Abstract
BACKGROUND:
Much research has found that smoking is one of the major risk factors for a variety of physical diseases and mental disorders; however, few studies have been conducted on smoking in Egypt. Furthermore, to the researcher's best knowledge, no study in Egypt has compiled data on smoking prevalence, motives, and levels of nicotine dependency. In order to fill in this gap, the current study has attempted to summarize the situation and construct an accurate picture of smoking in Egypt.
MATERIALS AND METHODS:
This cross-sectional study included 2000 Egyptian adults in Fayoum through a multistage cluster sampling technique. For data collection, the Socioeconomic Status Scale was deployed. In addition, Depression, Anxiety, Stress Scale (DASS), the Modified Reasons for Smoking Scale (MRSS), and Fagerstrom Test for Nicotine Dependence (FTND) were used. Data analysis performed using SPSS version 22.0. For qualitative data, Chi-square test was used to determine statistical significance. Bivariate Pearson correlation was used to test for the association between quantitative variables.
RESULTS:
Of the total sample of 2000 adults, 40.4% had anxiety and 24.3% had stress, and 19.5% showed severe to extremely severe level of depression. For MRSS, tension reduction or relaxation was found in 46.5% adults while 9.8% had high level of nicotine dependence. There was a statistically significant association between psychometric disorders, on one hand, and both smoking motivation and nicotine dependence, on the other (P < 0.001). The DASS score had a statistically significant correlation with age, smoking duration, nicotine dependence level, and MRSS subscales.
CONCLUSION:
Smoking is linked to psychological symptoms and shows a moderate to high level of nicotine dependence, with a higher level of dependency, smoking pleasure, stress reduction/ relaxation, and hand-mouth movement as motives for smoking. Furthermore, there was a correlation between nicotine dependence, on one hand, and depression and stress on the other.
Keywords: Depression, nicotine, smoking
Introduction
Smoking is known as a chronic nicotine dependence disorder that is considered as a major risk factor for a variety of diseases and disabilities affecting physical health of all body organs as well as mental health.[1,2] Tobacco was responsible for more than 7 million deaths worldwide in 2017.[3] If the current smoking patterns continue, the number of deaths by tobacco related diseases will have reached more than 8 million deaths by 2030. In other words, for every person who dies of smoking, at least 30 others live with a serious disease related to smoking.[4] According to World Health Organization's (WHO) reports, smoking has become more common in many developing countries, including Egypt.[5]
Anxiety, depression, bipolar disorder, and schizophrenia are examples of mental disorders that affect an individual's thought, mood, emotion, and behavior. Several studies have stressed that substantial impairment of health, disability, and inability to perform major tasks are the results of long-term use of alcohol, drugs, and tobacco. Approximately, one out of every four adults suffers from mental illness in the United States (US) and about 40% of adults smoke cigarettes.[6] The majority of psychiatric disorders have been linked to cigarette smoking. Cigarette smoking has been associated with an elevated risk of psychiatric disorders.[7]
From another perspective, nicotine dependence has proven to be difficult, especially, for people with psychiatric disorders since nicotine has mood-altering effects that can partially mask the negative symptoms of mental health issues. It induces a sense of relaxation, misleading users to believe that it decreases stress and anxiety.[8] It was found that smoking rates among people with those disorders are significantly higher than in the general population; i.e., it is 2-5 times higher in patients with multiple disorders such as schizophrenia, mood disorders, binge eating disorders, attention deficit and hyperactivity disorder, bulimia, and substance use disorders.[9]
Some studies have found that smoking and depression have a complicated relationship because nicotine causes the release of the chemical substance dopamine (the brain's positive trigger). From another angle, since depressive patients' dopamine levels are low, they rely on cigarettes to boost their dopamine levels to feel better. Furthermore, smoking has dopamine-producing mechanism effect in the brain, resulting in a decrease in dopamine supply and thus prompting people to smoke more.[1]
Similarly, depression, anxiety, and emotional disorders have been found to increase the risk of smoking experiments, frequent smoking, and nicotine dependence. They also lead to maladaptive cognitive and emotional responses to tobacco.[10] Evidence suggests that clinicians' lack of active involvement in urging smokers to quit may be due to their belief that depressed smokers are not motivated to quit, thinking that smoking is a form of self-medication and that quitting would exacerbate depression symptoms.[11] In other words, high levels of depression, anxiety, and stress in addition to low motivation for change are the main obstacles to the failure of smoking cessation programs.[12]
A review of the literature has revealed a high failure rate in smoking cessation.[12] In order to contribute to successful smoking cessation, high motivation and multiple quitting attempts are required.[13] Quitting the use of tobacco requires special attention. For instance, the offer of quit-smoking assistance, which is the focus of the WHO's seventh report on the global tobacco epidemic, is an important part of any tobacco-control plan. Current tobacco users will quit if the global targets for lowering tobacco use are met. For instance, WHO monitors the implementation of the six MPOWER tobacco-reduction measures and encourages nations to adopt them.[13]
Owing to the significance of smoking and the resultant diseases and psychological disorders, the low rate of success of smoking cessation programs, and the lack of research in these areas in Egypt, the current study attempts to address these research gaps by determining the association between psychometric disorders (depression, anxiety, and stress) and each of smoking motivations and levels of nicotine dependence in the study group to improve the success rate of cessation programs.
Materials and Methods
This is a cross-sectional descriptive study of Al-Fayoum governorate population, Egypt. The multistage cluster sampling used in the study was carried out in four stages. The first stage was a cluster random sample of six governorate districts from which three were chosen. In the second stage, four primary healthcare facilities were chosen in each district. The third stage was to select one population block in each primary healthcare facility catchment area. In each population block, a street was randomly selected for the fourth stage. The first house was also randomly chosen, followed by a normal selection of every second house. Epi Info 2000 software version (Atlanta, Georgia) was used to compute sample size.[14] The minimum sample size was 2000 adults with a type I error of 0.05 and an 85% power level.[15] Ethical approval was obtained from the Institutional Review Board vide Letter No. 73 dated 11/06/2020 and informed written consent was taken from all participants.
Data was collected using a self-administered Arabic questionnaire. Illiterate participants were all interviewed. The questionnaire was divided into four parts. The first part comprised14 questions on sociodemographic status as measured by Socioeconomic Status Scale (SESS). With a total score of 48, this scale covered questions on parental education, occupation, family domain, home sanitation, and economic domain. Low socioeconomic status was defined as receiving <40% of the overall score (ranging from 0 to 19.2), medium socioeconomic status was defined as obtaining 40% to 70% of the overall score (ranging from 19.2 to 33.6), and high socioeconomic status defined as obtaining more than 70% of the overall score (ranging from 33.6 to 48).[16]
The second part comprised 21 items to measure the level of depression, anxiety, and stress using Depression, Anxiety, and Stress Scale (DASS-21). A well-established self-administered tool that assesses depression, anxiety, and stress and has high reliability and validity was employed. This included three subscales of seven items each for depression, anxiety, and stress. Scores ranged from zero to three, so the total score was determined by summing the scores for the related items and multiplying by two, then graded as “mild,” “moderate,” “severe,” and “extremely severe” degrees [Table 1].[17]
Table 1.
Sub scale for depression, anxiety, and stress
| Degrees | Depression | Anxiety | Stress |
|---|---|---|---|
| Normal | 0-9 | 0-7 | 0-14 |
| Mild | 10-13 | 8-9 | 15-18 |
| Moderate | 14-20 | 10-14 | 19-25 |
| Severe | 21-27 | 15-19 | 26-33 |
| Extremely severe | >28 | >20 | >34 |
The Modified Reasons for Smoking Scale (MRSS) was used in the third part to assess the motivation to smoke. The MRSS is a 21-item self-administered practical easily understood questionnaire categorized into levels. Identification of reasons and motivations of smoking may help in smoking cessation counseling. It involved seven sub-scales, namely, Dependency, Smoking Pleasure Reduction/Relaxation Anxiety, Social Contact, Arousal, Habit/Automatism, and Hand-mouth Activity, each with three items. The overall score was calculated by adding the scores of the associated items, and then categorized as either “high” (≥11 points) or “low to moderate” (<11 points) based on the results.[18]
The fourth part involved six items to determine the level of nicotine addiction, using the Fagerstrom Test Nicotine Dependence (FTND). This six-part easy, short, and simple test assesses the intensity of physical dependence on tobacco use. In scoring the FTND, yes/no items were scored from zero to one and multiple-choice items were scored from zero to three. The items were summed to yield a total score of zero to ten. The higher the total Fagerström score, the more intensive the patient's physical dependence on nicotine. The total score was graded as “low” at (1–2 score), “low to moderate” (3–4 score), or “high to moderate” (4–5 score). Dependence was classified as either “low” (5–7 score) or “high” ((≥8 score).[19]
The study procedures were carried out in accordance with the Helsinki Declaration's ethical standards and were reviewed by a research ethics committee at the Faculty of Medicine, Fayoum University. The study participants were informed of the study's goals and the confidentiality of their information prior to the distribution of the questionnaire. Participation in the study was voluntary and a written consent was signed by all participants.
A pilot study was conducted on 200 participants, which represented 10% of the study population. Four scales were used in the study. The questionnaire was developed in English, translated into Arabic, with the help of a professional bilingual specialist. Questionnaires were distributed and completed by participants to test the clarity of questions and assess validity and reliability. Problematic questions were modified and revised by a specialist. Reliability of the questionnaire was tested by Cronbach's alpha test. Cronbach's alpha value was0.798 for SESS, 0.875 for DASS, 0.859 for MRSS, and 0.831 for FTND. Regarding validity, a correlation test was used between different items with P < 0.05 and correlation coefficient ranging between 0.22 and 0.78.
Data analysis was conducted, using the Social Science Statistical Package (SPSS) program version 22 (IBM, Armonk, NY.USA). The test used for qualitative data was Chi-square test. Bivariate Pearson correlation was used to test the association among quantitative variables. Significance was set at <0.05.
Results
A total of 2000 adults with a mean age of (31.6 ± 12.8) years comprising 1067 (53.4%) males and 933 (46.6%) females took part in the study. In terms of socioeconomic status, 1225 participants (61.2%) lived in rural areas and 775 (38.8%) lived in urban areas. The socioeconomic status of 332 (16.5%) participants was low, for 1385 (69.3%) it was medium, and for 283 (14.2%) participants socioeconomic status was high.
As regards smoking habit, 848 participants (42.4%) had smoked for a mean duration of (11.9 ± 9.3) years, and 99 participants (5%) had succeeded in quitting. Of the smokers, 765 participants (90.2%) smoked cigarettes, 50 (5.9%) smoked shisha, 15 (1.8%) smoked both cigarettes and Shisha, and finally 18 (2.1%) participants smoked cannabis [Figure 1].
Figure 1.
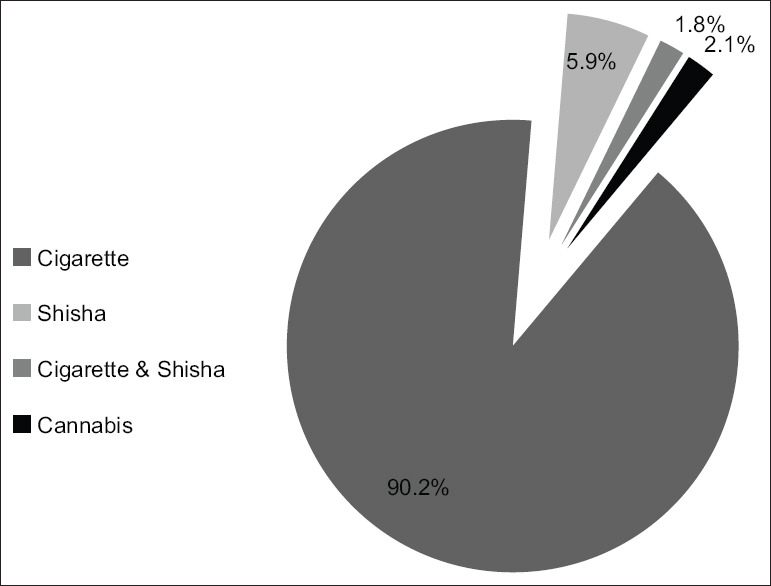
Types of smoking among study group
The findings showed that although 807 (40.4%) participants had anxiety and 485 (24.3%) had stress, only 389 (19.5%) participants showed severe to extremely severe levels of depression. For MRSS, tension reduction or relaxation was found in 440 participants (46.5%), pleasure of smoking found in 245 (25.9%) participants, hand-mouth activity in 243 (25.7%), high level of dependence in 237 (25%), social interaction found in 140 (14.8%), stimulation in 122 (12.9%), and habit/automatism in 56 (5.9%) participants. According to a Fragment test for nicotine dependence, only 93 (9.8%) participants had a high level of nicotine dependence and 406 (42.9%) had a moderate level of nicotine dependency [Table 2].
Table 2.
Frequency distribution of depression, anxiety and stress scale, modified reasons for smoking scale, and fagerstrom test for nicotine dependence scales among study subjects (n=2000)
| Variables | N (%) |
|---|---|
| DASS score (n=2000) | |
| Depression | |
| Normal | 862 (43.1) |
| Mild | 303 (15.2) |
| Moderate | 446 (22.3) |
| Severe | 215 (10.8) |
| Extremely severe | 174 (8.7) |
| Anxiety | |
| Normal | 550 (27.5) |
| Mild | 167 (8.4) |
| Moderate | 475 (23.8) |
| Severe | 270 (13.5) |
| Extremely severe | 537 (26.9) |
| Stress | |
| Normal | 765 (38.3) |
| Mild | 321 (16.1) |
| Moderate | 490 (21.5) |
| Severe | 333 (16.7) |
| Extremely severe | 152 (7.6) |
| MRSS scale (n=947) | |
| Dependence | |
| Low to moderate | 710 (75.0) |
| High | 237 (25.0) |
| Pleasure of smoking | |
| Low to moderate | 702 (74.1) |
| High | 245 (25.9) |
| Tension reduction/relaxation | |
| Low to moderate | 507 (53.5) |
| High | 440 (46.5) |
| Social interaction | |
| Low to moderate | 807 (85.2) |
| High | 140 (14.8) |
| Stimulation | |
| Low to moderate | 825 (87.1) |
| High | 122 (12.9) |
| Habit/automatism | |
| Low to moderate | 891 (94.1) |
| High | 56 (5.9) |
| Hand-mouth activity | |
| Low to moderate | 704 (74.3) |
| High | 243 (25.7) |
| FTND (n=947) | |
| Low | 217 (22.9) |
| Low to moderate | 231 (2.4) |
| Moderate | 406 (42.9) |
| High | 93 (9.8) |
DASS=Depression, Anxiety, and Stress Scale, MRSS=Modified Reasons for Smoking Scale, FTND=Fagerstrom test for nicotine dependence
There was a statistically significant higher percentage of severe and extremely severe degree of depression (14.6% and 13%), anxiety (17.7% and 39.3%), and stress (21.5% and 13.4%) respectively, with P < 0.001 among smokers, (7.8%, 5.4%, 10.3%, 16.9%, 13.1%, and 3.2%, respectively) among nonsmokers and (9.1%, 7.1%, 12.1%, 26.3%, 14.1%, and 4.1%, respectively) among former smokers [Table 3].
Table 3.
Frequency distribution of depression, anxiety, and stress among study participants by smoking status (n=2000)
| DASS score | Nonsmoker (n=1053) N (%) | Smoker (n=848) N (%) | Quit smoking (n=99) N (%) | P-value |
|---|---|---|---|---|
| Depression | ||||
| Normal | 552 (52.4) | 263 (31.0) | 47 (47.5) | <0.001 |
| Mild | 162 (15.4) | 128 (15.1) | 13 (13.1) | |
| Moderate | 200 (19.0) | 223 (26.3) | 23 (23.2) | |
| Severe | 82 (7.8) | 124 (14.6) | 9 (9.1) | |
| Extremely severe | 57 (5.4) | 110 (13.0) | 7 (7.1) | |
| Anxiety | ||||
| Normal | 389 (36.9) | 132 (15.6) | 29 (29.3) | <0.001 |
| Mild | 112 (10.6) | 51 (6.0) | 4 (4.0) | |
| Moderate | 266 (25.3) | 181 (21.4) | 28 (28.3) | |
| Severe | 108 (10.3) | 150 (17.7) | 12 (12.1) | |
| Extremely severe | 178 (16.9) | 333 (39.3) | 26 (26.3) | |
| Stress | ||||
| Normal | 515 (48.9) | 216 (25.5) | 34 (34.4) | <0.001 |
| Mild | 152 (14.4) | 145 (17.1) | 24 (24.2) | |
| Moderate | 215 (20.4) | 191 (22.5) | 23 (23.2) | |
| Severe | 137 (13.1) | 182 (21.5) | 14 (14.1) | |
| Extremely severe | 34 (3.2) | 114 (13.4) | 4 (4.1) |
DASS=Depression, Anxiety, and Stress Scale
Concerning MRSS, there was a statistically significant higher percentage of a high degree of dependence, pleasure of smoking, tension reduction/relaxation, and hand-mouth activity (P < 0.05) among smokers than among former smokers (26.5%, 27.5%, 48.9%, and 27% versus 12.1%, 12.1%, 25.3%, and 14.1%). In addition, there was a statistically significant higher percentage of moderate to high degree of nicotine dependence in smokers (53.5%) than in former smokers (45.5%), with P = 0.003 [Table 4].
Table 4.
Comparison of modified reasons for smoking scale and fagerstrom test for nicotine dependence scales among smoking groups
| MRSS scale | Smoker (n=848) N (%) | Quit smoking (n=99) N (%) | P-value |
|---|---|---|---|
| Dependence | |||
| Low to moderate | 623 (73.5) | 87 (87.9) | 0.001* |
| High | 225 (26.5) | 12 (12.1) | |
| Pleasure of smoking | |||
| Low to moderate | 615 (72.5) | 87 (87.9) | 0.001* |
| High | 233 (27.5) | 12 (12.1) | |
| Tension reduction/relaxation | |||
| Low to moderate | 433 (51.1) | 74 (74.7) | <0.001* |
| High | 415 (48.9) | 25 (25.3) | |
| Social interaction | |||
| Low to moderate | 716 (84.4) | 91 (91.9) | 0.06 |
| High | 132 (15.6) | 8 (8.1) | |
| Stimulation | |||
| Low to moderate | 735 (86.7) | 90 (90.9) | 0.3 |
| High | 113 (13.3) | 9 (9.1) | |
| Habit/automatism | |||
| Low to moderate | 797 (94.0) | 94 (94.9) | 0.8 |
| High | 51 (6.0) | 5 (5.1) | |
| Hand-mouth activity | |||
| Low to moderate | 619 (73.0) | 85 (85.9) | 0.005* |
| High | 229 (27.0) | 14 (14.1) | |
| FTND | |||
| Low | 181 (21.3) | 36 (36.4) | 0.003* |
| Low to moderate | 214 (25.2) | 17 (17.2) | |
| Moderate | 365 (43.0) | 41 (41.4) | |
| High | 88 (10.5) | 5 (5.1) |
*Statistical significance P<0.05. MRSS=Modified Reasons for Smoking Scale, FTND=Fagerstrom test for nicotine dependence
There was a statistically significant association between the level of nicotine dependency and levels of both depression and stress in smokers. Smokers with high nicotine dependence levels showed severe and extremely severe levels of both depression (12.5%, and 19.3%, respectively) and stress (26.1% and 22.7%, respectively), but there was no effect of the degree of nicotine dependence on anxiety levels [Table 5].
Table 5.
Comparison of depression, anxiety, and stress by nicotine dependence categories among smoking groups
| DASS score | Nicotine dependence categories | P-value | |||
|---|---|---|---|---|---|
|
| |||||
| Low (n=181) N (%) | Low to moderate (n=214) N (%) | Moderate (n=365) N (%) | High (n=88) N (%) | ||
| Depression | |||||
| Normal | 56 (30.9) | 81 (37.9) | 104 (28.5) | 22 (25.0) | 0.03* |
| Mild | 40 (22.1) | 29 (13.6) | 48 (13.2) | 11 (12.5) | |
| Moderate | 45 (24.9) | 52 (24.3) | 99 (27.1) | 27 (30.7) | |
| Severe | 23 (12.7) | 25 (11.7) | 65 (17.8) | 11 (12.5) | |
| Extremely severe | 17 (9.4) | 27 (12.6) | 49 (13.4) | 17 (19.3) | |
| Anxiety | |||||
| Normal | 41 (22.7) | 31 (14.5) | 53 (14.5) | 8 (9.1) | 0.06 |
| Mild | 10 (5.5) | 16 (7.5) | 19 (5.2) | 6 (6.8) | |
| Moderate | 41 (22.7) | 50 (23.4) | 79 (21.6) | 11 (12.5) | |
| Severe | 30 (16.6) | 32 (15.0) | 67 (18.4) | 21 (23.9) | |
| Extremely severe | 59 (32.6) | 85 (39.7) | 147 (40.3) | 42 (47.7) | |
| Stress | |||||
| Normal | 61 (33.7) | 60 (28.0) | 80 (21.9) | 15 (17.0) | 0.02* |
| Mild | 30 (16.6) | 40 (18.7) | 64 (17.5) | 11 (12.5) | |
| Moderate | 37 (20.4) | 52 (24.3) | 83 (22.7) | 19 (21.6) | |
| Severe | 32 (17.7) | 37 (17.3) | 90 (24.7) | 23 (26.1) | |
| Extremely severe | 21 (11.6) | 25 (11.7) | 48 (13.2) | 20 (22.7) | |
*Statistical significance P<0.05. FTND=Fagerstrom test for nicotine dependence, DASS=Depression, Anxiety, and Stress Scale
The results showed that there was a statistically significant positive correlation, with P < 0.001, between the DASS score (depression, anxiety, and stress) with both FTND and MRSS scale, which indicated an association of increase in nicotine dependence score and an increase in DASS score. In addition, age was in a negative correlation with depression and a positive correlation with both anxiety and stress. The duration of smoking positively correlated with both depression and stress [Table 6].
Table 6.
Correlation between depression, anxiety, and stress and study variables among smokers
| Variables | Depression r (P-value) | Anxiety r (P-value) | Stress r (P-value) |
|---|---|---|---|
| Age (years) | −0.13 (0.001)* | 0.08 (0.02)* | 0.07 (0.02)* |
| Smoking duration | −0.09 (0.01)* | 0.06 (0.07) | 0.10 (0.002)* |
| FTND | 0.12 (0.001)* | 0.15 (0.001)* | 0.18 (0.001)* |
| MRSS scale | |||
| Dependence | 0.22 (0.001)* | 0.17 (0.001)* | 0.26 (0.001)* |
| Pleasure of smoking | 0.16 (0.001)* | 0.22 (0.001)* | 0.25 (0.001)* |
| Tension reduction/relaxation | 0.17 (0.001)* | 0.19 (0.001)* | 0.34 (0.001)* |
| Social interaction | 0.13 (0.001)* | 0.18 (0.001)* | 0.23 (0.001)* |
| Stimulation | 0.15 (0.001)* | 0.20 (0.001)* | 0.22 (0.001)* |
| Habit/automatism | 0.27 (0.001)* | 0.30 (0.001)* | 0.21 (0.001)* |
| Hand-mouth activity | 0.21 (0.001)* | 0.19 (0.001)* | 0.18 (0.001)* |
*Statistical significance P<0.05. FTND=Fagerstrom test for nicotine dependence, MRSS=Modified Reasons for Smoking Scale
With regard to the type of smoking, there was a statistically significant higher percentage of moderate to severe nicotine dependence among hashish smokers, with P = 0.02 (P = 0.02). However, there was no significant difference in DASS score among different types of smokers.
Finally, there was an association between the degree of nicotine dependence and the reasons of smoking. There was a statistically significant positive correlation between FTND scale and MRSS subscales as a dependency (r = 0.40, P < 0.001), pleasure of smoking (r = 0.23, P = 0.02), social interaction (r = 0.36, P < 0.001), stimulation (r = 0.3, P < 0.001), and habit/automatism (r = 0.64, P < 0.001). However, there was no statistically significant correlation with tension reduction, or hand-mouth activity subscale with P > 0.05.
Discussion
Assuming that existing tobacco control measures are maintained in all countries, the global incidence of tobacco use is expected to drop to around one-fifth (20.9%) of the global population by 2025.[20]
The current study found that depression, anxiety, and stress were prevalent in 41.7%, 64.2%, and 45.8% of the study participants, respectively. Unlike the current findings, an Iranian study found a lower prevalence of depression (29%), anxiety (32.2%), and stress (34.8%).[21] However, the present findings were in line with the findings of an Egyptian study; which showed that 65%, 73%, and 59.9% of the participants suffered from depression, anxiety, and stress, respectively.[22] As for nicotine dependence, the current study showed a prevalence of high level nicotine dependency in 9.8% of participants, moderate level in 42.9%, low to moderate level in 2.4% and finally low nicotine dependency in 22.9%. In contrast to our findings, a study in El Mansoura reported high nicotine dependence in 58.2% of the study group, but moderate and low nicotine-dependent participants were 17.5% and 24.3% respectively.[23]
In the current study, 42.4% of the participants smoked, with a mean smoking duration of (11.9 ± 9.3) years and 5% of them had been successful in quitting. Of the smokers, 90.2% used to smoke cigarettes, 5.9% used to smoke Shisha, and 1.8% used to smoke both cigarettes and Shisha, and 2.1% used to smoke cannabis. This result is in accord with Al-Naggar et al.,[22] who found that 57% of the study population smoked, which is significantly higher than was found in a study in Malaysia, where only 17.64% of the study population smoked.[24] In El Mansoura, most participants were current smokers (68.7%), while 18.7% of them were ex-smokers.[23]
The current study looked at the link between smoking on one hand and anxiety, stress, and depressive symptoms on the other. This finding corroborates the findings of a study from Singapore that showed a link between tobacco use and depression and anxiety. The study also found that smoking-related co-morbidities worsened anxiety, stress, and depression, creating a vicious cycle. It also had an impact on the success of smoking cessation.[25] In agreement with the current study, a Tunisian study revealed that smokers had a two-fold higher rate of severe depressive disorder than non-smokers.[12]
As for the association between nicotine dependence and psychometric disorders, the current study found a statistically significant association between nicotine dependence and DASS score for psychiatric symptoms in smokers, particularly cannabis smokers. This finding agrees with several studies that discovered a strong association between nicotine dependence and psychiatric morbidity such as stress, anxiety and depression.[25,26] Smokers with depression had greater difficulty in quitting.[25] Similarly, the current study found a strong association of high nicotine dependence levels and severe/extremely severe depression and stress; however, no association was found between smoking and anxiety levels, which agreed with a study conducted by Wootton.[27] Unlike the current study and the Wootton' study, a study of Indonesian adolescents found an association between nicotine dependency and anxiety.[28]
As regards former smokers, the current research found no statistically significant association between nicotine dependence and psychiatric diseases. In addition to the general health benefits of quitting smoking, psychiatric symptoms such as anxiety and depression also improved.[29,30] In other words, there is a link between smoking cessation and a reduction in stress, anxiety, and depression.[31]
From another perspective, the current study reported statistically significant higher degrees of nicotine dependency, pleasure of smoking, tension reduction/relaxation, and hand-mouth activity among smokers than former smokers.
On the reasons for smoking, several studies have attributed smoking to pleasure, pressure, and stress. For instance, an Indian study found that tension, fun, and peer pressure were the key reasons for starting to smoke.[30] In another Indian study, the main reasons for continuing smoking were the reduction of mental stress, the enjoyment of smoking and addiction.[32] In an Egyptian study, the most common motives for smoking were habit (40.8%), sense of loneliness (31.1%), overcoming anxiety (28.6%), life stresses (28.2%), pressure from family and friends (12.7%), overcoming negative feelings (6.8%), and oppositional behavior (4.9%).[23] Similarly, stress, pleasure, peer and social pressure were the most common reasons for starting to smoke as revealed in an Iranian study.[33] Four basic motivational features of smokers' actions were in a Belgium paper: Smoking to increase a pleasant/positive effect, smoking to minimize a negative effect, smoking as a habit or with no attempt to mitigate/increase any effect, or smoking due to addiction.[34]
The score of psychiatric morbidity (depression, anxiety, and stress) in the current study had a statistically significant positive correlation with age, smoking duration, nicotine dependence level, and the MRSS subscales. These findings agreed with a Kazakhstan study that found no significant differences in the prevalence of depressive symptoms based on age. While the age group 36-45 years had the highest percentage of people without symptoms, the age group of over 60s had the highest percentage of people with severe symptoms.[35]
Finally, there were some limitations in the conduct of the study. The first limitation was the logistic difficulty in obtaining zoning information to apply the sample technique. Secondly, using four scales to assess the study outcomes was time-consuming and required a lot of work in preparation, translation, and data collection and entry. In addition, illiterate participants needed much clarification and help to complete the questionnaire.
Conclusion
Our findings showed that smoking is linked to psychological symptoms and show moderate to high level of nicotine dependence. The motives for smoking involved a higher level of dependency, smoking pleasure, stress reduction/relaxation, and hand-mouth movement. Furthermore; there was a correlation between nicotine dependence, on one hand, and depression and stress, on the other. Smokers' mental health was negatively affected by their smoking motivation and nicotine addiction. To start a smoking cessation program, the current study recommends the identification of causes and motives that keep people smoking and act as barriers to the quitting therapy. It also recommends identification of psychiatric symptoms associated with smoking to be handled professionally in the program to go through the withdrawal phase safely and successfully. Therefore, both psychological and nicotinic factors should be dealt with.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mental Health Foundation Agency. Smoking and Mental Health. [Last accessed on 2021 Feb 14]. Available from: https://www.mentalhealth.org.uk/a-to-z/s/ smoking-and-mental-health .
- 2.Pawlina MM, Rondina Rde C, Espinosa MM, Botelho C. Depression, anxiety, stress, and motivation over the course of smoking cessation treatment. J Bras Pneumol. 2015;41:433–9. doi: 10.1590/S1806-37132015000004527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. WHO Report on the Global Tobacco Epidemic, 2017: Monitoring Tobacco Use and Prevention Policies. [Last accessed on 2021 Feb 14]. Available from: https://apps.who.int/iris/ handle/10665/255874 .
- 4.Center for Disease Control and Prevention (CDC) Smoking and Tobacco use. Fast Fact sheet. 2020. [Last accessed on 2021 Feb 15]. Available from: https:// www.cdc.gov/tobacco/data_statistics/fact_sheets/fast_facts/ index.htm#:~:text=If%20the%20pattern%20of%20smoking, to%20tobacco%20use%20by%202030.&text=Cigarette%20smoking%20is%20responsible%20for,resulting%20from%20secondhand%20smoke%20exposurE .
- 5.Fouda S, Kelany M, Moustafa N, Abushouk AI, Amro Hassane A, Ahmad Sleem, et al. Tobacco smoking in Egypt: A scoping literature review of its epidemiology and control measures. East Mediterr Health J. 2018;24:198–215. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC). Tobacco Use and Quitting Among Individuals with Behavioral Health Conditions. [Last accessed on 2020 Sep 18]. Available from: https://www.cdc.gov/tobacco/ disparities/mental-illness-substance-use/index.htm .
- 7.Yuan S, Yao H, Larsson SC. Associations of cigarette smoking with psychiatric disorders: Evidence from a two-sample Mendelian randomization study. Sci Rep. 2020;10:13807. doi: 10.1038/s41598-020-70458-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC). Vital Signs Fact Sheet: Adult Smoking Focusing on People with Mental Illness, February 2013. National Center for Chronic Disease and Health Promotion, Office on Smoking and Health, 2013. [Last accessed on 2021 Feb 10]. Available from: https://www.cdc.gov/vitalsigns/pdf/2013-02-vitalsigns. pdf .
- 9.Sciberras E, Mulraney M, Silva D, Coghill D. Prenatal risk factors and the etiology of ADHD-Review of existing evidence. Curr Psychiatry Rep. 2017;19:1. doi: 10.1007/s11920-017-0753-2. [DOI] [PubMed] [Google Scholar]
- 10.Leventhal AM, Ray LA, Rhee SH, Unger JB. Genetic and environmental influences on the association between depressive symptom dimensions and smoking initiation among Chinese adolescent twins. Nicotine Tob Res. 2012;14:559–68. doi: 10.1093/ntr/ntr253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Das S, Prochaska JJ. Innovative approaches to support smoking cessation for individuals with mental illness and co-occurring substance use disorders. Expert Rev Respir Med. 2017;11:841–50. doi: 10.1080/17476348.2017.1361823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ghali H, Rejeb OB, Fredj SB, Khéfacha S, Dhidah L, Rejeb MB, et al. Smoking dependence and anxio-depressive disorders in Tunisian smokers attending the smoking cessation clinic in a university hospital. J Egypt Public Health Assoc. 2019;94:9. doi: 10.1186/s42506-019-0012-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. WHO Report on the Global Tobacco Epidemic, 2019: Offer Help to Quit Tobacco Use. [Last accessed on 2021 Oct 12]. Available from: https://www.who.int/publications/i/ item/9789241516204 .
- 14.CDCEPI INFO VERSION 7.0.8.3 READ ME FILE. CDC. [Last accessed on 2011 Nov 17]. Available from: https://www.cdc.gov/epiinfo/index.html .
- 15.Mirzaei M, Yasini Ardekani SM, Mirzaei M, Dehghani A. Prevalence of depression, anxiety and stress among adult population: Results of Yazd health study. Iran J Psychiatry. 2019;14:137–46. [PMC free article] [PubMed] [Google Scholar]
- 16.Fahmy SI, Nofal LM, Shehata SF, El Kady HM, Ibrahim HK. Updating indicators for scaling the socioeconomic level of families for health research. J Egypt Public Health Assoc. 2015;90:1–7. doi: 10.1097/01.EPX.0000461924.05829.93. [DOI] [PubMed] [Google Scholar]
- 17.Norton PJ. Depression Anxiety and Stress Scales (DASS-21): Psychometric analysis across four racial groups. Anxiety Stress Coping. 2007;20:253–65. doi: 10.1080/10615800701309279. [DOI] [PubMed] [Google Scholar]
- 18.Fiala KA, D'Abundo ML, Marinaro LM. Construct validity and reliability of college students' responses to the reasons for smoking scale. J Am Coll Health. 2010;58:571–7. doi: 10.1080/07448481003622294. [DOI] [PubMed] [Google Scholar]
- 19.Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström test for nicotine dependence: A revision of the Fagerström tolerance questionnaire. Br J Addict. 1991;86:1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization. WHO Global Report on Trends in Prevalence of Tobacco use 2000-2025. World Health Organization. 3rd ed. 2019. [Last accessed on 2021 Feb12]. p. 5. Available from: https://www.who.int/ publications/i/item/who-global-report-on-trends-in-prevalenceof- tobacco-use-2000-2025-third-edition .
- 21.Fawzy M, Hamed SA. Prevalence of psychological stress, depression and anxiety among medical students in Egypt. Psychiatry Res. 2017;255:186–94. doi: 10.1016/j.psychres.2017.05.027. [DOI] [PubMed] [Google Scholar]
- 22.Al-Naggar RA, Bobryshev YV, Anil S. Pattern of shisha and cigarette smoking in the general population in Malaysia. Asian Pac J Cancer Prev. 2014;15:10841–6. doi: 10.7314/apjcp.2014.15.24.10841. [DOI] [PubMed] [Google Scholar]
- 23.Abu Nazel M, Elkady H, Abd Allah S, Ibrahim R. Pattern and correlates of tobacco smoking among mentally ill male patients in El-Mamoura psychiatric hospital, Alexandria, Egypt. J Egypt Public Health Assoc. 2017;92:167–76. [PubMed] [Google Scholar]
- 24.Abd Rashid R, Kanagasundram S, Danaee M, Abdul Majid H, Sulaiman AH, Ahmad Zahari MM, et al. The prevalence of smoking, determinants and chance of psychological problems among smokers in an urban community housing project in Malaysia. Int J Environ Res Public Health. 2019;16:1762. doi: 10.3390/ijerph16101762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ho CS, Tan EL, Ho RC, Chiu MY. Relationship of anxiety and depression with respiratory symptoms: Comparison between depressed and non-depressed smokers in Singapore. Int J Environ Res Public Health. 2019;16:163. doi: 10.3390/ijerph16010163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Branstetter SA, Muscat JE, Mercincavage M. Time to first cigarette: A potential clinical screening tool for nicotine dependence. J Addict Med. 2020;14:409–14. doi: 10.1097/ADM.0000000000000610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wootton RE, Richmond RC, Stuijfzand BG, Lawn RB, Sallis HM, Taylor GM, et al. Evidence for causal effects of lifetime smoking on risk for depression and schizophrenia: A Mendelian randomisation study. Psychol Med. 2020;50:2435–43. doi: 10.1017/S0033291719002678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fahrizal Y, Risdiana N, Rustyawati F. The correlation between nicotine dependence level and anxiety in Indonesian adolescent smokers. Open Access Mac J Med Sci. 2021;9:177–81. [Google Scholar]
- 29.de Souza ES, Crippa JA, Pasian SR, Martinez JA. Modified reasons for smoking scale: Translation to Portuguese, cross-cultural adaptation for use in Brazil and evaluation of test-retest reliability. J Bras Pneumol. 2009;35:683–9. doi: 10.1590/s1806-37132009000700010. [DOI] [PubMed] [Google Scholar]
- 30.Boksa P. Smoking, psychiatric illness and the brain. J Psychiatry Neurosci. 2017;42:147–9. doi: 10.1503/jpn.170060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zarghami M, Taghizadeh F, Sharifpour A, Alipour A. Efficacy of smoking cessation on stress, anxiety, and depression in smokers with chronic obstructive pulmonary disease: A randomized controlled clinical trial. Addict Health. 2018;10:137–47. doi: 10.22122/ahj.v10i3.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chezhian C, Murthy S, Prasad S, Kasav JB, Mohan SK, Sharma S, et al. Exploring factors that influence smoking initiation and cessation among current smokers. J Clin Diagn Res. 2015;9:C08–12. doi: 10.7860/JCDR/2015/12047.5917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.De Wilde KS, Tency I, Boudrez H, Temmerman M, Maes L, Clays E. The modified reasons for smoking scale: Factorial structure, validity and reliability in pregnant smokers. J Eval Clin Pract. 2016;22:403–10. doi: 10.1111/jep.12500. [DOI] [PubMed] [Google Scholar]
- 34.Araújo AJ. Reasons for smoking or reasons for quitting, that is the question: Can administering the modified reasons for smoking scale make a difference in clinical practice? J Bras Pneumol. 2019;45:e20190253. doi: 10.1590/1806-3713/e20190253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Turgunova L, Laryushina Y, Turmukhambetova A, Koichubekov B, Sorokina M, Korshukov I. The incidence of depression among the population of central kazakhstan and its relationship with sociodemographic characteristics. Behav Neurol 2017. 2017. [Last accessed on 2021 Feb12]. p. 2584187. Available from: https://www.hindawi.com/ journals/bn/2017/2584187/ [DOI] [PMC free article] [PubMed]


