Abstract
Background
A variety of state-level restrictions were placed on abortion care in response to the COVID-19 pandemic, leading to drops in utilization and delays in time to abortion. Other pandemic-related factors also may have impacted receipt of abortion care, potentially exacerbating existing barriers to care. Massachusetts is an ideal setting to study the impact of these other pandemic-related factors on abortion care utilization because there was no wide-scale abortion policy change in response to the pandemic.
Objective
This study aimed to evaluate the impact of the COVID-19 pandemic on abortion care utilization and disparities in utilization by patient age in Massachusetts.
Study Design
Using the electronic medical records from all abortions that occurred at the Planned Parenthood League of Massachusetts from May 1, 2017 through December 31, 2020 (N=35,411), we performed time series modeling to estimate monthly changes in the number of abortions from the expected counts during the COVID-19 pandemic. We also assessed if legal minors (<18 years) experienced delays in time to abortion, based on gestational age at procedure, and whether minors were differentially impacted by the pandemic.
Results
There were 1725 less abortions than expected, corresponding to a 20% drop, from March 2020 to December 2020 (95% prediction interval, −2025 to −1394) with 888 less (20% reduction) abortions among adults, 792 (20% reduction) less among young adults, and 45 (27% reduction) among minors. Adults and young adults experienced significant reductions in the number of abortions beginning in March 2020, whereas decreases among minors did not begin until July 2020. The rate of abortions occurring ≥12 weeks gestational age was unchanged during the COVID-19 pandemic among minors (adjusted rate ratio, 0.92; 95% confidence interval, 0.55–1.51) and among adults (adjusted rate ratio, 0.92; 95% confidence interval, 0.78–1.09). Young adults had a lower rate of second trimester abortion during the pandemic (adjusted rate ratio, 0.79; 95% confidence interval, 0.66–0.95).
Conclusion
Despite uninterrupted abortion service provision, abortion care utilization decreased markedly in Massachusetts during the pandemic. There was no evidence of an increase in second trimester abortions in any age group. Further research is needed to determine if a decline in the pregnancy rate or other factors, such as financial and travel barriers, fear of infection, or privacy concerns, may have contributed to this decline.
Key words: abortion access, abortion care, COVID-19, health disparities, health service utilization
Introduction
Noting that service disruptions can have life-altering consequences for individuals, leading clinical organizations in the United States quickly affirmed that abortion is an essential health service that should continue uninterrupted during the COVID-19 pandemic.1 , 2 Despite this clinical and public health consensus, 11 US states classified abortions as nonessential care during the early pandemic, curtailing provision during the state of public health emergency.3 For example, Texas Governor Greg Abbott ordered a stop to abortion procedures for 30 days beginning on March 22, 2020, as part of a broader order to conserve healthcare resources during an anticipated surge of illness and hospitalizations related to the pandemic.4 Given the time-sensitive nature of abortion care, these COVID-19 era bans could significantly impact population health by leading to delays in accessing, or outright denial of, abortion care.5 However, the overall impact of the pandemic on abortion care access outside of such bans has not yet been explored in the research literature.
AJOG at a Glance.
Why was this study conducted?
This study aimed to assess the impact of the COVID-19 pandemic on abortion care utilization in the absence of state-level restrictions and to investigate disparities in abortion care utilization and delays in receipt of abortion care by patient age.
Key findings
Abortion care utilization decreased by 20% in Massachusetts during the first 10 months of the COVID-19 pandemic (March 2020–December 2020). For minors, the decline in abortion care utilization began in July 2020, whereas it began immediately among young adults and adults in March 2020. There was no evidence of an increase in second trimester abortions across any age group. The proportion of second trimester abortions dropped among young adults during the first 10 months of the pandemic.
What does this add to what is known?
This study investigated abortion care utilization in the absence of state-level restrictions on abortion care in Massachusetts. Abortion care utilization was hypothesized to drop during the COVID-19 pandemic, which was confirmed by this study.
In addition to direct restrictions placed on abortion care, other pandemic-related factors may have affected access. Stay-at-home orders may have complicated travel to a clinic, especially among individuals requiring childcare. The risk for SARS-CoV-2 exposure may have discouraged some individuals from seeking any medical care, including for abortions, especially among those whose household members have preexisting health conditions that increase their risk for severe COVID-19 disease.6 , 7 These factors further compounded the limitations on abortion access for individuals living in US states that had abortion restrictions in place before the pandemic, such as mandatory waiting periods and parental involvement laws, which place substantial burdens on patients at baseline.8 , 9 These burdens are not equally distributed; thus, disproportionately affecting individuals who identify as people of color and legal minors in the United States.10
In 38 states, parental involvement in a minor’s decision to have an abortion is required, and several studies have demonstrated that these laws cause delays in accessing abortion care, although the effects vary across states.11, 12, 13, 14 From 1981 through 2020, Massachusetts’ parental consent law required that minors <18 years of age either obtain parental consent for abortion care or bypass the requirement via a hearing with a superior court judge.15 , 16 During the COVID-19 public health emergency, some superior court hearings in Massachusetts, including judicial bypass, were permitted to occur remotely for the first time.17 Although this practice avoids unnecessarily exposing young people, attorneys, and court staff to the risk of viral transmission, it may lead to additional privacy concerns for young people, particularly for those engaged in remote schooling with parents working from home (70% in April 202018) or with parents who are unemployed (15% in April 202019).
The goal of the present analysis was to assess the impact of the prevaccination phase of the COVID-19 pandemic on abortion rates in the Commonwealth of Massachusetts and to evaluate if there were disparities according to patient age. Although state and national governments enacted a wide variety of restrictions and supports for abortion access during the early pandemic, relevant policies and healthcare infrastructure did not change in Massachusetts.17 , 20 The state’s stay-at-home orders always allowed travel for healthcare and essential services, public transportation never fully closed (although service was reduced), and abortion services were explicitly characterized as essential by the state. At the same time, abortion providers could not mail mifepristone because of federal restrictions in the United States.21 Therefore, there was no rapid expansion in nor restriction on abortion access in the state other than the effects of COVID-19 on patients’ own life circumstances, fertility, and ability to access care. The state of Massachusetts therefore served as a useful case to quantify the impact of the pandemic per se on abortion rates in the absence of wide-scale policy change.
In the present analysis, we quantified changes in the number of abortions in comparison with what was expected based on time trends from previous years during the first 10 months of the COVID-19 pandemic, overall and by age group. Second, as a surrogate for abortion access, we evaluated whether the gestational age at presentation for abortion changed during the COVID-19 pandemic and assessed if legal minors (<18 years) experienced a greater delay than young adults and adults. We hypothesized that the COVID-19 pandemic would lead to fewer abortions and later average gestational age at abortion in all age groups. We expected these impacts to be more pronounced among minors who face additional barriers to care at baseline.
Materials and Methods
We extracted information on all abortions that occurred at Planned Parenthood of Massachusetts (PPLM) clinics between May 1, 2017 through December 31, 2020, from the electronic medical records (EMRs) (N=35,411). This gave a final sample size of 30,020 individuals because some patients received multiple abortions during the study period. We included both medication and surgical abortions. All study procedures were approved by the Partners Human Research Committee (institutional review board).
We collected the following variables for each abortion: patient age, insurance status, patient race and ethnicity (self-reported), date of abortion, and gestational age at abortion estimated using ultrasound. Gestational age was reported categorically as 8 weeks and then in increasing increments of 1 week. For these patient covariates, we operationalized age categorically with 3 distinct groups, namely minors (<18 years of age), young adults (18–26 years of age), and adults (≥27 years of age). The distinction between young adults and adults reflects potential differences in care seeking because of the Affordable Care Act, which allows individuals to remain covered by their parents’ commercial insurance through the age of 26 years. Insurance status refers to the insurance type that was used on the date of service, coded as private, public, self-pay, or private charitable fund. Based on the available responses in the EMRs, race and ethnicity were combined into the following 6 categories: (1) Hispanic (including Latino, Latina, and Latinx), (2) non-Hispanic White, (3) non-Hispanic Black (Black, African American, or African), (4) non-Hispanic Asian or Asian Indian, (5) non-Hispanic other (American Indian, Alaska Native, Native Hawaiian, Pacific Islander, or other), or (6) declined to answer or missing.
We reported all patient characteristics by time epoch to assess differences before and during the COVID-19 pandemic using chi-squared tests. The time epochs comprised abortions between March 16 through December 31 in 2018, 2019, and 2020, respectively. This date range was chosen because the Massachusetts’ Governor enacted a series of interventions to slow the spread of COVID-19 on March 15, 2020,17 and Monday, March 16, 2020, was the day PPLM implemented clinical changes in response to COVID-19.
In the primary analysis, time series modeling was used to quantify changes in the monthly count of abortions during the COVID-19 period for each age group. The goal of this analysis was to describe any changes in the abortion rate attributable to the COVID-19 pandemic by age group. Baseline data from the pre–COVID-19 period (May 1, 2017 to February 29, 2020) was used to estimate the expected number of abortions during each month of the COVID-19 period (March 1, 2020 to December 31, 2020). Note that for the analysis, abortions were categorized at the monthly level to avoid moving holidays that lead to multiday closings in some years and not others and therefore the COVID-19 period was indicated to start on March 1, 2020.22 We modeled the monthly counts () using a generalized linear model with log link and Poisson distribution. We included a term for the month to capture trend (t), a term for the number of days clinics were open for month t (), and Fourier terms to capture seasonality:
| (Eq.1) |
To flexibly model time trends and seasonality, we fit the model separately for each age group. We reported the deviation between the expected and observed counts for each month with 95% prediction intervals (PIs), calculated using a parametric bootstrap procedure. These statistical methods were employed during the COVID-19 pandemic and are described in greater detail to perform syndromic surveillance23 and estimate excess deaths.24 Finally, we performed several model checking procedures to assess the validity of the modeling assumptions in the age group time series models.
To formally compare abortion utilization by age group, we modified the Poisson regression model (Eq. 1) to include the entire time range with additional terms for age group, COVID-19 period (before vs during pandemic), and an interaction between age group and COVID-19 period. We also adjusted for the monthly distribution of race and ethnicity and insurance status because these variables are associated with abortion utilization and delay and may have impacted who received an abortion during the early COVID-19 pandemic.25 , 26
The secondary analysis investigated if the COVID-19 pandemic was associated with delays in the time to abortion and if minors were differentially impacted when compared with young adults and adults. We first assessed if the distribution of gestational age at abortion changed during the pandemic among minors using a Kruskal-Wallis test. To assess the differential impact among minors, we modeled the monthly number of abortions occurring at or after 12 weeks’ gestation using the same Poisson regression model described above with the addition of an offset term for the number of monthly abortions. All data cleaning and analyses were conducted in R V3.6.0 (The R Foundation, Vienna, Austria).
Results
Over the period of March 15 to December 31 for each year, the total number of abortions at PPLM declined from 7936 in 2018 and 7958 in 2019 to 6388 in 2020 (Table 1 ). However, there was no difference in the distribution of patient age groups by year. The proportion of abortions taking place at ≥12 weeks of gestational age was lower during the pandemic in 2020 (7.3%) than in 2019 (8.3%) and 2018 (8.7%) (P=.008). There were differences in the distribution of race and ethnicity between 2020 and the previous time epochs (P<.001). During the COVID-19 period, 18.5% of individuals declined to provide or had missing race and ethnicity data compared with 8.3% in 2019 and 9.4% in 2018. There was a steady increase in the use of public insurance (19.1% to 21.4%) and a decrease in self-paid procedures (18.4% to 15.7%) over the 3 year study period (P<.001).
Table 1.
Patient characteristics for March 15 through December 31 time periods
| Characteristics | Before COVID-19 (March–Dec. 2018) (n=7936) |
Before COVID-19 (March–Dec. 2019) (n=7958) |
During COVID-19 (March–Dec. 2020) (n=6388) |
P value |
|---|---|---|---|---|
| Patient age group | .581 | |||
| Minor (<18 y) | 150 (1.9) | 149 (1.9) | 112 (1.8) | |
| Young adult (18–26 y) | 3739 (47.1) | 3698 (46.5) | 2931 (45.9) | |
| Adult (27+ y) | 4047 (51.0) | 4111 (51.7) | 3345 (52.4) | |
| ≥8 wk at procedure | 2831 (35.7) | 2646 (33.2) | 2235 (35.0) | .004 |
| ≥12 wk at procedure | 692 (8.7) | 663 (8.3) | 467 (7.3) | .008 |
| Patient race and ethnicity | <.001 | |||
| Hispanic | 1641 (20.7) | 1803 (22.7) | 1432 (22.4) | |
| Non-Hispanic White | 3418 (43.1) | 3340 (42.0) | 2361 (37.0) | |
| Non-Hispanic Black | 1237 (15.6) | 1294 (16.3) | 904 (14.2) | |
| Non-Hispanic Asian or Asian Indian | 486 (6.1) | 464 (5.8) | 247 (3.9) | |
| Non-Hispanic other | 406 (5.1) | 447 (5.0) | 262 (4.1) | |
| Declined to answer or missing | 748 (9.4) | 661 (8.3) | 1182 (18.5) | |
| Insurance typea | <.001 | |||
| Abortion fund | 182 (2.3) | 272 (3.4) | 199 (3.1) | |
| Private | 4774 (60.2) | 4774 (60.0) | 3818 (59.8) | |
| Public | 1519 (19.1) | 1604 (20.2) | 1365 (21.4) | |
| Self-pay | 1459 (18.4) | 1307 (16.4) | 1000 (15.7) | |
| Missing | 2 (0.0) | 1 (0.0) | 6 (0.1) |
Data are presented as number (percentage).
Fulcher et al. Abortion care utilization during COVID-19. Am J Obstet Gynecol 2022.
Excludes n=9 missing values from statistical test.
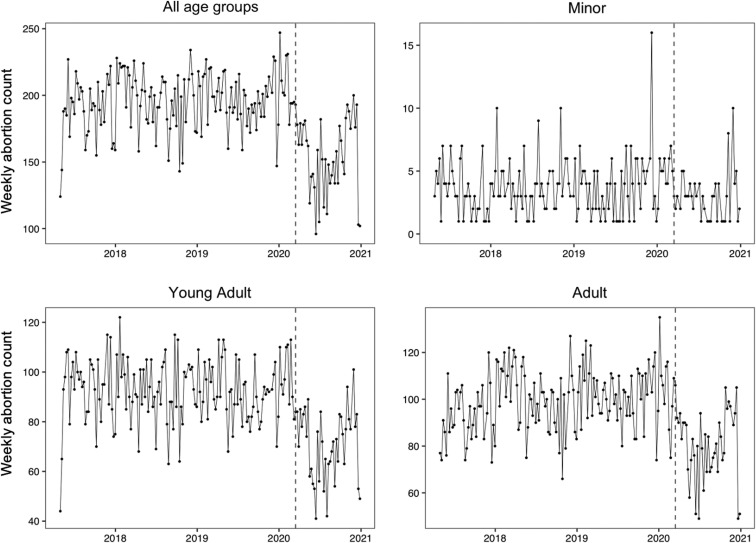
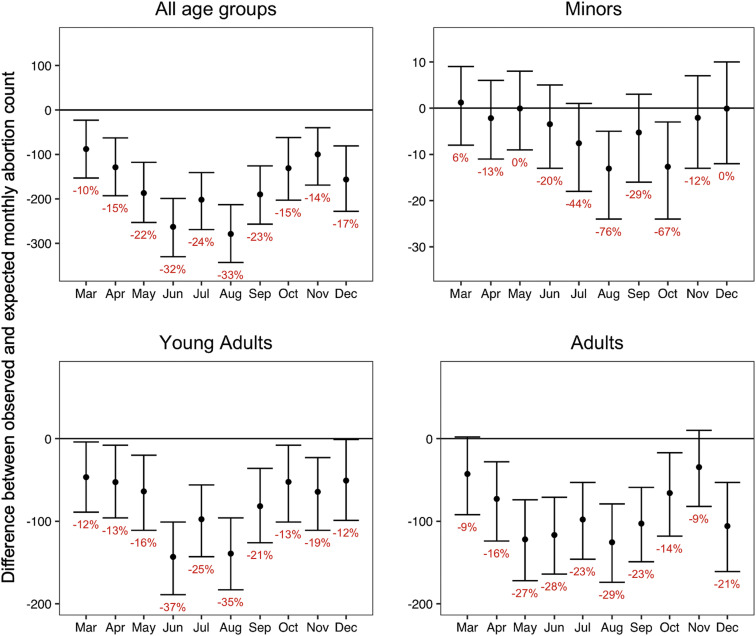
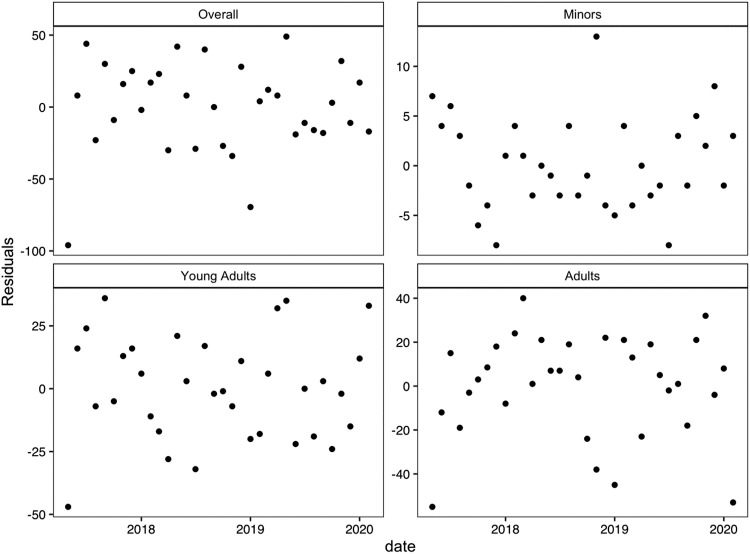
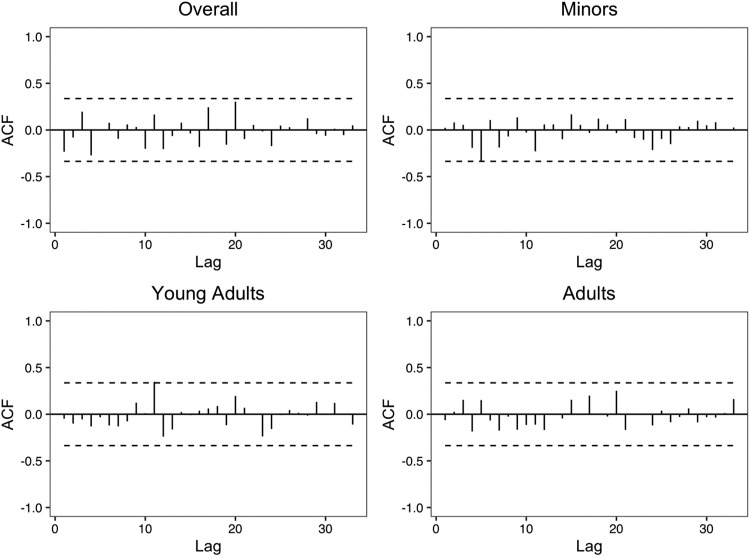
During the COVID-19 period, there was an estimated 20% drop in the number of abortions among all combined ages when compared with the expected number (95% PI, −23% to −17%) (Table 2 ). The number of abortions decreased abruptly after March 15, 2020, for adults and young adults. For minors, evidence of a decline began in July (−44%; 95% PI, −67% to 13%) with a significant drop in August (−77%; 95% PI, −86% to −56%) (Figure 1 ). Adults and young adults had a lower-than-expected number of abortions for all 10 months of the COVID-19-period. Among minors, the number of abortions was close to the expected number during the months of March through June, lower than expected in July through October, and returned to the expected number by November (Figure 2 ). For all age groups, the deviation in the number of abortions from the expected was largest in August 2020 and began to rebound toward expected thereafter. We found no evidence of overdispersion (Appendix A) or autocorrelation (Supplemental Figures 1 and 2) in these models. After adjusting for race and ethnicity and insurance status in the Poisson regression model, there were no significant differences in the deviations over the COVID-19 period between the age groups (Table 3 ; Supplemental Table 1).
Table 2.
Cumulative deviation and percentage by age group with 95% prediction intervals (March 1, 2020 through December 31, 2020)
| Age group | Total deviation | Percentage change |
|---|---|---|
| Overall n=22,282 | −1725 (−2025 to −1394) | −20% (−23% to −17%) |
| Minors (<18 y) n=411 | −45 (−93 to −3) | −27% (−43% to −2%) |
| Young adults (18–26 y) n=10,368 | −792 (−1009 to −583) | −20% (−25% to −16%) |
| Adults (≥27 y) n=11,503 | −888 (−1113 to −666) | −20% (−24% to −16%) |
Fulcher et al. Abortion care utilization during COVID-19. Am J Obstet Gynecol 2022.
Figure 1.
Weekly number of abortions from May 1, 2017 to December 31, 2020
Fulcher et al. Abortion care utilization during COVID-19. Am J Obstet Gynecol 2022.
Figure 2.
Monthly deviation in number of abortions with 95% prediction intervals
Percentage change from expected in red text (March 1, 2020 to December 31, 2020).
Fulcher et al. Abortion care utilization during COVID-19. Am J Obstet Gynecol 2022.
Supplemental Figure 1.
Scatterplot of residuals for each age group model
Fulcher et al. Abortion care utilization during COVID-19. Am J Obstet Gynecol 2022.
Supplemental Figure 2.
Autocorrelation function plot for each age group model
Fulcher et al. Abortion care utilization during COVID-19. Am J Obstet Gynecol 2022.
Table 3.
Poisson regression models to estimate impact of COVID-19 on abortion utilizationa and delayb by age group with adjustment for seasonality, monthly trends, race and ethnicity, and insurance status (May 1, 2017–December 1, 2020; N=35,411)
| Model | Adjusted rate ratiod | 95% confidence interval | P valuec |
|---|---|---|---|
| Abortion utilization | |||
| Minors | 0.78 | (0.64–0.96) | — |
| Young adults | 0.77 | (0.73–0.81) | .880 |
| Adults | 0.82 | (0.79–0.86) | .635 |
| Abortion occurring at or after 12 wk | |||
| Minors | 0.92 | (0.55–1.55) | — |
| Young adults | 0.79 | (0.66–0.95) | .584 |
| Adults | 0.92 | (0.78–1.09) | .992 |
Fulcher et al. Abortion care utilization during COVID-19. Am J Obstet Gynecol 2022.
Full utilization model results are presented in Supplemental Table 1
Full delay model results are presented in Supplemental Table 2
Hypothesis test of interaction terms to assess differential impact of COVID-19 among minors
Effect estimate comparing COVID-19 to pre-COVID-19 period.
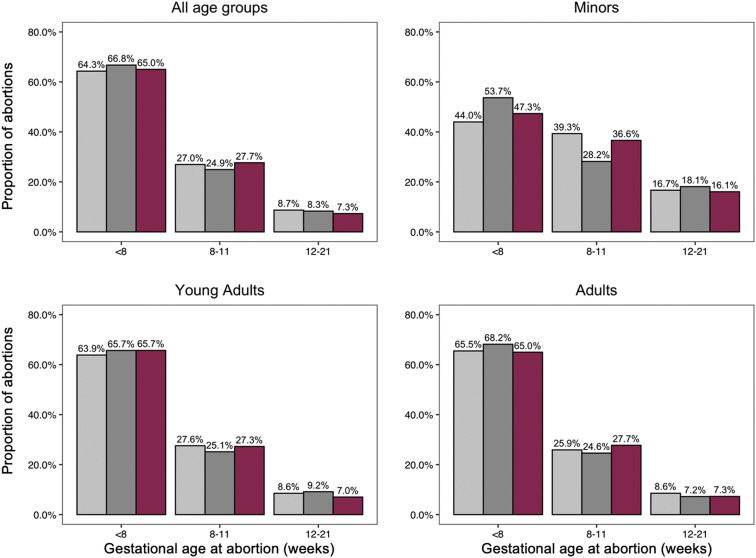
Regardless of time epoch, young adults underwent abortions at an earlier gestational age than minors. The distribution of gestational age by week at the procedure did not differ substantially during the COVID-19 pandemic when compared with the prepandemic period among minors (P=.413) (Figure 3 ). In 2019, 9.2% of young adults compared with 18.1% of minors had an abortion at or after 12 weeks’ gestational age. This relationship persisted during the COVID-19 pandemic with 7.0% of young adults undergoing an abortion at or after 12 weeks when compared with 16.1% of minors.
Figure 3.
Gestational age at abortion by time epoch and age group (March 15–December 31)
Light gray indicates data for 2018, dark gray indicates data for 2019, and red indicates data for 2020.
Fulcher et al. Abortion care utilization during COVID-19. Am J Obstet Gynecol 2022.
In the model for abortion delay, we found no change in the rate of undergoing an abortion procedure at or after 12 weeks among adults and minors during the COVID-19 pandemic (Table 3), although the confidence interval for minors was wide (adjusted rate ratio [RR], 0.92; 95% confidence interval [CI], 0.55–1.55). However, young adults had a lower rate of abortion procedure at or after 12 weeks during the pandemic than before the pandemic (RR, 0.79; 95% CI, 0.66–0.95). Minors had a higher rate of later abortions compared to young adults and adults in all time periods (Supplemental Table 2); the relationship between age and gestational age remained unchanged during the COVID-19 pandemic (P=.584 for minors v. young adults; P=.992 for minors v. adults) (Table 3). In Supplemental Table 3, we provide an alternate, individual-level analysis using a logistic regression model and found similar results.
Comment
Principal findings
Massachusetts had minimal service disruptions and no major policy changes related to abortion access during the prevaccination phase of the COVID-19 pandemic, but the number of abortions dropped dramatically for all age groups in the spring and summer of 2020. Despite drops in abortion care utilization across all age groups, we found that the proportion of abortions occurring during the second trimester was unchanged among minors and adults, whereas it decreased for young adults.
Results in the context of what is known
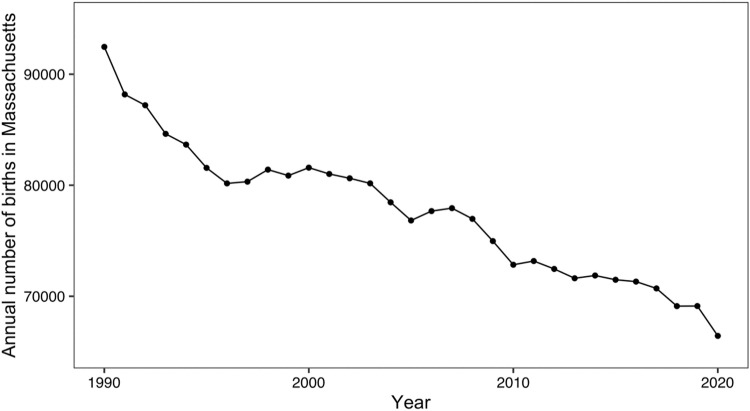
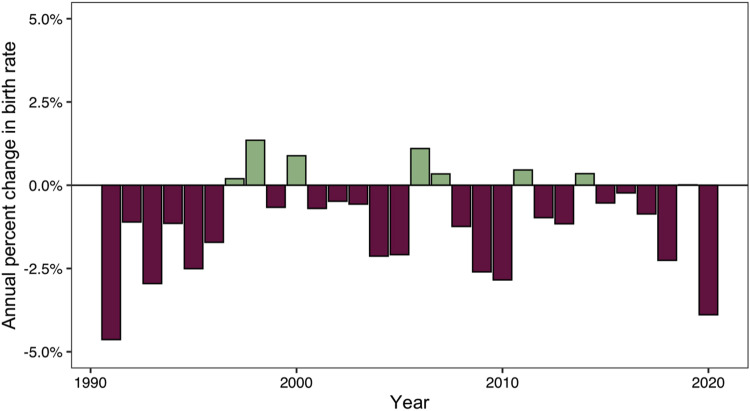
A decrease in conceptions because of decreased sexual activity following the issuing of national and state emergencies in mid-March 2020 could explain some of the decline in abortion rates. Pregnancy and birth data for the state of Massachusetts for the 2021 calendar year have not been published yet. However, Massachusetts experienced a decline in births in the first year of the pandemic. The overall number of births in Massachusetts declined by 3.89% from 69,117 in 2019 to 66,429 in 2020 (Supplemental Figures 3 and 4), the second largest yearly drop observed since 1990.27 Moreover, national monthly statistics revealed that the birth rate dropped by 7.66% in December 2020 (vs December 2019) and by 9.41% in January 2021 (vs January 2020), potentially reflecting fewer conceptions at the national level during the early COVID-19 pandemic.28
Supplemental Figure 3.
Annual number of births in Massachusetts from 1990 to 2020
Fulcher et al. Abortion care utilization during COVID-19. Am J Obstet Gynecol 2022.
Supplemental Figure 4.
Annual percentage change in number of births in Massachusetts from 1990 to 2020
All data can be found in Massachusetts state-level birth reports for 1990 to 2017 at https://www.mass.gov/lists/birth-data. Reports for the remaining years can be found at https://www.cdc.gov/nchs/data/nvsr/nvsr70/nvsr70-02-508.pdf (2019), https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_13-508.pdf (2018), and https://www.cdc.gov/nchs/data/vsrr/vsrr012-508.pdf (2020).
Fulcher et al. Abortion care utilization during COVID-19. Am J Obstet Gynecol 2022.
The number of abortions among young adults and adults dropped as early as March 2020, which cannot be attributed to a decline in pregnancy rate following the Massachusetts Governor’s orders on March 15, 2020. It is possible that sexual activity among adults and young adults started declining before the Governor’s orders as awareness of the emerging global pandemic spread in January and February 2020. Conversely, the apparent rebound in the number of abortions after August 2020 may be partially because of gradual reductions in COVID-19 restrictions in the summer months. The Massachusetts Governor’s orders introduced a phased reopening of businesses and social gatherings beginning on May 18, 2020, potentially leading to a rebound in the pregnancy rate.29 This is also corroborated by the rebound in the national birth rate after February 2021.28
Notably, the declines in pregnancy and birth rates from these published reports are smaller than what was observed in our study, which could be caused by (1) individuals shifting abortion care from PPLM clinics to other providers, (2) individuals choosing to continue their pregnancies, or (3) individuals being unable to obtain an abortion. However, it is unlikely that people sought care outside of PPLM clinics at a higher rate during the pandemic because the clinics had no interruption in abortion care during the pandemic and did not need to shift any resources to care for patients with COVID-19.30 There is also no evidence that people chose to continue pregnancies at a higher rate during the pandemic; in fact, a national survey indicated a precipitous drop in the proportion of pregnancy-capable individuals desiring a birth during the pandemic.31 Of these options, the most likely explanation may be that more individuals were unable to obtain a wanted abortion because of financial barriers, fear of infection, increased life chaos, childcare responsibilities, and increases in intimate partner violence—all phenomena that have been documented worldwide during the pandemic.32 , 33
Researchers hypothesized that delays in abortion care would occur during the pandemic,34 especially among minors because previous studies have shown later gestational ages at the abortion procedure for minors when compared with adults.35 , 36 Our findings align with these previous studies because minors were more likely to have a second trimester abortion than young adults and adults in all time periods. However, we did not find evidence of a delay in time to abortion among minors during the pandemic.
Clinical implications
The decrease in abortions during the second trimester observed among young adults and no change among minors and adults could be because of widespread societal closures of workplaces and schools, allowing individuals to obtain abortion care quickly precisely because they did not require time off from these other obligations to seek care. Because these findings were coupled with a decline in abortion care utilization, further research is needed to understand whether this was a result of faster access to abortion care once pregnant or an increase in the frequency of individuals continuing undesired pregnancies.
In December 2021, the US Food and Drug Administration announced that the prohibition on mailing the abortifacient drug mifepristone directly to patients is permanently lifted. Moving forward, expanded access to telemedicine abortion could increase access to abortion and further reduce second trimester abortion rates. As much of the United States returns to prepandemic levels of social interaction, sexual activity may also increase. It is imperative in this context that individuals can access essential sexual and reproductive healthcare, including contraception for those wishing to prevent pregnancy, and have continued access to abortion for individuals in need.
Research implications
Future research should explore how much of the decline in abortion rates during the early pandemic can be attributed to fewer pregnancies when compared with other factors, such as travel barriers, fear of infection, or privacy concerns. Data on birth rates in the early months of 2021 will provide more information on whether a decline in pregnancy rates is responsible for the decline in abortions during these months. In addition, our data set did not specify which minors received judicial bypass (vs parental consent) for their abortion. Additional studies among minors seeking judicial bypass are crucial to explain how the pandemic, and specifically the option for virtual bypass hearings, impacted the timing and receipt of abortion care.
Strengths and limitations
Previous studies on abortion care utilization during the pandemic are limited to states that had abortion bans in response to COVID-19. This study investigated abortion utilization in a state where abortion was consistently considered an essential health service, allowing us to investigate the impact of the pandemic on patients’ own life circumstances, fertility, and ability to access care.
This study had several limitations. First, there were more missing race and ethnicity data during the pandemic, likely because this question was assessed during a telehealth visit by a provider (vs self-reported on a tablet by the patient). It is possible that the missing race determination was not random, thereby classifying some races as missing more often than others. Such misclassification of race would have masked true racial differences in outcomes across time epochs presented in Table 1. Furthermore, because of the large amount of missing data on race, it prevented us from replicating the age and COVID-19 period interaction analysis by race and ethnicity. Future studies could help to fill this gap. Health systems should work to ensure that race and ethnicity data in medical records are not lost during the pandemic to ensure that investigators can properly characterize the role of racism in driving COVID-19–related reproductive health disparities.37 , 38 Second, the number of abortions among minors is small (n=261), which may preclude detection of smaller but meaningful differences in procedural timing before vs during the COVID-19 pandemic when compared with older age groups. However, the main conclusion that minors experienced similar declines in the number of abortions than older age groups and were not more likely to have second trimester abortions during the pandemic is supported by the analytical findings.
Conclusions
Despite uninterrupted abortion service provision in the state of Massachusetts, abortion care utilization decreased markedly in the state during the pandemic. However, there was no evidence of an increase in second trimester abortions within any age group. To ensure timely access to abortion care during this and future pandemics, it is imperative to understand whether these declines are because of a decrease in the pregnancy rate or other factors.
Acknowledgments
We thank Timothy James McAndrew, BA, and Cindy Jewett, MSW for assisting with data abstraction. The findings and conclusions in this article are those of the authors and do not necessarily reflect the views of the Planned Parenthood Federation of America, Inc.
Footnotes
The authors report no conflict of interest.
This study did not receive any funding.
Cite this article as: Fulcher IR, Onwuzurike C, Goldberg AB, et al. The impact of the COVID-19 pandemic on abortion care utilization and disparities by age. Am J Obstet Gynecol 2022;226:819.e1-15.
Appendix A
Statistical tests
We performed a test of equidispersion in the Poisson model and found no evidence of overdispersion (all P values >.17). We also performed the Breusch-Godfrey test for autocorrelation in the residuals and found no evidence of autocorrelation (all P values >.23).
Residual plots
Residual and autocorrelation function plots for each model can be found below and reveal no evidence of autocorrelation.
Appendix B
Supplemental Table 1.
Poisson regression model to estimate rate of abortion by age group and time period (May 2017–December 2020; N=35,411)
| Group | Estimated log abortion rate ratios | Standard error | P value |
|---|---|---|---|
| Intercept | 1.746 | 0.119 | <.001 |
| COVID-19 period (reference: pre-March 2020) | −0.243 | 0.102 | .017 |
| Age group category (reference: minors) | |||
| Young adults | 3.216 | 0.062 | <.001 |
| Adults | 3.268 | 0.065 | <.001 |
| Interaction term COVID-19 period by age group |
|||
| Young adults | −0.016 | 0.104 | .880 |
| Adults | 0.049 | 0.103 | .635 |
| Race and ethnicitya | |||
| Hispanic | −0.029 | 0.011 | .010 |
| Non-Hispanic Asian or Asian Indian | −0.037 | 0.017 | .023 |
| Non-Hispanic Black | −0.023 | 0.008 | .005 |
| Non-Hispanic White | −0.008 | 0.003 | .008 |
| Insurance type categorya | |||
| Private | −0.009 | 0.024 | .698 |
| Public | −0.006 | 0.007 | .362 |
| Self-pay | −0.006 | 0.011 | .598 |
| Seasonality terms | |||
| cos1 | 0.010 | 0.009 | .260 |
| cos2 | −0.011 | 0.008 | .174 |
| sin1 | −0.055 | 0.008 | <.001 |
| sin2 | 0.006 | 0.008 | .431 |
| Number of days open per month | 0.046 | 0.005 | <.001 |
| Month number | 0.001 | 0.001 | .558 |
Fulcher et al. Abortion care utilization during COVID-19. Am J Obstet Gynecol 2022.
Adjusting for monthly distribution of demographic groups excluding unkown subgroups; subgroup proportions were centered and scaled with 1-unit increase corresponding to a 10% increase in subgroup proportion.
Supplemental Table 2.
Poisson regression model to estimate rate of abortion occurring at or after 12 weeks by age group and time period (May 2017–December 2020; N=35,411)
| Group | Estimated log rate ratios | Standard error | P value |
|---|---|---|---|
| Intercept | −2.038 | 0.401 | <.001 |
| COVID-19 period (reference: pre-March 2020) | −0.082 | 0.265 | .757 |
| Age group category (reference: minors) | |||
| Young adults | −0.631 | 0.177 | <.001 |
| Adults | −0.613 | 0.184 | .001 |
| Interaction term COVID-19 period by age group |
|||
| Young adults | −0.150 | 0.274 | .584 |
| Adults | −0.003 | 0.270 | .992 |
| Race and ethnicitya | |||
| Hispanic | −0.012 | 0.037 | .742 |
| Non-Hispanic Asian or Asian Indian | −0.046 | 0.053 | .389 |
| Non-Hispanic Black | −0.036 | 0.027 | .173 |
| Non-Hispanic White | −0.015 | 0.010 | .116 |
| Insurance type categorya | |||
| Private | −0.139 | 0.067 | .039 |
| Public | −0.016 | 0.019 | .404 |
| Self-pay | −0.060 | 0.031 | .050 |
| Seasonality terms | |||
| cos1 | 0.095 | 0.030 | .002 |
| cos2 | −0.058 | 0.027 | .036 |
| sin1 | 0.009 | 0.028 | .747 |
| sin2 | −0.054 | 0.028 | .050 |
| Number of days open per month | 0.011 | 0.017 | .521 |
| Month number | −0.002 | 0.002 | .457 |
Fulcher et al. Abortion care utilization during COVID-19. Am J Obstet Gynecol 2022.
Adjusting for monthly distribution of demographic groups excluding unknown subgroups; subgroup proportions were centered and scaled with 1-unit increase corresponding to a 10% increase in subgroup proportion.
Supplemental Table 3.
Alternate logistic regression model to estimate odds of abortion occurring at or after 12 weeks by age group and time period (n=14,339)
| Group | Estimated log odds ratiosa | Standard error | P value |
|---|---|---|---|
| Intercept | −1.034 | 0.255 | <.001 |
| COVID-19 period (reference: March 2019–Dec. 2019) | −0.211 | 0.351 | .547 |
| Age group category (reference: minor) | |||
| Young adult | −0.677 | 0.222 | .002 |
| Adult | −0.927 | 0.222 | <.001 |
| Interaction term COVID-19 period by age group |
|||
| Young adult | −0.110 | 0.364 | .763 |
| Adult | 0.179 | 0.362 | .622 |
| Race and ethnicity (reference: unknown) | |||
| Hispanic | −0.113 | 0.107 | .290 |
| Non-Hispanic Asian or Asian Indian | −0.246 | 0.177 | .166 |
| Non-Hispanic Black | −0.080 | 0.116 | .490 |
| Non-Hispanic White | −0.067 | 0.098 | .493 |
| Non-Hispanic other | −0.226 | 0.176 | .198 |
| Insurance type category (reference: abortion fund) | |||
| Private | −0.545 | 0.148 | <.001 |
| Public | −0.211 | 0.154 | .171 |
| Self-pay | −0.826 | 0.170 | <.001 |
Fulcher et al. Abortion care utilization during COVID-19. Am J Obstet Gynecol 2022.
Estimated with multivariate logistic regression with a binary outcome of an abortion occurring at or after 12 weeks’ gestation. Only abortions between March 15 and December 31 in 2019 and 2020 were included (n=14,436). The logistic model included terms for age group, time epoch (2020 vs 2019), and interaction terms between age group and time epoch. We also adjusted for race or ethnicity and insurance status. We excluded 7 abortions with missing values for insurance type for a final sample size of 14,339 abortions. We accounted for multiple abortions per person with generalized estimating equations using an exchangeable correlation structure.
Appendix C
References
- 1.Bayefsky M.J., Bartz D., Watson K.L. Abortion during the Covid-19 pandemic - ensuring access to an essential health service. N Engl J Med. 2020;382:e47. doi: 10.1056/NEJMp2008006. [DOI] [PubMed] [Google Scholar]
- 2.American College of Obstetricians and Gynecologists Joint statement on abortion access during the COVID-19 outbreak. 2020. https://www.acog.org/news/news-releases/2020/03/joint-statement-on-abortion-access-during-the-covid-19-outbreak Available at:
- 3.Jones R.K., Lindberg L., Witwer E. COVID-19 abortion bans and their implications for public health. Perspect Sex Reprod Health. 2020;52:65–68. doi: 10.1363/psrh.12139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.White K., Kumar B., Goyal V., Wallace R., Roberts S.C.M., Grossman D. Changes in abortion in Texas following an executive order ban during the coronavirus pandemic. JAMA. 2021;325:691–693. doi: 10.1001/jama.2020.24096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohen B., DS, Joffe C., Obstacle Course . University of California Press; Oakland, CA: 2020. The everyday struggle to get an abortion in America. [Google Scholar]
- 6.Zhou F., Yu T., Du R., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fulcher I.R., Neill S., Bharadwa S., Goldberg A.B., Janiak E. State and federal abortion restrictions increase risk of COVID-19 exposure by mandating unnecessary clinic visits. Contraception. 2020;102:385–391. doi: 10.1016/j.contraception.2020.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jerman J., Frohwirth L., Kavanaugh M.L., Blades N. Barriers to abortion care and their consequences for patients traveling for services: qualitative findings from two states. Perspect Sex Reprod Health. 2017;49:95–102. doi: 10.1363/psrh.12024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Joyce T., Kaestner R. The impact of mandatory waiting periods and parental consent laws on the timing of abortion and state of occurrence among adolescents in Mississippi and South Carolina. J Pol Anal Manage. 2001;20:263–282. [Google Scholar]
- 10.Dehlendorf C., Harris L.H., Weitz T.A. Disparities in abortion rates: a public health approach. Am J Public Health. 2013;103:1772–1779. doi: 10.2105/AJPH.2013.301339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guttmacher Institute Parental involvement in minors’ abortions. 2021. https://www.guttmacher.org/state-policy/explore/parental-involvement-minors-abortions Available at:
- 12.Janiak E., Fulcher I.R., Cottrill A.A., et al. Massachusetts’ parental consent law and procedural timing among adolescents undergoing abortion. Obstet Gynecol. 2019;133:978–986. doi: 10.1097/AOG.0000000000003190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Joyce T. Parental consent for abortion and the judicial bypass option in Arkansas: effects and correlates. Perspect Sex Reprod Health. 2010;42:168–175. doi: 10.1363/4216810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Altindag O., Joyce T. Judicial bypass for minors seeking abortions in Arkansas versus other states. Am J Public Health. 2017;107:1266–1271. doi: 10.2105/AJPH.2017.303822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bellotti vs Baird, 443 U.S. 622; 1979. Available at: https://tile.loc.gov/storage-services/service/ll/usrep/usrep443/usrep443622/usrep443622.pdf. Accessed June 2, 2021.
- 16.NARAL Pro-Choice Massachusetts ROE act coalition celebrates passage of abortion access legislation. 2020. https://prochoicemass.org/2020/12/29/roe-act-coalition-celebrates-passage-abortion-access-legislation/ Available at:
- 17.Commonwealth of Massachusetts Order prohibiting gatherings of more than 25 people and on-premises consumption of food or drink. 2020. https://www.mass.gov/doc/march-15-2020-large-gatherings-25-and-restaurants-order/download Available at:
- 18.Poll L.A. Americans like working at home. 2021. https://www.usnews.com/news/national-news/articles/2021-02-12/majority-of-americans-work-remotely-a-year-into-coronavirus-pandemic-poll-finds Available at:
- 19.Congressional Research Service Unemployment rates during the COVID-19 pandemic. 2021. https://fas.org/sgp/crs/misc/R46554.pdf Available at:
- 20.Commonwealth of Massachusetts Order temporarily closing all public and private elementary and secondary schools. 2020. https://www.mass.gov/doc/march-15-2020-school-closure-order/download Available at:
- 21.United States Food & Drug Administration Approved risk evaluation and mitigation strategies (REMS) 2020. https://www.accessdata.fda.gov/scripts/cder/rems/index.cfm?event=RemsDetails.page&REMS=390 Available at:
- 22.Hyndman RJ, Athanasopoulos G. Forecasting: principles and practice. 2018. Available at: https://otexts.com/fpp2/. Accessed March 1, 2021.
- 23.Fulcher I.R., Boley E.J., Gopaluni A., et al. Syndromic surveillance using monthly aggregate health systems information data: methods with application to COVID-19 in Liberia. Int J Epidemiol. 2021;50:1091–1102. doi: 10.1093/ije/dyab094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weinberger D.M., Chen J., Cohen T., et al. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Intern Med. 2020;180:1336–1344. doi: 10.1001/jamainternmed.2020.3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Janiak E., Kawachi I., Goldberg A., Gottlieb B. Abortion barriers and perceptions of gestational age among women seeking abortion care in the latter half of the second trimester. Contraception. 2014;89:322–327. doi: 10.1016/j.contraception.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 26.Drey E.A., Foster D.G., Jackson R.A., Lee S.J., Cardenas L.H., Darney P.D. Risk factors associated with presenting for abortion in the second trimester. Obstet Gynecol. 2006;107:128–135. doi: 10.1097/01.AOG.0000189095.32382.d0. [DOI] [PubMed] [Google Scholar]
- 27.Hamilton B.E., Martin J.A., Osterman M.J.K. Births: provisional data for 2020. National Vital Statistics System. 2021. https://www.cdc.gov/nchs/data/vsrr/vsrr012-508.pdf Available at: [PubMed]
- 28.Morse A. Fewer babies born in December and January but number started to rise in March. United States Census Bureau. 2021. https://www.census.gov/library/stories/2021/09/united-states-births-declined-during-the-pandemic.html Available at:
- 29.Commonwealth of Massachusetts Reopening protocols & business restrictions (archive) 2022. https://www.mass.gov/info-details/covid-19-state-of-emergency#reopening-protocols-&-business-restrictions-(archive)- Available at:
- 30.Solis S. Coronavirus response: hospitals must cancel colonoscopies, knee replacements; abortions can continue as scheduled. 2020. https://www.masslive.com/coronavirus/2020/03/coronavirus-response-hospitals-must-cancel-colonoscopies-knee-replacements-abortions-can-continue-as-scheduled.html Available at:
- 31.Lindberg L.D., VandeVusse A., Mueller J., Kirstein M. Guttmacher Institute; 2020. Early impacts of the COVID-19 pandemic: findings from the 2020 Guttmacher survey of reproductive health experiences.https://www.guttmacher.org/report/early-impacts-covid-19-pandemic-findings-2020-guttmacher-survey-reproductive-health Available at: [Google Scholar]
- 32.Gosangi B., Park H., Thomas R., et al. Exacerbation of physical intimate partner violence during COVID-19 pandemic. Radiology. 2021;298:E38–E45. doi: 10.1148/radiol.2020202866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hamadani J.D., Hasan M.I., Baldi A.J., et al. Immediate impact of stay-at-home orders to control COVID-19 transmission on socioeconomic conditions, food insecurity, mental health, and intimate partner violence in Bangladeshi women and their families: an interrupted time series. Lancet Glob Health. 2020;8:e1380–e1389. doi: 10.1016/S2214-109X(20)30366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ruggiero S., Brandi K., Mark A., et al. Access to later abortion in the United States during COVID-19: challenges and recommendations from providers, advocates, and researchers. Sex Reprod Health Matters. 2020;28:1774185. doi: 10.1080/26410397.2020.1774185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rogers J.L., Boruch R.F., Stoms G.B., DeMoya D. Impact of the Minnesota Parental Notification Law on abortion and birth. Am J Public Health. 1991;81:294–298. doi: 10.2105/ajph.81.3.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ellertson C. Mandatory parental involvement in minors’ abortions: effects of the laws in Minnesota, Missouri, and Indiana. Am J Public Health. 1997;87:1367–1374. doi: 10.2105/ajph.87.8.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Onwuzurike C., Diouf K., Meadows A.R., Nour N.M. Racial and ethnic disparities in severity of COVID-19 disease in pregnancy in the United States. Int J Gynaecol Obstet. 2020;151:293–295. doi: 10.1002/ijgo.13333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goldfarb I.T., Clapp M.A., Soffer M.D., et al. Prevalence and severity of coronavirus disease 2019 (COVID-19) illness in symptomatic pregnant and postpartum women stratified by Hispanic ethnicity. Obstet Gynecol. 2020;136:300–302. doi: 10.1097/AOG.0000000000004005. [DOI] [PMC free article] [PubMed] [Google Scholar]