ABSTRACT
Background
Injury patients are at risk for mental health problems, which could result in slower recovery and affect health-related quality of life (HRQoL), health care utilization, and return to work (RTW).
Objective
In this study, we determined the prevalence of symptoms indicative of probable depression, anxiety, and post-traumatic stress disorder (PTSD) and their association with HRQoL, health care utilization, and RTW in adult injury patients.
Method
Data on unintentional injuries in adult patients were retrieved from the Dutch Injury Surveillance System (DISS) and a six-month follow-up questionnaire that included the Hospital Anxiety and Depression Scale (HADS) and Impact of Event Scale-Revised (IES-R) to assess depression, anxiety, and posttraumatic stress disorder (PTSD) symptoms, and items on HRQoL (measured with the EQ-5D-5 L and EQ visual analogue scale), health care utilization and RTW. Logistic regression analyses assessed the association between depression, anxiety, and PTSD and HRQoL, health care utilization, and RTW.
Results
At six months post-injury, 22% (n = 665/3060) of included patients had scores indicative of probable anxiety disorder (14%), depression (16%), and/or PTSD (6%). These patients had reduced EQ-5D utility scores [β: −0.26 (95% CI: −0.28, −0.23)] and were less likely to RTW [OR: 2.12 (95% CI: 1.34, 3.37)] compared to their counterparts. Both mental and physical health care utilization were significantly higher in patients with symptoms indicative of depression, anxiety, and/or PTSD.
Conclusions
In injury patients, there is a high occurrence of depression, anxiety, and PTSD symptoms, which is associated with lower HRQoL, higher health care utilization, and lower RTW rates. These results underline the importance of screening and treatment of these symptoms in this population to enhance good recovery of injury patients.
KEYWORDS: Mental health, injury, health-related quality of life, health care utilization, return to work
HIGHLIGHTS
Our results highlight the importance of mental health support in the injury patient population, the necessity of a multidimensional rehabilitation process, and the need to focus on multiple mental health disorders, in research and clinical settings.
Short abstract
Antecedentes: Los pacientes lesionados se encuentran en riesgo de desarrollar problemas de salud mental, los cuales podrían resultar en recuperación más lenta y podrían afectar la calidad de vida relacionada con la salud (HRQoL en sus siglas en inglés), la utilización de los servicios de salud, y el retorno al trabajo (RTW en sus siglas en inglés).
Objetivo: En este estudio, determinamos la prevalencia de síntomas indicativos de probable depresión, ansiedad y de trastorno de estrés postraumático (TEPT) y su asociación con la HRQoL, con la utilización de servicios de salud, y el RTW en pacientes adultos lesionados.
Método: Se recuperaron datos de pacientes adultos con lesiones no intencionales desde el Sistema Holandés de Vigilancia de Lesiones (DISS) y desde un cuestionario a los seis meses de seguimiento que incluyó la Escala Hospitalaria de Ansiedad y Depresión (HADS) y la Escala -revisada- del Impacto del Evento (IES-R) para evaluar síntomas de depresión, ansiedad y estrés postraumático (TEPT), también ítems sobre HRQoL (medida con la escala EQ-5D-5 L y la escala visual análoga EQ), utilización de servicios de salud, y RTW. Se aplicó análisis de regresión logística para evaluar la asociación entre depresión, ansiedad y TEPT y la HRQoL, utilización de servicios de salud y RWT.
Resultados: A los 6 meses de seguimiento tras la lesión, el 22% (n = 665/3060) de los pacientes incluidos tuvo puntajes indicativos de probable trastorno de ansiedad (14%), depresión (16%) y/o TEPT (6%). Estos pacientes habían reducido los puntajes de la escala EQ-5D [β: −0.26 (95% CI: −0.28,-0.23)] y tuvieron menos probabilidad de RTW [OR: 2.12 (95% CI: 1.34, 3.37)] comparados con su contraparte. La utilización de servicios de salud tanto física como mental fue significativamente más alta en los pacientes con síntomas indicativos de depresión, ansiedad y/o TEPT.
Conclusiones: En los pacientes lesionados, existe una alta incidencia de depresión, ansiedad y síntomas de TEPT, los cuales se asociaron con una menor HRQoL, mayor uso de servicios de salud, y menores tasas de RTW. Estos resultados subrayan la importancia del tamizaje y tratamiento de estos síntomas en esta población, para aumentar una buena recuperación de los pacientes lesionados.
PALABRAS CLAVE: Salud mental, calidad de vida relacionada a la salud, lesiones, retorno al trabajo, utilización de servicios de salud
Short abstract
背景: 受伤患者有出现心理健康问题的风险, 这可能导致更缓慢的康复并影响健康相关生活质量 (HRQoL), 医护利用率和重返工作岗位 (RTW)。
目的: 在本研究中, 我们在成年受伤患者中确定了可能患有抑郁, 焦虑和创伤后应激障碍 (PTSD) 的表征症状流行率及其与 HRQoL, 医护利用率和 RTW 的关联。
方法: 成年患者意外受伤的数据来自荷兰伤害监测系统 (DISS), 以及一个六个月随访问卷, 包括评估抑郁, 焦虑和创伤后应激障碍 (PTSD) 症状的医院焦虑和抑郁量表 (HADS) 和事件影响量表 - 修订版 (IES-R), 以及 HRQoL (使用 EQ-5D-5 L 和 EQ 视觉模拟量表测量), 医护利用率和 RTW 的条目。 使用逻辑回归分析评估了抑郁, 焦虑和 PTSD 与 HRQoL, 医护利用率和 RTW 之间的关联。
结果: 在受伤后 6 个月时, 22% (n = 665/3060) 的纳入患者的评分表明可能患有焦虑 (14%), 抑郁 (16%) 和/或 PTSD (6%)。这些患者的 EQ-5D 效用评分降低 [β: −0.26 (95% CI: −0.28,-0.23)] 并且与其同行相比不太可能 RTW [OR: 2.12 (95% CI: 1.34,3.37)] 。在有抑郁, 焦虑和/或 PTSD 症状的患者中, 心理和身体医护利用率显著更高。
结论: 在受伤患者中, 抑郁, 焦虑和 PTSD 症状的发生率较高, 这与较低的 HRQoL, 较高的医护利用率和较低的 RTW 率相关。这些结果强调了在该人群中筛查和治疗这些症状以促进受伤患者良好康复的重要性。
关键词: 心理健康, 健康相关生活质量, 受伤, 重返工作岗位, 医护利用率
1. Introduction
Injuries are an important public health problem and a leading cause of mortality and morbidity (Roth et al., 2018). The majority of injuries are unintentional and caused by falls or road traffic incidents (World Health, 2014). Due to advanced health care and preventative measures, mortality rates in the trauma population have decreased over the last decades (Abubakar, Tillmann, & Banerjee, 2015). While the vast majority of injured individuals survive, many face long-term physical disability, but also impairment in social functioning, lack of productivity, and psychological distress, which could be categorized by symptoms of depression, anxiety, or post-traumatic stress (Bryant et al., 2010; Holbrook, Anderson, Sieber, Browner, & Hoyt, 1999; O’Donnell et al., 2013; Zatzick et al., 2007).
Evidence suggests a relationship between physical injury and mental health problems, which is not necessarily related to the injury severity (O’Donnell et al., 2013; Quale, Schanke, Frøslie, & Røise, 2009; Ramchand, Marshall, Schell, & Jaycox, 2008). Mental health symptoms are found to be an important determinant for long-term disability in injury patients (O’Donnell et al., 2013). The management of both the physical injury and the mental health problems may contribute to improvements in patient outcomes (Quale et al., 2009). Previous studies on mental health symptoms in injury patients mainly showed that there is a relationship between post-traumatic stress symptoms and functional outcomes (Herrera-Escobar et al., 2020; Holbrook et al., 2005; O’Donnell et al., 2009; Zatzick et al., 2008). Screening for and treatment of mental health disorders may therefore have a positive effect on the physical recovery of these patients. However, there is still limited research on these relationships of mental health symptoms with other outcomes, including health-related quality of life (HRQoL), return to work (RTW), and health care utilization in injury patients. Moreover, most studies used only small study samples. Additionally, they mostly investigated one specific mental health disorder and there is a lack of research on the combination of mental health problems (i.e. anxiety, depression, and post-traumatic stress) after injury (Wiseman, Foster, & Curtis, 2013).
A recent study by Herrera-Escobar et al. who studied the association between anxiety, depression, and PTSD with functional outcome after severe injury, found that one out of five patients screened positive for at least one mental health disorder. These patients were more likely to have chronic pain and functional limitations (Herrera-Escobar et al., 2020). Few large-scale studies have assessed the prevalence of multiple mental health disorders in injury patients and the association with other outcomes including health care utilization, HRQoL, and functional outcome, such as RTW. To fill the gaps in what is currently known, the current study included a large general injury population from the Netherlands. The aims of this study were to 1) determine the prevalence of anxiety, depression, and PTSD symptoms, six months after injury, and 2) determine the association of these mental health symptoms with health care utilization, RTW, and HRQoL.
2. Methods
2.1. Study population
This is a cohort study in the general Dutch injury population using data from the Dutch Injury Surveillance System (DISS). Data were collected from the DISS registry and from a survey that was administered six months after Emergency Department (ED) visit. The DISS gathers data on patients of all ages with intentional or unintentional injuries visiting the ED of one of 14 hospitals throughout the Netherlands and includes patients with all injury severities (Roth et al., 2018). These 14 hospitals are a representative sample of hospitals in the Netherlands with a mix of academic and non-academic hospitals in both rural and urban areas. The following data is registered in the DISS: age, sex, injury characteristics (e.g. cause, mechanism, severity of injury) and health care utilization during hospital admission (e.g. length of stay). Cause of injury was categorized as: home and leisure injuries, traffic injuries, sports injuries, or occupational injuries. The nature of injury groups was based on the EUROCOST classification (World Health, 2014).
2.2. DISS six-month follow-up questionnaire
To get more insight into long-term consequences of injury and post-hospital health care utilization, the Consumer Safety Institute performs follow-up studies. Follow-up questionnaires were sent to a stratified sample of injury patients registered in the DISS, six-months after their visit to an ED. Injury patients, who visited an ED in the Netherlands, were stratified by type of injury and if patients were hospitalized. Those who were hospitalized and had severe, less common injuries were overrepresented in the sample. Questionnaires were sent between January 2017 and December 2017, to those who had a place of residence in the Netherlands, unintentional injuries, and survived hospital discharge. The questionnaire included an informed consent form and all participants signed the informed consent form. To increase the response rates, patients who did not respond to the survey, received a reminder. In the current study, patients <18 years were excluded from the analyses.
2.2.1. Demographics
The follow-up questionnaire included items on basic demographics (comorbidity, living situation, educational level), mental health symptoms, health care utilization, RTW, and HRQoL. The presence of comorbidity included respiratory disease, heart disease, previous stroke, diabetes mellitus, hernia, (rheumatoid) arthritis, cancer, and other. Patients were categorized into ‘no comorbidity, ‘one comorbidity’ or ‘two or more comorbidities. Living situation was categorized as: living together with a partner and/or other family members in the same household or living alone. Level of education was categorized according to the 2011 International Standard Classification of Education (ISCED) into low (primary school, lower secondary school or lower vocational training), middle (intermediate and higher secondary school, or intermediate vocational training), and high (higher vocational training or university education).
2.2.2. Mental health
The Hospital Anxiety and Depression Scale (HADS) was administered to detect depression and anxiety symptoms and the Impact of Event Scale-Revised (IES-R) to detect PTSD symptoms. Patients were asked to respond to the questions with respect to their injury and indicate how much they were distressed during the past seven days for each item.
The HADS is a 14-item measure: 7 items for evaluating anxiety symptoms (HADS-A subscale) and 7 items for evaluating depression symptoms (HADS-D subscale). Higher HADS total scores indicate increased symptom severity. Scores for each item ranged from 0–3, and a subscale score of 11 or higher signifies the presence of anxiety or depression symptoms indicative of anxiety disorder and clinical depression (Zigmond & Snaith, 1983).
The IES-R is a 22-item instrument that measures intrusive re-experiences of the trauma and avoidance of trauma-related stimuli. Scores of each item ranged from 0–4. A cut-off score of 33 or higher signifies the presence of posttraumatic stress symptoms indicative of PTSD (Creamer, Bell, & Failla, 2003).
Those with scores above the cut-off for anxiety, depression, and/or PTSD symptoms are referred to as those with probable mental health disorders.
2.2.3. Health care utilization, RTW and HRQoL
Patients were asked to report the number of specialist consultations, visits to a rehabilitation centre, general practitioner, physiotherapist, and to a mental health professional (psychologist, psychotherapist, psychiatrist), and the number of weeks of receiving home care (e.g. nursing care, help with daily activities) as a consequence of their injury, in the six months after injury. Patients who were employed at the time of injury were asked whether they had been absent from work due to their injury in the last six months, as well as whether they were still absent at six months post-injury. The 5-dimensional, 5-level EuroQol instrument (EQ-5D-5 L) is an instrument designed to measure generic HRQoL. The items represent five different dimensions of health: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. There are five ordered response options: ‘no problems’, ‘slight problems’, ‘moderate problems’, ‘severe problems’ or ‘extreme problems/unable to’ (Zatzick et al., 2007). The scores of the dimensions (1 to 5 in each dimension), can be converted into a health utility score. Patients are asked to choose the response option that best describes their health today. The Dutch value set was used to calculate the utility score ranging from 0 (death) to 1 (full health) (Holbrook et al., 1999). The EQ-5D-5 L also includes a visual analogue scale (EQ VAS), measuring the patient’s self-rated health, consisting of a scale ranging from 0 (worst imaginable health state) to 100 (best imaginable health state).
2.3. Data analysis
Descriptive statistics were used for sociodemographic characteristics. Bivariate analyses including the Kruskal–Wallis Test and the Pearson’s Chi-squared test were used to compare participants with or without probable mental health disorders. A non-response analysis was conducted to determine whether responders differed from non-responders regarding age, sex, cause of injury, number of injuries, and hospitalization. Chi-square tests were used for categorical variables and Mann Whitney U test for continuous variables. Logistic regression analyses were performed to investigate the association between probable mental health disorders and health care utilization, RTW, EQ-5D utility score, and EQ VAS. Regression models were adjusted for sex, age, educational level, comorbidity status, living situation, cause of injury, number of injuries, and length of hospital stay. For the regression analyses, missing baseline characteristics were imputed using multivariate imputation by chained equation (MICE) approach based on an imputation model including all baseline characteristics and six-month outcomes, using the mice package in R (Van Buuren & Groothuis-Oudshoorn, 2011). Results were pooled using Rubin’s rules (Rubin, 2004). Analyses were performed in SPSS V.25 (statistical package for social sciences, Chicago, Illinois, USA) and R (version 4.1.0) (R foundational for statistical computing, Vienna, Austria) (R Core Team, 2020).
2.4. Results
2.4.1. Baseline characteristics
In total, 3165 adults (≥18 years) who presented to an ED with unintentional injury, responded to the six-month follow-up questionnaire (Supplementary Fig. 1). Non-response analysis showed that participants were significantly older, more often female, had more often multiple injuries and were more often hospitalized than non-respondents (Supplementary Table 1). There were 3060 patients who completed the HADS and IES-R. Of these patients, 665 (21.7%) scored above the cut-off score of anxiety, depression, and/or PTSD symptoms. Baseline characteristics for patients with or without probable mental health disorders are reported in Table 1. Those with probable mental health disorder(s) were older, were more often female, had a lower educational level, were more likely to live alone, had comorbidities, and were more likely to have been hospitalized (p < .001). Depression (n = 473, 15.5%) occurred most frequently, followed by anxiety (n = 434, 14.2%) and PTSD (n = 187, 6.1%). Nearly half (48.6%) of patients with at least one probable disorder, also screened positive for another probable mental health disorder (Figure 1).
Table 1.
Baseline characteristics for patients with or without mental health disorders
| Characteristics | Without probable mental health disorder(s) | With probable mental health disorder(s) | p-value |
|---|---|---|---|
|
N |
2395 (78.3%) |
665 (21.7%) |
|
| Age, median [IQR] | 64 [51–82] | 71 [55–82] | <0.001 |
| Male sex | 1098 (45.8%) | 251 (37.7%) | <0.001 |
| Highest educational levela | <0.001 | ||
| Low | 989 (44.3%) | 348 (58.3%) | <0.001 |
| Middle | 588 (26.3%) | 147 (24.6%) | |
| High | 658 (29.4%) | 102 (17.1%) | |
| Living situation, aloneb | 606 (25.9%) | 277 (43.4%) | <0.001 |
| Comorbiditiesc | <0.001 | ||
| None | 1385 (60.0%) | 219 (33.9%) | |
| One | 617 (26.7%) | 214 (33.1%) | |
| Two or more | 306 (13.3%) | 213 (33.0%) | |
| Cause of trauma | <0.001 | ||
| Home and leisure | 1350 (56.4%) | 449 (67.5%) | |
| Traffic | 600 (25.1%) | 161 (24.2%) | |
| Sports | 288 (12.0%) | 26 (3.9%) | |
| Occupational | 157 (6.6%) | 29 (4.4%) | |
| Number of injuries | 0.438 | ||
| One | 1763 (73.6%) | 483 (72.6%) | |
| Two | 449 (18.7%) | 122 (18.3%) | |
| Three or more | 183 (7.6%) | 60 (9.0%) | |
| Hospitalization | 1136 (47.4%) | 424 (63.8%) | <0.001 |
| Hospital length of stay in days, median [IQR]d | 4 [2-7] | 5 [3-9] | <0.001 |
IQR Interquartile Range.
a230 (7.5%) missing values.
b82 (2.7%) missing values.
c106 (3.5%) missing values.
dMean length of stay for hospitalized patients, 101 (3.3%) missing values.
Figure 1.
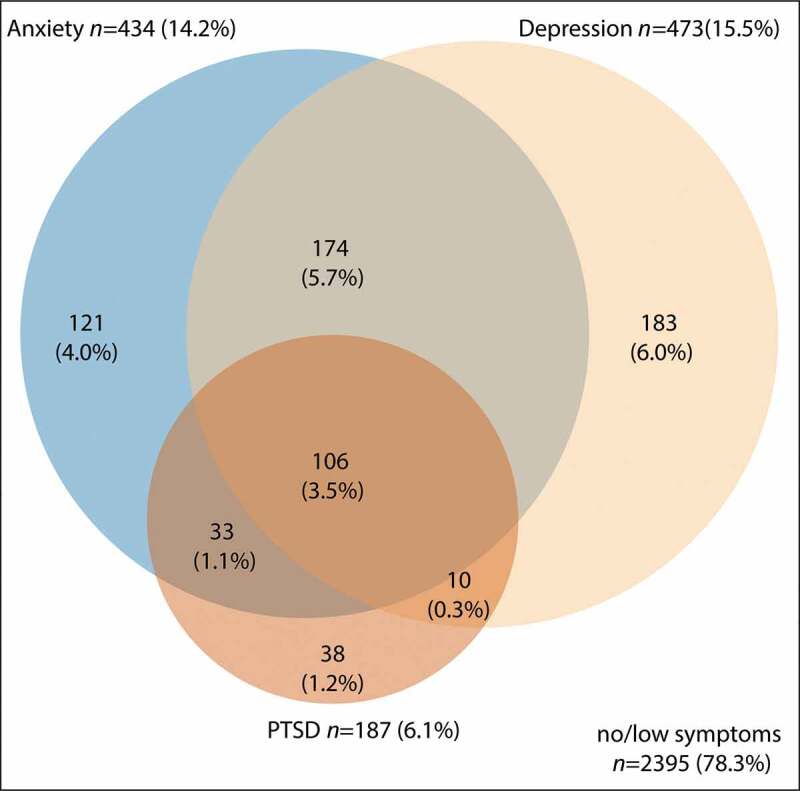
Venn diagram for anxiety, depression and PTSD six months after injury (total n = 3060). Blue: Anxiety symptoms HADSA ≥8. Beige: Depression symptoms HADSD ≥8, Orange: PTSD symptoms IESR ≥33.
2.4.2. Health-related quality of life
The proportion of patients who experienced problems on the five dimensions of the EQ-5D-5 L increased with the number of probable mental health disorders (Figure 2). Patients who did not meet the criteria of any mental disorder reported least often problems in any dimension. Additionally, the EQ-5D-5 L utility scores of those with one or more probable mental health disorders (EQ-5D-5 L utility score: 0.50, EQ VAS score 55.7) were significantly lower compared to patients with no probable mental health disorder (EQ-5D-5 L utility score: 0.82, EQ VAS score: 76.5) (Table 2). HRQoL was the lowest in the group with all three probable mental health disorders (EQ-5D-5 L utility score: 0.28, EQ VAS score: 47.9). After adjusting for potential confounders, those with any probable mental health disorder had lower EQ-5D utility [B: −0.26 (95% CI −0.28;-0.24)] and EQ VAS scores [B: −16.77 (95% CI −18.30;-15.23)] compared to those with no probable mental health disorder (Table 2).
Figure 2.
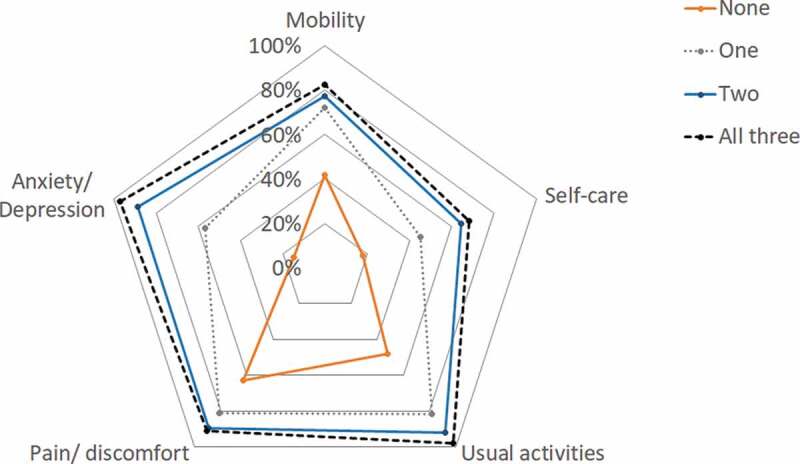
Proportion of patients reporting any problems on the EQ-5D-5 L dimensions at six months after injury.
Table 2.
Unadjusted EQ-5D-5 L utility and EQ VAS scores by probable mental health disorder and adjusted association between probable mental health disorders and health-related quality of life
| Mental health disorder | N | EQ-5D utility score, mean (SD)a | Adjusted B (95% CI)c | EQ VAS score, mean (SD)b |
Adjusted B (95% CI)c |
|---|---|---|---|---|---|
| Any disorder | |||||
| No | 2396 | 0.82 (0.19) | Ref | 76.5 (16.2) | Ref |
| Yes | 666 | 0.50 (0.31) | −0.26 (−0.28;-0.24) | 55.7 (20.0) | −16.77 (−18.30;-15.23) |
| Probable anxiety disorder | |||||
| No | 2626 | 0.80 (0.21) | Ref | 74.9 (17.4) | Ref |
| Yes | 434 | 0.47 (0.32) | −0.28 (−0.30;-0.25) | 54.3 (19.7) | −16.40 (−18.15;-14.64) |
| Probable depression | |||||
| No | 2587 | 0.81 (0.19) | Ref | 75.5 (16.8) | Ref |
| Yes | 473 | 0.43 (0.31) | −0.31 (−0.33;-0.29) | 52.3 (19.3) | −18.06 (−19.77;-16.34) |
| Probable PTSD | |||||
| No | 2873 | 0.77 (0.23) | Ref | 73.2 (18.3) | Ref |
| Yes | 187 | 0.44 (0.33) | −0.28 (−0.31;-0.25) | 54.9 (22.4) | −14.70 (−17.30;-12.11) |
| Probable anxiety disorder, depression and/or PTSD | |||||
| None | 2396 | 0.82 (0.19) | Ref | 76.5 (16.2) | Ref |
| One | 342 | 0.61 (0.26) | −0.16 (−0.18;-0.14) | 60.0 (19.3) | −12.64 (−14.54;-10.74) |
| Two | 218 | 0.44 (0.31) | −0.32 (−0.35;-0.30) | 52.8 (19.4) | −19.10 (−21.43;-16.77) |
| All Three | 106 | 0.28 (0.31) | −0.47 (−0.51;-0.43) | 47.9 (20.1) | −23.69 (−26.89;-20.49) |
Abbreviations: OR: Odds Ratio, RTW: return to work, PTSD: post-traumatic stress disorder.
a191 (6.2%) missing values.
b106 (3.5%) missing values.
cAdjusted for sex, age, living situation, comorbidity status, educational level, length of hospital stay, cause of injury, number of injuries.
2.4.3. Health care utilization and RTW
At six months, patients who reported elevated symptoms of depression, anxiety, and/or PTSD, also more often reported physical and mental health care utilization compared to those without elevated symptoms (Table 3). Additionally, an increasing number of probable mental health disorders was found to be associated with more health care utilization (Supplementary table 2). Regarding mental health care, 18.7% of those who had any mental health disorder reported receiving mental health treatment, compared to 3.6% of respondents with no mental health disorder. The highest percentage of using psychological care was found for respondents with posttraumatic symptoms indicative of PTSD (30.7%).
Table 3.
Six-month health care utilization and return to work among those with or without probable mental health disorders
| Probable Mental health disorder |
|||||
|---|---|---|---|---|---|
| None | Any disorder | Probable anxiety disorder | Probable depression | Probable PTSD | |
| N = 2396 | N = 666 | N = 434 | N = 473 | N = 187 | |
| Health care utilization | |||||
| General practitionerb | 700 (30.5%) | 310 (51.7%) | 209 (53.6%) | 223 (52.8%) | 103 (62.4%) |
| Mean (SD) number of visitsa | 2.3 (5.0) | 3.2 (3.6) | 3.2 (3.2) | 3.3 (3.9) | 3.6 (4.0) |
| Specialistc | 1377 (61.1%) | 403 (68.5%) | 280 (72.2%) | 279 (66.9%) | 116 (71.2%) |
| Mean (SD) number of visitsa | 3.0 (3.2) | 3.7 (3.7) | 3.7 (3.8) | 3.6 (3.4) | 4.1 (4.1) |
| Rehabilitationd | 160 (7.0%) | 99 (17.3%) | 70 (18.7%) | 69 (17.3%) | 32 (19.8%) |
| Mean (SD) number of visitsa | 10.9 (16.9) | 14.5 (24.4) | 14.4 (25.8) | 15.7 (27.7) | 13.7 (25.7) |
| Physiotherapye | 1133 (50.9%) | 343 (59.5%) | 240 (63.0%) | 240 (59.0%) | 113 (69.3%) |
| Mean (SD) number of visitsa | 13.8 (12.0) | 16.0 (14.4) | 15.6 (14.6) | 16.8 (15.5) | 14.6 (13.6) |
| Mental health treatmentf | 84 (3.6%) | 119 (18.7%) | 97 (23.6%) | 83 (18.4%) | 55 (30.9%) |
| Mean (SD) number of visitsa | 7.3 (9.6) | 6.9 (11.7) | 7.1 (12.3) | 6.6 (10.7) | 7.1 (11.6) |
| Home careg | 365 (16.3%) | 191 (34.2%) | 122 (33.2%) | 141 (36.6%) | 53 (32.1%) |
| Mean (SD) number of weeksa | 9.7 (7.7) | 12.8 (8.7) | 13.3 (9.0) | 13.0 (8.8) | 13.4 (8.2) |
| Productivity lossh | |||||
| No absence from work | 294 (29.7%) | 28 (15.8%) | 18 (13.8%) | 15 (16.0%) | 4 (6.6%) |
| RTW <6 months | 549 (55.4%) | 72 (40.7%) | 53 (40.8%) | 27 (28.7%) | 28 (45.9%) |
| No RTW <6 months | 148 (14.9%) | 77 (43.5%) | 59 (45.4%) | 52 (56.3%) | 29 (47.5%) |
aMean number of visits/weeks for patients with ≥1 visit/week.
b168 (5.5%) missing values for general practitioner visits.
c219 (7.2%) missing values for specialist visits.
d219 (7.2%) missing values for rehabilitation care visits.
e258 (8.4%) missing values for physiotherapy visits.
f66 (2.2%) missing values for mental health care visits.
g260 (8.5%) missing values for home care.
hIncludes patients who were employed before the injury (n = 1167).
After adjusting for potential confounders, respondents with any probable mental health disorder were more likely to visit a GP [OR: 2.25 (95% CI 1.85;2.73)], specialist [OR: 1.42 (95% CI: 1.16;1.75)] and to receive rehabilitation care [OR: 2.25 (95% CI: 1.67;3.03)], physical therapy [OR: 1.38 (95% CI: 1.13;1.68)], mental health care [OR: 5.63 (95% CI: 4.09;7.78)] and home care [OR: 1.62 (95% CI: 1.27;2.07)] than respondents with no probable mental health disorder (Table 4). Additionally, respondents with a higher number of mental health disorders were more likely to use both physical and mental health services.
Table 4.
Adjusted association between probable mental health disorders and health care utilization and RTW
| Health care utilization |
||||||||
|---|---|---|---|---|---|---|---|---|
| General practitioner |
Specialist |
Rehabilitation |
Physical therapy |
Mental health care |
Home care |
No RTWa |
||
| Mentalhealth disorder | N | OR [CI95] | OR [CI95] | OR [CI95] | OR [CI95] | OR [CI95] | OR [CI95] | OR [CI95] |
| Any disorder | ||||||||
| No | 2396 | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Yes | 666 | 2.25 [1.85;2.73] | 1.42 [1.16;1.75] | 2.25 [1.67;3.03] | 1.38 [1.13;1.68] | 5.63 [4.09;7.78] | 1.62 [1.27;2.07] | 2.13 [1.38;3.33] |
| Probable anxiety disorder | ||||||||
| No | 2626 | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Yes | 434 | 2.22 [1.77;2.78] | 1.64 [1.29;2.01] | 2.45 [1.77;3.40] | 1.60 [1.26;2.02] | 6.59 [4.76;9.12] | 1.58 [1.19;2.10] | 2.32 [1.44;3.74] |
| Probable depression | ||||||||
| No | 2587 | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Yes | 473 | 2.25 [1.79;2.81] | 1.30 [1.03;1.65] | 1.84 [1.32;2.57] | 1.29 [1.02;1.62] | 4.10 [2.92;5.64] | 1.42 [1.08;1.87] | 2.56 [1.51;4.32] |
| Probable PTSD | ||||||||
| No | 2873 | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Yes | 187 | 3.06 [2.19;4.28] | 1.47 [1.03;2.09] | 2.22 [1.42;3.46] | 2.12 [1.49;3.02] | 6.33 [4.32;9.29] | 1.44 [0.97;2.16] | 3.17 [1.72;5.87] |
| Probable anxiety disorder, depression and/or PTSD | ||||||||
| None | 2396 | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| One | 342 | 1.76 [1.37;2.26] | 1.38 [1.06;1.80] | 2.00 [1.37;2.92] | 1.11 [0.86;1.43] | 3.20 [2.10;4.90] | 1.62 [1.19;2.22] | 1.21 [0.64;2.29] |
| Two | 218 | 2.65 [1.95;3.60] | 1.20 [0.88;1.66] | 2.32 [1.48;3.63] | 1.51 [1.10;2.07] | 7.57 [4.94;11.60] | 1.76 [1.21;2.57] | 3.14 [1.61;6.14] |
| All Three | 106 | 3.88 [2.46;6.11] | 2.38 [1.43;3.97] | 3.04 [1.72;5.37] | 2.50 [1.55;4.04] | 13.06 [7.85;21.73] | 1.36 [0.80;2.30] | 4.41 [1.88;10.36] |
Adjusted for sex, age, living situation, comorbidity status, educational level, length of hospital stay, cause of injury, number of injuries.
Abbreviations: N: number of patients, OR: Odds Ratio, CI95: 95% confidence interval, RTW: return to work, PTSD: post-traumatic stress disorder.
aincludes patients who were employed before the injury (n = 1167).
Regarding RTW for patients in paid employment pre-injury, 85.1% of patients without probable mental health disorders returned to work within six months after injury, compared to 56.5% of patients with a mental health disorder (Table 3). Patients with a probable mental health disorder had higher odds of not returning to work within six months after injury [OR: 2.13 (95% CI: 1.38;3.33)] (Table 4). Respondents with symptoms indicative of probable PTSD had the highest odds of no RTW [OR: 3.17 (95% CI: 1.72;5.87)]. Patients with symptoms indicative of all three probable disorders were 4.5 times more likely not to return to work within six months compared to those without probable mental health disorders [OR: 4.41 (95% CI: 1.88;10.36)].
2.5. Discussion
The current study investigated the association of symptoms indicative of probable anxiety disorder, depression, and PTSD with health care utilization, RTW, and HRQoL in adult patients six months after injury. We found that one in five patients met the criteria for at least one probable mental health disorder and nearly half of these patients had a co-occurrence of multiple probable mental health disorders. The presence of probable mental health disorders was associated with lower HRQoL, and a higher likelihood of both mental and physical health care utilization and not returning to work.
Symptoms indicative of depression and anxiety disorder were more common than PTSD, and co-occurrence of probable mental health disorders was observed frequently, which is consistent with previous research (Herrera-Escobar et al., 2020). Previous studies have shown an overlap of symptoms of PTSD, anxiety, and depression and it is suggested that mental health symptoms are likely to be more severe when disorders are co-occurring (Barbano et al., 2019; Elhai, Grubaugh, Kashdan, & Frueh, 2008; Kessler, Chiu, Demler, & Walters, 2005; Price & van Stolk-cooke, 2015). This may also explain the finding that patients with co-occurring probable mental health disorders had worse HRQoL and RTW outcomes and higher health care utilization. This adds to previous studies that also found a relationship between the number of probable mental health disorders and HRQoL and between the number of probable mental health disorders and RTW (Herrera-Escobar et al., 2020; Zatzick et al., 2008). These patients might have a more complicated recovery and poorer treatment response. The worse outcomes for those with multiple probable mental health disorders underline the need for clinicians to screen and treat patients for a spectrum of mental health problems.
Patients with mental health problems reported higher mental and physical health care utilization. However, it is concerning that less than 20% of patients with any probable mental health disorder and less than 40% of patients with all three probable disorders reported use of mental health services. A substantial group of patients with mental health symptoms do not receive mental health treatment after injury. A previous study found similar results and reported that 26% of those who met the criteria for PTSD or depression at six-months post-injury received professional help (Wong et al., 2009). They found a strong relationship between physician referral and mental health service utilization. While our study did not include data on referral status, health care providers may play an important role in the early identification of patients with mental health problems and in facilitating access to mental health services after physical injury. Another explanation for the low rates of mental health care could be that physical rehabilitation after injury is seen as a priority. The majority of patients with mental health problems also present physical symptoms, such as pain, headaches, fatigue, and worsening of chronic disease symptoms (Kirmayer et al., 1993). This is in accordance with our study since patients with probable mental health disorders experienced more problems on all five dimensions of the EQ-5D. With a focus on the somatic symptoms, a diagnosis for psychiatric disorders might be missed. A correct diagnosis and treatment for mental and somatic symptoms are important as misdiagnosing or not diagnosing a patient can lead to further morbidity and impairment. We reported on cross-sectional six-month associations, and it is unclear what the direction of the association was. Previous studies have suggested an interaction between post-traumatic distress symptoms and physical functioning (Ramchand et al., 2008). Treatment of mental health disorders in the recovery period after injury may therefore have a positive effect on physical recovery. This highlights the necessity of a multidimensional rehabilitation process, with a focus on both physical and mental functioning.
Our study indicated that those with probable mental health disorders were older, were more often female, had a lower educational level, were more likely to live alone, had comorbidities, and were more likely to have been hospitalized. This is in accordance with risk factors of impaired physical and mental outcome found in other studies (Haider et al., 2020) There are several important pre-injury characteristics, including previous traumatic events and history of mental health disorders, which were not included in this study but could have influenced the mental health problems of these patients. These important pre-injury characteristics should be included in future studies to further investigate important risk factors for mental health problems after physical injury. Additionally, other outcome variables not included in this study, such as pain levels, are also found to be associated with mental health and functional outcome in other studies (Herrera-Escobar, Kaafarani, Velmahos, Salim, & Haider, 2018).
The current study investigated several probable mental health disorders alongside each other in a large cohort of injury patients. Apart from this major strength, there are several limitations. First, a clinician evaluation by a health professional is needed to diagnose a patient with anxiety, depression, or PTSD. In the current study, we used self-reported questionnaires to measure anxiety, depression, and PTSD symptoms and labelled patients with symptoms above certain thresholds as having a probable disorder. However, these questionnaires alone cannot be used to clinically diagnose a mental health disorder. Secondly, the patient history of psychiatric disorders was not assessed. Therefore, we were not able to distinguish between patients who had mental health problems prior to the injury and those who developed mental health problems within the six-month period after injury. Third, the participation rate was low and the responders were significantly older, more often female, and more often hospitalized than those who were lost to follow-up, which may limit the generalizability of this study to other injury patient samples. The results of this study might show an overestimation of the mental health problems in the injury population, as those with probable mental health disorders were also significantly older, more often female, and more often hospitalized than those without probable mental health disorders. The non-response rate was higher compared to other studies in injury populations. Our study differs from other studies with the inclusion of both hospitalized and non-hospitalized patients of all injury severity levels, resulting in a mild injury population. One explanation for the high non-response rate might be caused by non-response of patients who were fully recovered at the time of the first questionnaire at six months. Lastly, the analyses in this study were cross-sectional. Therefore, no causal inference between probable mental health disorders and other studied outcomes can be made. Future studies should have a long-term, longitudinal follow-up, including pre-injury data on for example the history of traumatic events, mental health disorders, and HRQoL which might be important confounding factors. Additionally, future research is needed to develop strategies to improve the mental health of injury patients, which in turn may facilitate a good recovery with lower long-term health care utilization, higher RTW rates, and higher HRQoL. This study confirms the high occurrence of mental health problems after injury and its association with higher health care utilization, lower RTW rates, and lower HRQOL. Our results highlight the importance of mental health support in this patient population, the necessity of a multidimensional rehabilitation process, and the need to focus on multiple disorders, in research and clinical settings. Early identification and treatment of mental health disorders after injury may improve HRQoL and RTW, and reduce health care utilization.
Supplementary Material
Funding Statement
Funding was received from the Dutch Ministry of Health, Welfare and Sport for the follow-up DISS study in 2017.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are only available on request. Requests may be sent to: Martien Panneman m.panneman@veiligheid.nl. The data presented in this study are not publicly available due to information that could compromise the privacy of research participants.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Ethics approval
All procedures performed involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Approval by the METC was not required according to the METC of the Academic Medical Center of the University of Amsterdam (W16_394 # 17.004).
Supplementary material
Supplemental data for this article can be accessed here.
References
- Abubakar, I. I., Tillmann, T., & Banerjee, A. (2015). Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet, 385(9963), 117–10. doi: 10.1016/S0140-6736(14)61682-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbano, A. C., der Mei, W. F., deRoon‐Cassini, T. A., Grauer, E., Lowe, S. R., Matsuoka, Y. J., & Shalev, A. Y. (2019). Differentiating PTSD from anxiety and depression: Lessons from the ICD‐11 PTSD diagnostic criteria. Depression and Anxiety, 36(6), 490–498. doi: 10.1002/da.22881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant, R. A., O’Donnell, M. L., Creamer, M., McFarlane, A. C., Clark, C. R., & Silove, D. (2010). The psychiatric sequelae of traumatic injury. American Journal of Psychiatry, 167(3), 312–320. doi: 10.1176/appi.ajp.2009.09050617 [DOI] [PubMed] [Google Scholar]
- Creamer, M., Bell, R., & Failla, S. (2003). Psychometric properties of the impact of event scale—revised. Behaviour Research and Therapy, 41(12), 1489–1496. doi: 10.1016/j.brat.2003.07.010 [DOI] [PubMed] [Google Scholar]
- Elhai, J. D., Grubaugh, A. L., Kashdan, T. B., & Frueh, B. C. (2008). Empirical examination of a proposed refinement to DSM-IV posttraumatic stress disorder symptom criteria using the national comorbidity survey replication data. Journal of Clinical Psychiatry, 69(4), 597. doi: 10.4088/JCP.v69n0411 [DOI] [PubMed] [Google Scholar]
- Haider, A. H., Herrera-Escobar, J. P., Al Rafai, S. S., Harlow, A. F., Apoj, M., Nehra, D., … Salim, A. (2020). Factors associated with long-term outcomes after injury: Results of the functional outcomes and recovery after trauma emergencies (forte) multicenter cohort study. Annals of Surgery, 271(6), 1165–1173. doi: 10.1097/SLA.0000000000003101 [DOI] [PubMed] [Google Scholar]
- Herrera-Escobar, J. P. Seshadri A. J., Stanek E., Lu K., Han K., Sanchez S., Kaafarani H. M. A., Salim A., Levy-Carrick N. C., Nehra D. (2020). Mental health burden after injury: It’s about more than just posttraumatic stress disorder. Annals of Surgery, 274(6), e1162–e1169. doi: 10.1097/SLA.0000000000003780 [DOI] [PubMed] [Google Scholar]
- Herrera-Escobar, J. P., Kaafarani, H. M. A., Velmahos, G., Salim, A., & Haider, A. H. (2018). Association of pain after trauma with long-term functional and mental health outcomes. Journal of Trauma and Acute Care Surgery, 85(4), 773–779. doi: 10.1097/TA.0000000000002017 [DOI] [PubMed] [Google Scholar]
- Holbrook, T. L., Anderson, J. P., Sieber, W. J., Browner, D., & Hoyt, D. B. (1999). Outcome after major trauma: 12-month and 18-month follow-up results from the trauma recovery project. Journal of Trauma and Acute Care Surgery, 46(5), 765–773. doi: 10.1097/00005373-199905000-00003 [DOI] [PubMed] [Google Scholar]
- Holbrook, T. L., Hoyt, D. B., Coimbra, R., Potenza, B., Sise, M., & Anderson, J. P. (2005). Long-term posttraumatic stress disorder persists after major trauma in adolescents: New data on risk factors and functional outcome. Journal of Trauma and Acute Care Surgery, 58(4), 764–771. doi: 10.1097/01.TA.0000159247.48547.7D [DOI] [PubMed] [Google Scholar]
- Kessler, R. C., Chiu, W. T., Demler, O., & Walters, E. E. (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry, 62(6), 617–627. doi: 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirmayer, L. J. Robbins, J. M., Dworkind, M., & Yaffe, M. J. (1993). Somatization and the recognition of depression and anxiety in primary care. The American Journal of Psychiatry, 150(5), 734–741. doi: 10.1176/ajp.150.5.734 [DOI] [PubMed] [Google Scholar]
- O’Donnell, M. L., Holmes, A. C., Creamer, M. C., Ellen, S., Judson, R., McFarlane, A. C., & Bryant, R. A. (2009). The role of post-traumatic stress disorder and depression in predicting disability after injury. Medical Journal of Australia, 190(S7), S71–S74. doi: 10.5694/j.1326-5377.2009.tb02474.x [DOI] [PubMed] [Google Scholar]
- O’Donnell, M. L., Varker, T., Holmes, A. C., Ellen, S., Wade, D., Creamer, M., … Forbes, D. (2013). Disability after injury: The cumulative burden of physical and mental health. The Journal of Clinical Psychiatry, 74(2), 137–143. doi: 10.4088/JCP.12m08011 [DOI] [PubMed] [Google Scholar]
- Price, M., & van Stolk-cooke, K. (2015). Examination of the interrelations between the factors of PTSD, major depression, and generalized anxiety disorder in a heterogeneous trauma-exposed sample using DSM 5 criteria. Journal of Affective Disorders, 186, 149–155. doi: 10.1016/j.jad.2015.06.012 [DOI] [PubMed] [Google Scholar]
- Quale, A. J., Schanke, A.-K., Frøslie, K. F., & Røise, O. (2009). Severity of injury does not have any impact on posttraumatic stress symptoms in severely injured patients. Injury, 40(5), 498–505. doi: 10.1016/j.injury.2008.11.006 [DOI] [PubMed] [Google Scholar]
- R Core Team . (2020). A language and environment for statistical computing. 2013. R Foundation for Statistical Computing. http://www.R-project.org/ [Google Scholar]
- Ramchand, R., Marshall, G. N., Schell, T. L., & Jaycox, L. H. (2008). Posttraumatic distress and physical functioning: A longitudinal study of injured survivors of community violence. Journal of Consulting and Clinical Psychology, 76(4), 668. doi: 10.1037/0022-006X.76.4.668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth, G. A. Abate, D., Abate, K. H., Abay, S. M., Abbafati, C., Abbasi, N., . & Borschmann, R. (2018). Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. The Lancet, 392(10159), 1736–1788. doi: 10.1016/S0140-6736(18)32203-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin, D. B. (2004). Multiple imputation for nonresponse in surveys (Vol. 81). New York: John Wiley & Sons. doi: 10.1002/9780470316696 [DOI] [Google Scholar]
- Van Buuren, S., & Groothuis-Oudshoorn, K. (2011). mice: Multivariate imputation by chained equations in R. Journal of Statistical Software, 45(1), 1–67. doi: 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- Wiseman, T., Foster, K., & Curtis, K. (2013). Mental health following traumatic physical injury: An integrative literature review. Injury, 44(11), 1383–1390. doi: 10.1016/j.injury.2012.02.015 [DOI] [PubMed] [Google Scholar]
- Wong, E. C., Schell, T. L., Marshall, G. N., Jaycox, L. H., Hambarsoomians, K., & Belzberg, H. (2009). Mental health service utilization after physical trauma: The importance of physician referral. Medical Care, 47(10), 1077. doi: 10.1097/MLR.0b013e3181a80fc9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health, O. (2014). Injuries and violence: The facts 2014.
- Zatzick, D. F. Rivara, F. P., Nathens, A. B., Jurkovich, G. J., Wang, J. I. N., Fan, M. Y., . & Mackenzie, E. J . (2007). A nationwide US study of post-traumatic stress after hospitalization for physical injury. Psychological Medicine, 37(10), 1469–1480. doi: 10.1017/S0033291707000943 [DOI] [PubMed] [Google Scholar]
- Zatzick, D., Jurkovich, G. J., Rivara, F. P., Wang, J., Fan, M.-Y., Joesch, J., & Mackenzie, E. (2008). A national US study of posttraumatic stress disorder, depression, and work and functional outcomes after hospitalization for traumatic injury. Annals of Surgery, 248(3), 429–437. doi: 10.1097/SLA.0b013e318185a6b8 [DOI] [PubMed] [Google Scholar]
- Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are only available on request. Requests may be sent to: Martien Panneman m.panneman@veiligheid.nl. The data presented in this study are not publicly available due to information that could compromise the privacy of research participants.


