Executive summary
The story of dying in the 21st century is a story of paradox. While many people are overtreated in hospitals with families and communities relegated to the margins, still more remain undertreated, dying of preventable conditions and without access to basic pain relief. The unbalanced and contradictory picture of death and dying is the basis for this Commission.
How people die has changed radically over recent generations. Death comes later in life for many and dying is often prolonged. Death and dying have moved from a family and community setting to primarily the domain of health systems. Futile or potentially inappropriate treatment can continue into the last hours of life. The roles of families and communities have receded as death and dying have become unfamiliar and skills, traditions, and knowledge are lost. Death and dying have become unbalanced in high-income countries, and increasingly in low-and-middle-income countries; there is an excessive focus on clinical interventions at the end of life, to the detriment of broader inputs and contributions.
The COVID-19 pandemic has meant that death is prominent in daily media reports and health systems have been overwhelmed. People have died the ultimate medicalised deaths, often alone but for masked staff in hospitals and intensive care units, unable to communicate with family except electronically. This situation has further fuelled the fear of death, reinforcing the idea of health-care services as the custodian of death.
Climate change, the COVID-19 pandemic, environmental destruction, and attitudes to death in high-income countries have similar roots—our delusion that we are in control of, and not part of, nature. Large sums are being invested to dramatically extend life, even achieve immortality, for a small minority in a world that struggles to support its current population. Health care and individuals appear to struggle to accept the inevitability of death.
Philosophers and theologians from around the globe have recognised the value that death holds for human life. Death and life are bound together: without death there would be no life. Death allows new ideas and new ways. Death also reminds us of our fragility and sameness: we all die. Caring for the dying is a gift, as some philosophers and many carers, both lay and professional, have recognised. Much of the value of death is no longer recognised in the modern world, but rediscovering this value can help care at the end of life and enhance living.
Treatment in the last months of life is costly and a cause of families falling into poverty in countries without universal health coverage. In high-income countries between 8% and 11·2% of annual health expenditure for the entire population is spent on the less than 1% who die in that year. Some of this high expenditure is justified, but there is evidence that patients and health professionals hope for better outcomes than are likely, meaning treatment that is intended to be curative often continues for too long.
Conversations about death and dying can be difficult. Doctors, patients, or family members may find it easier to avoid them altogether and continue treatment, leading to inappropriate treatment at the end of life. Palliative care can provide better outcomes for patients and carers at the end of life, leading to improved quality of life, often at a lower cost, but attempts to influence mainstream health-care services have had limited success and palliative care broadly remains a service-based response to this social concern.
Rebalancing death and dying will depend on changes across death systems—the many inter-related social, cultural, economic, religious, and political factors that determine how death, dying, and bereavement are understood, experienced, and managed. A reductionist, linear approach that fails to recognise the complexity of the death system will not achieve the rebalancing needed. Just as they have during the COVID-19 pandemic, the disadvantaged and powerless suffer most from the imbalance in care when dying and grieving. Income, education, gender, race, ethnicity, sexual orientation, and other factors influence how much people suffer in death systems and the capacity they possess to change them.
Radically reimagining a better system for death and dying, the Lancet Commission on the Value of Death has set out the five principles of a realistic utopia: a new vision of how death and dying could be. The five principles are: the social determinants of death, dying, and grieving are tackled; dying is understood to be a relational and spiritual process rather than simply a physiological event; networks of care lead support for people dying, caring, and grieving; conversations and stories about everyday death, dying, and grief become common; and death is recognised as having value.
Systems are constantly changing, and many programmes are underway that encourage the rebalancing of our relationship with death, dying, and grieving. Communities from varied geographies are challenging norms and rules about caring for dying people, and models of citizen and community action, such as compassionate communities, are emerging. Policy and legislation changes are recognising the impact of bereavement and supporting the availability of medication to manage pain when dying. Hospitals are changing their culture to openly acknowledge death and dying; health-care systems are beginning to work in partnership with patients, families, and the public on these issues and to integrate holistic care of the dying throughout health services.
Key messages.
-
•
Dying in the 21st century is a story of paradox. Although many people are overtreated in hospitals, still more remain undertreated, dying of preventable conditions and without access to basic pain relief.
-
•
Death, dying, and grieving today have become unbalanced. Health care is now the context in which many encounter death and as families and communities have been pushed to the margins, their familiarity and confidence in supporting death, dying, and grieving has diminished. Relationships and networks are being replaced by professionals and protocols.
-
•
Climate change, the COVID-19 pandemic, and our wish to defeat death all have their origins in the delusion that we in control of, not part of, nature.
-
•
Rebalancing death and dying will depend on changes across death systems—the many inter-related social, cultural, economic, religious, and political factors that determine how death, dying, and bereavement are understood, experienced, and managed.
-
•
The disadvantaged and powerless suffer most from the imbalance in care for those dying and grieving.
-
•
The Lancet Commission on the Value of Death sets out five principles of a realistic utopia, a new vision of how death and dying could be. The five principles are: the social determinants of death, dying, and grieving are tackled; dying is understood to be a relational and spiritual process rather than simply a physiological event; networks of care lead support for people dying, caring, and grieving; conversations and stories about everyday death, dying, and grief become common; and death is recognised as having value.
-
•
The challenge of transforming how people die and grieve today has been recognised and responded to by many around the world. Communities are reclaiming death, dying and grief as social concerns, restrictive policies on opioid availability are being transformed and health-care professionals are working in partnership with people and families, but more is needed.
-
•
To achieve our ambition to rebalance death, dying and grieving, radical changes across all death systems are needed. It is a responsibility for us all, including global bodies and governments, to take up this challenge. The Commission will continue its work in this area.
These innovations do not yet amount to a whole system change, but something very close to the Commission's realistic utopia has been achieved in Kerala, India, over the past three decades. Death and dying have been reclaimed as a social concern and responsibility through a broad social movement comprised of tens of thousands of volunteers complemented by changes to political, legal, and health systems.
To achieve the ambition of radical change across death systems we present a series of recommendations, outlining the next steps that we urge policy makers, health and social care systems, civil society, and communities to take. Death and dying must be recognised as not only normal, but valuable. Care of the dying and grieving must be rebalanced, and we call on people throughout society to respond to this challenge.
Introduction
“How pathetic it was to try to relegate death to the periphery of life when death was at the centre of everything.”
Elif Shafak, Turkish novelist
The proposition of the Lancet Commission on the Value of Death is that our relationship with death and dying has become unbalanced, and we advocate a rebalancing. At the core of this rebalancing must be relationships and partnerships between people who are dying, families, communities, health and social care systems, and wider civic society.
In high-income countries, death and dying have become unbalanced as they moved from the context of family, community, relationships, and culture to sit within the health-care system. Health care has a role in the care of the dying, but interventions at end of life are often excessive,1, 2 exclude contributions from families and friends,3 increase suffering,4, 5 and consume resources that could otherwise be used to meet other needs.6 This lack of balance in high-income countries is spreading to low-and-middle-income countries, a form of modern colonialism, and the imbalance may be worse in low-and-middle-income countries, as this report will show.
The relationship with death and dying in low-and-middle-income countries is unbalanced as the rich receive excessive care, while the poor, the majority, receive little or no attention or relief of suffering and have no access to opioids, as the Lancet Commission on Global Access to Palliative Care and Pain Relief showed.7 Excessive treatment for the rich and inadequate or absent care for the poor is a paradox and a failing of global health and solidarity.
Readers may wonder about the title of the Commission: the Lancet Commission on the Value of Death. The title has its origins in the Lancet planning a Commission on the value of life. It's an age-old idea that a good life and a good death go together. Our title has proved to be a rich source of thinking, helping us recognise the value of death in a world that tends to deny death any value. The simplest proposition of the value of death is that “without death every birth would be a tragedy”, and in a very crowded world we are the edge of such a tragedy. In the report we explore the many values of death.
The Commission began its work before the COVID-19 pandemic arrived, bringing death to television screens every night. Dying on a ventilator, looked after by masked and gowned staff, and only able to communicate with family through screens, is the ultimate medicalised death. Yet even in high-income countries, many have died at home with minimal support, and in low-and-middle-income countries hundreds of thousands have died with no care from health professionals. The capacity of health services was exceeded in many countries during the course of 2020 and 2021. The Commissioners wondered whether death and dying rising so high on the agenda would change attitudes to death and dying, perhaps bringing greater acceptance of death and a recognition of its imbalanced nature. As 2021 draws to a close, we see no evidence of such a change. Indeed, we see signs of the opposite: governments have prioritised attempts to reduce only the number of deaths and not the amount of suffering; huge emphasis has been placed on ventilators and intensive care and little on palliative care; bereavement has been overlooked; anxiety about death and dying seems to have increased;8, 9 death and dying has come to belong still more to health care, with families and communities excluded; and we hear from Commissioners stories of doctors increasing their efforts to fend off death from causes other than COVID-19. The great success with vaccines has perhaps further fuelled the fantasy that science can defeat death. Scholarly research on changes in attitudes to death and dying is limited at this early stage, but the historian Yuval Noah Harari has asked whether the pandemic will change attitudes to death and dying and what humanity's takeaway will be: “In all likelihood, it will be that we need to invest even more efforts in protecting human lives. We need to have more hospitals, more doctors, more nurses. We need to stockpile more respiratory machines, more protective gear, more testing kits.”10
At the start of the COVID-19 pandemic we thought that perhaps a report on the value of death would not be welcome after millions of deaths, but we now think the opposite—that the pandemic makes our report more relevant, and our recommendations will make us better able to respond to the next pandemic.
Although the pandemic seems not to have encouraged greater acceptance of death, it has been accompanied by a rapid rise in concern about the ecological crisis, including climate change. COP26 (Conference of the Parties), the annual UN meeting on climate change, held in Glasgow in November, 2021, achieved far greater media coverage and stronger commitments to reduce carbon emissions than any previous meeting, although the commitments are not enough to prevent serious harm to health. This increase in concern has various roots, but the pandemic has reminded us that we are part of nature, not in control of nature. The pandemic and the ecological crisis are both caused by our failure to recognise our connection with nature and our destruction of the natural environment. The Commission believes that the drive to fend off death and pursue a dramatic extension in length of life also arises from a failure to recognise that we are part of nature; and as financial cost and carbon consumption are closely related to expensive care, treatment at the end of life will be an important contribution to the carbon footprint of health care. Were it a country, health care would be the world's fifth largest emitter of greenhouse gases.11 Unfortunately, the carbon footprint of most health systems is rising when it needs to fall to net-zero by the middle of the century.12 Panel 1 discusses further the connection between climate change, the ecological crisis, and death and dying.
Panel 1. Death and the climate crisis.
The Covid-19 pandemic has revealed our global interdependence and the fragility of our support systems and economy. The Canadian archeologist and author, Ronald Wright, described how every empire that has ever existed has collapsed, usually for ecological reasons.13 Now, he points out, we are one global empire. The COVID-19 pandemic will pass, like the epidemics before it, but damage to the climate and the planet will be irreparable. The Intergovernmental Panel on Climate Change (IPCC) advises that we have only a dozen years to avoid that damage,14 but carbon emissions are increasing by about 7% annually, not decreasing by 7%, as the IPCC says is necessary.
Everything, and especially death, must be thought of in the context of the climate crisis. Before the pandemic we were on track for a temperature increase of 8·5 degrees Celsius over preindustrial levels, which, as Nature pointed out, would lead us to conditions like that of the Permian extinction event, when some 95% of all life forms were made extinct.15 The IPCC says that global temperature increases must be kept below 1·5°C. Already we are close to an increase of 1·3°C, and the effects are being felt now.
Carbon emissions are a function of the number of humans, currently 7·9 billion, and the carbon they each consume. The average Briton consumes 5·6 metric tons of carbon each year (16·1 tons for Americans), whereas the average Bangladeshi consumes 0·6 metric tons. If the world is to reach net-zero carbon emissions by 2050 then people in rich countries will have to consume much less carbon and shift resources to lower income countries. The UK Health Alliance on Climate Change says that this shift would mean, for example, Britons consuming 0·5 metric tons each year16—a dramatic change, but one that would lead to an improvement in health as people drive less, exercise more, and eat diets low in animal products and high in fruit and vegetables.
Health systems account for a substantial proportion of country's carbon emissions—12% in the USA and 5% in the UK.12 Carbon emissions from health systems are currently increasing,12 although some organisations are attempting to reverse this trend. NHS England has published a detailed plan of how it plans to reach net-zero by 2045.17
The carbon footprint of health systems can be reduced by activities like switching to renewable energy, reducing travel, and redesigning buildings, but it will also mean changing clinical practice. Increasingly the carbon consumption of clinical activity will matter more than the financial cost, and methods exist to capture this consumption.18 This Commission has summarised evidence of excessive treatment at the end of life. We now need to assemble evidence on the carbon cost: while the dead consume no carbon, the disposal of bodies does.
About three quarters of people in Britain are cremated after death, releasing carbon into the air. Alkaline hydrolysis, in which the body is dissolved, has about a seventh of the carbon footprint of cremation, and the resulting fluid can be used as fertiliser. A Dutch study of the disposal of bodies found that the lowest amount of money that it would theoretically cost to compensate in terms of the carbon footprint per body was €63·66 for traditional burial, €48·47 for cremation, and €2·59 for alkaline hydrolysis.19 Composting or natural burial are alternatives.
If we are to survive the climate crisis then almost everything will have to change, including health care, end-of-life care, and how we dispose of the dead. In the widely acclaimed novel Overstory, a eulogy to trees and nature, a leading environmentalist asks the audience at a conference what they can best do to counter climate change and environmental destruction: her answer is, to die.
Structure of the report
Section 1 of the report defines the territory and methods of the Commission, including the limitations and what it has not been possible to cover in this report. Section 2 presents a brief survey of the facts and figures of death and dying in the 21st century.
The Commission recognises that rebalancing death and dying will depend on changes across death systems: the many inter-related social, cultural, economic, religious, and political factors that determine how death, dying, and bereavement are understood, experienced and managed.20 Section 3 describes the concept of a death system.
Sections 4 to 10 describe death systems now, covering philosophical and religious underpinnings; historical origins; the influence of power and inequities; the role of families and communities; consumerism and choice; the dominance of health care; and the importance of economics.
Following this examination of historic and contemporary death systems, in section 11 the Commission uses scenario planning to imagine five different but plausible futures for death and dying.
Section 12 outlines the features of a realistic utopia,21 a concept developed by the American philosopher John Rawls (1921–2002), which shares principles of how the Commissioners would like to see death and dying change in a way that is achievable. It is a radically different future envisioned by the Commission in which life, wellbeing, death, and grieving are in balance.
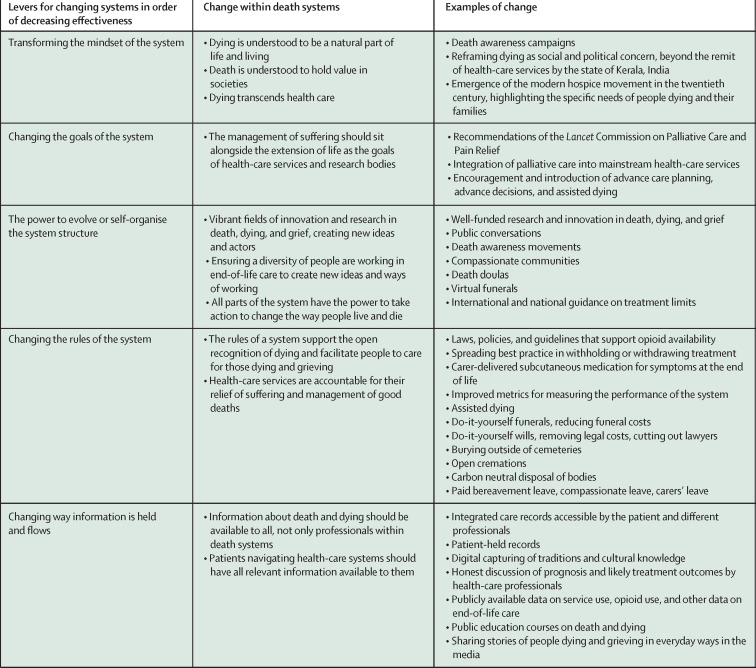
Recognising that creating the “realistic utopia” will depend on many changes within death systems, section 13 discusses why systems are hard to change and how they might be changed. The section also gives examples of changes in systems that are underway.
Section 14 gives a detailed and critical account of the end-of-life system in Kerala, South India, as it represents the system closest to the realistic utopia the Commission has described.
Section 15 lists the Commission's recommendations for change, and the final section, section 16, proposes the next steps the Commission will take to try and achieve this change.
Section 1: Defining our territory and methods
Death can occur through conflict, accident, natural disaster, pandemic, violence, suicide, neglect, or disease, but this Commission focuses particularly on the time from when a person develops a life-limiting illness or injury through their death and into the bereavement affecting the lives of those left behind. We do not address specific diseases, conditions, or age groups, but rather draw on a wide-ranging series of examples to show the depth and breadth of the challenge. These examples are not intended to be systematic or exhaustive but rather illustrative. We draw on a range of different materials from case study and reflection to national datasets and empirical work and have used scoping rather than systematic literature searches.
The Commission has drawn its membership from around the world, but much of the evidence reported on comes from high-income countries. What we describe, both the problems and the possibilities, has relevance for all settings.
The Commissioners (see end of this report] include health and social care professionals, social scientists, health scientists, economists, a philosopher, a political scientist, patients, a carer, religious leaders, activists, community workers, and a novelist.
We acknowledge the diversity of experience in death, dying, and grief and how race, gender, sexuality, poverty, disability, age, and many other potential forms of marginalisation shape experiences and outcomes at these times. The intersectional nature of these aspects of people's lives and identities means marginalisation is rarely due to a single factor. We have attempted to be reflexive as people, Commissioners, and authors, to understand how our own worldviews, cultural backgrounds, identities, professional disciplines, and experiences determine our perspectives and actions. In recognition of the inclusive and reflexive spirit of this report, we endeavour to use terms in their broadest and most inclusive sense throughout. Words such as person, patient, family, carer, illness, community, relationship, and many others should be understood in this context.
We have reflected that we should have done more to include the voice of patients and carers, although all Commissioners brought their own personal experiences of death and bereavement. We are conscious that there are many voices we have not heard, but we see this report as the start of a conversation and hope to hear from further voices after publication.
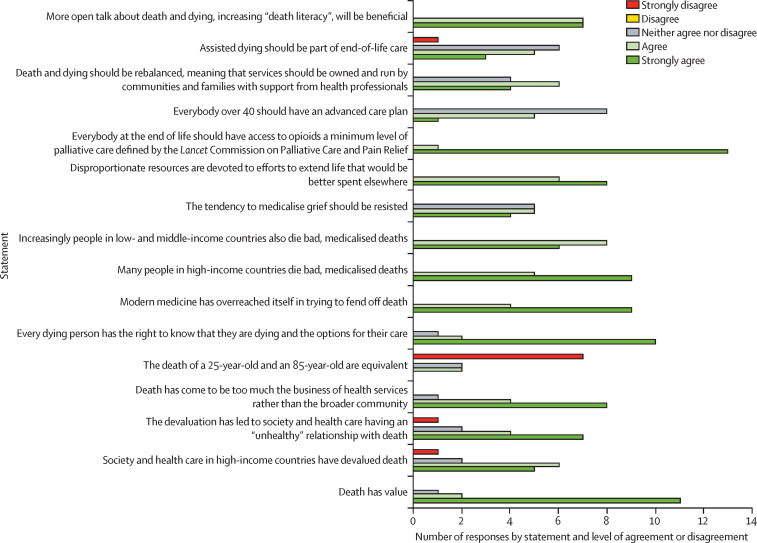
We have chosen the term “health-care professionals” to denote all those working in health-care settings, including doctors, nurses, and allied health professionals, but we acknowledge that there exists an appreciable variation in approach and practice within these groups. We also appreciate the role social care professionals play at the end of life, and the interdependent relation between health and social care in many countries around the world. Over the course of the past 3 years, the Commissioners met together physically three times, held frequent virtual meetings, and communicated regularly by email. We commissioned working papers from other authors and have drawn on many sources of knowledge and understanding. The report has contributors with differing views. We have not sought agreement or conformity in our argument but have attempted to capture the tensions that exist among Commissioners. Figure 1 shows agreements and disagreements on a range of issues, including assisted dying, which we expected to divide Commissioners; there was more agreement than our intense discussions had led us to think.
Figure 1.
Level of agreement and disagreement among commissioners on statements about death and dying
Not all commissioners responded to the survey; 14 commissioners participated.
The Commission has created an open website with more than 70 background papers relating to death and dying. Much of what is included in our report is rewritten and condensed versions of those entries. The report has been through five major restructurings, two of them after the first round of editorial and peer review. Death and dying are distinct, multi-layered, and culturally charged concepts. Death can be seen as simply the end of life; as the opposite of health—although the Commission believes that it is healthy to die; as a symbol, classically a skeleton or a grim reaper; as a failure (and many would argue that doctors or health-care professionals can see death as a failure, inspiring them to do all they can to defeat death); as a punishment for moral failure; as an escape from the suffering of life; as a gateway to Heaven, Valhalla, Nirvana, or the many other religious and cultural depictions of eternal bliss or to a version of Hell; or as an essential part of a cycle of ending and beginning.
The Commission has generally been narrower in its use of the words death and dying. We see dying as a process. We have not set a timeframe, understanding that people may be dying for years, months, days, hours, minutes, or seconds. We understand death as an event but with recent changes in technology, failing organs that previously heralded death can be replaced, meaning that death is an evolving and complex concept. Only within the past decade did an international consensus attempt to define how death is determined.22
Defining death
In 2014, WHO convened the second meeting of a task force on the determination of death,23 acknowledging that the line between life and death was being increasingly blurred by medical technology. It concluded that although there are multiple ways to die, including neurological and cardiovascular pathways, they all lead to the same irreversible state of being dead. As a result, the algorithms of circulatory and neurological death were merged, with a single endpoint. The definition of death relies on certain clinical signs such as absence of a response, pulse, breathing, and pupillary reflexes.
The WHO guidance relates to death in medical institutions or under professional care and is based on clinical signs interpreted by professionals. A large proportion of deaths around the world take place outside clinical oversight, and the signs and symptoms are interpreted by lay people with experience of death and dying. The recognition of death is often linked with the traditions, rituals, and funeral practices of the particular culture.24 Panel 2 describes how in places in rural Malawi, the village elders and then the village head's representative confirm death. The head's signal that a death has occurred starts the vigil and mourning process.
Panel 2. Lay determination of death in Malawi.
Luckson Dullie, member of the Commission, writes:
In rural Malawi death is confirmed by the elders. There is no exact checklist, but experience from having witnessed so many deaths has taught them that dying people lose weight fast; their strength fails; they speak little or incomprehensibly; and their breath is often shallow and laboured. The elders know that often dying people do not want to look you in the face, or when they do, their face is blank, empty, because the spirit has already departed. When they think death has occurred, the elders feel for the pulse in the neck, but the most tell-tale sign is cold armpits. The process of confirmation of death can take 2 hours or longer. During this time, the elders must ensure that the body lies straight and that the mouth and the eyes are closed. Children are not allowed in the room. Once death is confirmed, a message must be dispatched to the village head. Until the village head is told and they or their representative confirms the death, no one is allowed to cry out loud. The village head's confirmation signals the start of vigil and mourning process.
Section 2: The facts and figures of death and dying in the 21st century
At first sight, mortality trends over the past 30 years suggest a success story. Global life expectancy has risen steadily throughout the world, increasing from 67·2 years in 2000 to 73·5 years in 2019,25 with important gains made in low-and-middle-income countries. This success has been driven by falls in deaths from communicable disease, maternal and neonatal conditions, and malnutrition.26 But healthy life expectancy (years lived in self-reported good health) has not kept pace with overall life expectancy: years lived without good health have increased between 2000 and 2019—from 8·6 years to 10 years.25
In many high-income countries in the past decade, life expectancy gains have stalled, or in some cases reversed. In the UK, life expectancy increases slowed from 2011 to 2020 and fell for women in the most deprived 10% of neighbourhoods.27 In the USA, life expectancy fell from 1990 to 2000 for women with fewer than 12 years of formal education28 Life expectancy in the USA has also fallen in younger age groups (10–65 years), probably reflecting the opioid epidemic.29 As 2021 closes, the COVID-19 pandemic is far from over, particularly in low-and-middle-income countries. The pandemic's effects on life expectancy are not complete and have not yet been measured in most countries—but reductions are likely to be more than a year in most countries. Data are available for the USA, where life expectancy fell by 1·87 years (to 76·87 years) between 2018 and 2020. The reductions have been very unequal, with life expectancy falling by 3·88 years among Hispanic people, 3·25 years among non-Hispanic Black people, and 1·36 years among non-Hispanic White people.30 In England, life expectancy has fallen from 80 years for males and 83·7 years for females in 2019 to 78·7 years for males and 82·7 years for females in 2020, a similar level to a decade ago.31 As in the USA, the reductions have been greatest among those who are deprived.32
As deaths from infection and maternal and perinatal causes fall in many low-and-middle-income countries, the proportion of deaths from non-communicable disease rises. In Bangladesh, non-communicable disease accounted for 10% of deaths in 1986, but more than three-quarters by 2006, a very rapid transition.33 This change presents new challenges for already stretched health services. Cure for non-communicable disease is not possible, and instead interventions must focus on prevention, harm reduction, and self-management, acknowledging the complex social determinants of these chronic conditions.
Table 1 shows the mortality rates, life expectancy, causes of death, serious health-related suffering, and degree of inequality for seven selected countries represented by the Commissioners. The countries range from high-income to low-income. It illustrates the differences that persist among countries despite global trends. Life expectancy in Malawi is two decades less than that in the UK. Deaths from infection, maternal and perinatal causes, and malnutrition account for 4% of deaths in China but 26% in India and 60% in Malawi. Hundreds of thousands of deaths annually are associated with serious health-related suffering (as defined by the Lancet Commission on Global Access to Palliative Care and Pain Relief7, 40).
Table 1.
Mortality, life expectancy, causes of death, health related suffering, and degree of inequality for seven selected countries represented on the Commission
| Crude death rate per 1000 (2019)34 |
Life expectancy, years (2019)34 |
Income inequality, based on coefficient (2020)35 | Probability of dying aged 15–60 years (per 100; 2019)34 | Under 5 mortality (deaths per 1000 livebirths; 2019)34 | Maternal mortality (per 100 000 livebirths; 2019)36 | Deaths from communicable diseases and maternal, prenatal, and nutrition conditions (% of total; 2016)37 | Deaths from non-communicable disease (% of total; 2016)38 | Age-standardised death rate from suicide (per 100 000; 2016)39 | Deaths associated with serious health-related suffering*(thousands; 2015)40 | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Men | Women | ||||||||||
| High income | ||||||||||||
| UK | 9·4 | 81·3 | 79·6 | 84·7 | 32·4% | 6·8 | 4 | 7 | 8% | 89% | 7·6 | 317 |
| USA | 8·8 | 78·9 | 76·3 | 81·4 | 45% | 11·2 | 7 | 19 | 5% | 88% | 13·7 | 1310 |
| Middle income | ||||||||||||
| China | 7·3 | 76·9 | 74·8 | 79·2 | 46·5% | 7·9 | 11 | 29 | 4% | 89% | 8 | 5501 |
| India | 7·3 | 69·7 | 68·5 | 71 | 35·2% | 17·9 | 37 | 145 | 26% | 63% | 16·5 | 3983 |
| Mexico | 6·1 | 75·1 | 72·2 | 77·9 | 48·2% | 14 | 15 | 33 | 10% | 80% | 5·2 | 229 |
| Low income | ||||||||||||
| Malawi | 6·5 | 64·3 | 61·1 | 67·4 | 46·1% | 27·4 | 51 | 349 | 60% | 32% | 7·8 | 78 |
| Bangladesh | 5·5 | 72·6 | 70·9 | 74·6 | 32·1% | 13·6 | 30 | 173 | 26% | 67% | 6·1 | 409 |
Population estimated to be experiencing serious health-related suffering and in need of palliative care based on 20 conditions. Total deaths are weighted by a conversion factor or multiplier for each condition based on review by a panel of experts who deliberated on different considerations and incorporated published evidence as well as their own experience as providers of palliative care. The conditions considered were: atherosclerosis, cerebrovascular disease, chronic ischaemic heart disease, congenital malformations, degeneration of the central nervous system, dementia, diseases of the liver, haemorrhagic fevers, HIV, inflammatory disease of the central nervous system, injury, poisoning, and external causes, leukaemia, lung diseases, malignant neoplasms, musculoskeletal disorders, non-ischaemic heart diseases, premature birth and birth trauma, protein energy malnutrition, renal failure, and tuberculosis.
Table 2 shows how deaths in most high-income and middle-income countries occur more often in hospitals or other institutions, such as nursing or care homes. Limited data are available for low-income countries. The shift from home to institutions is relatively recent, often occurring over the past generation.
Table 2.
Place of death, health-care use, and hospital expenditures at the end of life in different countries
|
Place of death for diseases associated with palliative care need41* |
Inpatient health-care use in last 30 days of life for decedents of any age with any cancer42† | Health expenditures in last 30 days of life for decedents with cancer42‡ | Health expenditures in last 180 days of life for decedents with cancer42‡ | Health expenditures in last 30 days of life as % of health expenditures in last 180 days of life for decedents with cancer42 | |||||
|---|---|---|---|---|---|---|---|---|---|
| Home | Hospital | Long-term care institution | Primary care institution | Other institution or other | |||||
| High income | |||||||||
| Belgium | 24·8% | 50·8% | 23·8% | § | 0·6% | 14 455 (52·9%) | 6206 (6929) | 17 022 (17 642) | 36% |
| Canada | 12·9% | 61·4% | 20·8% | § | 4·8% | 16 917 (60·2%) | 10 843 (13 710) | 23 333 (28 922) | 46% |
| Czech Republic | 18·4% | 64·0% | 16·8% | § | 0·8% | § | § | § | § |
| France | 22·3% | 63·9% | 11·0% | § | 2·8% | § | § | § | § |
| Germany | § | § | § | § | § | 14 468 (47·8%) | 3326 (4394) | 10 033 (9858) | 33% |
| Hungary | § | 66·2% | .. | § | 33·8% | § | § | § | § |
| Italy | 44·4% | 45·7% | 6·1% | § | 3·8% | § | § | § | § |
| Netherlands | 34·5% | 24·6% | 34·5% | § | 6·4% | 3155 (43·7%) | 4766 (9653) | 18 414 (28 673) | 26% |
| New Zealand | 22·5% | 28·1% | 33·4% | 13·0% | 3·0% | § | § | § | § |
| Norway | .. | .. | .. | § | .. | 7052 (63·9%) | 3646 (7227) | 11 640 (14 398) | 31% |
| Spain (Andalusia)¶ | 35·1% | 57·3% | 7·3% | § | 0·3% | § | § | § | § |
| South Korea (Republic of Korea) | 13·5% | 84·9% | 1·3% | § | 0·3% | § | § | § | § |
| UK (England) | 21·7% | 47·5% | 17·8% | 11·6% | 1·3% | 65 616 (50·8%) | 6934 (6842) | 22 005 (20 920) | 32% |
| UK (Wales) | 21·2% | 58·6% | 12·0% | 6·5% | 1·7% | § | § | § | § |
| USA¶ | 31·5% | 37·8% | 22·0% | 3·8% | 5·0% | § | § | § | § |
| Middle income | |||||||||
| Mexico | 53·0% | 44·4% | § | § | 2·7% | § | § | § | § |
Based on death certificate data for 2008; population estimated to be in need of palliative care on the basis of ten conditions: cancer, renal failure, liver failure, chronic obstructive pulmonary disease, diseases of the nervous system (Alzheimer's disease, Parkinson's disease, motor neurone disease, Huntington's disease), and HIV/AIDS.
Hospitalisation in acute care hospital, number (%).
Mean (SD) per-capita hospital expenditures in US$ (2010; 2011 health-specific purchasing power parity conversion).
Data not available.
Reference year for place of death of patients with cancer: USA 2007, Spain (Andalusia) 2010.
Panel 3 contrasts two deaths in India: one a sudden death in India two generations ago with the whole family, including the children, gathering around the dead man in the family home and taking part in rituals; whereas the modern death is slow and distressing and occurs in intensive care, with even the man's son unable to visit.
Panel 3. Dying now and years ago in India.
M R Rajagopal, member of the Commission, writes:
When I recently saw a doctor-colleague facing the impending death of his son-in-law from cancer, the transformation that happened in our society over two generations became obvious to me.
The most striking memory is the expression of the dying man's 15-year-old son, who was walking in the background choosing books and cramming them into bags. He was not part of the conversation; when he came close the conversation flagged. He was being given an unspoken message: “This is grown-up talk; kids are not part of it”. He responded by pretending not to. He was being sent away to live with an uncle so that his father's illness and death would not disturb his studies.
From two generations back I remember the sudden death of my uncle when I was a child. He was in his late twenties. Nobody knew what ailed him. He just collapsed and died. My grandmother woke me in the middle of the night and carried me 5 km to my dead uncle's home. When I woke in the morning the extended family from far and near had assembled. No one was excluded. We children were part of everything that happened. Every family member had more than one opportunity to touch the dead man. People cried, the grieving women who were close relatives wailed loudly.
For the next 16 days many relatives stayed on all through the day. Their number dwindled as days passed. The more distant relatives left after cremation but returned for the fifth day and 16th day ceremonies. The closer family were throughout. The extended family took over all the expenses of that household during the 16 days following death. Those were the years closely following India's independence from colonial rule; poverty was extreme. But somehow, the extended family members scraped together enough. Women from the extended family took over the kitchen preparing and serving everyone simple meals and looking after all the children.
As I was growing up, I saw many more deaths. The elders in the society oversaw dying, empowered by having seen many deaths—how the limbs got cold, how the rattling in the throat became obvious, and how the pattern of breathing changed. Without anyone teaching anything in a classroom, younger generations took in lessons.
But by no means was death invariably benevolent and beautiful. When the physical suffering in people with diseases like cancer was extreme, no philosophising, compassion, or companionship helped enough. The suffering was excruciating. People just stood watching helplessly. The village physician, who practised Ayurveda, would visit but had little to offer. But the fact that he called helped enormously. The dying person and the family members were never alone in their suffering or grief.
Those deaths of years ago contrast starkly with the death of my colleague's son-in-law. A normal dying process was stretched out over weeks by interventions including an endotracheal tube and artificial ventilation of his lungs (but no pain relief). At the height of his suffering, he tried to pull out the tubes and cables, but his arms and legs were bound to the bed. His wife and father-in-law could visit him for only 5 minutes a couple of times a day, and each time had to watch the man dying a thousand deaths, his dignity and personhood violated in the worst possible way. Eventually, when the doctors suggested a tracheotomy and total parenteral nutrition, the family said no. The man died without seeing his son one last time, and the son was denied one last hug.
Table 2 also provides details of health spending in the last year of life. Health-care expenditure is known to be high and to increase during the last year of a person's life in many countries. These data describe health spending in six high-income countries in the last 6 months of life and demonstrate that costs in the last 30 days before death were disproportionately high compared with those in the 6 months before death.
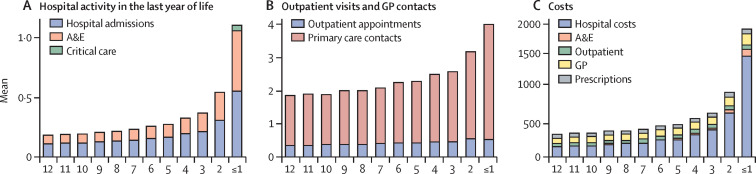
Figure 2 shows use of health services in the last year of life in England, with a steady increase across the year in hospital admissions and visits to the accident and emergency department, with a particularly dramatic increase in the last month of life.43 It is also in the last month that there are admissions to intensive care. It is questionable whether these increases in the last month of life provide benefit for patients and their families, or whether they may in fact be increasing suffering. Costs also increase across the year, with again a dramatic increase in the last month. Most of the costs arise from hospital care. The authors of the study also note that “healthcare utilisation and costs decrease with age at death, and are higher in men, patients dying from cancer, and patients with high comorbidities.”43
Figure 2.
Health-care use and costs in the last 12 months of life
(A) Use of inpatient care. (B) Primary and hospital outpatient care. (C) Total costs by cost type. A&E=accident and emergency department. GP=general practitioner. Reproduced from Luta and colleagues by permission of BMJ Publishing Group.43
Further studies, which the report summarises in the section on the economics of death systems, support the trend of substantially increased health spending in the last weeks of life. Some studies judge the treatments to be futile—for example, artificial nutrition for dying patients,44 chemotherapy in the last 30 days of life,4 or antimicrobial therapy at the end of life.2 Overtreatment at the end of life is part of the broader and pervasive challenge of overuse of medical services, defined as the provision of services likely to produce more harm than good.6
Experiences of dying today
“I came into it [caring for someone dying at home] not knowing you could care for somebody at home but she was dying and not dying fast enough for the hospital system and they kept sending her home and taking her back in and then sending her home again because they needed the bed. And it was very distressing and without any knowledge I decided that we could do better and brought her home…I managed to care for Mum until she died at home which was a great experience for everybody, her family and me.”
Carer in Australia45
Death and dying have changed profoundly over the past 70 years in high-income and middle-income countries, and increasingly in low-income countries. The shifting role of family, community, professionals, institutions, the state, and religion has meant that health care is now the main context in which many people encounter death. People may be unaware that alternatives are possible, as the quote above illustrates. Within this acute health-care setting, death and dying are seen as clinical problems and reduced to a series of separate biomedical markers and tests. Recognition of dying is often made late, if at all, and interventions can continue into the last days of life with minimal attention to suffering.46
As health care has moved to occupy the centre stage, families and communities have been pushed back. Death is not so much denied but invisible. Dying people are whisked away to hospitals or hospices, and whereas two generations ago most children would have seen a dead body, people may now be in their 40s or 50s without ever seeing a dead person. The language, knowledge, and confidence to support and manage dying are being lost, further fuelling a dependence on health-care services. The social and cultural setting of death, essential for providing meaning, connection, and lifelong support for those grieving, risks disappearing. Health-care professionals cannot substitute for the sense of coherence, the rituals and traditions, nor long-term mutual support that families and communities bring to people who are dying or grieving. “The experiment of making mortality a medical experience is just decades old. It is young. And the evidence is it is failing”, writes the surgeon Atul Gawande in his book Being Mortal.46
The impact of a stripped-back, atomised death and bereavement has been seen during the COVID-19 pandemic. People have died alone and families have been unable to say goodbye and prevented from coming together in grief. The effects of this situation will resonate for years to come.
Table 3, which is adapted from the work of the sociologist Lyn Lofland, presents a summary of the shifting trends in death and dying over the past 70 years.47 Defining death has become progressively more complex,23 and the technology accompanying death more sophisticated. Deaths from chronic disease have come to predominate with the consequence that dying takes weeks, months, or years. As the familiarity with death and dying has diminished, countries have witnessed a growth in movements aiming to increase awareness or control over the dying process. We have, argues Lofland, entered an age of “thanatological chic”.47
Table 3.
The changing nature of death and dying (adapted from Lofland)47
| Before 1950 | 1950 | 2019 | |
|---|---|---|---|
| Level of medical technology | Low | Increasing | High and increasing |
| Detection of terminal disease | Poor | Improving | High |
| Definition of death | Simple | Still simple | Complex |
| Deaths from acute disease (mostly rapid) | High | Still high | Low |
| Deaths from injuries (mostly rapid) | High | Still high | Lower |
| Deaths from chronic disease (mostly slow) | Low | Increasing | The majority |
| Length of dying | Short | Still mostly short | Long |
| Passivity in response to a person dying | Common | Decreasing | Gone in western medicine |
| Involvement of doctors in dying | Low | Increasing | High |
| Number of doctors in UK per 100 000 people | Fewer than 26 | 26 | 280 |
| Familiarity with death among the population | High | Still high | Low |
| Activities to manage death (death awareness campaigns, advance care planning, assisted dying, etc) | Low | Low | High |
| Community involvement in death and dying | High | Falling | Low |
| Meaning in death and dying | Mostly supplied through faith and faith organisations | Faith and faith organisations still have an important role | Inadequately supplied by multiple organisations, including the health system |
A striking inconsistency with the progressive medicalisation of death and dying is that it has not led to a parallel increase in relief of symptoms such as pain with low-cost, evidence-based methods, nor has it led to universal access to palliative care services at the end of life. Although some countries have established palliative care services, WHO estimates that globally only 14% of people in need can access such care.48 The Lancet Commission on Pain Relief and Palliative Care exposed the stark global inequities in access to opioids.7 Increases in clinical interventions, technology, and institutional care have not reduced—and may have increased—global suffering.
The story of dying in the 21st century is a story of paradox. While many people are overtreated in hospitals, with families and communities relegated to the margins, still more remain undertreated, dying of preventable conditions and without access to basic pain relief. The unbalanced and contradictory picture of death and dying today is the basis for this Commission.
Section 3: Death systems
Hospitals may be the site of dying for many people in the 21st century, but the fault for the unbalanced nature of death and dying does not rest solely with health-care services. Death and dying are intrinsic parts of life. Societies have long sought to understand and provide meaning to these universal events. The cultural anthropologist and psychoanalyst Ernest Becker (1924–74) argued in his Pulitzer-prize-winning book The Denial of Death that fear of death is the dominant driver of culture, religion, art, and human behaviour.49 The wider sociocultural, political, and economic context determines how, where, and why people die and grieve.
Robert Kastenbaum first described the concept of a death system as “interpersonal, socio-physical and symbolic networks through which an individual's relationship to mortality is mediated by society”20 Death systems are the means by which death and dying are understood, regulated, and managed. These systems implicitly or explicitly determine where people die, how people dying and their families should behave, how bodies are disposed of, how people mourn, and what death means for that culture or community. Systems are shaped by social, cultural, religious, economic, and political contexts and evolve over time. One culture's death system can seem strange and even abhorrent to people from other systems.50
Panel 4 describes some of the components of death systems—for example, people, places, and symbols—and panel 5 describes the functions of the system, including, for example, caring for the dying and making sense of death.
Panel 4. Components of the death system (adapted from Kastenbaum)20.
People
Doctors, nurses, police, funeral workers, florists, coroners, life insurance brokers, lawyers, soldiers, religious leaders; ultimately all people will be affected by death and all will die
Places
Mortuaries, hospitals, memorials, cemeteries, battlefields
Times
Annual remembrance days such as the Day of the Dead in Mexico, All Souls Day in Christianity, Anzac Day in Australia and New Zealand, two-minute silences following disasters, private reflections on anniversaries of deaths
Objects
Coffins, urns, funeral pyres, mourning clothes, obituaries, books relating to death and dying, electric chairs, gallows, guns
Symbols and images
Deities responsible for death or war, rituals such as the last prayers in many religions, wearing of black armbands, language and euphemisms for dying, images of skull and crossbones, skeletons
Panel 5. Functions of the death system (adapted from Kastenbaum)20.
Warning and predicting death
Public health and travel warnings, health and safety regulations, extreme weather warnings, climate change predictions
Preventing death
Services such as the police and firefighters, scientists researching vaccines and cures for diseases, screening programmes for disease
Caring for dying people
Practices that support those dying, including practices of family carers, primary healthcare, hospices and palliative care units, death doulas, religious leaders, hospitals, morphine availability, advance care planning
Disposing of dead people
The tasks all societies must perform in disposing safely of corpses and the rituals and funereal customs that accompany these tasks
Social consolidation after death
Processes that allow families or communities to adjust to the loss; social networks and support, compassionate leave from work, bereavement groups or counselling
Making sense of death
Religious, spiritual, or philosophical reflections on the meaning of death or an afterlife, memorialising
Killing
Norms that dictate when and how killing is socially sanctioned, such as in war, in capital punishment, in assisted dying, or the killing of animals
Kastenbaum was writing from an Anglocentric perspective, but all cultures create death systems. Researchers explored death and dying among the indigenous Sámi people in Northern Scandinavia and concluded that despite differences in core concepts—for example, depending on seasonal changes and relationships rather than calendar time—Kastenbaum's model provides a useful tool for understanding this death system.51 Similarly, a group studying the preparations made for death by rural Chinese elders found that the tasks, rituals, imagery, meaning, and roles resonated broadly with the structure developed by Kastenbaum.52
Understanding complex or so-called wicked problems through a systems lens is an approach increasingly required for understanding and intervening in issues such as obesity,53 homelessness,54 or gender inequality.55 Margaret Chan, the director general of WHO from 2006 to 2017, talked of the need for responses to these complex problems from the “whole-of-government and whole-of-society.”56 People have come to these approaches after realising that more reductionist approaches achieve little.
The death system is one of many complex adaptive systems that exist and intersect throughout societies and include, for example, primary care services, education systems, financial systems, families, and communities. Complex adaptive systems have defining features: most importantly, they do not follow linear causation, nor allow simple solutions to problems.57 They exist in a complex web of interacting personal, social, political, religious, and economic drivers. Attempts to reduce a complex adaptive system to the sum of its linear parts to explain how it works, and how to intervene, will be unsuccessful, as their behaviour is emergent and unpredictable. It is the relationship between parts that offers the most insight into how a complex system functions. They are not closed but have blurred boundaries and interact with their environment and other systems. Systems adapt, change, and evolve over time just as death systems have done. Small interventions or changes at one point can have considerable unintended consequences at another: as the famous metaphor suggests, a butterfly beating its wings in New Mexico can cause a hurricane in China. Complex adaptive systems are often fine-tuned to achieve a specific purpose and have feedback loops that ensure they continue to achieve that purpose. Positive feedback loops can also occur, causing sudden shifts in behaviours or outcomes.
Death systems are unique to societies and cultures, but the trends described in Table 1, Table 2 suggest that patterns are emerging across systems. The increased number of deaths in hospital means that ever fewer people have witnessed or managed a death at home. This lack of experience and confidence causes a positive feedback loop that reinforces a dependence on institutional care of the dying. Medical culture, fear of litigation, and financial incentives contribute to overtreatment at the end of life, further fuelling institutional deaths and the sense that professionals must manage death. Social customs influence the conversations in clinics and in intensive care units, often maintaining the tradition of not discussing death openly. More undiscussed deaths in institutions behind closed doors further reduce social familiarity with and understanding of death and dying.
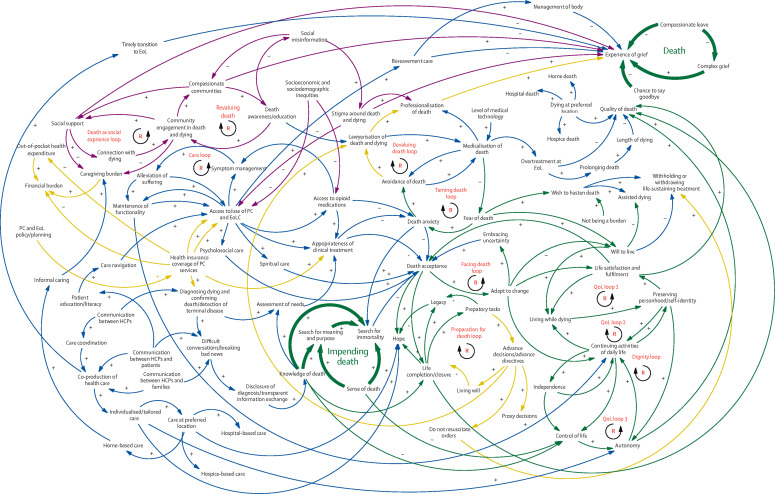
Figure 3 represents one illustration of an aspect of a death system, the end-of-life care system, capturing the complexity, the non-linearity, and the existence of positive and negative feedback loops. The end-of-life system is mapped in a causal loop diagram to show its non-linear and dynamic nature with reinforcing and balancing feedback loops. Arrows track interactions among variables, with polarity noted by plus and minus symbols. The illustrative map centres around two key events—impending death (based on knowledge of death) and death itself—and is primarily focused on the patient's experience of the death trajectory, with the experiences of family and informal caregivers also being incorporated. The map goes beyond physiology to function and health capabilities, which include wellbeing and the capacity to achieve.58, 59 A map of a whole death system would include much more—for example, systems for preventing death and funereal customs.
Figure 3.
An example of a dynamic map of an end-of-life system
EoL=end of life. HCPs=health-care providers. PC=primary care. QoL=quality of life. R=reinforcing loop. B=balancing loop.
Section 4: Philosophical and religious underpinnings of death systems
Many philosophies and religions view life and death as part of a cycle where death is not seen as an ending but as a gateway to the next phase of life. The concept of Samsara—the continuous cycle of birth, life, death, and rebirth—is shared by several world religions, including Hinduism, Jainism, Sikhism, and Buddhism. The cycle of death and rebirth is dependent on karma, whereby actions in one life exert an influence on your future lives.
A belief in the continuity between the worlds of the living and the dead and of the continued existence of and interaction with those who have died underpins many belief systems. With indigenous African philosophies, the belief in the enduring presence of those who have died and of their continued interaction with the living is a defining feature, underpinning all spiritual life.60 Ancestors are not transformed into deities but rather remain as versions of the people they were when living.61 The interconnected nature of the living and the dead, with those who have died remaining present and active in the lives of the living, is a key feature of many African death systems.62
In New Zealand Māori traditions, a dying person must pass through the veil or ārai that separates the physical and metaphysical worlds.63 This transition is the focus of the care provided by the family or whānau at the end of life and allows the person to take up their place in the ancestral world.
Western philosophy, by contrast, has held death to be a final endpoint. In the Phaedo, Plato (429–347 BCE) describes the very activity of philosophising as a practice, or apprenticeship, for death.64 This same notion is taken up by Michel de Montaigne (1533–1592) in his essay That to Study Philosophy is to Learn to Die.65 The contemplative life of the philosopher is a way to approach death in a state of tranquillity. The philosopher seeks to show that death should not be feared. Epicurus (341–270 BCE) argues that “death, the most frightening of bad things, is nothing to us; since, when we exist, death is not yet present, and when death is present, then we do not exist.”66 Montaigne argues that to overcome the fear of death we must become death's neighbour and, in this way, “domesticate” death.65
The three Abrahamic faiths, Judaism, Islam, and Christianity, all share a belief in an afterlife and in resurrection. Judaism teaches that at the moment of death, the body and the soul separate and that while the body may disintegrate, the soul, the self, is eternal. Christianity preaches an afterlife in which after the Day of Judgement the good will reside eternally in heaven, while the sinful will be sent to hell. Belief in an afterlife is one of the six articles of faith in Islam, which believes in separation of the soul and the body after death. All three religions hold that life is a divine gift from God.
Confucianism does not talk about death directly but argues that seeking to prolong life can come at the expense of ren (benevolence, or supreme virtue); it may be necessary to accept death in order to have ren accomplished. Buddhism explicitly understands suffering as natural in four areas – in sickness, ageing, and death, but also in living itself. In Daoism, the context for discussing death is natural law, the way of following nature: death helps us to experience the whole process of life, to take a holistic view on life. Death is interior to life, a necessary part of life according to natural law.
This idea of the balanced natural law allows death to be valued as a homoeostatic mechanism necessary to life. Death is essential to life because without it there would be no life. Without death every birth would be a tragedy. It allows the old to give way to the young, evolution, and renewal. Similarly, death allows for new ideas and progress. As the German physicist Max Planck (1858–1947) observed, science advances not because scientists change their minds but because new generations come along.67 This principle is often paraphrased as “Science advances, one funeral at a time.”
This kind of argument is “consequentialist”: death has value because of consequences it enables or permits. Such arguments predominate, perhaps because it appears irrational to claim that death is valuable in and of itself, but some philosophers have argued just that.
Martin Heidegger (1889–1976) refocused philosophical attention on death from understanding the nature of death to our relation with death.68 He argued that our own death is not something that we can experience directly, whereas we can experience the imminence of our death. We can have a relation with our death which is yet to come. Death stands before us as the one event that it is impossible to avoid. Heidegger argues that it is an event for which no one can take responsibility on our behalf, no one else can die my death for me and through understanding this, facing up to this, and owning one's death, we may authentically become who we are. This points to a way in which death may give value to life.68
The French philosopher Emmanuel Levinas has said, “for us who witness the death of another person…there is in the death of the other his or her disappearance, and the extreme loneliness of that disappearance. I think that ‘the Human’ consists precisely in opening oneself to the death of the other, in being preoccupied with his or her death.”69 With this, Levinas shifts the focus again from our relation with our own death to our relation with the deaths of others. Panel 6 explores in more depth the concept of the value of death as a gift.
Panel 6. The gift of death.
In a recent interview the palliative care specialist and author Kathryn Mannix talked about the bereaved families who were not able to be present when their loved ones were dying of COVID-19: “These people don't know what the real story was and they realise that this not knowing is terrible, that being at a deathbed isn't a duty, but a gift.”70
The distinction between duty and gift takes us to the heart of thinking about the value of death. Duty is often understood as an obligation. In many cultures, caring for an ageing or dying parent is deemed to be a filial duty. In his essay De Brevitate Vitae [On the Shortness of Life], the classical Roman writer Seneca (died 65 CE) reflects on our sense that death comes too early in life, that we always “die before our season”.71 Death comes too soon because we fritter away so much of our lives on worthless activities. We wouldn't, he argues, give away our property, so why give away our lives? This transactional thinking reduces the value of death to what Karl Marx (1818–83) called “exchange value”.
Mannix's notion of the gift challenges this thinking and chimes with the work of the French anthropologist Marcel Mauss (1872–1950), who studied Native American culture and explored how the gift of being with dying people can build human relations based on reciprocity and exceed the regulated contract of exchange: there is a generosity in the gift that goes beyond any possibility of return.72
This thinking is developed by the French Jewish thinker Emmanuel Levinas (1906–95) who recognises that value derives from the uniqueness of a person's death and that one person's death is not simply equivalent to and therefore cannot be exchanged with another.69 There is no way by which the dying person can avoid their death. There is nothing, in that sense, that I can do. In being-for the other in their dying there is no return to be gained on my investment. There can only be loss. In this way, I am with the dying person in the same way that I am with a friend. There is a being-with, a communing, an attending-to, which is an end and a value in itself.
The value of this being-with in death does not derive from what follows as a consequence: the relation itself is the value. But what is the nature of this relation? Levinas talks of “a gratuitous movement of presence.”69 It is gratuitous because it is a giving that not only does not expect any return but that goes beyond the possibility of receiving anything in return. What can we give to the person who is dying? First and foremost, it is a gift of time—to give my time over to the person who is dying. To give time to the other in death is the condition of possibility of the being-with which is itself the condition of possibility of communing with the dying person, and thus in turn of community more generally. In the generosity of the gift of time to the person who is dying, a new sense of value is created, and with it a new possibility for giving value to death and to dying.
This might sound fanciful, but the palliative care physician and writer Kathryn Mannix has said that “being at a deathbed isn't a duty, but a gift”.70 Irish writer Kevin Toolis described attending his father's wake as a gift because it taught him how to die.73 There are also many accounts in both academic studies and general writing of people finding dying to be a positive rather than negative experience.74 Gandhi (1869–1948) talked of the joy he found in nursing his brother-in-law as he died: “all other pleasures and possessions pale into nothingness before service which is rendered in a spirit of joy.”75
For many communities, illness, death, and grief are times at which connections are at their strongest. The Zulu phrase umuntu ngumuntu ngabantu (“A person is a person through other persons”) is a core idea underpinning and defining Ubuntu philosophy, which is sometimes referred to as the African conception of humanism.76 Personhood exists within a community and is premised on connectedness, famously described by the cleric and theologian Desmond Tutu (1931–2021) in his quote: “My humanity is caught up, is inextricably bound up, in yours. We belong in a bundle of life.”77 Kenyan philosopher John Mbiti (1931–2019) has explained Ubuntu (meaning “humanity”) as “I am because we are, and since we are, therefore I am,”78 which contrasts with the saying by French philosopher René Descartes (1596–1650) “I think, therefore I am.” An important application is that “whatever happens to the individual happens to the whole community, and whatever happens to the community happens to the individual as well.”79 When an individual dies, their death is inextricably linked to and experienced by the community.
Religious, philosophical, and spiritual perspectives on death and dying are fundamental to understanding different death systems, informing many of the implicit assumptions, values, and behaviours that define them.
Section 5: Historical origins of death systems
Archaeological exploration of graves and burial sites can provide insights into historical practices around death, dying, and bereavement and the death systems they were part of. Many sites are now major tourist attractions, such as the pyramids in Egypt or the Terracotta Army in China, and they offer important insights into human responses to mortality and loss. Archaeological materials relating to historical care of the dead have been used to facilitate discussions about contemporary death and dying and understand and reflect on biases, expectations, and norms.80
The historian Philippe Ariès (1914–1984) examined death from a Western perspective and identified four phases.81 Before the 12th century he describes a period of “Tamed death,” where death was familiar, and people knew how to die. The dying and their families accepted death calmly; they knew when death was coming and what to do; dying was a public event attended by children. Later came “One's own death,” where death became more personalised. The imminence of judgement, introduced by Christianity, meant the dying had heaven to hope for or hell to fear; they had a stake in their death. The 18th century saw a shift towards “Thy death,” where death began to be dramatised, revered, and feared and was seen as discrete from the normal flow of life. Ariès describes the final phase as “Forbidden death,” which coincides with the arrival of scientific progress and the modern hospital: death is “unwanted and fought against…on the hospital bed, while one is unconscious, alone, and…[trying] to eschew death until the last minutes.”81
The social critic Ivan Illich (1926–2002) argued that death has become steadily medicalised since the Middle Ages.83 In the 15th and 16th centuries, doctors in Palermo, Fez, and Paris argued intensely about whether medicine could prolong life, with many insisting that attempts to interfere with the natural order were blasphemous. The English philosopher Francis Bacon (1561–1626) was the first to describe prolonging life as one of the functions of medicine, but it was another 150 years before this role became a possibility. At first only the rich could expect that doctors would delay death. However, argued Illich, by the 20th century this expectation had come to be seen as a civic right. “Thanks to the medicalisation of death, healthcare has become a monolithic world religion,” writes Illich; “‘Natural death’ is now the point at which the human organism refuses any further input of treatment.”82 He also argued that what he called “mechanical death” had been exported: “The white man's image of death has spread with medical civilisation and has been a major force in colonialisation.” The growing movement to decolonise global health “by grounding it in a health justice framework that acknowledges how colonialism, racism, sexism, capitalism and other harmful ‘-isms’ pose the largest threat to health equity”83 is a response to this historical background, as is the movement to decolonise death studies, death practices,84 and end-of-life care.7
Section 6: Power, discrimination, and inequity in death systems
Death systems are not benign. They can replicate and reinforce discrimination and inequity. Power resides within systems, and the systems often maintain the interests of those holding power.
Individual or community experiences of death, dying, and bereavement are determined by a constellation of factors such as political unrest or conflict, access to and trust in health-care services, relationships, discrimination or oppression, poverty, education, and many others. These determinants interact with each other to create unique sets of experiences for people at the end of life. These non-medical aspects of why, how, and where people die or grieve are understood collectively as the social and structural determinants of death, dying, and bereavement. They share a great deal with the social determinants of health.85
2020 will be remembered as a year in which these determinants of death, dying, and bereavement loomed large. Firstly, the coronavirus pandemic brought death into the daily lives of all people around the world. Understood initially as an indiscriminate virus, infecting rich and poor people equally, data soon emerged showing that mortality and morbidity were concentrated among disadvantaged people, with increased death rates for many minority ethnic communities in high-income countries.86 A second major event of 2020, the murder of a Black man, George Floyd, by a police officer in the USA, sparked a global protest. These events forced wider recognition of the influences of discrimination, inequity, power, and oppression on how and why people die.87
The impact of race, gender, sexuality, socioeconomic status, or other forms of discrimination on mortality rates, access to care, or the incidence of diseases or conditions is well established. Black mothers in the USA are three times more likely to die from preventable pregnancy-related complications than are White mothers88 and this racial difference has persisted despite nationwide efforts to improve maternal mortality. Black Americans are at twice the risk of losing a mother and about 50% greater risk of losing a father by age 20 years compared with White Americans.89 Growing evidence on adverse childhood experiences provides an explanation of how cycles of disadvantage and trauma can persist within families and communities, with important effects on mortality rates.90
People identifying as LGBQT+ have increased rates of preventable deaths and face barriers accessing health services.91 Rates of cardiovascular disease, disability, and poor mental health are higher in adults older than 50 years who identify as lesbian, gay, or bisexual, compared with heterosexual populations.91 Improving access to end-of-life care has been highlighted as a specific challenge.92
Women are traditionally viewed as the caregivers at times of ill-health and dying: women spend on average 2·5 times as much time on unpaid care and domestic work as men.93 The Lancet Commission on Women and Health found that women contribute almost 5% of global gross domestic product through health caring and that about half of this is unpaid work.94 Unpaid caring, much of which consists of caring for ill or dying people, tends to be undervalued and unprotected and is undertaken with little or no training or support.95
The data show inequity across the life course because of race, ethnicity, class, gender, or sexual orientation but people do not experience these factors in isolation. Intersectionality is the understanding of how these factors interact and intersect to create different and multiple experiences of discrimination and disadvantage.96 Being female is linked with disadvantage, but being a migrant woman of colour, an unpaid carer, or a lesbian woman with a disability is likely to bring further disadvantage. In panel 7 , Mpho Tutu van Furth, a Black South African woman, and Commissioner, reflects on race, gender, and the value of death.
Panel 7. Race and the value of death.
“Race is not real, yet it can control us. We now understand that race is an idea constructed by a power elite to justify the dehumanisation of people in order to subjugate, exploit, enslave, and kill them without repercussion.”
Hanuman Goleman97
Mpho Tutu van Furth, member of the Commission, writes:
This Commission has centred the story of the value of death in a relatively wealthy, mostly White, and predominantly western perspective. What this means is that White, western, and relatively wealthy is the norm to which every other experience must refer. Most people in the world do not have to wrestle with an over-medicalised death, they have minimal access to quality health care.
I cannot address the perceptions and experiences of two thirds of the world population. I will speak to my own experience. I am a Black South African woman and the mother to two African American children. In the two contexts in which I lived longest, South Africa and the USA, Black people have never had to engage in a fight to die. Society and the medical world have considered Black lives cheap. I was a teenager when the Soweto uprisings erupted in 1976. I saw then the naked brutality of the apartheid police. I understood then how cheap Black lives were to the White regime. The police first used tear and rubber bullets on the protesters. Then they used batons, rawhide whips, and live ammunition on the children.
Growing up I saw the White flight from ageing and death. I wondered why my mother didn't hide her grey hairs or guard her girlish figure like the mothers of my White friends. “I earned my grey” she would say. She, coming from a culture in which our elders were honoured, even revered. “I have daughters” she would say turning gracefully, and gratefully, into her old age. The cause of death is birth. Black people had no illusion that we could avoid death. Black South Africans did not desire immortality. In death we would be gathered to our ancestors. “Going home” to our forebears was considered the reward for life well lived.
The experience of the vast majority of Black people in the post-apartheid South Africa closely resembles that of African Americans. Although they are putatively citizens of a free non-racist society, health, wealth, and opportunity in South Africa remains largely in the hands of the white population. As in the USA, the referential norm is White. In both societies the Black person is “othered”. The consequences of this othering and the opportunity hoarding which is its partner are evident in the COVID-19 pandemic.
The COVID-19 pandemic was initially described as an equal opportunity assailant striking rich and poor, Black and White alike. It soon became evident that this was untrue. The rich could escape to their second homes. The middle class could, for the most part, work from home. It is the poor who are bearing the brunt of this pandemic. In South Africa one legacy of apartheid is the vast overpopulated Black townships that surround every city. People live cheek by jowl. In many homes there is no running water. Social distancing is an unachievable dream. If they have work, the denizens of the townships are not people who can work from home. This population of cooks, cleaners, and grocery store clerks probably carried the killer virus from the affluent White suburbs to the impoverished townships. For African Americans the story is much the same. In addition to being essential workers, African Americans bear the imprint of the constant stress of institutionalised racism in their bodies. This “weathering” can be the underlying condition that leads to elevated rates of COVID-19 related deaths among African Americans.
The value of death is culture and race bound. In order to ascribe the correct value to death we must assign the right price to every life.
Applying the concept of intersectionality is central to a systems understanding of contemporary death, dying, and bereavement. Different aspects of people's lives intersect to determine how they die or grieve, and recognising the differences can help move systems beyond a traditional model based on western health care.
Power and death
Power is the uncomfortable reality behind systems change. Power exists in relationships, structures, and systems. Often invisible, it underpins all sections of this report, from avoidable mortality, to caregiving, to conceptualisations of a good death. Ageism, ableism, sexism, racism, heteronormatism, or colonialism are all examples of how power can be exerted. Power is often seen as coming from the top, but power also influences relations within families and communities, between patients and health-care professionals, and between communities and statutory institutions.98
There are many examples of power being exerted in death systems around the world. During the first wave of the COVID-19 pandemic in the UK, power structures influenced the indiscriminate placement of do-not-attempt-resuscitation orders for older people living in care homes or for people with disabilities,99 and similarly, personal protective equipment was not provided for staff working in these settings.100 In situations where a family is unable to pay hospital medical bills, hospital staff will often refuse to release the body of the deceased until payment is made. This practice appears to have intensified during the COVID-19 pandemic.
Considering power relationships is essential for understanding social, health, and death systems and how they might be changed. If those with most power—for example, those who control resources, hospitals, and health professionals—are reluctant to change, then change will be difficult.
Section 7: Individuals, families, and communities within death systems
The will to live, death anxiety, and the will to die
The psychological notion of a powerful drive for self-preservation was described as the will to live, wille zum leben, by the German philosopher Arthur Schopenhauer (1788–1860). Schopenhauer's notion derives from the earlier idea of conatus, which is characterised by the Dutch philosopher Baruch Spinoza (1632–1677) in the following way: “each thing, as far as it lies in itself, strives to persevere in its being.” The will to live is influenced by physical and psychological symptoms such as pain, breathlessness, or depression, but is often more strongly influenced by existential factors such as losing hope, the feeling of being a burden, or the sense that life has no purpose or meaning.101, 102 Researchers identify a complex mix of physical and psychosocial variables that influence the will to live: breathlessness, absence of a spouse, and high anxiety all correlated with a low “will to live score.”102, 103 A strong will to live is correlated with low anxiety and a strong religious affiliation.102 The will to live can be influenced by receiving diagnoses such as cancer, but it remains strong for many with metastatic cancer.104 A loss of the will to live correlates with a desire to hasten death and suicidal ideation.105
Ernest Becker proposed that our fear of death is the main force behind much of human culture and behaviour.49 Managing this terror of death has led to several influential theories of death anxiety (panel 8 ), which in turn suggest interventions that might temper the will to live or the wish to die. Regret theory suggests that past regret (of things unaccomplished) and future regret (of things that may not be accomplished) underpin death anxiety and could be mitigated by techniques such as life review and future planning.107
Panel 8. Terror management theory.
Terror management theory106 was derived from cultural anthropologist Ernest Becker's effort to elucidate the motivational underpinnings of human behaviour.49 The theory starts with the Darwinian assumption that human beings share with all forms of life a basic biological predisposition toward self-preservation in the service of survival and reproduction. Humans are, however, unique in their facility for abstract symbolic thought and mental “time-travel.” This facility has allowed humans to proliferate in diverse environments, but it also gives rise to the unsettling realisations that life is finite, death can occur at any time, and we are embodied creatures who are ultimately no more important than lizards or potatoes.
Terror management theory suggests that awareness of death, tragedy, and corporeality engenders potentially debilitating existential terror that has led us to develop defences against this death anxiety. To “manage” existential terror humans embrace cultural worldviews: beliefs about reality that infuse life with meaning and purpose by providing an account of the origin of the universe and prescriptions for standards of social conduct. Meeting or exceeding the standards conduct yields self-esteem: the perception that one is a person of value in a world of meaning. Self-esteem fosters psychological equanimity by buffering anxiety (in general, and of death in particular) in the present and increasing the prospect for immortality in the future. Immortality can be literal, through the heavens, afterlives, reincarnations, resurrections, and the indestructible souls central to most religions; or symbolic, by having children, amassing great fortunes, producing great works of art or science, or being a member of a great and enduring tribe or nation. People are therefore highly motivated to maintain faith in their cultural worldviews and self-esteem as a psychological buffer against existential dread.
Experimental psychologists have tested Becker's theory by conducting experiments exploring how humans behave when faced with reminders of their death.106 The buffer to death anxiety, they suggest, relates to raising self-esteem and helping people to stay connected with their cultural worldview. They find that reminders of their own deaths lead people to fear those with different world views and may also lead doctors towards more extreme medicine. The antidote may be for doctors to become more aware of their own death anxiety in training, and for societal interventions to promote self-esteem in the dying together with opportunities for kindness and more tolerant connection with those different to ourselves.
Accompanying the will to live is the desire to hasten death. A meta-analysis in 2017 of eight studies from high and upper-middle income countries exploring the “wish to hasten death” confirmed that attention to all forms of suffering is a prerequisite to promoting the will to live.108 Pain, fatigue, breathlessness, cognitive impairment, and loss of independence were compelling reasons for a wish to hasten death. Terror due to uncertainty about the future and of the dying process, objectification (“the colon cancer in Bed 4”), the need for self-determination, and the desire to spare others the burden of care were the key existential reasons cited for a wish to die.108
A new cohort of patients to study are those who choose an assisted death in countries where this practice is legal. The results are similar–a sense of burden and a loss of meaning drive the pursuit of an assisted death, rather than unbearable physical symptoms.109 A “sense of aching loneliness,” the “pain of not mattering,” and a sense that their “life story has ended” influenced the wish for death to come sooner.110 However, new relationships can counteract loneliness and suicidal thinking.111
The desire to hasten death may be acceptable in some religions or cultures. Indian culture had a traditionally socially acceptable form of the voluntarily ending of life. In Jainism it is called santara or sallekhana and in Hinduism prayopavesham or samadhi marana. In principle this practice entails a person coming to the realisation that they have no responsibilities or desires left. With the consent of religious elders, the person enters a slow process of fasting, where they give up one item of food a time, so that hunger pangs are tolerable. Over a few weeks or months the person dies, often amid chants. This tradition is much less practised now than in the past, because the social view of what is ethically right has changed and because the legal position is uncertain. The argument in favour of the practice is that it is based on a person finishing responsibilities in the world, coming to a state of no desires, and voluntarily accepting death as the inevitable culmination of life.
There is evidence that the will to live can keep people alive. A study looking at the death records of 70 million Americans found that death rates were much higher after key events such as birthdays, Christmas, and Thanksgiving.112 It is highly likely that emotions, positive and negative, can influence a prognosis, but the tyranny of “positive thinking” can lead to ambivalence, guilt, and bad decisions.113
Grief, bereavement, and mourning
Grief is the natural emotional consequence of attachment and loss, whether it is the loss of limb, country, employment, marriage, or other crucial relationships, and mourning is the public face of that grief. Although there are many sources of loss, the word bereavement refers specifically to the loss of an important relationship through death and can be associated with many physical and mental health problems.114, 115 Bereavement can also lead to sudden death of a surviving partner or to suicide.116
The psychiatrist Elizabeth Kübler-Ross (1926–2004) described the “five stages of grief” in 1970, suggesting that people who are bereaved must move through denial, anger, bargaining, depression, and acceptance to complete their grief.117 More recent theories state that grief is not something to be completed but rather something to be integrated into the bereaved person's life. The grief counsellor Lois Tonkin has proposed a model of “growing around grief”: grief does not fade away but becomes part of the person and life of the grieving.118 Similarly, with the “dual process model”, the grieving accept their loss but also confront it, creating a new relationship with the person who has died.119 With the “continuing bonds” model, the aim is not to detach from the person who has died but to create and celebrate continuing bonds with the person.120 All these models describe the importance of continued connection with those who have died, mirroring many religious or spiritual perspectives on death and grief.60, 63
A central component of many mourning practices is a funeral or a formal disposal of the dead body. Functions of a funeral vary but can include: an opportunity to reflect on the life of the deceased person, to ease their passage to the next life, to demonstrate love and respect for the deceased person, or for the community to say goodbye and to support each other in grief. The absence of funerals, or attendance of pared back, virtual funerals during the COVID-19 pandemic prompted many people to reflect on their role in death systems. A recent rapid, mixed-methods review explored the evidence of effect of funeral practices on bereaved relatives' mental health and outcomes; although the review was inconclusive, qualitative evidence underlined the importance of the bereaved being able to shape the rituals in a way that was meaningful for them.121 The review also highlighted the important role that funeral staff play in supporting bereaved people, a finding supported by other studies.122
Relationships and social networks
Multiple studies in recent years have emphasised the role that relationships and social networks play in a range of areas, including smoking,123 obesity,124 and survival,125 overshadowing the role of health-care interventions. Relationships are important beyond their role in health outcomes—they influence all aspects of our lives and deaths. Carlo Rovelli, a quantum physicist, has stated that relationships are fundamental to the universe and all life: we only exist in relation to others, and “reality is made up of relations rather than objects”.126
Placing relationships rather than interventions or treatments at the centre of people's lives and deaths requires a shift across all aspects of society. In Radical Help, the social entrepreneur and designer Hilary Cottam describes what this change would look like for the welfare state in the UK, arguing that traditional services and institutions based on fixing problems for people are outdated and out of step with modern challenges.127 Instead, the focus should be on supporting individuals, families, and communities to build their own capabilities and connections with each other. She writes: “Relationships—the simple human bonds between us—are the foundation of good lives…Without strong bonds with others, or with unhealthy relationships, very few of us can feel fulfilled—or even function.”127
Although death and dying are increasingly controlled by health systems, most care of the dying, hour by hour, is the responsibility of the dying themselves, family, friends, and the community. When patients are in hospital, nurses spend about 5% of their time in face-to-face interactions with patients128 and doctors spend only about 13–15 minutes a day in contact with an individual patient.129 The time spent with patients dying at home is even less. This situation has been termed the 95% rule, meaning that 95% of the care of the dying is undertaken by lay communities130 despite the dominance of health-care systems.
In many settings around the world, the communities undertaking this 95% of care are experienced, knowledgeable, and capable in supporting people at the end of life, but for others, this confidence has slowly been lost. Kevin Toolis describes in My Father's Wake how his family and community managed the dying, death, wake, and burial of his father in the village where he was born in rural Ireland.73 The traditional Irish way of death is no longer present in the cities and is fading in the countryside, but Toolis thinks that something of the tradition can return. Many people were present as his father died, and his dying merged with his wake. Not only his family but the whole village, including children and teenagers, came to the wake, touching the body, drinking tea, and telling stories, often sharing stories of tragedies that had not been shared before. “A rite that survived the fall of Troy and a thousand generations before the rise of the Western Death Machine can easily survive the retransplantation back to our cities of glass and concrete. We need to find our way again with death. To be human is to be mortal, and to be mortal is to love, live and die amidst the lives of everyone around you on the island or in the city. And to embrace rather than deny our mortal fate.”73
Efforts to support this retransplantation can be seen around the world. The death doula movement is an attempt to build skills and capacity relevant to death within communities.131 The movement challenges professionally led models of support for people dying, while acknowledging that many individuals or families do not have the skills or confidence to care for someone as they die. Navigating death systems can be difficult, and death doulas can challenge established norms such as where someone is allowed to die or be buried, or the role family members can take in caring.132
The global compassionate communities movement aims to build community capacity in end-of-life care.3 It developed in response to the professionalisation of care for those dying and grieving and the increasing marginalisation of communities from that caring.133 Some projects begin when services such as hospices or clinics engage in a dialogue with local communities to understand experiences, wishes, and challenges around death, dying, and care, while others develop from lay communities themselves. They are based explicitly on the principles of community development—people taking action on issues that affect them and building skills that they can use to support themselves and others.
In compassionate community projects, people form networks in their village or on their street and identify and support those who are dying, caring, or grieving. If a service such as a hospice or clinic is involved, it supports this process by creating a space for these networks to grow, providing clinical support, sharing knowledge and skills, linking members of the community, and ensuring safety and legitimacy: many people are fearful of knocking on others' doors and wish for support to do so at the start. The result is often a partnership between lay community networks and professional networks. These networks are often working in isolation and attempts to bring them together are essential.133
Compassionate communities now exist in 19 countries, including India, Australia, Canada and the US, and countries in Europe and Latin America.134 They are a global movement with an international association.135 The Lien Foundation quality of death index now includes measures of community engagement in its assessment of the quality of services.136 The movement has been important in challenging professionally dominated models of palliative care.137
Disadvantaged communities
Naturally occurring community networks, or ones that are newly created through initiatives such as compassionate communities, may exist in many countries and communities, but they are by no means a given. Research has shown that areas with high levels of poverty and social disadvantage have smaller networks and a lack of relationships across and within communities,138 particularly with local services such as the police, housing, and health care, increasing their sense of isolation and abandonment.139 In such places the conditions for developing partnerships first need to be created. Asset-based approaches, which start with people's lived experience of the area and recognise the strengths and capacities of people to support and affect change, are increasingly being advocated to create these conditions. These developments need service providers to understand the barriers to living well as a starting point for conversations about death and dying and working in partnership.
Some of the social norms for caring, dying, and grieving can reinforce and perpetuate inequities. For example, widows are some of the most marginalised women in the world. In many communities, women's status and security comes from (heterosexual) marriage. When a woman's husband dies, she can be stigmatised and banned from inheriting property or assets, prevented from subsequent employment, or forced into further marriages or damaging cleansing rituals.140 These deeply rooted cultural practices have been highlighted as contributing significantly to gender inequality and gender-based violence around the world. While many of these practices are seen in low-and-middle-income countries, widowhood predisposes to disadvantage in many high-income settings. In the USA and Germany it can manifest as pensioner poverty or limited health insurance.141 Women or men in same-sex relationships can be similarly disadvantaged when their partner dies, as they may be banned from inheriting property or assets and excluded from funerals or mourning rituals. This disadvantage may happen particularly in countries that do not allow or recognise same-sex marriage or civil partnerships and can predispose to disenfranchised and complex grief.142
Societal and civic responses
A vibrant countercultural death movement is building in many countries with death cafes,143 festivals,144, 145 awareness weeks,146 or public campaigns.147 These movements illustrate that large groups in communities do wish to talk collectively about death, dying, and loss and are creating new opportunities in society to do so. Many widely read books have been published recently on how to die, the process of dying, and understanding our mortality. Setting death and dying in their social or cultural context through a best-selling book, an interactive exhibition in a shopping centre,148 or as the story line in a telenovela can bring powerful change in how people see or understand them. Evidence suggests that talking collectively about these issues can lead to an improvement in people's attitudes and capabilities for dealing with death.149
In response to Taiwan having one of the fastest ageing societies in the world, Taipei City has led an ambitious programme of activities to promote discussion and action on issues of ageing and death. It has embedded the Compassionate City Charter throughout the city. This charter draws on the Healthy Cities public health movement150, 151 and outlines the steps a city, town, or village can take to normalise death and dying and create a society that supports them. It now has several initiatives throughout the city involving schools, businesses, and temples supported by the mayor and council. These initiatives are exploring what it means to have a good death and death literacy of citizens.152
Death, dying, and grief have not been immune to the far-reaching impacts of social media. A host of new virtual spaces now exist to share and discuss illness, dying, death, and grief. Social media provides opportunities for online communities to come together to grieve collectively. A person can design a goodbye message that will only be visible to others after their death, or curate their social media feed or digital legacy that others will see after their death.153 When Facebook is informed that a user has died, it converts the page to a memorial page. It is estimated that by 2098 there will be more accounts held by dead members than by those who are alive, meaning that Facebook might come to represent a global virtual cemetery.154 Social media profiles allow the continued connection and interaction between the deceased and the bereaved that contemporary models of grieving support (see above).
A good death
A recent meta-systematic review of the conditions for a good death found 11 conditions, which in order of importance are: relief from physical pain and other physical symptoms; effective communication and relationship with health-care providers; the performance of cultural, religious, or other spiritual rituals; relief from emotional distress or other forms of psychological suffering; autonomy with regards to treatment-related decision-making; dying in the preferred place; life not being prolonged unnecessarily; awareness of the deep significance of what is happening; emotional support from family and friends; not being a burden on anyone; and the right to terminate one's life.155 The authors observe that “Most conditions for a good death could be offered to most dying people, without costly medical infrastructure or specialized knowledge.”
These systematic reviews drew on studies across 16 countries, all of which were high-income or upper-middle-income countries. Less is known about people's preferences in low-income and middle-income countries. One study of perceptions of a good death in northern Tanzania found some congruence with the themes from existing systematic reviews but highlighted cultural values that prioritise community and family above self.156 This is an important finding, reported in other studies, but often missing as Western narratives of autonomy dominate published reports.
Ideas of what constitutes a good death are not new. Historical texts such as Ars Moriendi and Bardo Thodol or the Tibetan Book of the Dead preceded the ever-increasing number of best-selling books, research studies, guidelines, and media stories today. Society and culture exert a strong influence over the conceptions of good or bad deaths, and the behaviours of people dying, caring, or grieving can follow strictly enforced social norms. With health care's movement into death and dying, it too has imposed a set of clinical requirements on those dying and caring. Many of these cultural, religious, and clinical requirements can support those dying by guiding care from the family, prioritising pain relief, or prescribing rituals and a structure for those bereaved. But, as with other social norms, those who deviate may be subject to moral judgment or sanctions.
This burgeoning industry surrounding the good death has led many to fear that the pressure to achieve a good death may be undermining the experience of dying itself. While it is important to understand what people value when dying, an unintended consequence may be a pressure on dying people and their families to experience the good death laid out by these criteria and a sense of failure if they fall short. There are parallels here with the social pressure in some countries on women to have a so-called natural birth.
The writer and former palliative care physician Columba Quigley wrote: “Life is a messy and often chaotic experience, yet we seem to be on a mission to tidy it up neatly at the final hour. Death is unknown to all of us and adding an adjective like ‘good’ does not make it any more knowable. Medicine struggles with this not knowing, so we try to control the beast by prescribing a more palatable version, one that creates an illusion of certainty. By defining the ‘good death’ as a list of tick-boxable criteria, we are losing sight of the individual. The concept of the good death objectifies those in the Land of the Dying by attempting to attach medically manageable, quantifiable measures to a wholly subjective experience.” (C Quigley, personal communication)
Omission of death and dying from health conversations and reports
This Commission takes the view that death and dying are a part of life, but that they are often treated as if they are not. The existence or otherwise of a taboo on death and dying has stimulated much debate, but what is certain is the omission of these experiences from health reports, policies, and strategic documents. A study of the strategies of 152 health and wellbeing boards in England identified 150 strategies, and end-of-life care was mentioned in only 78 (52%) and prioritised in only six (4%).157 As the study observed, prioritisation of end-of-life care has been the subject of extensive rhetoric, but the implementation falls very short.
Claire Morris, director of advocacy for the Worldwide Hospice Palliative Care Alliance, tells the story of arriving late for a meeting with a British overseas aid minister and finding the representatives of organisations concerned with heart disease, cancer, AIDS, malaria, and tuberculosis already there. “Thank goodness you've come,” said one of the representatives, “now we can talk about end-of-life care” (C Morris, personal communication). The implication is that these representatives for diseases that kill tens of millions every year would not otherwise have felt able to discuss end-of-life care.
As an example, we examined reports on healthy aging from WHO,158 the US Institute of Medicine,159 and the UK All Party Parliamentary Group for Longevity,160 and they either make no mention of death and dying or mention it in a single sentence or two. It is as if dying is not part of healthy ageing. The Lancet has pointed out that WHO advice on responding to COVID-19 made no mention of palliative care,161 while the Lancet Commission on Liver Disease does not mention dying from liver disease.162 Even the important report Health Equity in England: The Marmot Review 10 Years On does not discuss death or inequalities in dying.27 The UK National Health Service (NHS) Ten Year Plan for England includes end-of-life care in only part of a single paragraph in a report of more than 120 pages, despite the fact that deaths will increase by more than 10% in the next 10 years.163
Section 8: Choice and consumerism in death systems
“‘Natural death’” is now the point at which the human organism refuses any further input of treatment…. Dying has become the ultimate form of consumer resistance.”
Ivan Illich82
In recent years there have been major shifts in the relationship between health professionals and patients and in the expectations of patients and the wider public of health-care services.
The 1960s counterculture challenged the conventional hierarchies of power. The sociologist Erving Goffman (1922–1982) popularised the notion of “total institutions” like hospitals where behaviour is controlled and people are treated alike.164 Eliot Freidson (1923–2005), another sociologist, exposed medical paternalism and power;165 and social philosopher Michel Foucault (1926–1984) documented how power operated in institutions and showed how the doctor's knowledge of the patient's body is the basis of medical power.166
This critique of professional power had major consequences in that it changed the communication between doctor and patient. The sick person was recast from a passive patient taking a doctor's orders to an active agent making choices about her or his own life. Nowhere was this shift more clearly seen than in cancer in the 1970s in countries such as the UK and USA, countries that prioritise individual autonomy. Here doctors moved from not disclosing to patients that they had a terminal diagnosis or discussing prognosis to telling them that they were dying.
Over the same time some people have come to expect much more from services. A renowned UK oncologist, Karol Sikora, recently said on a primetime news programme: “We're a consumer society. Anything we want is just a click away. Yet the NHS is the last bastion of communism.”167 He was implying that unfettered choice is a citizen's right and that the state has an obligation to meet these choices. But how does this fit with universal health-care systems in which the concentration is on need, not demands, and not everything can be available to everybody? Drawing parallels with services that are “a click away” may also promote the magical thinking that longevity is purchasable.
But while some people want more from health services, others want less, or want the right to end their lives when or as they choose.
Assisted dying
Suicide is no longer illegal in most countries. By contrast, helping someone to end their life, for example by providing them with lethal drugs is, in most countries, a criminal offence (known as “assisting a suicide”). It makes no difference to the criminal nature of the action whether the person was dying or requested death, or the action was compassionate.
Increasingly, however, across the world, governments are creating exemptions to the criminal acts of suicide and culpable homicide to allow for medical assistance in dying. Worldwide, approximately 100 million people now have access to some form of assisted dying legislation. Assisted dying is lawful in nine US states and the District of Columbia, Canada, the Netherlands, Belgium, Luxembourg, Spain, Switzerland, and four Australian states. New Zealand has passed legislation that was approved in a national referendum in 2020. The Constitutional Court of Colombia legalised assisted dying, but the government has not yet legislated. Assisted dying is being debated in many countries and legalisation appears likely to spread.
Switzerland is unusual in never having had a complete prohibition on assisting suicide. This has resulted in the outsourcing of assisted dying from countries where it is banned to organisations in Switzerland. People seeking to end their lives in Switzerland must be able to self-administer the medication, making the process “suicide” rather than “murder”. Data from one of the organisations, Dignitas, show that from 1998 to 2018, 2591 people from 53 countries came to die, mostly from other European countries—Germany (1237), Great Britain (415), France (330) and Italy (129)—but also from the USA (101), Canada (64), Israel (51), and Australia (32).168
The nature of assisted dying varies among different jurisdictions, providing opportunities to inform debates with evidence and practical experience. We consider here the situations in Oregon, USA, and in Canada.
The Oregon Death with Dignity Act came into force in 1997 “because a majority of voting Oregonians believed that persons afflicted with certain terminal illnesses should have the legal right to hasten their deaths.”169 By January, 2021, a total of 2895 people had received prescriptions for the lethal dose of medication, and 1905 people had died from ingesting the medication, in Oregon since legalisation in 1997.170 The number of assisted deaths increases steadily each year: there were 245 in 2020, compared with 191 in 2019. In 2020, assisted dying accounted for 0·6% of deaths. Most patients were aged 65 years or older (81%) and White (97%) and had died of cancer (66%) or heart disease (11%).170
The Canadian legislation came about in 2015 in the province of Quebec (and 2016 in the rest of the country) after the Supreme Court ruled that the blanket ban on assisted dying was contrary to Canada's Charter of Rights and Freedoms. The law allows a broader range of people than in Oregon to apply for assisted dying, and people can opt for injections from clinicians or to take the drugs themselves. In some parts of the country up to 7% of people die with medical assistance, but Canadian authorities expect the figure to stabilise at about 4% for the country.171
In Oregon and Canada, those applying for assisted dying must be citizens, to prevent so-called death tourism. They must be aged 18 years or older and capable of consent when applying for assisted dying. None of the jurisdictions allows assisted dying in response to advance directives, although this practice has been recommended in Canada.171 In Oregon the applicants must have a terminal disease and be expected to die within 6 months. Canada has no time specification but requires a “a grievous and irremediable medical condition” and initially a “reasonably foreseeable death”; this latter requirement has been struck out by the courts, making assisted dying now available to people with intolerable suffering from any cause. In practice, people who receive assisted deaths are predominantly older than 65 years, White, and well-educated, and most (around three-quarters) have cancer.171
In Oregon only doctors can provide assisted dying, but Canada allows nurses as well. No clinician is obliged to provide assisted dying, although in Canada doctors do have an obligation to pass on requests to those willing to provide assisted dying.
Both jurisdictions have specific application processes, but one key question is whether clinicians can introduce to patients the option of assisted dying. In Canada they can, and there is guidance on doing so.
Canada and the US jurisdictions with assisted dying have reporting requirements, which make public how many patients obtained a prescription and how many patients ingested the drugs, as well as key demographic data.172
There are further questions that demand more societal or policy responses than legal, and that require more research as systems of assisted dying are embedded and extend (panel 9 ). Countries and states thinking of introducing assisted dying need to consider all these questions, and increasingly there is an evidence base to study.
Panel 9. Societal and policy questions regarding assisted dying.
-
•
What are the societal costs of legalising and not legalising?
-
•
Does legalising assisted dying increase or decrease suicide rates?
-
•
Does not legalising encourage underground practices (as with illegal abortions)?
-
•
Is trust in doctors affected?
-
•
What safeguarding measures are needed?173
-
•
What are the economic costs and benefits?
-
•
Does legalising assisted dying undermine palliative care?
-
•
Should those undergoing assisted dying be allowed to donate organs?
Advance care planning
Advance care planning aims to explore, document, and share a person's wishes about their future care, such that when they are no longer able to communicate their wishes can continue to be respected.174 It is a complex intervention concerned with personal reflection, knowledge about disease trajectories and likely changes, discussions with family and clinicians, and interaction with health-care systems. The components of advance care planning vary among countries, but they include: general expressions of wishes for care (advance statements); decisions made in advance that have legal force (advance directives); surrogate decision makers (powers of attorney); and decision-making processes by others (best interests or substituted judgment).
A review of systematic reviews published in 2018 found weak evidence that advance care planning can lead to improved communication at the end-of-life, dying in the preferred place, and health-care savings.175
Most research into advance care planning comes from high income countries, which has led to an overemphasis on autonomy and individual decision making. Family-centred or relational frameworks have received much less attention. The adaptation of existing models of individualised advance care planning to include collective decision making is a priority.
Most discussions focus on the refusal of health-care interventions, but for many people around the world, the refusal of such interventions is irrelevant, as basic health-care services are often inaccessible.
More recent innovations seek to use advance care planning as a tool to promote wellbeing rather than simply reducing harm. Uptake and outcomes might be improved by placing decisions about refusing certain treatments in a broader narrative about how people would wish to be cared for, the trust they wish to develop with health-care professionals and services, how they might be supported to live in the best way until their death, and the role and presence of family and friends.176
Advance directives
Advance directives are legal statements that allow patients to refuse treatment should they become unable to consent. Internationally the first statute to permit advance refusal of life-sustaining treatment was the Patient Self-Determination Act 1991 in the USA.177 It was passed in the wake of the case of Nancy Cruzan, who had been in a vegetative state for nearly 7 years by the time her parents' application to withdraw her feeding tube reached the Supreme Court. Initially this request was denied on the basis that “clear and convincing evidence” was required that she would not have wanted life-sustaining treatments. Within a month of the ruling, the Society for the Right to Die had received nearly 300 000 requests for advance directive forms from people trying to ensure that “clear and convincing evidence” was available should they themselves ever be in that situation.
In India the historic Supreme Court judgment of March, 2018, authorised “living wills” enabling people to refuse life-sustaining treatment in advance if they were to become terminally ill or if they were in a permanent vegetative state. This event followed the national debate occasioned by an application to withdraw life-sustaining treatment from Aruna Shanbaug, a young nurse in Mumbai who was raped, strangled, and left to die. She was then maintained for 42 years in a vegetative state in the hospital where she had worked.
Advance refusals can be important to individuals precisely because families sometimes fight for treatments that the patient themselves might have refused, and because family members can disagree about what the person would have wanted, causing distress and delay.
Ethical commitments can make it hard for doctors, families, and lawmakers to consider withdrawing life-sustaining treatments even when the patient, or their family, do not want treatment to be continued. Without a written attestation from the patient, it can be the case that “doctors and families often just don't know a patient's wishes and fear the awesome responsibility of guessing what the patient would have thought was best.”177 A formal record of treatment refusals (and making sure that people know about it) offers the best available protection for individuals seeking to avoid “a fate worse than death.” The case of Polly Kitzinger, who did not have an advance directive, explores this concept further and is included in the appendix.
Defensive medicine, litigation, and the courts
The main involvement of lawyers in death historically has been with wills and estates, but lawyers today are often involved with advance decisions or lasting powers of attorney. They are also increasingly involved through patients, families, and doctors resorting to the courts as the means of ruling on the cessation or continuation of life-sustaining treatment.
There have been several high-profile cases in England in which the parents of dying children could not reach an accord with their doctors. In the cases of Charlie Gard and Alfie Evans, both very young children with life-limiting conditions, the hospitals involved sought permission from the High Court to withdraw treatment. In both cases, the court ruled in favour of the doctors. Both children have since died. In France, the case of Vincent Lambert, who died in July, 2019, after more than a decade in a persistent vegetative state, divided both the nation and his own family. He died after France's highest appeal court allowed doctors to withdraw life-support.
There is a consensus that such disputes should, where possible, be resolved without recourse to the courts. The Irish senator and lawyer Michael McDowell has publicly criticised doctors for their over-readiness to use the courts: “Doctors confront a difficult medicolegal situation and decide to resolve their difficulty by bringing about litigation in which their ethical options and duties are effectively transferred to the judiciary”.178 Hospital ethics committees and professional mediation might remove some of the onus from individual doctors. The age of deference to authority figures such as doctors has passed; we live in the age of shared decision-making, democratisation of knowledge, and social media. It is likely that these disputes will become more common, making it important to improve the ways of resolving them.
Section 9: The economics of the death system
SunLife Insurance has analysed the cost of funerals and ceremonies at the end of life across 35 countries where data were available and found that the country with the highest expenses was Japan, where the average cost was 3 million Yen (£22 320), two-thirds of the average annual salary.179 Other countries with high expenses for the end of life in terms of the proportion of average annual salary were China (45%) and Germany (16%). The countries with least expenses were Russia (1·3%), Poland (2·3%), and India (2·4%). Costs for end-of-life care are tending to increase ahead of inflation: in Britain, SunLife reported, costs have risen by 39% since 2010, some 10% higher than the rate of inflation.180
These costs can come suddenly and put great financial pressure on families and may push some into poverty. But a more common cause of poverty and bankruptcy is catastrophic health costs, at least some of which are spent on treatment at the end of life, when the treatment for the dying patient may be both futile and increase suffering.
A 2007 study defined expense on medical care as catastrophic if it was more than 40% of an individual's “capacity to pay” and used that definition to estimate that 150 million people annually were impoverished through catastrophic expenditure on health.181 The World Bank and WHO, which define expense on medical care as catastrophic if it is more than 10% of a patient's overall income, reported 926·6 million people in 2015 to have incurred catastrophic health expenditure.182 The World Bank and the UN reported that half the world's population in 2003 was at risk catastrophic expenditure from having to pay for surgery.183 That proportion has fallen to a quarter globally, but it remains at about half for people in sub-Saharan Africa.183 Medical costs are the most common cause of bankruptcy in the USA, a high income country without universal health care.184 Many people, including those in lower income countries simply forego or have no access to treatment.
Some of the catastrophic health-care expenditures are likely to be at the end of life, but global data are not available on how many people and their families are impoverished from paying for such care. A study from China of 792 patients with cancer who died between June 2013 and June 2016 found that 80% of the patients received life-extending treatment, with more than 94% of the families experiencing catastrophic health expenditure and more than four-fifths falling below the poverty line as a result.185
Health spending, including both government and private out-of-pocket spending, now averages roughly 9% of gross domestic product (GDP) in high-income countries. Use of healthcare—and therefore costs—increase steadily in the last year of life, particularly in the last month, as figure 2 shows with data from England.43
Spending on those in the last year of life accounts for a disproportionate share of total health care spending.186, 187 For example, between 8% and 11·2% of annual health-care expenditures for the entire population in the USA, Taiwan, and the Netherlands are for the less than 1% of the population who die during the year (table 4 ).187 This disproportionate share of spending at the end of life has been identified as evidence of wasteful health spending or overtreatment,202 but determining whether treatment was inappropriate, appropriate, or futile depends both on how the terms are defined and on whether one considers the perspective of the individual patient or that of society.
Table 4.
Share of total annual health expenditures going towards people who die
| Year | Age group | Type of expenditure* | Percentage of study population who died in calendar year | Percentage of total health-care costs towards those in their last year of life | |
|---|---|---|---|---|---|
| Australia (New South Wales) | |||||
| Kardamanidis et al, 2007188 | 2002 | >65 years | Hospital | 3·5%† | 20·1% |
| Canada (Ontario) | |||||
| Tanuseputro et al, 2015189 | FY 2011 to FY 2013 | All ages | Total | 0·66%† | 10% |
| Canada (Quebec) | |||||
| French et al, 2017187 | 2011 | All ages | Hospital | .. | 22·73% |
| Canada (British Columbia) | |||||
| Payne et al, 2009190 | 2001 | >65 years | Total | 4·2% | 22% |
| Payne et al, 2009190 | 1991 | >65 years | Total | 3·8% | 20% |
| Denmark | |||||
| French et al, 2017187 | 2011 | All ages | Total | 0·87%† | 10·95% |
| England | |||||
| French et al, 2017187 | 2011 | All ages | Hospital | .. | 14·59% |
| Aragon et al, 2016191 | FY 2011 | All ages | Hospital | 4·19% | 10·4% |
| Finland | |||||
| Häkkinen et al, 2008192 | 1998 | >65 years | Total | .. | 14·3% |
| France | |||||
| French et al, 2017187 | 2011 | All ages | Medical | .. | 8·5% |
| Germany | |||||
| French et al, 2017187 | 2011 | Privately insured‡ | Total | 0·35% | 10·96% |
| Japan | |||||
| French et al, 2017187 | 2011 | < 75 years | Medical | 0·67% | 5·93% |
| Netherlands | |||||
| French et al, 2017187 | 2011 | All ages | Total | .. | 10·01% |
| Polder et al, 2006193 | 1999 | All ages | Total | 0·89% | 11·1% |
| Stooker et al, 2001194 | 1993 | All ages | Medical | .. | 10% |
| Norway | |||||
| Melberg et al, 2013195 | 2010 | All ages | Hospital | 3·7% | 10·6% |
| South Africa | |||||
| Ranchod et al, 2015196 | 2011 | Privately insured‡ | Medical | 1·2% | 5·38% |
| Ranchod et al, 2015196 | 2010 | Privately insured‡ | Medical | 1·2% | 6·57% |
| Ranchod et al, 2015196 | 2009 | Privately insured‡ | Medical | 1·2% | 5·23% |
| Ranchod et al, 2015196 | 2008 | Privately insured‡ | Medical | 1·2% | 3·93% |
| Taiwan | |||||
| French et al, 2017192 | 2011 | All ages | Total | 0·66% | 11·2% |
| USA | |||||
| French et al, 2017187 | 2011 | All ages | Total | 0·68%† | 8·45% |
| Aldridge and Kelley, 2015186 | 2011 | All ages | Total | 0·68%† | 13% |
| Riley and Lubitz, 2010197 | 2006 | >65 years | Medicare | 4·5%† | 25·1% |
| Riley and Lubitz, 2010197 | 1978 | >65 years | Medicare | 4·5%† | 28·3% |
| Hogan et al, 2001198 | 1998 | >65 years | Total | 5% | 27·4% |
| Hoover et al, 2002199 | 1996 | >65 years | Total | 5%† | 22% |
| Calfo et al, 2015200 | 1999 | >65 years | Medicare | 6% | 27·9% |
| Calfo et al, 2015200 | 1998 | >65 years | Medicare | 5·9% | 27·8% |
| Calfo et al, 2015200 | 1997 | >65 years | Medicare | 5·8% | 27% |
| Calfo et al, 2015200 | 1996 | >65 years | Medicare | 5·7% | 26·7% |
| Calfo et al, 2015200 | 1995 | >65 years | Medicare | 5·6% | 26·5% |
| Calfo et al, 2015200 | 1994 | >65 years | Medicare | 5·5% | 26·5% |
| Lubitz and Riley, 1993201 | 1988 | All ages | Medicare | 4·6%† | 28·6% |
| Lubitz and Riley, 1993201 | 1985 | All ages | Medicare | 4·8%† | 27·4% |
| Lubitz and Riley, 1993201 | 1980 | All ages | Medicare | 4·9%† | 30·8% |
| Lubitz and Riley, 1993201 | 1976 | All ages | Medicare | 4·7%† | 28·2% |
FY=financial year.
Total: includes expenses for hospital stays, doctor visits, pharmaceuticals, nursing home care, and other long-term care. Medical: expenditure hospital services (inpatient, outpatient, emergency) and other professional medical services such as dental care, pharmaceuticals, etc. Does not include nursing home care and long-term care. Hospital: expenditure on inpatient, outpatient, and emergency care incurred in the hospital setting. Medicare: expenses covered by the Medicare plans A and B in USA, available only for people older than 65 years, people younger than 65 years who have a disability, and patients with end-stage renal disease.
Data from Canada (Ontario and British Columbia), Finland, France, Netherlands (Polder et al, 2006; Stooker et al, 2001), Taiwan, and USA (all except data from Calfo et al, 2015, and Hogan et al, 2001) cover beneficiaries who were users and non-users of the available health-care services. Where utilisation statistics were available, percentages of study populations who died in the calendar year have been adjusted to users-only for these studies. In Australia (NSW), 4% of the population older than 65 years died during the study period. 82·7% of the population older than 65 were hospitalised at least once in their last year of life. Data from Denmark, the Netherlands (French et al, 2017), and Taiwan are drawn from full population administrative databases that cover all health expenditures including long-term care expenditures. Deaths reported for these countries are for the entire population. Data from Australia, Canada (Quebec), and England cover only inpatient hospital expenses. Data from Norway cover both inpatient and outpatient hospital expenses. Deaths are limited to the population with hospital related use or expense in last year of life. Data from Australia, Canada (Quebec), Denmark, England, Germany, Japan, Netherlands (French et al, 2017; Stooker et al, 2001), South Africa, and USA (Calfo et al, 2015; Hogan et al, 2001) analyse expenditure only for health-care service users. Data from Denmark, England, France, Netherlands, Norway, Taiwan and USA (Aldridge and Kelley, 2015; French et al, 2017) are representative of the country's full population. For studies where data on Medicare use were inaccessible, average use between the years 2008 and 2013 (91%) was used. The percentage of the population who died in a year in South Africa (Ranchod et al, 2015) is the average for mortality data available from 2008 to 2011 for the study population.
Includes all ages.
Classic economists define overtreatment as any treatment where the costs exceed the value of the benefits received. They believe that consumers are rational and can weigh the costs and benefits (both monetary and non-monetary) of their decisions to make optimal choices. Using this definition, high expenditure at the end of life is not evidence of overtreatment from the patient's perspective. In fact, one might reasonably conclude the opposite: Nobel prize-winning economist Gary Becker and colleagues argue that if a person's wealth has no value after death (that is, if they do not care about leaving a bequest) then they should be willing to spend all of their money on treatments even if they only marginally extend life and or have only small chances of success.203 Many new treatments do extend life only marginally and have low success rates—and yet are very expensive.
Hope and bias as causes of overtreatment
As the benefits of treatment are uncertain, calculation of expected treatment benefits requires awareness and understanding of probabilities. Individuals who are uninformed or misinterpret probabilities may overestimate the benefits. There is evidence that people do overestimate the benefits, especially those with serious illnesses.204 In one study of 1193 patients receiving palliative chemotherapy for advanced cancer, two-thirds of patients with lung cancer and four out of five patients with colorectal cancer expected the treatment to cure their illness, even though the treatment was not intended to be curative.205 While the details of the communication between oncologist and patient were not studied, the findings show that participants may not comprehend the intention of their treatment, or attach different meaning to it, calling into question the basis of the informed consent for the treatment.
Hope can encourage people subconsciously to access only a subset of relevant information that is consistent with a desired outcome.206 The mind discounts information that is not consistent with the desired outcome (confirmation bias) and by not updating beliefs when new information runs counter to the desired outcome (optimistic update bias).207, 208 Hope also increases the likelihood that people will believe that their illness is less serious than objective data might support, allowing patients to hold onto a low possibility of a favourable outcome and disregard the much greater probability of an unfavourable outcome.209 A recent study of patients with advanced cancer confirms that higher levels of hope increase all these biases.210 Carers, whose level of hope may exceed that of their loved ones, have these same biases.
Doctors are also biased in their assessment of the benefits of treatment for patients with life limiting conditions.211 Clinicians may recommend treatments if there are any potential benefits, irrespective of costs. They may also recommend additional treatments because to do so is easier than trying to communicate the futility of additional interventions. Lastly, they may recommend additional treatments as a way for the patient to maintain hope, despite the clinical futility.211 These phenomena can lead to overtreatment for individual patients at the end of life.212, 213
Third-party payment as a cause of overtreatment
Nearly all high-income countries, and many low-income and middle-income countries, offer publicly funded health care. There is some evidence that public funding results in patients possibly receiving more treatment than they would receive if they had to bear the full costs personally themselves.214 The RAND Health Insurance Experiment (1971–1986) found that when consumers were required to finance their own health care, spending was about 30% lower, suggesting that about a third of health care would fit an economist's definition of overtreatment.215
This type of overtreatment due to third-party funding might be greater at the end of life. To minimise overtreatment, many governments employ cost-effectiveness thresholds, which set limits on additional funding for health gains.216 These thresholds are typically presented in terms of the cost per quality adjusted life year (QALY) gained. In the UK, for example, the threshold set by the National Institute for Health and Care Excellence (NICE) is in the range of £20 000 to £30 000 per QALY.217 Treatments that have incremental cost-effectiveness ratios above this range are not funded.217 However, some governments have been willing to have higher thresholds for treatments for people with life-limiting conditions. For example, in 2009 the UK raised the cost-effectiveness threshold for moderately life-extending treatments to £50 000 per QALY.218
Do these higher thresholds represent a willingness by citizens to pay more for treatments for those with life limiting conditions? A systematic review of 23 studies, albeit with different data, methods, and countries represented, found eight studies that showed the public were willing to pay more and 11 that showed no public preference (results from four studies were considered inconclusive).219
One way to determine whether overtreatment at the societal level is occurring at the end of life—ie, that those treatments are being provided at higher cost-effectiveness ratios than other services—is to compare the percentage of annual expenditures that are for patients who die to the death rate in that year. If all treatments were funded at the same threshold, then spending on treatments at the end of life as a percentage of total annual medical spending would be roughly equal to the country's death rate (supplemental information available on request). Yet, as shown in table 4, a disproportionate share of total annual health expenditure in high-income countries goes towards treatments for people who die. This finding is consistent with the hypothesis that treatments at the end of life are being provided at much higher thresholds than for other treatments.
The Sustainable Development Goals include universal health coverage,220 but it is important to recognise that unless efforts are made to ensure the costs of treatment do not exceed the expected benefits, overtreatment at the end of life is likely. This imbalance means that resources are not available for other components of universal health care.6 Early access to palliative care tends to lead to better health outcomes and a more cost-effective use of resources, sometimes even leading to cost savings.221 Earlier referral to palliative care and greater use of advance care plans, patient decision aids, health communication strategies, care pathways, and cost-effectiveness analysis should reduce levels of overtreatment. The essential package of palliative care and pain relief health services advocated by the Lancet Commission on Palliative Care and Pain Relief is supported by strong evidence of cost effectiveness.7
Section 10: Health care in death systems
Health-care systems are where an increasing majority of people meet death, and they form a substantial component of many death systems. Experiences with the health-care system shape our relation with and attitudes to death and dying.
The pursuit of immortality
The world's oldest story, the Epic of Gilgamesh, which was written in 2000 BCE, tells how the hero sought immortality. The dream of immortality has flourished ever since, and there are now a variety of well-funded companies and organisations trying to turn the dream into a reality. The Scottish-born Ian Morrison, who was formerly president for the Institute for the Future and lives in California, jokes “Scots see death as imminent. Canadians see death as inevitable. And Californians see death as optional.”222 The world is moving more in the direction of California than that of Scotland.
The philosopher Stephen Cave has postulated that there are four narratives that capture attempts at immortality, and modern medicine and research has a stake in all four narratives.223
Immortality Story 1: The Elixir Story
Almost every culture has had a version of the story that a magical elixir will be found that will enable us to live forever and keep us young. Modern medicine and science, with nanotechnology, genetics, biological engineering, and regenerative medicine, present a contemporary version of this magical elixir.
Immortality Story 2: The Resurrection Story
The resurrection of Christ is to many the most familiar version of this story, and it was Christianity's promise of eternal life for all, not just emperors, that drew Romans away from their traditional gods to the new religion. Today the Alcor Life Extension Foundation has more than 150 patients with their heads or bodies deeply frozen, ready to be brought back to life when medicine is able to cure the disease that led to their death.224 Cloning, carried out already with sheep, is being explored in humans and is an alternative form of resurrection.
Immortality Story III: The Story of the Soul
The soul, described by St Augustine (354–430) as “a special substance, endowed with reason, adapted to rule the body” is understood across cultures to transcend the physical body. Today, technology is being used to harness this story of immortality through so-called mind uploading, or digital immortality.225
Immortality Story IV: The Legacy Story
This is perhaps the most familiar route to immortality—writing a great symphony or novel, winning a crucial battle, or making any great achievement that means we will be remembered and celebrated for ever. A modern version is to create a digital avatar, in which every bit of data from you (all that you've written and said, and all words about you from others) is used to create a representation that will exist electronically and continue you after you die.226 Many people might hope for this from their entries on Facebook or Instagram.
Biogerontology
Biogerontology is the study of the biological mechanisms that control ageing, with the ultimate aim of developing interventions to delay death. The discipline regards itself as a Cinderella science, given little in the way of government funding, and viewed with suspicion by both the public and other biomedical researchers. Nevertheless, it has a journal published by a major science publisher.227
In some animals, selective breeding and caloric restriction can lead to substantial increases in longevity. There is no evidence that such interventions work in humans.228 Various drugs and nutritional supplements (called nutraceuticals) have been postulated as effective anti-ageing treatments, but, as some biogerontologists concede, trials looking at interventions to delay ageing would be extremely difficult to conduct, as the only meaningful endpoint would be age at death, which would probably occur several decades after commencing the intervention. Nevertheless, there is a growing belief within biogerontology that effective strategies to delay ageing will inevitably emerge. They argue that if ageing can be delayed in other mammals, then it is only a matter of time until it can be delayed in humans, too. The biogerontologist Richard A Miller wrote in 2002: “Thus one can, with some confidence, expect that an effective anti-ageing intervention might increase the mean and maximal human life span by about 40 percent”.228
The compression of morbidity: a real phenomenon or wishful thinking?
The concept of “compression of morbidity” was introduced by the American physician James F Fries in 1980 and has proved highly influential.229 He predicted that through the compression of morbidity, the time spent with chronic illness at the end of life would be reduced and that there would be a rapid final deterioration leading to death. He argued that the length of the human life is fixed, as although average life expectancy is increasing, maximum life expectancy remains relatively constant, and through the adoption of a healthy lifestyle, chronic disease can increasingly be postponed. It follows from these two premises that the time between birth and first permanent infirmity must increase and that the average period of infirmity must decrease.229 This concept implicitly underpins much medical research and treatment.
The Commission asked several leaders in research whether medical research is trying to cure all diseases and if so, what we would die of. The leaders answered that there was an attempt to cure all diseases but there was no expectation of curing them all. The main aims of research were to lengthen healthy life and reduce the period of ill health at the end of life.
Compression of morbidity has been explored in the Cognitive Function and Ageing Studies, a series of population-based studies on people older than 65 years conducted in the UK. Comparing a series of variables in 1991 and again in 2011, the findings showed that when healthy life expectancy was used as the primary outcome there was a mild, relative compression of morbidity over this time. When cognitive impairment-free life expectancy was measured, there was a definite compression of morbidity, but when disability-free life expectancy was assessed, there was dynamic equilibrium—that is, less severe disability increased, but more severe disability did not.230 The key message from these studies is that one measure is not enough: whether you get compression or expansion of morbidity depends on what measure of health you use and which age group you look at.
The authors of the Cognitive Function and Ageing Studies concluded in 2018230, 231:
“Between 2015 and 2035 multimorbidity prevalence is estimated to increase, the proportion with 4+ diseases almost doubling, and two-thirds of those with 4+ diseases will have mental ill-health. Life expectancy gains (men 3·6 years, women 2·9 years) will be spent mostly with 4+ diseases (men 2·4 years, women 2·5 years) resulting from increased prevalence rather than longer survival with comorbidity. Over the next 20 years there will be an expansion, not compression, of morbidity, particularly complex multi-morbidity (4+ diseases).”
In 2010 a detailed review of compression of morbidity examined data trends in the USA.232 The review found that during 1998 to 2008, mortality declines had slowed, mobility functioning had deteriorated, and length of life with disease increased. The authors concluded that, although a compelling idea, the compression of morbidity may be as illusory as immortality itself.232 Yet despite evidence that compression of morbidity is not being achieved, the concept continues to exert a profound influence over the understanding of health, the role of health care, and the goals of medical research.
Ageing, dementia, and frailty
Life expectancies are generally increasing worldwide, and as a result, people are dying further into old age. Dying aged over 85 years is different to dying when younger, even to dying aged 65–85.233 Dementia, multi-morbidity, and frailty are more common in those over 85. Dementia is now the leading cause of death overall for women and for men older than 80 years in the UK.234 These conditions require an integrated social and health-care response, but such support is often unavailable. Many of the oldest old have no family caregivers. For those who do, the burden of care placed on elderly partners or children can be high. The caregivers may also be unwell themselves. Paying for care at home or elsewhere is expensive and can lead to the loss of savings, property, and inheritance. The preferences and wishes of the oldest old remain largely unexplored. Death is often understood as part of everyday life, and common assumptions, such as wishing to be with family or connected with communities, may not hold as people withdraw from the world.235
Care homes, which are called nursing, assisted living, long-term care, or rest homes in some settings, are increasingly the place of dying for many around the world (table 2). This presents a challenge. Care homes must tread a careful line between being a home and being places for rehabilitation, health care, safety, and dying. Care homes have been described as the hospices of the future,236 but achieving equity in provision of care at the end of life is a formidable challenge. Issues such as staff training and turnover, support with clinical decision making at the end of life, access to medical or specialist support, and high workloads can make provision of holistic care at the end of life difficult.237 The rapid spread of COVID-19 through many care homes around the world, the lack of access to personal protective equipment and the disproportionate number of deaths highlight the lack of support for, or prioritisation of, the vulnerable residents and staff.
Recognising dying
All scientific or technical advances carry with them cultural or social implications. As death, like childbirth, moved from the province of family and home and towards hospital care, a complex human event became “defined in medical terms, described using medical language, understood through the adoption of a medical framework or ‘treated’ with a medical intervention.”238
The issue with dying in this context is that dying has no clear distinct, unequivocal “diagnosis” for clinicians to determine: the dying of a person with interstitial lung disease and overwhelming breathlessness is distinct from that of a person with widespread cancer and anorexia-cachexia, which is different again from the dying of a person with an aortic aneurysm dissecting over hours. Yet the endpoint is the same, and the process is labelled as dying in all these cases.
The recognition of dying may be early or late, depending on the clinical condition of the person, the clinicians, and those close to the person. The effect of early or late recognition may have important implications for the person, their loved ones, and the clinicians involved in care.
Despite an increasing literature on diagnosing dying,239 the lack of clear, explicit criteria of what constitutes dying limits the idea of a diagnosis of dying, so it remains a concept of limited usefulness. Doctors and nurses are often reluctant to give prognoses on the outcome of serious illness and the time of death and are notoriously inaccurate when they do so.240 A range of tools have been developed to support this process,241 but diagnosing dying remains an imprecise science.
Despite this complexity, some distinct patterns can be discerned at a population level in groups of conditions. The trajectories shown in figure 4 capture some of the experiences of people dying from the common conditions of cancer, organ failure, or physical and cognitive decline.242 Although these models are not predictive for individual cases, they illustrate the types of experiences that people may face.
Figure 4.
Trajectories of dying with cancer (top), organ failure (middle), and frailty (bottom)
Reproduced from Murray and colleagues by permission of BMJ Publishing Group.242
The difficult conversation:” Breaking bad news, communication, and prognostication
The phrase “the difficult conversation” has become shorthand for the honest and wide-ranging discussion that should—but often doesn't—take place between a dying person and their health-care team. A report from the Royal College of Physicians in the UK, Talking About Dying: How to Begin Honest Conversations About What Lies Ahead, reported that only 8% of people with cancer who said that they had thoughts and feelings about their death had shared these reflections with their health-care team. Among those who had, only 19% of the conversations were initiated by the health-care professional.243 Too often the conversation takes place at a time of crisis, generally during an emergency admission to hospital.
The obstacles to these conversations are many and various. In a busy clinic or ward round, it is easy for doctors to avoid the conversation by ordering another scan or round of chemotherapy. There may be a fear of extinguishing hope, with doctors worrying that a candid discussion on prognosis could lead to despair. Contemporary hospitals have a “fix-it” approach to acute illness, regardless of the prognosis, often driven by rigid protocols that ignore the likelihood of success. Modern medical care is increasingly splintered and atomised, with poor communication and cooperation between primary and hospital care, and lack of clarity on the responsibility for having such conversations; doctors in acute specialities might regard the difficult conversation as the role and responsibility of specialists in palliative care. Collusion with families might also contribute to the problem: well-meaning relatives may pressurise doctors into not telling dying people that they are dying. Many societies support a focus on communal or relational autonomy rather than individual autonomy—in this setting, families are usually given information first, and discussions then take place about how much to disclose to the patient. In many cultures, it is not acceptable to speak directly of death or to prognosticate when someone may die. Furthermore, some people dying will be unable, cognitively or emotionally, to have this conversation. The conversation may be impossible for people of extreme old age or those with advanced dementia, although members of the Commission report that rich conversations to convey wishes, preferences, and choices can still be had with people living with dementia. It can often be difficult to be sure when a person has begun to die, that they are—to use the oxymoronic term—actively dying, although the time to initiate such conversations would ideally take place before active dying.
The difficult conversation need not be difficult. The conversation should be a process rather than a single conversation: ideally it comprises a series of discussions. In his book Being Mortal, the surgeon Atul Gawande suggested that a series of five questions could be used as a frame for these conversations.46 These questions are: what is your understanding of where you are and of your illness? What are your fears or worries for the future? What are your goals and priorities? What outcomes are acceptable to you? What are you willing to sacrifice and not? And later, what would a good day look like?
The very fact that this conversation is called “difficult” is emblematic of the obstacles to it. This conversation should be termed “essential”, not “difficult”. A cultural shift is required within the medical profession and healthcare more generally so that this conversation is viewed as a professional responsibility for the doctor or health-care professional and a right for all people and families who wish it.
Withholding or withdrawing treatment
In clinical care—and particularly in intensive care units—decisions often must be made about withholding or withdrawing treatments. The clinical aspects of these decisions are important, but ethical, legal, cultural, religious, and financial aspects also influence the decisions (panel 10 ).
Panel 10. Deaths in intensive care in high-income and low-income countries.
An accepted principle in intensive care medicine is that intensive care should be provided for those with the greatest chance of benefiting from the care. The demand for intensive care exceeds availability throughout the world. Intensive care ideally should not be provided those for whom death seems unavoidable, although the practice of palliative care in the intensive care unit is growing.244
Decisions about whom to admit to intensive care are inevitably complex, although the chance for the patient to benefit is a prime criterion. The Intensive Care National Audit and Research Centre (ICNARC) has been collecting data and conducting research in intensive care in England, Wales, and Northern Ireland for 25 years and has seen an increase in the number of intensive care beds and a drop in mortality.245 The centre has developed a score that predicts accurately the chance of a patient dying in intensive care and produced for the Commission data on patients who had 80% or greater chance of dying (or 20% or less chance of surviving) in intensive care.246
In 2018–19 there were 163 340 total admissions to adult intensive care, with 30 195 deaths (18·5%). Over the decade 2009–19, 93 870 patients with a greater than 80% chance of dying were admitted, accounting for 6.4% of all admissions; 57·5% of the admissions were for men, and the average age of those admitted was 68·6 years. The proportion of admissions varied across critical care units from 0 to 14·5% (median 6·5%, interquartile range 5·1–7·9%). After excluding readmissions of the same patient within the same acute hospital stay, overall acute hospital mortality for these patients was 89·5% (80 593 of 90 047), reflecting the accuracy of the predictive score. Over the decade the proportion of these admissions declined slightly, but the absolute number increased slightly as the number of intensive care beds increased.
Nobody can say whether these rates are right or wrong, but they are interesting in providing data on the degree to which treatment continues when the risk of death is high. It is reassuring that there has been no increase in the proportion of high-risk patients admitted, showing that there is no increasing tendency to treat those likely to die.
The sparse data from low-income countries are much more disturbing. High-income countries have 33–240 intensive care beds per million population, whereas low-income countries may have only 1 per million—despite conditions that require intensive care being much more common.247, 248 Following the principle that patients most likely to benefit should take priority, one would expect death rates in low-income countries to be lower. But they seem to be much higher: of 360 patients admitted to a university hospital's intensive care unit in Tanzania, 46% died in the unit.249 In a similar intensive care unit in Malawi, 110 patients died in one year—a mortality rate of 36% (T Baker, unpublished data shared with the Commission). These figures are substantially higher than the 8–18% mortality rates seen in intensive care units in high-income countries.248
Patients who die in intensive care in low-income countries are typically young and very sick: the median age of those who died in the Malawian cohort was 34 (interquartile range 25–42): 85% had at least one severely deranged vital sign at arrival on the intensive care unit and 45% had a cardiac arrest requiring cardiopulmonary resuscitation either before or on admission to the unit.
Our colleagues from Malawi conclude: “Enhanced community engagement, improved patient selection for ICU care and an increased focus on dignified dying could lead to substantial gains including improving deaths for many.”
The World Federation of Societies of Intensive and Critical Care Medicine has highlighted substantial variation in practice across the world: some countries have laws that state that withholding and withdrawing treatment are equivalent; some countries have no legal advice or guidelines regarding withholding or withdrawing treatment; in some countries withholding treatment is legal but withdrawing it illegal.250
One of the central concepts in making clinical decisions about withholding or withdrawing treatments is an understanding of whether the treatment is likely to benefit the patient. Various terms have been used to capture the likelihood that a treatment will not lead to benefit. The term medical futility, although widely used, has more recently been deemed misleading and calls have been made for it to be reserved for treatments that have no possibility of working.251 Terms such as “potentially inappropriate” are now being used for treatments that have at least some chance of benefiting the patient, but clinicians believe that competing ethical considerations justify not providing them.251 Use of these “potentially inappropriate” treatments is widely reported across the world—for example, insertion of feeding tubes into dying patients in England and Wales252 or intensive care support for end-stage cancer patients in Brazil.253 These treatments continue because of difficulties with defining and agreeing over what is futile, what is potentially inappropriate, and what might be effective; a fear of culpability; poor communication with and among patients and families; hubris; and a belief that medicine's first priority is to extend life.
In high-income settings, decisions to withdraw treatments are increasingly common. In the UK around two-thirds of deaths in intensive care units occur after a decision to withdraw treatment.254 Higher figures are reported across 22 European intensive care units: the proportion of patients dying with treatment limitations in place increased from 68% to 89% between 1999 and 2016, and deaths without treatment limitations in high-income settings are becoming increasingly rare.255
Paradoxically, despite the paucity of resources, withdrawal of treatment is more unusual in India than in high-income countries.256, 257 While the poor die at home with no palliative care, those who can afford to pay get disease-focused, organ-centred care that may have a negative effect on the dying person and on their family. The dying process can be stretched by artificial life-support measures to weeks and sometimes longer with renal dialysis, artificial ventilation, and total parenteral nutrition or extracorporeal membrane oxygenators. This treatment can lead to enormous physical, social, mental, and spiritual suffering. It can also bankrupt families.258
Indian figures of limitation of life support in intensive care unit are as low as 22–36%,256, 257 and two-thirds of these limitations result in discharge of the person from hospital at the end of life, usually with documentation of “leaving against medical advice” (LAMA). This documentation absolves the hospital of responsibility but condemns the patient to death with no symptom control or any palliative care. As a 2020 editorial in the Indian Journal of Critical Care Medicine points out “It is often done in the setting of futility and in the setting of inability to pay, and with the tacit encouragement of doctors and hospital administrators.”259
Beneficent omissions and withdrawal aversion
In many jurisdictions, withdrawing life-sustaining treatment after it has been started—for example, removing a ventilator or feeding tube—is treated as legally and ethically equivalent to withholding that treatment in the first place. Both are treated as so-called beneficent omissions—that is, they are neither negligent omissions nor, unlike delivering a lethal substance, are they acts done with the intention of ending a life. In practice, however, there is lack of clarity among some health-care providers in such jurisdictions, who view withdrawing (but not withholding) treatment as an action causing death. This results in what has been called withdrawal aversion.260 Because they are unable to make a distinction between an intention to cause death and an intention to allow natural death, some clinicians equate withdrawal of life-sustaining treatments with euthanasia and are reluctant to withdraw treatments even when the law permits it.261 Withdrawal aversion is sometimes incorporated into national laws. For example, the Israeli Law on the Patient Nearing Death allows for withholding the next cycle of ventilation but not the cessation of continuous ventilation.262
Do not attempt cardiopulmonary resuscitation decisions
One of the most commonly discussed beneficent omissions is the withholding of cardiopulmonary resuscitation. The incidence of do not attempt cardiopulmonary resuscitation (DNACPR) decisions is highly variable throughout the world. Two surveys of decision making by health-care professionals in relation to DNACPR decisions across 36 countries illustrate not only the complex clinical factors that may influence a decision, but also economic, legal, cultural, and religious considerations.263, 264 A survey of decision making in higher-income settings, including Canada, the USA, Europe, Australia, Brazil, Japan, and Turkey, found large variations in physician practice both among and within countries, including whether decisions are written or verbal and the likelihood of involving nurses or other professionals in the decision-making process.263 The same survey was used in 16 Asian countries and found a series of factors to be independently associated with a reluctance to make a DNACPR decision.264 These included a reluctance to involve families or surrogates in decision making, a belief that there would be exposure to legal consequences, and religious views of the physician. Increasing out-of-pocket expenditure for families was associated with a higher likelihood of completion of a DNACPR decision. The authors point to the importance of all countries having an ethicolegal framework in place to guide these complex decisions.264
Hospice and palliative care
In the second half of the 20th century, several authors began to highlight the needs of the dying. A series of case studies describing the realities of dying in hospital showed the burden of unrelieved symptoms and the abandoning of patients who could no longer be cured.265, 266 The psychiatrist Elisabeth Kübler-Ross, whose work on grieving has already been mentioned, explored the impact of a terminal diagnosis with patients and health-care students in a series of seminars at the University of Chicago, culminating in her book On Death and Dying.117 In Britain the nurse, social worker, and physician Cicely Saunders (1918–2005), working in east London with dying patients, developed a new model for care of the dying and their families, setting the management of physical symptoms alongside psychological, spiritual, and social considerations.267
A core tenet in this movement to care for the dying was that, alongside an urgent need for pain and symptom relief, care of the dying required a holistic approach. This approach recognised death as a natural part of life, necessitating opportunities for human connection, the presence of family and friends, and opportunities to reflect and understand what was taking place. The hospices that grew up to support this movement were in some ways recreating the deathbed scenes from earlier years, where families gathered, important matters were settled, and final words shared. Palliative care services have been shown to improve quality of life and symptom burden268 and to be cost-neutral or cost-effective.269
Hospices, and the discipline of palliative care that followed, clearly articulated that dying people have the right to clear communication, relief of their symptoms, and compassionate care. WHO supported the early development of the discipline, focusing initially on cancer pain and developing an important series of early guidelines. WHO defines palliative care as “an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual”.270 More recent discussions have focused on the essential components of palliative care and on the role of relieving severe suffering versus an emphasis on life-limiting illnesses.271
Despite palliative care being recognised as a component of universal health care,272 an integral part of primary health care in the Astana Declaration,273 and following calls for it to be recognised as a human right,274 the WHO estimates that still only 14% of those in need of palliative care receive it.48 The Lancet Commission on Palliative Care and Pain Relief highlighted the stark inequity of current provision around the world, specifically the lack of access to basic pain relief.7 Substantial disparities also exist within all countries regarding access to palliative care services, with access following the same inverse gradients seen with access to most health-care services—that is, those who need the care the most receive the least. Funding is variable, with many services around the world dependent on charity. In some countries, palliative care services have been integrated into statutory or public health services, but more often they remain outside central funding, bringing risk and challenges to universal accessibility, but also opportunities for innovation.
Hospices situated outside the mainstream health-care setting succeeded in providing a “safe place to suffer”, but they also facilitated an unintended separation of dying people. This movement of dying people into a separate institution under specialist care reinforced the idea that care of the dying was specialised and for experts only. It encouraged the sense that other health-care professionals are relieved from managing this part of a patient's illness and life and the further professionalising of an event in life that had been managed in the community. An attempt in England to return this skill and capacity to those working in acute hospitals, where most people in Britain die, through an integrated care pathway for the dying failed badly (panel 11 ).
Panel 11. Lessons from the failure of an attempt to improve the experience of dying in acute hospitals.
The widespread introduction of the Liverpool Care Pathway for end-of-life care into acute hospitals in the UK (apart from Wales) was an attempt to extend palliative care beyond hospices and specialists into routine care in acute hospitals.275 It proved a failure but taught lessons that are broadly applicable.275 The pathway was first published in the late 1990s and was an integrated care pathway detailing standardised care to be delivered to dying patients and their families. It went through 12 iterations before it was abolished in 2013.
While anecdotal evidence suggested that the pathway helped clinicians and others provide a high-quality experience of dying within a National Health Service (NHS) setting, it was let down by three serious failings:
-
•
First, an assumption that what worked in British hospices—institutions dedicated to care of dying people and staffed by highly skilled practitioners—could work in busy NHS hospitals with different priorities and lacking staff skilled in end-of-life care.
-
•
Second, although the concept of an integrated pathway of care itself was acceptable, it was implemented with little or often no training, and consequently many of its actions were reduced to a “tick-box exercise” and a “one-size-fits-all solution”.
-
•
Third, despite the pathway being endorsed by national professional organisations, it severely lacked the research evidence that is expected in the adoption of any other new health technology.
Early studies did show anecdotal and qualitative evidence of benefit,276, 277, 278, 279 but the studies did not include any controlled trials, and some had been written by the authors who had developed and promoted the pathway.
Just as the review into the pathway was being published, a formal cluster randomised controlled trial did appear, evaluating how the pathway had performed clinically in an Italian hospital setting.280 The trial failed to show a significant difference in the distribution of the overall quality of care toolkit scores between the wards in which the Italian version of the pathway was implemented and the control wards.
The most damning evidence, which sealed the fate of the pathway, came from the revelation that NHS hospitals were being paid to reach targets for using the pathway.275 This incentive contributed to the unchecked use of the pathway in hospitals and departments that had little or no training and were using it inappropriately.
After the abolition of the pathway a coalition of 21 national organisations concerned with end-of-life care declared five priorities for “care when it is thought that a person may die within the next few days or hours of life”281 and the UK National Institute for Health and Care Excellence (NICE) developed recommendations for clinical practice in the last days of life. This guidance had an emphasis on individualised rather than a routine checklist approach to care of dying people.282
The UK has other packages of care for looking after the dying—including the Gold Standards Framework,283 which is primarily intended for use in primary care, and the Amber Care Bundle.284 There has been little or no concern about these packages, and certainly no scandal. But none of the packages are based on the controlled trials that are expected for most interventions in health care.
We should not conclude from this story that guidelines on end-of-life care should not be attempted, but rather that they need to be based on high quality evidence, should be introduced with training and regular audit, and should not be financially incentivised. Plus, they must be used as guidance not a checklist: “Don't just read the guidance, and particularly do not just use the checklist. Engage your brains and your hearts, read and implement evidence-based guidelines, and that is what will improve care.”275
The debate about who is responsible for care of the dying continues today, with discussions over specialist, generalist, and primary palliative care, and newer developments, such as the compassionate communities and the public health and palliative care movements, which hold that rather than end-of-life care being a health-care issue it should instead sit within a community-led framework.3
As this report makes clear, many questions around death, dying, end-of-life care, and grieving have not been answered, but, as panel 12 shows, little funding is available and much remains to be done.
Panel 12. Research in palliative and end-of-life care.
The universal nature of death belies the vanishingly small amount invested in research that aims to understand and improve how we die. In the UK, less than 0·2% of biomedical research funding is allocated to palliative and end-of-life care research.285 The UK National Cancer Research Institute allocates less than 0·5% of its total research spend to end-of-life care research.286 In the USA, the National Cancer Institute allocates around 1% of total research spend to end-of-life care.286 Analysis of research spend on dementia among G7 countries shows that basic and medical research dominates, with just 4·9% of research spend directed towards improving health and social care for the people affected.287
Four fifths of the need for palliative care need is in low-income and middle-income countries,7 yet only a quarter of these countries have contributed to palliative care research.288 Palliative care needs will rise quickly among older people, people with dementia, and people in low-and-middle income countries, yet there is little evidence on how best to provide palliative care to these groups.289, 290
Patients and carers are often missing from exercises to set research priorities, and consequently research is often service-orientated rather than patient-orientated.291 While some efforts exist to understand the wishes and research priorities of the general public, truly participatory work is rarely funded or published.
Population-level information on dying depends on good data collection systems. In many countries, basic descriptive and epidemiological data about how and where people die are limited. Accurate cause-specific mortality data are available for only a third of the world's population.292 Data collection systems to understand care provision, costs, and outcomes (including where people die) are necessary to build effective health systems but are lacking, especially in low-income and middle-income countries. Patient-reported and proxy-reported outcome measures are essential both to understand symptom burden and palliative care need, and for use in research to ascertain the effectiveness of interventions. There are currently many potential tools in use, with varying scientific validity.293 Use of a common set of validated outcome measures would help large scale collaborative research and meta-analysis of existing datasets.
Substantial differences exist in research capacity globally. Only 40% of European countries have at least one full professor of palliative medicine.294 Without specialists to conduct research and train subsequent generations research will stall. Investment in research capacity in low-income and middle-income countries through academic infrastructure is urgently needed. Models such as the African Palliative Care Collaboration illustrate how this can take place.295
Research regulation must be proportionate. If overly burdensome or inconsistent, patients may be harmed as the most important questions, the most vulnerable populations, and the most innovative methods are seen as too high risk to be worth trying. There has been a perception that it would be unethical to involve people facing the end of life in research. It is now increasingly understood that it is unethical not to offer them the opportunity to be involved.
Substantial and sustained investment in research is needed to understand not only what problems are faced by dying people and their carers, but also how we can tackle them. Current research is weighted towards the “what”: identifying and surveying the extent of needs and issues. Given the increasing number of people in need of care globally, research into responses and interventions is urgently required. Systematic appraisal of the evidence base to identify what is already known and where gaps remain will ensure research builds on current knowledge rather than duplicates it. Aligning this research with patient, public, and policy priorities will help ensure its value for society.
Section 11: Future scenarios for death and dying
“The future is already here—it's just not very evenly distributed.”
Attributed to William Gibson
The future is unpredictable. The unexpected happens, often with major impacts. A pandemic, for example, was expected, but COVID-19 has many features that were not predicted, meaning that tests of preparedness for a pandemic proved to be inadequate. Nevertheless, some thought of how the future might look is important in preparing for it. Scenarios are one way of doing this and came into use after the wholly unforeseen oil shock of 1974. Scenarios are not predictions of the future but rather sketches of plausible futures with the limits of plausibility set wide. They are not what people would like to happen but rather what might happen. They have been used to think about the future of South Africa after Apartheid,296 the UK's NHS,297 and scientific publishing.298 They are in many ways devices for thinking about the present, recognising things that will be important whatever the future brings.
Elaborate methods can be used to produce scenarios, but there is value in simply shared imaginings. We have imagined here five scenarios of the future of death and dying. The notion that the future is already here but not evenly distributed is true of these five scenarios.
Scenario 1: death overwhelms health systems
A surge of deaths from a pandemic, mass famine resulting from climate change, or some other unforeseen cause overwhelms health systems
Most people in human history have not died under the care of doctors or other health professionals. They have died at home, while travelling, through starvation, or on battlefields. Death is now associated in many countries with doctors and hospitals, yet a large rise in the death rate—from a pandemic, mass famine resulting from climate change, a nuclear war, or some other unforeseen cause—could easily overwhelm health systems. Indeed, this has happened in health systems in many countries during the COVID-19 pandemic, and the limits of such systems were laid bare.
Scenario 2: “immortality” and inequality
Medicine is successful with extending life but at great cost, increasing global inequality
Medical research uses genetics, big data, nanotechnology, artificial intelligence, cryogenics, and other methods to increase the length of life considerably. At the same time, private companies develop ways of “downloading minds” to allow some people to achieve a form of immortality. These methods are extremely expensive, making them available to few people. The very rich can access the technology and live much longer, while the poor continue to have much shorter lives.
Scenario 3: climate response—greater equality
The world and end-of-life care become much more equal
The climate crisis causes people to recognise our global interdependence and the rich to accept reducing their carbon consumption and access to expensive health care. Resources—financial and health-care workers—are redistributed from rich to poorer countries. Universal health care, including care at the end of life and the minimum package of palliative care,7 becomes available to all.
Scenario 4: rebalancing—focus on health-care system reform and the goals of medicine
Creating health and relieving suffering are prioritised alongside extending life
Rising health-care expenditure at the end of life and a recognition of how poorly people are dying leads to a global campaign to reframe the goals of health care. This campaign leads to a culture shift, wherein health-care workers understand their duty to mitigate suffering and increase quality of life and death, rather than prolonging the dying process. Psychological, social, and spiritual health comes at last to be regarded as equally important to physical health, and the focus of health care shifts from disease to the person, from longevity to wellbeing, and from institutions to community. Health professionals provide support to the dying and grieving when necessary but no longer dominate end-of-life care.
Scenario 5: assisted dying spreads
Assisted dying becomes a component of universal health care
Assisted dying spreads to all almost high-income countries and many low-income and middle-income countries. People must have the mental capacity to request an assisted death. It is available not only to those judged to be near the end of life but also to all people with unbearable suffering, those developing dementia, and those who are “tired of life”. It is tightly regulated but provided by many health-care professionals, including those working in palliative care, and in some countries up to a quarter of people die in this way.
Section 12: Reimagining death and dying—the Commission's realistic utopia
“[A realistic utopia] joins reasonableness and justice with conditions enabling citizens to realize their fundamental interests.”
John Rawls21
The above scenarios represent imagined possibilities of what might happen in the future. The actual future is most likely to be a combination of these scenarios, or perhaps something we have not envisaged. But governments, civil society, and health-care services are not passive in death, dying, and grief. The ability to shape the future sits with us all. The Commission believes that profound, rather than incremental, change is needed to transform how we relate to death, and how we die.
The concept of a realistic utopia was first encapsulated by the philosopher John Rawls as he attempted to define a radically different vision of future society.21 Crucially, although a realistic utopia is radical, it is also achievable. The core principles on which it is created must be shared across a society, and a systems approach is essential. We describe a realistic utopia for death, dying, and grief in the future and outline its five principles.
(1). The social determinants of death, dying, and grieving are tackled
The social and political determinants of health—including income, employment, educational opportunity, physical environments, gender equality, social supports, access to healthy food and health services, and all the policies and legislations that provide for these—determine not only how people live but also how they die and grieve. Many deaths and much suffering globally are the consequence of inequity and disadvantage and are avoidable. Poor deaths often follow poor lives. In our realistic utopia these social determinants of death, dying, and grieving are tackled, meaning people can live healthier lives and die more equitable deaths.
(2). Dying is understood to be a relational and spiritual process rather than simply a physiological event
In the realistic utopia, societies and health-care systems recognise that death is principally a relational and spiritual process rather than simply a physiological event. As a result, the balance of care changes. Relationships are prioritised and made central to care and support when dying or grieving, across all settings from care homes and hospitals to people's homes. The quality of relationships between health-care professionals and patients shifts from the transactional to those based on connection and compassion.
(3). Networks of care lead support for people dying, caring, and grieving
Such networks are composed of family and wider community members alongside professionals. Cutting across the usual dividing lines of lay or professional care, these networks of people at the end of life, families, doctors, nurses, paid and unpaid carers, and community members challenge traditional power differences, allowing people to participate as equals. The two facets of lay and professional care are no longer seen as separate, and efforts are made to integrate these two essential components. Each person dying or grieving has a such a network explicitly created around them.
(4). Conversations and stories about everyday death, dying, and grief become common
Death, dying and grieving are acknowledged as natural parts of life, and stories of people experiencing these events in everyday ways are shared and discussed through the media, in film and television, in schools, and within communities. These universal experiences are recognised and addressed in national and global policies, reports, and strategies. The open and balanced discussion of these topics leads to a series of wider public conversations, debate, and action.
(5). Death is recognised as having value
Although not always welcome, death has inescapable purpose and value. The realistic utopia recognises that death allows for birth, growth, and change: without death, civilisation would be unsustainable. Furthermore, the value in being with people who are dying is understood. By giving time, attention, and compassion as people die, we connect with them and with our shared fragility, pushing us to acknowledge our interdependence and understand what is at the core of human relationships.
Section 13: Transforming death systems
The principles of the Commission's realistic utopia are high-level, allowing different versions to be interpreted and created in different cultures and communities. Moving from what the Commission has argued is an unsatisfactory present to a better future requires the current death systems in place to be changed. But can systems, which are complex, non-linear, with interdependent and connected parts, be changed by those who wish for reform? Such change is certainly not as straightforward and predictable as mending a clock or even sending someone into space, and unintended consequences are always a possibility. Guides exist for changing complex social systems,299 and there are examples of systems of varying complexity that have changed for the better—improved gender equality in many societies, the fall in aircraft fatalities, and the improvement in 5-year survival from many cancers. By contrast, the recognition that obesity is best conceptualised and tackled as a system has not yet led to reductions in obesity in most countries.53 System change takes time. It is also important to recognise that systems are not static: they are constantly changing. Indeed, this report has described how death systems have changed dramatically in a few lifetimes, and the future scenarios outline how systems might change further.
The Commission cannot write a simple prescription for changing death systems for the better, but we have shared principles and make a set of recommendations (section 15), that would improve death systems. Systems are not changed by individuals or even Commissions, but by multiple actors at multiple points, and there are many groups today who are actively attempting to change death systems. We list examples in figure 5 . This is not an exhaustive list, and there will be value in extending and deepening maps of current death systems and in understanding attempts to change death systems. Mapping, learning, and changing in response to what is learned are fundamental to systems change.
Figure 5.
Points for leverage within systems, adapted from Meadows300 with examples of current initiatives
Figure 5, which lists attempts to change death systems, is built around leverage points identified by the American environmental scientist Donella Meadows (1941–2001), who in the book Limits to Growth recognised the interdependence of populations, the environment, and economies (all of which are systems), and was an early champion of sustainability.300, 301
In her book, Meadows attempts to rank the leverage points for changing systems, with the most important and effective leverage point being to change mindsets or the paradigm of the system. As described earlier in this report, there have been many attempts to change the mindset of seeing death as unfamiliar, terrifying, and purely negative, through death awareness campaigns, death cafes, death festivals, and a proliferation of books and films. There is little evidence on the effectiveness or otherwise of these activities, and more evidence is needed. The major, generously funded, Project on Death in America, which ran from 1994 to 2003, aimed to transform the culture and experience of dying and bereavement in the USA, but it was not an unqualified success.302 The project funded arts-based activities, public engagement programmes, research, and education programmes for health-care professionals. The evaluation of the project concluded that it was a “necessary if not sufficient condition” for transforming the culture and experience of dying and bereavement.302, 303 The effect of the COVID-19 pandemic on the death system has not yet been fully evaluated, but there is emerging evidence that anxiety about death may have increased.9 The pandemic might also have increased public appetite for a heightened medical response to death.10
A second leverage point is to change the goals of a system, and the primary goal of the health system, the custodian of death in high-income countries, is to preserve and extend life. This goal has led to heavy investment in research to prevent death and extend life, and often to overtreatment at the end of life. Many are arguing for a shift of resources to researching ways to improve experience at the end of life, and the palliative care movement works to reduce suffering and improve the quality of care at the end of life. Increasing numbers of people are using advanced care plans and advanced decisions and directives to exert control over their care at the end of life and their dying. Campaigns for assisted dying are also aiming to change the goals of death systems.
Many forces are at work on the third point of leverage, the power to evolve or self-organise the structure of systems. The movements for compassionate cities and communities, as described earlier in this report, are good examples of such forces and are spreading across the globe. The death doula movement, which operates in many countries, has a specific aim to “bring dying ‘home’ in our communities as we believe it is all of our business and not the sole preserve of experts and professionals.”131 Again, more evaluation is needed to understand how these approaches challenge and reform current experience and practice. Multiculturalism can also change the death system, introducing different cultural practices—for example, Hindus in Britain campaigning for open cremation. A move as simple as encouraging open coffins at funerals could change death systems.
Changing the rules within systems can lead to change, and perhaps the introduction of assisted dying in an increasing number of countries and states is the most powerful example of laws changing the death system. In many countries it is the law rather than cost that blocks availability of opioids. Rules can also change at lower levels—for example, increasing the range of practices, like giving injections and medication, that can be performed by family carers and community health workers.
Meadows identifies as a further leverage point changing the way that information is held and flows. Traditionally health records have belonged to health professionals, not patients and citizens, but increasingly patients and citizens are being given not just access to records but control of them.304 This move has been compared to the Reformation, which shifted power from the church to people, and it can help shift power relationships at the end of life.305 People often come close to death without them or their family understanding that they are dying, and the need for health professionals to conduct the ineptly named “difficult conversation” is being widely promoted by professional and non-professional organisations, as we have described.
Some of the multiple changes being made to death systems are likely to move systems closer to the Commission's realistic utopia, but others might work against it. After the publication of this report, the Commission and its networks will study, learn from, support, and encourage developments that move death systems towards the realistic utopia. Some readers might view the realistic utopia as unrealistic, but there is already a death system that is moving towards to the Commission's realistic utopia—in Kerala, in South India. We thus give space to describing the system, its origins and spread, and its strengths, weaknesses and need for further development.
Section 14: Care at the end of life in Kerala
While many of the above examples present work at one leverage point or one aspect of a system, the changes seen in care for people at the end of life in the southern Indian state of Kerala (population approximately 35 million) over the past three decades represent much more complete system change.
India comprises over one-sixth of the world's population and has around 60 million deaths each year. With basic health care out of reach for millions and many people bankrupted through catastrophic out-of-pocket spending on health care in India, Kerala has emerged as a symbol of hope for low cost, equitable, and participatory palliative care, including end-of-life care. The success of this model rests on a series of paradigm shifts relating to how illness, dying, caring, and grieving are viewed within the state.
In 1993 a civil society organisation was formed by two doctors, M R Rajagopal (a member of the Commission) and Suresh Kumar, and a volunteer, Asoka Kumar, with the aim of managing the pain and other symptoms of people with serious illness. It was based in an outpatient clinic in a medical college in Kozhikode. Although community donations supported the work and volunteers assisted, the project was based on a clinical model of palliative care. The inadequacy of this model soon became evident: people needing the care could not travel to attend the clinic; family members were losing a day's wages, on which they depended heavily, to come and attend the clinic; and the complex social, emotional, and spiritual needs people described could not be met by a distant clinical service, even with volunteer support.306 Two years later, the team started moving out to visit bed-bound patients in their homes.
The next paradigm shift took place in 2000, when the initiative reframed how death and dying were understood by health-care workers and communities alike. They stated that dying from a life-limiting illness is a social problem with medical aspects, rather than the commonly held converse view. The initiative held discussions with local communities through religious organisations, activists, and local businesses, asking if they felt that caring for and supporting dying or chronically ill people was a societal concern. Kerala has a long history of social action, and the response was resoundingly that this was a societal concern. This model of community organising and action was a familiar part of Keralan life.307
Communities responded by starting their own local networks to identify and support people who were dying or had a chronic illness. An umbrella organisation, the Neighbourhood Network in Palliative Care, was formed in 2001 to provide support with training for volunteers, access to medical and nursing skills, and initial funds to start the work. Groups were run by people from the local communities, such as farmers, teachers, and local businesspeople, and drew on existing community resources and assets. Doctors and nurses undertook the clinical roles, but importantly, the cooperatives of community volunteers led the service. Principles of equity within the project were made clear from the outset with the statement “every volunteer is a leader”.306 By 2007 there were close to 100 autonomous centres running throughout Kerala with a network of thousands of volunteers supporting them and donations coming from the local community.
This model of care transformed how people lived and died in the state. People with incurable illnesses now had people coming to visit them at home, supporting their families with care, mobilising community resources to raise finances to keep children in school, providing food for the family, and helping bereaved spouses find work to support their families. Medical and nursing care was provided free of charge, and honest conversations about prognosis were held. Volunteers also promoted public health messages to communities, challenging misconceptions such as cancer being contagious, and spreading the message locally to stop people smoking or chewing betel nut. Community initiatives were particularly effective in fighting the social stigma against people living with HIV and AIDS. Volunteers focused on giving families the tools to care for a dying person in a sustainable way. For example, for people who could no longer swallow and who had a nasogastric tube in place, families were taught to use coconut water for hydration. Coconut water is a safe and sterile replacement for water and minerals and is readily accessible to almost all people in Kerala.
Wider participation in the movement came from diverse groups, such as the police, who would refer people into the initiatives and provide transport, students, who would often fundraise to set up a clinic and home-care service from their campus, and, once the movement became better known, local political groups and the media.
Volunteer groups also act as advocates for the local community and challenge powerful local institutions. Tension initially existed with private oncology services. The initiative was viewed with suspicion by these services, who thought they were trying to take patients away from the private sector. Through discussions and shared care, oncologists from the public and private sectors were brought onside with ideas of death not being a failure, of palliative care, and of care at home. Today many partnerships exist whereby patients under the care of the Neighbourhood Network in Palliative Care can access inpatient beds or transport from local private hospitals free of charge. The landscape of how people approach the end of life when dying from chronic and incurable illnesses was revolutionised in many parts of the state.
Yet there were still many areas in the state that had no volunteer groups and no coverage. The project had begun in the north of the state, an area perceived to be more open to community action and civic responsiveness. There were concerns that the same approach would not work further south. There were also concerns that the Neighbourhood Network in Palliative Care was in effect creating a parallel system of care for the chronically ill, absolving the health systems of their responsibility to support people when seriously ill or dying. At the same time, local volunteer units started responding to other concerns raised by local people: for example, how poorly chronic psychiatric conditions were being managed in the community; the limited rehabilitation options for young men who became paraplegic after falling from coconut trees as part of their employment; and the devastating financial costs on families of renal replacement therapy. Volunteers responded to these calls, which were beyond the scope of most palliative care services, by setting up new initiatives. In the words of one volunteer, “We see suffering and not diseases.”
Caution was also drawn in romanticising the community response. Communities are not benign, homogenous entities waiting to share resources. Competing interests and power bases exist within them. Building links with one group may reinforce existing inequalities or disadvantage for other groups. This issue was discussed openly from the start, and dialogue and learning continue within the projects. It was understood that the assumptions on which projects were planned and implemented on may need revisiting as communities evolve and adapt to interventions.307 The meaning of the term community is explored further in the appendix.
The second paradigm shift came in 2005 when the Government of Kerala responded to the groundswell of community action to create a state palliative care policy. The policy was declared in 2008, stating that palliative care should be participatory and work closely with community actors. It further described how all primary health-care units should provide palliative care in collaboration with local volunteer units.309
The desire was to embed this model of home-based, volunteer-led care at the end of life throughout all primary health-care centres as a core component of universal health coverage. At the same time a media campaign through the largest regional newspaper in India, Malayala Manorama, spoke to the public about the needs of people who are dying or living with chronic illness and of the role societies play in supporting them. The newspaper received over 5000 calls in three days from people wishing to volunteer in the movement. This second shift rapidly expanded the number of services available and reintegrated the skills from the movement into mainstream health-care services.
Today, over 1600 institutions deliver palliative care services throughout the state; of the 2000 palliative care services in India, 80% are in Kerala, and tens of thousands of volunteers have been trained. At least limited palliative care services are available in every district in Kerala and these services are estimated to reach over 70% of those in need, compared with the national average for India of 23%.310 The spread of the model through the public health system has provided many benefits in terms of access and setting quality standards for care, but some consider this progress to be at the cost of innovation and the ability to respond to new concerns raised by the community. The restrictions posed by service delivery through a health-care system limits health-care workers, who deliver only what they are contracted to do. This tension continues, but the partnerships that have developed among public and private health-care services and local volunteer collectives show how these tensions can be negotiated and services and communities can work together on a common platform.
The model is recognised by the WHO as a collaborating centre, the WHO Collaborating Centre for Community Participation in Palliative Care and Long Term Care. As part of this collaboration, the model is being tested in other states in India (Puducherry, West Bengal, Manipur, and Delhi) and in Bangladesh, Indonesia, Myanmar, and Thailand.
Policy reform
In addition to caring for people with serious illness and at the end of life, the initiatives in Kerala transformed policy regarding opioids in the state and the relevant law by the Indian Parliament.
Working with the Pain and Policy Studies Group at the University of Wisconsin–Madison, palliative care leaders were successful in persuading the Government of India to accept model rules on palliative care and opioid use for adoption by state governments. The states were not legally bound to accept them, but some state governments did comply, including Kerala in 1998. The amended rules allowed trained health-care professionals to prescribe opioids, and supply issues were resolved. Pallium India was formed in 2003 with the intention of building palliative care capacity beyond Kerala and challenging the complex legislation across the 28 different states that was restricting opioid availability and use. In 2014, the Indian Parliament amended the 1985 Narcotic Drugs and Psychotropic Substances law, drastically simplifying the process for prescribing opioids and improving access to opioids for moderate to severe pain, including at the end of life, throughout India. Sustained advocacy led to the announcement of the National Program for Palliative Care by the Government of India in 2012, initiation of a postgraduate course in palliative medicine in 2012, inclusion of palliative care in national health policy in 2017, and inclusion in undergraduate medical education from 2019.
Global application of the Kerala model: a possibility?
The model that has developed in Kerala since the early 1990s is an example of profound systems change. It has succeeded in changing narratives around death and dying, building a powerful community response, increasing the number of people able to access care, influencing state and national policy, and challenging models of care globally. It has succeeded in redefining care at the end of life as a public concern beyond services and professionals.
As a result, interest has developed in whether this model might work in other contexts. Many sites around the world have been influenced by the work undertaken in Kerala, but we consider its translation to two further sites: West Bengal, and London, UK.
In 2014 the Sanjeevani Palliative Care Society was inaugurated as an experiment in community mobilisation in palliative care in Nadia district, West Bengal. The context differs in many respects to that of Kerala—for example, life expectancy, literacy, and government spending on health are all lower.311 Furthermore, West Bengal does not have a long history in civic or grassroots action, with politics and political affiliation instead dominating cultural and social life. The initiative that developed needed to be responsive to these differences, and as a result, the role of political and government leaders was more central. Despite these differences in structure, over 1000 volunteers were recruited following the initial awareness event in 2014, and more than 900 remained active in 2016.311 The project has grown to cover 30 panchyats (districts) in West Bengal. It remains based on a model of volunteer action, with volunteers leading the care and increasingly the decision making. Although it differed from the Kerala model of volunteer ownership from the outset, the project represents a substantial change to the professionally led models of care in the remainder of the state and reflects a change in attitudes to community organising in health.
In 2014, in an urban hospice in east London, UK, the Compassionate Neighbours project was initiated based on the principles of the Neighbourhood Network in Palliative Care from Kerala.312 It aimed to develop a volunteer-led, community response to end-of-life care. The context again differed from that in Kerala in terms of demographics and health and social care structures, but there was a similarity in the strong history of community activism among local residents. While the core aims of the project were to build community networks and action in end-of-life care, an additional aim was to challenge the professionally led model of care that had arisen in the UK and to understand what a shared lay/professional model would look like. The project developed to have 200 compassionate neighbour volunteers by 2016 across three districts in London. The initiative has been adopted across ten further hospices with over 2000 compassionate neighbours now involved in the work.312 An evaluation of the project described the three crucial factors in its success: (1) recognising and challenging power differentials across communities and institutions from the start; (2) placing relationships at the centre of the work, among people, communities, and institutions; and (3) building of agency not only for volunteers but people at the end of life.313
Lessons for transforming death systems
Examples of the different settings in which the Kerala model has been developed illustrate that local interpretations are needed for success. In all sites, many people volunteered to support people dying, caring, and grieving and remained engaged with the work, showing that there is a desire to support others at these times. Relationships and connections among volunteers—with people at the end of life and their families, and with wider community groups—were drivers for people's engagement and the success of the projects. They provide examples of how civil society and health-care services can work together to care for people as they die.
Section 15: Recommendations
Radical change across death systems is achievable but requires action from all in society. The realistic utopia sets out a vision for future death, dying, and grieving, and these recommendations provide a route through which it may be achieved.
Recognising that systems vary greatly across and within countries, we have made these recommendations general, but we ask that any person, group, or organisation adopting them makes them locally and contextually relevant and SMART (specific, measurable, attainable, relevant, and time-bound).
Recommendations for all
Relationships are fundamental to death, dying and grief. Relationships and networks across society must be placed at the centre of efforts to improve experiences at the end of life.
In whatever country context, high or low income, the responsibility for dying well should not fall solely to health and social services, nor solely to communities; a partnership approach involving shared power, shared decision making, and codesign of services is essential to enable people to die well.
The substantial inequities underpinning how people die globally must be widely acknowledged and steps taken to reduce them. Recognition of intersectional and structural disadvantages by class, gender, race, and geography must be key to this acknowledgment. In particular, the disproportionate role of and burden on women in community care and support in death, dying, and grieving, must be recognised and challenged.
The recommended essential package of palliative care and pain relief health services7 must be provided as a minimum by the health services of all countries. Policies supporting this package, such as opioid access, availability, and education, should be implemented. The package must also include access to personal protective equipment.
Death literacy—the knowledge and skills that people need to navigate death systems—must be developed for all.
Recommendations for civil society
Models of community action in death and dying—such as the compassionate communities, and death education and awareness movements—should be expanded in ways that are sensitive to local populations and led by actors beyond those in palliative care.
Stories and experiences of people dying and grieving in routine, ordinary circumstances from all parts of society should be shared through a range of media to provide a realistic understanding of what happens at the end of life and in grief.
Rituals, traditions, and support structures around death, dying, and grieving should be preserved but re-examined by communities to ensure that they do not reinforce inequities.
Recommendations for health and social care systems
The management of suffering should sit alongside the extension of life as a goal of health-care services and research bodies across settings.
Education on death, dying, and end-of-life care for a person and their family must be integral, substantial, and mandatory in the curriculum of every health and social care student and continuing education for practicing professionals.
All health and social care professionals in all countries and systems must be competent in caring for dying patients and their families. These are core skills, and dying patients should be referred to specialist palliative care services (where available) only when specialist support is necessary.
Patients and families should be provided with clear information about the uncertainties as well as the potential benefits, risks, and harms of interventions in potentially life-limiting illness to enable more informed decisions.
For people with a life-limiting illness, conversations about the fact that they are likely to die from their disease must be sensitively offered throughout their disease course. This conversation should be a core professional duty of the health-care team.
Specialist palliative care should focus on education, research, building capacity of general health-care workers, and extending reach and equity in access to the palliative-care approach rather than just delivering specialist services.
People are increasingly likely to die in care homes, so efforts to improve the experience of living, dying, and grieving in care homes, and adequate resourcing, must be a priority.
Recommendations to researchers and research funders
Funders of research should invest in programmes, institutions, and communities to experiment with rebalancing death and dying.
Funders of research should reflect this rebalancing by increasing spending on end-of-life-care research alongside research aimed at preventing and curing disease. This research should include diverse and innovative work outside health systems, in marginalised populations, and in low-income and middle-income countries.
Research should focus on evaluating options for care at the end of life in low-income and middle-income settings, concentrating on defining and making widely available an essential package of care and services.7
Research funding calls should focus on the development of long-term partnerships, processes, and sustainable work alongside short-term projects to address specific questions.
Research on death, dying, and suffering at the end of life should be undertaken by people from a broad range of areas and disciplines beyond palliative care and include citizens and patients as equal partners in the research.
Research efforts should include understanding, defining, and reducing overtreatment at the end of life.
More research is merited on how information technology and social media are transforming understanding and experiences of death and dying and how their use might be developed further to promote the rebalancing and revaluing of death and dying.
Recommendations to governments and policy makers
Families and communities should not be impoverished by out-of-pocket expenditure for treatments at the end of life, and governments should identify ways to support and manage spending at this time.
The palliative-care approach should be available alongside disease-modifying treatment options, and models of insurance cover or payment should not force patients to choose one over the other.
All countries with universal health care should find ways—perhaps through citizens' juries or other democratic mechanisms—to establish how much citizens are willing to spend on treatments intended to extend life for people with life-limiting disease, recognising that increased spending at the end of life will mean less spending elsewhere. People should be asked how they wish resources to be balanced between hospital treatment and community partnerships and care.
Policies to support informal carers and paid compassionate or bereavement leave should be created and promoted in all countries.
National programmes should be initiated to ensure that everyone has the opportunity to make an advance care plan. Mechanisms should exist to share these plans across health and social care services, alongside access for patients and carers.
Legislators considering the introduction of assisted dying should study the experience of where this practice has already been introduced and think deeply about who will qualify for assisted dying, who will decide who qualifies, who will provide the service, and how it will be managed and regulated.
All countries should have clear guidelines on withholding and withdrawing treatment, reflecting relevant legal, ethical, cultural, and religious perspectives and the distinction between this and assisted dying.
Plans, policies, strategies, and reports on health and social care and wellbeing more broadly should always include consideration of death, dying, and grieving.
Section 16: Next steps
The Commission sees the publication of this report as a beginning, not an end, an opportunity to re-evaluate our relationship with death, and a catalyst for radical change. We have described how death and dying have come to be seen as a primarily physiological event managed by health professionals. Physiological death is an inescapable fact, but we advocate a shift in focus away from excessive dependence on the health-care system and to see it as the social, psychological, physical, and spiritual event that it is. The consequences of our current narrow medicalised focus have included transactional rather than relational care, overtreatment and undertreatment at the end of life, reduced dignity, increased suffering, and poor use of resources.
To achieve our ambition, many changes across systems are needed. We intend our realistic utopia to inspire a collective vision for the future. Our recommendations outline the next steps we would urge policy makers, health and social care systems, civil society, and communities to take.
Beginning in 2022, we will lead a diverse programme of events following on from this report, aiming to embed its recommendations globally and to see the realistic utopia take shape in practice. The Commission will seek to raise funding to experiment with implementing versions of our realistic utopia in different settings. We welcome partnership with participants from every country and with different perspectives in this endeavour. We hope this work will lead to a global network of individuals and institutions working for reform.
We conclude with our core contention: death and dying must be recognised as not only normal, but valuable. Care of the dying and grieving must be rebalanced, and we call on people throughout society to respond to this challenge.
Declaration of interests
LS is an honorary consultant at the WHO Collaborating Centre for Community Participation in Palliative Care and Long Term Care. RS is the chair of Patients Know Best, a for-profit company that gives patients and citizens access to and control of their health and social care records. The system can be used to include advanced care plans and advance directives. He is unpaid but has equity in the company. He is also the unpaid chair of the Point of Care Foundation, which works to humanise health and social care, including at the end of life, and of the UK Health Alliance on Climate Change, which brings together many royal colleges, the British Medical Association, The Lancet, and BMJ to mitigate the effects of climate change and emphasise the risks and potential benefits to health. He holds shares in the UnitedHealth Group, a health and wellbeing company operating in the USA, UK, and other countries, that offers end-of-life services. SHA received an honorarium in 2018 by Mundipharma for leading a publication on cancer pain in low-income and middle-income countries. MH is employed as Head of Information Support at Hospice UK. Hospice UK is the national charity for hospice and end-of-life care. It works to ensure all adults and children living with a terminal or life-shortening illness receive the care and support they need, when they need it. CK, like most people, has personal experience of deaths and prolongation of life that influence the way she thinks as a scholar about these issues. She has written about these publicly, in particular the unwanted prolongation of her sister Polly's life contrary to her best interests, and her mother's death, which was greatly supported by an advance decision to refuse treatment and a lasting power of attorney for health and welfare. CK is also on a number of committees, working parties, and charities related to death and dying, including the core group of the British Medical Association group revising the guidance on clinically assisted nutrition and hydration, and the Guideline Development Group on Prolonged Disorders of Consciousness of the Royal College of Physicians. FMK reports consulting fees unrelated to this paper from Merck KGaA/EMD Serono for work on gender equity in leadership, non-financial support from Grunenthal Foundation, and grants from Roche, Vitas Healthcare, Chinoin, Grunenthal, and Novartis, outside the submitted work. JN is the Chair of University College Hospitals NHS Foundation Trust and Whittington Health NHS Trust. MRR is the unpaid chair of Pallium India, a charitable trust in India that works towards integration of palliative care with health care, and the unpaid director of Trivandrum Institute of Palliative Sciences, a WHO Collaborating Centre for Training and Policy on Access to Pain Relief. ES reports personal fees from the Social Science Research Council during the conduct of the study; and personal fees from Saitama Prefectural University (Japan), Kyoto University (Japan), and the University of Tokyo (Japan), outside the submitted work. KES is funded by a National Institute for Health Research Clinician Scientist Fellowship (CS-2015-15-005) and is the Laing Galazka Chair in Palliative Care at King's College London, funded by an endowment from Cicely Saunders International and the Kirby Laing Foundation. The views expressed are those of the authors and not necessarily those of the NHS, the National Institute for Health Research, or the Department of Health and Social Care. All other authors declare no competing interests.
Acknowledgments
Acknowledgments
The Commission received funding from GW4—the four universities of the West of England (Bath, Bristol, Cardiff, and Exeter)—to hold a meeting in Bristol, UK, and from the Rockefeller Foundation, which funded a meeting of the Commission at Bellagio, Italy. The National Institute for Health Research Bristol Biomedical Research Centre (Jane Blazeby) provided administrative support, and St Christopher's Hospice supported LS in writing up the manuscript. The Abe Fellowship supported ES's participatation in the Commission. KES is the Laing Galazka Chair in palliative care at King's College London, funded by an endowment from Cicely Saunders International and the Kirby Laing Foundation. We thank GW4, the Rockefeller Foundation, and Jane Blazeby for funding; Carol Davies for executive assistance; and the following for material that was used in preparing the report: T Baker, M J Bates, T Bleakley, L Hawryluck, J Hughes, Intensive Care National Audit and Research Centre, P W Keeley, R K Kayambankadzanja, A Kraus, D Miller, C Morris, E Namisango, L C Quigley, C O Schell, T Walter, I Williams, and N Yamaguchi.
The Lancet Commission on the Value of Death
Writing team: Libby Sallnow, Richard Smith. Commissioners: Afsan Bhadelia, Jane Blazeby, Tracey Bleakley, Yali Cong, Luckson Dullie, Robin Durie, Eric A Finkelstein, Nahla Gafer, Sam Guglani, Malcolm Johnson, Celia Kitzinger, Jenny Kitzinger, Felicia Marie Knaul, Arnoldo Kraus, Julia Neuberger, Seamus O'Mahony, M R Rajagopal, Libby Sallnow, Eriko Sase, Sheldon Solomon, Richard Smith, Ros Taylor, Mpho Tutu van Furth, Katrina Wyatt.
Contributors
All authors contributed material to the first draft of the report. LS and RS prepared and revised the three drafts of the report. Specific author contributions: LS wrote the sections on contemporary death systems, Kerala and the realistic utopia. She restructured early drafts, edited the full drafts of the manuscript including the key messages, recommendations and executive summary and revised the final manuscript with RS. RS wrote sections on immortality, climate change and death, and various other sections and the first and revised drafts of the executive summary, introduction, methods, and conclusions. Using the contribution of many authors he edited the first draft of the report. LS and he then prepared the final version in response to comments from reviewers and other authors and commissioners. SHA contributed to drafting sections of the manuscript and contributed to reviewing, editing, and commenting on manuscript drafts. AB participated in discussions on the content of the whole report, contributed to drafting the sections on metrics and methods, as well as in the development of diagrams and recommendations, and read and approved the final report. CC participated in discussions on the content of the whole report, contributed to drafting sections on grief, bereavement, and loneliness, and read and approved the final report. YC contributed to the philosophy section. BD contributed to the writing and data analysis of the economics section. LD participated in discussions on the content of the whole report, contributed to drafting the section on community re-evaluation, and read and approved the final report. RD participated in commissioner meetings; was primary author of the philosophy sections of “Section 4: Philosophical and religious underpinnings of death systems”, including panel 6, contributed to the understanding the role of communities, and was primary author of the panel on the nature of community (appendix); contributed to the understanding of death systems, and to the writing about systems theory in “Section 3: Death systems”; and reviewed and provided comments on the manuscript drafts. EAF participated in commissioner meetings, contributed to writing the economics section, and reviewed and provided comments on the manuscript drafts. SG participated in discussions on the content of the whole report and contributed to drafting sections on the problem, values and death, conversations around and the diagnosing of death, and health economics. SG read and approved the final report. MH contributed to drafting the section (with some background literature searching) on hospice and palliative care and participated in some discussions on the content of the whole report. MH also contributed to the drafting of a background paper, Can hospices tame the fear of death? BSH contributed to the further development of the manuscript designs during a common workshop. She reviewed and revised the chapter on the contribution of hospice and palliative care written by MH, ES, and SR. Together with SR, BSH is responsible for the contribution on care homes and dementia. This work included a literature search, writing process, and development of figures. AK drafted the section of the report on grief and bereavement and reviewing and provided comments on the manuscript drafts. CK contributed to the writing of sections of the report on assisted dying and advance directives, participated in discussions and revisions on the report as a whole and read and approved the final report. FMK participated in regular commissioner meetings, provided bridge information from the Lancet Commission on Global Access to Palliative Care and Pain Relief report, and reviewed and provided comments on the report. SAM participated in commissioner meetings, contributed to the writing of sections of the report, and reviewed and provided comments on the manuscript drafts. JN contributed to the drafting of sections of the report and reviewed and provided comments on the manuscript draft. SoM wrote five discussion papers for this document: these relate to: (1) the compression of morbidity; (2) the good death; (3) the lawyerisation of death; (4) biogerontology and the science of ageing; and (5) the difficult conversation. Edited versions of these papers appear in the final text. MRR contributed to literature searching and writing the manuscript. SR contributed to the writing of the advance care planning section, participated in commissioner meetings, and reviewed and provided comments on the manuscript drafts. ES contributed to the literature search, data collection, data analysis, and data interpretation, and to writing the manuscript. KES wrote the first draft of the section of the report on research in palliative care and reviewed and provided comments on the manuscript drafts. SS participated in discussions on the content of the taming death section of the report and wrote a working paper on terror management theory describing how conscious and non-conscious death anxiety influences human attitudes and behaviour in general, and in medical practice. RT contributed to the original draft, drafted paragraphs on the will to live, power and gender, and hospice care, provided ongoing comments on structure and revisions, and approved the final submission. MTvF participated in commissioner meetings, contributed to the writing of sections of the report, and reviewed and provided comments on the manuscript drafts. KW participated in discussions on the content of the whole report, contributed to drafting the section on communities including developing the diagrams, and read and approved the final report.
Supplementary Material
References
- 1.Langton JM, Blanch B, Drew AK, Haas M, Ingham JM, Pearson SA. Retrospective studies of end-of-life resource utilization and costs in cancer care using health administrative data: a systematic review. Palliat Med. 2014;28:1167–1196. doi: 10.1177/0269216314533813. [DOI] [PubMed] [Google Scholar]
- 2.Juthani-Mehta M, Malani PN, Mitchell SL. Antimicrobials at the end of life: an opportunity to improve palliative care and infection management. JAMA. 2015;314:2017–2018. doi: 10.1001/jama.2015.13080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kellehear A. Routledge; Oxford: 2005. Compassionate Cities. [Google Scholar]
- 4.National Confidential Enquiry into Patient Outcome and Death (NCEPOD) NCEPOD; London: 2008. For better, for worse? a review of the care of patients who died within 30 days of receiving systemic anti-cancer therapy. [Google Scholar]
- 5.Cassell EJ. Oxford University Press; Oxford: 2004. The nature of suffering and the goals of medicine. [Google Scholar]
- 6.Brownlee S, Chalkidou K, Doust J, et al. Evidence for overuse of medical services around the world. Lancet. 2017;390:156–168. doi: 10.1016/S0140-6736(16)32585-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Knaul FM, Farmer PE, Krakauer EL, et al. Alleviating the access abyss in palliative care and pain relief—an imperative of universal health coverage: the Lancet Commission report. Lancet. 2017;391:1391–1454. doi: 10.1016/S0140-6736(17)32513-8. [DOI] [PubMed] [Google Scholar]
- 8.Menzies RE, Neimeyer RA, Menzies RG. Death anxiety, loss, and grief in the time of COVID-19. Behav Change. 2020;37:111–115. [Google Scholar]
- 9.Özer Ö, Özkan O, Özmen S, Erçoban N. Investigation of the effect of COVID-19 perceived risk on death anxiety, satisfaction with life, and psychological well-being. Omega (Westport) 2021 doi: 10.1177/00302228211026169. published online June 19. [DOI] [PubMed] [Google Scholar]
- 10.Harari YN. Will coronavirus change our attitudes to death? Quite the opposite. Guardian. 2020 https://www.theguardian.com/books/2020/apr/20/yuval-noah-harari-will-coronavirus-change-our-attitudes-to-death-quite-the-opposite published online April 20. [Google Scholar]
- 11.Healthcare Without Harm Healthcare's carbon footprint. Healthcare without harm. 2019. https://www.arup.com/perspectives/publications/research/section/healthcares-climate-footprint
- 12.Watts N, Amann M, Arnell N, et al. The 2019 report of The Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet. 2019;394:1836–1878. doi: 10.1016/S0140-6736(19)32596-6. [DOI] [PubMed] [Google Scholar]
- 13.Wight R. House of Anansi Press; Toronto: 2004. A short history of progress. [Google Scholar]
- 14.Masson-Delmotte VP, Zhai H-O, Pörtner D, et al. World Meteorological Organization; Geneva: 2018. Global Warming of 1.5°C. An IPCC Special Report on the impacts of global warming of 1.5°C above pre-industrial levels and related global greenhouse gas emission pathways, in the context of strengthening the global response to the threat of climate change, sustainable development, and efforts to eradicate poverty. [Google Scholar]
- 15.Foster GL, Royer DL, Lunt DJ. Future climate forcing potentially without precedent in the last 420 million years. Nat Commun. 2017;8 doi: 10.1038/ncomms14845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.UK Health Alliance for Climate Change Call to action. 2021. https://action.ukhealthalliance.org/page/76199/petition/1
- 17.NHS England . NHSEI; London: 2020. Delivering a ‘Net Zero’ National Health Service.https://www.england.nhs.uk/greenernhs/publication/delivering-a-net-zero-national-health-service/ [Google Scholar]
- 18.Sustainable Healthcare Coalition Sustainable care pathways guidance. https://shcpathways.org/
- 19.Kremer W. Dissolving the dead. 2017. https://www.bbc.co.uk/news/resources/idt-sh/dissolving_the_dead
- 20.Kastenbaum R. CV Mosby; St Louis, MO: 1977. Death, society, and human experience. [Google Scholar]
- 21.Rawls J. Harvard University Press; Cambridge: 1993. Law of the peoples. [Google Scholar]
- 22.Shemie SD, Hornby L, Baker A, et al. The International Guidelines for Determination of Death phase 1 participants, in collaboration with the World Health Organization. International guideline development for the determination of death. Intensive Care Med. 2014;40:788–797. doi: 10.1007/s00134-014-3242-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.WHO . WHO; Geneva: 2017. Clinical criteria for the determination of death. WHO technical expert consultation. [Google Scholar]
- 24.Jyh-Gang H, Ying-Wei W. Application of signs of dying identified in traditional Chinese, Tibetan, and modern Western medicine in terminal care. Tzu Chi Med J. 2012;24:12–15. [Google Scholar]
- 25.Wang H, Abbas KM, Abbasifard M, et al. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1160–1203. doi: 10.1016/S0140-6736(20)30977-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murray CJ, Abbafati C, Abbas KM, et al. Five insights from the global burden of disease study 2019. Lancet. 2020;396:1135–1159. doi: 10.1016/S0140-6736(20)31404-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marmot M. Health equity in England: the Marmot review 10 years on. BMJ. 2020;368:m693. doi: 10.1136/bmj.m693. [DOI] [PubMed] [Google Scholar]
- 28.Montez JK, Zajacova A. Why is life expectancy declining among low-educated women in the United States? Am J Public Health. 2014;104:e5–e7. doi: 10.2105/AJPH.2014.302146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harper S, Riddell CA, King NB. Declining life expectancy in the United States: missing the trees for the forest. Annu Rev Public Health. 2021;42:381–403. doi: 10.1146/annurev-publhealth-082619-104231. [DOI] [PubMed] [Google Scholar]
- 30.Woolf SH, Masters RK, Aron LY. Effect of the covid-19 pandemic in 2020 on life expectancy across populations in the USA and other high income countries: simulations of provisional mortality data. BMJ. 2021;373 doi: 10.1136/bmj.n1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.King's Fund . King's Fund; London: 2021. What is happening to life expectancy in England?https://www.kingsfund.org.uk/publications/whats-happening-life-expectancy-england [Google Scholar]
- 32.UCL Institute of Global Equity . UCL Institute of Global Equity; London: 2021. Build back fairer in Greater Manchester: health equity and dignified lives.https://www.instituteofhealthequity.org/resources-reports/build-back-fairer-in-greater-manchester-health-equity-and-dignified-lives/build-back-fairer-in-greater-manchester-main-report.pdf [Google Scholar]
- 33.Ahsan KZ, Alam N, Kim Streatfield P. Epidemiological transition in rural Bangladesh, 1986-2006. Glob Health Action. 2009;19:2. doi: 10.3402/gha.v2i0.1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.United Nations World Mortality Report. 2019. https://www.un.org/en/development/desa/population/publications/pdf/mortality/WMR2019/WorldMortality2019DataBooklet.pdf
- 35.World Population Review Gini coefficient by country. 2020. https://worldpopulationreview.com/countries/gini-coefficient-by-country/
- 36.World Bank Maternal mortality ratio (modeled estimate, per 100,000 live births) 2019. https://data.worldbank.org/indicator/SH.STA.MMRT
- 37.World Bank Cause of death, by communicable diseases and maternal, prenatal and nutrition conditions (% of total) https://data.worldbank.org/indicator/SH.DTH.COMM.ZS
- 38.WHO NCD mortality and morbidity. 2016. https://www.who.int/gho/ncd/mortality_morbidity/en/
- 39.WHO Suicide rate estimates, age-standardized. Estimates by country. 2016. https://apps.who.int/gho/data/node.main.MHSUICIDEASDR?lang=en
- 40.Institute for Advanced Study of the Americas Burden of serious health-related suffering. Country data sheet. 2015. https://mia.as.miami.edu/initiatives/hemispheric-health/lancet-palliative-care/background-resources/index.html
- 41.Pivodic L, Pardon K, Morin L, et al. the EURO IMPACT Place of death in the population dying from diseases indicative of palliative care need: a cross-national population-level study in 14 countries. J Epidemiol Community Health. 2016;70:17–24. doi: 10.1136/jech-2014-205365. [DOI] [PubMed] [Google Scholar]
- 42.Bekelman JE, Halpern SD, Blankart CR, et al. Comparison of site of death, health care utilization, and hospital expenditures for patients dying with cancer in 7 developed countries. JAMA. 2016;315:272–283. doi: 10.1001/jama.2015.18603. [DOI] [PubMed] [Google Scholar]
- 43.Luta X, Diernberger K, Bowden J, et al. Healthcare trajectories and costs in the last year of life: a retrospective primary care and hospital analysis. BMJ Support Palliat Care. 2020;02 doi: 10.1136/bmjspcare-2020-002630. bmjspcare-2020-002630. [DOI] [PubMed] [Google Scholar]
- 44.Kim DY, Lee SM, Lee KE, et al. An evaluation of nutrition support for terminal cancer patients at teaching hospitals in Korea. Cancer Res Treat. 2006;38:214–217. doi: 10.4143/crt.2006.38.4.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Horsfall D, Noonan K, Leonard R. Bringing our dying home: how caring for someone at end of life builds social capital and develops compassionate communities. Health Sociol Rev. 2012;21:373–378. [Google Scholar]
- 46.Gawande A. Profile Books; London: 2015. Being Mortal. Illness, Medicine and What Matters in the End. [DOI] [PubMed] [Google Scholar]
- 47.Lofland LH. MIT Press; Cambridge: 2019. The craft of dying. [Google Scholar]
- 48.WHO Palliative care. https://www.who.int/news-room/fact-sheets/detail/palliative-care
- 49.Becker E. Free Press; New York: 1973. Denial of Death. [Google Scholar]
- 50.Doughty C. Weidenfeld & Nicolson; London: 2017. From here to eternity: travelling the world to find the good death. [Google Scholar]
- 51.Kroik L, Lindqvist O, Stoor K, Tishelman C. The past is present: death systems among the Indigenous Sámi in Northern Scandinavia today. Mortality. 2020;25:470–489. [Google Scholar]
- 52.Liu Y, van Schalkwyk GJ. Death preparation of Chinese rural elders. Death Stud. 2019;43:270–279. doi: 10.1080/07481187.2018.1458760. [DOI] [PubMed] [Google Scholar]
- 53.Swinburn BA, Kraak VI, Allender S, et al. The global syndemic of obesity, undernutrition, and climate change: the Lancet Commission report. Lancet. 2019;393:791–846. doi: 10.1016/S0140-6736(18)32822-8. [DOI] [PubMed] [Google Scholar]
- 54.Fowler PJ, Hovmand PS, Marcal KE, Das S. Solving homelessness from a complex systems perspective: insights for prevention responses. Annu Rev Public Health. 2019;40:465–486. doi: 10.1146/annurev-publhealth-040617-013553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hay K, McDougal L, Percival V, et al. Disrupting gender norms in health systems: making the case for change. Lancet. 2019;393:2535–2549. doi: 10.1016/S0140-6736(19)30648-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chan M. Address by Dr Margaret Chan, WHO Director-General at the 66th session of the WHO Regional Committee for Europe. 2016. https://www.euro.who.int/en/about-us/governance/regional-committee-for-europe/past-sessions/66th-session/speeches-and-presentations/address-by-dr-margaret-chan,-who-director-general-at-the-66th-session-of-the-who-regional-committee-for-europe
- 57.Plsek PE, Greenhalgh T. Complexity science: the challenge of complexity in health care. BMJ. 2001;323:625–628. doi: 10.1136/bmj.323.7313.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sen AK. Harvard University Press; Cambridge, MA: 1992. Inequality reexamined. [Google Scholar]
- 59.Ruger JP. Health capability: conceptualization and operationalization. Am J Public Health. 2010;100:41–49. doi: 10.2105/AJPH.2008.143651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Diagne S. In: A companion to African philosophy. Wiredu K, editor. Blackwell; Oxford: 2004. Islam in Africa: examining the notion of an African identity within the Islamic world. [Google Scholar]
- 61.Menkiti IA. In: A companion to African philosophy. Wiredu K, editor. Blackwell; Oxford: 2004. On the normative conception of a person. [Google Scholar]
- 62.Baloyi L, Makobe-Rabothata M. In: Toward sustainable development through nurturing diversity: proceedings from the 21st International Congress of the International Association for Cross-Cultural Psychology. Jackson LTB, Meiring D, Van de Vijver FJR, Idemoudia ES, Gabrenya WK Jr, editors. 2014. The African conception of death: a cultural implication.https://scholarworks.gvsu.edu/iaccp_papers/119/ [Google Scholar]
- 63.Moeke-Maxwell T, Mason K, Toohey F, Dudley J. In: Textbook of palliative care. MacLeod R, Van den Block L, editors. Springer; 2019. Pou Aroha: an indigenous perspective of Māori palliative care, Aotearoa New Zealand. [Google Scholar]
- 64.Plato . In: Phaedo. Hackforth R, editor. Cambridge University Press; Cambridge: 1955. [Google Scholar]
- 65.de Montaigne M. In: The complete works. Frame DM, editor. Everyman's Library; London: 2003. [Google Scholar]
- 66.Epicurus . In: The Epicurus reader. Inwood B, editor. Hackett Publishing Company; Indianapolis: 1994. [Google Scholar]
- 67.Planck MK. Philosophical Library; New York: 1950. Scientific autobiography and other papers. [Google Scholar]
- 68.Heidegger M. In: Being and time. Macquarrie J, Robinson E, editors. Basil Blackwell; Oxford: 1962. [Originally published as Sein und Zeit. Tübingen: Max Niemeyer, 1927.]. [Google Scholar]
- 69.Levinas E. In: Alterity and transcendence. Smith M B, editor. The Athlone Press; London: 1999. [Originally published as Altérité et Transcendence. Paris: Fata Morgana, 1995.]. [Google Scholar]
- 70.Cooke R. Is there a better way to die? Guardian. 2020 https://www.theguardian.com/society/2020/jul/05/is-there-a-better-way-to-die published online July 5. [Google Scholar]
- 71.Seneca . In: Moral essays volume II. Loeb Classical Library 254. Basore J W, editor. Harvard University Press; Cambridge: 1932. On the shortness of life. [Google Scholar]
- 72.Mauss M. WW Norton & Company; New York: 2000. The gift: the form and reason for exchange in archaic societies. [Google Scholar]
- 73.Toolis K. W&N; London: 2018. My father's wake. [Google Scholar]
- 74.Kellehear A. Columbia University Press; New York: 2014. The inner life of the dying person. [Google Scholar]
- 75.Gandhi MK. Prakash Book Depot; New Delhi: 2009. My experiments with truth. [Google Scholar]
- 76.Sibanda P. The dimensions of ‘Hunhu/Ubuntu’ (humanism in the African sense): the Zimbabwean conception. IOSR Journal of Engineering. 2014;4:26–29. [Google Scholar]
- 77.Tutu D. Images; Mulgrave: 2000. No future without forgiveness. [Google Scholar]
- 78.Mbiti JS. Heinemann; Portsmouth: 1992. African religions and philosophy. [Google Scholar]
- 79.Ngubane S. In: Death across cultures: death and dying in non-western cultures. Selin H, Rakoff R, editors. Springer; New York: 2019. Death and burial practices in contemporary Zulu culture, South Africa. [Google Scholar]
- 80.Croucher K, Büster L, Dayes J, et al. Archaeology and contemporary death: Using the past to provoke, challenge and engage. PLoS One. 2020;15 doi: 10.1371/journal.pone.0244058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Aries P. In: Western attitudes toward death: from the middle ages to the present. Ranum PM, editor. John Hopkins University Press; Baltimore: 1974. [Google Scholar]
- 82.Illich I. Marion Boyars; London: 1975. Limits to medicine. [Google Scholar]
- 83.Büyüm AM, Kenney C, Koris A, Mkumba L, Raveendran Y. Decolonising global health: if not now, when? BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2020-003394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Collective for Radical Death Studies About CRDS. 2021. https://radicaldeathstudies.com/about-crds/
- 85.WHO Social Determinants of Health. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1
- 86.Public Health England . PHE; London: 2020. Disparities in the risk and outcomes of COVID-19.https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/908434/Disparities_in_the_risk_and_outcomes_of_COVID_August_2020_update.pdf [Google Scholar]
- 87.Abbasi J. Taking a closer look at COVID-19, health inequities, and racism. JAMA. 2020;324:427–429. doi: 10.1001/jama.2020.11672. [DOI] [PubMed] [Google Scholar]
- 88.Petersen EE, Davis NL, Goodman D, et al. Racial/ethnic disparities in pregnancy-related deaths—United States, 2007–2016. MMWR Morb Mortal Wkly Rep. 2019;68:762–765. doi: 10.15585/mmwr.mm6835a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Umberson D, Olson JS, Crosnoe R, Liu H, Pudrovska T, Donnelly R. Death of family members as an overlooked source of racial disadvantage in the United States. Proc Natl Acad Sci USA. 2017;114:915–920. doi: 10.1073/pnas.1605599114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 91.Williams H, Varney J. Taylor, Fish J, Durr P, Elan-Cane C. The lesbian, gay, bisexual and trans public health outcomes framework companion document. London: Department of Health, undated. https://www.london.gov.uk/sites/default/files/LGBT%20Public%20Health%20Outcomes%20Framework%20Companion%20Doc.pdf
- 92.Cloyes KG, Hull W, Davis A. Palliative and end-of-life care for lesbian, gay, bisexual, and transgender (LGBT) cancer patients and their caregivers. Semin Oncol Nurs. 2018;34:60–71. doi: 10.1016/j.soncn.2017.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.International Labour Organization . International Labour Office; Geneva: 2017. World employment social outlook: trends for women 2017. [Google Scholar]
- 94.Langer A, Meleis A, Knaul FM, et al. Women and health: the key for sustainable development. Lancet. 2015;386:1165–1210. doi: 10.1016/S0140-6736(15)60497-4. [DOI] [PubMed] [Google Scholar]
- 95.Mackinnon CJ. Applying feminist, multicultural, and social justice theory to diverse women who function as caregivers in end-of-life and palliative home care. Palliat Support Care. 2009;7:501–512. doi: 10.1017/S1478951509990514. [DOI] [PubMed] [Google Scholar]
- 96.Crenshaw K. Demarginalizing the intersection of race and sex: a black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. Univ Chic Leg Forum. 1989;1:139–167. [Google Scholar]
- 97.Goleman H. Checking my inner world: race is not real, yet it can control us. Tricycle. 2016 https://tricycle.org/trikedaily/checking-my-inner-world/ published online July 11. [Google Scholar]
- 98.Khan H. NESTA; London: 2018. How to change power in health.https://www.nesta.org.uk/blog/how-to-change-power-in-health [Google Scholar]
- 99.Care Quality Commission . CQC; London: 2021. Protect, respect, connect—decisions about living and dying well during COVID-19. [Google Scholar]
- 100.House of Commons Public Accounts Committee . Parliament; London: 2021. COVID-19: government procurement and supply of personal protective equipment. [Google Scholar]
- 101.Chochinov HM, Kristjanson LJ, Hack TF, Hassard T, McClement S, Harlos M. Burden to others and the terminally ill. J Pain Symptom Manage. 2007;34:463–471. doi: 10.1016/j.jpainsymman.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 102.Tataryn D, Chochinov HM. Predicting the trajectory of will to live in terminally ill patients. Psychosomatics. 2002;43:370–377. doi: 10.1176/appi.psy.43.5.370. [DOI] [PubMed] [Google Scholar]
- 103.Khan L, Wong R, Li M, et al. Maintaining the will to live of patients with advanced cancer. Cancer J. 2010;16:524–531. doi: 10.1097/PPO.0b013e3181f45b90. [DOI] [PubMed] [Google Scholar]
- 104.Rodin G, Zimmermann C, Rydall A, et al. The desire for hastened death in patients with metastatic cancer. J Pain Symptom Manage. 2007;33:661–675. doi: 10.1016/j.jpainsymman.2006.09.034. [DOI] [PubMed] [Google Scholar]
- 105.Brown GK, Steer RA, Henriques GR, Beck AT. The internal struggle between the wish to die and the wish to live: a risk factor for suicide. Am J Psychiatry. 2005;162:1977–1979. doi: 10.1176/appi.ajp.162.10.1977. [DOI] [PubMed] [Google Scholar]
- 106.Solomon S, Greenberg J, Pyszczynski T. Random House; New York: 2015. The worm at the core: on the role of death in life. [Google Scholar]
- 107.Tomer A, Eliason G. Toward a comprehensive model of death anxiety. Death Stud. 1996;20:343–365. doi: 10.1080/07481189608252787. [DOI] [PubMed] [Google Scholar]
- 108.Rodríguez-Prat A, Balaguer A, Booth A, Monforte-Royo C. Understanding patients' experiences of the wish to hasten death: an updated and expanded systematic review and meta-ethnography. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2017-016659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Guy M, Stern TA. The desire for death in the setting of terminal illness: a case discussion. Prim Care Companion J Clin Psychiatry. 2006;8:299–305. doi: 10.4088/pcc.v08n0507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.van Wijngaarden E, Leget C, Goossensen A. Ready to give up on life: the lived experience of elderly people who feel life is completed and no longer worth living. Soc Sci Med. 2015;138:257–264. doi: 10.1016/j.socscimed.2015.05.015. [DOI] [PubMed] [Google Scholar]
- 111.Span P. Loneliness can be deadly for elders; friends are the antidote. New York Times. 2016 published Dec 30. [Google Scholar]
- 112.Shimizu M, Pelham BW. Postponing a date with the Grim Reaper: ceremonial events and mortality. Basic Appl Soc Psych. 2008;30:36–45. [Google Scholar]
- 113.Ehrenreich B. Smile! You've got cancer. Guardian. 2010 https://www.theguardian.com/lifeandstyle/2010/jan/02/cancer-positive-thinking-barbara-ehrenreich published Jan 2. [Google Scholar]
- 114.Stroebe M, Schut H, Stroebe W. Health outcomes of bereavement. Lancet. 2007;370:1960–1973. doi: 10.1016/S0140-6736(07)61816-9. [DOI] [PubMed] [Google Scholar]
- 115.Erlangsen A, Runeson B, Bolton JM, et al. Association between spousal suicide and mental, physical, and social health outcomes: a longitudinal and nationwide register-based study. JAMA Psychiatry. 2017;74:456–464. doi: 10.1001/jamapsychiatry.2017.0226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Raphael B. Basic Books; New York: 1983. The anatomy of bereavement. [Google Scholar]
- 117.Kübler-Ross E. Macmillan; New York: 1969. On death and dying. [Google Scholar]
- 118.Tonkin L. Growing around grief—another way of looking at grief and recovery. Bereave Care. 1996;15:10. [Google Scholar]
- 119.Stroebe M, Schut H. The dual process model of coping with bereavement: rationale and description. Death Stud. 1999;23:197–224. doi: 10.1080/074811899201046. [DOI] [PubMed] [Google Scholar]
- 120.Klass D, Silverman PR, Nickman S. Taylor & Francis; Abingdon: 1996. Continuing bonds: new understandings of grief. [Google Scholar]
- 121.Burrell A, Selman LE. How do funeral practices impact bereaved relatives' mental health, grief and bereavement? A mixed methods review with implications for COVID-19. Omega (Westport) 2020 doi: 10.1177/0030222820941296. published online July 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Aoun SM, Lowe J, Christian KM, Rumbold B. Is there a role for the funeral service provider in bereavement support within the context of compassionate communities? Death Stud. 2019;43:619–628. doi: 10.1080/07481187.2018.1506835. [DOI] [PubMed] [Google Scholar]
- 123.Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008;358:2249–2258. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357:370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 125.Holt-Lunstad J, Robles TF, Sbarra DA. Advancing social connection as a public health priority in the United States. Am Psychol. 2017;72:517–530. doi: 10.1037/amp0000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Rovelli C. Penguin; London: 2021. Helgoland. [Google Scholar]
- 127.Cottam H. Virago; London: 2018. Radical help: how we can remake the relationships between us and revolutionise the welfare state. [Google Scholar]
- 128.Hendrich A, Chow MP, Skierczynski BA, Lu Z. A 36-hospital time and motion study: how do medical-surgical nurses spend their time? Perm J. 2008;12:25–34. doi: 10.7812/tpp/08-021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Brodwin E, Radovanovic D. Here's how many minutes the average doctor actually spends with each patient. Business Insider UK. 2006 published online April 6. [Google Scholar]
- 130.Kellehear A. The social nature of dying and the social model of health. In: Abel J, Kellehear A (eds). Oxford Textbook of Public Health Palliative Care. Oxford: Oxford University Press (in press).
- 131.End of Life Doula UK What is an end of life doula? https://eol-doula.uk/what-is-an-end-of-life-doula/
- 132.Rawlings D, Tieman J, Miller-Lewis L, Swetenham K. What role do Death Doulas play in end-of-life care? A systematic review. Health Soc Care Community. 2019;27:e82–e94. doi: 10.1111/hsc.12660. [DOI] [PubMed] [Google Scholar]
- 133.Horsfall D, Leonard R, Noonan K, Rosenberg J. Working together–apart: exploring the relationships between formal and informal care networks for people dying at home. Prog Palliat Care. 2013;21:331–336. [Google Scholar]
- 134.Special issue supplement: conference abstracts from the 6th Public Health Palliative Care International Conference. Prog Palliat Care. 2020;28:123–188. [Google Scholar]
- 135.Public Health Palliative Care International Creating compassionate communities. https://www.phpci.org/
- 136.Economist Intelligence Unit . Lien Foundation; Singapore: 2015. The quality of death: ranking end of life care across the world. [Google Scholar]
- 137.Kellehear A. Compassionate cities: global significance and meaning for palliative care. Prog Palliat Care. 2020;28:115–119. [Google Scholar]
- 138.Durie R, Wyatt K. Connecting communities and complexity: a case study in creating the conditions for transformational change. Crit Public Health. 2013;23:174–187. [Google Scholar]
- 139.Durie R, Wyatt K. New communities, new relations: the impact of community organization on health outcomes. Soc Sci Med. 2007;65:1928–1941. doi: 10.1016/j.socscimed.2007.05.039. [DOI] [PubMed] [Google Scholar]
- 140.Loomba Foundation . Loomba Foundation; London: 2016. World widows report. [Google Scholar]
- 141.Hungerford TL. The economic consequences of widowhood on elderly women in the United States and Germany. Gerontologist. 2001;41:103–110. doi: 10.1093/geront/41.1.103. [DOI] [PubMed] [Google Scholar]
- 142.Doka K, editor. Disenfranchised grief: recognising hidden sorrow. Lexington Books; Lanham: 1989. [Google Scholar]
- 143.Miles L, Corr CA. Death cafe. Omega (Westport) 2017;75:151–165. doi: 10.1177/0030222815612602. [DOI] [PubMed] [Google Scholar]
- 144.Smith R. Death festival: Day one. BMJ Opinion. 2012 https://blogs.bmj.com/bmj/2012/01/30/richard-smith-death-festival-day-one published online Jan 30. [Google Scholar]
- 145.Institute of Palliative Medicine Kerala Curios Festival. https://www.instituteofpalliativemedicine.org/eventdetail.php
- 146.Matters D. Awareness week. https://www.dyingmatters.org/AwarenessWeek
- 147.Lien Foundation Life before death. http://lifebeforedeath.com/about-us/
- 148.Shepherd A. The final call: how to talk about death. BMJ. 2019;365 doi: 10.1136/bmj.l2192. [DOI] [PubMed] [Google Scholar]
- 149.Miller-Lewis L, Tieman J, Rawlings D, Parker D, Sanderson C. Can exposure to online conversations about death and dying influence death competence? An exploratory study within an Australian massive open online course. Omega (Westport) 2020;81:242–271. doi: 10.1177/0030222818765813. [DOI] [PubMed] [Google Scholar]
- 150.Kellehear A. Compassionate communities. Routledge; 2015. The Compassionate City Charter: inviting the cultural and social sectors into end of life care; pp. 76–87. [Google Scholar]
- 151.Ashton J, Grey P, Barnard K. Healthy cities—WHO's new public health initiative. Health Promot Int. 1986;1:319–324. [Google Scholar]
- 152.Huang CY, Huang SJ, Chao KI, et al. The 2020 Taipei declaration for universal palliative care. J Palliat Med. 2020;23:747–748. doi: 10.1089/jpm.2020.0026. [DOI] [PubMed] [Google Scholar]
- 153.Dead Social About Dead Social and the services we provide. http://deadsocial.org/about
- 154.Horton H. Dead could outnumber the living on Facebook by 2098. Telegraph. 2016, March 7 https://www.telegraph.co.uk/technology/2016/03/07/dead-could-outnumber-the-living-on-facebook-by-2098/ [Google Scholar]
- 155.Zaman M, Mohapatra A, Espinal-Arango S, Jadad A. What would it take to die well? A systematic review of systematic reviews on the conditions for a good death. Lancet Healthy Longevity. 2021;2:e593–e600. doi: 10.1016/S2666-7568(21)00097-0. [DOI] [PubMed] [Google Scholar]
- 156.Gafaar TO, Pesambili M, Henke O, Vissoci JRN, Mmbaga BT, Staton C. Good death: an exploratory study on perceptions and attitudes of patients, relatives, and healthcare providers, in northern Tanzania. PLoS One. 2020;15 doi: 10.1371/journal.pone.0233494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Sleeman KE, Leniz J, Higginson IJ, Bristowe K. Is end-of-life care a priority for policymakers? Qualitative documentary analysis of health care strategies. Palliat Med. 2018;32:1474–1486. doi: 10.1177/0269216318786333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.WHO . World Health Organization; Geneva: 2020. Decade of Health Aging. [Google Scholar]
- 159.Institute of Medicine Food and Nutrition Board . National Academies Press; Washington (DC): 2012. Nutrition and healthy aging in the community: workshop summary. [PubMed] [Google Scholar]
- 160.All Party Parliamentary Group for Longevity . All Party Parliamentary Group for Longevity; London: 2020. The health of the nation: a strategy for healthier longer lives. [Google Scholar]
- 161.Lancet Palliative care and the COVID-19 pandemic. Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30822-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Williams R, Aithal G, Aleaxnder GJ, et al. Unacceptable failures: the final report of the Lancet Commission into liver disease in the UK. Lancet. 2020;395:226–239. doi: 10.1016/S0140-6736(19)32908-3. [DOI] [PubMed] [Google Scholar]
- 163.Bleakley T, Smith R, Taylor R. Has the NHS Long Term Plan forgotten we are all going to die? Lancet. 2019;393:387–389. doi: 10.1016/S0140-6736(19)30201-6. [DOI] [PubMed] [Google Scholar]
- 164.Goffman E. Vintage; New York City: 1961. Asylums. [Google Scholar]
- 165.Friedson E. Aldine; Piscatawy: 2006. Professional dominance: the social structure of medical care. [originally published 1970]. [Google Scholar]
- 166.Foucault M. Routledge; London: 2003. The birth of the clinic: an archaeology of medical perception. [originally published in French, 1963]. [Google Scholar]
- 167.Sikora K. “The NHS is the last bastion of communism.”. BBC Newsnight. 2017 https://www.bbc.co.uk/news/av/world-39051561 published online Feb 22. [Google Scholar]
- 168.Dignitas Data on deaths at Dignitas. http://www.dignitas.ch/images/stories/pdf/statistik-ftb-jahr-wohnsitz-1998-2018.pdf
- 169.Oregon Health Authority Death with dignity act. https://www.oregon.gov/oha/PH/ProviderPartnerResources/Evaluationresearch/deathwithdignityact/Pages/index.aspx
- 170.Public Health Division. Center for Health Statistics Oregon death with dignity act. 2020 data summary. 2020. https://www.oregon.gov/oha/PH/PROVIDERPARTNERRESOURCES/EVALUATIONRESEARCH/DEATHWITHDIGNITYACT/Documents/year23.pdf
- 171.Smith R. Learning from Canada about assisted dying. BMJ Opinion. 2020 https://blogs.bmj.com/bmj/2020/01/22/richard-smith-learning-from-canada-about-assisted-dying/ [Google Scholar]
- 172.Government of Canada Fourth interim report on medical assistance in dying in Canada. 2019. https://www.canada.ca/en/health-canada/services/publications/health-system-services/medical-assistance-dying-interim-report-april-2019.html
- 173.Sleeman K. Assisted dying—how safe is safe enough? BMJ Opinion. 2018 https://blogs.bmj.com/bmj/2018/03/08/katherine-sleeman-assisted-dying-how-safe-is-safe-enough/ [Google Scholar]
- 174.Rietjens JAC, Sudore RL, Connolly M, et al. Definition and recommendations for advance care planning: an international consensus supported by the European Association for Palliative Care. Lancet Oncol. 2017;18:e543–e551. doi: 10.1016/S1470-2045(17)30582-X. [DOI] [PubMed] [Google Scholar]
- 175.Jimenez G, Tan WS, Virk AK, Low CK, Car J, Ho AHY. Overview of systematic reviews of advance care planning: summary of evidence and global lessons. J Pain Symptom Manage. 2018;56:436. doi: 10.1016/j.jpainsymman.2018.05.016. 59.e25. [DOI] [PubMed] [Google Scholar]
- 176.Abel J, Kellehear A, Millington Sanders C, Taubert M, Kingston H. Advance care planning re-imagined: a needed shift for COVID times and beyond. Palliat Care Soc Pract. 2020 doi: 10.1177/2632352420934491. published online Aug 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Pope TM. Legal briefing: the new patient self-determination act. J Clin Ethics. 2013;24:156–167. [PubMed] [Google Scholar]
- 178.McDowell M. Medical profession should ‘shoulder its own ethical burden’. Medical Independent. 2017 https://www.medicalindependent.ie/medical-profession-should-shoulder-its-own-ethical-burden/ published online Sept 21. [Google Scholar]
- 179.SunLife The cost of dying across the world. https://www.sunlife.co.uk/over-50-life-insurance/international-cost-of-dying/
- 180.SunLife The cost of dying 2021 report. https://www.sunlife.co.uk/siteassets/documents/cost-of-dying/cost-of-dying-report-2021.pdf/
- 181.Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, Evans T. Protecting households from catastrophic health spending. Health Aff (Millwood) 2007;26:972–983. doi: 10.1377/hlthaff.26.4.972. [DOI] [PubMed] [Google Scholar]
- 182.WHO. World Bank . World Health Organization; Geneva: 2019. Global Monitoring Report on Financial Protection in Health 2019.https://www.who.int/publications/i/item/9789240003958 [Google Scholar]
- 183.Shrime MG, Dare AJ, Alkire BC, O'Neill K, Meara JG. Catastrophic expenditure to pay for surgery worldwide: a modelling study. Lancet Glob Health. 2015;3(suppl 2):S38–S44. doi: 10.1016/S2214-109X(15)70085-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Himmelstein DU, Thorne D, Warren E, Woolhandler S. Medical bankruptcy in the United States, 2007: results of a national study. Am J Med. 2009;122:741–746. doi: 10.1016/j.amjmed.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 185.Leng A, Jing J, Nicholas S, Wang J. Catastrophic health expenditure of cancer patients at the end-of-life: a retrospective observational study in China. BMC Palliat Care. 2019;18:43. doi: 10.1186/s12904-019-0426-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Aldridge MD, Kelley AS. The myth regarding the high cost of end-of-life care. Am J Public Health. 2015;105:2411–2415. doi: 10.2105/AJPH.2015.302889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.French EB, McCauley J, Aragon M, et al. End-of-life medical spending in last twelve months of life is lower than previously reported. Health Aff (Millwood) 2017;36:1211–1217. doi: 10.1377/hlthaff.2017.0174. [DOI] [PubMed] [Google Scholar]
- 188.Kardamanidis K, Lim K, Da Cunha C, Taylor LK, Jorm LRJ. Hospital costs of older people in New South Wales in the last year of life. Med J Aust. 2007;187:383–386. doi: 10.5694/j.1326-5377.2007.tb01306.x. [DOI] [PubMed] [Google Scholar]
- 189.Tanuseputro P, Wodchis WP, Fowler R, et al. The health care cost of dying: a population-based retrospective cohort study of the last year of life in Ontario, Canada. PLoS One. 2009;10 doi: 10.1371/journal.pone.0121759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Payne G, Laporte A, Foot DK, Coyte PC. Temporal trends in the relative cost of dying: evidence from Canada. Health Policy. 2009;90:270–276. doi: 10.1016/j.healthpol.2008.09.017. [DOI] [PubMed] [Google Scholar]
- 191.Aragon MJ, Chalkley M, Rice NJ. Medical spending and hospital inpatient care in England: an analysis over time. Fisc Stud. 2016;37:405–432. [Google Scholar]
- 192.Häkkinen U, Martikainen P, Noro A, Nihtilä E, Peltola M. Aging, health expenditure, proximity to death, and income in Finland. Health Econ Policy Law. 2008;3:165–195. doi: 10.1017/S174413310800443X. [DOI] [PubMed] [Google Scholar]
- 193.Polder JJ, Barendregt JJ, van Oers H. Health care costs in the last year of life--the Dutch experience. Soc Sci Med. 2006;63:1720–1731. doi: 10.1016/j.socscimed.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 194.Stooker T, van Acht JW, van Barneveld EM, et al. Costs in the last year of life in The Netherlands. Inquiry. 2001;38:73–80. doi: 10.5034/inquiryjrnl_38.1.73. [DOI] [PubMed] [Google Scholar]
- 195.Melberg HO, Godager G, Gregersen FA. Hospital expenses towards the end of life. Tidsskr Nor Laegeforen. 2013;133:841–844. doi: 10.4045/tidsskr.12.0802. [DOI] [PubMed] [Google Scholar]
- 196.Ranchod S, Bloch J, Abraham M. An actuarial perspective on healthcare expenditure in the last year of life. South African Actuarial Journal. 2015;15:31–49. [Google Scholar]
- 197.Riley GF, Lubitz JD. Long-term trends in Medicare payments in the last year of life. Health Serv Res. 2010;45:565–576. doi: 10.1111/j.1475-6773.2010.01082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Hogan C, Lunney J, Gabel J, Lynn J. Medicare beneficiaries' costs of care in the last year of life. Health Aff (Millwood) 2001;20:188–195. doi: 10.1377/hlthaff.20.4.188. [DOI] [PubMed] [Google Scholar]
- 199.Hoover DR, Crystal S, Kumar R, Sambamoorthi U, Cantor JC. Medical expenditures during the last year of life: findings from the 1992-1996 Medicare current beneficiary survey. Health Serv Res. 2002;37:1625–1642. doi: 10.1111/1475-6773.01113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Calfo S, Smith J, Zezza M. Centers for Medicare and Medicaid Services, Office of the Actuary; 2015. Last year of life study.https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/ActuarialStudies/Downloads/Last_Year_of_Life.pdf [Google Scholar]
- 201.Lubitz JD, Riley GF. Trends in Medicare payments in the last year of life. N Engl J Med. 1993;328:1092–1096. doi: 10.1056/NEJM199304153281506. [DOI] [PubMed] [Google Scholar]
- 202.Emanuel EJ, Emanuel LL. The economics of dying. The illusion of cost savings at the end of life. N Engl J Med. 1994;330:540–544. doi: 10.1056/NEJM199402243300806. [DOI] [PubMed] [Google Scholar]
- 203.Becker G, Murphy K, Philipson T. The value of life near its end and terminal care. National Bureau of Economic Research. Working paper 13333. 2007. https://www.nber.org/system/files/working_papers/w13333/w13333.pdf
- 204.Chen CH, Kuo SC, Tang ST. Current status of accurate prognostic awareness in advanced/terminally ill cancer patients: systematic review and meta-regression analysis. Palliat Med. 2017;31:406–418. doi: 10.1177/0269216316663976. [DOI] [PubMed] [Google Scholar]
- 205.Weeks JC, Catalano PJ, Cronin A, et al. Patients' expectations about effects of chemotherapy for advanced cancer. N Engl J Med. 2012;367:1616–1625. doi: 10.1056/NEJMoa1204410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Greenwald AG. The totalitarian ego: fabrication and revision of personal history. Am Psychol. 1980;35:603. [Google Scholar]
- 207.Martindale DA. Confirmatory bias and confirmatory distortion. J Child Custody. 2005;2:31–48. [Google Scholar]
- 208.Eil D, Rao JM. The good news-bad news effect: asymmetric processing of objective information about ourself. Am Econ J Microecon. 2011;3:114–138. [Google Scholar]
- 209.Zeckhauser R, Sunstein CR. Harvard Environmental Economics Program; Cambridge, Mass: 2009. Dreadful possibilities, neglected probabilities; pp. 116–124. Discussion paper 2009-03. [Google Scholar]
- 210.Finkelstein EA, Baid D, Cheung YB, et al. Hope, bias and survival expectations of advanced cancer patients: A cross-sectional study. Psychooncology. 2021;30:780–788. doi: 10.1002/pon.5675. [DOI] [PubMed] [Google Scholar]
- 211.Glare P, Virik K, Jones M, et al. A systematic review of physicians' survival predictions in terminally ill cancer patients. BMJ. 2003;327:195–198. doi: 10.1136/bmj.327.7408.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Lyu H, Xu T, Brotman D, et al. Overtreatment in the United States. PLoS One. 2017;12 doi: 10.1371/journal.pone.0181970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Cardona-Morrell M, Kim J, Turner RM, Anstey M, Mitchell IA, Hillman K. Non-beneficial treatments in hospital at the end of life: a systematic review on extent of the problem. Int J Qual Health Care. 2016;28:456–469. doi: 10.1093/intqhc/mzw060. [DOI] [PubMed] [Google Scholar]
- 214.Cutler DM, Zeckhauser RJ. The anatomy of health insurance. Handbook of Health Economics. 2000;1:563–643. [Google Scholar]
- 215.Manning WG, Newhouse JP, Duan N, Keeler EB, Leibowitz A, Marquis MS. Health insurance and the demand for medical care: evidence from a randomized experiment. Am Econ Rev. 1987;77:251–277. [PubMed] [Google Scholar]
- 216.Angelis A, Lange A, Kanavos P. Using health technology assessment to assess the value of new medicines: results of a systematic review and expert consultation across eight European countries. Eur J Health Econ. 2018;19:123–152. doi: 10.1007/s10198-017-0871-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.National Institute for Health and Clinical Excellence Guide to the methods of technology appraisal. London, 2004. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/191504/NICE_guide_to_the_methods_of_technology_appraisal.pdf [PubMed]
- 218.National Institute for Health and Clinical Excellence Consultation paper. Value based assessment of health technologies. 2014. https://www.nice.org.uk/Media/Default/About/what-we-do/NICE-guidance/NICE-technology-appraisals/VBA-TA-Methods-Guide-for-Consultation.pdf
- 219.Shah KK, Tsuchiya A, Wailoo AJ. Valuing health at the end of life: a review of stated preference studies in the social sciences literature. Soc Sci Med. 2018;204:39–50. doi: 10.1016/j.socscimed.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 220.UN . United Nations; New York: 2015. Sustainable Development Goals.https://www.un.org/sustainabledevelopment/sustainable-development-goals/ [Google Scholar]
- 221.Yadav S, Heller IW, Schaefer N, et al. The health care cost of palliative care for cancer patients: a systematic review. Support Care Cancer. 2020;28:4561–4573. doi: 10.1007/s00520-020-05512-y. [DOI] [PubMed] [Google Scholar]
- 222.Morrison I. Healthcare costs and choices in the last years of life. Hospitals and Health Networks. 2015 https://mail.yahoo.com/d/folders/1/messages/AIzcgGdZ9X0NX0lB-ANu6AuQJ44 [Google Scholar]
- 223.Cave S. Biteback; London: 2013. Immortality: the quest to live forever and how it drives civilisation. [Google Scholar]
- 224.Alcor Life Extension Foundation Extend your life with cryonics. https://alcor.org/
- 225.Hauskeller M. My brain, my mind, and I: some philosophical assumptions of mind-uploading. Int J Machine Consciousness. 2012;4:187–200. [Google Scholar]
- 226.Digital Legacy Association Digital Legacy Association. https://digitallegacyassociation.org/
- 227.Springer Biogerontology. https://www.springer.com/journal/10522
- 228.Miller RA. Extending life: scientific prospects and political obstacles. Milbank Q. 2002;80:155–174. doi: 10.1111/1468-0009.00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Fries JF. Aging, natural death, and the compression of morbidity. N Engl J Med. 1980;303:130–135. doi: 10.1056/NEJM198007173030304. [DOI] [PubMed] [Google Scholar]
- 230.Cognitive Functioning and Aging Study Cognitive Functioning and Aging Study. http://www.cfas.ac.uk/
- 231.Jagger C, Matthews FE, Wohland, et al. A comparison of health expectancies over two decades in England: results of the Cognitive Function and Ageing Study I and II. Lancet. 2016;387:779–785. doi: 10.1016/S0140-6736(15)00947-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Crimmins EM, Beltrán-Sánchez H. Mortality and morbidity trends: is there compression of morbidity? J Gerontol B Psychol Sci Soc Sci. 2010;66:75–86. doi: 10.1093/geronb/gbq088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Abarshi E, Echteld MA, Van den Block L, Donker G, Deliens L, Onwuteaka-Philipsen B. The oldest old and GP end-of-life care in the Dutch community: a nationwide study. Age Ageing. 2010;39:716–722. doi: 10.1093/ageing/afq097. [DOI] [PubMed] [Google Scholar]
- 234.Office for National Statistics Leading causes of death, UK: 2001 to 2018. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/articles/leadingcausesofdeathuk/latest
- 235.Fleming J, Farquhar M, Brayne C, Barclay S, et al. Death and the oldest old: attitudes and preferences for end-of-life care - qualitative research within a population-based cohort study. PLoS One. 2016;11 doi: 10.1371/journal.pone.0150686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Russell S, Taylor R. Are care homes the hospices of the future? British Geriatrics Society. 2019 https://www.bgs.org.uk/blog/are-care-homes-the-hospices-of-the-future [Google Scholar]
- 237.Kinley J, Hockley J, Stone L, et al. The provision of care for residents dying in U.K. nursing care homes. Age Ageing. 2014;43:375–379. doi: 10.1093/ageing/aft158. [DOI] [PubMed] [Google Scholar]
- 238.Conrad P. Johns Hopkins University Press; Baltimore: 2007. The medicalization of society: on the transformation of human conditions into treatable disorders. [Google Scholar]
- 239.Kennedy C, Brooks-Young P, Brunton Gray C, et al. Diagnosing dying: an integrative literature review. BMJ Support Palliat Care. 2014;4:263–270. doi: 10.1136/bmjspcare-2013-000621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Glare PA, Sinclair CT. Palliative medicine review: prognostication. J Palliat Med. 2008;11:84–103. doi: 10.1089/jpm.2008.9992. [DOI] [PubMed] [Google Scholar]
- 241.Chu C, White N, Stone P. Prognostication in palliative care. Clin Med (Lond) 2019;19:306–310. doi: 10.7861/clinmedicine.19-4-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Murray SA, Kendall M, Mitchell G, Moine S, Amblă s-Novellas J, Boyd K. Palliative care from diagnosis to death. BMJ. 2017;356:j878. doi: 10.1136/bmj.j878. [DOI] [PubMed] [Google Scholar]
- 243.Royal College of Physicians . Royal College of Physicians; London: 2018. Talking about dying: how to begin honest conversations about what lies ahead. [Google Scholar]
- 244.Mercadante S, Gregoretti C, Cortegiani A. Palliative care in intensive care units: why, where, what, who, when, how. BMC Anesthesiol. 2018;18:106. doi: 10.1186/s12871-018-0574-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Intensive Care National Audit and Research Centre Intensive Care National Audit and Research Centre. https://www.icnarc.org/
- 246.Ferrando-Vivas P, Jones A, Rowan KM, Harrison DA. Development and validation of the new ICNARC model for prediction of acute hospital mortality in adult critical care. J Crit Care. 2017;38:335–339. doi: 10.1016/j.jcrc.2016.11.031. [DOI] [PubMed] [Google Scholar]
- 247.Murthy S, Leligdowicz A, Adhikari NK. Intensive care unit capacity in low-income countries: a systematic review. PLoS One. 2015;10 doi: 10.1371/journal.pone.0116949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Adhikari NK, Fowler RA, Bhagwanjee S, Rubenfeld GD. Critical care and the global burden of critical illness in adults. Lancet. 2010;376:1339–1346. doi: 10.1016/S0140-6736(10)60446-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Engdahl Mtango S, Lugazia E, Baker U, Johansson Y, Baker T. Referral and admission to intensive care: a qualitative study of doctors' practices in a Tanzanian university hospital. PLoS One. 2019;14 doi: 10.1371/journal.pone.0224355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Myburgh J, Abillama F, Chiumello D, et al. the Council of the World Federation of Societies of Intensive and Critical Care Medicine End-of-life care in the intensive care unit: report from the Task Force of World Federation of Societies of Intensive and Critical Care Medicine. J Crit Care. 2016;34:125–130. doi: 10.1016/j.jcrc.2016.04.017. [DOI] [PubMed] [Google Scholar]
- 251.Kon AA, Shepard EK, Sederstrom NO, et al. Defining futile and potentially inappropriate interventions: a policy statement from the Society of Critical Care Medicine Ethics Committee. Crit Care Med. 2016;44:1769–1774. doi: 10.1097/CCM.0000000000001965. [DOI] [PubMed] [Google Scholar]
- 252.Johnston SD, Tham TC, Mason M. Death after PEG: results of the National Confidential Enquiry into patient outcome and death. Gastrointest Endosc. 2008;68:223–227. doi: 10.1016/j.gie.2007.10.019. [DOI] [PubMed] [Google Scholar]
- 253.Cruz VM, Camalionte L, Caruso P. Factors associated with futile end-of-life intensive care in a cancer hospital. Am J Hosp Palliat Care. 2015;32:329–334. doi: 10.1177/1049909113518269. [DOI] [PubMed] [Google Scholar]
- 254.Braganza MA, Glossop AJ, Vandana AV. Treatment withdrawal and end-of-life care in the intensive care unit. BJA. 2017;17:396–400. [Google Scholar]
- 255.Sprung CL, Cohen SL, Sjokvist P, et al. the Ethicus Study Group End-of-life practices in European intensive care units: the Ethicus Study. JAMA. 2003;290:790–797. doi: 10.1001/jama.290.6.790. [DOI] [PubMed] [Google Scholar]
- 256.Mani RK. Limitation of life support in the ICU: ethical issues relating to end of life care. Indian J Crit Care Med. 2003;7:112. [Google Scholar]
- 257.Kapadia F, Singh M, Divatia J, et al. Limitation and withdrawal of intensive therapy at the end of life: practices in intensive care units in Mumbai, India. Crit Care Med. 2005;33:1272–1275. doi: 10.1097/01.ccm.0000165557.02879.29. [DOI] [PubMed] [Google Scholar]
- 258.Selvaraj S, Farooqui HH, Karan A. Quantifying the financial burden of households' out-of-pocket payments on medicines in India: a repeated cross-sectional analysis of National Sample Survey data, 1994–2014. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2017-018020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Divatia JV. End-of-life care in the intensive care unit: better late than never? Indian J Crit Care Med. 2020;24:375–377. doi: 10.5005/jp-journals-10071-23496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Wilkinson D, Butcherine E, Savulescu J. Withdrawal aversion and the equivalance test. Am J Bioeth. 2019;19:21–28. doi: 10.1080/15265161.2019.1574465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Kitzinger J, Kitzinger C. Why futile and unwanted treatment continues for some PVS patients (and what to do about it). Case study, context and policy recommendations. Int J Mental Health Capacity Law. 2017;129:84–149. [Google Scholar]
- 262.Barilan YM. The new Israeli law on the care of the terminally ill: conceptual innovations waiting for implementation. Perspect Biol Med. 2007;50:557–571. doi: 10.1353/pbm.2007.0042. [DOI] [PubMed] [Google Scholar]
- 263.Yaguchi A, Truog RD, Curtis JR, et al. International differences in end-of-life attitudes in the intensive care unit: results of a survey. Arch Intern Med. 2005;165:1970–1975. doi: 10.1001/archinte.165.17.1970. [DOI] [PubMed] [Google Scholar]
- 264.Phua J, Joynt GM, Nishimura M, et al. the ACME Study Investigators and the Asian Critical Care Clinical Trials Group Withholding and withdrawal of life-sustaining treatments in intensive care units in Asia. JAMA Intern Med. 2015;175:363–371. doi: 10.1001/jamainternmed.2014.7386. [DOI] [PubMed] [Google Scholar]
- 265.Hinton JM. The physical and mental distress of the dying. Q J Med. 1963;32:1–21. [PubMed] [Google Scholar]
- 266.Glaser BG, Strauss AL. Aldine Transaction; New Jersey: 1965. Awareness of dying. [Google Scholar]
- 267.Saunders C. A personal therapeutic journey. BMJ. 1996;313:1599–1601. doi: 10.1136/bmj.313.7072.1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Kavalieratos D, Corbelli J, Zhang D, et al. Association between palliative care and patient and caregiver outcomes: a systematic review and meta-analysis. JAMA. 2016;316:2104–2114. doi: 10.1001/jama.2016.16840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Smith S, Brick A, O'Hara S, Normand C. Evidence on the cost and cost-effectiveness of palliative care: a literature review. Palliat Med. 2014;28:130–150. doi: 10.1177/0269216313493466. [DOI] [PubMed] [Google Scholar]
- 270.WHO Definition of palliative care. https://www.who.int/cancer/palliative/definition/en/
- 271.Ryan S, Wong J, Chow R, Zimmermann C. Evolving definitions of palliative care: upstream migration or confusion? Curr Treat Options Oncol. 2020;21:20. doi: 10.1007/s11864-020-0716-4. [DOI] [PubMed] [Google Scholar]
- 272.WHO . World Health Organization; Geneva: 2014. WHA.19. Strengthening of palliative care as a component of comprehensive care throughout the life course. [DOI] [PubMed] [Google Scholar]
- 273.WHO . World Health Organization; Astana: 2018. Declaration on primary health care. [Google Scholar]
- 274.Radbruch L, Payne S, de Lima L, Lohmann D. The Lisbon challenge: acknowledging palliative care as a human right. J Palliat Med. 2013;16:301–304. doi: 10.1089/jpm.2012.0394. [DOI] [PubMed] [Google Scholar]
- 275.Neuberger J, Aaronovitch D, Bonser T, et al. Department of Health; London: 2013. More care, less pathway: a review of the Liverpool Care Pathway. [Google Scholar]
- 276.Gambles M, Stirzaker S, Jack BA, Ellershaw JE. The Liverpool Care Pathway in hospices: an exploratory study of doctor and nurse perceptions. Int J Palliat Nurs. 2006;12:414–421. doi: 10.12968/ijpn.2006.12.9.21869. [DOI] [PubMed] [Google Scholar]
- 277.Veerbeek L, van Zuylen L, Swart SJ, et al. The effect of the Liverpool Care Pathway for the dying: a multi-centre study. Palliat Med. 2008;22:145–151. doi: 10.1177/0269216307087164. [DOI] [PubMed] [Google Scholar]
- 278.van der Heide A, Veerbeek L, Swart S, van der Rijt C, van der Maas PJ, van Zuylen L. End-of-life decision making for cancer patients in different clinical settings and the impact of the LCP. J Pain Symptom Manage. 2010;39:33–43. doi: 10.1016/j.jpainsymman.2009.05.018. [DOI] [PubMed] [Google Scholar]
- 279.Mullick A, Beynon T, Colvin M, et al. Liverpool Care Pathway carers survey. Palliat Med. 2009;23:571–572. doi: 10.1177/0269216309106459. [DOI] [PubMed] [Google Scholar]
- 280.Costantini M, Romoli V, Leo SD, et al. Liverpool Care Pathway for patients with cancer in hospital: a cluster randomised trial. Lancet. 2014;383:226–237. doi: 10.1016/S0140-6736(13)61725-0. [DOI] [PubMed] [Google Scholar]
- 281.Leadership Alliance of the Care of Dying People one chance to get it right: improving people's experience of care in the last few days and hours of life. Publications Gateway Reference 01509. 2014. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/323188/One_chance_to_get_it_right.pdf
- 282.National Institute for Health and Care Excellence . National Institute for Health and Care Excellence; London: 2015. Care of dying adults in the last days of life. NICE Guideline.https://www.nice.org.uk/guidance/ng31 [PubMed] [Google Scholar]
- 283.Badger F, Plumridge G, Hewison A, Shaw KL, Thomas K, Clifford C. An evaluation of the impact of the Gold Standards Framework on collaboration in end-of-life care in nursing homes. A qualitative and quantitative evaluation. Int J Nurs Stud. 2012;49:586–595. doi: 10.1016/j.ijnurstu.2011.10.021. [DOI] [PubMed] [Google Scholar]
- 284.Bristowe K, Carey I, Hopper A, et al. Patient and carer experiences of clinical uncertainty and deterioration, in the face of limited reversibility: a comparative observational study of the AMBER care bundle. Palliat Med. 2015;29:797–807. doi: 10.1177/0269216315578990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.UK Clinical Research Collaboration . London Medical Research Council; 2015. Igniting Our potential.http://hrcsonline.net/wpcontent/uploads/2017/09/UK_Health_Research_Analysis_Report_2014_WEB.pdf [Google Scholar]
- 286.Sleeman KE, Gomes B, Higginson IJ. Research into end-of-life cancer care—investment is needed. Lancet. 2012;379:519. doi: 10.1016/S0140-6736(12)60230-X. [DOI] [PubMed] [Google Scholar]
- 287.Pickett J, Brayne C. The scale and profile of global dementia research funding. Lancet. 2019;394:1888–1889. doi: 10.1016/S0140-6736(19)32599-1. [DOI] [PubMed] [Google Scholar]
- 288.Pastrana T, Vallath N, Mastrojohn J, et al. Disparities in the contribution of low- and middle-income countries to palliative care research. J Pain Symptom Manage. 2010;39:54–68. doi: 10.1016/j.jpainsymman.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 289.Sleeman KE, de Brito M, Etkind S, et al. The escalating global burden of serious health-related suffering: projections to 2060 by world regions, age groups, and health conditions. Lancet Glob Health. 2019;7:e883–e892. doi: 10.1016/S2214-109X(19)30172-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Evans CJ, Ison L, Ellis-Smith C, et al. Service delivery models to maximize quality of life for older people at the end of life: a rapid review. Milbank Q. 2019;97:113–175. doi: 10.1111/1468-0009.12373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Hasson F, Nicholson E, Muldrew D, et al. International palliative care research priorities: a systematic review. BMC Palliat Care. 2020;19:16. doi: 10.1186/s12904-020-0520-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Sands MB, O'Connell DL, Piza M, Ingham JM. In: Oxford Textbook of Palliative Medicine. 5th edn. Cherny N, Fallon M, Kaasa S, Portenoy R, Currow D, editors. Oxford University Press; Oxford: 2015. The epidemiology of death and symptoms: planning for population-based palliative care; pp. 1–57. [Google Scholar]
- 293.Higginson IJ, Evans CJ, Grande G, et al. Evaluating complex interventions in end of life care: the MORECare statement on good practice generated by a synthesis of transparent expert consultations and systematic reviews. BMC Med. 2013;11:111. doi: 10.1186/1741-7015-11-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Carrasco JM, Lynch TJ, Garralda E, et al. Palliative care medical education in European universities: a descriptive study and numerical scoring system proposal for assessing educational development. J Pain Symptom Manage. 2015;50:516. doi: 10.1016/j.jpainsymman.2015.04.019. 23.e2. [DOI] [PubMed] [Google Scholar]
- 295.Harding R, Powell RA, Downing J, et al. Generating an African palliative care evidence base: the context, need, challenges, and strategies. J Pain Symptom Manage. 2008;36:304–309. doi: 10.1016/j.jpainsymman.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 296.Kahane A. Berrett-Koehler Publishers; 2012. Transformative scenario planning: working together to change the future. [Google Scholar]
- 297.Ling T. Which way to a healthy future? Reflections on the Madingley Scenarios. Foresight. 1999;1:17–34. [Google Scholar]
- 298.Rhoods S, Babor A. The future of global research: A case study on the use of scenario planning in the publishing industry. Learn Publ. 2018;31:254–260. [Google Scholar]
- 299.Abercrombie R, Harries E, Wharton R. New Philanthropy Capital; London: 2015. Systems change. a guide to what it is and how to do it.https://www.thinknpc.org/resource-hub/systems-change-a-guide-to-what-it-is-and-how-to-do-it/ [Google Scholar]
- 300.Meadows DH, Meadows DL, Randers J, Behrens WW., 3rd . Universe Books; New York: 1972. The limits to growth; a report for the club of Rome's project on the predicament of mankind. [Google Scholar]
- 301.Meadows DH. Sustainability Institute; Hartland: 1999. Leverage points: places to intervene in a system. [Google Scholar]
- 302.Project on Death in America . Open Society; New York: 2004. Transforming the culture of dying: the project on death in America 1994–2003. [Google Scholar]
- 303.Clark D. The project on death in America: twenty years on. 2014. http://endoflifestudies.academicblogs.co.uk/the-project-on-death-in-america-twenty-years-on/ published online Sept 11.
- 304.New JP, Leather D, Bakerly ND, McCrae J, Gibson JM. Putting patients in control of data from electronic health records. BMJ. 2018;360 doi: 10.1136/bmj.j5554. [DOI] [PubMed] [Google Scholar]
- 305.Clark AW. A Reformation for our times. Free up the canon. BMJ. 2009;338 doi: 10.1136/bmj.b1375. [DOI] [PubMed] [Google Scholar]
- 306.Rajagopal MR, Kumar S. A model for delivery of palliative care in India—the Calicut experiment. J Palliat Care. 1999;15:44–49. [PubMed] [Google Scholar]
- 307.Sallnow L, Chenganakkattil S. The role of religious, social and political groups in palliative care in Northern Kerala. Indian J Palliat Care. 2005;11:10. [Google Scholar]
- 309.Paleri AK. Showing the way forward: pain and palliative care policy of the government of Kerala. Indian J Palliat Care. 2008;14:51. [Google Scholar]
- 310.Jain V. Palliative care in India: trials, tribulations, and future prospects. J Mahatma Gandhi Inst Med Sci. 2018;23:55–58. [Google Scholar]
- 311.Vijay D, Zaman S, Clark D. Translation of a community palliative care intervention: Experience from West Bengal, India. Wellcome Open Research. 2018;3 doi: 10.12688/wellcomeopenres.14599.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Attridge C, Richardson H. Compassionate neighbours–an innovative model building caring communities. BMJ Support Palliat Care. 2018;8:362. [Google Scholar]
- 313.Sallnow ES. University of Edinburgh; 2018. Collective social capital: a study of new public health and end-of-life care.https://era.ed.ac.uk/handle/1842/33037 PhD Thesis. [Google Scholar]
Uncited References
- 308.Kumar S. Community participation in palliative care: Reflections from the ground. Prog Palliat Care. 2020;28:83–88. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.