ABSTRACT
Background
As a highly infectious disease with human-to-human transmission characteristics, COVID-19 has caused panic in the general public. Those who have recovered from COVID-19 may experience discrimination and internalized stigma. They may be more likely to worry about social interaction and develop social anxiety.
Objectives
This study investigated the associations among hospitalization factors, social/interpersonal factors, personal factors, and social anxiety to reveal the mechanism of social anxiety in COVID-19 survivors.
Methods
A cross-sectional, multicenter telephone survey was conducted from July to September 2020 in five Chinese cities (i.e. Wuhan, Nanning, Shenzhen, Zhuhai, and Dongguan); adult COVID-19 survivors were recruited 6 months after they were discharged from the hospital. Linear regressions and path analysis based on the minority stress model were conducted to test the relationships among hospitalization, social/interpersonal factors, personal factors, and social anxiety.
Results
The response rate was 74.5% (N = 199, 55.3% females). Linear regression analyses showed that various hospitalization, social/interpersonal, and personal factors were statistically significantly associated with social anxiety. Path analysis showed that the proposed model fit the data well (χ2(df) = 3.196(3), p = .362, CFI = .999, NNFI = .996, RMSEA = .018). Internalized stigma fully mediated the association between perceived discrimination/social support and social anxiety, while it partially mediated the association between perceived affiliate stigma and social anxiety.
Conclusions
The results suggest that social/interpersonal and personal factors have a stronger association with social anxiety than hospitalization factors and highlight the importance of internalized stigma in understanding the mechanisms of these relationships. Clinical psychologists can refer to these modifiable psychosocial factors to develop efficient interventions for mental health promotion.
KEYWORDS: COVID-19 survivor, hospitalization, social anxiety, psychosocial factors, minority stress, China
HIGHLIGHTS
Internalized stigma fully mediated the effects of perceived discrimination and social support on social anxiety and partially mediated the effect of perceived affiliate stigma on social anxiety.
Short abstract
Antecedentes: Como una enfermedad altamente infecciosa con características de transmisión de persona a persona, el COVID-19 ha causado pánico en el público en general. Aquellos que se han recuperado del COVID-19 pueden experimentar discriminación y estigma internalizado. Es más probable que se preocupen por la interacción social y desarrollen ansiedad social.
Objetivos: Este estudio investigó las asociaciones entre factores de hospitalización, factores sociales /interpersonales, factores personales y ansiedad social para revelar el mecanismo de ansiedad social en sobrevivientes de COVID-19.
Métodos: Se realizó una encuesta telefónica transversal multicentro de julio a septiembre de 2020 en cinco ciudades chinas (es decir, Wuhan, Nanning, Shenzhen, Zhuhai y Dongguan). Se reclutaron sobrevivientes adultos de COVID-19 seis meses después de ser dados de alta del hospital. Se realizaron regresiones lineales y análisis de ruta basados en el modelo de estrés de minoría para probar las relaciones entre la hospitalización, los factores sociales/interpersonales, los factores personales y la ansiedad social.
Resultados: La tasa de respuesta fue del 74,5% (N = 199, 55,3% mujeres). Los análisis de regresión lineal mostraron que varios factores de hospitalización, sociales/interpersonales y personales se asociaron de manera estadísticamente significativa con la ansiedad social. El análisis de ruta mostró que el modelo propuesto se ajustaba bien a los datos (χ2 (df) = 3.196 (3), p = .362, CFI = .999, NNFI = .996, RMSEA = .018). El estigma internalizado medió completamente la asociación entre discriminación/apoyo social percibido y ansiedad social, mientras que medió parcialmente la asociación entre el estigma percibido de afiliados y ansiedad social.
Conclusiones: Los resultados sugieren que los factores sociales/interpersonales y personales tienen una asociación más fuerte con la ansiedad social que los factores de hospitalización y resaltan la importancia del estigma internalizado en la comprensión de los mecanismos de estas relaciones. Los psicólogos clínicos pueden referirse a estos factores psicosociales modificables para desarrollar intervenciones eficientes para la promoción de la salud mental.
PALABRAS CLAVE: Sobreviviente de COVID-19, hospitalización, ansiedad social, factores psicosociales, estrés minoritario, China
Short abstract
研究背景: 新型冠状病毒肺炎作为一种具有人传人特征的高传染性疾病, 在公众中一度引起了较大恐慌。感染过该疾病的康复者往往会被内在污名化, 甚至可能遭受歧视, 因而很可能会顾虑人际交往, 进而产生社交焦虑。
研究目的: 本研究通过调查住院治疗经历, 人际社交因素, 个人因素与社交焦虑之间的关系, 揭示出新型冠状病毒肺炎幸存者在康复后的社交焦虑形成机制。
研究方法: 本研究基于一项横断面调查, 以电话访谈的形式于2020年7月至9月进行, 在中国五个城市 (武汉, 南宁, 深圳, 珠海和东莞) 对新冠病毒肺炎幸存者进行出院半年的随访调查, 形成了一个多中心研究。招募对象为成年的新冠病毒肺炎幸存者。分析方法采用线性回归模型以及基于少数群体压力模型的路径分析, 探讨住院, 人际社交因素, 个人因素与社交焦虑之间的关联机制。
分析结果: 受访者的应答率为 74.5% (获得的样本量为 199,其中女性占 55.3%) 。线性回归分析表明, 各种住院相关因素, 人际社交因素及个人因素均与社交焦虑显著相关。路径分析模型的数据拟合较好 (χ2(df) = 3.196(3), p= .362, CFI = .999, NNFI = .996, RMSEA = .018) 。内在化的污名在歧视感知与社交焦虑, 以及社会支持与社交焦虑的关系中承担完全中介效应, 在连带污名与社交焦虑之间承担局部中介效应。
结论: 研究结果表明, 人际社交和个人因素与社交焦虑存在相关性, 相对而言比住院因素与社交焦虑的相关性更强, 这强调了内在化的污名对理解这些关系的潜在形成机制的重要性。临床心理医生可以利用这些可改变的心理社会因素, 制定出高效的干预措施来促进心理健康。
关键词: 新冠康复者, 住院经历, 社交焦虑, 心理社会因素, 少数群体压力, 中国
As a worldwide pandemic lasting for more than one year, coronavirus disease 2019 (COVID-19) became a public health emergency of international concern (WHO, 2020). Its significant mental health consequences, such as psychological stress (Olashore, Akanni, Fela-Thomas, & Khutsafalo, 2021) and sleep problems (Alimoradi et al., 2021), on the general population have been well documented. Infection and hospitalization experiences are believed to substantially increase traumatic stress, which may adversely affect not only mental health but also social functioning among survivors (D. Liu et al., 2020; Mazza et al., 2020). In light of the evidence that trauma and infectious diseases play significant roles in the development of social anxiety (Kuo, Goldin, Werner, Heimberg, & Gross, 2011; Michail & Birchwood, 2014), social anxiety may be prevalent among COVID-19 survivors. However, we did not identify any studies on social anxiety in this population.
Social anxiety is typically defined as anxiety about being judged or evaluated by others (Kessler et al., 2005; Schneier, Johnson, Hornig, Liebowitz, & Weissman, 1992). With a lifetime prevalence of 13.3%, it is the third most common psychiatric disorder after depression (17%) and alcohol dependence (14%) (Kessler et al., 1994). It is well established that social anxiety is significantly associated with a range of mental disorders and behavioural problems among people with infectious diseases, such as acquired immunodeficiency syndrome (AIDS) (Hart, James, Purcell, & Farber, 2008). Therefore, we consider that social anxiety may be especially relevant in understanding social life and health among COVID-19 survivors, as public discrimination and stigma towards these individuals are not uncommon. This study investigated social anxiety as a mental health consequence of stigmatization among people who had been hospitalized for diagnosed COVID-19 and then discharged in China. Our analyses focused on a comprehensive set of factors that are potentially associated with social anxiety.
1. Hospitalization experience and social anxiety
The first set of potential predictors of social anxiety in COVID-19 survivors is hospitalization experience. Several hospitalization-related causes of mental distress, including severity of COVID-19 symptoms at admission, negative experiences and pain during treatment, can be expected. For example, treatment for COVID-19 (e.g. in the intensive care unit-ICU) may induce extreme stress, manifesting in patients’ fear of death from life-threatening symptoms, pain from medical interventions, limited ability to communicate, and feelings of loss of control (Shaw et al., 2009; Twigg, Humphris, Jones, Bramwell, & Griffiths, 2008). COVID-19 patients may also feel lonely and isolated and have adjustment issues during admission to the hospital (Patil, Datar, Shetty, & Naphade, 2021). These negative experiences might lead to or exacerbate social anxiety in COVID-19 survivors for several reasons. Primarily, poor physical health status has been linked to social worth, social competence, and thus social anxiety (Jackson & Cunningham, 2015; Jaremka & Pacanowski, 2019). In addition, traumatic experiences during hospitalization have been linked to stress resistance and negative stress coping (Guzmán-Parra et al., 2019), which may leave persons vulnerable to social anxiety.
2. Social/interpersonal factors and social anxiety
The second set of factors as potential causes of social anxiety in the survivors includes social/interpersonal factors, such as perceived discrimination, perceived affiliate stigma, and social support. Stigma and discrimination are likely the consequences of multiple socioecological drivers, such as fear associated with infection or quarantine, misinformation, the infodemic (i.e. excessive circulation of misinformation), and blame of oneself or others for contracting the disease (Logie, 2020). As COVID-19 has caused panic among the general public, survivors may experience negative treatment from others, such as refusal of housing, verbal abuse or gossip, and social devaluation, which is referred to as discrimination or public stigma (Ransing et al., 2020). Additionally, survivors may perceive that due to their previous identity as a patient with COVID-19, even their family members experience negative treatment or socially withdraw (i.e. perceived affiliate stigma) (Chiu, Yang, Wong, & Li, 2015).
We hypothesized that such stigma-related experiences during interactions with others might lead to social anxiety, given that stigma has been found to result in social avoidance, anticipated humiliation (Birchwood et al., 2007), poor life satisfaction, and low self-efficacy (Wright, Gronfein, & Owens, 2000; Yanos, Rosenfield, & Horwitz, 2001). Some studies have tested the association between perceived discrimination and mental health problems in COVID-19 survivors (D. Liu et al., 2020). However, no studies have investigated the association between perceived discrimination/perceived affiliate stigma and social anxiety in this population. In addition, social support is potentially important as a protective factor of mental health and social well-being. We identified four studies investigating the association between social support and mental health among COVID-19 patients (Cai et al., 2020; Dong et al., 2020; Qi et al., 2020; Sun et al., 2020). However, none of them investigated social anxiety as a mental health outcome.
3. Internalized stigma and social anxiety
The third type of factor of social anxiety is related to self-perceptions of COVID-19 survivors. Previous work has demonstrated that those who have experienced infectious disease may endorse negative reactions from the public, devalue themselves, and socially withdraw, which is referred to as internalized stigma or self-stigma (Yang, Mak, Ho, & Chidgey, 2017). People who have been subjected to stigma and subsequently internalized it are more likely to be reluctant to seek social communication and experience shame and self-doubt (Sahoo et al., 2020). A fear and avoidance of interpersonal situations would also increase their risk of social anxiety (Stein & Stein, 2008). Moreover, self-stigma has been found to be related to some significant predictors of social anxiety and social well-being, such as low self-esteem, self-efficacy, perceived social worth and a high rate of overall psychopathology (Lysaker, Yanos, Outcalt, & Roe, 2010). We anticipated that internalized stigma might exacerbate social anxiety, as studies have suggested that internalized stigma can lead to social avoidance among persons with mental illness (Cassano, Pini, Saettoni, Rucci, & Dell’Osso, 1998). However, no studies have yet investigated internalized stigma or its association with social anxiety among COVID-19 survivors.
Furthermore, internalized stigma may play a mediating role in explaining the associations between hospitalization/interpersonal factors and social anxiety. According to the minority stress model, external stress, such as discrimination from the public, is distal minority stress, while internalized stigma is proximal minority stress (Meyer, 2003). Based on Meyer (2003), proximal stress stems from the negative self-regard developed by minority individuals in response to negative societal attitudes directed towards them; internalized sigma is one of the most adverse consequences of being socially excluded and discriminated against. Therefore, external stress, such as hospitalization experience and interpersonal experience due to the COVID-19 patient/survivor identity, would lead to negative self-perceptions such as internalized stigma, which in turn may give rise to social anxiety symptoms. However, we have not identified any study testing such a mediating effect of internalized stigma.
4. The present study
Based on this literature review, the study aimed to investigate the abovementioned potential factors of social anxiety among COVID-19 survivors. In particular, the potential factors were related to clinical records and experiences during hospitalization (e.g. severity of COVID-19 symptoms, treatment), social/interpersonal (e.g. perceived discrimination, perceived affiliate stigma, social support) and personal variables (e.g. internalized stigma) that increase the level of social anxiety. We hypothesized that negative experiences regarding hospitalization, perceived discrimination, perceived affiliate stigma, and internalized stigma would be positively associated with social anxiety, while social support would be negatively associated with it. In addition to the associations of these factors with social anxiety, their interrelationships were further investigated based on the minority stress model. We hypothesized that hospitalization and interpersonal factors would be associated with personal factors (internalized stigma), which in turn might raise the level of social anxiety.
5. Methods
5.1. Study design and data collection
The data set was collected from a cross-sectional survey among COVID-19 survivors with different infection severities at the six-month follow-up after hospital treatment. The survivors were interviewed by telephone due to epidemic prevention and privacy protection efforts, and the study was conducted from July to September 2020. The study sites were conveniently selected, including five hospitals located in five Chinese cities (i.e. Wuhan, Nanning, Shenzhen, Zhuhai, and Dongguan). Wuhan, the capital city of Hubei Province, was the epicentre of the COVID-19 outbreak and was the most affected by the pandemic in China. Shenzhen, Zhuhai, and Dongguan constitute a city cluster that is an important component of the Guangdong-Hong Kong-Macao Greater Bay Area (GBA). These regions contained the second largest proportion of COVID-19 cases of the whole country. Nanning is the capital city of Guangxi Province in the mountainous southern region, where the economy is relatively underdeveloped. It is a second-tier city, and it was less affected by the COVID-19 pandemic. Thus, a multicenter study was formed with different types of areas in terms of both the epidemic situation and economic development.
Participants were adult survivors who had been discharged from hospitals from February 1 to 30 April 2020. According to the treatment guidelines in China, COVID-19 survivors need to have 14-day centralized quarantine and 14-day home quarantine after hospital discharge. The contact information of the survivors was collected by the hospitals for follow-up health care services. Medical staff in the five participating hospitals assisted with recruitment by contacting all discharged COVID-19 patients listed in registries by telephone. The staff screened prospective participants based on their eligibility to join the study, briefed them about the purpose and logistics of the survey, and invited them to complete a telephone interview. In practice, the response rate may have been improved since the survivors were informed in advance; in addition, telephone interviews were more favourable for the survivors’ privacy and psychological safety than face-to-face interviews (Wang, Fu, Ju, Xiao, & Zou, 2021). At the appointed time, interviewers conducted the telephone interview, which took approximately 35 minutes to complete. Verbal consent was obtained before the telephone interview. The participants were assured that identifiable information would be kept confidential and that refusal to participate would not influence their right to use any services. No incentive was provided to the participants. Ethics approval was obtained based on our full respect for survivors’ privacy and strict observance of epidemic prevention regulations.
6.
5.2. Development of the questionnaire
A panel consisting of one epidemiologist, two public health researchers, a health psychologist, and a clinician was formed to develop the questionnaire for the current study.
6. Measures
6.1. Background and prehospitalization variables
The background information of participants included age, sex, permanent resident status, highest education level, marital relationship status, monthly personal income, employment status, and whether they had children. Participants were also asked to report whether they received a diagnosis of any chronic diseases (i.e. hypertension, diabetes, cancers, and other chronic heart/lung/liver/renal diseases) before SARS-CoV-2 infection and whether they had family member(s) who had been infected with SARS-CoV-2 or died from infection. Information on help-seeking for mental health problems during and after hospitalization and whether patients received positive SARS-CoV-2 nucleic acid testing after discharge was also recorded.
6.2. Hospitalization variables
Participants’ information about the clinical classification of COVID-19 at hospital admission, days of hospital stay, ICU admission, use of invasive ventilation and corticosteroid therapy, and presence of severe complications of COVID-19 were extracted from their medical records. The survey also assessed their experiences of witnessing painful symptoms and death of other COVID-19 patients staying in the same ward.
6.3. Social/interpersonal variables
Social support was measured by four questions to quantify the extent of emotional and instrumental (e.g. financial) support received from family and friends (Yang et al., 2020). Items were rated on a 10-point Likert scale ranging from 0 (none) to 10 (tremendous). The scale had good reliability in the current sample (Cronbach’s alpha = .80). Perceived discrimination was measured by nine questions asking whether the participants experienced any negative treatment after discharge, including being fired, being treated unfairly, and being socially excluded by family members, colleagues, and the community (0 = no and 1 = yes; Cronbach’s alpha = .69). Perceived affiliate stigma was measured by seven questions assessing the extent to which the survivors perceived their family members endorsing and internalizing COVID-19 stigma (1 = strongly disagree to 4 = strongly agree). The scale had excellent reliability in the current sample (Cronbach’s alpha = .94).
6.4. Personal variables
Internalized stigma was characterized by the Self-Stigma Scale (Mak & Cheung, 2010). The scale was originally developed among mental health consumers and has been used in the context of infectious diseases. We adapted the scale to the COVID-19 context by replacing ‘mental health consumers’ with ‘SARS-CoV-2’. A sample item is ‘I fear that others would know that I was infected with SARS-Cov-2’. Items were rated on a Likert scale from 1 (strongly disagree) to 4 (strongly agree). The Cronbach’s alpha was .94 in the current sample.
6.5. Outcomes
Social anxiety was defined according to the Chinese version of the social anxiety subscale of the Self-consciousness Scale (Scheier & Carver, 1985; Shek, 1994). The scale has been found to be associated with many mental disorders, such as social phobia and major depression (Hope & Heimberg, 1988; Takishima-Lacasa, Higa-mcmillan, Ebesutani, Smith, & Chorpita, 2014). No cut-off point has been reported, and it is not intended for making clinical diagnoses. It tests individuals’ negative feelings during social interactions (e.g. ‘Large groups make me nervous.’) Participants rated the items on 5-point Likert scales, ranging from 1 (does not apply to me at all) to 5 (applies to me very much). A higher score reflects a higher level of social anxiety. The Cronbach’s alpha was .90 in the present study.
7. Statistical analysis
Descriptive statistics were computed for both background and psychosocial variables. Using univariate linear regression analyses, we tested the associations of these variables with social anxiety. Standardized regression coefficients (β) and 95% confidence intervals (CIs) were reported. The significant variables are shown in the table and included in further analyses to identify the mechanism of social anxiety. Path analysis examined the hypothesized directionality of relationships among the constructs and the overall fit of the model. Mediation effects of internalized stigma were tested by bootstrapping analyses. The 95% CIs of indirect effects were obtained from 5000 bootstrap resamples. The level of statistical significance was .05. SPSS version 24.0 and AMOS were used for data analyses.
8. Results
Of the 317 recovered COVID-19 patients discharged from the selected hospitals, 27 were under 18 years old, 22 changed their telephone numbers and one died in a car accident. The remaining 267 eligible patients were contacted by the research team, and 68 of them refused to participate in the study due to lack of time. Finally, 199 eligible patients provided consent and completed the telephone survey. The response rate was 74.5%, specifically 63.3% (31 of 49) in Wuhan, 76.0% (38 of 50) in Shenzhen, 76.5% (39 of 51) in Zhuhai, 77.8% (35 of 45) in Dongguan, and 77.8% (56 of 72) in Nanning.
Table 1 presents the summary statistics of all variables used in the analyses. Among all 199 survivors ranging in age from 18 to 86, over half of them were 50 years old or below (63.8%, n = 127) and female (53.3%, n = 106). Most of the participants were married or cohabiting with a partner (81.9%, n = 163) and had at least one child (80.4%, n = 160). More than half had not attained tertiary education (55.3%, n = 110), and close to 60% did not have full-time work (59.8%, n = 119). Over 73% had no permanent residency in the city where they were hospitalized (73.4%, n = 146) and had personal income less than ¥6,000 per month (74.4%, n = 148). Regarding infection experience, 44.7% (n = 89) of participants reported having at least one family member infected with SARS-CoV-2, and 1.5% (n = 3) had family members who had died from infection. Nearly all of the participants had no ICU experience during the treatment (97.5%).
Table 1.
Background characteristics, somatic and psychosocial status of the participants (n = 199)
| Background characteristics | n | % | Mean | SD |
|---|---|---|---|---|
| Sex | ||||
| Male | 93 | 46.7 | ||
| Female | 106 | 53.3 | ||
| Age group (years) | 42.72 | 17.53 | ||
| 18–30 | 33 | 16.6 | ||
| 31–40 | 59 | 29.6 | ||
| 41–50 | 35 | 17.6 | ||
| 51–60 | 33 | 16.6 | ||
| >60 | 39 | 19.6 | ||
| Highest education attained | ||||
| Middle school or below | 53 | 26.6 | ||
| High school | 57 | 28.7 | ||
| College and above | 86 | 43.2 | ||
| Refuse to disclose | 3 | 1.5 | ||
| Relationship status | ||||
| Currently single | 36 | 18.1 | ||
| Married/cohabited with a partner | 163 | 81.9 | ||
| Having children | ||||
| No | 39 | 19.6 | ||
| Yes | 160 | 80.4 | ||
| Permanent residents of the city | ||||
| No | 146 | 73.4 | ||
| Yes | 53 | 26.6 | ||
| Employment status | ||||
| Full-time employment | 80 | 40.2 | ||
| Free-lanced | 31 | 16.1 | ||
| Students | 15 | 7.5 | ||
| Unemployed | 17 | 8.5 | ||
| Retired | 55 | 27.6 | ||
| Monthly personal income (¥) | ||||
| No fixed income | 71 | 35.7 | ||
| <3,000 | 25 | 12.6 | ||
| 3,000–5,999 | 52 | 26.1 | ||
| 6,000–9,999 | 24 | 12.1 | ||
| ≥10,000 | 27 | 13.6 | ||
| Diagnosis of any chronic diseases before infection | 67 | 33.7 | ||
| Having at least one family member infected with SARS-Cov-2 | 89 | 44.7 | ||
| Having a family member died of COVID-19 | 3 | 1.5 | ||
| Receiving positive SARS-Cov-2 nucleic acid testing results | 7 | 3.5 | ||
| Help-seeking for mental health problems during hospitalization | 85 | 42.7 | ||
| Help-seeking for mental health problems after discharge | 44 | 22.1 | ||
| Hospitalization variables | ||||
| Clinical classification of COVID-19 at entry | ||||
| Asymptomatic | 3 | 1.5 | ||
| Mild | 42 | 21.1 | ||
| Common | 111 | 55.8 | ||
| Severe | 25 | 12.6 | ||
| Critically severe | 18 | 9.0 | ||
| ICU (No) | 194 | 97.5 | ||
| Invasive assisted ventilation (No) | 192 | 96.5 | ||
| Hormone therapy (No) | 175 | 87.9 | ||
| Serious complications (No) | 188 | 94.5 | ||
| Length of stay (days) | 20.88 | 15.83 | ||
| Sequelae of COVID-19 before discharge | 12 | 6.0 | ||
| Social/interpersonal variables | ||||
| Social support | 28.05 | 9.61 | ||
| Perceived discrimination | 1.72 | 1.84 | ||
| Perceived affiliate stigma | 13.80 | 5.48 | ||
| Personal variable | ||||
| Internalized stigma | 18.22 | 6.89 | ||
| Outcome variable | ||||
| Social anxiety | 12.07 | 4.73 |
Table 2 presents the significant correlates of social anxiety. Sex, whether one had children, monthly personal income, clinical classification of COVID-19, positive SARS-CoV-2 nucleic acid testing, perceived discrimination, perceived affiliate stigma, social support, and internalized stigma were significantly associated with social anxiety (p < .050). Specifically, females and those with children were more likely to develop social anxiety than their counterparts. Clinical classification of COVID-19 and most of the posthospitalization variables were risk factors for social anxiety. Only the median level of monthly personal income and social support were protective factors negatively associated with social anxiety.
Table 2.
Associations between background/independent variables and social anxiety
| Background characteristics | Social Anxiety |
|
|---|---|---|
| β (95% CI) | p | |
| Sex | ||
| Male | ref | |
| Female | .209 | .003 |
| (.681, 3.279) | ||
| Having children | ||
| No | ref | |
| Yes | .154 | .029 |
| (.186, 3.485) | ||
| Monthly personal income (¥) | ||
| No fixed income | ref | |
| <3,000 | −.031 | .682 |
| (−2.600, 1.705) | ||
| 3,000–5,999 | −.195 | .015 |
| (−3.788, −.410) | ||
| 6,000–9,999 | −.012 | .872 |
| (−2.364, 2.006) | ||
| ≥10,000 | −.105 | .175 |
| (−3.535, .650) | ||
| Receiving positive SARS-Cov-2 nucleic acid testing results | .188 | .008 |
| (1.285, 8.352) | ||
| Hospitalization variables | ||
| Clinical classification of COVID-19 at entry | ||
| Asymptomatic | ref | |
| Mild | .371 | .125 |
| (−1.197, 9.768) | ||
| Common | .651 | .024 |
| (.812, 11.548) | ||
| Severe | .466 | .021 |
| (1.021, 12.232) | ||
| Critically severe | .368 | .038 |
| (.335, 11.777) | ||
| Social/interpersonal variables | ||
| Perceived discrimination | .411 | <.001 |
| (.710, 1.355) | ||
| Perceived affiliate stigma | .453 | <.001 |
| (.284, .500) | ||
| Social support | −.245 | <.001 |
| (−.187, −.053) | ||
| Personal variable | ||
| Internalized stigma | .578 | <.001 |
| (.319, .477) | ||
Figure 1 presents the proposed mediation model of social anxiety. The model showed excellent model fit, χ2(df) = 3.196(3), p = .362, CFI = .999, NNFI = .996, RMSEA = .018. Only social support was significantly negatively associated with internalized stigma. The association of the clinical classification of COVID-19 at admission with internalized stigma was marginally significant (B = .810, β = .103, p = .055). Internalized stigma was positively associated with social anxiety (B = .294, β = .427, p < .001). Regarding the direct effect on social anxiety, only the effect of perceived affiliate stigma was significant (B = .172, β = .200, p = .003), while the effect of perceived discrimination was marginally significant (B = .318, β = .127, p = .052). The indirect effects of perceived discrimination (B = .296, β = .118, 95% CI = .080 ~ .183, p = .006), perceived affiliate stigma (B = .116, β = .135, 95% CI = .076 ~ .222, p = .005), and social support (B = −.005, β = −.113, 95% CI = −.189~-.063, p = .007) on social anxiety through internalized stigma were significant. The indirect effect of the clinical classification of COVID-19 at admission through internalized stigma was marginally significant (B = .238, β = .044, 95% CI = .005 ~ .097, p = .074).
Figure 1.
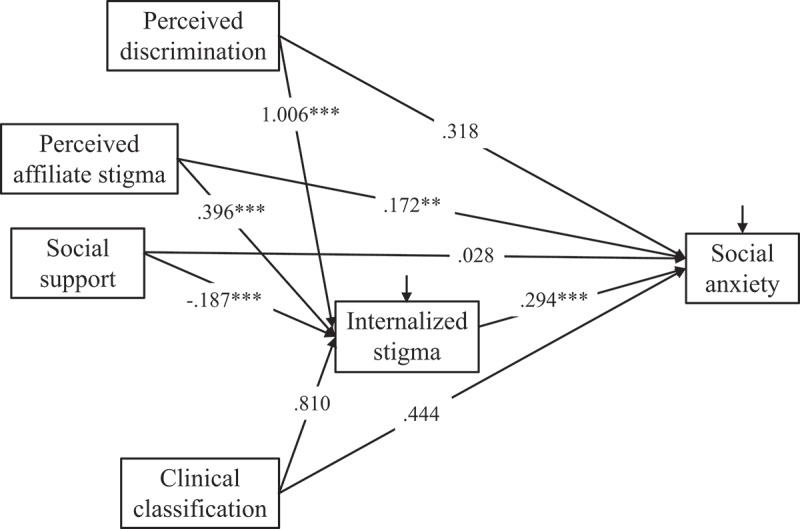
The mediation model of social anxiety.
Path analysis was performed (χ2(df) = 3.196(3), p = .362, CFI = .999, NNFI = .996, RMSEA = .018). Unstandardized path coefficients (B) are presented. The covariances between interpersonal factors (i.e. perceived discrimination, perceived affiliate stigma, and social support) are not shown for simplicity. *p < .05, **p < .01, ***p < .001.
9. Discussion
The COVID-19 pandemic is a traumatic event and may lead to severe and long-term consequences on mental health, quality of life and well-being, particularly for survivors. As part of this emerging picture, this study provides preliminary evidence regarding social well-being-related consequences. To the best of our knowledge, this is the first study aimed at exploring social anxiety and its potential factors (i.e. sociodemographic, hospitalization-related, social/interpersonal and personal variables) among COVID-19 survivors. It is also the first study investigating internalized stigma, which is easily neglected as a potential form of traumatic stress in the COVID-19 pandemic. In general, the results support our hypotheses.
Being female, having children, having lower income, and receiving positive results of SARS-CoV-2 nucleic acid testing were significant background and risk factors for social anxiety. This may be because individuals belonging these groups tend to have lower social capital or coping resources and experience multiple daily life stresses, thus experiencing more negative emotions and social anxiety than their counterparts. These results may also be explained by intersectionality theory (Crenshaw, 1989), which suggests that marginalized individuals often have multiple minority identities (e.g. being female and being infected with SARS-CoV-2) and are especially vulnerable to stress and mental health problems. To test this assumption, subgroup analyses and comparison studies that included both COVID-19 survivors and those who did not suffer from COVID-19 would be key approaches for future research.
Consistent with the initial predictions, high levels of severity of COVID-19 at admission, low social support, high perceived discrimination, high perceived affiliate stigma, and high internalized stigma were potential factors of social anxiety among COVID-19 survivors. Severe symptoms, poor physical health status and unfavourable self-perceptions due to the identity of COVID-19 survivors can be personal sources of stress (Guo et al., 2020), and perceptions related to the negative experiences of their family members and unsupportive social environment are social and interpersonal sources of stress (H. Liu et al., 2020). These factors may further reduce one’s coping resources as well as perceived and actual social competence, thus increasing one’s social anxiety. These results are consistent with the findings in other minority populations, such as people living with HIV (Chan & Mak, 2019). However, unlike other stigmatizing conditions, COVID-19 has recently emerged and is still underexamined. A number of questions have yet to be addressed to better understand the experiences and consequences of COVID-19-related symptoms, stigma, and social well-being impact. For example, questions remain regarding whether the condition of COVID-19 is more stigmatizing (e.g. causing more stigmatized reactions from the public and the patients) than other infectious diseases (e.g. AIDS) and other types of stigmatizing conditions (e.g. race and sexual minority identity) and whether such a condition will have lasting effects on survivors’ self-identity, social treatment (e.g. discrimination and social status loss), social interactions (e.g. identity concealment) and social well-being (e.g. social anxiety) (Pieterse, Todd, Neville, & Carter, 2012).
Furthermore, we found that internalized stigma significantly mediated the relationships of COVID-19 symptoms, perceived discrimination, perceived affiliate stigma, and social support with social anxiety. This finding suggests that the self-internalization process is a key underlying mechanism that explains how symptoms and social/interpersonal factors may affect social well-being among COVID-19 survivors. More specifically, the full mediating effects operating in the associations of COVID-19 symptoms, perceived discrimination, and social support with social anxiety highlight the role of internalized stigma and suggest that COVID-19 symptoms and related social/interpersonal experiences would have significant effects only when they induce negative self-perceptions or adversely affect the self-identity of survivors. According to the findings in other disease groups (Drewes, Langer, Ebert, Kleiber, & Gusy, 2020), such a negative self-identity or self-perception may be continuous and have a lasting effect on survivors even after they have recovered or even when the COVID-19 pandemic and related discrimination from the public have ended. On the other hand, the partial mediating effect of internalized stigma on the relationship between perceived affiliate stigma and social anxiety suggests that other mediators (e.g. status and reactions in interpersonal dimensions) may also exist and explain this relationship. For example, the perceived affiliate stigma of survivors may reduce relationship quality and negatively affect interaction with family members, which may in turn increase their social anxiety. These potential mediators need to be tested in future work.
The mediating effects found in the study have both theoretical and practical implications. Theoretically, the results provide preliminary support for applying the minority stress model (Meyer, 2015) to understand social well-being and the development of social anxiety and other mental health problems, such as depression and posttraumatic stress disorder, among COVID-19 survivors. Other types of minority stress, such as anticipated stigma, may also be applicable and should be explored in future work. Attribution theory (Jones & Davis, 1965) is another important theory to understand the internalization process of stigma, suggesting that people with internal attributions for a stigmatizing condition (e.g. did not actively adopt preventive measures against COVID-19) are more likely to endorse related stigma than those with external attributions. Qualitative studies are needed, which could potentially provide a better understanding of the attributions of COVID-19 infection among survivors. In addition, it is practically important to explore psychological mediators, as they can be modified through personal efforts and psychological interventions. For example, cognitive behavioural therapy (CBT) may be useful to enhance awareness of how COVID-19-related stress affects self-perception and social well-being, facilitate cognitive restructuring and positive self-affirmation, and develop adaptive stress coping skills. Resilience enhancement and self-empowerment training may also benefit survivors by reducing self-blame and self-stigma. Interventions on social and interpersonal factors may require more efforts from multiple stakeholders and take longer to take effect. Enhancing governmental support, reducing fear, blame and discrimination towards survivors, and advocating social equality at the community level may be a good start and be more effective in collectivist cultures, such as Chinese cultures, in which social cohesion is valued. Finally, it is suggested to better understand and intervene in the potential modifiable moderators (e.g. resilience) between COVID-19 symptom severity and mental/social health outcomes.
This study has several limitations. First, the study had a relatively small sample size for path analysis, and the participants were recruited from only five cities in China. Future studies should validate the model with a large sample size. Generalization of the findings to other geographic locations should be performed cautiously. Second, this study used a cross-sectional study design, which limits causal inference. Third, we were not able to collect information on the survivors who refused to participate in the study. Those who refused to participate in the survey may have had different characteristics (e.g. living in rural areas) from the participants. Thus, selection bias might exist. Fourth, most of the measures (except the hospitalization-related factors) were self-reported and might be susceptible to recall bias. Moreover, the measure of social anxiety used in this study is not a diagnostic tool and does not have a cut-off. Thus, the proportion of individuals with clinically diagnosed social anxiety disorder in this population remains unknown. Finally, we did not have records of participants’ mental health status before and during their hospitalization. This is a significant limitation, as mental health status prior to recovery from COVID-19 could also be a significant risk factor for social anxiety (Blanco et al., 2011).
Supplementary Material
Acknowledgments
We are grateful to Yusheng Jie for his support on study design. And we thank Qishu Huang and Yuxi Li for sparing some time to make preparations for the survey. We also give thanks to Tanwei Yuan and Yiguo Zhou who provided assistance in formatting citations.
Funding Statement
This study was supported by the Natural Science Foundation of China Excellent Young Scientists Fund [82022064], Natural Science Foundation of China International/Regional Research Collaboration Project [72061137001], Natural Science Foundation of China Young Scientist Fund [81703278], the Australian National Health and Medical Research Commission (NHMRC) Early Career Fellowship [APP1092621], the High Level Project of Medicine in Longhua, Shenzhen [HLPM201907020105], the National Key Research and Development Program of China [2020YFC0840900], and Guangxi Medical and Health Appropriate Technology Development and Application Project [S2020124]. All funding parties did not have any role in the design of the study or in the explanation of the data.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability
The raw data are not publicly available due to national epidemic prevention and privacy policies.
Ethics approval
Ethics approval was obtained from the Sun Yat-sen University (Shenzhen) (Ref#2020-031).
Supplementary material
Supplemental data for this article can be accessed here.
References
- Alimoradi, Z., Broström, A., Tsang, H. W. H., Griffiths, M. D., Haghayegh, S., Ohayon, M. M., … Pakpour, A. H. (2021). Sleep problems during COVID-19 pandemic and its’ association to psychological distress: A systematic review and meta-analysis. EClinicalMedicine, 36, 100916. doi: 10.1016/j.eclinm.2021.100916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birchwood, M., Trower, P., Brunet, K., Gilbert, P., Iqbal, Z., & Jackson, C. (2007). Social anxiety and the shame of psychosis: A study in first episode psychosis. Behaviour Research and Therapy, 45(5), 1025–11. doi: 10.1016/j.brat.2006.07.011 [DOI] [PubMed] [Google Scholar]
- Blanco, C., Xu, Y., Schneier, F. R., Okuda, M., Liu, S. M., & Heimberg, R. G. (2011). Predictors of persistence of social anxiety disorder: A national study. Journal of Psychiatric Research, 45(12), 1557–1563. doi: 10.1016/j.jpsychires.2011.08.004 [DOI] [PubMed] [Google Scholar]
- Cai, X., Hu, X., Ekumi, I. O., Wang, J., An, Y., Li, Z., & Yuan, B. (2020). Psychological distress and its correlates among COVID-19 survivors during early convalescence across age groups. The American Journal of Geriatric Psychiatry, 28(10), 1030–1039. doi: 10.1016/j.jagp.2020.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassano, G. B., Pini, S., Saettoni, M., Rucci, P., & Dell’Osso, L. (1998). Occurrence and clinical correlates of psychiatric comorbidity in patients with psychotic disorders. The Journal of Clinical Psychiatry, 59(2), 60–68. doi: 10.4088/jcp.v59n0204 [DOI] [PubMed] [Google Scholar]
- Chan, R. C. H., & Mak, W. W. S. (2019). Cognitive, regulatory, and interpersonal mechanisms of HIV stigma on the mental and social health of men who have sex with men living with HIV. American Journal of Men’s Health, 13(5), 1557988319873778. doi: 10.1177/1557988319873778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu, M. Y., Yang, X., Wong, H. T., & Li, J. H. (2015). The mediating effect of affective stigma between face concern and general mental health - The case of Chinese caregivers of children with intellectual disability. Research in Developmental Disabilities, 36, 437–446. doi: 10.1016/j.ridd.2014.10.024 [DOI] [PubMed] [Google Scholar]
- Crenshaw, K. (1989). Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum, 1989(1), 29, Article 8. Retrieved from http://chicagounbound.uchicago.edu/uclf/vol1989/iss1/8 [Google Scholar]
- Dong, Y. C., Su, T., Jiao, P. Q., Kong, X. Y., Zheng, K. L., Tang, M., … Wu, S. X. (2020). Prevalence and factors associated with depression and anxiety of hospitalized patients with COVID-19. medRxiv. doi: 10.1101/2020.03.24.20043075 [DOI] [Google Scholar]
- Drewes, J., Langer, P. C., Ebert, J., Kleiber, D., & Gusy, B. (2020). Associations between experienced and internalized HIV stigma, adversarial growth, and health outcomes in a nationwide sample of people aging with HIV in Germany. AIDS and Behavior, 25(4), 1037–1046. doi: 10.1007/s10461-020-03061-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo, Q., Zheng, Y., Shi, J., Wang, J., Li, G., Li, C., … Yang, Z. (2020). Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: A mixed-method study. Brain, Behavior, and Immunity, 88, 17–27. doi: 10.1016/j.bbi.2020.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guzmán-Parra, J., Aguilera-Serrano, C., García-Sanchez, J. A., García-Spínola, E., Torres-Campos, D., Villagrán, J. M., … Mayoral-Cleries, F. (2019). Experience coercion, post-traumatic stress, and satisfaction with treatment associated with different coercive measures during psychiatric hospitalization. International Journal of Mental Health Nursing, 28(2), 448–456. doi: 10.1111/inm.12546 [DOI] [PubMed] [Google Scholar]
- Hart, T. A., James, C. A., Purcell, D. W., & Farber, E. (2008). Social anxiety and HIV transmission risk among HIV-seropositive male patients. AIDS Patient Care and STDs, 22(11), 879–886. doi: 10.1089/apc.2008.0085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hope, D. A., & Heimberg, R. G. (1988). Public and private self-consciousness and social phobia. Journal of Personality Assessment, 52(4), 626–639. doi: 10.1207/s15327752jpa5204_3 [DOI] [PubMed] [Google Scholar]
- Jackson, S. L., & Cunningham, S. A. (2015). Social competence and obesity in elementary school. American Journal of Public Health, 105(1), 153–158. doi: 10.2105/ajph.2014.302208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaremka, L. M., & Pacanowski, C. R. (2019). Social anxiety symptoms moderate the link between obesity and metabolic function. Psychoneuroendocrinology, 110, 104425. doi: 10.1016/j.psyneuen.2019.104425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, E. E., & Davis, K. E. (1965). From acts to dispositions: The attribution process in person perception. In Berkowitz L. (Ed.), Advances in experimental social psychology (Vol. 2, pp. 219–266). New York: Academic Press. doi: 10.1016/S0065-2601(08)60107-0 [DOI] [Google Scholar]
- Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. doi: 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Kessler, R. C., McGonagle, K. A., Zhao, S., Nelson, C. B., Hughes, M., Eshleman, S., … Kendler, K. S. (1994). Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the USA. Results from the National Comorbidity Survey. Archives of General Psychiatry, 51(1), 8–19. doi: 10.1001/archpsyc.1994.03950010008002 [DOI] [PubMed] [Google Scholar]
- Kuo, J. R., Goldin, P. R., Werner, K., Heimberg, R. G., & Gross, J. J. (2011). Childhood trauma and current psychological functioning in adults with social anxiety disorder. Journal of Anxiety Disorders, 25(4), 467–473. doi: 10.1016/j.janxdis.2010.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, D., Baumeister, R. F., Veilleux, J. C., Chen, C., Liu, W., Yue, Y., & Zhang, S. (2020). Risk factors associated with mental illness in hospital discharged patients infected with COVID-19 in Wuhan, China. Psychiatry Research, 292, 113297. doi: 10.1016/j.bbi.2020.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, H., Li, X., Chen, Q., Li, Y., Xie, C., Ye, M., & Huang, J. (2020). Illness perception, mood state and disease-related knowledge level of COVID-19 family clusters, Hunan, China. Brain, Behavior, and Immunity, 88, 30–31. doi: 10.1016/j.bbi.2020.05.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logie, C. H. (2020). Lessons learned from HIV can inform our approach to COVID-19 stigma. Journal of the International AIDS Society, 23(5), e25504. doi: 10.1089/apc.2008.0085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lysaker, P. H., Yanos, P. T., Outcalt, J., & Roe, D. (2010). Association of stigma, self-esteem, and symptoms with concurrent and prospective assessment of social anxiety in schizophrenia. Clinical Schizophrenia & Related Psychoses, 4(1), 41–48. doi: 10.3371/csrp.4.1.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak, W. W., & Cheung, R. Y. (2010). Self-stigma among concealable minorities in Hong Kong: Conceptualization and unified measurement. American Journal of Orthopsychiatry, 80(2), 267–281. doi: 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Mazza, M. G., De Lorenzo, R., Conte, C., Poletti, S., Vai, B., Bollettini, I., … Benedetti, F. (2020). Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain, Behavior, and Immunity, 89, 594–600. doi: 10.1016/j.janxdis.2010.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. doi: 10.1002/jia2.25504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer, I. H. (2015). Resilience in the study of minority stress and health of sexual and gender minorities. Psychology of Sexual Orientation and Gender Diversity, 2(3), 209–213. doi: 10.1037/sgd0000132 [DOI] [Google Scholar]
- Michail, M., & Birchwood, M. (2014). Social anxiety in first-episode psychosis: The role of childhood trauma and adult attachment. Journal of Affective Disorders, 163, 102–109. doi: 10.1037/0033-2909.129.5.674 [DOI] [PubMed] [Google Scholar]
- Olashore, A. A., Akanni, O. O., Fela-Thomas, A., & Khutsafalo, K. (2021). The psychological impact of COVID-19 on health-care workers in African Countries: A systematic review. Asian Journal of Social Health and Behavior, 4(3), 85–97. doi: 10.4103/shb.shb_32_21 [DOI] [Google Scholar]
- Patil, S. T., Datar, M. C., Shetty, J., & Naphade, N. (2021). Psychological consequences and coping strategies of patients undergoing treatment for COVID-19 at a tertiary care hospital: A qualitative study. Asian Journal of Social Health and Behavior, 4(2), 62–68. doi: 10.4103/shb.shb_5_21 [DOI] [Google Scholar]
- Pieterse, A. L., Todd, N. R., Neville, H. A., & Carter, R. T. (2012). Perceived racism and mental health among Black American adults: A meta-analytic review. Journal of Counseling Psychology, 59(1), 1–9. doi: 10.1037/a0026208 [DOI] [PubMed] [Google Scholar]
- Qi, R., Chen, W., Liu, S., Thompson, P. M., Zhang, L. J., Xia, F., … Lu, G. M. (2020). Psychological morbidities and fatigue in patients with confirmed COVID-19 during disease outbreak: Prevalence and associated biopsychosocial risk factors. medRxiv: The Preprint Server for Health Sciences. doi: 10.1037/a0026208 [DOI] [Google Scholar]
- Ransing, R., Ramalho, R., de Filippis, R., Ojeahere, M. I., Karaliuniene, R., Orsolini, L., … Adiukwu, F. (2020). Infectious disease outbreak related stigma and discrimination during the COVID-19 pandemic: Drivers, facilitators, manifestations, and outcomes across the world. Brain, Behavior, and Immunity, 89, 555–558. doi: 10.1101/2020.05.08.20031666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahoo, S., Mehra, A., Suri, V., Malhotra, P., Yaddanapudi, L. N., Dutt Puri, G., & Grover, S. (2020). Lived experiences of the Corona survivors (patients admitted in COVID wards): A narrative real-life documented summaries of internalized guilt, shame, stigma, anger. Asian Journal of Psychiatry, 53, 102187. doi: 10.1016/j.bbi.2020.07.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheier, M. F., & Carver, C. S. (1985). The self-consciousness scale: A revised version for use with general populations. Journal of Applied Social Psychology, 15(8), 687–699. doi: 10.1111/j.1559-1816.1985.tb02268.x [DOI] [Google Scholar]
- Schneier, F. R., Johnson, J., Hornig, C. D., Liebowitz, M. R., & Weissman, M. M. (1992). Social phobia. Comorbidity and morbidity in an epidemiologic sample. Archives of General Psychiatry, 49(4), 282–288. doi: 10.1001/archpsyc.1992.01820040034004 [DOI] [PubMed] [Google Scholar]
- Shaw, R. J., Harvey, J. E., Bernard, R., Gunary, R., Tiley, M., & Steiner, H. (2009). Comparison of short-term psychological outcomes of respiratory failure treated by either invasive or non-invasive ventilation. Psychosomatics, 50(6), 586–591. doi: 10.1016/s0033-3182(09)70860-6 [DOI] [PubMed] [Google Scholar]
- Shek, D. T. (1994). Assessment of private and public self-consciousness: A Chinese replication. Journal of Clinical Psychology, 50(3), 341–348. doi: [DOI] [PubMed] [Google Scholar]
- Stein, M. B., & Stein, D. J. (2008, Mar 29). Social anxiety disorder. The Lancet, 371(9618), 1115–1125. doi: 10.1016/s0140-6736(08)60488-2 [DOI] [PubMed] [Google Scholar]
- Sun, N., Wei, L., Wang, H., Wang, X., Gao, M., Hu, X., & Shi, S. (2020). Qualitative study of the psychological experience of COVID-19 patients during hospitalization. Journal of Affective Disorders, 278, 15–22. doi: 10.1016/j.jad.2020.08.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takishima-Lacasa, J. Y., Higa-mcmillan, C. K., Ebesutani, C., Smith, R. L., & Chorpita, B. F. (2014). Self-consciousness and social anxiety in youth: The revised self-consciousness scales for children. Psychological Assessment, 26(4), 1292–1306. doi: 10.1037/a0037386 [DOI] [PubMed] [Google Scholar]
- Twigg, E., Humphris, G., Jones, C., Bramwell, R., & Griffiths, R. D. (2008). Use of a screening questionnaire for post-traumatic stress disorder (PTSD) on a sample of UK ICU patients. Acta Anaesthesiologica Scandinavica, 52(2), 202–208. doi: 10.1111/j.1399-6576.2007.01531.x [DOI] [PubMed] [Google Scholar]
- Wang, B., Fu, L., Ju, N., Xiao, X., & Zou, H. (2021). Interviews to better understand the burden of mental health disease among COVID-19 survivors: Things to consider. Journal of Affective Disorders. doi: 10.1016/j.jad.2021.02.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . (2020, January 26). World Health Organization. WHO Director-General’s statement on IHR Emergency Committee on Novel Coronavirus (2019-nCoV). Retrieved from https://www.who.int/director-general/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov)
- Wright, E. R., Gronfein, W. P., & Owens, T. J. (2000). Deinstitutionalization, social rejection, and the self-esteem of former mental patients. Journal of Health and Social Behavior, 41(1), 68–90. doi: 10.2307/2676361 [DOI] [PubMed] [Google Scholar]
- Yang, X., Mak, W. W., Ho, C. Y., & Chidgey, A. (2017). Self-in-love versus self-in-stigma: Implications of relationship quality and love attitudes on self-stigma and mental health among HIV-positive men having sex with men. AIDS Care, 29(1), 132–136. doi: 10.1080/09540121.2016.1200714 [DOI] [PubMed] [Google Scholar]
- Yang, X., Wang, Q., Wang, X., Mo, P. K. H., Wang, Z., Lau, J. T. F., & Wang, L. (2020). Direct and indirect associations between interpersonal resources and posttraumatic growth through resilience among women living with HIV in China. AIDS and Behavior, 24(6), 1687–1700. doi: 10.1007/s10461-019-02694-3 [DOI] [PubMed] [Google Scholar]
- Yanos, P. T., Rosenfield, S., & Horwitz, A. V. (2001). Negative and supportive social interactions and quality of life among persons diagnosed with severe mental illness. Community Mental Health Journal, 37(5), 405–419. doi: 10.1023/a:1017528029127 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data are not publicly available due to national epidemic prevention and privacy policies.


