Abstract
In low-income and middle-income countries (LMICs), emerging digital mental health interventions should be accompanied by regular and comprehensive assessment of available scientific evidence. This review aims to support efforts to monitor progress in digital mental health research, ensuring new evidence can guide researchers, clinicians, policymakers and program managers positioned to adopt and implement these digitally-enabled treatments. In accordance with PRISMA guidelines, an electronic database search from 2016 to 2020 yielded 37 digital intervention studies for detection, diagnosis, prevention, treatment, and/or management of a broad range of mental disorders in 13 LMICs. This date range was selected to update previous reviews. Most studies involved online interventions and many reported feasibility and acceptability, reflected by participant satisfaction or program adherence. About half the studies (N=23) reported clinical benefits based on changes in mental health. For depression and mood disorders, some digital interventions showed improvements in depressive symptoms, quality of life, treatment adherence, and recovery. However, sample sizes were small and studies focused primarily on adults. Further limiting generalizability was the lack of consistency in clinical assessment and measurement tools between studies. No studies reported worsening symptoms, negative acceptability or dissatisfaction with digital interventions, suggesting possible publication bias. While digital interventions show promise, it remains difficult to conclude that digital interventions are effective from these studies, as it is prudent to exercise caution before drawing conclusions about clinical effectiveness. This review reflects continued growth in digital mental health research in LMICs and further highlights the need for rigorous evaluation of effectiveness and cost-effectiveness.
Keywords: mental health, low- and middle-income country, digital technology, digital psychiatry, global health
1. Introduction
Mental disorders are a leading contributor to the global burden of disease, with mental illness accounting for 32.4% of years lived with disability and 13% of disability-adjusted life-years (Vigo et al., 2016). In low-income and middle-income countries (LMICs), there is a significant care gap (Pathare et al., 2018), with up to 90% of people with mental disorders not receiving adequate treatment and follow up (Becker and Kleinman, 2012; Patel et al., 2010; Patel and Prince, 2010). Globally, technology continues to emerge as a promising tool for offering direct support to individuals living with mental disorders, improving quality of services, and making evidence-based treatments more widely available (Bhugra et al., 2017). Digital health technologies typically encompass any form of remote or online platform or mobile device that can be used or designed to deliver a mental health intervention. This includes smartphone apps, online programs, text messaging, telepsychiatry, and wearable devices such as smart watches (Lipschitz et al., 2019). Effective digital health innovations present an opportunity to address the global discrepancy in mental healthcare provision.
In LMICs, a lack of awareness and adequate mental health services, social welfare and legislation to protect those with mental illness from stigma and discrimination are barriers to accessing services and promoting recovery from mental illness (Knaak et al., 2017; Koschorke et al., 2014; Semrau et al., 2015). Moving towards digital and online services may present an opportunity to enable individuals to access adequate mental healthcare in communities where mental health services may not be otherwise available. In cases where stigma and discrimination are particularly severe, such that an individual may fear social isolation or other inhumane responses to their mental illness, such as restraints (Semrau et al., 2015), digital technologies could present safe and confidential ways for people to access mental health interventions.
In high-income countries, the application of technology in healthcare is increasing rapidly (Price et al., 2014), with emphasis on new digital approaches for supporting mental and behavioural health care (Bhugra et al., 2017). Digital applications have demonstrated promise in reducing symptoms of mental disorders such as depression (Firth et al., 2017), psychotic disorders (Gire et al., 2017) and other severe mental illnesses (Naslund et al., 2015), and improving medication adherence (Rootes-Murdy et al., 2018). These include smartphone delivery of cognitive behavioural therapy (Baumel et al., 2016), and apps for the early identification of relapse in psychotic disorders (Ben-Zeev et al., 2018). However, depending on digital mental health interventions that have been developed and studied in higher income countries, namely ‘WEIRD’ countries (i.e., Western, Educated, Industrialized, Rich, and Democratic), may bias conclusions and limit generalizability (Henrich et al., 2010). Therefore, to address this limitation, it is necessary to explore studies that have employed digital mental health interventions in LMICs.
Mounting research from lower-income countries suggests the potential benefit of digital mental health technologies in these settings (Fairburn and Patel, 2017; Naslund et al., 2019), as reflected in recent reviews. However, these reviews have also highlighted gaps in the evidence. For instance, a 2017 review found 49 studies that supported the feasibility, acceptability, and potential clinical effectiveness of online, mobile, and text-messaging services aimed at the treatment or prevention of mental disorders in over 20 LMICs (Naslund et al., 2017). It was found that online, text-messaging, and telephone support interventions showed promise in decreasing mental health symptoms. However, many included studies also did not include adequate comparison conditions, were not rigorously designed trials, or reported limited information on average effect sizes, the relative effectiveness of mental health interventions for different populations, and the variability in these effects across studies. For instance, fewer than half of the 49 studies summarized in the 2017 review reported significant improvements in mental health outcomes or symptoms. In general, insufficient details were reported in many studies to enable replication, with the review concluding that more research is required to determine clinical effectiveness of technological interventions and how to scale up and integrate use of technology into existing health systems (Naslund et al., 2017).
Furthermore, Kaonga and Morgan (2019) reviewed studies of digital tools including mobile and online modalities for mental health care, focused on improving psychological support and treatment adherence in resource-limited settings. This review did not provide comprehensive summaries of the included studies, which employed a wide range of designs, and were mostly pilot studies, without consistent reporting of outcomes. Importantly, of the 67 studies included, only 31 were from LMICs, making it difficult to determine whether the acceptability and potential clinical benefits of digital mental health programs from low-resource settings in higher income countries can generalize to LMICs (Kaonga and Morgan, 2019). Of the 31 studies from LMICs, only 4 reported significant improvements in mental health outcomes, highlighting a gap with reporting on effectiveness (Kaonga and Morgan, 2019).
Lastly, a review by Jimenez-Molina et al. (2019) identified 22 studies of Internet-based interventions focused on prevention and treatment of mental disorders including depression, anxiety, and substance use in Latin America. This review suggests that there were favorable short-term results in less than half of the interventions including reduction in stress, anxiety, and depression. However, the studies mostly had short term follow-up and reported difficulty in participant retention and adherence to the online treatment protocols. Nine of the included studies reported improvements on mental health outcomes, with many studies unable to report effectiveness due to high attrition rates and methodological limitations including unclear sample groups (Jiménez-Molina et al., 2019). The limited reporting of clinical efficacy among these Internet interventions, combined with methodological challenges, makes it difficult to inform efforts to scale up these programs in real world settings.
These recent reviews of published studies highlight a mix of promising examples as well as important future directions for the field. Another important consideration is that there continues to be an unprecedented increase in the number of available commercial mental health technologies, which raises concerns that the emergence of new digital applications and devices has not been accompanied by similar progress in scientific evidence to support their use for addressing mental disorders (Naslund et al., 2019). For instance, over 10,000 mental health apps are available for download via commercial app stores (Torous et al., 2019); though, most of these commercially available apps have no reliable or high-quality scientific evidence as support (Larsen et al., 2019; Lau et al., 2020). In LMICs, this concern is especially relevant as growth of technology is even less likely to be accompanied by robust research evidence. This stems from general neglect and under-prioritisation of mental health on research agendas in many LMICs (Becker and Kleinman, 2013). Furthermore, governance and regulation of mental healthcare systems and policies in LMICs are low (Petersen et al., 2017), suggesting that regulatory bodies in place in many countries may be insufficient to match the unprecedented increase in the development of mental health technologies. Additionally, public access to commercial digital mental health applications is becoming increasingly easy given that wireless connectivity is becoming more widely available even in rural areas, and that smartphone prices continue to decrease (We Are Social, 2020).
To respond to this rapid evolution of the field of digital health technologies in global mental health, regular and comprehensive assessment of studies as they become available is required. This will also contribute further to the development of mental healthcare technologies that are safe, evidence-based and offer potential for the greatest benefit to those living with mental disorders in LMICs. In the current review, we aimed to address the need for regular monitoring of digital mental health research in low income settings by specifically expanding on these recent reviews that summarise use of digital mental health interventions in LMICs (Jiménez-Molina et al., 2019; Kaonga and Morgan, 2019; Naslund et al., 2017). We build on these studies not only by updating the review of published studies in this field, but also by providing a comprehensive synthesis and assessment of methodological quality of current research findings from LMICs.
A large number of new interventions studies have been published since the review by Naslund et al. (2017), so the current review accounts for the increasing use of technology and smartphone access in many LMICs. The current review also expands upon the review by Kaonga and Morgan (2019) by including studies of interventions applied specifically in LMICs (rather than low-resource settings in higher-income countries), and expands on the review by Jiménez-Molina et al. (2019) by including studies beyond Latin America. Furthermore, to address a key gap in the prior reviews, we aim to provide a comprehensive summary of the potential clinical benefits of digital mental health interventions in LMICs. Our goal is to contribute to ensuring that new studies reporting clinical effectiveness are summarized in a way that can guide both researchers and clinicians, as well as policymakers and program managers responsible for the adoption and implementation of safe and effective new services into practice.
2. Methods
2.1. Search Strategy
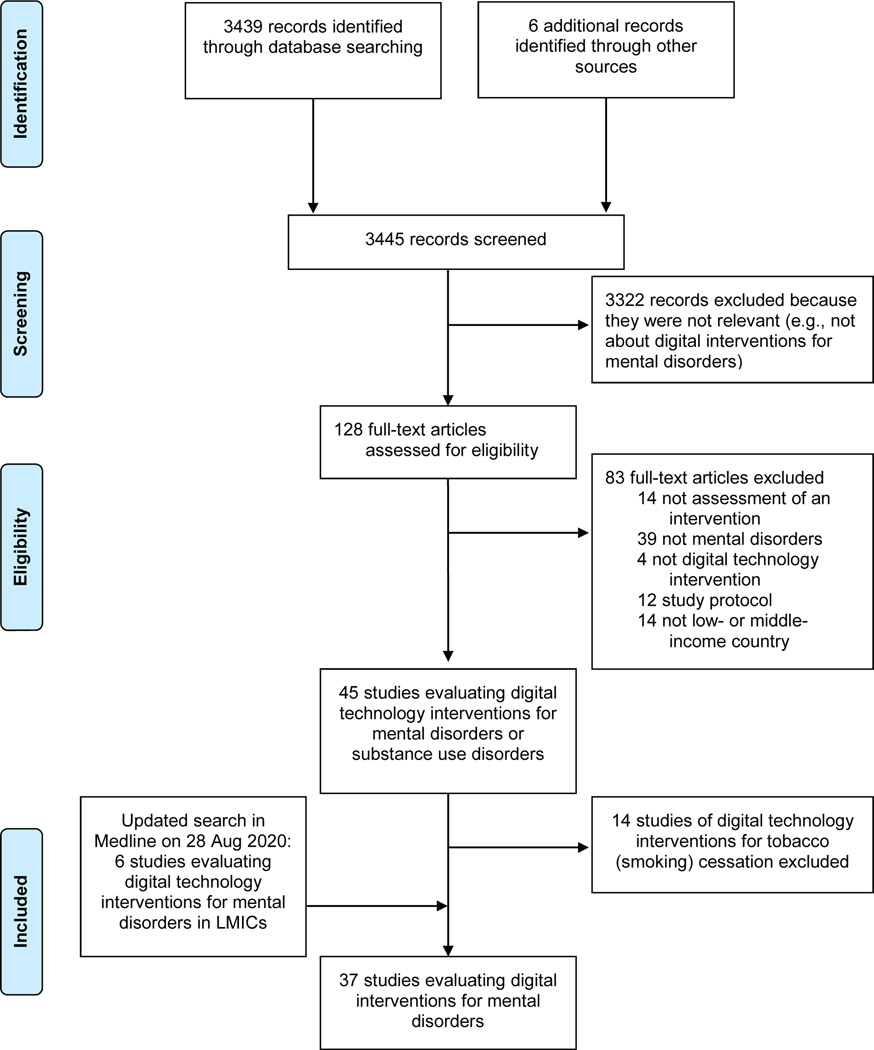
This review adhered to the Preferred Reporting Items for Systematic and Meta-Analyses (PRISMA) reporting guidelines (Moher et al., 2009). A search was undertaken using Medline, with time limits placed between 2016/08/01 and 2019/07/16. The search was subsequently updated to include relevant studies from 2019/07/16 to 2020/08/28. Studies prior to 2016/08/01 were not considered in this search as these were previously summarised in the review by Naslund et al. (2017), the earliest of the three prior reviews. The search strategy was adapted from the search strategies described in prior reviews (Jiménez-Molina et al., 2019; Kaonga and Morgan, 2019; Naslund et al., 2017). The complete list of search terms are in Table 1.
Table 1.
Terms used in Medline search
| Search | Search Terms* |
|---|---|
| “Mental illness” | ((((“serious mental illness” OR “serious and persistent mental illness” OR “severe mental illness” OR “mental illness” OR “mental health” OR “mental disorder” OR “schizophrenia” OR “bipolar disorder” OR “schizoaffective disorder” OR “major depressive disorder” OR “major depressive disorder” OR “depression” OR “anxiety” OR “affective disorder” OR “psychotic disorders” OR “psychosis” OR “posttraumatic stress disorder” OR “ptsd” OR “stress disorder” OR “antipsychotic”)) OR (“alcohol” OR “substance use” OR “substance use disorder” OR “substance related disorder” OR “alcohol” OR “alcohol use disorder” OR “alcoholism” OR “amphetamine” OR “cocaine” OR “crack cocaine” OR “marijuana” OR “cannabis” OR “opioid” OR “heroin” OR “morphine” OR “tobacco” OR “street drugs” OR “drug abuse” OR “illicit drugs” OR “recreational drugs” OR “smoking” OR “cigarette”)) OR (“mental disorders”[MeSH Terms] OR “Anxiety Disorders” [MeSH] OR “Stress Disorders, Traumatic”[MeSH] OR “Mood Disorders”[MeSH] OR “Depressive Disorder”[MeSH] OR “Schizophrenia and Disorders with Psychotic Features”[MeSH] OR “Psychotic Disorders”[MeSH])) OR (“SubstanceRelatedDisorders”[MeSH] OR “AlcoholRelatedDisorders”[MeSH] OR “AmphetamineRelatedDisorders”[MeSH] OR “CocaineRelated Disorders” [MeSH] OR “Marijuana Abuse”[MeSH] OR “OpioidRelated Disorders”[MeSH] OR “Tobacco Use Disorder” [MeSH] OR “Street Drugs”[MeSH] OR “Crack Cocaine”[MeSH] OR “Smoking”[MeSH] OR “Tobacco Use”[MeSH]) |
| “Technology” | ((“Telemetry” OR “Telemedicine” OR “Telepsychiatry” OR “Telehealth” OR “Telecare” OR “Telemental health” OR “eHealth” OR “uHealth” OR “Connected Health” OR “online” OR “internet” OR “Internet health” OR “Web Browser” OR “Website” OR “Webbased” OR “Social Media” OR “Facebook” OR “Mobile Health” OR “Mobile Technology” OR “Mobile phone” OR “Cellular Phone” OR “Cellphone” OR “Smartphone” OR “text message” OR “SMS” OR “text messaging” OR “Artificial Intelligence” OR “Game Theory” OR “UserComputer Interface” OR “Computer Simulation” OR “Speech Recognition Software” OR “Therapy, ComputerAssisted” OR “Remote Sensing Technology” OR “Remote Consultation”)) OR (“Telemetry[MeSH] OR “Telemedicine”[MeSH] OR “Internet[MeSH] OR “Web Browser”[MeSH] OR “Social Media”[MeSH] OR “Cellular Phone”[MeSH] OR “Text Messaging”[MeSH] OR “Artificial Intelligence”[MeSH] OR “Game Theory”[MeSH] OR “UserComputer Interface”[MeSH] OR “Computer Simulation”[MeSH] OR “Speech Recognition Software”[MeSH] OR “Therapy, ComputerAssisted”[MeSH] OR “RemoteSensing Technology”[MeSH]) |
| “Low- and middle-income countries” | ((((“Afghanistan” OR “Benin” OR “Burkina Faso” OR “Burundi” OR “Cambodia” OR “Central African Republic” OR “Chad” OR “Comoros” OR “Congo” OR “Democratic Republic of Congo” OR “Eritrea” OR “Ethiopia” OR “The Gambia” OR “Guinea” OR “GuineaBissau” OR “Haiti” OR “Democratic Republic of Korea” OR “Liberia” OR “Madagascar” OR “Malawi” OR “Mali” OR “Mozambique” OR “Nepal” OR “Niger” OR “Rwanda” OR “Sierra Leone” OR “Somalia” OR “South Sudan” OR “Tanzania” OR “Togo” OR “Uganda” OR “Zimbabwe”)) OR (“Armenia” OR “Bangladesh” OR “Bhutan” OR “Bolivia” OR “Cabo Verde” OR “Cape Verde” OR “Cameroon” OR “Republic of Congo” OR “Cote d’Ivoire” OR “Djibouti” OR “Egypt” OR “El Salvador” OR “Georgia” OR “Ghana” OR “Guatemala” OR“Guyana” OR “Honduras” OR “India” OR “Indonesia” OR “Kenya” OR “Kiribati” OR “Kosovo” OR “Kyrgyz Republic” OR “Kyrgyzstan” OR “Lao PDR” OR “Laos” OR “Lesotho” OR “Mauritania” OR “Micronesia” OR “Moldova” OR “Morocco” OR “Myanmar” OR “Nicaragua” OR “Nigeria” OR “Pakistan” OR “Papua New Guinea” OR “Philippines” OR “Samoa” OR “Sao Tome and Principe” OR “Senegal” OR “Solomon Islands” OR “Sri Lanka” OR“Sudan” OR “Swaziland” OR “Syria” OR “Syrian Arab Republic” OR “Tajikistan” OR “TimorLeste” OR “Ukraine” OR “Uzbekistan” OR “Vanuatu” OR “Vietnam” OR “Yemen” OR “Zambia”)) OR (“Albania” OR “Algeria” OR “American Samoa” OR “Angola” OR “Azerbaijan” OR “Belarus” OR “Belize” OR “Bosnia and Herzegovina” OR “Botswana” OR “Brazil” OR “Bulgaria” OR “China” OR “Colombia” OR “Costa Rica” OR “Cuba” OR “Dominica” OR “Dominican Republic” OR “Ecuador” OR “Fiji” OR “Gabon” OR “Grenada” OR “Iran” OR “Iraq” OR “Jamaica” OR “Jordan” OR “Kazakhstan” OR “Libya” OR “Macedonia” OR “Malaysia” OR “Maldives” OR “Marshall Islands” OR “Mauritius” OR “Mexico” OR “Mongolia” OR “Montenegro” OR “Namibia” OR “Palau” OR “Panama” OR “Paraguay” OR “Peru” OR “Romania” OR “Serbia” OR “South Africa” OR “St. Lucia” OR “St. Vincent and the Grenadines” OR “Suriname” OR “Thailand” OR “Tonga” OR “Tunisia” OR “Turkey” OR “Turkmenistan” OR “Tuvalu”)) OR (“Developing Countries”)[Mesh] OR (“Africa”)[Mesh] OR (“Asia”)[Mesh] OR (“South America”)[Mesh] OR (“Caribbean Region”)[Mesh] OR (“Central America”)[Mesh]) |
Mesh indicates Medical Subject Heading
2.2. Inclusion & Exclusion Criteria
Studies included in the review evaluated technological interventions for the prevention or treatment of mental disorders. ‘Technological interventions’ involved digital, online or mobile technologies, including telephones (e.g., telepsychiatry), mobile phones (e.g., SMS texting services) and smartphones (e.g., smartphone applications), programs delivered via the Internet (e.g., websites for internet-delivered CBT), and/or wearable technologies. The main component of the interventions must be technology-based for studies to be included. ‘Mental disorder’ encompassed any specifically defined (ICD or DSM) common or serious psychological disorders, as well as other more general psychological health terms such as ‘stress’, ‘psychological distress’, ‘(improving) mental health/ill-health’ or ‘suicide’, as long as a clear definition of the concept and a measurement instrument were given. Interventions could target multiple disorders or symptom clusters in the same study, as long as they were all clearly defined. Mental disorders had to be the primary disorder for a paper to be included.
Outcomes included clinical effectiveness, feasibility, acceptability, efficacy, costs and/or cost-effectiveness, patient, carer or mental health-worker satisfaction, as well as other clinical or mental health related outcomes, such as quality of life, self-esteem, coping and functioning. While outcomes could be varied in this search, the primary outcome must be directly related to the patients themselves. For example, a study investigating a digital intervention targeting caregiver well-being as the primary outcome was excluded. However, if caregiver well-being was an outcome secondary to patient well-being, the study was included. Study designs were also varied, including randomised controlled trials, pilot trials, case control studies and naturalistic studies; however, trial protocols, descriptions of intervention development, discussion or opinion pieces, qualitative content analysis and/or review articles were excluded.
Low- and middle-income countries (LMICs) were defined according to the 2015 World Bank classification. Additionally, countries were included in the search that had recently transitioned from middle- to high-income classification (e.g., Chile, Uruguay), to allow for more inclusive eligibility criteria.
2.3. Study selection & Data extraction
The lead researcher (HFC) screened titles and abstracts to identify articles to undergo full-text review. No language restrictions were applied, and English abstracts were obtained for non-English articles. Studies written in Spanish were directly translated by HFC, and any other non-English language articles were translated using Google Translate. Potentially eligible studies were shared with coauthors (RA and JAN). HFC extracted data including country of origin, sample description, method design and duration, outcome measures and main results, and summarised these details in a table. KA and DD updated the literature search and conducted data extraction for new eligible studies before adding these to the tables. JAN reviewed the table of included studies to confirm eligibility and accuracy in data extraction. HFC, KA and DD finalized the summary table. Due to heterogeneity of the included studies and reported outcomes, and given that this review aimed to summarise recent evidence, a quantitative synthesis of the findings was not possible. Fourteen studies assessing technological interventions for smoking (tobacco) cessation were identified in this search. Due to widespread prevalence of tobacco smoking, along with its relative social acceptance and lack of sanctioning in LMICs, tobacco cessation is often assessed separately from other mental health conditions and addiction in research. Therefore, these 14 studies will be summarised separately.
2.4. Quality Assessment
To assess the quality of included studies, we used the MQRS (Methodological Quality Rating Scale) along with the scoring instructions provided to assess each of the included studies (Miller & Wilbourne, 2002). The scale measures 12 dimensions of methodological quality with cumulative ratings ranging from 0 (lowest quality) to 16 (highest quality) and has been widely used to evaluate study quality in mental health services research, including in prior reviews (Cabassa et al., 2017; Fortuna et al., 2020; Whiteman et al., 2016). Studies with a quality rating score of at least 14 are considered to be high-quality studies (Miller & Wilbourne, 2002).
3. Results
3.1. Characteristics of Included Studies
We identified 37 studies of digital technology for the detection, diagnosis, prevention, treatment, and/or management of mental disorders in 13 LMICs across 7 geographical regions (East Asia, n = 10; South Asia, n = 5; Central or Latin America, n = 11; Middle East, n = 3; Eastern Europe or Western/Central Asia, n = 3; South-East Asia, n = 2; Africa, n = 3). We arranged studies by disorder type, into the following 5 categories: depression and mood disorders; anxiety disorders and post-traumatic stress disorder; alcohol or substance use disorders; community mental health services including common and severe mental disorders; and suicide prevention. In the sections below, we summarize key findings for each category of included studies. Studies targeting more than one type of disorders were summarised in both tables and are mentioned in subsequent relevant sections in the text.
3.2. Digital interventions for depression and mood disorders
Nearly half of included studies (48%; n = 18 out of 37) targeted depression or mood disorders. As summarized in Table 2, these studies primarily focused on depression in adults, and used online interventions. Arjadi et al. (2018) described an Internet-based behavioural activation programme for major depression in Indonesia, which led to improvements in depressive symptoms and remission rates at follow-up. An online mindfulness intervention from China led to improvements in depression compared to control (Ma et al., 2018). Osorio et al. (2017) described an online intervention for symptom monitoring to prevent relapse and encourage treatment retention, and found that depressive symptoms did not increase during the trial. Tulbure et al. (2018a) implemented an internet-supported intervention for depression in Romania and observed improvement in depressive symptoms. Furthermore, Tulbure et al. (2018b) tested a web-based transdiagnostic intervention in Romania and found improvements in mood disorder symptoms and quality of life measures. One study by Anttila et al. (2019) targeting adolescent depression trialled an internet-delivered program for high school psychosocial wellbeing in Thailand, though no significant differences in depression emerged post-intervention. Yang et al. (2019) tested a mindfulness intervention delivered over WeChat, a highly popular social media platform in China for perinatal depression, which improved depressive symptomatology. Yeung et al. (2018) describe a Chinese-adapted version of MoodGYM, an online CBT-based intervention, which resulted in improved depressive symptoms compared to the care-as-usual control (Yeung et al., 2018).
Table 2.
Digital interventions for depression and mood disorders
| Authors & Country | Disorder | Trial type | Sample | Methods | Instruments | Outcome measures | Time points | Findings |
|---|---|---|---|---|---|---|---|---|
| Adewuya et al. (2019); Nigeria | Depression | Pilot RCT | 895 patients (average age 34.9 years; age range 18–60; 55% female) at 10 primary care centres in Lagos, diagnosed with depression | Mobile telephone adherence support for management of depression (McHPriC Project). Clinics were randomised either to mobile telephone supported Collaborative Stepped Care (mCSC) or control group, consisting of ordinary CSC (oCSC) | PHQ-9, WHODAS, Quality of Life (QoL) Brief version, attendance logs | Rate of adherence to intervention, recovery rate, QoL, cost-effectiveness, and acceptance | Baseline, 6 and 12 months | mCSC group had significantly better intervention adherence rate than oCSC at 6 months (90% vs 67.8%; 95% CI 1.22–1.40) and at 12 months (78.1% vs 59.2%; 96% CI 1.20–1.43). mCSC had higher depression recovery rate, QoL scores, retention in treatment, cost-effectiveness and acceptance of intervention |
| Anttila et al. (2019); Thailand | Adolescent psychologica l well-being | Quasi-experimental (feasibility) | 167 adolescent high-school students (aged 15–19 years; average 15.9 years; 68.3% female) at three high schools in Southern Thailand | 7-week web-based programme (DepisNet-Thai) for supporting the mental wellbeing (depression and stress) of students in a high school setting. Includes 5 weekly modules each lasting 50 minutes (Psychological stress, physical wellbeing, Me and my family, Me and my friendships, Me and my society). Intervention group completed the programme in groups of 11–14 with a tutor per group. Active control group used the programme independently; passive control had no access to programme | PHQ-9, PSS, CSQ-8 | Depression, psychological stress, satisfaction, acceptance and usage of service | Baseline, 11 weeks from baseline | No statistically significant changes emerged at follow-up for satisfaction between the groups. Difference between programme users (group and independent) and non-users (passive control group) were non-significant. Acceptance was higher among those who used the programme independently (39%; p = .001). Usability feedback did not differ significantly between groups |
| Arjadi et al. (2018); Indonesia | Major depressive disorder (MDD) or persistent depressive disorder (PDD) | RCT | 313 participants (over 16 years, average 24.5 years, 81% female) recruited in community settings, scoring 10+ on the PHQ-9, and with internet access | Internet-based behavioural activation and lay counsellor support by email or chat (Guided Act and Feel Indonesia; GAF-ID). Sessions lasted 30–60 minutes per week for 10 weeks for each participant. Control group received online psychoeducation without counselling | PHQ-9; SCID | Self-reported PHQ-9 scores (depressive symptoms) | Baseline, 10-weeks (post-test), 3- and 6-months follow-up | At 10 weeks (post-test, PHQ-9 scores were significantly lower in the GAF-ID group than the control group (mean difference −1.26, p =.017). GAF-ID group had 50% higher chance of remission at 10 weeks (p<.0001). These effects were sustained at 3- and 6-month follow-up |
| Guo et al. (2020); China | Postpartum Depression | RCT | 284 participants (pregnant women aged 18–40l, 2nd or 3rd trimester after 34 weeks, 9 or above on EPDS, have internet and fluent in Chinese) | Internet-based program (6-week MBSP). Contained 6 sequential steps with various guiding exercises. 10 hours of training with 36 episodes, 6 episodes a week each lasting about 15 minutes. | EPDS, BDI, MAAS, SCS, CPBQ, PSI, WHO-5 | Mindfulness, self-compassion, depressive symptoms | Baseline,3 months from baseline, 1 year from baseline | Intervention group showed significant (p < 0.05) improvement at 3 months and further improved at 1 year compared to control. Intervention group dropped EPDS scores below 9, seeing most depressive symptoms alleviated and falling within reference range after one year. |
| Ma et al. (2018); China* | Psychological distress (depression and anxiety) | RCT | 192 participants (aged 18–47; average 27.8 years; 42% female) recruited by web-based advertisements | 8-week online mindfulness intervention, with participants divided into 3 conditions: group mindfulness (GMBI), self-directed (SDMBI) and a discussion group (DG), as well as a blank control group | FFMQ, DERS, SRAS, SRDS | Mindfulness, self-reported symptoms of anxiety and depression, emotion regulation | Baseline, 8 weeks (post-test) | Mindfulness, emotion regulation and depression scores improved significantly in the GMBI and SDMBI groups pre- to post-test, with medium to large effect sizes (Cohen’s d values between 0.44 – 0.75). Between-group analysis showed that these outcome changes were highest in GMBI groups than all others |
| Martinez et al. (2018); Chile | Adolescent depression | RCT | 143 adolescents aged between 13–19 years (average 15.4 years; 81.1% female), recruited from primary care centres in the Araucanía region | Remote Collaborative Depression Care (RCDC) for adolescents, consisting of 3 months of continuous remote supervision by psychiatrists, shared electronic health records, and telephone support. Control received EUC | BDI, KIDSCREEN | Depressive symptoms, health-related QoL, adherence to medications | Baseline, 12-weeks (post-test) | Patients showed higher adherence to pharmacological treatment. RCDC participants were more satisfied with psychological assistance than the EUC control group. No significant differences emerged in depressive or QoL scores between the groups |
| Maulik et al. (2017); India* | Common Mental Disorders (CMDs) | Pre-post evaluation | 238 participants (aged 18–92; average 39.7 years; 58.6% female) with CMDs, recruited from clinics in 30 rural villages | SMART: Systematic Medical Appraisal Referral and Treatment. This project trained lay village health workers and primary care physicians to screen, diagnose and manage individuals with CMDs using an electronic decision support system | PHQ-9, GAD-7, Knowledge, Attitude and Behaviour, Barriers to Access Care Evaluation; Treatment Stigma Subscale | Change in mental health utilisation and depression/anxiety scores, stigma, mental health awareness | Baseline, 3-months (post-test) | Significant reduction in depression scores between start and end of intervention among those who screened positive at the beginning of trial. Service utilisation increased, as well as awareness of mental health and stigma |
| Mehrotra et al. (2018); India | Depression | Pilot pre-post evaluation | 78 participants (aged over 17, average 32.3 years; 48.7% female) with major depression or dysthymia and significant impairment in functioning. | Practise and Use Self-Help for Depression (PUSH-D): a guided self-help app with 10 modules based on CBT, IPT, supportive psychotherapy and positive psychology. Participants completed the intervention for between 6–8 weeks for 2 hours a week. | BDI-II, PHQ-9, WSAS, RS-ES, WBI | Depression, functioning, self-esteem, well-being | Baseline, mid-way through intervention, post-test, and 2-month follow-up | Depression scores decreased significantly from baseline to post-assessment, with large effect sizes (r = .68 - .82, p < .01). Well-being also increased within this timeframe. |
| Menezes et al. (2019); Brazil & Peru | Depression | Pilot pre-post evaluation | 66 patients (21 in Sao Paulo, 42 in Lima) at Family Health Care clinics in São Paulo and Lima , aged over 21 and with hypertension or diabetes and PHQ-9 > 10 | Emotional Control intervention (CONEMO): mobile-phone delivered, with support of a nurse/nursing assistant. Consists of 18 behavioural activation sessions over 6 weeks (3 sessions per week) | PHQ-9, WHODAS | Depressive symptoms, functioning | Baseline, 6 weeks (post-test) | At post-test, 65% of participants in Sao Paulo and 81% in Lima had achieved 50% reduction in depressive symptoms |
| Moeini et al. (2019); Iran | Depression | RCT | 128 participants, high school students in Iran Hamadan City (all female, mild to moderate depressive symptoms, 15–17 years) | 2-phased DAD online course, first phase was qualitative study consisting of 2 interviews and group discussion. Second phase was preliminary website developed on data collected from phase 1, addressing common depressive themes using multimedia modules | CES-D, PSSS-R | Depressive symptoms, psychosocial measures | Baseline, 12 week, 24 week | Intervention group showed significant improvement in depressive symptoms in first follow-up (from 22.6 to 18.5 mean score on CES-D). These attenuated by 24 week (to 19.5 mean). |
| Ofoegbu et al. (2020); Nigeria | Depression | Group randomized trial | 192 EdTech students identified as having depression in Nigeria (62% female, age 19–29 years) | 10-week online intervention with GIAI, regular guidance from therapists via phone and internet who were staff of federal universities, and followed ICBT principles. Online modules included psychoeducation, peer support, cognitive disputation, role play, behavioral homework, and depression management. | BDI-II | Depressive symptoms | Baseline, 10-weeks, 14 weeks follow-up | First follow-up showed significant reduction in depressive symptoms of intervention group. Further follow-up indicated significant reduction in the intervention group, indicating GIAI was significantly efficacious in reducing depression. |
| Osorio et al. (2017); Colombia | Depression | Pilot feasibility/acceptability study | 15 patients discharged from treatment for MDD (18–65 years, n=10 female) | ASCENSO: online programme to support depression treatment and relapse prevention. The program includes reminder emails and web-based modules for symptom monitoring | PHQ-9, semi-structured interview | Depressive symptoms, usage of programme. | Baseline, every 2 weeks, post-test (8 weeks). | About half the sample made partial use of the programme; though only one participant completed all scheduled online monitoring. There was no reported increase in depressive symptoms during the trial. Participants reported favourable opinions |
| Rojas et al. (2018); Chile | Depression (major depressive episode) | Open-label (nonrandomised) trial | 250 patients from community hospitals in rural locations, (between 18–70 years, average 41.3 years, 86.4% female) with major depressive episode | Remote Collaborative Care for Depression (RCDC) for people living in rural areas in Chile. Programme used shared electronic health records, remote supervision and telephone monitoring. Once a week a specialist mental health team reviewed patient data and provided remote assistance. The intervention lasted 3 months. Control group received CAU | BDI-I, SF-36, SMAQ | Depressive symptoms, treatment adherence, health-related QoL | Baseline, 3- and 6-months follow-up | At 6 months follow-up, RCDC group showed higher satisfaction (OR 1.94; 95% CI 1.25–3.00) and better treatment adherence (OR 1.81; 95% CI 1.02–3.19) than CAU. No statistically significant differences emerged in depressive symptoms between the two groups. |
| Torrey et al. (2020); Colombia** | Depression and Alcohol Use Disorder | RCT | 2656 patients screened (1943 urban, 713 small town, 62% females, 37% 18–44 years and 63% older than 45) | 5-year multicenter intervention, DIADA, aiming to evaluate implementation of technology-supported screening, diagnosis, and care of depression among adults in primary care at six sites in Colombia. New primary care site implements the intervention every 6 months. | PHQ-9 | Depression symptoms, unhealthy substance use | Baseline, 6 months for second location, 1 year for first location | Primary care doctors trained with DIADA increased the percentage of patients diagnosed as having depression from next to 0% to 17% at different locations |
| Tulbure et al. (2018a); Romania | Depression | RCT | 79 participants (over 18 years, average 32.1 years, 82.3% female), recruited from local and national media, with BDI score between 14–50 and a diagnosis of current MDD or dysthymia | Two internet-supported interventions for depression: conventional CBT (C-CBT) or religious CBT (R-CBT). Control was waitlist | BDI-II, ATQ, QIDS-SR, BAI, QOLI, GQ, DURI | Depressive and anxious symptoms, QoL | Baseline, post-test and 6-months follow-up | Significant differences emerged in outcomes among the 3 conditions (Cohen’s d .45–1.89) in favour of the interventions. No significant differences emerged between C-CBT and R-CBT |
| Tulbure et al. (2018b); Romania | Depression and anxiety (transdiagnostic intervention) | RCT | 105 participants recruited from local and national media and diagnosed with anxiety and/or affective disorder | Web-based transdiagnostic intervention based on Unified Protocol for Transdiagnostic Treatment of Emotional Disorders that addresses common underlying mechanisms of anxiety and depression. Programme lasted 10 weeks. Control was waitlist | BDI, PSWQ, SPI, QOLI, WSAS, ODSIS, APS-R, PCL-5, YBOCS | Symptoms of anxiety and mood disorder, QoL, perfectionism, anxiety, sensitivity, social and work adjustment | Baseline, 10 weeks (post-test), 6-month follow-up | Relative to waitlist control, the intervention group appeared to show improvements in the primary outcome measures, anxiety sensitivity, symptom interference and QoL |
| Yang et al. (2019); China | Maternal (perinatal) depression and anxiety | RCT | 123 pregnant women over the age of 18 (average 31.3 years), recruited from outpatient clinics of women’s hospitals, and screening positive for depressive or anxious symptoms | Online mindfulness intervention, delivered over WeChat. 4 sessions, each lasting ~40 minutes, over 8 weeks. Control group received routine prenatal care | GADS, PHQ, FFMQ | Anxiety, depression and mindfulness | Baseline, 8 weeks (post-test) | Participants in the intervention group showed greater declines in depressive and anxious symptoms (p<.001) compared with those in the control group, as well as a significant improvement in mindfulness skills |
| Yeung et al. (2018); China | Depression | Pilot RCT | 75 adults from outpatients clinics, with significant depressive symptoms (as judged by a clinician), aged over 18 (average 33 years; 77% female) | Chinese translated version of MoodGYM along with CAU. MoodGYM is a computerised version of CBT for depression, consisting of 5 interactive modules. Participants completed 1 per week, and received weekly reminder emails or phone calls. Control group received CAU | CES-D | Depressive symptoms | Baseline, 5 weeks (post-test) | Intervention group showed a significantly higher improvement in depressive symptoms than control group (11 vs 5.9 points post-test, p=.02), with a medium effect size (d=.6) |
Indicates the presence of this study in Table 2 for depression and mood disorders in addition to Table 3 for anxiety disorders
Indicates the presence of this study in Table 2 for depression and mood disorders in addition to Table 4 for substance use and alcohol use disorders APS-R: Almost Perfect Scale-Revised
ATQ: Automatic Thoughts Questionnaire
BAI: Beck’s Anxiety Inventory
BDI/BDI-II: Beck’s Depression Inventory (Version I or II)
CES-D: Centre for Epidemiologic Studies Depression Scale
CPBQ: Child Prosocial Behavior Questionnaire
DURI: Duke University Religion Index
EPDS: Edinburgh Postnatal Depression Scale
FFMQ: Five Facet Mindfulness Questionnaire
GADS: Generalised Anxiety Disorder Scale
GQ: Gratitude Questionnaire
KIDSCREEN: quality of life questionnaire for children and adolescents
MAAS: Mindful Attention Awareness Scale
ODSIS: Overall Depression Severity and Impairment Scale
PCL-5: PTSD Checklist
PHQ-9: Patient Health Questionnaire
PSI: Psychological Screening Inventory
PSSS-R: Perceived-Social-Support-Scale-Revised
PSWQ: Penn State Worry Questionnaire
QIDS-SR: Quick Inventory of Depressive Symptomatology (Self-Report)
QoL: Quality of Life
QOLI: Quality of Life Index
RCT: randomised controlled trial
cRCT: cluster randomised controlled trial
RS-ES: Rosenberg Self-Esteem Scale
SCID: Structured Clinical Interview
SCS: Self-Compassion Scale
SF-36: Short Form Health Survey
SMAQ: Simplified Medication Adherence Questionnaire
SPI: Social Phobia Inventory
WBI: Well-Being Index
WHODAS: WHO Disability Assessment Schedule
WHO-5: World Health Organization- Five Well-Being Index
WSAS: Work and Social Adjustment Scale
YBOCS: Yale-Brown Obsessive Compulsive Scale
In another study from China, Guo et al. (2020) tested a 6-week internet-based program for mindfulness and self-compassion. At 3 months and 1 year following the intervention, participants showed decreases in depressive symptoms. A study in Iran demonstrated that an online course addressing common causes of depression significantly improved depressive symptoms in a 12-week follow up for female high school students (Moeini et al., 2019). Furthermore, a study on students implementing a 10-week online intervention in Nigeria demonstrated significant reduction in depressive symptoms compared to baseline (Ofoegbu et al., 2020). A multicenter intervention using a digital kiosk to support depression screening, diagnosis, and care in primary care facilities in Colombia resulted in an increase in the percentage of patients diagnosed with depression (Torrey et al., 2020).
Four studies used mobile phones for depression. In Nigeria, one study piloted mobile-telephone supported collaborative stepped care for depression, with the mobile-phone intervention group showing significantly lower depressive symptoms and quality of life compared to the control (Adewuya et al., 2019). Menezes et al. (2019) piloted a mobile-phone delivered emotional control intervention (CONEMO) in Peru and Brazil, and found that a high proportion of participants in each country achieved recovery from depressive symptoms at follow up (Menezes et al., 2019). In India, a guided self-help smartphone app based on principles of cognitive behavioural and interpersonal therapies was piloted, with improvements in depression and well-being emerging post-intervention (Mehrotra et al., 2018).
Two studies tested telepsychiatry through videoconferencing, including a Remote Collaborative Care framework for depression in Chile using shared health records, remote supervision and telephone support, with one study targeting adolescent depression (Martínez et al., 2018b) and the other targeting adult depression in rural areas (Rojas et al., 2018). Both reported positive treatment adherence and satisfaction, though depressive symptoms did not differ compared to the control groups. Finally, Maulik et al. (2017) trialled a digital decision support system (SMART) designed to help healthcare workers recognise, diagnose and manage common mental disorders including depression. The authors report a significant reduction in depression symptoms in patients screened using the SMART system.
3.3. Digital interventions for anxiety disorders and post-traumatic stress disorder
Table 3 lists studies evaluating Internet-based interventions for anxiety disorders including panic disorder, child and adolescent anxiety disorder, social anxiety, and post-traumatic stress disorder (PTSD). Ma et al. (2016) reported significant improvements in anxiety scores in China following 8 weeks of an online mindfulness intervention. In a study of an electronic decision support system in India to screen, diagnose, and manage common mental disorders, findings after three months of using the intervention demonstrated a significant reduction in anxiety scores (Maulik et al., 2017). In Romania, Ciuca et al. (2018) found that 12 weeks of online CBT appeared to reduce symptoms of panic disorder compared to a waitlist control (Ciuca et al., 2018). In a study of online CBT for child and adolescent anxiety disorders in Iran, anxiety symptoms at 12 weeks were lower compared to the control group (Karbasi and Haratian, 2018). In China, Kishimoto et al. (2016) tested an 8-week online CBT program for social anxiety disorder in adults (Kishimoto et al., 2016). At 8 weeks, symptoms of anxiety reduced in both experimental groups compared to the waitlist control (Kishimoto et al., 2016). In Brazil, Coelhoso et al. (2019) found that an 8-week intervention administered through a well-being mobile app significantly decreased overall and work-related stress in addition to significantly increasing general well-being in adult women participants.
Table 3.
Digital interventions for anxiety disorders and post-traumatic stress disorder
| Authors & Country | Disorder | Trial type | Sample | Methods | Instruments | Outcome measures | Time points | Findings |
|---|---|---|---|---|---|---|---|---|
| Cárdenas- López et al. (2016); Mexico | PTSD and Acute Stress Disorder (ASD) associated with trauma | Nonrandomised open-label trial | 9 individuals (aged 18–65 years) who were victims or witnesses of assault, kidnapping, or other criminal violence, recruited from a psychological assistance centre | Participants were separated into PTSD and ASD. Intervention consisted of 610 individual sessions once a week, lasting 90 mins each, with a clinical psychologist. Sessions 4–10 consisted of virtual reality scenario exposure. During sessions, participants were asked to talk about the traumatic event in first person in as much detail as possible | CAPS-I, PSS-SR, BDI, Treatment satisfaction questionnaire | PTSD and anxiety symptoms, depressive symptoms, satisfaction with intervention | Baseline, 12 weeks (post-test) | Post-treatment evaluation revealed a 30% improvement in measures of stress, anxiety and depression in both PTSD and ASD groups. A significant effect of time emerged pre- to post-test (p<.001), but there were no significant differences across groups (p>.05) |
| Ciuca et al. (2018); Romania | Panic disorder | RCT | 111 participants (aged 18–65, average 35.2 years, 68% female) recruited through media and GP recommendation s, diagnosed with panic disorder | Internet CBT (iCBT): 12 weeks of guided (via real-time video sessions) or unguided internet CBT. Control group was waitlist | PDSS-SR, PDSQ | Self-report panic symptoms | Baseline, 12 weeks (post-test), 6-month follow-up | Both active treatment conditions (guided and unguided iCBT) showed superior symptom outcomes (guided iCBT vs control: d=1.04–1.36; non-guided vs control: d=.07–1.06). Treatment gains were maintained at follow-up and guided iCBT became superior to unguided iCBT at 6 month follow-up (p<.05) |
| Coelhoso et al. (2019); Brazil | Psychological distress | 2-arm RCT | 148 women aged 20–60 years who completed high school, owned a mobile device, recruited from private tertiary care hospital in Sao Paulo, Brazil | Well-being mobile app had an 8-week program with 4 classes per week with a brief theoretical portion and a 15-min guided practice. The active control app also provided 4 assessments per week to encourage self-observation in participants and also conducted web-based questionnaires to assess subjective levels of stress and well-being at baseline, midintervention, and postintervention. | PSS-10, WHO-5 | Symptoms of Stress, 10-Item Perceived Stress Scale, 5-Item World Health Organization Well-Being Index | Baseline, 4 weeks (midinterven tion), and 8 weeks after baseline (postintervention) | The intervention group and control group showed significant increase in general well-being as a function of time (p=0.006). However, only the intervention group showed significant increase in work-related well-being (P<0.001) and significant reduction in work-related stress (p=0.004) and overall stress (p<0.001) |
| Karbasi & Haratian (2018); Iran | Child and adolescent anxiety | RCT | 30 girls aged 10–18 (average 14.2 years) with anxiety disorders, recruited from clinics of child and adolescent psychiatry in Isfahan | iCBT for anxiety disorders, consisting of 7 stages in a 3-month period. Participants did 1 hour each day of assignments for each stage. Control was CAU | SCARED | Symptoms of anxiety | Baseline, 3 months (post-test) | Intervention group post-test scores were significantly lower than control group scores (p<.001) |
| Kishimoto et al. (2016); China | Social anxiety | Controlled trial | 197 participants (average 24.6 years; 73% female), 75 of which had social anxiety disorder | iCBT for 8 weeks with and without guidance (weekly email by supervising therapist). Control was waitlist | SIAS, SPS, BDI | Symptoms of social anxiety | Baseline, 8 weeks (post-test) | For SIAS scores, both iCBT conditions were superior to waitlist control (guided vs waitlist: p<.001; unguided vs waitlist: p<.001), with small to large effect sizes (d = 0.29 – 1.03). No difference arose between the two iCBT conditions (p = .81). For SPS scores, both iCBT conditions were superior to waitlist control (p<.001), while the two iCBT conditions did not differ |
| Darvish et al. (2019); Iran | War-related PTSD | RCT | 66 male war veterans with PTSD (aged 42–61 years; average 48.4 years), recruited from the outpatient clinic of a hospital | Text messaging-based psychiatric nursing programme. Texts were sent daily to participants for 6 months. Content of messages covered: welcome message, description of PTSD symptoms, methods of accepting/dealing with PTSD, self-control, relaxation, deep breathing, insomnia, diet, suicidal thoughts. Control group received CAU | SRS-PTSD, SF-36 | PTSD symptom severity and QoL | Baseline, 6 months (post-test) | In the intervention group, a significant improvement in PTSD symptoms was observed pre- to post-intervention (p=.001) and also in QoL (p=.001). Frequency of recurrence of PTSD symptoms was significantly lower in the intervention group at 6 months (p=.03) |
| Ma et al. (2018); China* | Psychological distress (depression and anxiety) | RCT | 192 participants (aged 18–47; average 27.8 years; 42% female) recruited by web-based advertisements | 8-week online mindfulness intervention, with participants divided into 3 conditions: group mindfulness (GMBI), self-directed (SDMBI) and a discussion group (DG), as well as a blank control group | FFMQ, DERS, SRAS, SRDS | Mindfulness, self-reported symptoms of anxiety and depression, emotion regulation | Baseline, 8 weeks (post-test) | Mindfulness, emotion regulation and anxiety scores improved significantly in the GMBI and SDMBI groups pre- to post-test, with medium to large effect sizes (Cohen’s d values between 0.44 – 0.75). Between-group analysis showed that these outcome changes were highest in GMBI groups than all others |
| Maulik et al. (2017); India* | Common Mental Disorders (CMDs) | Pre-post evaluation | 238 participants (aged 18–92; average 39.7 years; 58.6% female) with CMDs, recruited from clinics in 30 rural villages | SMART: Systematic Medical Appraisal Referral and Treatment. This project trained lay village health workers and primary care physicians to screen, diagnose and manage individuals with CMDs using an electronic decision support system | PHQ-9, GAD-7, Knowledge, Attitude and Behaviour, Barriers to Access Care Evaluation; Treatment Stigma Subscale | Change in mental health utilisation and depression/anxiety scores, stigma, mental health awareness | Baseline, 3-months (post-test) | Significant reduction in anxiety scores between start and end of intervention among those who screened positive at the beginning of trial. Service utilisation increased, as well as awareness of mental health and stigma |
| Wang et al. (2016); China | Pre-post clinical evaluation | PTSD associated with different categories of trauma | 56 urban survivors of different trauma types and 90 rural survivors of 2008 Sichuan earthquake (aged 16–70; 24.5% female) | Chinese version of My Trauma Recovery (CMTR): a web-based self-help intervention for trauma. Participants accessed the programme for 1 month on their own or guided by volunteers in a counselling centre | PDS, SCL-D,, CSS, SFI | PTSD symptoms, depressive symptoms, coping, functioning | Baseline, 1 month (post-test), 3-month follow-up | 2 of the intervention modules showed consistent associated with improvement in PTSD and depressive symptoms, coping self-efficacy and social functioning. Other modules, such as relaxation, were associated with improvement in PTSD but a negative change in two social variables |
Indicates the presence of this study in Table 2 for depression and mood disorders in addition to Table 3 for anxiety disorders
CAPS-I: Clinician-Administered PTSD Scale
CSS: Crisis Support Scale
PDS: Posttraumatic Diagnostic Scale
PDSS-SR: Panic Disorder Severity Scale - Self-Report
PDSQ: Psychiatric and Diagnostic Screening Questionnaire
PSS-SR: PTSD Symptom Scale - Self-Report
PSS-10: Perceived Stress Scale-10 Item
SCARED: Screen for Child Anxiety Related Emotional Disorders
SCL-D: Symptom Checklist for Depression
SFI: Social Functioning and Impairment Questionnaire
SIAS:Social Interaction Anxiety Scale
SPS: Social Phobia Scale
SRS-PTSD: Self-Rating Scale for Post-Traumatic Stress Disorder
STAI: State-Trait Anxiety Inventory for Adults
WHO-5: World Health Organization- Five Well-Being Index
Of the studies targeting PTSD, one from Mexico used virtual reality, where victims or witnesses of violent crimes were exposed to virtual reality scenarios and asked to relay the traumatic event in as many details as possible (Cárdenas-López et al., 2016). At 12-weeks, participants showed improvement in measures of stress, anxiety and depression. In another study, Wang et al. (2016) tested an adapted version of the online My Trauma Recovery self-help intervention for traumas of diverse nature in China, including natural disaster (i.e., earthquake) (Wang et al., 2016). The triggers and self-talk modules of the programme were associated with improvements in PTSD and depression, coping self-efficacy and social functioning, and the relaxation module was associated with improvements in PTSD. In a study from Iran, war veterans with PTSD received daily texts with information about signs and symptoms of PTSD, relaxation techniques, diet, suicidal thoughts and behaviour (Darvish et al., 2019). At 6 months, improvements in PTSD symptoms and quality of life were observed, as well as lower frequency of recurrence of post-traumatic symptoms.
3.4. Digital intervetions for alcohol use and substance use disorders
As summarized in Table 4, four studies targeted alcohol use disorders, and three studies targeted substance use, including heroin, marijuana and methamphetamine. In Brazil, Baldin et al. (2018) tested a web intervention for binge-drinking in nightclub attendees (Baldin et al., 2018). Intervention participants were exposed to normative feedback relating to alcohol consumption, risk of dependence, financial consequences, driving while under the influence, and tips to reduce damage. After 6 months, there appeared to be reductions in problem drinking among intervention participants. Bedendo et al. (2019) found that a web-based personalised normative feedback intervention for college students could reduce the number of typical drinks consumed compared to the control group (Bedendo et al., 2019). In India, Nandyal et al. (2019) evaluated the feasibility and acceptability of using mobile telephones to follow up with patients with Alcohol Dependence Syndrome. It was found that after 6 months, the collection of outcomes was improved by 35% and that almost 30% of patients were able to remain completely abstinent from alcohol during this follow-up period. A multicenter study in Colombia, also mentioned in section 3.2 above, implemented a digital kiosk to identify and treat alcohol use disorder and found that this intervention increased the percentage of patients diagnosed with the disorder across different primary care sites (Torrey et al., 2020).
Table 4.
Digital interventions for substance use and alcohol use disorders
| Authors & Country | Disorder | Trial type | Sample | Methods | Instruments | Outcome measures | Time points | Findings |
|---|---|---|---|---|---|---|---|---|
| Baldin et al. (2018); Brazil | Binge drinking | RCT | 465 nightclub patrons from Sao Paulo, classified as problem drinkers (aged 18–55; average 24.7 years, 35.5% female) | Web-based intervention consisting of exposure to normative feedback regarding alcohol consumption, risk, money spent, drink-driving, risk classification (AUD) and tips to reduce alcohol-related damage. Control group had no intervention and just completed a questionnaire about drinking behaviour (AUDIT) | AUDIT | Various measures of drinking behaviour | Baseline, 6 months | A significant reduction in binge-drinking during the week was observed in 38% of participants in the experimental group at 6 months; this reduction was not seen in the control group. However, upon observation of group-time interaction, the results are not significant and the reduction in ‘lack of control’ when drinking was marginally significant only |
| Bedendo et al. (2019); Brazil | Alcohol use disorder | RCT | 4460 college students (between 18–30 years; average 22 years; 51% female), divided into high and low motivation, recruited through Email and Facebook | Web-based Personalised Normative Feedback (PNF) intervention, consisting of several components: 1) drinking profile (AUDIT risk level, binge-drinking frequency); 2) gender-specific normative comparisons; 3) practical costs (e.g. money spent on alcohol); 4) alcohol-related consequences; 5) low-risk drinking limits and protective strategies. Students took 5–10 minutes to complete the intervention at each time point. Control group received the basic assessment only (no PNF) | AUDIT | AUDIT score, typical number of drinks consumed | Baseline, 1– 3- and 6months. | PNF intervention reduced the number of typical drinks consumed at all follow-up points compared to control (all p values <.05). Low motivation students receiving PNF experienced an increase in AUDIT score at T3 (p<.001) |
| Liang et al. (2018); China | Substance use (principally heroin but also other) | Pilot RCT | 75 participants (aged 18–65; average 41.6 years; 29.3% female) who had used heroin in the last 30 days. Recruited from methadone maintenance treatment clinics and a social worker consortium | S-Health: a bilingual smartphone app based on principles of CBT to support addiction recovery. Participants received text messages and daily surveys on cravings, affect, triggers, responses to triggers, and social contexts | I-PANAS-SF, urine tests, Addiction Severity Index | Cravings, affect, trigger thoughts, place and situations, responses to triggers, social context, urine test-confirmed abstinence | Baseline, 4 weeks (post-test) | At post-test, 26.2% of intervention group and 50% of control group had positive urine tests (p=.06). The number of self-reported days using drugs in the intervention group was lower than controls (p<.05) |
| Nandyal et al. (2019); India | Alcohol Dependence Syndrome (ADS) | Feasibility/ac ceptability study | 51 participants (diagnosed with ADS, age 22–58) | After initial assessment of patients in psychiatry department of tertiary care hospital, a follow-up was conducted after 6 months through a combination of in-person and phone interviews with patients and caregivers. | Short alcohol dependence data questionnaire, rotter’s scale for locus of control, clinical institute of withdrawal assessment of alcohol scalerevised | ADS symptoms, consumption of alcohol | Baseline, 6 months | After 6 months, 27.5% of participants had complete abstinence. 72% of participants had lapses/relapses, and 62% were abstinent for 1 month at the time of follow-up. The collection of outcomes was improved by 35.2%. The lower rate of abstinence is hypothesized to be caused by the ability to contact patients via mobile phone for patients who dropped out of hospital visits. |
| Tiburcio et al. (2018); Mexico | Substance use (marijuana, inhalants, cocaine) | RCT | 74 participants (over 17 years; average age not given, but most aged 18–25; 12.2% female) recruited from two addiction treatment centres | Web-based help programme for drug abuse and concurrent depression (PAADD), based on the transtheoretical model of change, and incorporating elements of CBT. Completion of programme required approx. 8 weeks if used for 1 hour per week. A second group received ASSIST self-help guide. Control group received CAU | ASSIST, Timeline Followback, DAST-20, RCQ | Number of days of substance use, severity of substance use, depressive symptoms, readiness to change | Baseline, 8 weeks (post-test), 1-month follow-up | No significant difference arose in average number of days of substance use or severity of substance abuse between the three conditions. Both outcomes decreased independent of group, with moderate to strong effect size (between d = −0.7 and −1.1). A reduction in depressive symptoms was also observed, again independent of group |
| Torrey et al. (2020); Colombia** | Alcohol Use Disorder and Depression | RCT | 2656 patients screened (1943 urban, 713 small town, 62% females, 37% 18–44 years and 63% older than 45) | 5-year multicenter intervention, DIADA, aiming to evaluate implementation of technology-supported screening, diagnosis, and care of depression among adults presenting or primary care visits at six sites in Colombia. New primary care site implements the intervention every 6 months. | PHQ-9 | Depression symptoms, unhealthy substance use | Baseline, 6 months for second location, 1 year for first location | Primary care doctors trained with DIADA increased the percentage of patients diagnosed as having Alcohol Use Disorder from next to 0% to 2% at different locations |
| Zhu et al. (2018); China | Substance use (methampheta mine) | RCT | 40 male patients at a compulsory methamphetamine rehabilitation centre in Shanghai (aged 18–49; average 33 years). Patients had moderate to severe addiction | Mobile-based cognitive addiction therapy app (CCAT) (and detox) based on cognitive rehabilitation therapy, with the aim of improving cognitive function and eliminating 33 years). Patients had moderate to severe addiction drug-related attention bias. Intervention was delivered for 4 weeks: 20 sessions total, 5 times a week, each session approx. 60 mins. Control group received CAU | CogState test, ISL, CPAL, DDT, IGT, BART | Cognitive function, impulsive risk-decision making, attention bias | Baseline, 4 weeks (post-test) | Compared to control, CCAT significantly improved cognitive function (p=.01) and impulsive risk-decision making (p<.001) in experimental group |
Indicates the presence of this study in Table 2 for depression and mood disorders in addition to Table 4 for substance use and alcohol use disorders
ASSIST: Alcohol, Smoking and Substance Involvement Screening Test
AUDIT: Alcohol Use Disorders Identification Test
BART: Balloon Analogue Risk Task
CPAL: Continuous Paired Association Learning task
DAST-20: Drugs Abuse Screening Test
DDT: Delay Discounting Task
IGT: Iowa Gambling Task
I-PANAS-SF: Positive and Negative Affect Schedule
ISL: International Shopping List
PHQ-9: Patient Health Questionnaire
RCQ: Readiness to Change Questionnaire
Among the studies targeting substance use, one piloted S-Health, a smartphone app based on principles of CBT to support recovery from addiction, with a sample consisting principally of people with heroin addiction in China (Liang et al., 2018). Participants received daily messages and surveys through the app to measure cravings, mood, triggers and other aspects relating to cognitive components of addiction. The intervention group had fewer positive urine tests (indicating relapse) and fewer self-reported days using drugs compared to the control group. Another study from China compared an app-delivered cognitive addiction therapy (CCAT) for methamphetamine use disorder focused on ameliorating patients’ cognitive functioning and reducing drug-related cognitive biases with regular detoxification treatment (Zhu et al., 2018). Participants in the CCAT group showed higher performance on measures of cognitive function than the control, though no substance use-related outcomes were reported. In a 3-arm study from Mexico, individuals with substance use disorders including marijuana, inhalants and cocaine dependence, were allocated to a web-based program for drug abuse and concurrent depression (PAADD) based on the transtheoretical model of change along with elements of CBT, a self-help guide based on ASSIST (Alcohol, Smoking and Substance Involvement Screening Test), or care-as-usual (Tiburcio et al., 2018). There were decreases in the average days of drug use and severity of dependence across all conditions, though no significant differences between groups.
3.5. Digital interventions for community mental health services including common and severe mental disorders
Four studies aimed to improve community based mental health services for a range of disorders including schizophrenia and psychotic disorders using SMS reminders and digital support systems for frontline healthcare workers (Table 5). In India, Singh et al. (2017) conducted a randomized controlled trial of a text-messaging intervention to improve follow-up for patients at a community mental health clinic (Singh et al., 2017). Results showed a higher proportion of participants receiving text-message reminders attended their appointment compared to the control group. A pilot study from South Africa tested a multi-component intervention for adults with psychotic disorders which integrated care-as-usual, a psychoeducation session, and text message reminders for doctor appointments (Sibeko et al., 2017). At follow up, intervention participants appeared to show better understanding of their diagnosis, and were less likely to miss their first clinic visit and to experience relapse in the 9 months following hospital discharge, though differences compared to usual care were not significant. In a second study from India, the feasibility and initial clinical effectiveness of an Internet-based computerized Clinical Decision Support System for healthcare workers, based on the DSM-IV and ICD-10 criteria, was piloted in rural areas for people with a various psychiatric diagnoses (e.g., mood disorders, substance and alcohol use disorders, stress disorders and psychotic disorders) (Malhotra et al., 2019). The online intervention included 3 separate modules for diagnosis, management, and follow-up, and emerged as feasible and acceptable to patients and health care workers, and achieved high sensitivity in screening for all disorders, but low positive predictive values for most disorders except substance and alcohol use. Lastly, a randomized controlled trial from China tested LEAN (Lay health supporters, E-platform, Award and iNtegration) for adults with schizophrenia in rural, resource-poor communities (Xu et al., 2019). This programme used text messages to remind participants of medication, provide health education, and promote self-monitoring of early signs of relapse. At 6 months, the intervention group was significantly more likely to have adhered to medication than the control group, and showed a significant reduction in risk of relapse and hospital readmission.
Table 5.
Digital interventions for community mental health services including common and severe mental disorders
| Authors & Country | Disorder | Trial type | Sample | Methods | Instruments | Outcome measures | Time points | Findings |
|---|---|---|---|---|---|---|---|---|
| Malhotra et al. (2019); India | Mental health problems (general) in remote areas of India | Feasibility/initial clinical effectiveness study | 2594 psychiatric patients in rural areas. Most common diagnoses were mood disorders, substance or alcohol use disorders, anxiety and stress-related disorders and psychotic disorders | Internet-based, computerized Clinical Decision Support System (CDSS): a digital diagnostic and management application to improve delivery of mental healthcare in rural areas. Included 3 modules for diagnosis, management and follow-up respectively, based on DSM-IV and ICD-10 criteria. The aim was to replicate a routine clinical situation. Psychologist or social worker used the app to interview patients, choose medication or psychotherapy as per CDSS guidelines. Patient was assessed at follow-up using the relevant module | MINI/MINI-KID, measures of validity, reliability, feasibility and satisfaction | Validity, reliability and feasibility of CDSS; satisfaction with intervention | Unclear. Follow-up timepoints varied depending on the nature of a participant’s illness and treatment | Sensitivity of screening tool was high for all disorders (ranging from 48–99%). Positive predictive values were low for most disorders except alcohol and substance use disorders. Online diagnostic module was acceptable/satisfactory to patients and interviewers |
| Sibeko et al. (2017); South Africa | Psychotic disorder (various) | Pilot RCT | 77 participants (average 35.5 years; 28.6% female) with schizophrenia spectrum disorder, bipolar mood disorder, or substance use induced psychotic disorder, recruited from Valkenburg hospital | A treatment-partner and text message intervention. Incorporated CAU with addition of 1) a treatment partner contracting and psychoeducation session and 2) text message reminders of clinic appointments. The aim of the intervention was to improve adherence to mental health services for people with psychotic disorder. Control group received CAU | PANSS, CGI, GAF, CAN,, EUROQUOL, VAS, MARS | Clinic attendance, adherence, symptoms, readmission rate at 9 months | Baseline, post-discharge, 3-month follow-up | At 3-month follow-up, intervention participants understood their diagnosis better than CAU group. CAU group were more likely to miss their first clinic visit and relapse in the 9 months following discharge, and to show worsening PANSS scores. Efficacy outcomes tended to favour the intervention but did not reach statistical significance |
| Singh et al. (2017); India | Unspecified diagnoses (various mental illnesses) | RCT | 214 patients (40.6% female) | Intervention to improve follow-up rates at a community mental health clinic. SMS group received SMS 1 day before appointment at clinic. Control group received no SMS. At second-level intervention patients from both groups who missed first appointment were given a voice call reminder | Measure of attendance | Attendance at clinic | No fixed time points | At first SMS intervention level, 62.3% of SMS group reached their appointment, compared to 45.4% of the CAU group. At second-level intervention, 66 of 88 came for follow-up. Diagnosis of alcohol dependence was significantly associated with missing appointments |
| Xu et al. (2019); China | Schizophrenia | RCT | 278 community-dwelling villagers with schizophrenia (average 46 years; 55.4% female) | LEAN intervention: Lay health supporters, Eplatform, Award and iNtegration). This featured recruitment of lay health support and text messages for medication reminders, psycho- and health education, monitoring of early signs of relapse, and linkage to primary healthcare for people with schizophrenia in rural resource-poor China. Control group received CAU | Score of adherence to antipsychotic medication, BARS, DAI, CGI for schizophrenia, WHODAS, GASS | Medication adherence, patient symptoms, functioning, relapse, re-hospitalisation, death for any reason, violence | Baseline, 6 months | Medication adherence was significantly improved at 6 months (0.48 in control group, 0.61 in intervention; representing a 27% improvement in the LEAN group), with moderate effect size of d = 0.38 reported, as well as a significantly reduced risk of relapse and re-hospitalisation with the intervention. The two groups did not differ on other outcomes |
BARS: Brief Adherence Rating Scale
CAN: Camberwell Assessment of Unmet Needs
CGI: Clinical Global Impressions
DAI: Drug Attitude Inventory
EUROQUOL: Quality of Life measurement
GAF: Global Assessment of Function
GASS: Glasgow Antipsychotic Side-Effect Scale
MARS: Medication Adherence Rating Scale
VAS: Visual Analogue Scale
3.6. Digital interventions for suicide prevention
Two studies focused on suicide prevention using mobile and web-based interventions (Table 6). In the first study, college students in China and Australia completed two mini-modules covering risk factors, warning signs, stigma surrounding suicide, and perceived barriers to help-seeking (Han et al., 2018). Compared to an attentional control group, the experimental group showed improvement in suicide literacy, though there were no differences in help-seeking beliefs and intentions. In Mexico, Martinez-Miranda et al. (2019) conducted a pilot study to determine feasibility and acceptability of an intervention using a virtual conversational agent accessible by mobile app for the prevention and detection of suicidal behaviours (Martínez-Miranda et al., 2019). At 8 weeks, participants favourably rated the emotional competence of the virtual conversational agent and showed high programme adherence (though no outcomes related to change in suicidal behaviors were reported).
Table 6.
Digital interventions for suicide prevention
| Authors & Country | Disorder | Trial type | Sample | Methods | Instruments | Outcome measures | Time points | Findings |
|---|---|---|---|---|---|---|---|---|
| Han et al. (2018); China (and Australia) | Suicidal thoughts, tendencies and behaviour | RCT | 156 Chinese students and 101 Australian students (18–30 years, average 19.3 years; 79.5% female) from universities in China and Australia | Brief, two-module online psychoeducational program (ProHelp) to encourage help-seeking behaviour for university students with suicidal ideation and behaviour. These modules each lasted 5 minutes, and addressed risk factors, warning signs, stigma and perceived barriers to help-seeking, with the aim of preventing suicide in university students. Control group completed an attentional control programme | GHSQ, Attitudes Towards Seeking Professional Psychological Help Scale; LSS, SSS; BHSS, PHQ-9 | Professional help-seeking beliefs, intentions and attitudes; suicide literacy, stigma, social support, self-reliance, preparedness to assist a suicidal friend, evaluation of program | Baseline, post-test, 1-month follow-up | No significant difference was found between control and experimental group on professional help-seeking beliefs and intentions. Both groups’ help-seeking attitudes increased during study (p=.003 at post-test, p=.008 at follow-up). A significant improvement in suicide literacy at post-test was found for the experimental group (p=.015) |
| Martinez-Miranda et al. (2019); Mexico | Suicidal behaviour | Exploratory pilot acceptability study | 18 participants (20–53 years; average 31.5 years; 11 female) recruited by mental health specialists | Embodied virtual conversational agent used as the main interface of HelPath: a mobile application addressed to individuals detected with suicidal behaviours (ideation, planning or attempt). Participants were invited to use HelPath daily for 8 weeks, as well as a fortnightly interview face-to-face with the specialist | Unstructured brief interviews; Likert-based questionnaire to assess ECA features | Acceptability of program, emotional competence of ECA, adherence | Baseline, follow-up each 2 weeks, 8 weeks (post-test) | ECA emotional competence and adherence rate were rated positively |
BHSS: Barriers to Help-Seeking Scale
CSQ-8: Client Satisfaction Questionnaire
DERS: Difficulties in Emotion Regulation Scale
HHS: Herth Hope Scale
GAD-7: Generalised Anxiety Disorder Questionnaire
GHSQ: General Help-Seeking Questionnaire
LSS: Literacy of Suicide Scale
MINI/MINIKID: Mini International Neuropsychiatric Interview
MLQ: Meaning in Life Questionnaire
PSS: Perceived Stress Scale
SRAS: Self-Rating Anxiety Scale
SRDS: Self-Rating Depression Scale
STS: Self-Transcendence Scale
SSS: Stigma of Suicide Scale
ZSAS: Zung Self-Rating Anxiety Scale
ZSDS: Zung Self-Rating Depression Scale
3.7. Quality Assessment of Included Studies
As outlined in Table 7, the quality scores of the included studies varied widely, from 2 to 13, with an average of 8.6 (SD= 2.6) and a median of 9. A total of 17 studies scored at least 10 on the MQRS, suggesting moderate quality. Of these, only two studies had scores of 13. No studies were considered high quality, meeting the criteria of 14 or greater. Among the moderate quality studies, most used randomized controlled designs and reported well-defined outcome measures. The remaining studies scored below 10, with the main drivers of lower quality being the short follow up length, low follow up rate, and lack of independent outcome assessment.
Table 7.
Assessment of methodological quality of included studies.
| Quality Criteria* | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | Total Quality Score (0 Low to 16 High) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author (year) | A. Study Design (0–3) | B. Replicability (0–1) | C. Baseline (0–1) | D. Quality Control (0–1) | E. Follow-Up Length (0–2) | F. Follow-Up Rate (0–2) | G. Objective Measurement of Outcomes (0–1) | H. Dropouts (0–1) | I. Independent (0–1) | J. Analyses (0–1) | K. Study Site (0–1) | L. Collateral (0–1) | |
| Depression & Mood Disorders | |||||||||||||
| Adewuya et al. (2019); Nigeria | 3 | 1 | 1 | 1 | 2 | 2 | 1 | 1 | 0 | 1 | 0 | 0 | 13 |
| Anttila et al. (2019); Thailand | 1 | 1 | 1 | 0 | 0 | 2 | 0 | 1 | 0 | 1 | 1 | 0 | 8 |
| Arjadi et al. (2018); Indonesia | 3 | 0 | 1 | 0 | 1 | 2 | 1 | 0 | 0 | 1 | 0 | 0 | 9 |
| Guo et al. (2020); China | 3 | 1 | 1 | 1 | 2 | 2 | 1 | 1 | 0 | 1 | 0 | 0 | 13 |
| Ma et al. (2018); China* | 3 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 5 |
| Martinez et al. (2018); Chile | 3 | 1 | 1 | 0 | 0 | 2 | 1 | 1 | 0 | 1 | 0 | 0 | 10 |
| Maulik et al. (2017); India* | 3 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 7 |
| Mehrotra et al. (2018); India | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| Menezes et al. (2019); Brazil & Peru | 1 | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 1 | 1 | 0 | 10 |
| Moeini et al. (2019); Iran | 3 | 0 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 1 | 0 | 0 | 11 |
| Ofoegbu et al. (2020); Nigeria | 3 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 8 |
| Osorio et al. (2017); Colombia | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 5 |
| Rojas et al. (2018); Chile | 2 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 0 | 0 | 12 |
| Torrey et al. (2020); Colombia** | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 6 |
| Tulbure et al. (2018a); Romania | 3 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 9 |
| Tulbure et al. (2018b); Romania | 3 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 10 |
| Yang et al. (2019); China | 3 | 1 | 1 | 1 | 0 | 2 | 1 | 0 | 0 | 1 | 0 | 0 | 10 |
| Yeung et al. (2018); China | 3 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 10 |
| Anxiety & Post-traumatic Stress disorders | |||||||||||||
| Cárdenas-López et al. (2016); Mexico | 2 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 5 |
| Ciuca et al. (2018); Romania | 3 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 9 |
| Coelhoso et al. (2019); Brazil | 3 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 9 |
| Karbasi & Haratian (2018); Iran | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 4 |
| Kishimoto et al. (2016); China | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 5 |
| Darvish et al. (2019); Iran | 3 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 7 |
| Ma et al. (2018); China* | 3 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 5 |
| Maulik et al. (2017); India* | 3 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 7 |
| Wang et al. (2016); China | 1 | 1 | 0 | 0 | 0 | 2 | 1 | 0 | 0 | 1 | 0 | 0 | 6 |
| Substance Use and Alcohol Use Disorders | |||||||||||||
| Baldin et al. (2018); Brazil | 3 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 10 |
| Bedendo et al. (2019); Brazil | 3 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 10 |
| Liang et al. (2018); China | 3 | 1 | 1 | 0 | 0 | 2 | 1 | 1 | 0 | 1 | 0 | 0 | 10 |
| Nandyal et al. (2019); India | 2 | 1 | 0 | 0 | 1 | 2 | 1 | 1 | 0 | 1 | 0 | 0 | 9 |
| Tiburcio et al. (2018); Mexico | 3 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 11 |
| Torrey et al. (2020); Colombia** | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 6 |
| Zhu et al. (2018); China | 3 | 1 | 0 | 1 | 0 | 2 | 1 | 1 | 0 | 1 | 0 | 0 | 10 |
| Severe Mental Disorders | |||||||||||||
| Malhotra et al. (2019); India | 3 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 9 |
| Sibeko et al. (2017); South Africa | 3 | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 1 | 0 | 0 | 11 |
| Singh et al. (2017); India | 3 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 5 |
| Xu et al. (2019); China | 3 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 1 | 0 | 0 | 12 |
| Suicide Prevention | |||||||||||||
| Han et al. (2018); China (and Australia) | 3 | 0 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 1 | 0 | 0 | 10 |
| Martinez-Miranda et al. (2019); Mexico | 1 | 1 | 0 | 1 | 0 | 2 | 1 | 1 | 0 | 1 | 0 | 0 | 8 |
MQRS (Methodological Quality Rating Scale) measures 12 dimensions of methodological quality with cumulative ratings ranging from 0 (poorest quality) to 16 (highest quality), with scores of ≥14 considered high quality (Miller & Wilbourne, 2002).
4. Discussion
We identified 37 studies published between 2016 and 2020 evaluating digital interventions for the treatment and prevention of mental disorders in LMICs. Our review expands on recent reviews (Jiménez-Molina et al., 2019; Kaonga and Morgan, 2019; Naslund et al., 2017), reflecting continued growth in digital mental health research in LMICs. Included studies were primarily from East Asia (i.e., China) (Guo et al., 2020; Han et al., 2018; Kishimoto et al., 2016; Liang et al., 2018; Ma et al., 2018; Wang et al., 2016; Xu et al., 2019; Yang et al., 2019; Yeung et al., 2018; Zhu et al., 2018) and Central or Latin America (Baldin et al., 2018; Bedendo et al., 2019; Cárdenas-López et al., 2016; Coelhoso et al., 2019; Martínez et al., 2018b; Martínez-Miranda et al., 2019; Menezes et al., 2019; Osorio et al., 2017; Rojas et al., 2018; Tiburcio et al., 2018; Torrey et al., 2020), followed by South Asia (i.e. India) (Malhotra et al., 2019; Maulik et al., 2017; Mehrotra et al., 2018; Nandyal et al., 2019; Singh et al., 2017). Fewer studies were from Africa (Adewuya et al., 2019; Ofoegbu et al., 2020; Sibeko et al., 2017), Southeast Asia (Anttila et al, 2019; Arjadi et al., 2018), Eastern Europe (Ciuca et al., 2018; Tulbure et al., 2018a; Tulbure et al., 2018b), or the Middle East (Darvish et al., 2019; Karbasi & Haratian, 2018; Moeini et al., 2019). No studies were identified from Western or Central Asia. Our review has the strength of adding new evidence to support potential benefits of digital interventions across various cultural contexts and a broad range of mental health problems. However, our findings suggest that, while lower-income countries in some geographical regions are producing a relatively high amount of research, other areas such as Africa and Western, Central and Southeast Asia are less well-served by research.
4.1. Which mental disorders are being targeted by digital intervention studies in LMICs?
Nearly half the studies evaluated digital interventions targeting depression and mood disorders, which is expected as depression accounts for the highest mental health-related global burden of disease (Rehm and Shield, 2019), and is consistent with prior reviews of digital mental health interventions in LMICs and other low-resource settings (Kaonga and Morgan, 2019; Naslund et al., 2017) as well as high income countries (Lal and Adair, 2014). Remaining studies targeted anxiety disorders and post-traumatic stress disorder, alcohol use and substance use disorders, and community mental health services including care for psychotic disorders. Only two studies addressed suicide prevention, which is perhaps unsurprising considering the social and religious stigma, and legal implications, associated with suicide in many countries (Khan, 2005; Uddin et al., 2019).
4.2. Are digital mental health interventions acceptable in LMICs?
Several studies reported outcomes relating to feasibility and acceptability, including program usage, adherence to interventions, satisfaction or favorability. Consistent with prior research, digital interventions appeared to be well received by participants, with favourable reporting of satisfaction and acceptance (Adewuya et al., 2019; Anttila et al., 2019; Cárdenas-López et al., 2016; Han et al., 2018; Malhotra et al., 2019; Martínez-Miranda et al., 2019; Nandyal et al., 2019; Osorio et al., 2017). These favourable satisfaction ratings suggest that digital and online delivery of mental health interventions may be suitable and acceptable for diverse patient populations, given the variability in geographical locations in the included studies. Participant-reported acceptability is also important as this may increase intervention engagement and sustained use, which in turn could contribute to greater improvements in desired mental health outcomes. Future studies of digital technology for mental health should explore specific intervention features associated with participant satisfaction and acceptability, and if these features vary by different contexts in LMICs, and whether modifying these features can result in greater intervention uptake and improvements in clinical outcomes.
4.3. Are digital interventions effective in treating mental health conditions in LMICs?
This updated review found a greater proportion of current studies reporting potential effectiveness and overall change in mental health outcomes, suggesting that there have been improvements in design and implementation of digital mental health interventions in LMICs as well as application of more rigorous research methods as the field continues to advance. This is also reflected by the large number of randomized controlled trials (n = 27; 73%); yet, despite moderate quality ratings observed in close to half of the included studies, there were no studies considered high quality on the MQRS (Miller & Wilbourne, 2002). Importantly, nearly two thirds of included studies (n = 23) reported improvements in mental health measures at follow-up (Adewuya et al., 2019; Arjadi et al., 2018; Bedendo et al., 2019; Ciuca et al., 2018; Coelhoso et al., 2019; Guo et al., 2020; Karbasi and Haratian, 2018; Darvish et al., 2019; Kishimoto et al., 2016; Liang et al., 2018; Ma et al., 2018; Maulik et al., 2017; Mehrotra et al., 2018; Menezes et al., 2019; Moeini et al., 2019; Ofoegbu et al., 2020; Tulbure et al., 2018a; Tulbure et al., 2018b; Wang et al., 2016; Xu et al., 2019; Yang et al., 2019; Yeung et al., 2018; Zhu et al., 2018). Of these studies, 15 involved online (n = 14) or computer software (n = 1) interventions, 7 were mobile apps, and one was an SMS text-messaging service. Most studies targeted depression or anxiety disorders (n = 20), with a further two studies addressing alcohol or substance abuse, and one study targeted schizophrenia.
Where effect sizes were given, these were generally promising. Studies of online interventions reported effect sizes, including Tulbure et al. (2018a), who reported Cohen’s d values between 0.45 and 1.89, indicating a reduction in depressive symptoms after using online CBT in Romania, that was maintained at 6 months. An online mindfulness intervention in China reported reductions in anxiety and depression with medium to large effect sizes (d = 0.44 – 0.75) (Ma et al., 2018). Kishimoto et al. (2016) noted reductions in anxiety with their internet CBT intervention, with effect sizes between d = 0.29 and 1.03. These studies suggest that online interventions could be effective in reducing symptoms of anxiety and depression in some settings. However, only Tulbure et al. (2018a) had a follow-up period of 6 months, while Ma et al. (2018) had no follow-up period. Without a meaningful follow-up period, it is not possible to determine whether effects are sustained over time, a notable limitation reflected in the methodological quality assessment for many of the included studies, where 23 studies (62%) had less than 6-months follow up. Considering the high recurrence rates and chronicity of common mental disorders, it is crucial to understand whether mental health interventions are effective in the long term (Koopmans et al., 2011).
It is difficult to draw conclusions about whether digital interventions are more effective for treating some mental disorders than others, due to the disproportionate number of studies targeting each disorder type. The finding that most studies evaluating digital interventions for common mental disorders reported significant findings (n = 20 out of 23) is promising. These findings also point to the potential applicability of digital technologies in treating mental disorders across diverse social and cultural contexts. However, many of these studies were limited by small sample sizes, short follow-up periods, and only 8 of the studies reporting positive findings included standardised effect sizes.
Additionally, where control groups were present, it is important to note that several studies reported no differences between intervention and control groups (Anttila et al., 2019; Baldin et al., 2018; Cárdenas-López et al., 2016; Martínez et al., 2018b; Rojas et al., 2018; Sibeko et al., 2017; Tiburcio et al., 2018). The nature of the interventions trialled in these studies was varied, with two telepsychiatry interventions, one SMS-based intervention, three web-based and one virtual reality intervention reporting no statistically significant differences in clinical outcomes. However, several of these studies reported other positive findings which could be of potential clinical interest. For example, although there was no significant improvement in symptoms, participants with psychotic disorders receiving Sibeko et al.’s (2017) SMS intervention reported better understanding their diagnosis than control participants. This may present clinical utility, as cognitive insight and awareness in psychosis may be associated with more favourable therapy outcomes (Perivoliotis et al., 2009). In two telepsychiatry studies, Rojas et al. (2018) and Martinez et al. (2018) reported better medication adherence in the intervention groups compared with the control. Although these findings were not paired with statistically significant improvements in depressive symptoms, they could suggest clinical utility of digital services in enhancing treatment adherence among patients with depression. Furthermore, the heterogeneity in the types of outcome measures, and study durations limits the possibility of conducting a meta-analysis on the included studies, which would be necessary to determine the efficacy of digital mental health interventions in LMICs. This demonstrates that despite increasing volumes of research on the topic and frequent reporting of clinical outcomes, there remain limitations for drawing conclusions about the relative effectiveness of these digital mental health interventions and the variability across diverse settings and population groups.
4.4. Which technologies are most suitable to deliver interventions?
More than half of the studies used online interventions accessible from a mobile device or computer, involving either new content developed specifically for the study or adaptations to existing evidence-based psychosocial treatments such as CBT or mindfulness therapy (Anttila et al., 2019; Arjadi et al., 2018; Baldin et al., 2018; Bedendo et al., 2019; Ciuca et al., 2018; Guo et al., 2020; Han et al., 2018; Karbasi and Haratian, 2018; Kishimoto et al., 2016; Ma et al., 2018; Moeini et al., 2019; Ofoegbu et al., 2020; Osorio et al., 2017; Tiburcio et al., 2018; Tulbure et al., 2018a; Tulbure et al., 2018b; Wang et al., 2016; Yang et al., 2019; Yeung et al., 2018). For example, one study described cultural adaptations to an existing program, such as adapting a Chinese version of My Trauma Recovery (Wang et al., 2016), while another study used a well-established and popular social media platform called WeChat to deliver a mindfulness intervention to pregnant women in China (Yang et al., 2019). Interestingly, this study by Yang et al. (2019) was the only study identified in this review using a popular social media platform, which highlights a gap in the current literature. With most of the world’s social media users located in LMICs, there may be opportunities to leverage the widespread reach of these platforms to support mental health promotion efforts and service delivery (Naslund et al., 2020). Our findings illustrate continued growth in the use of online interventions for mental disorders, and further confirm the feasibility and acceptability of these programs in low-resource settings, as well as offer new insights about the potential clinical effectiveness for common mental disorders such as depression or anxiety (Jiménez-Molina et al., 2019; Martínez et al., 2018a). Our findings also align with global efforts to increase accessibility to affordable broadband (e.g., the United Nations’ Sustainable Development Goal (SDG) 9.c: “strive to provide universal and affordable access to the Internet in least developed countries by 2020” (United Nations Development Programme, 2016)) and highlight the promise of leveraging Internet to deliver mental health care to individuals in lower resource areas of the world.
Mobile phones represented another widely used approach for intervention delivery in the included studies, comprising smartphone applications, text-messaging service (SMS), or phone calls (Adewuya et al., 2019; Coelhoso et al., 2019; Darvish et al., 2019; Liang et al., 2018; Martínez-Miranda et al., 2019; Mehrotra et al., 2018; Menezes et al., 2019; Nandyal et al., 2019; Sibeko et al., 2017; Singh et al., 2017; Zhu et al., 2018). The finding that smartphone delivered mental health interventions are increasingly being tested and reported is promising, especially as mental health apps are continuously being released to the public with little to no empirical evidence behind them (Larsen et al., 2019). Text message and mobile applications appeared to show promise in supporting care for a multitude of disorders, from mild depression to PTSD and psychotic disorders. This evidence suggests that mobile phone applications, if designed and tested rigorously, may provide a means for treating and managing a range of mental illnesses across a variety of contexts and clinical settings. Mounting research on the use of mobile health applications could inform the development and implementation of stronger regulations to guide the safe use of these technologies in lower resource settings. For example, if relevant governing bodies in different countries can draw from lessons learned in empirical research, it may help guide new regulations to ensure that mental health apps being released for easy download to the general public are subject to stringent privacy protections and methodological criteria, including effectiveness, safety and feasibility (Jacobson et al., 2020).
4.5. How do findings from digital mental health studies translate into practice in LMICs?
Despite accumulating evidence presented in this review, uptake by clinics and integration of digital technology into mental health care practice remains disappointingly low, even in higher-income settings (Torous et al., 2018). Efforts to increase global connectivity and accessibility to the Internet and mobile devices are underway (United Nations Development Programme, 2016), though remain behind international targets set under the Connect 2020 Agenda (ITU, 2020). Significant gaps in access to Internet and mobile technologies persist across many regions and are often neglected (Lutz, 2019). The low access to mobile phones or mobile Internet among women when compared to men is a persistent challenge that is especially apparent in impoverished settings globally (Naslund et al., 2019; Rowntree, 2018; Välimäki et al., 2016). Interestingly, with digital technology emerging as a promising approach for promoting mental health and treating some mental disorders, as reflected in this review and other recent reviews, there may be opportunities to align mental health care priorities with existing sustainable development priorities related to increasing digital technology access. For instance, goals to increase access to technology (outlined in SDG 9) could complement efforts to increase access to evidence-based mental health services (SDG 3) (United Nations Development Programme, 2016), thereby potentially allowing individuals at elevated risk of mental health problems, such as suicide, access to online mental health resources (Scherr et al., 2019). As many barriers persist to the implementation and delivery of in-person mental health services and integration of mental health care into existing health systems, by highlighting this important alignment of technological development and mental health care priorities to policymakers and other key decision makers, it may be possible to advocate for the roll out and implementation of promising digital mental health services in LMICs. This also highlights the potential importance of involving frontline health workers in co-creating and designing digital mental health interventions to ensure that new technologies are contextually relevant and to support successful adoption and seemless integration into existing health systems and community mental health services (Khan et al., 2020; Muke et al., 2019; Naslund et al., 2019; Raviola et al., 2019). Such efforts would still require careful consideration of the best evidence available for digital mental health, the need to address privacy and ethical challenges, recognition of stigma, and specific needs and preferences of population groups in greatest need of quality mental health care (Jacobson et al., 2020; Merchant et al., 2020).
4.6. Limitations
Our review has limitations to consider. Our goal was to offer an update over recent reviews on the emerging use of digital technology for treating mental disorders in LMICs. Although this allowed for a broad scope, as reflected by the wide variation in study design and outcomes reported, this made a quantitative synthesis of findings and meta-analysis not possible. Given the heterogeneity of included studies, an assessment of risk of bias was not conducted, further increasing risk of selection bias, though we conducted an assessment of methodological quality of the included studies. Furthermore, we limited our search to MEDLINE, as the prior reviews identified a large number of entries that were not focused on use of digital technology for mental health. Although use of MEDLINE may provide a sufficient and accurate search on its own (Rice et al., 2016) and allows for the use of MeSH headings to improve search efficiency (Chang, Heskett & Davidson, 2006), the lack of complementary searches of other databases has the potential for leaving relevant studies undetected. We found that there were no studies that reported a worsening of symptoms in any intervention group, and no studies reporting negative acceptability or dissatisfaction with digital interventions among participants. The lack of negative findings may reflect the hype surrounding digital mental health and suggests publication bias, whereby only positive findings are published. Additionally, we found that the included studies generally had low methodological quality as indicated by our MQRS scores. Even though the MQRS rating scale threshold is arbitrarily set at 14 or greater, this quality scale was developed based on the independent assessment of over 360 clinical trials (Miller & Wilbourne, 2002). Therefore, this illustrates the low methodological quality of the current studies relative to existing clinical research, thereby highlighting continued challenges with reliably interpreting research findings in digital mental health research.
The studies in this review largely targeted adults (ages 18–65), making it difficult to draw conclusions about the acceptability of digital interventions for children and adolescents, or the elderly, which are demographic groups at increased risk for mental disorders. Interestingly, we found only one study reporting cost-effectiveness of the digital intervention compared to the control condition (Adewuya et al., 2019). The low number of studies assessing costs indicates an important area for future research and highlights the need to investigate such characteristics as validity, reliability, feasibility, and effectiveness in the context of costs. Determining cost-effectiveness of digital mental health interventions is crucial towards gaining support from investors and stakeholders, and thereby supporting the successful delivery and implementation of digital mental health interventions. Finally, despite not excluding non-English language studies in our search, we recognise that papers in languages other than English may have been missed.
5. Conclusions & Directions for Future Research
Our review builds on previous reviews by tracking the growth in digital mental health research in LMICs over the last four years. Our findings further confirm the feasibility and acceptability of digital mental health interventions, and provide new insights on effectiveness of digital approaches in low-resource settings. Importantly, our findings are also consistent with mounting evidence of digital mental health technologies from higher income countries (Firth et al., 2017; Henson et al., 2019; Lal and Adair, 2014; Naslund et al., 2015). Therefore, our review combined with recent emerging evidence highlights the broader opportunities for digital interventions to target the burden of mental illness and global shortages in the provision of evidence-based mental healthcare services. In recognizing that digital technology holds potential to reduce demand for in-person clinic attention, improve treatment adherence, reduce symptoms of mental illness, lower rates of relapse and readmission, provide on-demand psychological support in the absence of in-person care, and provide access for even the most hard-to-reach groups (such as rural areas, areas of conflict or natural disasters, and people affected by stigma), there is need for continued rigorous research on effectiveness and cost-effectiveness.
To date, digital mental health research has largely been centered in specific regions or health systems, with limited collaboration across diverse contexts, cultures, or countries. The need for collaboration between researchers, clinicians, engineers, persons with lived experience, policymakers, and other stakeholders is clear; however, new initiatives should engage stakeholders across both higher and lower income countries. Future endeavours should step beyond a focus on common mental disorders, to include studies of varied groups and disorders to reflect the mental health needs and care disparities across low-income settings (Merchant et al., 2020). There is a need for rigorous randomized controlled trials with larger sample sizes to allow for greater confidence in the clinical significance and power of findings and allow for synthesis of high quality evidence. Studies should report standardised effect sizes as well as statistical significance, to ensure that findings can be compared across studies and to allow for meaningful conclusions to be drawn about effectiveness. Furthermore, barriers to accessing care, such as cultural interpretations of mental illness, stigma, discrimination and financial difficulties are relevant and should be taken into consideration by researchers embarking on intervention trials. Such efforts could generate novel findings about mechanisms of action for achieving clinically meaningful outcomes, improve acceptability of interventions, ensure generalizability of findings, and accelerate efforts to sustain digital mental health interventions and integrate high quality mental health care into underresourced health systems.
Figure 1.
PRISMA Flow diagram of studies included in the systematic review
Highlights:
Review builds on recent reviews and rapid growth of digital mental health in LMICs.
Review identified 37 studies from 13 LMICs published from 2016 to 2020.
Studies of digital programs to detect, diagnose, prevent and treat mental disorders.
Findings confirm feasibility and acceptability of digital mental health in LMICs.
Continued need for rigorous effectiveness and cost-effectiveness studies.
Acknowledgements:
Dr. Naslund reports receiving funding from the National Institute of Mental Health (Grant number: 5U19MH113211). The funder played no role in the study design; collection, analysis, or interpretation of data; writing of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Conflict of Interest
The authors report no conflict of interest.
Declaration of Interest: The authors report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adewuya AO, Momodu O, Olibamoyo O, Adegbaju A, Adesoji O, Adegbokun A, 2019. The effectiveness and acceptability of mobile telephone adherence support for management of depression in the Mental Health in Primary Care (MeHPriC) project, Lagos, Nigeria: A pilot cluster randomised controlled trial. Journal of affective disorders 253, 118–125. [DOI] [PubMed] [Google Scholar]
- Anttila M, Sittichai R, Katajisto J, Välimäki M, 2019. Impact of a web program to support the mental wellbeing of high school students: a quasi experimental feasibility study. International journal of environmental research and public health 16(14), 2473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arjadi R, Nauta MH, Scholte WF, Hollon SD, Chowdhary N, Suryani AO, Uiterwaal CS, Bockting CL, 2018. Internet-based behavioural activation with lay counsellor support versus online minimal psychoeducation without support for treatment of depression: a randomised controlled trial in Indonesia. The Lancet Psychiatry 5(9), 707–716. [DOI] [PubMed] [Google Scholar]
- Baldin YC, Sanudo A, Sanchez ZM, 2018. Effectiveness of a web-based intervention in reducing binge drinking among nightclub patrons. Revista de saude publica 52, 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumel A, Correll CU, Hauser M, Brunette M, Rotondi A, Ben-Zeev D, Gottlieb JD, Mueser KT, Achtyes ED, Schooler NR, 2016. Health technology intervention after hospitalization for schizophrenia: service utilization and user satisfaction. Psychiatric Services 67(9), 1035–1038. [DOI] [PubMed] [Google Scholar]
- Becker AE, Kleinman A, 2012. Introduction An Agenda for Closing Resource Gaps in Global Mental Health: Innovation, Capacity Building, and Partnerships. Harvard review of psychiatry 20(1), 3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker AE, Kleinman A, 2013. Mental health and the global agenda. New England Journal of Medicine 369(1), 66–73. [DOI] [PubMed] [Google Scholar]
- Bedendo A, Ferri CP, de Souza AAL, Andrade ALM, Noto AR, 2019. Pragmatic randomized controlled trial of a web-based intervention for alcohol use among Brazilian college students: Motivation as a moderating effect. Drug and alcohol dependence 199, 92–100. [DOI] [PubMed] [Google Scholar]
- Ben-Zeev D, Brian RM, Jonathan G, Razzano L, Pashka N, Carpenter-Song E, Drake RE, Scherer EA, 2018. Mobile Health (mHealth) Versus Clinic-Based Group Intervention for People With Serious Mental Illness: A Randomized Controlled Trial. Psychiatric Services, appi. ps. 201800063. [DOI] [PubMed] [Google Scholar]
- Bhugra D, Tasman A, Pathare S, Priebe S, Smith S, Torous J, Arbuckle MR, Langford A, Alarcón RD, Chiu HFK, 2017. The WPA-lancet psychiatry commission on the future of psychiatry. The Lancet Psychiatry 4(10), 775–818. [DOI] [PubMed] [Google Scholar]
- Cabassa LJ, Camacho D, Vélez-Grau CM, & Stefancic A. (2017). Peer-based health interventions for people with serious mental illness: a systematic literature review. Journal of psychiatric research, 84, 80–89. [DOI] [PubMed] [Google Scholar]
- Cárdenas-López G, de la Rosa A, Durón R, Durán X, 2016. Virtual reality exposure for trauma and stress-related disorders for city violence crime victims. International Journal of Child Health and Human Development 9(3), 315–322. [Google Scholar]
- Ciuca AM, Berger T, Crişan LG, Miclea M, 2018. Internet-based treatment for panic disorder: A three-arm randomized controlled trial comparing guided (via real-time video sessions) with unguided self-help treatment and a waitlist control. PAXPD study results. Journal of anxiety disorders 56, 43–55. [DOI] [PubMed] [Google Scholar]
- Coelhoso CC, Tobo PR, Lacerda SS, Lima AH, Barrichello C, Amaro E Jr, & Kozasa EH (2019). A New Mental Health Mobile App for Well-Being and Stress Reduction in Working Women: Randomized Controlled Trial. Journal of medical Internet research, 21(11), e14269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darvish A, Khodadadi Hassankiadeh N, Abdoosti S, Mojgan Ghapandar Kashani M, 2019. Effect of Text Messaging-based Psychiatric Nursing Program on Quality of Life in Veterans with Post-Traumatic Stress Disorder: A Randomized Controlled Trial. International journal of community based nursing and midwifery 7(1), 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, Patel V, 2017. The impact of digital technology on psychological treatments and their dissemination. Behaviour research and therapy 88, 19–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth J, Torous J, Nicholas J, Carney R, Pratap A, Rosenbaum S, Sarris J, 2017. The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials. World Psychiatry 16(3), 287–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortuna KL, Naslund JA, LaCroix JM, Bianco CL, Brooks JM, Zisman-Ilani Y, Muralidharan A, & Deegan P. (2020). Digital Peer Support Mental Health Interventions for People With a Lived Experience of a Serious Mental Illness: Systematic Review. JMIR Mental Health, 7(4), e16460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gire N, Farooq S, Naeem F, Duxbury J, McKeown M, Kundi PS, Chaudhry IB, Husain N, 2017. mHealth based interventions for the assessment and treatment of psychotic disorders: a systematic review. Mhealth 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo L, Zhang J, Mu L, & Ye Z. (2020). Preventing Postpartum Depression With Mindful Self-Compassion Intervention: A Randomized Control Study. The Journal of nervous and mental disease, 208(2), 101–107. [DOI] [PubMed] [Google Scholar]
- Han H, Zhang JY, Hser Y-I, Liang D, Li X, Wang SS, Du J, Zhao M, 2018. Feasibility of a mobile phone app to support recovery from addiction in China: secondary analysis of a pilot study. JMIR mHealth and uHealth 6(2), e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henrich J, Heine SJ, & Norenzayan A. (2010). Most people are not WEIRD. Nature, 466(7302), 29–29. [DOI] [PubMed] [Google Scholar]
- Henson P, Wisniewski H, Hollis C, Keshavan M, Torous J, 2019. Digital mental health apps and the therapeutic alliance: initial review. BJPsych open 5(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- ITU, 2020. Connect 2020 Agenda for Global Telecommunication/ICT Development. Telecommunication Development Sector (ITU-D), Geneva, Switzerland. [Google Scholar]
- Jacobson NC, Bentley KH, Walton A, Wang SB, Fortgang RG, Millner AJ, Coombs III G, Rodmand AM, Coppersmithd DD, 2020. Ethical dilemmas posed by mobile health and machine learning in psychiatry research. Bull World Health Organ 98(4), 270–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiménez-Molina Á, Franco P, Martínez V, Martínez P, Rojas G, Araya R, 2019. Internet-based interventions for the prevention and treatment of mental disorders in Latin America: A scoping review. Frontiers in psychiatry 10, 664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaonga NN, Morgan J, 2019. Common themes and emerging trends for the use of technology to support mental health and psychosocial well-being in limited resource settings: a review of the literature. Psychiatry research, 112594. [DOI] [PubMed] [Google Scholar]
- Karbasi A, Haratian A, 2018. The efficacy of internet-based cognitive behavioral therapy on the anxiety disorders among adolescent girls. Advanced biomedical research 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan M, 2005. Suicide prevention and developing countries. Journal of the royal society of medicine 98(10), 459–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan A, Shrivastava R, Tugnawat D, Singh A, Dimidjian S, Patel V, Bhan A, Naslund JA (2020). Design and Development of a Digital Program for Training Non-specialist Health Workers to Deliver an Evidence-Based Psychological Treatment for Depression in Primary Care in India. Journal of Technology in Behavioral Science. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kishimoto T, Krieger T, Berger T, Qian M, Chen H, Yang Y, 2016. Internet-based cognitive behavioral therapy for social anxiety with and without guidance compared to a wait list in China: a propensity score study. Psychotherapy and psychosomatics 85(5), 317–319. [DOI] [PubMed] [Google Scholar]
- Koopmans PC, Bültmann U, Roelen CA, Hoedeman R, van der Klink JJ, Groothoff JW, 2011. Recurrence of sickness absence due to common mental disorders. International archives of occupational and enviromental health, 84(2), 193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lal S, Adair CE, 2014. E-mental health: a rapid review of the literature. Psychiatric Services 65(1), 24–32. [DOI] [PubMed] [Google Scholar]
- Larsen ME, Huckvale K, Nicholas J, Torous J, Birrell L, Li E, Reda B, 2019. Using science to sell apps: evaluation of mental health app store quality claims. NPJ digital medicine 2(1), 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau N, O’Daffer A, Colt S, Yi-Frazier JP, Palermo TM, McCauley E, Rosenberg AR, 2020. Android and iPhone mobile appls for psychosocial wellness and stress management: systematic search in app stores and literature review. JMIR Mhealth Uhealth 8(5), e17798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang D, Han H, Du J, Zhao M, Hser Y-I, 2018. A pilot study of a smartphone application supporting recovery from drug addiction. Journal of substance abuse treatment 88, 51–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipschitz J, Hogan T, Bauer M, Mohr D, 2019. Closing the research-to-practice gap in digital psychiatry: the need to integrate implementation science. The Journal of Clinical Psychiatry 80(3) [DOI] [PubMed] [Google Scholar]
- Lutz C, 2019. Digital inequalities in the age of artificial intelligence and big data. Human Behavior and Emerging Technologies 1(2), 141–148. [Google Scholar]
- Ma Y, She Z, Siu AF-Y, Zeng X, Liu X, 2018. Effectiveness of online mindfulness-based interventions on psychological distress and the mediating role of emotion regulation. Frontiers in psychology 9, 2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malhotra S, Chakrabarti S, Shah R, 2019. A model for digital mental healthcare: Its usefulness and potential for service delivery in low-and middle-income countries. Indian journal of psychiatry 61(1), 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez P, Rojas G, Martínez V, Lara MA, Pérez JC, 2018a. Internet-based interventions for the prevention and treatment of depression in people living in developing countries: a systematic review. Journal of affective disorders 234, 193–200. [DOI] [PubMed] [Google Scholar]
- Martínez V, Rojas G, Martínez P, Zitko P, Irarrázaval M, Luttges C, Araya R, 2018b. Remote collaborative depression care program for adolescents in Araucanía Region, Chile: randomized controlled trial. Journal of medical Internet research 20(1), e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez-Miranda J, Martínez A, Ramos R, Aguilar H, Jiménez L, Arias H, Rosales G, Valencia E, 2019. Assessment of users’ acceptability of a mobile-based embodied conversational agent for the prevention and detection of suicidal behaviour. Journal of medical systems 43(8), 246. [DOI] [PubMed] [Google Scholar]
- Maulik PK, Kallakuri S, Devarapalli S, Vadlamani VK, Jha V, Patel A, 2017. Increasing use of mental health services in remote areas using mobile technology: a pre–post evaluation of the SMART Mental Health project in rural India. Journal of global health 7(1), 010408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehrotra S, Sudhir P, Rao G, Thirthalli J, Srikanth T, 2018. Development and pilot testing of an internet-based self-help intervention for depression for Indian users. Behavioral Sciences 8(4), 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menezes P, Quayle J, Claro HG, Da Silva S, Brandt LR, Diez-Canseco F, Miranda JJ, Price LN, Mohr DC, Araya R, 2019. Use of a mobile phone app to treat depression comorbid with hypertension or diabetes: a pilot study in Brazil and Peru. JMIR mental health 6(4), e11698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merchant R, Torous J, Rodriguez-Villa E, Naslund JA, 2020. Digital technology for management of severe mental disorders in low-income and middle-income countries. Current Opinion in Psychiatry, 33, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, & Wilbourne PL 2002. Mesa Grande: A methodological analysis of clinical trials of treatment for alcohol use disorders. Addiction, 97(3), 265–277. [DOI] [PubMed] [Google Scholar]
- Moeini B, Bashirian S, Soltanian AR, Ghaleiha A, & Taheri M. (2019). Examining the Effectiveness of a Web-Based Intervention for Depressive Symptoms in Female Adolescents: Applying Social Cognitive Theory. Journal of research in health sciences, 19(3), e00454. [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, 2009. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine 151(4), 264–269. [DOI] [PubMed] [Google Scholar]
- Muke SS, Shrivastava RD, Mitchell L, Khan A, Murhar V, Tugnawat D, Shidhaye R, Patel V, Naslund JA, 2019. Acceptability and feasibility of digital technology for training community health workers to deliver brief psychological treatment for depression in rural India. Asian Journal of Psychiatry 45, 99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nandyal M, Chandramouleeswaran S, & Braganza D. (2019). Feasibility of mobile telephonic follow-up among patients with alcohol dependence syndrome. The National medical journal of India, 32(2), 77–82. [DOI] [PubMed] [Google Scholar]
- Naslund JA, Aschbrenner KA, Araya R, Marsch LA, Unützer J, Patel V, Bartels SJ, 2017. Digital technology for treating and preventing mental disorders in low-income and middle-income countries: a narrative review of the literature. The Lancet Psychiatry 4(6), 486–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Bondre A, Torous J, Aschbrenner KA, 2020. Social media and mental health: benefits, risks, and opportunities for research and practice. Journal of Technology in Behavioral Science, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Gonsalves PP, Gruebner O, Pendse SR, Smith SL, Sharma A, Raviola G, 2019. Digital Innovations for Global Mental Health: Opportunities for Data Science, Task Sharing, and Early Intervention. Current Treatment Options in Psychiatry, 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Marsch LA, McHugo GJ, Bartels SJ, 2015. Emerging mHealth and eHealth interventions for serious mental illness: a review of the literature. Journal of mental health 24(5), 321–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Shidhaye R, Patel V, 2019. Digital technology for building capacity of nonspecialist health workers for task sharing and scaling up mental health care globally. Harvard Review of Psychiatry, 27(3), 181–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ofoegbu TO, Asogwa U, Otu MS, Ibenegbu C, Muhammed A, & Eze B. (2020). Efficacy of guided internet-assisted intervention on depression reduction among educational technology students of Nigerian universities. Medicine, 99(6), e18774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osorio JHV, Jacob MK, Bauer S, Moessner M, Duque DE, Guzmán ÁEC, Botero LDB, Osorio LCC, Mesa CHM, Patiño JE, 2017. Uso de e-mental health para el seguimiento posterapia de pacientes con depresión en Colombia. Revista Virtual Universidad Católica del Norte(52), 41–56. [Google Scholar]
- Patel V, Maj M, Flisher AJ, SILVA MJ, KOSCHORKE M, Prince M, Tempier R, Riba M, Sanchez M, Campodonico FD, 2010. Reducing the treatment gap for mental disorders: a WPA survey. World Psychiatry 9(3), 169–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Prince M, 2010. Global mental health: a new global health field comes of age. Jama 303(19), 1976–1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pathare S, Brazinova A, Levav I, 2018. Care gap: a comprehensive measure to quantify unmet needs in mental health. Epidemiology and psychiatric sciences 27(5), 463–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perivoliotis D, Grant P, Peters E, Ison R, Kuipers E, Beck A, 2009. Cognitive insight predicts favorable outcome in cognitive behavioral therapy for psychosis. Psychosis 2(1), 23–33. [Google Scholar]
- Petersen I, Marais D, Abdulmalik J, Ahuja S, Alem A, Chisholm D, Egbe C, Gureje O, Hanlon C, Lund C, 2017. Strengthening mental health system governance in six low- and middle-income countries in Africa and South Asia: challenges, needs and potential strategies. Health policy and planning 32(5), 699–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price M, Yuen EK, Goetter EM, Herbert JD, Forman EM, Acierno R, Ruggiero KJ, 2014. mHealth: a mechanism to deliver more accessible, more effective mental health care. Clinical psychology & psychotherapy 21(5), 427–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raviola G, Naslund JA, Smith SL, Patel V, 2019. Innovative models in mental health delivery systems: task sharing care with non-specialist providers to close the mental health treatment gap. Current Psychiatry Reports, 21, 44. [DOI] [PubMed] [Google Scholar]
- Rehm J, Shield KD, 2019. Global burden of disease and the impact of mental and addictive disorders. Current psychiatry reports 21(2), 10. [DOI] [PubMed] [Google Scholar]
- Rojas G, Guajardo V, Martínez P, Castro A, Fritsch R, Moessner M, Bauer S, 2018. A remote collaborative care program for patients with depression living in rural areas: open-label trial. Journal of medical Internet research 20(4), e158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rootes-Murdy K, Glazer KL, Van Wert MJ, Mondimore FM, Zandi PP, 2018. Mobile technology for medication adherence in people with mood disorders: A systematic review. Journal of affective disorders 227, 613–617. [DOI] [PubMed] [Google Scholar]
- Rowntree O, 2018. Connected Women: The Mobile Gender Gap Report 2018, London, UK. [Google Scholar]
- Scherr S, Haim M, Arendt F, 2019. Equal access to online information? Google’s suicide-prevention disparities may amplify a global digital divide. New Media & Society 21(3), 562–582. [Google Scholar]
- Sibeko G, Temmingh H, Mall S, Williams-Ashman P, Thornicroft G, Susser ES, Lund C, Stein DJ, Milligan PD, 2017. Improving adherence in mental health service users with severe mental illness in South Africa: a pilot randomized controlled trial of a treatment partner and text message intervention vs. treatment as usual. BMC research notes 10(1), 584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh G, Manjunatha N, Rao S, Shashidhara H, Moirangthem S, Madegowda RK, Binukumar B, Varghese M, 2017. Use of mobile phone technology to improve follow-up at a community mental health clinic: A randomized control trial. Indian journal of psychological medicine 39(3), 276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiburcio M, Lara MA, Martínez N, Fernández M, Aguilar A, 2018. Web-based intervention to reduce substance abuse and depression: a three arm randomized trial in Mexico. Substance use & misuse 53(13), 2220–2231. [DOI] [PubMed] [Google Scholar]
- Torous J, Andersson G, Bertagnoli A, Christensen H, Cuijpers P, Firth J, Haim A, Hsin H, Hollis C, Lewis S, 2019. Towards a consensus around standards for smartphone apps and digital mental health. World Psychiatry 18(1), 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torous J, Nicholas J, Larsen ME, Firth J, Christensen H, 2018. Clinical review of user engagement with mental health smartphone apps: evidence, theory and improvements. Evidence-Based Mental Health, ebmental-2018–102891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torrey WC, Cepeda M, Castro S, Bartels SM, Cubillos L, Obando FS, Camblor PM, Uribe-Restrepo JM, Williams M, Gómez-Restrepo C, & Marsch LA (2020). Implementing Technology-Supported Care for Depression and Alcohol Use Disorder in Primary Care in Colombia: Preliminary Findings. Psychiatric services (Washington, D.C.), 71(7), 678–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tulbure BT, Andersson G, Sălăgean N, Pearce M, Koenig HG, 2018a. Religious versus conventional internet-based cognitive behavioral therapy for depression. Journal of religion and health 57(5), 1634–1648. [DOI] [PubMed] [Google Scholar]
- Tulbure BT, Rusu A, Sava FA, Sălăgean N, Farchione TJ, 2018b. A web-based transdiagnostic intervention for affective and mood disorders: randomized controlled trial. JMIR mental health 5(2), e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uddin R, Burton N, Maple M, Kha S, Khan A, 2019. Suicidal ideation, suicide planning, and suicide attempts among adolescents in 59 low-income and middle-income countries: a population-based study. The Lancet child & adolescent health 3(4), 223–233. [DOI] [PubMed] [Google Scholar]
- United Nations Development Programme, 2016. UNDP Policy and Programme Brief: UNDP Support to the Implementation of the 2030 Agenda for Sustainable Development. United Nations Development Programme,, New York, NY. [Google Scholar]
- Välimäki M, Athanasopoulou C, Lahti M, Adams CE, 2016. Effectiveness of social media interventions for people with schizophrenia: a systematic review and meta-analysis. Journal of medical Internet research 18(4), e92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigo D, Thornicroft G, Atun R, 2016. Estimating the true global burden of mental illness. The Lancet Psychiatry 3(2), 171–178. [DOI] [PubMed] [Google Scholar]
- Wang Z, Wang J, Maercker A, 2016. Program use and outcome change in a Web-based trauma intervention: individual and social factors. Journal of medical Internet research 18(9), e243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- We Are Social, 2020. Digital in 2020. We Are Social Ltd., New York, NY. [Google Scholar]
- Whiteman KL, Naslund JA, DiNapoli EA, Bruce ML, & Bartels SJ (2016). Systematic review of integrated general medical and psychiatric self-management interventions for adults with serious mental illness. Psychiatric Services, 67(11), 1213–1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu DR, Xiao S, He H, Caine ED, Gloyd S, Simoni J, Hughes JP, Nie J, Lin M, He W, 2019. Lay health supporters aided by mobile text messaging to improve adherence, symptoms, and functioning among people with schizophrenia in a resource-poor community in rural China (LEAN): A randomized controlled trial. PLoS medicine 16(4), e1002785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang M, Jia G, Sun S, Ye C, Zhang R, Yu X, 2019. Effects of an Online Mindfulness Intervention Focusing on Attention Monitoring and Acceptance in Pregnant Women: A Randomized Controlled Trial. Journal of midwifery & women’s health 64(1), 68–77. [DOI] [PubMed] [Google Scholar]
- Yeung A, Wang F, Feng F, Zhang J, Cooper A, Hong L, Wang W, Griffiths K, Bennett K, Bennett A, 2018. Outcomes of an online computerized cognitive behavioral treatment program for treating chinese patients with depression: A pilot study. Asian journal of psychiatry 38, 102–107. [DOI] [PubMed] [Google Scholar]
- Zhu Y, Jiang H, Su H, Zhong N, Li R, Li X, Chen T, Tan H, Du J, Xu D, 2018. A newly designed mobile-based computerized cognitive addiction therapy app for the improvement of cognition impairments and risk decision making in methamphetamine use disorder: Randomized controlled trial. JMIR mHealth and uHealth 6(6), e10292. [DOI] [PMC free article] [PubMed] [Google Scholar]