes were heterogeneous and large enough to include representation across all levels along variables of interests such as age, education, and occupational statuses within the target frame, enabling the covariances of these variables with mental health to be modelled. However, we should be careful extrapolating the results beyond the UK population as the sample was primarily recruited within the UK. Self-report questionnaires have inherent limitations; but conversely, collection of such large-scale data using in-person interviews during the pandemic would have been impractical. Finally, short versions of symptom rating tools were used; but the rationale for doing so was to help maximise participation.
It is evident from this study that there are sustained negative impacts of the pandemic on mental health, these are larger for some sub-populations and especially so in vulnerable psychiatric groups. By pooling together longitudinal studies with common methodological issues, such findings may be overlooked in emerging meta-analyses.
Role of the funding source
This work was supported by the Dementia Research Institute, Care Research and Technology Centre. SRC's role in this work was funded by Wellcome (110049/Z/15/Z & A). PJHs role was supported by the NIHR Maudsley BRC.
Disclosures
AH is owner and director of Future Cognition Ltd., which develops online cognitive paradigms for other academics, and co-owner and Director with PJH of H2CD Ltd., which hosts online cognitive and mental health studies. SRC receives honoraria for editorial work at Elsevier journals. JEG receives honoraria from Springer Publishing for editorial work and from Elsevier Publishing. Other authors report no disclosures.
Acknowledgements
The authors would like to thank Dr. Ibrahim Aslan for kind assistance in preparing this manuscript for submission.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.comppsych.2022.152298.
Appendix A. Supplementary data
Supplementary material. Additional methodological details and results tables.
References
- 1.Holmes E.A., O’Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taquet M., Luciano S., Geddes J.R., Harrison P.J. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8(2):130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hampshire A, Hellyer P, Soreq E, Trender W, Mehta MA, Ioannidis K, et al. Dimensions and modulators of behavioural and mental-health changes during the COVID-19 pandemic: an N=343,017 study. Nat Commun In press, doi: 10.1101/2020.06.18.20134635. [DOI]
- 4.Mansfield K.E., Mathur R., Tazare J., Henderson A.D., Mulick A.R., Carreira H., et al. Indirect acute effects of the COVID-19 pandemic on physical and mental health in the UK: a population-based study. Lancet Digit Health. 2021;3(4) doi: 10.1016/S2589-7500(21)00017-0. e217-e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. 2021;8(2):141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robinson E., Sutin A.R., Daly M., Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic. medRxiv. 2021 doi: 10.1101/2021.03.04.21252921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chamberlain S.R., Grant J.E., Trender W., Hellyer P., Hampshire A. Post-traumatic stress disorder symptoms in COVID-19 survivors: online population survey. BJPsych Open. 2021;7(2) doi: 10.1192/bjo.2021.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spitzer R.L., Kroenke K., Williams J.B., Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 9.Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kwong A.S.F., Pearson R.M., Adams M.J., Northstone K., Tilling K., Smith D., et al. Mental health before and during the COVID-19 pandemic in two longitudinal UK population cohorts. Br J Psychiatry. 2020;1-10 doi: 10.1192/bjp.2020.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bendau A., Kunas S.L., Wyka S., Petzold M.B., Plag J., Asselmann E., et al. Longitudinal changes of anxiety and depressive symptoms during the COVID-19 pandemic in Germany: the role of pre-existing anxiety, depressive, and other mental disorders. J Anxiety Disord. 2021;79 doi: 10.1016/j.janxdis.2021.102377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gordon-Smith K., Saunders K., Geddes J.R., Harrison P.J., Hinds C., Craddock N., et al. Large-scale roll out of electronic longitudinal mood-monitoring for research in affective disorders: report from the UK bipolar disorder research network. J Affect Disord. 2019;246:789–793. doi: 10.1016/j.jad.2018.12.099. [DOI] [PubMed] [Google Scholar]
- 13.Ioannidis K., Askelund A.D., Kievit R.A., van Harmelen A.L. The complex neurobiology of resilient functioning after childhood maltreatment. BMC Med. 2020;18(1):32. doi: 10.1186/s12916-020-1490-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material. Additional methodological details and results tables.