Abstract
Attachment security may be a mechanism by which exposure to early life adversity affects subsequent generations. We used a prospective cohort design to examine this possibility in a convenience sample of 124 women (age = 23–45 years, M = 32.32 [SD = 4.83] years; 57.3% White, 22.6% Asian) who provided self-reports of attachment style during pregnancy using the Attachment Style Questionnaire, of whom 96 (age = 28–50 years, M = 36.67 [SD = 4.90] years; 60.4% White, 19.8% Asian) were reassessed when their child was preschool-age (M = 4.38 [SD = 1.29] years). Women self-reported on their own childhood maltreatment severity and their child’s current emotional and behavioral problems using the Childhood Trauma Questionnaire and the Child Behavior Checklist for ages 1.5–5, respectively. Maternal childhood maltreatment severity was associated with less secure, and more avoidant and anxious attachment. Mediation analyses revealed further that less secure maternal attachment, but not avoidant or anxious attachment, mediated the associations between maternal childhood maltreatment and offspring emotional and behavioral problems. These findings suggest that improving maternal attachment security, which can be identified even prior to the child’s birth, is an important target to consider for intervention efforts aimed at minimizing adverse intergenerational effects of early life adversity.
Keywords: Childhood maltreatment, Adult attachment, Pregnancy, Intergenerational effects
Introduction
The adverse effects of stressful experiences can be transmitted across generations [1]. Severe stress exposure in parents, including experiencing childhood maltreatment, is a risk factor for emotional and behavioral problems in offspring [2, 3]. In particular, maternal experiences of maltreatment during childhood are associated with increased rates of offspring emotional difficulties across childhood and adolescence [4-6].
Adverse experiences in childhood have been associated with the development of insecure attachment styles in adulthood [7]. Adult attachment is often conceptualized along three dimensions or “attachment styles” drawn from infant–caregiver attachment theory [8, 9]: attachment avoidance, attachment anxiety, and attachment security [10, 11]. In this model of adult attachment, adults who identify most strongly with the avoidant style report feeling uncomfortable getting close to or trusting others; those identifying with the anxious style report worrying that close others do not really love them or may leave them; and those who identify with the secure style report being confident that they can depend on and trust in others [10].
Maternal attachment style is a potential mechanism for the intergenerational effects of mothers’ history of childhood maltreatment on risk for emotional and behavioral problems in their offspring. Childhood maltreatment is associated with elevated rates of avoidant and anxious attachment styles across development [12], and attachment styles tend to remain stable into adulthood [13-15]. Further, there is evidence that a mother’s attachment style during their child’s early life affects child development: avoidant attachment in mothers has been associated with developmental delay in infants [16] and mothers’ attachment insecurity has been prospectively associated with higher internalizing symptoms in their children [17]. Although researchers have found that adult attachment style mediates the effects of early life adversity on risk for psychopathology in adults [18, 19], there have been fewer investigations of intermediate mechanisms for intergenerational transmission of environmentally conferred risks. One previous paper has found evidence that avoidant and anxious adult attachment styles mediate the association between maternal adverse childhood experiences and child internalizing and externalizing symptoms [20]; however in this study, both maternal attachment style and child behavioral problems were assessed when children were 60 months of age. Because attachment style describes a framework for mutual interpersonal relationships and despite the generally observed stability of attachment style over time, it is possible that the child’s inherent temperament and characteristics may affect the mother’s attachment style if assessed post birth. In order to identify the causal direction of any association, therefore, it is important to measure maternal attachment style prior to any relational interactions with the child, i.e., before the child is born. If maternal attachment style in pregnancy mediates the effect of maternal childhood maltreatment severity on risk for emotional and behavioral problems in offspring, then attachment style may be a modifiable treatment target in peripartum women whose offspring are at elevated risk for psychopathology.
The current study examined the links among the severity of mothers’ experiences of childhood maltreatment, their attachment styles during pregnancy, and their offspring’s emotional and behavioral problems. Using a longitudinal design, we assessed maternal attachment security when women were in their third trimester of pregnancy. Following the birth of their children, women were then contacted again when these children were between ages 18 to 72 months in order to obtain assessments of their children’s current emotional and behavioral problems. A retrospective report was used to assess the severity of women’s exposure to maltreatment during their own childhoods. Based on findings that maternal maltreatment experiences in childhood are associated with offspring psychopathology [2, 3, 21] and that maternal adult attachment style is linked to offspring psychopathology in childhood [17], we hypothesized that maternal attachment security mediates the association of maternal childhood maltreatment history with offspring emotional and behavioral problems.
Methods
Participants
Participants were 124 women who were recruited from local obstetric clinics, the Stanford Women’s Wellness psychiatric clinic, and through postings in the community between September 2011 and July 2016 during their pregnancies, comprising a convenience sample that was enriched for psychopathology via recruitment in the psychiatric clinic. Participants were, on average, 32.3 years old (SD = 4.6 years) at the initial assessment. More than half of the respondents were Caucasian (60%) and had a graduate degree (59%). Of the 124 women in the initial sample, 96 completed a longitudinal follow-up assessment when the child with whom they were pregnant at the initial assessment was between 18 and 72 months of age (M child age = 52.6 ± 15.5 months). Additional sample characteristics are detailed in Table 1. All study procedures were approved by the Stanford University Institutional Review Board, and all participants provided informed consent prior to participating.
Table 1.
Sample demographics
| Sample with child follow-up data (N = 96) |
|
|---|---|
| Maternal age at intake | Mean ± SD years |
| 32.32 ± 4.83 | |
| Maternal race\ethnicity | Number (percent) |
| White | 58 (60) |
| East Asian or East Asian American | 13 (14) |
| South Asian or South Asian American | 6 (6) |
| Hispanic | 8 (8) |
| Black or African American | 1 (1) |
| More than one | 10 (10) |
| Maternal education | Number (percent) |
| Some college credit, no degree | 3 (3) |
| Trade/technical/vocational training | 2 (2) |
| Associate degree | 4 (4) |
| Bachelor’s degree | 29 (30) |
| Graduate degree | 57 (59) |
| Other | 1 (1) |
| Maternal employment status | Number (percent) |
| Employed for wages | 49 (51) |
| Self-employed | 13 (14) |
| Out of work but not looking for work | 3 (3) |
| Homemaker | 28 (29) |
| Student | 1 (1) |
| Unable to work | 1 (1) |
| Other | 1 (1) |
| Maternal marital status | Number (percent) |
| Single, never married | 4 (4) |
| Married or domestic partnership | 89 (93) |
| Separated | 3 (3) |
| Income | Number (percent) |
| $0–5000 | 1 (1) |
| $30,001–60,000 | 7 (7) |
| $60,001–90,000 | 6 (6) |
| $90,001–150,000 | 23 (24) |
| Greater than $150,000 | 56 (58) |
| Maternal parity | Number (percent) |
| Primiparous (1) | 63 (66) |
| Multiparous (0) | 33 (34) |
| Child age | Mean ± SD years |
| 4.38 ± 1.29 | |
| Child sex | Number (percent) |
| Male (1) | 48 (51) |
| Female (0) | 46 (49) |
| Child race\ethnicity | Number (percent) |
| White | 53 (55) |
| Asian | 14 (15) |
| Hispanic | 10 (10) |
| Black or African American | 1 (1) |
| Native Hawaiian/Pacific Islander | 1 (1) |
| More than one | 17 (18) |
Procedures
Women participated in an initial session in the third trimester of pregnancy during which they completed a self-report assessment of attachment style (ASQ [22]). Beginning in 2017, these women were re-contacted to complete an online survey hosted on REDCap [23, 24]. At this follow-up assessment, women completed a series of questionnaires. The present analyses focus on their reports of their childhood maltreatment experiences via the Childhood Trauma Questionnaire (CTQ [25]) and reports of their child’s emotional and behavioral problems via the Child Behavior Checklist (CBCL/1.5–5 [26, 27]). Participants who did not complete surveys after initial prompts received e-mail reminders and, if necessary, telephone prompts. Twenty-five eligible participants did not respond to invitations to complete the follow-up survey; the final sample is composed of 96 women who completed both the initial assessment and the follow-up survey.
Measures
Attachment Style
The Attachment Style Questionnaire (ASQ [22]) is a 40-item self-report questionnaire designed to assess adult attachment. The ASQ yields 5 subscales: “confidence” (8 items), “relationships as secondary” (7 items), “need for affirmation” (7 items), “discomfort with closeness” (10 items), and “preoccupation with relationships” (8 items). Each item is rated on a six-point scale from 1 (totally disagree) to 6 (totally agree). A factor analysis of this measure [28] and recent review of adult attachment measures [29] indicate that these subscales map onto three dimensions of attachment—secure, anxious, and avoidant—here referred to as “attachment domains.” Consistent with this previous work, we took the sum of the “need for affirmation” and “preoccupation with relationships” subscales to create a total score for the anxious attachment domain and took the sum of the “relationships as secondary” and “discomfort with closeness” subscales to create a total score for the avoidant attachment domain. The score on the “confidence” subscale served as the score for the secure attachment domain. In this sample, the ASQ demonstrated good to excellent internal consistency across domains: Cronbach’s alphas were good for the secure and anxious attachment domains (0.84 and 0.87, respectively), and excellent for the avoidant attachment domain (0.91).
Maternal Childhood Maltreatment
The Childhood Trauma Questionnaire (CTQ [25]) was used to assess maternal history of childhood abuse and neglect. For each potential experience of abuse and neglect, mothers rated the severity of their experience on a five-point Likert scale from 1 (never true) to 5 (very often true). Total maternal childhood maltreatment was a summed score of the following 5 CTQ subscales: emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect (range 0 to 75, higher scores reflect more severe maltreatment). This variable was square-root-transformed and outlier scores were winsorized to ± 3 standard deviations from the mean in order to normalize the distribution.
Child Emotional and Behavioral Problems
The Child Behavior Checklist for ages 1.5–5 (CBCL/1.5–5 [26, 27]) is designed to assess internalizing and externalizing symptoms in children age 18 months through 5 years based on maternal report. Responses were scored using the Achenbach System of Empirically Based Assessment (ASEBA) computer scoring program [30, 31] that yielded a total summed score of all child problem items. Total scores were also transformed using a square-root-transformation. The CTQ was administered prior to the CBCL in the survey; we did not use counterbalancing in the administration of these measures.
Statistical Analysis
Descriptive statistics were calculated for sociodemographic characteristics for the entire sample (Table 1). Mediation analyses were carried out using SPSS Statistics (v26). We used independent mediation models to test whether each attachment domain (i.e. secure, anxious, avoidant) mediated the association between maternal childhood maltreatment severity and offspring emotional and behavioral problems (see Fig. 1). Lastly, we conducted a single mediation model with all attachment domains and appropriate covariates included simultaneously to examine the indirect effect of each domain over and above the others.
Fig. 1.
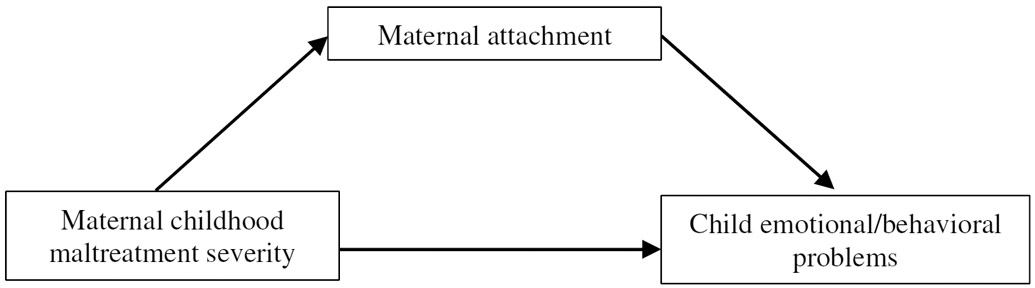
Proposed mediation model
Child age, sex of child, maternal parity, and maternal age were included as covariates on the paths linking maternal childhood maltreatment severity and maternal attachment to child psychopathology symptoms in each of the first three models because these factors may influence the effect of maternal childhood maltreatment on offspring symptoms, but are not likely to influence maternal attachment security given the stability of adult attachment over time [13, 15] and across pregnancy [32].
Mediation models were tested using PROCESS [33], a single-step nonparametric resampling procedure (1000 samples with replacement) for testing indirect effects. In this framework, the indirect effect is the product of the two coefficients from two paths: the adjusted effect of maternal childhood maltreatment severity on maternal attachment style and the adjusted effect of maternal attachment style on child emotional and behavioral problems. To test the statistical significance of the indirect effect, we calculated a 95% bias-corrected bootstrap confidence interval (CI). If the 95% CI does not include 0, then the indirect effect is considered statistically significant, supporting mediation. In the supplement, we also report analyses conducted using the MacArthur approach [34, 35].
Results
Correlations
Bivariate correlations among maternal childhood maltreatment severity, attachment domains, child emotional and behavioral problems, child age, sex of child, maternal parity, and maternal age are presented in Table 2. Maternal childhood maltreatment severity was significantly associated with all three attachment domains in mothers (rsecure = − 0.28, 95% CI [− 0.46, − 0.07], p = 0.009; ranxious=0.39, 95% CI [0.19, 0.55], p < 0.001; ravoidant=0.35, 95% CI [0.15, 0.52], p < 0.001), and with emotional and behavioral problems in children (r = 0.36, 95% CI [0.17, 0.53], p < 0.001). Secure, anxious, and avoidant attachment in mothers were significantly associated with child emotional and behavioral problems; secure attachment was associated with fewer child problems (r = − 0.35, 95% CI [− 0.52, − 0.16], p < 0.001), and anxious and avoidant attachment were associated with more child problems (r = 0.28, 95% CI [0.07, 0.46], p = .008; r=0.24, 95% CI [0.03, 0.43], p = 0.024, respectively). These effects are in the small to medium range based on conventions provided by Cohen [36].
Table 2.
Correlations and descriptive statistics for study variables
| sfdsddAS | Maternal childhood maltreatment severitya |
Secure attachment |
Anxious attachment |
Avoidant attachment |
Child problemsa |
Child age | Child sex | Maternal parity |
Maternal age |
|---|---|---|---|---|---|---|---|---|---|
| Maternal childhood maltreatment severity | 1 | − 0.28** | 0.39** | 0.35** | 0.36* | 0.11 | 0.06 | − 0.01 | 0.12 |
| Secure attachment | 1 | − 0.58** | − 0.65** | − 0.35** | 0.34** | 0.01 | − 0.06 | 0.08 | |
| Anxious attachment | 1 | 0.52** | 0.28** | − 0.24* | 0.11 | − 0.09 | − 0.10 | ||
| Avoidant attachment | 1 | 0.24* | − 0.12 | − 0.02 | > − 0.01 | 0.03 | |||
| Child problems | 1 | 0.15 | 0.06 | 0.06 | 0.02 | ||||
| Child age | 1 | 0.17 | − 0.11 | 0.27** | |||||
| Sex of child (male = 1) | 1 | 0.19 | 0.15 | ||||||
| Maternal parity (primiparous = 1) | 1 | − 0.22* | |||||||
| Maternal age | 1 | ||||||||
| Mean (SD) or % | 12.08 (12.10) | 27.93 (6.21) | 33.68 (11.74) | 31.15 (13.23) | 44.48 (9.84) | 4.38 (1.29) | 52% | 61% | 36.67 (4.90) |
| Range | 0–65 | 8–40 | 9–69 | 4–71 | 28–83 | 1.61–6.32 | 0–1 | 0–1 | 28–50 |
| N availableb | 91 | 118 | 118 | 118 | 90 | 92 | 91 | 122 | 92 |
Descriptives included here are based on scores prior to square root transformation
Sample sizes vary across measures due to reduced participation in the second wave of data collection; some participants not complete all measures in the follow-up survey
p < 0.05
p < 0.01
Mediation Models
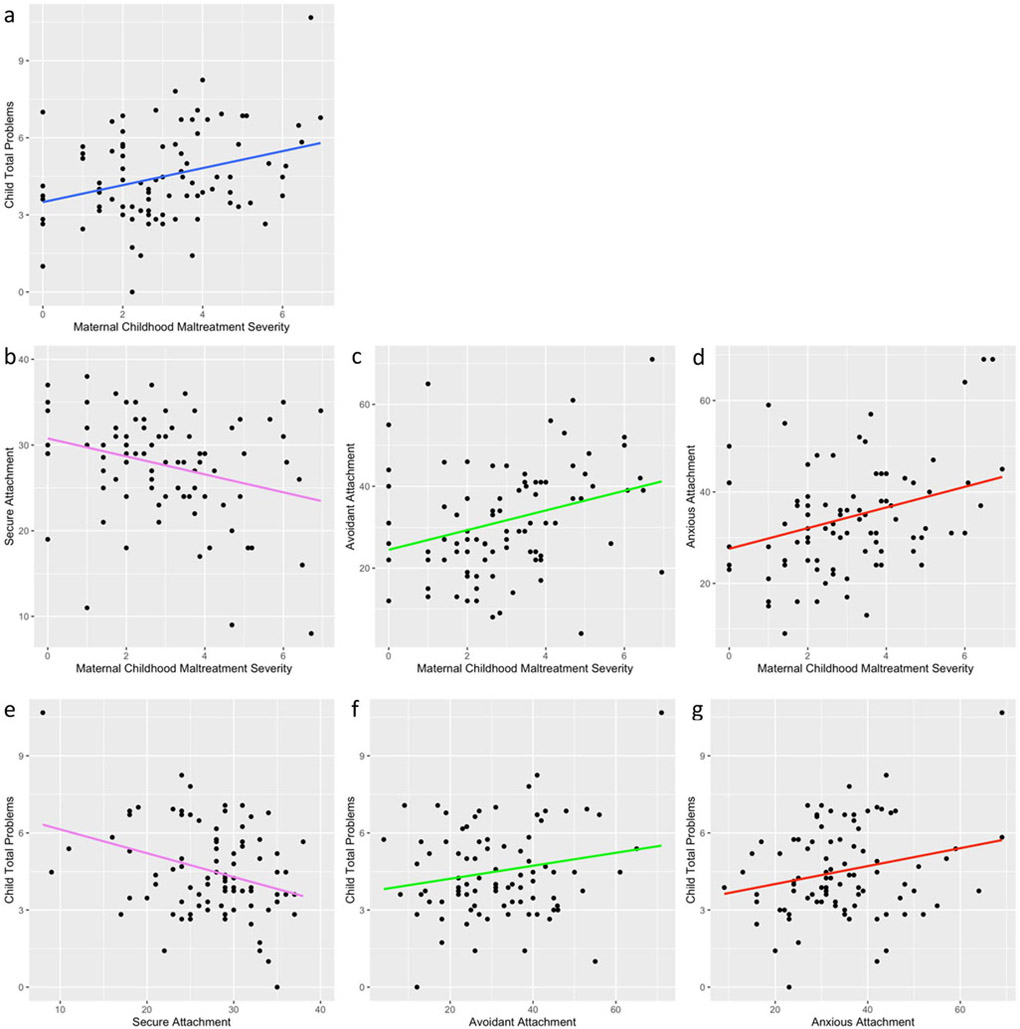
Scatter plots depicting the linear associations between variables entered into the mediation model are presented in Fig. 2. Consistent with our hypothesis, the secure attachment domain mediated the relation between maternal childhood maltreatment severity and child emotional and behavioral problems (standardized indirect effect = 0.09, 95% CI [0.003 0.21]). We did not find evidence that the anxious attachment or avoidant attachment domains mediated this association. These results are summarized in Table 3.
Fig. 2.
Scatterplots depicting linear associations between maternal childhood maltreatment severity, child emotional and behavioral problems, and each measured attachment domain. Coefficients of determination for each regression plot: a R2 = 0.10; b R2 = 0.08; c R2 = 0.09; d R2 = 0.10; e R2 = 0.10; f R2 = 0.04; g R2 = 0.06
Table 3.
Summary of single-step mediation analyses
| Mediator | Direct effect of maternal childhood maltreatment severity |
Direct effect on child emotional/ behavioral problems |
Indirect effect (standardized) |
|---|---|---|---|
| Secure maternal attachment | − 1.09 (− 1.86, − 0.33) | − 0.09 (− 0.16, − 0.03) | 0.09 (0.003, 0.21) |
| Anxious maternal attachment | 2.48 (1.02, 3.94) | 0.03 (− 0.01, 0.06) | 0.07 (− 0.03, 0.19) |
| Avoidant maternal attachment | 2.68 (1.04, 4.32) | 0.02 (− 0.01, 0.05) | 0.04 (− 0.04, 0.18) |
Estimate (95% bias corrected bootstrap confidence intervals). Bolded values indicate significant effects
Finally, to examine the unique effect of secure attachment relative to the combined effects of the other attachment domains, a multiple mediator model with all attachment domains entered as simultaneous mediators in a single-step mediation with child age, sex of child, maternal parity, and maternal age included as covariates on all paths was conducted. The indirect effect of secure attachment remained significant, even when the anxious and avoidant attachment domains were included as simultaneous mediators. Indirect effects from this multiple mediator model are summarized in Table 4.
Table 4.
Summary of mediation analysis with all three attachment domains included
| Mediator | Indirect effect (unstandardized) | Indirect effect (standardized) |
|---|---|---|
| Secure maternal attachment | 0.11 (0.01, 0.26) | 0.10 (0.01, 0.23) |
| Anxious maternal attachment | 0.03 (− 0.06, 0.14) | 0.03 (− 0.06, 0.14) |
| Avoidant maternal attachment | − 0.04 (− 0.12, 0.09) | 0.04 (− 0.04, 0.15) |
| All attachment domains | 0.10 (− 0.03, 0.30) | 0.10 (− 0.04, 0.26) |
Estimate (95% bias corrected bootstrap confidence intervals). Bolded values indicate a significant indirect effect
Results obtained using the MacArthur approach also primarily revealed mediation through secure maternal attachment style, although we also observed a significant indirect effect of anxious maternal attachment style using this method (see Supplement).
Discussion
In a longitudinal sample of 96 mothers and their offspring, we examined the associations among maternal history of childhood maltreatment, maternal attachment security during pregnancy, and offspring emotional and behavioral problems in early life. Bivariate correlation analyses revealed a negative association of small effect between maternal childhood maltreatment severity and maternal attachment security, and moderate positive associations between maternal childhood maltreatment severity and both avoidant and anxious attachment. Maternal childhood maltreatment severity was moderately associated with emotional and behavioral problems in offspring. Further, there was a negative association of medium effect between maternal attachment security and child problems, and small positive associations between maternal anxious and avoidant attachment and child problems [36].
Scores on the secure attachment domain mediated the association between severity of maternal childhood maltreatment and emotional and behavioral problems in offspring; greater maternal attachment security was associated with fewer emotional and behavioral problems in children of mothers who experienced maltreatment in childhood. Although severity of maternal childhood maltreatment was associated with maternal anxious and avoidant attachment scores, these attachment domains did not mediate the association with offspring problems. Using a less conservative approach (see supplement), there was evidence that anxious attachment may also be a mediator, in agreement with the results of Cooke et al. [20]. Notably, however, when all three attachment domains were included in a multiple mediator model, only secure attachment mediated the association between the severity of maternal childhood maltreatment and offspring emotional and behavioral problems. Consistent with previous work, our results indicate that maltreatment during childhood may have intergenerational effects, given that these experiences were associated with elevated emotional and behavioral problems in the offspring of women who were assessed in pregnancy. Overall, our findings indicate that maternal attachment security may be a useful target for intervention, either for identifying families at risk who may benefit postnatally from existing parenting interventions, or as a new intervention target that can be influenced prenatally in order to improve the outcomes of children of mothers who experienced childhood maltreatment. While adult attachment security is relatively stable over time [13, 15] and across the transition to parenthood [32], there is evidence that it can be altered by psychotherapeutic interventions [37-39]. Obtaining a measure of maternal attachment security proximal to the transition to parenthood may provide helpful information regarding risk for offspring dysfunction, and help to identify individuals who may benefit from psychotherapeutic or parenting interventions [38]. The foundation for emotional health across the lifespan is formed in early childhood [41-43]. Given that symptoms of psychopathology can emerge as early as toddlerhood [26, 44, 45] and predict both long-term emotional and behavioral problems [46] and later psychiatric diagnoses [47, 48], identifying predictors of risk is important for determining approaches to intervention.
Although elucidating the pathway from maternal experiences of childhood maltreatment to offspring psychopathology is useful for identifying potential treatment targets and mother–child dyads who may be at elevated risk for negative outcomes, an unanswered question concerns the mechanisms that link maternal attachment style in pregnancy with subsequent child functioning. Candidate mechanisms include the attachment relationship between the mother and child, and specific caregiving behaviors provided by the mother. Fraiberg, Adelson, and Shapiro [49] introduced the metaphor of “ghosts in the nursery,” in which parents’ past traumas are posited to affect their ability to provide sensitive and responsive caregiving for their infants. Consistent with this theory, empirical evidence suggests that histories of childhood maltreatment and unresolved trauma in mothers are associated with distorted prenatal representations of the infant [50], as well as problematic trauma-specific reflective functioning and disorganized infant attachment [51]. Further, a mother’s own childhood experiences with caregivers may influence her attachment style in ways that affect how she perceives and cares for her child [52, 53]. It is important to note that early life experiences, though important, are not likely to be the unique determinants of attachment security. There is evidence that both genetics [54] and experiences in adulthood influence attachment style [10].
There are alternative and non-mutually exclusive explanations to consider when examining the link between maternal maltreatment history and child psychopathology. Parenting practices provide one potential pathway given that maternal exposure to childhood maltreatment is associated with poorer quality mother–child interactions and increased parenting distress [55]. Another framework suggests that maternal childhood maltreatment severity changes the gestational environment, rendering offspring more vulnerable to emotional and behavioral problems and later psychopathology via biological embedding of life experiences and fetal risk for health and disease [56, 57]. Consistent with this framework, previous studies have documented the adverse effects of maternal prenatal stress on offspring temperament [58], physiology [59, 60], and neuroendocrinology [61]. We are unable to determine the unique influences of each of these possibilities in the present study.
Based on the present findings, it is possible that interventions targeting maternal attachment will improve mental health outcomes in the offspring of women with histories of childhood maltreatment. Further, this work suggests that a focus on increasing attachment security will be more effective than attempts to eradicate anxious or avoidant tendencies. In this context, there are several interventions that may be useful for caregivers of young children, such as the Attachment, Regulation, and Competency framework (ARC [62]), Attachment and Biobehavioral Catch-up (ABC [40]), and the Circle of Security intervention (COS [63]) for parents and children. Our findings support the use of maternal attachment as a useful measure for identifying families who may benefit from these existing interventions. Alternatively, given that we found evidence that maternal attachment security during pregnancy is important for child functioning, interventions aimed at improving mental health in at-risk offspring that focus on adult attachment relationships may be offered to pregnant women prior to the birth of their child. Strengthening the social bonds between the mother and her close associates will help ensure that children are born into the predictable, loving, supportive environments that will give them the best start in life.
Several modalities of adult psychotherapy have been found to improve adult attachment security [37, 39, 64-66], including psychodynamic-interpersonal [37, 64, 66], cognitive-behavioral [66], and integrated [67] approaches. Levy et al. [65] found a significant increase in secure attachment in individuals with borderline personality disorder who were assigned to a group-based transference-focused intervention, but not in individuals who were assigned to a dialectical behavioral therapy or psychodynamic supportive group. Similarly, Kilmann et al. [38] implemented a brief attachment-focused group intervention with women classified as avoidant or anxiously attached, and found that women who received the intervention reported improved interpersonal relationships, reduced engagement in dysfunctional relationship thinking, and more secure attachment patterns at 6-month follow-up. Taken together, these findings indicate that increases in attachment security coincide with improvements in interpersonal functioning, a promising target for women transitioning to motherhood. Further, activating attachment security via contextual priming has been found to increase empathic behaviors and inhibits personal distress [68]. Thus, targeting maternal attachment security may positively affect parenting behaviors by reducing parental distress and increasing parental empathy. Additional research is needed to determine whether targeting maternal attachment security or parenting behaviors directly is more effective in reducing psychopathology in children of mothers who experienced maltreatment in childhood.
While these findings are important in extending results of previous investigations concerning the effects of parental life history on child outcomes, we should note several limitations of this study. First, all measures included were self-report, and may be influenced by social desirability or demand characteristics. For example, participants may be reluctant to report avoidant or anxious attachment tendencies or may report otherwise biased estimates of their own attachment security. They may also be reluctant to endorse sensitive items related to childhood maltreatment experiences, leading to possible underreporting of childhood maltreatment severity.
Given that the assessments of childhood maltreatment and child behavioral and emotional problems were not counterbalanced, we cannot rule out the possibility that there may be order effects. There is evidence that maternal characteristics influence reports of child behavior [68]. Other researchers have addressed this concern by obtaining data on child behavior from multiple informants [17]. The inclusion of a second rater’s report of offspring behavior, such as a report from the child’s other parent or teacher, would strengthen the present study. In addition, despite well-validated age-based norms supporting the utility of the CBCL in examining emotional and behavioral problems in children between 18 and 72 months of age [31], there are significant developmental changes that occur over this period that could influence our conclusions. Future studies with larger samples would benefit from considering age as a moderator of these associations to examine potential stability or change across development. Second, we obtained information on maternal history of childhood maltreatment using retrospective report [25], which may be influenced by memory for childhood events. Retrospectively-reported childhood adverse experiences have been found to have low to moderate agreement with experiences prospectively documented throughout childhood [69].
With this study design in particular, it is possible that post-birth experiences influence recall of childhood events, or that attachment style influences reporting of childhood experiences, such that women with insecure attachment styles might either over- or under-report experiences as traumatic compared with securely attached women. More broadly, although we did not collect information on maternal childhood temperament or personality, it is possible that maternal characteristics influenced experiences of maltreatment and, potentially, their attachment styles and offspring emotional and behavioral problems. Future studies may benefit from using genetically informed designs (e.g., [70, 71]) in order to elucidate the pathways linking maternal childhood experiences to offspring outcomes. Further, the CTQ does not measure additional characteristics of maltreatment experiences, including the onset, chronicity, and frequency of these experiences. Finally, this sample was not representative of the general U.S. population, given lower representation of Black and Hispanic or Latinx populations, higher representation of Asian or Asian American populations, and higher levels of education and income. This may limit the generalizability of our results. Larger and more population-representative samples would allow investigators to examine offspring sex/gender, age, and race/ethnicity as moderators of these associations.
Summary
Stressful experiences in early life can adversely influence long-term behavior, including in ways that propagate to individuals’ offspring. The mechanisms by which early life stress exerts effects that span generations may include attachment styles. The current study adds to previous work mapping pathways from women’s experiences in childhood and their young offspring’s mental health through attachment security reported in pregnancy. We provide evidence that maternal attachment security explains, in part, the association between maternal childhood experiences of maltreatment and offspring psychopathology. Our findings have relevant clinical implications given that attachment security has been found to predict response to psychotherapeutic interventions [72], and because, in contrast to life history, attachment security can be modified in the context of psychotherapy [38, 67].
Supplementary Material
Acknowledgements
We thank Nicole Wilcox, MD, Susan Crowe, MD, Lin Lee, CNM, and Maria Greulich, CNM for their assistance with the initial recruitment of the cohort. We would also like to acknowledge all the women who provided their time and information to this research.
Funding
Salary support during recruitment was provided by an NIMH T32 Training Grant at the Stanford University Department of Psychiatry (5T32MH019938-19; PI: Schatzberg; trainee: Robakis). Collection of the follow-up data was funded by a Stanford University Maternal and Child Health Research Institute Clinician-Educator grant and a Stanford Psychiatry Departmental Innovator Grant to TR. Salary support was also provided by a Jacobs Foundation Early Career Research Award to KH (2017-1261-05). The Stanford REDCap platform (http://redcap.stanford.edu) is developed and operated by Stanford Medicine Research IT team. The REDCap platform services at Stanford are subsidized by (a) Stanford School of Medicine Research Office, and (b) the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1 TR001085.
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the Stanford University Institutional Review Board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s10578-020-01073-7) contains supplementary material, which is available to authorized users.
References
- 1.Bowers ME, Yehuda R (2016) Intergenerational transmission of stress in humans. Neuropsychopharmacology 41:232–244. 10.1038/npp.2015.247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Plant DT, Jones FW, Pariante CM, Pawlby S (2017) Association between maternal childhood trauma and offspring childhood psychopathology: mediation analysis from the ALSPAC cohort. Br J Psychiatry 211:144–150. 10.1192/bjp.bp.117.198721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Babcock Fenerci RL, Allen B (2018) From mother to child: Maternal betrayal trauma and risk for maltreatment and psychopathology in the next generation. Child Abus Negl 82:1–11. 10.1016/j.chiabu.2018.05.014 [DOI] [PubMed] [Google Scholar]
- 4.Rijlaarsdam J, Stevens GWJM, Jansen PW et al. (2014) Maternal childhood maltreatment and offspring emotional and behavioral problems: maternal and paternal mechanisms of risk transmission. Child Maltreat 19:67–78. 10.1177/1077559514527639 [DOI] [PubMed] [Google Scholar]
- 5.Min MO, Singer LT, Minnes S et al. (2013) Mediating links between maternal childhood trauma and preadolescent behavioral adjustment. J Interpers Violence 28:831–851. 10.1177/0886260512455868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Myhre MC, Dyb GA, Wentzel-Larsen T et al. (2014) Maternal childhood abuse predicts externalizing behaviour in toddlers: a prospective cohort study. Scand J Public Health 42:263–269. 10.1177/1403494813510983 [DOI] [PubMed] [Google Scholar]
- 7.Oshri A, Sutton TE, Clay-Warner J, Miller JD (2015) Child maltreatment types and risk behaviors: associations with attachment style and emotion regulation dimensions. Pers Individ Dif 73:127–133. 10.1016/j.paid.2014.09.015 [DOI] [Google Scholar]
- 8.Bowlby J (1969) Attachment and loss. In: Attachment, Vol. 1 [Google Scholar]
- 9.Ainsworth MDS, Blehar MC, Waters E, Wall SN (1978) Patterns of attachment: a psychological study of the strange situation. Erlbaum, Hillsdale [Google Scholar]
- 10.Hazan C, Shaver P (1987) Romantic love conceptualized as an attachment process. J Pers Soc Psychol 52:511–524. 10.1037/0022-3514.52.3.511 [DOI] [PubMed] [Google Scholar]
- 11.Hazan C, Shaver PR (1990) Love and work: an attachment-theoretical perspective. J Pers Soc Psychol 59:270–280. 10.1037/0022-3514.59.2.270 [DOI] [Google Scholar]
- 12.Sroufe LA (2005) Attachment and development: a prospective, longitudinal study from birth to adulthood. Attach Hum Dev 7:349–367. 10.1080/14616730500365928 [DOI] [PubMed] [Google Scholar]
- 13.Fraley RC (2002) Attachment stability from infancy to adulthood: Meta-analysis and dynamic modeling of developmental mechanisms. Personal Soc Psychol Rev 6:123–151 [Google Scholar]
- 14.Waters E, Merrick S, Treboux D et al. (2000) Attachment security in infancy and early adulthood: a twenty-year longitudinal study. Child Dev 71:684–689. 10.1111/1467-8624.00176 [DOI] [PubMed] [Google Scholar]
- 15.Waters E, Weinfield NS, Hamilton CE (2000) The stability of attachment security from infancy to adolescence and early adulthood. Child Dev 71:703–706. 10.1111/1467-8624.00179 [DOI] [PubMed] [Google Scholar]
- 16.Alhusen JL, Hayat MJ, Gross D (2013) A longitudinal study of maternal attachment and infant developmental outcomes. Arch Womens Ment Health 16:521–529. 10.1007/s00737-013-0357-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reck C, Nonnenmacher N, Zietlow AL (2016) Intergenerational transmission of internalizing behavior: the role of maternal psychopathology, child responsiveness and maternal attachment style insecurity. Psychopathology 49:277–284. 10.1159/000446846 [DOI] [PubMed] [Google Scholar]
- 18.Widom CS, Czaja SJ, Kozakowski SS, Chauhan P (2018) Does adult attachment style mediate the relationship between childhood maltreatment and mental and physical health outcomes? Child Abuse Negl 76:533–545. 10.1016/j.chiabu.2017.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bifulco A, Kwon J, Jacobs C et al. (2006) Adult attachment style as mediator between childhood neglect/abuse and adult depression and anxiety. Soc Psychiatry Psychiatr Epidemiol 41:796–805. 10.1007/s00127-006-0101-z [DOI] [PubMed] [Google Scholar]
- 20.Cooke JE, Racine N, Plamondon A et al. (2019) Maternal adverse childhood experiences, attachment style, and mental health: pathways of transmission to child behavior problems. Child Abus Negl 93:27–37. 10.1016/j.chiabu.2019.04.011 [DOI] [PubMed] [Google Scholar]
- 21.Babcock Fenerci RL, DePrince AP (2018) Intergenerational transmission of trauma: maternal trauma–related cognitions and toddler symptoms. Child Maltreat 23:126–136. 10.1177/1077559517737376 [DOI] [PubMed] [Google Scholar]
- 22.Feeney JA, Noller P, Hanrahan M (1994) Assessing adult attachment. In: Sperling MB, Berman WH (eds) Attachment in adults: clinical and developmental perspectives. Guilford Press, New York, pp 128–152 [Google Scholar]
- 23.Harris PA, Taylor R, Thielke R et al. (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harris PA, Taylor R, Minor BL et al. (2019) The REDCap consortium: building an international community of software platform partners. J Biomed Inform 95:103208. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bernstein DP, Stein JA, Newcomb MD et al. (2003) Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abus Negl 27:169–190. 10.1016/S0145-2134(02)00541-0 [DOI] [PubMed] [Google Scholar]
- 26.Achenbach TM (1999) The Child Behavior Checklist and related instruments. In: The use of psychological testing for treatment planning and outcomes assessment, 2nd edn. Lawrence Erlbaum Associates Publishers, Mahwah, pp 429–466 [Google Scholar]
- 27.Achenbach TM, Rescorla LA (2000) Manual for the ASEBA preschool forms & profiles. University of Vermont, Burlington [Google Scholar]
- 28.Brennan KA, Clark CL, Shaver PR (1998) Self-report measurement of adult attachment: an integrative overview. In: Simpson JA, Rholes WS (eds) Attachment theory and close relationships. Guilford Press, New York, pp 46–76 [Google Scholar]
- 29.Ravitz P, Maunder R, Hunter J et al. (2010) Adult attachment measures: a 25-year review. J Psychosom Res 69:419–432. 10.1016/j.jpsychores.2009.08.006 [DOI] [PubMed] [Google Scholar]
- 30.Achenbach TM, Rescorla LA (2013) Achenbach system of empirically based assessment. In: Volkmar FR (ed) Encyclopedia of autism spectrum disorders. Springer, New York, pp 31–39 [Google Scholar]
- 31.Rescorla LA (2005) Assessment of young children using the Achenbach System of Empirically Based Assessment (ASEBA). Ment Retard Dev Disabil Res Rev 11:226–237. 10.1002/mrdd.20071 [DOI] [PubMed] [Google Scholar]
- 32.Stern JA, Fraley RC, Jones JD et al. (2018) Developmental processes across the first two years of parenthood: stability and change in adult attachment style. Dev Psychol 54:975–988. 10.1037/dev0000481 [DOI] [PubMed] [Google Scholar]
- 33.Hayes A (2013) Introduction to mediation, moderation, and conditional process analysis. Guilford Press, New York [Google Scholar]
- 34.Kraemer HC, Kiernan M, Essex M, Kupfer DJ (2008) How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Heal Psychol 27:S101–S108. 10.1037/0278-6133.27.2(Suppl.).S101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kraemer HC, Wilson GT, Fairburn CG, Agras WS (2002) Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry 59:877–883. 10.1001/archpsyc.59.10.877 [DOI] [PubMed] [Google Scholar]
- 36.Cohen J (1988) Statistical power analysis for the behavioral sciences. Routledge Academic, New York [Google Scholar]
- 37.Travis LA, Binder JL, Bliwise NG, Lynn Horne-Moyer H (2001) Changes in clients’ attachment styles over the course of time-limited dynamic psychotherapy. Psychotherapy 38:149–159. 10.1037/0033-3204.38.2.149 [DOI] [Google Scholar]
- 38.Kilmann PR, Laughlin JE, Carranza LV et al. (1999) Effects of an attachment-focused group preventive intervention on insecure women. Gr Dyn Theory Res Pract 3:138–147. 10.1037/1089-2699.3.2.138 [DOI] [Google Scholar]
- 39.Kirchmann H, Steyer R, Mayer A et al. (2012) Effects of adult inpatient group psychotherapy on attachment characteristics: an observational study comparing routine care to an untreated comparison group. Psychother Res 22:95–114. 10.1080/10503307.2011.626807 [DOI] [PubMed] [Google Scholar]
- 40.Dozier M, Bernard K (2017) Attachment and Biobehavioral Catch-up: addressing the needs of infants and toddlers exposed to inadequate or problematic caregiving. Curr Opin Psychol 15:111–117. 10.1016/j.copsyc.2017.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shonkoff JP, Phillips DA (2000) From neurons to neighborhoods: the science of early childhood development. National Academy Press, Washington: [PubMed] [Google Scholar]
- 42.Britto PR, Lye SJ, Proulx K et al. (2017) Nurturing care: promoting early childhood development. Lancet 389:91–102. 10.1016/S0140-6736(16)31390-3 [DOI] [PubMed] [Google Scholar]
- 43.Coverdale GE, Long AF (2015) Emotional wellbeing and mental health: an exploration into health promotion in young people and families. Perspect Public Health 135:27–36. 10.1177/1757913914558080 [DOI] [PubMed] [Google Scholar]
- 44.Visser JC, Smeekens S, Rommelse N et al. (2010) Assessment of psychopathology in 2- to 5-year-olds: applying the Infant-Toddler Social Emotional Assessment. Infant Ment Health J 31:611–629. 10.1002/imhj.20273 [DOI] [PubMed] [Google Scholar]
- 45.Petty CR, Rosenbaum JF, Hirshfeld-Becker DR et al. (2008) The child behavior checklist broad-band scales predict subsequent psychopathology: a 5-year follow-up. J Anxiety Disord 22:532–539. 10.1016/j.janxdis.2007.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pihlakoski L, Sourander A, Aromaa M et al. (2006) The continuity of psychopathology from early childhood to preadolescence: a prospective cohort study of 3–12-year-old children. Eur Child Adolesc Psychiatry 15:409–417. 10.1007/s00787-006-0548-1 [DOI] [PubMed] [Google Scholar]
- 47.Hofstra MB, Van Der Ende J, Verhulst FC (2002) Child and adolescent problems predict DSM-IV disorders in adulthood: a 14-year follow-up of a Dutch epidemiological sample. J Am Acad Child Adolesc Psychiatry 41:182–189. 10.1097/00004583-200202000-00012 [DOI] [PubMed] [Google Scholar]
- 48.Mesman J, Koot HM (2001) Early preschool predictors of preadolescent internalizing and externalizing DSM-IV diagnoses. J Am Acad Child Adolesc Psychiatry 40:1029–1036. 10.1097/00004583-200109000-00011 [DOI] [PubMed] [Google Scholar]
- 49.Fraiberg S, Adelson E, Shapiro V (1975) Ghosts in the nursery: a psychoanalytic approach to the problems of impaired infant-mother relationships. J Am Acad Child Psychiatry 14:387–421. 10.1016/S0002-7138(09)61442-4 [DOI] [PubMed] [Google Scholar]
- 50.Malone JC, Levendosky AA, Dayton CJ, Bogat GA (2010) Understanding the “ghosts in the nursery” of pregnant women experiencing domestic violence: prenatal maternal representations and histories of childhood maltreatment. Infant Ment Health J 31:432–454. 10.1002/imhj.20264 [DOI] [PubMed] [Google Scholar]
- 51.Berthelot N, Ensink K, Bernazzani O et al. (2015) Intergenerational transmission of attachment in abused and neglected mothers: the role of trauma-specific reflective functioning. Infant Ment Health J 36:200–212. 10.1002/imhj.21499 [DOI] [PubMed] [Google Scholar]
- 52.Huth-Bocks AC, Levendosky AA, Bogat GA, Von Eye A (2004) The impact of maternal characteristics and contextual variables on infant–mother attachment. Child Dev 75:480–496. 10.1111/j.1467-8624.2004.00688.x [DOI] [PubMed] [Google Scholar]
- 53.Crawford A, Benoit D (2009) Caregivers’ disrupted representations of the unborn child predict later infant-caregiver disorganized attachment and disrupted interactions. Infant Ment Health J 30:124–144. 10.1002/imhj.20207 [DOI] [PubMed] [Google Scholar]
- 54.Costa B, Pini S, Gabelloni P et al. (2009) Oxytocin receptor polymorphisms and adult attachment style in patients with depression. Psychoneuroendocrinology 34:1506–1514. 10.1016/j.psyneuen.2009.05.006 [DOI] [PubMed] [Google Scholar]
- 55.Lang AJ, Gartstein MA, Rodgers CS, Lebeck MM (2010) The impact of maternal childhood abuse on parenting and infant temperament. J Child Adolesc Psychiatr Nurs 23:100–110. 10.1111/j.1744-6171.2010.00229.x [DOI] [PubMed] [Google Scholar]
- 56.Buss C, Entringer S, Moog NK et al. (2017) Intergenerational transmission of maternal childhood maltreatment exposure: implications for fetal brain development. J Am Acad Child Adolesc Psychiatry 56:373–382. 10.1016/j.jaac.2017.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Harris A, Seckl J (2011) Glucocorticoids, prenatal stress and the programming of disease. Horm Behav 59:279–289. 10.1016/j.yhbeh.2010.06.007 [DOI] [PubMed] [Google Scholar]
- 58.Davis EP, Glynn LM, Schetter CD et al. (2007) Prenatal exposure to maternal depression and cortisol influences infant temperament. J Am Acad Child Adolesc Psychiatry 46:737–746. 10.1097/chi.0b013e318047b775 [DOI] [PubMed] [Google Scholar]
- 59.Gray SAO, Jones CW, Theall KP et al. (2017) Thinking across generations: unique contributions of maternal early life and prenatal stress to infant physiology. J Am Acad Child Adolesc Psychiatry 56:922–929. 10.1016/j.jaac.2017.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kapoor A, Dunn E, Kostaki A et al. (2006) Fetal programming of hypothalamo-pituitary-adrenal function: prenatal stress and glucocorticoids. J Physiol 572:31–44. 10.1016/j.poly.2005.06.060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hartman S, Freeman SM, Bales KL, Belsky J (2018) Prenatal stress as a risk—and an opportunity—factor. Psychol Sci 29:572–580. 10.1177/0956797617739983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Blaustein ME, Kinniburgh KM (2018) Treating traumatic stress in children and adolescents, second edition: how to foster resilience through attachment, self-regulation, and competency, 2nd edn. The Guilford Press, New York [Google Scholar]
- 63.Powell B, Cooper G, Hoffman K, Marvin B (2016) The circle of security intervention enhancing attachment in early parent-child relationships. The Guilford Press, New York [Google Scholar]
- 64.Fonagy P, Leigh T, Steele M et al. (1996) The relation of attachment status, psychiatric classification, and response to psychotherapy. J Consult Clin Psychol 64:22–31. 10.1037/0022-006X.64.1.22 [DOI] [PubMed] [Google Scholar]
- 65.Levy KN, Meehan KB, Kelly KM et al. (2006) Change in attachment patterns and reflective function in a randomized control trial of transference-focused psychotherapy for borderline personality disorder. J Consult Clin Psychol 74:1027–1040. 10.1037/0022-006X.74.6.1027 [DOI] [PubMed] [Google Scholar]
- 66.Tasca G, Balfour L, Ritchie K, Bissada H (2007) Change in attachment anxiety is associated with improved depression among women with binge eating disorder. Psychother Theory Res Pract Train 44:423–433. 10.1037/0033-3204.44.4.423 [DOI] [PubMed] [Google Scholar]
- 67.Kinley JL, Reyno SM (2013) Attachment style changes following intensive short-term group psychotherapy. Int J Group Psychother 63:53–75 [DOI] [PubMed] [Google Scholar]
- 68.Mikulincer M, Gillath O, Halevy V et al. (2001) Attachment theory and reactions to others’ needs: evidence that activation of the sense of attachment security promotes empathic responses. J Pers Soc Psychol 81:1205–1224. 10.1037/0022-3514.81.6.1205 [DOI] [PubMed] [Google Scholar]
- 69.Reuben A, Moffitt TE, Caspi A et al. (2016) Lest we forget: comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. J Child Psychol Psychiatry Allied Discip 57:1103–1112. 10.1111/jcpp.12621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Unternaehrer E, Greenlaw K, Hari Dass S et al. (2017) Intergenerational transmission of well being—genetic and epigenetic mechanisms. Eur Psychiatry 41:S29–S30. 10.1016/j.eurpsy.2017.01.146 [DOI] [Google Scholar]
- 71.Hannigan LJ, Eilertsen EM, Gjerde LC et al. (2018) Maternal prenatal depressive symptoms and risk for early-life psychopathology in offspring: genetic analyses in the Norwegian Mother and Child Birth Cohort Study. Lancet Psychiatry 5:808–815. 10.1016/S2215-0366(18)30225-6 [DOI] [PubMed] [Google Scholar]
- 72.Shorey HS, Snyder CR (2006) The role of adult attachment styles in psychopathology and psychotherapy outcomes. Rev Gen Psychol 10:1–20. 10.1037/1089-2680.10.1.1 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.