Summary
Background
Injuries are a significant public health concern globally. Papua New Guinea has failed to achieve all eight health millennium development goals, and in doing so has not prioritized injuries in previous health policies. Understanding costs related to injuries can ultimately guide policies for surgical service delivery in achieving local, and universal health coverage objectives.
Methods
A prospective cost of illness study was conducted at Alotau Provincial Hospital (only major referral hospital), in the Milne Bay Province of Papua New Guinea, from the 1st of June 2020 to the 21st of December 2020. A bottom up approach of micro costing was used to estimate the direct medical cost of trauma aetiologies, and injuries of patients admitted to the surgical ward at Alotau Provincial Hospital.
Findings
The mean cost of managing traumatic injuries was K45, 900.40 (US$13,311.12) per patient. The most common cause of injury was alcohol related injuries (n=32) with a total direct medical cost of K1, 417, 023.73 (US$410,936.88). The most common injury was fractures (n=40) with a total direct medical cost of K1, 907, 531.88 (US$553,184.25). The highest cost for trauma aetiologies were MVAs with a mean cost of K48, 687.40 (US$14, 119.35) per patient. The highest cost for injuries was abdominal trauma with a mean cost K55,929.69(US$16,219.61) per patient.
Interpretation
Poor regulation of alcohol and road safety is associated with high surgical costs. In an era of financial instability, reducing injuries is economical in acheiving health care objectives that rely heavily on adequate funding, and financing.
Funding
No funding source.
Keywords: Papua New Guinea, Direct medical cost, Trauma, Aetiologies, Injury
Research in Context.
Evidence before this study
In 2015, the Lancet Commission of Global surgery highlighted the need for more research in low to middle income populations where knowledge of financing surgical care was limited. Since then, 73 papers addressing the cost of surgery in low to middle income countries (LMICs) have been indexed on PubMed.
The commission stated that injuries and other surgical conditions would surpass communicable disease challenges. Up until 2014, Wesson et al in a systemic review of literature identified only 13 full economic evaluations of cost of injury studies and recommended that a standardized approach to economic evaluation of injury in LMICs was needed.
Added value of this study
In this study, we give an approach to calculating the direct medical cost of injuries in a LMIC. The costing takes into account the patient and hospital perspective, and will be the first of such studies globally to adapt this approach to micro cost injuries.
Implications of all the available evidence
This study will provide a standardized methodology that can be used in other LMICs to estimate direct medical costs. Further implications of this study includes; prioritizing injuries in health policies; health system financing; reviewing of current laws on alcohol; improving road safety, and improving local, and global health objectives.
Alt-text: Unlabelled box
Background
Injuries are a significant public health concern globally.1 The World Health Organization (WHO) estimates that 5.8 million people die each year as a result of traumatic injuries with over 90% of deaths occurring in low to middle income countries (LMICs).2,3 Efforts in these countries have focused on public health interventions for pandemic diseases like tuberculosis . This lack of priority has resulted in deaths from injuries accounting for 32% more fatality than AIDS, tuberculosis, and malaria combined.4
Motor vehicle accidents (MVA), violence and war, were reported to be the leading cause of injuries in developing countries.4 In the Western pacific region, the incidence of injuries is as high as 333 per 100 000 population in one population-based study in Fiji.5 In light of climate change and other disease patterns in the region, injuries will continue to reduce economic productivity if not addressed seriously.6
In Papua New Guinea (PNG), injuries are the number one cause of surgical admissions.7 This low to middle income country in the western pacific region has failed to achieve all eight of the United Nations Health Millennium Development Goals.8 Matthew et al estimates that over 1.1 million dollars was used to manage trauma in a provincial hospital in PNG.9 Understanding these costs can ultimately guide policies for surgical service delivery in achieving local, and universal health coverage objectives.10
The Lancet Commission on Global Surgery (LCoGS) in 2015, highlighted the need for more research in traumatic injury.11 Most publications in LMICs give little insight to policy makers on injury related costs.11 In PNG, and the Western Pacific Region, there remains no published literature on this topic. As such, the aim of this study was to estimate the direct medical costs of trauma aetiologies, and injuries in a resource limited setting of Alotau Provincial Hospital in Milne Bay Province of PNG.
Methodology
Design
A prospective cost of illness study was conducted at Alotau Provincial Hospital from the 1st of June 2020 to the 21st of December 2020.
Costing perspective and approach
A patient-hospital perspective of costing was used.12,13 A bottom up approach of micro costing was applied to estimate direct medical costs.14 Hospital fees were used to assess costs by patients. Consumables, laboratory investigations, stationary, electricity, water usage, and staff salaries were used to assess hospital costs.
Study setting
The study was conducted at Alotau Provincial Hospital. It is the only major referral hospital in the Milne Bay Province of PNG.15 This large maritime province in 2020 had an estimated population of 339, 275 people.15 27.8% of the population experience less than two hour delay in seeking secondary health care with an average surgical, anaesthesia and obstetric provider density of 1.8 per 100 000 population.16 Catastrophic expenditure is thus a risk for 29% of the population.16
Study participants
The inclusion criteria for this study were consecutive persons admitted from the emergency department of Alotau Provincial Hospital with traumatic injuries to the surgical ward. Patients were excluded if their injuries were treated at the emergency department; following which they were discharged.
The minimal sample size was obtained using the Yamane formula (n=N/1+N(e)2).17 Where n= sample size, e= margin of error, and N= population Size. A population size (N) of 98 was obtained from the number of admitted injuries from the emergency department to the surgical ward over a 6-month period (December 2019 – May 2020). Margin of error (e) was taken as 0.05. The minimum sample size for the 6-month period was 79.
Variables and data collection
A standard survey form was used to collect data on patient characteristics, and costs (Appendix 1). Patient characteristics included sex, age, cause of injury, injury, injury severity score, management, operation, operative time, length of hospital stay, high dependency ward admission, complications, and deaths. Costs include hospital fees, staff salaries, drugs, consumables, laboratory investigations, stationary, electricity, and water usage.
Direct medical costs for the emergency department, operating theatre, anaesthesia, surgical ward, and high dependency ward were captured in the survey form. A nursing officer was assigned at each department to tally, and record the resources used on each patient. Ongoing chart reviews were done by the authors to calculate water and electricity usage, and cross check the data collected against each of the patient's charts.
Hospital fees were inclusive for admissions, haematology investigations, biochemistry investigations, radiology investigations, and major surgery. Admission fees were for patients requiring surgical admission for inpatient treatment. Haematology investigations referred to full blood examinations. Biochemistry investigations were urea electrolyte and creatinine, and liver function investigations. Radiology investigations were for plain radiography. Major surgery fees were fees paid for any invasive procedure where the body cavity was entered, or for any surgical procedure booked as an emergency.
Each departments’ shift roster was reviewed to determine the number of hospital staff involved in treating the patient. Hospital staffs included community health workers, nursing officers, health extension officers, laboratory officers, physiotherapists, anaesthetic scientific officers, anaesthetic technical assistants, medicals officers, and porters. Community health workers have a certificate in nursing and their main role is to identify health needs, deliver health education, and apply preventative measures such as immunization. Nursing Officers’ have a degree in nursing and have various roles including patient monitoring, administration of treatment and assisting in surgery etc. Health extension officers have a degree in health Sciences (Rural health) and are trained to provide primary health care in rural areas and can also undertake administrative roles in running health facilities.
Laboratory officers have a degree in Basic Laboratory Sciences and are responsible for running medical laboratory tests involving microbiology, hematology, histology etc. Physiotherapists are involved in movement and exercise, manual therapy, and education for patients with injury, illness, and disability. Anaesthetic scientific officers have a diploma in anaesthetic science and are trained to competently administer anaesthesia to patients for surgery. Anaesthetic technical assistants are community health workers who have been clinically trained to assist anaesthetic scientific officers and anaesthetic medical officers to administer anaesthesia. Medical officers have a bachelor's degree in Medicine and Surgery and are primarily involved in the diagnosis and treatment of disease or injury. Porters are non-medical staff responsible for transporting patients and medical consumables within the hospital.
Patients with injuries were triaged by the emergency medical officer or health extension officer using the four-tier triage system.18 Patients requiring possible admission were reviewed by the surgical medical officer. Surgical admission for traumatic injuries were for patients whose medical goals were to manage; impending or complete airway obstruction, impaired breathing, bleeding (internal or external), shock, secondary complications of traumatic brain injury, intestinal and abdominal injuries, potentially disabling limb injuries, potentially unstable spinal cord injuries, and burns.19 Decision for operative management was made by the general surgeon following review with the surgical medical officer.
Injury was defined in this study as a physical injury diagnosed after clinical history, examination, and investigation. Trauma aetiology in this study was defined as cause of injury. They were categorized either as alcohol related injuries, falls, criminal attack, domestic violence, falling object injury, motor vehicle accident, burns, sporting injuries, and others.
The causes of injury were obtained from history taking. Alcohol related injuries referred to all injuries in this study sustained under the influence of alcohol, or sustained from someone under the influence of alcohol. All other causes were therefore non-alcohol related. Falls in this study were related to injuries sustained from falling. Injuries by criminal attack were those caused by persons with the intention to steal, or kill the victim. Injuries from domestic violence were those sustained within the home, or amongst relatives. Falling object injury were those sustained from any object falling from a height onto a person resulting in injury. Motor vehicle accidents in this study referred to injuries sustained from a moving motor vehicle by a pedestrian, passenger or driver. Burns were sustained from hot water, fire, or electricity. Sporting injuries were injuries sustained from participating in a sporting activity. Others referred to injuries that were sustained by other causes of injury.
Injuries in this study includes fractures, muscle/tendon injuries, head injuries, chest injuries, spinal injuries, abdominal injuries, polytraumatic injuries and burns. Fractures included both closed, and open fractures. Muscle and tendon injuries were injuries to the muscles, and tendons of the extremities only. Chest injuries included both penetrating, and blunt trauma to the thorax. Abdominal injuries also included both penetrating, and blunt trauma to the abdomen. Spinal injuries were either vertebral fractures, subluxations, or a foreign body within the spinal column. Burns in this study included electricity, hot water, fire and chemical burns. Polytraumatic injuries were defined in this study as two, or more traumatic injuries. An injury severity score out of 75 was given to each injury and was used to classify injuries into mild (1-8), moderate (9-15), severe (16-24), and profound (>25).20
Management in this study was defined as either conservative for those not requiring surgery, or surgical for those requiring surgical intervention. Operations in this study included all surgical procedures done in the operating theatre. Operating time was reported in minutes, and length of hospital stay in days. High dependency ward admissions were those patients admitted for airway, ventilatory support, and severe sepsis management. Complications in this study was defined as patients with severe sepsis or an acute to intermediate post-operative complication of bleeding, peritonitis, bowel obstruction, bed sores, pneumothorax, pneumonia, wound infection, and death. It was thus reported as yes for presence of complication, and no for absence of complications.
Costing analysis
The National Department of Health's Medical and Dental Catalogue was used to obtain costs of drugs, consumables, and laboratory investigations (https://abortion-policies.srhr.org/documents/countries/02-PNG-Medical-and-Dental-Catalogue-Department-of-Health-2012.pdf).21 Drugs, and consumables not in the medical, and dental catalogue were excluded from the survey. Costs of drugs, and consumables were calculated based on the unit cost in Kina as shown in Table 2.
Table 2.
Showing cost formulae.
| Cost formulae for drugs, consumables, water usage, electricity, hospital fees and staff salaries. |
| Cost per item = Cost of item (as per medical and dental catalogue) x Number of Units |
| Electricity cost per machine = [(Watts x 0.6968/unit) / 1000] x number of hours |
| Water cost per person = K1.50 × 1kL |
| Hospital fees per person = Admission fee + Haematology fee + Biochemistry fee + Major surgery fee |
| Fortnightly Staff salary = (Designation and pay class x Number of workers)/24 fortnights in a year |
| Total Direct Medical Cost per patient = Sum of all cost per item + Sum of all electricity cost per machine + Water cost per person + Hospital fees per person + Sum of Staff salary |
Drugs/consumable (https://abortion-policies.srhr.org/documents/countries/02-PNG-Medical-and-Dental-Catalogue-Department-of-Health-2012.pdf)
Hospital fees and Staff salaries (Supplemental Table 2).
The cost for electricity was calculated using the formula obtained from PNG power. Electricity consumption was calculated for the suction machine, anaesthetic machine, operative lights, and diathermy. A survey of 10 persons recruited showed water consumption was less than 1.5kL of water for each patient. As per water PNG band calculations the cost of water was thus estimated at K1.50 (US$0.44) per person.
All staff employed to Alotau Provincial Hospital are paid according to an annual base salary. Staff annual salaries and hospital fees were obtained from the Milne Bay Provincial Hospital office of policy, planning, and coordination. The fortnight salary was calculated and used for staff salary costs. Data and costs were analysed using Microsoft excel 2016.
Role of the funding sources
No funding sources.
Results
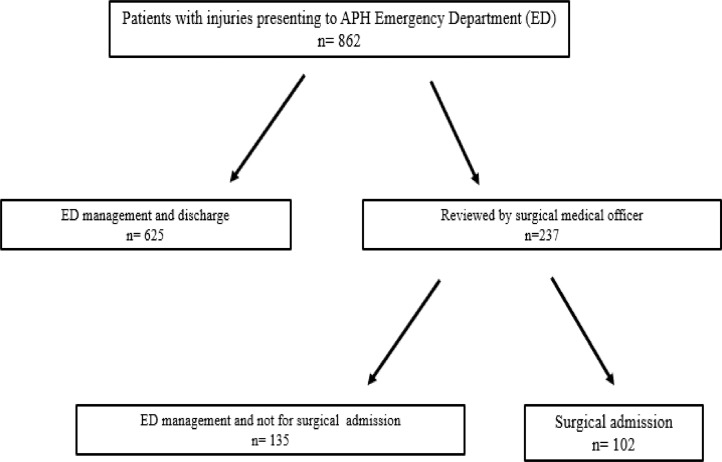
Table 1 shows the patients characteristics. A total of 102 continuous persons who were admitted with injuries were surveyed in this study as shown in Figure 1. The male to female ratio was 3:1. The mean age was 25.90 years. Alcohol caused injuries in 31.37% (n=32) of cases followed by falls with 30.39% (n=31). Fractures were seen in 39.22% (n=40) of cases followed by muscle/tendon injuries with 20.59% (n=21), and head injuries with 12.75% (n=13) of cases.
Table 1.
Showing demographic and clinical characteristics of trauma patients included in the study at APH, Milne Bay Province, Papua New Guinea, from the 1st of June 2020 to the 21st of December 2020.
| Characteristic | Total n=102 (%) |
|---|---|
| Sex | |
| Male | 77 (75.49) |
| Female | 25 (24.51) |
| Age group | |
| <5 | 6 (5.88) |
| 5-15 | 21 (20.59) |
| 16-25 | 33 (32.35) |
| 26-45 | 32 (31.37) |
| >45 | 10 (9.81) |
| Cause of injury | |
| Alcohol related injury | 32 (31.37) |
| Muscle and tendon injury | 10 |
| Head injury | 7 |
| Chest injury | 5 |
| Fracture | 5 |
| Polytraumatic injury | 2 |
| Spinal injury | 2 |
| Abdominal injury | 1 |
| Falls | 31 (30.39) |
| Fracture | 18 |
| Spinal injury | 5 |
| Head injury | 3 |
| Muscle and tendon injury | 2 |
| Abdominal injury | 1 |
| Fire burns | 1 |
| Chest injury | 1 |
| Criminal attack | 7 (6.86) |
| Fracture | 3 |
| Muscle and tendon injury | 1 |
| Polytraumatic injury | 2 |
| Abdominal injury | 1 |
| Domestic violence | 8 (7.84) |
| Muscle and tendon injury | 4 |
| Fracture | 2 |
| Chest injury | 1 |
| Head injury | 1 |
| Falling object injury | 9 (9.82) |
| Fracture | 6 |
| Chest injury | 1 |
| Abdominal injury | 1 |
| Head injury | 1 |
| Motor vehicle accident | 6 (6.88) |
| Abdominal injury | 1 |
| Fracture | 1 |
| Head injury | 1 |
| Muscle and tendon injury | 2 |
| Polytraumatic injury | 1 |
| Burns | 2 (1.96) |
| Hot water burn | 2 |
| Sporting injury | 4 (3.92) |
| Fracture | 4 |
| Others | 3 (2.94) |
| Muscle and tendon injury | 2 |
| Fracture | 1 |
| Injury | |
| Fractures | 40 (39.22) |
| Closed Femur fracture | 12 |
| Open Radius Ulna fracture | 8 |
| Open Tibia Fibular fracture | 7 |
| Closed Humerus fracture | 5 |
| Closed Tibia fracture | 3 |
| Closed Colles fracture | 2 |
| Open Interphalangeal fracture | 1 |
| Open Metatarsal fracture | 1 |
| Open Humerus fracture | 1 |
| Muscle/tendon injury | 21 (20.59) |
| Forearm laceration | 7 |
| Multiple lacerations | 5 |
| Scrotal laceration | 2 |
| Supraorbital laceration | 2 |
| Shoulder laceration | 2 |
| Back laceration | 1 |
| Elbow laceration | 1 |
| Foot laceration | 1 |
| Head injury | 13 (12.75) |
| Mild head injury | 7 |
| Severe head injury | 4 |
| Moderate head injury | 2 |
| Chest injury | 8 (7.84) |
| Pneumothorax | 5 |
| Hemopneumothorax | 2 |
| Flail chest | 1 |
| Spinal injury | 7 (6.86) |
| Vertebral fracture | 4 |
| Subluxation | 2 |
| Foreign body in situ | 1 |
| Abdominal injury | 5 (4.90) |
| Blunt abdominal injury with splenic injury | 2 |
| Penetrating abdominal injury with small bowel perforation | 2 |
| Blunt abdominal injury | 1 |
| Polytrauma | 5 (4.90) |
| Mild head injury with muscle and tendon injury | 1 |
| Pneumothorax, closed tibia fracture,closed femur fracture | 1 |
| Mild head injury with open radius ulna fracture | 1 |
| Spinal injury with closed radius fracture | 1 |
| Compound femur fracture with penetrating abdominal injury | 1 |
| Burns | 3 (2.94) |
| Hot water burns | 2 |
| Fire burns | 1 |
| Injury Severity Score | |
| Mild | 7 (6.86) |
| Moderate | 12 (11.76) |
| Severe | 6 (5.88) |
| Profound | 77 (75.49) |
| Management | |
| Conservative | 22 (21.57) |
| Surgical | 80 (78.43) |
| Operation (n=80) | |
| Examination under anesthesia and suturing | 14 (17.50) |
| Debridement and external fixation | 12 (15.00) |
| Open reduction and internal fixation | 12 (15.00) |
| Debridement | 9 (11.25) |
| Craniotomy | 8 (10.00) |
| Underwater seal drainage | 6 (7.50) |
| Exploratory laparotomy | 5 (6.25) |
| MUA and POP | 5 (6.25) |
| Amputation | 2 (2.50) |
| Laminectomy | 2 (2.50) |
| Olecranon pin insertion | 2 (2.50) |
| Skull tong traction | 2 (2.50) |
| Incision and drainage | 1 (1.25) |
| HDW admission | |
| Yes | 11 (10.78) |
| No | 91 (89.22) |
| Complications | |
| Yes | 7 (6.86) |
| No | 95 (93.14) |
| Death | |
| Yes | 2 (1.96) |
| No | 100 (98.04) |
Figure 1.
Showing surgical admissions from the Emergency Department of APH, Milne Bay Province, Papua New Guinea, from the 1st of June 2020 to the 21st of December 2020.
75.49% (n=77) of injuries had an injury severity score more than 25. Of the total cohort, 78.43% (n=80) of injuries were surgically managed. Examinations under anaesthesia and suturing was done in 17.50% (n=14) of injuries followed by debridement and external fixation done in 15.00% (n=12) of injuries and open reduction, and internal fixation, done also in 15.00% (n=12) of injuries.
The mean operative time was 1 hour and 30 minutes. The high dependency ward admission rate was 10.78%. The complication rate was 6.86%. Complications reported include; heart failure (n=1), severe sepsis (n=2), pneumothorax (n=1), airway obstruction (n=1), haemorrhagic shock (n=1), and wound site infection (n=1). Five patients with complications were appropriately treated. The mortality rate was 1.96%. One head injury patient died of aspiration pneumonitis, and one patient with multiple gunshot wounds died from haemorrhagic shock.
The mean length of hospital stay was 11.5 days. On average, 13 hospital staffs were involved in the treatment of patients; 3 nursing officer's, 2 community health workers, 2 medical officers, 1 health extension officer, 1 physiotherapist, 1 porter, 1 anaesthetic scientific officer, 1 anaesthetic technical assistant, and 1 laboratory officer.
The direct medical costs of trauma by causes are shown in Table 3. Alcohol related injuries were the most common cause of injuries accounting for K1, 417, 023.73 (US$410,936.88) in direct medical costs. The mean cost for aetiologies was highest amongst motor vehicle accidents with a direct medical cost of K48, 687.40 (US$14, 119.35) per patient followed by criminal attack with K48,497.44 (US$ 14,064.26) per patient, as shown in Figure 2.
Table 3.
Showing the direct medical costs of trauma by causes to APH, Milne Bay Province, Papua New Guinea, from the 1st of June 2020 to the 21st of December 2020.
| Cause | Number of patients (n=100) | Total direct medical cost (Kina) | Mean cost (Kina) | Mean US Dollars |
|---|---|---|---|---|
| Alcohol related injury | 31 | 1,417,023.73 | 45,710.44 | 13,256.03 |
| Falls | 30 | 1,372,911.36 | 45,763.71 | 13,271.48 |
| Falling object injury | 9 | 428,989.53 | 47,665.50 | 13,822.10 |
| Domestic violence | 8 | 349,296.33 | 43,662.04 | 12,661.99 |
| Criminal attack | 7 | 339,482.09 | 48,497.44 | 14,064.26 |
| Motor vehicle accident | 6 | 292,124.42 | 48,687.40 | 14,119.35 |
| Sporting injury | 4 | 192,016.41 | 48,004.10 | 13,921.19 |
| Others | 3 | 129,530.44 | 43,176.81 | 12,521.28 |
| Burns | 2 | 83,286.58 | 41,643.29 | 12,076.55 |
Based on the 2019 yearly average exchange rate obtained from bank of PNG: 1 KINA = 0.29 USD.
Figure 2.
Showing a column line graph of causes of injury by total direct medical costs and mean direct medical costs in Kina.
The direct medical costs by injuries are shown in Table 4. Fractures were found to be the most common injury reported with K 1,907,531.88 (US$553,184.25) incurred in direct medical costs. The mean cost for injury was highest amongst abdominal injuries with a direct medical cost of K55,929.69(US$16,219.61) per patient followed by fractures with K47,688.30 (US$ 13,829.61) per person, as illustrated in Figure 3.
Table 4.
Showing the direct medical costs of trauma by diagnosis to APH, Milne Bay Province, Papua New Guinea, from the 1st of June 2020 to the 21st of December 2020.
| Traumatic injury | Number of patients (n=100) | Total direct medical cost (Kina) | Mean cost (Kina) | Mean US Dollars |
|---|---|---|---|---|
| Fractures | 40 | 1,907,531.88 | 47,688.30 | 13,829.61 |
| Muscle/tendon injury | 21 | 924,903.46 | 44,043.02 | 12,772.48 |
| Head injury | 12 | 531,695.00 | 44,307.92 | 12,849.29 |
| Chest injury | 8 | 341,086.09 | 42,635.76 | 12,364.37 |
| Spinal injury | 7 | 311,274.88 | 44,467.84 | 12,895.67 |
| Abdominal injury | 5 | 279,648.47 | 55,929.69 | 16,219.61 |
| Polytraumatic injury | 4 | 178,906.32 | 44,726.58 | 12,970.71 |
| Burns | 3 | 129,614.79 | 43,204.93 | 12,529.43 |
Based on the 2019 yearly average exchange rate obtained from bank of PNG: 1 KINA = 0.29 USD.
Figure 3.
Showing a column line graph of traumatic injuries by total direct medical cost and mean cost per patient in Kina.
The cost of mortalities were K21,286.07 (US$6,172.96) and K55,894.07 (US$16,209.28) respectively with a total direct medical cost of K77,180.14 (US$22,382.24) and an average cost per mortality of K38,590.07 (US$11,191.12) as shown in Table 5. The total direct medical cost of trauma incurred during the study period was K4, 681,841.03 (US$ 1, 357, 733.90) with an average cost per patient of K45, 900.40 (US$13,311.12).
Table 5.
Showing the direct medical costs of trauma mortality at APH, Milne Bay Province, Papua New Guinea, from the 1st of June 2020 to the 21st of December 2020.
| Cause of death | Number of patients (n=2) | Total cost (Kina) | US dollars |
|---|---|---|---|
| Moderate head injury | 1 | 21,286.07 | 6,172.96 |
| Polytrauma | 1 | 55,894.07 | 16,209.28 |
Based on the 2019 yearly average exchange rate obtained from bank of PNG: 1 KINA = 0.29 USD.
Discussion
This study estimates the direct medical cost of trauma aetiologies and injuries in PNG. The mean demographic age and gender of persons in this study were consistent with LMICs whose poor economic growth, and low productivity were associated with trauma.6,22 The increased injury severity score's and high operative rate of injuries indicates timely surgical intervention.23 As a result, our complication and mortality rates are comparable to studies done in high volume trauma centres globally.24,25
In PNG, the government bears the financial costs of trauma compared to other LMIC's where out of pocket costs represents 30-50% of health care financing.8,26 This substantiates the economic need to address injuries that carry increased risk of morbidity and mortality.
Alcohol related costs make up more than 1% of the gross national product in high, and middle-income countries.27 Productivity loss, road traffic accidents, and legal fees in these same countries can cost up to US$10.36 billion.28 Avid campaigns have therefore ensued to address alcohol related injuries in developed countries.29 With poor profitability, alcohol industries turn to LMICs that have poor laws, and public health interventions against alcohol production and consumption.30 The result is an increase in socioeconomic problems and lawlessness giving rise to high medicals costs.
In 2020, motor vehicle accidents were the third most common cause of disability in developing countries.31 The treatment costs differed from high income countries (HIC) given the varying socioeconomic status, health systems and treatment options. Nevertheless, HICs still account for 53.4% of the total global loss, however, the burden of high treatment costs are greater in LMICs as shown in this study.3
Fractures carry a significant burden in LMICs and affects 779 people per 100 000 population.31 In high income countries the cost of treating fractures is expensive and lower costs seen in LMICs are a result of substandard fracture managements.31,32 This burden is similar for abdominal injuries that can represent almost 4% of an annual health budget despite lack of investigations like computer tomography and magnetic resonance imaging.33
PNG is considered a hot spot for crime.34 In this study, crime related injuries amounted to K339,482.09 (US$ 98,449.81) within 6 months. These costs were consistent with Wesson et al who further showed that appropriate interventions can avert medical costs by US$17,000.00.35 In 2018, WHO reported partial funding of safety strategies in PNG.36 This limits implementation and enforcement of policing given that simple measures like foot patrols significantly reduces crime rates in high violence areas.37
The issues faced in addressing injuries is multifactorial and involves a holistic approach from communities, health workers, administrators, legislators, and law enforcers. Mac Marshall in a report to WHO stated that the country had gone over the brink of alcohol related problems.38 In 2018, a team from the Constitutional Law Reform Commission of PNG stated that the laws regulating the manufacturing, sale and consumption of alcohol were no longer suitable.39
This study has various limitations. The medical and dental catalogue was last updated in 2012 and the direct medical costs for electricity usage for pathology and radiology were not included in this study. We could not obtain an updated catalogue as it was still under review. Electricity costs for pathology and radiology could not be obtained due to restrictions on non-laboratory and non-radiology staff. As a result, current costs presented may be underestimated. In our study, injuries relating to alcohol were obtained from history records. This presents uncertainties as we could not test for blood alcohol levels. Verification of alcohol in assaults also lack justifiable evidence when relying on history records alone. Blood alcohol testing should be introduced to verify alcohol levels and help with management.
Conclusion
Poor regulation of alcohol and road safety is associated with high surgical costs. As such, injuries must be made a priority in health policies and public health interventions. In an era of financial instability, reducing injuries is economical in achieving health care objectives that rely heavily on adequate funding, and financing.
Declaration of interests
We have no conflict of interest to declare.
Acknowledgments
Contributors
The study design, methodology, data verification, formal analysis and writing of original draft and editing was done by Dr Umo. The study idea, contribution to write up review and editing was done by Dr James. Data collection was done by Fiona Didilemu and Dr Borchem. Data analysis and data verification was done by Dr Inaido. Contribution to write up and data verification was done by Bernard Sinen and Dr Ikasa.
Acknowledgements
The authors would like to thank:
Dr Okaipa, Dr Pangiau, Mr Roidi and Mr Wolly of the Anaesthetic division of Alotau Provincial Hospital for their support and cooperation during this study.
Mr. Anthony, Mr. Marona and Sr. Sodias of the nursing division of Alotau Provincial Hospital for their cooperation in the study.
Ms. Stella Iwais of the office of Policy, Planning and Coordination, MPHA for providing the hospital fees and staff salaries.
Mr Charles Malaibe from PNG Power for assisting with electricity costs.
Data sharing statement
Data on summary of costs for hospital resources, salaries and hospital fees are provided in the supplementary file.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanwpc.2021.100379.
Appendix. Supplementary materials
References
- 1.Magruder KM, McLaughlin KA, DE Borbon. Trauma is a public health issue. Eur J Psychotraumatol. 2017;8(1) doi: 10.1080/20008198.2017.1375338. published online 2017 oct 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO (2018) Global status report on road safety, 2018. Available online: https://www.who.int/publications-detail-redirect/9789241565684
- 3.Chen S, Kuhn M, Prettner K, Bloom D. The global macroeconomic burden of road injuries: estimates and projections for 166 countries. Lancet planet health. 2019;3(3):e390–e398. doi: 10.1016/S2542-5196(19)30170-6. https://www.thelancet.com/pdfs/journals/lanplh/PIIS2542-5196(19)30170-6.pdf [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. World health report on road traffic injury prevention. 2004. http://www.who.int/violence_injury_prevention/publication/road_traffic/world_report/chapter2.pdf.
- 5.Wainiqolo I, Kafoa B, Kool B., et al. A profile of Injury in Fiji: findings from a population-based injury surveillance system (TRIP-10) BMC Public Health. 2012;12:1074. doi: 10.1186/1471-2458-12-1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miovsky M, Gavurova B, Ivankova V, Rigelsky M, Sejvl J. Fatal injuries and economic development in the population sample of Central and Eastern European Countries: the perspective of adolescents. Int J Public Health. 2020;65:1403–1412. doi: 10.1007/s00038-020-01449-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ponifasio P, Poki HO, Watters DA. Abdominal trauma in urban Papua New Guinea. PNG Med J. Mar-Jun 2001;441(1-2):36–42. PMID: 12418676. [PubMed] [Google Scholar]
- 8.Grundy J, Dakulala P, Wai K, Maalsen A, Whittaker M. Vol. 9. World Health Organization; New Dehli: 2019. (Papua New Guinea Health System Review). Regional Office for South East Asia. [Google Scholar]
- 9.Matthew PK, Kapua F, Soaki PJ, Watters DA. Trauma admissions in Southern Highlands of Papua New Guinea. Aust N Z J Surg. 1996 Oct; 66;(10):659–663. doi: 10.1111/j.1445-2197.1996.tb00712.x. [DOI] [PubMed] [Google Scholar]
- 10.Reynolds TA, Stewart B, Drewett I, et al. The impact of trauma care systems in Low and Middle Income countries: Needs and strategies. April 2016. Annual review of public health 37(1). https://pubmed.ncbi.nlm.nih.gov/28125389/ [DOI] [PubMed]
- 11.Meara JG, Leather AJ, Hagander L, et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386:569–624. doi: 10.1016/S0140-6736(15)60160-X. [DOI] [PubMed] [Google Scholar]
- 12.Shrime M.G. Getting Costs Right in Global Surgery. World J Surg. 2021 doi: 10.1007/s00268-021-06300-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Umo I, James K. The Direct Medical Cost of Acute Appendicitis Surgery in a Resource-Limited Setting of Papua New Guinea. World J Surg. 2021 Aug 14 doi: 10.1007/s00268-021-06290-2. [DOI] [PubMed] [Google Scholar]
- 14.Chen Y, Zhang Y, Jin T, Li H, Shi L. World Scientific Publishing; Singapore: 2018. Statistics in Economic Health. Handbook of Medical Statistics; pp. 775–778. [Google Scholar]
- 15.National Statistical Office . 2011. PNG Population Census 2011 report.https://actnowpng.org/sites/ [Cited 28 Oct 2019]. Available from URL: [Google Scholar]
- 16.James K, Bochem I, Taulo R, et al. Universal access to safe, affordable, timely surgical and anaesthetic care in Papua New Guinea: the six global health indicators. ANZ J Surg. 2020 doi: 10.1111/ans.16148. [DOI] [PubMed] [Google Scholar]
- 17.Adam Anokye. Sample Size Determination in Survey Research. Journal of Scientific Research and Reports. 2020;26:90–97. doi: 10.9734/JSRR/2020/v26i530263. [DOI] [Google Scholar]
- 18.Mitchell R, McKup J, Bue O, et al. Implementation of a novel three-tier triage tool in Papua New Guinea: A model for resource-limited emergency departments. Lancet Regional Health Western Pacific. 2020;5 doi: 10.1016/j.lanwpc.2020.100051. DECEMBER 01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mock C, Lormand JD, Goosen J, Joshipura M, Peden M. Guidelines for essential trauma care. Journal of Eme Nurs. Feb 2006;32(1):89–90. doi: 10.1016/j.j.2005.08.004. [DOI] [Google Scholar]
- 20.Bolorunduro OB, Villegas C, et al. Validating the Injury Severity Score (ISS) in different populations: ISS predicts mortality better among Hispanics and females. J Surg Res. 2011 Mar; 166;(1):40–44. doi: 10.1016/j.jss.2010.04.012. [PubMed] [Google Scholar] [DOI] [PubMed] [Google Scholar]
- 21.Medical and Dental Health Catalogue. Papua New Guinea National Health Department. 10th Ed. 2012. PDF. Available online: https://drive.google.com/uc?export=download&id=1OIJFZvSQ8STYTrP1UBSUDQ2NREdYFvBK.
- 22.Essue BM, Laba M., Knaul F, et al. In: Disease Control Priorities: Improving Health and Reducing Poverty. 3rd ed. Jamison DT, Gelband H, Horton S, Jha P, Laxminarayan R, Mock CN, Nugent R, editors. The International Bank for Reconstruction and Development/The World Bank; Washington (DC): 2017 Nov 27. Economic Burden of Chronic Ill Health and Injuries for Households in Low- and Middle-Income Countries. Chapter 6. PMID: 30212160. [PubMed] [Google Scholar]
- 23.Mitra B, Bade-Boon J, Fitzgerald MC, Beck B, Cameron PA. Timely completion of multiple life-saving interventions for traumatic haemorrhagic shock: a retrospective cohort study. Burns Trauma. 2019 Jul 18;7:22. doi: 10.1186/s41038-019-0160-5. PMID: 31360731;PMCID:PMC6637602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pape M., Giannakópoulos G.F., Zuidema W.P., et al. Is there an association between female gender and outcome in severe trauma? A multi-center analysis in the Netherlands. Scand J Trauma Resusc Emerg Med. 2019;27:16. doi: 10.1186/s13049-019-0589-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abe T, Komori A, Shiraishi A, et al. Trauma complications and in hospital mortality: failure to rescue. Crit Care. 2020;24:223. doi: 10.1186/s13054-020-02951-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mills A. Health Care Systems in Low- and Middle-Income Countries. N Engl J Med. 2014;370:552–557. doi: 10.1056/NEJMra1110897. [DOI] [PubMed] [Google Scholar]
- 27.Munter LD, Geraerds AJ, Jongh M, et al. Prognostic factors for medical and productivity costs, and return to work after trauma. PLOS ONE. 2020 doi: 10.1371/journal.pone.0230641. Published: March 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alcohol, tobacco & other drugs in Australia. Australian Institute of Health and Welfare. Available online: https://www.aihw.gov.au/reports/alcohol/alcohol-tobacco-other-drugs-australia/contents/impacts/economic-impacts
- 29.Walls H, Cook S, Matzopoulos R, Matzopoulos R, London L. Advancing alcohol research in low-income and middle-income countries: a global alcohol environment framework. BMJ Global Health. 2020;5 doi: 10.1136/bmjgh-2019-001958. https://gh.bmj.com/content/5/4/e001958.info [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walls H, Cook S, Matzopoulos R, Matzopoulos R, London L. Advancing alcohol research in low-income and middle-income countries: a global alcohol environment framework. BMJ Global Health. 2020;5 doi: 10.1136/bmjgh-2019-001958. https://gh.bmj.com/content/5/4/e001958.info [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cordero Daniella M, Miclau, et al. Vol. 3. OTA International; June 2020. p. e062. (The global burden of musculoskeletal injury in low and lower-middle income countries). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.El Ayoubi A, Bouhelo KPB, Chafik H, et al. Le coût médical direct de la prise en charge hospitalière des fractures de l'extrémité supérieure du fémur [Direct medical costs of hospital treatment of fractures of the upper extremity of the femur] Pan Afr Med J. 2017 Jun 20;27:133. doi: 10.11604/pamj.2017.27.133.6731. French. PMID: 28904663;PMCID:PMC5567962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Allard D, Burch VC. The cost of treating serious abdominal firearm related injuries in South Africa. S Afr Med J. 2005 Aug;95(8):591–594. PMID: 16201002. [PubMed] [Google Scholar]
- 34.Overseas Security Advisory Council. (2019). Papua New Guinea 2019 Crime & Safety Report. Retrieved from https://www.osac.gov/Country/PapuaNewGuinea/Content/Detail/Report/a60b5cea-2768-4872-8981-15f4aeaad1db
- 35.Wesson HK, Boikhutso N, Bachani AM, Hofman KJ, Hyder AA. The cost of injury and trauma care in low- and middle-income countries: a review of economic evidence. Health Policy Plan. 2014;29(6):795–808. doi: 10.1093/heapol/czt064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Global status report of Road Safety 2018. World Health Organization. Available Online: https://www.who.int/publications/i/item/9789241565684
- 37.Piza E., O'Hara BA. Saturation Foot-Patrol in a High-Violence Area: A Quasi-Experimental Evaluation. CrimRxiv. 2021 doi: 10.21428/cb6ab371.1d2aeed0. [DOI] [Google Scholar]
- 38.Marshall M. In: Alcohol and Public Health in 8 Developing Countries. Riley L., Marshall M., editors. WHO,Department of Mental Health and Substance Abuse; Geneva: 1999. ‘Country Profile on Alcohol in Papua New Guinea’; pp. 115–134. [Google Scholar]
- 39.Review of Laws on Use and Abuse Of Alcohol and Drugs. Constitutional and Law Reform Commission of PNG. 2018. Available Online: https://www.clrc.gov.pg/node/28
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.