Abstract
Purpose
To report a case of cystoid macular edema, uveitis, and vitreomacular traction in a patient with a history of breast cancer and taking anastrozole.
Observations
A 73-year-old female with a history of estrogen receptor-positive breast cancer and treatment with anastrozole presented with bilateral blurry vision, photophobia, and eye soreness. Optical coherence tomography (OCT) of both maculae revealed vitreomacular traction (VMT), an epiretinal membrane, cystoid macular edema (CME) in the right eye, and drusen without subretinal fluid bilaterally. Although later, macular OCT did show evidence of cystoid intraretinal spaces in the left eye as well. Fluorescein angiography showed bilateral petaloid leakage, bilateral slow disc leaking, as well as peripheral leakage in the right eye. Anastrozole was discontinued and, subsequent macular OCT showed release of VMT in the right eye, and eventual resolution of intraretinal cystoid spaces bilaterally.
Conclusions and importance
Stopping of anastrozole was associated in resolution of refractory CME in a patient on aromatase inhibitor therapy for breast cancer. It is therefore important to consider anastrozole and other aromatase inhibitor drugs as possible factors predisposing patients to the development of CME.
Keywords: Anastrozole, Cystoid macular edema, Uveitis, Vitreomacular traction, Breast cancer
1. Introduction
Anastrozole is a non-steroidal aromatase inhibitor (AI) that is used to treat estrogen receptor-positive breast cancer in post-menopausal women by reducing estrogen levels. Estrogen modulates vascular leakage, and estrogen receptors are found in the retina and retinal pigment epithelium (RPE).1, 2, 3 Therefore, we presume that decreasing levels of estrogen using AIs has the possibility of inciting vascular changes in the retina. Indeed, AIs have been shown in a cross-sectional study to be associated with structural decrease in retina nerve fiber layer thickness and a diminished retina multifocal electroretinography response.4 In case reports, anastrozole has also been associated with dry eye, disc swelling, retinal hemorrhages, vitreoretinal traction, cystoid macular edema (CME), and uveitis.5, 6, 7, 8, 9, 10 We report a patient taking anastrozole who presented with CME, vitreomacular traction (VMT), and retinal vasculitis mimicking pseudophakic macular edema but occurring remote to cataract surgery.
2. Case report
A 73-year-old female with a history of breast cancer treated with anastrozole presented in April 2018 with blurry vision and photophobia in both eyes. Ocular history was significant for uncomplicated cataract surgeries in December 2015 and August 2016 for the right and left eyes and bilateral early dry age-related macular degeneration. The patient reported a diagnosis of estrogen receptor-positive breast cancer and had undergone bilateral lumpectomy in 2014 when she was started on anastrozole. Other medical history was significant for hypertension.
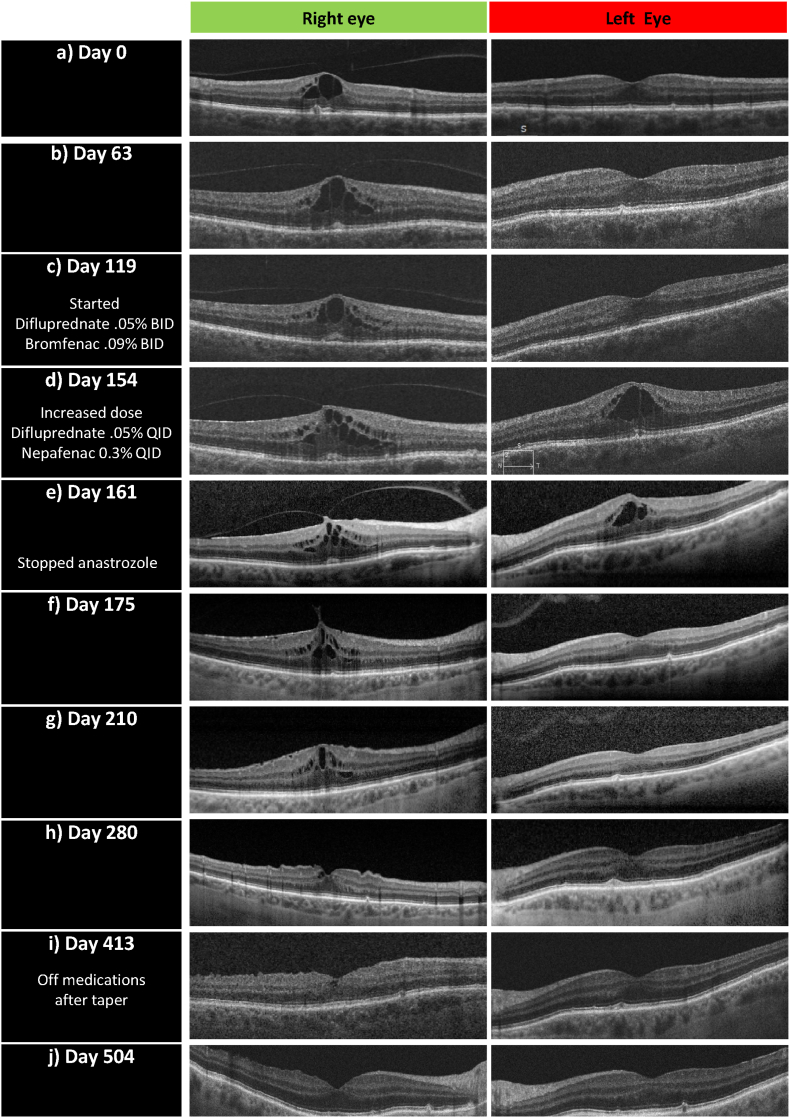
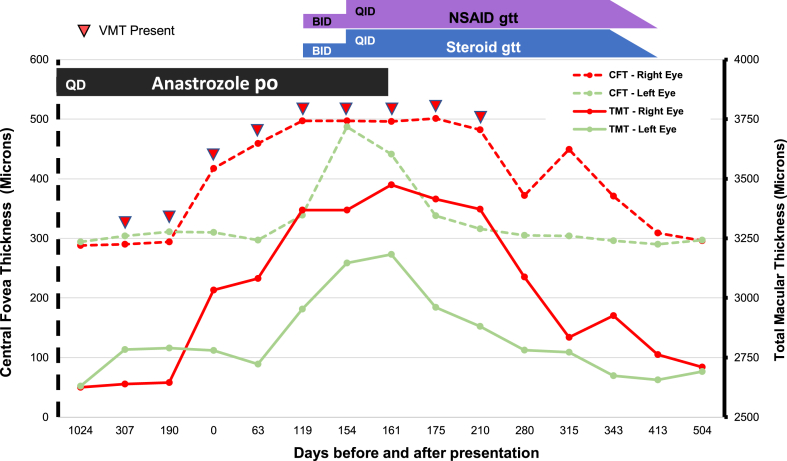
On presentation, visual acuity measured 20/40 and 20/50 in the right and left eyes. Anterior chambers on examination were deep and quiet. Both eyes were pseudophakic. OCT demonstrated VMT, epiretinal membrane (ERM) and CME in the right eye and a partial posterior vitreous detachment (PVD) without CME in the left eye (Fig. 1a). Two month follow up eye exam and OCT imaging were unchanged (Fig. 1b). However, the following month (119 days after presentation), she presented with eye soreness and photophobia. Her visual acuity was 20/200 and 20/60 without improvement on pinhole testing in the right and left eyes. Intraocular pressures were normal. Her anterior exam was significant for +1 cell without flare or keratic precipitates bilaterally. SD-OCT of the maculae continued to demonstrate the previously noted abnormalities (Fig. 1c). Despite the lack of evidence of cystoid spaces on OCT in the left eye, her macula thickened showing central fovea thicknesses that increased from 297 to 339 μm (Figs. 1c and 2). The patient was started on difluprednate 0.05% and bromfenac 0.09% two times a day in both eyes.
Fig. 1.
Optical Coherence Tomography Images of Right and Left Eyes Over Time. Legend: Progression of optical coherence tomography (OCT) images is shown with respect to treatment changes. Day 0 (a), OCT shows presence of vitreomacular traction (VMT), cystoid macular edema (CME), and epiretinal membrane in right eye (OD) and partial vitreous detachment without CME in left eye (OS). Day 119 (c), started on difluprednate and bromfenac (BID). Day 154 (d), switched to difluprednate and nepafenac (QID), OCT shows development of cystoid macular edema (CME) (OS). Day 161 (e), stopped anastrozole. Day 210 (g), OCT shows release of vitreomacular traction (OD) and resolution of CME (OS).
Fig. 2.
Central Foveal and Total Macular Thicknesses of Right and Left Eyes Over Time
Legend: Line plot showing the change in central foveal thickness (dashed lines) and total macular thickness (solid lines) over time in both right and left eyes. NSAID, steroid, and anastrozole treatment timelines are represented respectively by the purple, blue, and black bars. Significant events include patient presentation on day 0, starting difluprednate and bromfenac (BID) on day 119, switching to difluprednate and nepafenac (QID) on day 154, and stopping anastrozole on day 161. Vitreomacular traction was present until day 210 (inverted red triangles). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
One month later (154 days after presentation), the patient continued to have blurry vision but her photophobia and eye pain had resolved. Anterior chambers were deep and quiet bilaterally. Visual acuity worsened to 20/80 in the left eye. OCT of the right eye showed persistent VMT with worsening CME, and the left eye then showed CME with an increased central fovea thickness of 487 μm (Figs. 1d and 2). Difluprednate 0.05% was increased to four times daily and she was started on nepafenac 0.3% four times daily. Bromfenac 0.09% was discontinued.
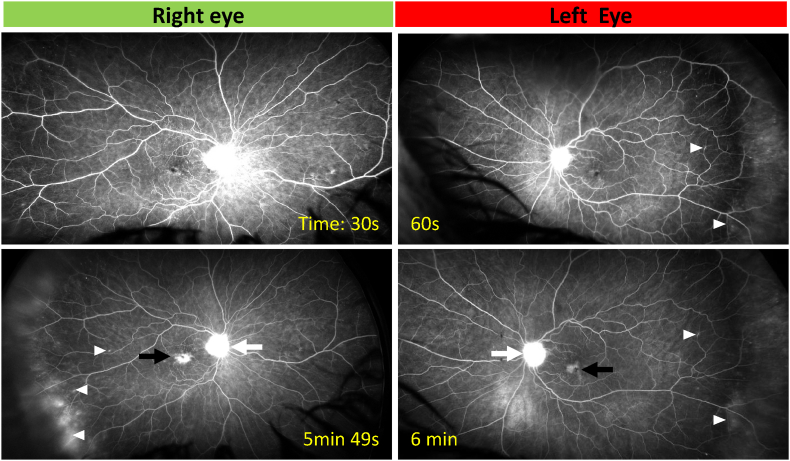
OCT findings the following week in the left eye showed slight improvement of intraretinal fluid and central fovea thickness on OCT (Figs. 1e and 2). Macula thicknesses were increased bilaterally (Fig. 2). Fluorescein angiography (FA) showed bilateral petaloid leakage in the macula, bilateral late disc leakage as well as peripheral leakage in the right eye (Fig. 3). A comprehensive uveitis work up was performed and results did not support a diagnosis of tuberculosis, syphilis, Toxoplasma, Sarcoidosis, HLAB27, and granulomatosis with polyangitis. Complete blood count with differential and Complete metabolic panels were normal. Additional testing showed anti-nuclear antibody immunofluorescence positivity (1:160), positive ANA IgG, positive Hep-2 cell fluorescence, and weakly positive Anti-Histone IgG, suggestive of drug-induced lupus serotype. Other antibodies were negative including anti-Ro, anti-La, anti-Scl, anti-CENP, anti-Jo, rheumatoid factor, thyroid antibodies, and antiphospholipid syndrome antibodies. Soluble IL-2R was found to be elevated (2 years later the patient was diagnosed with lymphoma). The patient consulted her oncologist and stopped anastrozole the next day.
Fig. 3.
Fluorescein Angiography Images of Left and Right Eyes
Legend: Fluorescein angiography of the right and left eye demonstrates peripheral vascular leakage (white triangles), petaloid macular edema (black arrow), and optic nerve (white arrow) leakage in both eyes.
Over several months following the discontinuation of anastrozole and tapering off topical medications, visual acuity improved to 20/25 bilaterally. Sequential OCTs showed improvement and eventual resolution of CME bilaterally and release of VMT in the right eye (Fig. 1f–j).
3. Discussion
The bilateral macular edema seen in this patient is believed to be secondary to anastrozole therapy in a well-controlled hypertensive patient without signs of any other retinopathy who had underwent uncomplicated cataract surgery 2 years previously. Despite 5 weeks of treatment with topical anti-inflammatories, the CME persisted in the right eye and worsened in the left eye. In addition to the petaloid leakage expected to be seen with CME, peripheral leakage in the right eye suggests increased retinal vascular permeability as a cause for the CME rather than VMT or ERM. Lastly, the CME greatly improved after the patient stopped her anastrozole therapy. The progression of OCT images was taken both Zeiss Cirrus and Heidelberg Spectralis imaging systems. Thickness measurements differ by 14 μm due to variation in measuring above (Zeiss) or below (Heidelberg) the retinal pigment epithelium.11 However, the changes in both central foveal thickness and total macular thickness observed exceed this variation in imaging measurement parameters.
As estrogen receptors have been identified in the retina, decreased levels of estrogen secondary to AI use may contribute to vascular leakage and breakdown of the blood-retina barrier, and this may occur more readily in patients with diabetes and hypertension.2,3 Previous case reports have suggested anastrozole and other AI medications as a possible cause of macular edema and uveitis.5,6,10 In this case, anastrozole may have likewise contributed to the anterior uveitis seen on presentation with CME.
Other aspects of the patient's history and work up may have contributed to the CME identified, but they were not thought to be the primary cause. Although the patient had a negative infectious work up, her inflammatory work up was significant for an ANA titer of 1:160 which does carry associations with retinal vascular leakage. Elevated Soluble IL-2R levels as seen in this patient are associated with acquired immunodeficiency, autoimmune disease, sarcoidosis, and a variety of leukemias and lymphomas. This patient was subsequently diagnosed with large B-cell lymphoma. Lastly, the patient underwent cataract extraction over 2 years prior to her presentation making pseudophakic macular edema (Irvine-Gass syndrome) unlikely. In this case, a positive ANA titer may have reduced her threshold to develop CME while on anastrozole.
In addition to vascular leakage, VMT and ERM could also be contributing factors to the intraretinal fluid in the right eye. We observed two events: non-central macular edema improved while the central macular edema persisted until VMT resolved. It should be noted, however, that female gender and menopause are known risk factors for VMT. As anastrozole decreases estrogen levels, the increase risk of VMT with anastrozole use has been suggested.8,12 The left eye imaging revealed a partial PVD and no ERM suggesting the lack of traction contributing to the CME in that eye. Both eyes recovered with topical anti-inflammatories and cessation of anastrozole therapy suggesting an inflammatory role as previously mentioned.
4. Conclusion
We present a case of a patient taking AI for a history of breast cancer and developed cystoid macular edema and retinal vascular leakage with a serological profile suggestive of drug induced lupus. With the decrease in estrogen levels secondary to AI therapy, we propose that the use of anastrozole may increase patient susceptibility to developing intraretinal fluid from inflammatory and tractional etiologies. Although the exact role of estrogen receptors identified in the retina and RPE remain unclear, AI use has been linked to VMT, uveitis, and macular edema.5,6,8,10 It is therefore important to consider anastrozole and other AI drugs as possible factors predisposing patients to the development of CME. In this case, when anastrozole use was stopped, in addition to topical anti-inflammatory therapy, both eyes experienced resolution of the CME as well as improvement in vision. Others have continued anastrozole therapy and successfully treated CME with just topical anti-inflammatories.5 Ophthalmologists and oncologists should work together to find treatments best suited for patients when considering CME induced by anastrozole therapy.
Patient consent
Written, informed patient consent was obtained for publication and health information access.
Funding
The work described was supported by:
Research to Prevent Blindness unrestricted grant to UC Irvine Department of Ophthalmology.
UC Irvine Institute for Clinical and Translational Science - KL2 Grant number is KL2 TR001416Ð_
Authorship
All authors attest that they meet the current ICJME criteria for Authorship.
Declaration of competing interest
All authors have no financial disclosures.
Acknowledgements
None.
References
- 1.Chakrabarti S., Lekontseva O., Davidge S.T. Estrogen is a modulator of vascular inflammation. IUBMB Life. 2008;60:376–382. doi: 10.1002/iub.48. [DOI] [PubMed] [Google Scholar]
- 2.Munaut C., Lambert V., Noël A., et al. Presence of oestrogen receptor type β in human retina. Br J Ophthalmol. 2001;85(7):877–882. doi: 10.1136/bjo.85.7.877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ogueta S.B., Schwartz S.D., Yamashita C.K., Farber D.B. Estrogen receptor in the human eye: influence of gender and age on gene expression. IOVS (Investig Ophthalmol Vis Sci) 1999;40(9):1906–1911. [PubMed] [Google Scholar]
- 4.Moschos M.M., Chatziralli I.P., Sergentanis T., et al. Electroretinographic and optical coherence tomography findings in breast cancer patients using aromatase inhibitors. Cutan Ocul Toxicol. 2016;35(1):13–20. doi: 10.3109/15569527.2014.1003267. [DOI] [PubMed] [Google Scholar]
- 5.Sathiamoorthi S., Ruddy K.J., Bakri S.J. Association of uveitis and macular edema with anastrozole therapy. JAMA Ophthalmol. 2018;136(7):837–839. doi: 10.1001/jamaophthalmol.2018.1700. [DOI] [PubMed] [Google Scholar]
- 6.Eisner A., Falardeau J., Toomey M.D., Vetto J.T. Retinal hemorrhages in anastrozole users. Optom Vis Sci. 2008;85(5):301–308. doi: 10.1097/OPX.0b013e31816bea3b. [DOI] [PubMed] [Google Scholar]
- 7.Coppes O.J., Lukas R.V., Fleming G.F., Nichols J., Tenney M., Bernard J. Bilateral optic disc swelling following anastrozole therapy. Neuro Ophthalmol. 2014;38(5):268–271. doi: 10.3109/01658107.2014.924968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eisner A., Thielman E.J., Falardeau J., Vetto J.T. Vitreo-retinal traction and anastrozole use. Breast Cancer Res Treat. 2009;117(1):9–16. doi: 10.1007/s10549-008-0156-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turaka K., Nottage J.M., Hammersmith K.M., Nagra P.K., Rapuano C.J. Dry eye syndrome in aromatase inhibitor users. Clin Exp Ophthalmol. 2013;41(3):239–243. doi: 10.1111/j.1442-9071.2012.02865.x. [DOI] [PubMed] [Google Scholar]
- 10.Moschos M.M., Chatziralli I.P., Zagouri F., Zografos G.C. Macular oedema due to letrozole: a first case report. Clin Exp Optom. 2012;95(6):646–650. doi: 10.1111/j.1444-0938.2012.00771.x. [DOI] [PubMed] [Google Scholar]
- 11.Sander B., Al-Abiji H.A., Kofod M., Jørgensen T.M. Do different spectral domain OCT hardwares measure the same? Comparison of retinal thickness using third-party software. Graefes Arch Clin. 2015;253(11) doi: 10.1007/s00417-015-3075-2. 1915-1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chuo J.Y., Lee T.Y., Hollands H., et al. Risk factors for posterior vitreous detachment: a case-control study. Am J Ophthalmol. 2006;142(6):931–937. doi: 10.1016/j.ajo.2006.08.002. [DOI] [PubMed] [Google Scholar]