Abstract
Purpose of Review
This review of the literature aims to explore the impact of the COVID-19 pandemic and the lockdown on teenagers’ mental health. We distinguish two groups: adolescents who had already been diagnosed with a mental disorder and the general population of adolescents.
Recent Findings
An increase in the number of mental health-related difficulties in adolescents has already been reported in previous health crises. Accordingly, the perceived well-being of teenagers declined during the COVID-19 pandemic. Adolescents with mental disorders were significantly more affected by the lockdown than those in the general population.
Summary
The effect of the COVID-19 crisis on the mental health of adolescents has been heterogeneous. The first pandemic wave was essentially associated with an increase of internalizing symptoms in adolescents, particularly anxiety, depression and eating disorders. The impact on externalizing symptoms was less clear, and seem to concern mostly adolescents with pre-existing behavioral disorders. During the second and later waves of the pandemic, an upsurge of suicidal ideation and attempts among adolescents have been reported in many countries.
Keywords: Pandemic, Mental disorder, Anxiety, Depression, Behavioral disorder, Suicide
Introduction
The coronavirus disease 2019 (COVID-19) pandemic began in China in December and soon affected the whole world. The coronavirus 2 version of Severe Acute Respiratory Syndrome (SARS-CoV-2) can cause respiratory symptoms, fever, coughing and, in the worst cases, pneumonia, kidney failure and even death [1]. In October 2021, when the COVID-19 pandemic was still very active in some countries, it was responsible for over 4 800 000 deaths [1]. In order to curb its propagation, exceptional health precautions have been set up in most countries worldwide [2].
This health crisis has led to a complete upheaval in the organization of society: lockdown, schools being shut down and family relations being reorganized. The COVID-19 pandemic and the lockdown have also had a strong impact on world economy, with a severe loss of jobs [3]. This reorganization has directly affected the adolescent population as teenagers got stuck at home with their families, under the unusual conditions of home schooling.
Continuity of home schooling was a major challenge for adolescents and their families during the lockdown period and may have contributed to the reinforcement of preexisting inequalities among those who are most in need of help. For instance, in France 2% of homes with youngsters aged under 17 are not equipped with internet and 49% of families have at least one schoolchild who has to work in a shared room [4]. Educational issues during the pandemic were sometimes a source of stress for the youngsters [5]. Besides, school and extracurricular activities are places where socialization is privileged and peer group attendance plays an essential role in their developmental trajectory, more so than in any other stage in life [6].
Social isolation and feelings of loneliness can lead to the development of anxiety and depression symptoms among children and adolescents [7]. Beyond social habits, this population is also sensitive to changes in the rhythm of their daily life [8]. The lockdown may have sometimes had a deleterious impact on adolescents’ health. Some studies in Europe, South America and Asia have shown significant changes in eating habits [9] and a decrease in physical activity among adolescents compared to the pre-pandemic period [10].
Whereas home confinement for some was the occasion to improve family relationships, it may have meant an increase in domestic conflicts for others [4, 11]. Periods of economic crisis are particularly well-known for being associated with an increase in domestic violence [12]. For example, from 2006 to 2014 in Greece, the lowering of family revenues was associated with an increase in conflicts and violence within families and an increase in pressure at school among adolescents as well. An increase in cannabis use was also found [13].
Thus, the COVID-19 pandemic and its consequences on the adolescents’ lives may have been mediated by stress and trauma factors. Experiences of previous health crises have shown that this type of event can promote the onset of anxiety and post-traumatic symptoms in children and, more generally, in families [14]. Nevertheless, that particular study referred to interviews with parents of children who had experienced epidemic waves (mostly H1N1) but did not distinguish the effects specifically according to age.
The COVID-19 health crisis has already been associated with a significant decrease in the perceived well-being of adolescents [15]. Indeed, the current context of the pandemic and the experience of the lockdown seems to have had a negative impact on their emotions and behaviors [16, 17] and, more generally, their mental health [18•]. They represent a population which is vulnerable to stress factors [19], particularly, adolescents with mental disorders whose access to care may have been disturbed by health precautions [18•] and for whom the sensitivity to the environment may be increased [19–21]. In Canada, adolescents with mental health-related difficulties were significantly more affected by the lockdown in terms of wellbeing, compared with adolescents from the general population [18•].
All these findings incited us to make a more detailed investigation into the impact of the COVID-19 pandemic on mental health in adolescents and to explore the risk factors associated.
Methods
We reviewed all articles dealing with the mental health of adolescents during the COVID-19 crisis. We looked for 2020 and 2021 publications in the MEDLINE database by combining the MeSH terms “Adolescent” and “coronavirus” to which we then added the terms “mental health” or “suicide” or “aggression” or “anxiety” or “mood disorders” or “post-traumatic stress disorders” or “eating disorders” or “behavioral disorders” or “lockdown.” A total of 1017 publications were screened. Our selection criteria were that the articles had to be about or include adolescents and deal with the impact on their mental health. The initial screening of articles was made by reading titles and, if necessary, abstracts. We retained 46 articles for our literature review. Some articles were extracted from the references. The publications were written in English and French and concerned European, Asian and American populations. Most of them covered descriptive studies but also authors’ reflections and guidance for families and mental health professionals. Other literature reviews were also consulted. Studies prior to the COVID-19 pandemic, as well as data on the adult and student populations could be used if they provided relevant items for our reflection.
We describe our results according to the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) [22], with a specific focus on disorders classified as “Behavioral and emotional disorders with onset usually occurring in childhood and adolescence” (codes F90-F98). We considered emotional disorders as internalized disorders because they are related to negative affectivity. Behavioral disorders are characterized as externalized disorders because they refer to behavioral expressions. Since suicide attempts are not referenced as a mental disorder in ICD-10, we have chosen to include these behaviors in our externalized behavioral disorders section.
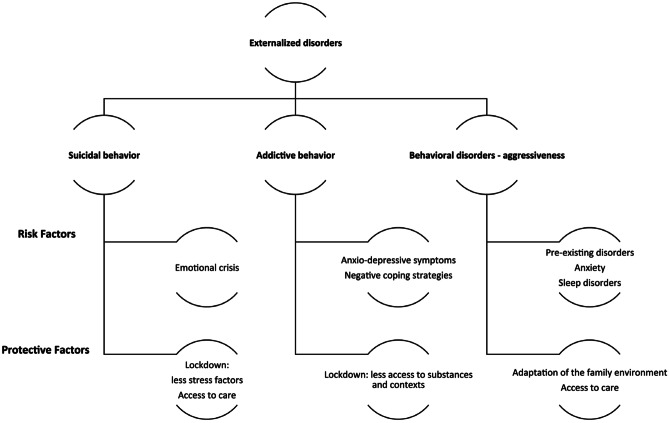
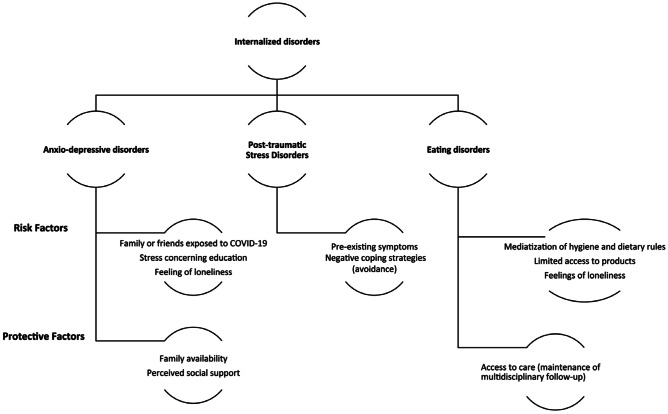
In our Results section, we will first address data related to externalized behavioral disorders (Fig. 1), particularly suicidal ideation and suicidal behavior [III.a], aggression, and addictive behavior [III.b]. Later, we will deal with internalized behavioral disorders (Fig. 2) such as anxiety, depression, post-traumatic stress disorder [III.c] and eating disorders [III.d].
Fig. 1.
Risk and protective factors of externalized disorders in adolescents during the COVID-19 pandemic
Fig. 2.
Risk and protective factors of internalized disorders in adolescents during the COVID-19 pandemic
Results
Suicidal Ideation and Behavior
Confinement measures, especially within families affected by unemployment, illness or domestic violence, could represent adverse childhood experiences and increase the risk of SB in adolescents [23]. Feelings of loneliness and depression are also risk factors for suicide among adolescents [24]. Lockdown measures could thus have increased SB in adolescents. However, reports during and after the confinement measures are divergent.
During lockdown in Japan, there was no significant increase in the suicide rate among youngsters aged under twenty when schools were shut down from March to May 2020. Regression analyses carried out using public sociodemographic data showed a slight decrease in the suicide rate compared with the same time of year in 2018 and 2019, but the study did not evaluate suicide ideation or attempts and covered only the first months of the COVID-19 pandemic [25]. Visits to the emergency department (ED) for psychiatric reasons decreased by 42% compared to 2019 during the lockdown period in Paris hospitals (France), especially in the 16-24-year-old age group [26]. A later retrospective study also in Paris found a 50% decrease in pediatric admissions related with SB during lockdown (Mars to May 2020), compared to adjacent time periods [27]. Although not restricted to adolescents, the average number of ED visits for suicide attempts or suicidal ideation in Madrid decreased among the general population in 2020 compared to the previous two years [28]. However, the decline in SB during the lockdown may be due to an actual reduction in suicidality but also to a decrease in the use of emergency services. A cross-sectional survey on more than 8000 persons aged 14 to 21 in Mexico informed a 21% rate of self-reported SB during the confinement [33].
More recently, a study comparing data from Mars 2020 to Mars 2021 with the prior year in Catalonia found a strong increase in the number of suicide attempts among adolescents starting after the end of confinement measures in Spain, in September 2020 [29]. The change was particularly prominent among girls, topping at a 195% increase. Epidemiological data in the USA show a similar tendency, ED visits for suicidal ideation or behavior decreased in the first months of the pandemic just after the declaration of national emergency and then increased during summer 2020. The rates continued to rise through the winter 2021 among adolescent girls (up by 50% compared to 2019) while staying constant in adolescent boys [30••].
In the early stages of the COVID-19 pandemic, confinement measures kept several anxiety factors at bay, such as a stressful school environment [31]. The health crisis encouraged also the use of online consulting and other alternative means for access to care. While this may have limited access to care for disadvantaged persons, it may have facilitated it for others, including suicidal adolescents [32]. Confinement was also the occasion to strengthen family relations and perceived support, reducing cognitive distortions, such as perceived burdensomeness and thwarted belongingness, which are linked with SB. Some consequences of the pandemic could thus have constituted protective factors against SB in adolescents [33]. The accumulation of risk factors during the pandemic, in particular the increase in internalized symptoms, seems to have favored situations of emotional crisis over the long term, thus leading to a subsequent increase in SB among adolescents (Fig. 1) [29, 33, 34].
Aggression and Addictive Behavior
In adolescents, negative emotions can result in greater irritability, aggressiveness and oppositional behaviors [21]. Adolescents with neurodevelopmental disorders such as attention deficit/hyperactivity disorder (ADHD) or autism spectrum disorders (ASD) were at a risk of exhibiting behavioral disorders during the lockdown period [21, 35, 36].
In France, an online survey of parents of children with ADHD found that about one third of them (34%) observed a worsening of their child's disorder during the lockdown. This aggravation was characterized by an increase in motor agitation, temper tantrums, oppositional and aggressive behavior. It appeared to be underpinned by anxiety, sleep disturbances (disruption of the circadian rhythm) and refuge in video games. A similar rate of parents (30%) reported a reduction in their child's inattention symptoms and agitation, related to a reduction in the constraints usually imposed by schooling [37]. In Italy, 35% out of 527 parents of children with ASD interviewed through a structured questionnaire reported an increase in the intensity of their child's behavior disorders and 41.5% noted an increase in the frequency of the crises during lockdown. The major predictive factor was the pre-existence of behavioral disorders. A large majority of families expressed difficulties to adapt themselves to the lockdown, particularly in the management of daily activities [38]. In both studies, behavioral changes are reported by parents based on qualitative data. Adolescents were not directly questioned, which does not allow a more specific exploration of their own experiences regarding anxiety or perceived stress in particular.
As far as the general population is concerned, a Chinese study conducted among students during the COVID-19 crisis nevertheless shows that the impact of the epidemic was not significantly related to aggressiveness which, on the contrary, appears to have been reduced in the worst hit geographical areas. Anxiety and altered quality of sleep were risk factors for aggression in this study [39].
The lockdown also encouraged the use of the internet and screens, essential for students to continue their education and maintain contact with peers during confinement [40]. However, an extensive use of screens, particularly during the night hours, has been associated with negative consequences such as disrupted sleep rhythms [41]. In India, over one hundred students from a cohort formed prior to the pandemic were questioned about their gaming behavior during the lockdown. Half of them reported an increase in gaming behavior during this period. Nevertheless, the authors did not observe any development or increase in problematic gaming behaviors. Students for whom gaming increased experienced more anxiety and stress about their schooling. They identified gaming as a strategy for coping with the perceived stress [5].
Conversely, in terms of substance use, a Canadian study showed a drop in heavy consumption among adolescents compared to the weeks prior to the lockdown. The authors make the link with the difficulty of access to certain substances in this context (electronic cigarette cannabis). Concerns about image among peer group, fear of the coronavirus and depressive affects were predictive factors of substance used in this study [42]. A second study also found a reduction in substance use among adolescents from clinical and community cohorts in Canada, compared to two months prior to confinement [18•]. Similarly, a large population-based longitudinal study in Iceland reported a significant reduction of alcohol, tobacco and e-cigarettes use in the 15-18 year-old group during the pandemic compared with previous years [43].
Two American studies show similar, but nuanced, results [44, 45]. In the first of them, 36.5% of young minors using the electronic cigarette before the crisis of COVID-19 had stopped smoking by May 2020 while 16.6% increased the amount of nicotine and 8.4% increased the THC consumption over the same period [44]. A longitudinal cohort study of 7842 adolescents interviewed between May and August 2020 found that substance use rates remained stable over time [45]. Anxiety-depressive symptoms and loss of family income in the context of the health crisis were associated with increased substance use [44, 45].
In summary, the impact of the COVID-19 crisis on aggressive and addictive behaviors depends on the population studied. The crisis, and particularly the confinement, seems to have favored the increase of externalized symptoms among adolescents with neurodevelopmental disorders and pre-existing behavioral problems [37, 38]. In the general adolescent population, there was no increase in aggressiveness or addictive behaviors [18•, 36, 42]. Confinement even seems to have played a protective role, probably mediated by a limited access to the substances [42, 45]. The relationship between the COVID-19 crisis and externalized behavioral disorders appears to be moderated by certain internalized symptoms such as anxiety, depression, worries about the pandemic or sleep disorders (Fig. 1) [18•, 36–38, 42, 44, 45].
Anxio-depressive Disorders and Post-traumatic Stress
The reduction in social contact due to the closing of schools and colleges could increase the risk of anxiety and depressive disorders in adolescents [16, 17]. Most studies on adolescents conducted in the course of this health crisis report high rates of anxiety-depressive symptoms [46, 47]. A large cross-sectional online survey carried out among Chinese adolescents aged twelve to eighteen estimates the prevalence rate of depression and anxiety symptoms at 43.7% and 37.4%, respectively, during the pandemic. Teenage girls seem to present a higher risk than boys of developing symptoms of anxiety and depression. Furthermore, this study brings forth a strong negative correlation between the difficulties related to mental health and the level of information and prevention concerning COVID-19 [46].
A longitudinal study conducted in Norway between February 2019 and June 2020 among adolescents aged 13–16 years shows a significant increase in anxiety-depressive symptoms, particularly among girls, since the beginning of the COVID-19 crisis. Living in a household with low socioeconomic level and a single parent were associated with these symptoms. The authors nevertheless encourage us to be cautious in interpreting these results, which could also be associated with the participants' age progression [48]. A second longitudinal study conducted in Iceland using three waves of school surveys (2016, 2018, 2020) among adolescents aged 15 to 18 show a significant increase in depressive symptoms, particularly among girls, between 2016 and October 2020 [43].
According to a general population survey conducted two weeks after the beginning of COVID-19 in China, 14.4% of adolescents and young adults reported symptoms of post-traumatic stress disorder (PTSD) [47]. Adolescents undergoing treatment for a major depressive episode in a cross-sectional study of Chinese adolescents were more likely to present PTSD symptoms one month after the onset of the COVID-19 crisis compared to control subjects [49]. Both studies highlight the importance of avoidance behaviors on mental disorders.
In summary, the COVID-19 crisis increased the risk of anxiety, depression and PTSD among adolescents. Socio-environmental vulnerability factors, worry about being affected by the disease and isolation due to health restrictions, pre-existing internalizing disorders and using negative coping strategies appear as key factors. Young girls were found to be the most affected. (Fig. 2) [50••].
Eating Disorders
Adolescents with eating disorders can be considered as a population at risk. Indeed, their problems may be accentuated by the "containment effect": psychological discomfort, related medical problems, emotional isolation, social and family difficulties [51]. In 2020, some studies have been published regarding adolescents but they focus mainly on the consequences of the lockdown and the way healthcare management was adapted [52–56]. Strict, inflexible dietary behaviors with a reduced range of foods may have been affected by the limitations in market supply and lead to family conflicts. Thus, the lockdown conditions could exacerbate negative affectivity and comorbid conditions in patients with eating disorders [56]. At the same time, state health responses to the spread of the SARS-CoV-2 epidemic have imposed coping challenges on medical institutions. The challenge has been to remotely monitor weight changes and physiological status, while offering psychological and emotional support [52–55]. The media coverage of dietary hygiene rules during lockdown may also play a role. The promotion of an ideal of thinness and the stigmatization of overweight people may have rigidified the control of self-image [57, 58].
A retrospective study at the Perth Children's Hospital in Australia found a 104% increase in the number of anorexic patients under the age of 16 admitted for somatic stabilization (severe undernutrition, risk of cardiovascular distress) in comparison with previous years [59]. Similar results were obtained in the USA showing a significant increase in the use of medical care for eating disorders after the implementation of restrictions due to the COVID-19 crisis among a population aged 8 to 26 years [60]. The explanatory hypothesis advanced by the authors is that health measures of social restriction have led to the loss of several protective factors and promoted comorbid symptoms/pathologies. In addition, delayed care because of the pandemic is probably associated with more ED visits and more severe clinical presentations.
Thus, it appears that the COVID-19 crisis, and particularly the confinement, was associated with an increased incidence of adolescent eating disorders, or at least an increase in the use of healthcare services for this reason. The impact of confinement on eating habits, the social isolation and the presence of comorbid internalized symptoms have been identified as risk factors in this population. The continuity of a multidisciplinary follow-up could nevertheless play a protective role (Fig. 2) [52–55].
Discussion
In this review, we explored the impact of the COVID-19 pandemic on adolescent mental health. We found that the health crisis was a risk factor for internalized disorders (anxiety, depression, PTSD symptoms and eating disorders) [47, 48, 60] and it was associated with an increase in SBs in the longer term [61]. Adolescents with pre-existing disorders were particularly vulnerable [50••].
Consequences on the Mental Health of Adolescents
Among the general adolescent population, the literature highlights the influence of the health crisis on the development of anxiety and depressive symptoms [46]. The environmental consequences related to the COVID-19 crisis also constituted a risk factor for adolescents with eating disorders [56]. The impact on externalized disorders appears to be more subtle [25, 39].
The data show that the presence of several vulnerability factors such as hyperkinetic disorders and sensitivity to changes in daily routines are risk factors for behavioral disorders in children and adolescents [37, 38, 62]. These results seem to be mediated by anxiety levels, sleep disorders, and the environmental and familiar context (reduced parental availability and negative emotions) [62]. While preliminary studies show an increase in the use of screens and video games during confinement [40, 40], excessive substance use among adolescents appears to have declined [18•, 42]. Indeed, certain stress factors have decreased at the beginning of the pandemic, such as bullying at school and academic and social pressure. In some families, parents were more available and also less exposed to anxiety-provoking factors. These conditions may have promoted a sense of support and resilience among adolescents [20, 37, 63, 64].
However, observations made at the beginning of the health crisis are reversed when taking into account a longer temporality. For instance, several studies published in 2021 show an increase in suicidal ideation and suicide attempts among adolescents [29, 30••, 61].
Advice for Families and Primary Prevention
Several articles and recommendations on prevention are available to help families and professionals.
Families are recommended to be attentive to healthy living, especially sleep [63, 65–67]. The management of screen time was also highlighted during the lockdown [68, 69].
The literature also emphasizes the need for coping strategies in times of health crisis, particularly for lockdown periods [65, 70]. Actively seeking strategies to handle crisis-related concerns and social distancing measures were encouraged. This could include maintaining social contact via available technology, learning about COVID-19 from credible sources of information or identifying effective emotional management strategies used in the past, for example [65]. These recommendations are relevant to the entire family, including children and parents. Indeed, past experience shows that active parental coping strategies are a protective factor against negative affect in their child in times of crisis [70]. For adolescents with pre-existing disorders who are particularly sensitive to changes in their environment and daily rituals, it is advisable to maintain a regular link with the care structure [71, 71].
Re-organizing Care for Mental Health
The health crisis has led to the reorganization of mental health services. First, during the lockdown period, telecommunications had to be promoted to ensure the care of patients [64, 72, 73]. An ongoing study protocol on a randomized trial is exploring the effects of brief on-line therapy on eleven to eighteen-year-old adolescents with anxiety disorders during the pandemic. The results of this study may contribute to supporting the interest of developing this type of care [74].
Secondly, hospital pediatric EDs have been particularly solicited for the management of adolescents. Indeed, the literature shows an increase in emergency room visits for eating disorders with severe somatic consequences, but also for suicidal ideation and suicide attempts among adolescents. This last increase is particularly observed during the most recent period of the pandemic, i.e., at a distance from the first wave and the first confinement [30••, 60, 61].
Thirdly, the pandemic has reduced the accessibility to healthcare in many cases. This concerns specifically adolescents with a precarious socio-familial environment (low socio-economic status, migrant family). Adolescents with pre-existing mental disorders or special needs were at a greater risk of developing negative emotions during the COVID-19 crisis.
Conclusion
Adolescents were affected by the reorganization of society due to the COVID-19 health crisis, and the lockdown in particular. The COVID-19 pandemic appears to have promoted the emergence of internalized symptoms among the general adolescent population and may have contributed to increase the occurrence and severity of these symptoms among those with pre-existing mental health conditions. The findings are more qualified for externalized disorders, in which adolescents with pre-existing behavioral disturbances are the most affected. Lockdown measures seem to provide also protective factors that lead to an initial decrease in SB and substance use problems. However, SBs have increased significantly among adolescents, particularly adolescent girls, in the later phases of the crisis. Wade et al. emphasize the interest of developing longitudinal studies to evaluate the effects of long-term confinement on the mental health of adolescents. The authors distinguish five common effects in psychopathology during development that may be explored: cumulative risks, sleeper (latent) effects, sensitizing effects, mechanistic effects and resilience [75].
The COVID-19 crisis has also given us the opportunity to develop other management methods. Based on this experience, it appears essential to pursue research about teleconsultation for adolescents, in order to validate these new practices scientifically. Mental healthcare services, after the challenge of adaptation imposed by the health measures in the early days of the pandemic, are now working to accommodate and care for a large number of vulnerable adolescents affected by the COVID-19 crisis.
Acknowledgements
We thank Theresa Sawyers for the English translation of the paper.
Compliance with Ethical Standards
Conflicts of Interests/Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Footnotes
This article is part of the Topical Collection on Mood Disorders
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.WHO Coronavirus Disease (COVID-19) Dashboard | WHO Coronavirus Disease (COVID-19) Dashboard [Internet]. [cité 22 sept 2020]. Disponible sur: https://covid19.who.int/.
- 2.Pandémie de Covid-19 : mesures barrières renforcées pendant le confinement et en phase de sortie de confinement. Bull Académie Natl Médecine. 1 July 2020;204(7):654‑5. [DOI] [PMC free article] [PubMed]
- 3.Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int J Surg. June 2020;78:185‑93. [DOI] [PMC free article] [PubMed]
- 4.Dubost, Pollak et Rey. Les inégalités sociales face à l’épidémie de Covid-19 - État des lieux et perspectives. Les dossiers de la DREES, 62. Disponible sur: https://drees.solidarites-sante.gouv.fr/sites/default/files/2020-10/DD62.pdf.
- 5.Balhara YPS, Kattula D, Singh S, Chukkali S, Bhargava R. Impact of lockdown following COVID-19 on the gaming behavior of college students. Indian J Public Health. juin. 2020;64(Supplement):S172–6. doi: 10.4103/ijph.IJPH_465_20. [DOI] [PubMed] [Google Scholar]
- 6.Orben A, Tomova L, Blakemore S-J. The effects of social deprivation on adolescent development and mental health. Lancet Child Adolesc Health. août. 2020;4(8):634–40. doi: 10.1016/S2352-4642(20)30186-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J Am Acad Child Adolesc Psychiatry. 3 juin 2020. [DOI] [PMC free article] [PubMed]
- 8.Imran N, Zeshan M, Pervaiz Z. Mental health considerations for children & adolescents in COVID-19 Pandemic. Pak J Med Sci. May 2020;36(COVID19-S4):S67–72. [DOI] [PMC free article] [PubMed]
- 9.Ruiz-Roso MB, de Carvalho Padilha P, Mantilla-Escalante DC, Ulloa N, Brun P, Acevedo-Correa D, et al. Covid-19 Confinement and Changes of Adolescent’s Dietary Trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients [Internet]. 17 juin 2020 [cité 3 nov 2020];12(6). Disponible sur: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7353171/. [DOI] [PMC free article] [PubMed]
- 10.Xiang M, Zhang Z, Kuwahara K. Impact of COVID-19 pandemic on children and adolescents’ lifestyle behavior larger than expected. Prog Cardiovasc Dis [Internet]. 30 avr 2020 [cité 22 sept 2020]; Disponible sur: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7190470/. [DOI] [PMC free article] [PubMed]
- 11.Craig S, Ames ME, Bondi BC, Pepler DJ. Rates of Adolescent Mental Health Problems, Substance Use, and Violence in the Home during COVID-19: Does Gender Matter? [Internet]. PsyArXiv; 2020 sept [cité 3 nov 2020]. Disponible sur: https://psyarxiv.com/kprd9/.
- 12.Schneider W, Waldfogel J, Brooks-Gunn J. The Great Recession and risk for child abuse and neglect. Child Youth Serv Rev. janv. 2017;72:71–81. doi: 10.1016/j.childyouth.2016.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kokkevi A, Stavrou M, Kanavou E, Fotiou A. The Repercussions of the Economic Recession in Greece on Adolescents and their Families. 30 sept 2014 [cité 3 nov 2020]; Disponible sur: https://www.oecd-ilibrary.org/content/paper/214f5736-en.
- 14.Sprang G, Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med Public Health Prep. févr 2013;7(1):105‑10. [DOI] [PubMed]
- 15.Pedersen W, Sletten MA. Life satisfaction among adolescents before and during the COVID-19 pandemic. Tidsskr Den Nor Laegeforening Tidsskr Prakt Med Ny Raekke. 30 2020;140(10). [DOI] [PubMed]
- 16.Buzzi C, Tucci M, Ciprandi R, Brambilla I, Caimmi S, Ciprandi G, et al. The psycho-social effects of COVID-19 on Italian adolescents’ attitudes and behaviors. Ital J Pediatr. 24 mai 2020;46(1):69. [DOI] [PMC free article] [PubMed]
- 17.Craig S, Ames M, Bondi BC, Pepler DJ. Canadian Adolescents’ Mental Health and Substance Use during the COVID-19 Pandemic: Associations with COVID-19 Stressors [Internet]. PsyArXiv; 2020. 10.31234/osf.io/kprd9
- 18.Hawke LD, Barbic SP, Voineskos A, Szatmari P, Cleverley K, Hayes E, et al. Impacts of COVID-19 on Youth Mental Health, Substance Use, and Well-being: A Rapid Survey of Clinical and Community Samples: Répercussions de la COVID-19 sur la santé mentale, l’utilisation de substances et le bien-être des adolescents : un sondage rapide d’échantillons cliniques et communautaires. Can J Psychiatry Rev Can Psychiatr. 2020;65(10):701–9. doi: 10.1177/0706743720940562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–60. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Ment Health. 2020;14:20. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cohen D. Appreciating COVID-19 as a child and adolescent psychiatrist on the move. L’Encephale. juin. 2020;46(3S):S99–106. doi: 10.1016/j.encep.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.CIM-10/ICD-10. Classification internationale des maladies. Dixième révision. Chapitre V(F), Troubles mentaux et troubles du comportement : descriptions cliniques et directives pour le diagnostic / coordination générale de la traduction française: C. B. Pull [Internet]. [cité 26 Oct 2021]. Disponible sur: https://apps.who.int/iris/handle/10665/43316.
- 23.Carballo JJ, Llorente C, Kehrmann L, Flamarique I, Zuddas A, Purper-Ouakil D, et al. Psychosocial risk factors for suicidality in children and adolescents. Eur Child Adolesc Psychiatry. juin. 2020;29(6):759–76. doi: 10.1007/s00787-018-01270-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gijzen MWM, Rasing SPA, Creemers DHM, Smit F, Engels RCME, De Beurs D. Suicide ideation as a symptom of adolescent depression. a network analysis. J Affect Disord. 12 sept 2020;278:68–77. [DOI] [PubMed]
- 25.Isumi A, Doi S, Yamaoka Y, Takahashi K, Fujiwara T. Do suicide rates in children and adolescents change during school closure in Japan? The acute effect of the first wave of COVID-19 pandemic on child and adolescent mental health. Child Abuse Negl. 23 août 2020;104680. [DOI] [PMC free article] [PubMed]
- 26.Pignon B, Gourevitch R, Tebeka S, Dubertret C, Cardot H, Dauriac-Le Masson V, et al. Dramatic reduction of psychiatric emergency consultations during lockdown linked to COVID-19 in Paris and suburbs. Psychiatry Clin Neurosci. 1 juill 2020. [DOI] [PMC free article] [PubMed]
- 27.Mourouvaye M, Bottemanne H, Bonny G, Fourcade L, Angoulvant F, Cohen JF, et al. Association between suicide behaviours in children and adolescents and the COVID-19 lockdown in Paris, France: a retrospective observational study. Arch Dis Child. sept. 2021;106(9):918–9. doi: 10.1136/archdischild-2020-320628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hernández-Calle D, Martínez-Alés G, Mediavilla R, Aguirre P, Rodríguez-Vega B, Bravo-Ortiz MF. Trends in Psychiatric Emergency Department Visits Due to Suicidal Ideation and Suicide Attempts During the COVID-19 Pandemic in Madrid, Spain. J Clin Psychiatry. 01 2020;81(5). [DOI] [PubMed]
- 29.Gracia R, Pamias M, Mortier P, Alonso J, Pérez V, Palao D. Is the COVID-19 pandemic a risk factor for suicide attempts in adolescent girls? J Affect Disord. 1 sept 2021;292:139–41. [DOI] [PMC free article] [PubMed]
- 30.•• Yard E, Radhakrishnan L, Ballesteros MF, Sheppard M, Gates A, Stein Z, et al. Emergency Department Visits for Suspected Suicide Attempts Among Persons Aged 12-25 Years Before and During the COVID-19 Pandemic - United States, January 2019-May 2021. MMWR Morb Mortal Wkly Rep. 18 juin 2021;70(24):888–94. This paper provides epidemiological data on the rates of ED’s visits among young people for suspected suicide attempts (including self-harm) in the US from 2019 to 2021. The results show at first a decrease of suicidal behavior in adolescents aged 12-17 years old during spring 2020 (first phase of the COVID-19 pandemic) and then a progressive increase of up to 50% among adolescent girls during the winter 2021, compared to the same periods in 2019.
- 31.Lueck C, Kearl L, Lam CN, Claudius I. Do emergency pediatric psychiatric visits for danger to self or others correspond to times of school attendance? Am J Emerg Med. 1 mai 2015;33(5):682–4. [DOI] [PubMed]
- 32.Fairchild RM, Ferng-Kuo S-F, Rahmouni H, Hardesty D. Telehealth Increases Access to Care for Children Dealing with Suicidality, Depression, and Anxiety in Rural Emergency Departments. Telemedicine and e-Health. 1 Nov 2020;26(11):1353‑62. [DOI] [PubMed]
- 33.Kazi F, Mushtaq A. Adolescents navigating the COVID-19 pandemic. Lancet Child Adolesc Health. 2021;5(10):692–3. doi: 10.1016/S2352-4642(21)00279-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hermosillo-de-la-Torre AE, Arteaga-de-Luna SM, Acevedo-Rojas DL, Juárez-Loya A, Jiménez-Tapia JA, Pedroza-Cabrera FJ, et al. Psychosocial Correlates of Suicidal Behavior among Adolescents under Confinement Due to the COVID-19 Pandemic in Aguascalientes, Mexico: A Cross-Sectional Population Survey. Int J Environ Res Public Health. 7 mai 2021;18(9):4977. [DOI] [PMC free article] [PubMed]
- 35.Cortese S, Asherson P, Sonuga-Barke E, Banaschewski T, Brandeis D, Buitelaar J, et al. ADHD management during the COVID-19 pandemic: guidance from the European ADHD Guidelines Group. Lancet Child Adolesc Health. juin. 2020;4(6):412–4. doi: 10.1016/S2352-4642(20)30110-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Amorim R, Catarino S, Miragaia P, Ferreras C, Viana V, Guardiano M. The impact of COVID-19 on children with autism spectrum disorder. Rev Neurol. 16 Oct 2020;71(8):285–91. [DOI] [PubMed]
- 37.Bobo E, Lin L, Acquaviva E, Caci H, Franc N, Gamon L, et al. Comment les enfants et adolescents avec le trouble déficit d’attention/hyperactivité (TDAH) vivent-ils le confinement durant la pandémie COVID-19 ? L’Encéphale. 1 juin 2020;46(3, Supplement):S85–92. [DOI] [PMC free article] [PubMed]
- 38.Colizzi M, Sironi E, Antonini F, Ciceri ML, Bovo C, Zoccante L. Psychosocial and Behavioral Impact of COVID-19 in Autism Spectrum Disorder: An Online Parent Survey. Brain Sci. juin. 2020;10(6):341. doi: 10.3390/brainsci10060341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang Y, Zhang H, Ma X, Di Q. Mental Health Problems during the COVID-19 Pandemics and the Mitigation Effects of Exercise: A Longitudinal Study of College Students in China. Int J Environ Res Public Health. janv 2020;17(10):3722. [DOI] [PMC free article] [PubMed]
- 40.Duan L, Shao X, Wang Y, Huang Y, Miao J, Yang X, et al. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J Affect Disord. 2020;1(275):112–8. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Messaadi N, Bayen S, Beghin L, Lefebvre J-M, Colleau S, Deken V, et al. [Association between screen time and sleep habits in 11-to-12-year-old French middle school students]. Rev Epidemiol Sante Publique. June 2020;68(3):179‑84. [DOI] [PubMed]
- 42.Dumas TM, Ellis W, Litt DM. What Does Adolescent Substance Use Look Like During the COVID-19 Pandemic? Examining Changes in Frequency, Social Contexts, and Pandemic-Related Predictors. J Adolesc Health. 1 Sept 2020;67(3):354–61. [DOI] [PMC free article] [PubMed]
- 43.Thorisdottir IE, Asgeirsdottir BB, Kristjansson AL, Valdimarsdottir HB, Jonsdottir Tolgyes EM, Sigfusson J, et al. Depressive symptoms, mental wellbeing, and substance use among adolescents before and during the COVID-19 pandemic in Iceland: a longitudinal, population-based study. Lancet Psychiatry. août. 2021;8(8):663–72. doi: 10.1016/S2215-0366(21)00156-5. [DOI] [PubMed] [Google Scholar]
- 44.Gaiha SM, Lempert LK, Halpern-Felsher B. Underage Youth and Young Adult e-Cigarette Use and Access Before and During the Coronavirus Disease 2019 Pandemic. JAMA Netw Open. 1 déc 2020;3(12):e2027572. [DOI] [PMC free article] [PubMed]
- 45.Pelham WE, Tapert SF, Gonzalez MR, McCabe CJ, Lisdahl KM, Alzueta E, et al. Early Adolescent Substance Use Before and During the COVID-19 Pandemic: A Longitudinal Survey in the ABCD Study Cohort. J Adolesc Health Off Publ Soc Adolesc Med. Sept 2021;69(3):390–7. [DOI] [PMC free article] [PubMed]
- 46.Zhou S-J, Zhang L-G, Wang L-L, Guo Z-C, Wang J-Q, Chen J-C, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. juin. 2020;29(6):749–58. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liang L, Ren H, Cao R, Hu Y, Qin Z, Li C, et al. The Effect of COVID-19 on Youth Mental Health. Psychiatr Q. 21 avr 2020;1–12. [DOI] [PMC free article] [PubMed]
- 48.Hafstad GS, Sætren SS, Wentzel-Larsen T, Augusti E-M. Adolescents’ symptoms of anxiety and depression before and during the Covid-19 outbreak - A prospective population-based study of teenagers in Norway. Lancet Reg Health Eur. juin 2021;5:100093. [DOI] [PMC free article] [PubMed]
- 49.Zhang H, Xu H, Huang L, Wang Y, Deng F, Wang X, et al. Increased occurrence of PTSD symptoms in adolescents with major depressive disorder soon after the start of the COVID-19 outbreak in China: a cross-sectional survey. BMC Psychiatry. 9 août 2021;21(1):395. [DOI] [PMC free article] [PubMed]
- 50.•• Meade J. Mental Health Effects of the COVID-19 Pandemic on Children and Adolescents: A Review of the Current Research. Pediatr Clin North Am. 2021;68(5):945–59. This 2021 review includes 18 studies examining the impact of the pandemic on anxio-depressive symptoms and their possible risk factors among adolescents, school-aged children and younger children. Considering age specific symptoms, the authors concluded that all age groups suffered from increased anxiety and depression compared with pre-pandemic levels. [DOI] [PMC free article] [PubMed]
- 51.Todisco P, Donini LM. Eating disorders and obesity (ED&O) in the COVID-19 storm. Eat Weight Disord. 1 juin 2020;1–4. [DOI] [PMC free article] [PubMed]
- 52.Barney A, Buckelew S, Mesheriakova V, Raymond-Flesch M. The COVID-19 Pandemic and Rapid Implementation of Adolescent and Young Adult Telemedicine: Challenges and Opportunities for Innovation. Journal of Adolescent Health. 1 Aug 2020;67(2):164‑71. [DOI] [PMC free article] [PubMed]
- 53.Davis C, Ng KC, Oh JY, Baeg A, Rajasegaran K, Chew CSE. Caring for Children and Adolescents With Eating Disorders in the Current Coronavirus 19 Pandemic: A Singapore Perspective. J Adolesc Health. 1 juill 2020;67(1):131–4. [DOI] [PMC free article] [PubMed]
- 54.Graell M, Morón-Nozaleda MG, Camarneiro R, Villaseñor Á, Yáñez S, Muñoz R, et al. Children and adolescents with eating disorders during COVID-19 confinement: Difficulties and future challenges. European Eating Disorders Review. 2020;28(6):864‑70. [DOI] [PubMed]
- 55.Waller G, Pugh M, Mulkens S, Moore E, Mountford VA, Carter J, et al. Cognitive-behavioral therapy in the time of coronavirus: Clinician tips for working with eating disorders via telehealth when face-to-face meetings are not possible. Int J Eat Disord. 2020;53(7):1132–41. doi: 10.1002/eat.23289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Touyz S, Lacey H, Hay P. Eating disorders in the time of COVID-19. J Eat Disord. 20 Dec 2020;8(1):19. [DOI] [PMC free article] [PubMed]
- 57.Fernández-Aranda F, Casas M, Claes L, Bryan DC, Favaro A, Granero R, et al. COVID-19 and implications for eating disorders. Eur Eat Disord Rev. mai. 2020;28(3):239–45. doi: 10.1002/erv.2738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pearl RL. Weight Stigma and the « Quarantine-15 ». Obes Silver Spring Md. 2020;28(7):1180–1. doi: 10.1002/oby.22850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Haripersad YV, Kannegiesser-Bailey M, Morton K, Skeldon S, Shipton N, Edwards K, et al. Outbreak of anorexia nervosa admissions during the COVID-19 pandemic. Arch Dis Child. Mars 2021;106(3):e15. [DOI] [PubMed]
- 60.Lin JA, Hartman-Munick SM, Kells MR, Milliren CE, Slater WA, Woods ER, et al. The Impact of the COVID-19 Pandemic on the Number of Adolescents/Young Adults Seeking Eating Disorder-Related Care. J Adolesc Health Off Publ Soc Adolesc Med. 2021;69(4):660–3. doi: 10.1016/j.jadohealth.2021.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hill RM, Rufino K, Kurian S, Saxena J, Saxena K, Williams L. Suicide Ideation and Attempts in a Pediatric Emergency Department Before and During COVID-19. Pediatrics. Mars 2021;147(3):e2020029280. [DOI] [PubMed]
- 62.Nissen JB, Højgaard DRMA, Thomsen PH. The immediate effect of COVID-19 pandemic on children and adolescents with obsessive compulsive disorder. BMC Psychiatry. 20 Oct 2020;20(1):511. [DOI] [PMC free article] [PubMed]
- 63.Imran N, Zeshan M, Pervaiz Z. Mental health considerations for children & adolescents in COVID-19 Pandemic. Pak J Med Sci. May 2020;36(COVID19-S4):S67‑72. [DOI] [PMC free article] [PubMed]
- 64.Guessoum SB, Lachal J, Radjack R, Carretier E, Minassian S, Benoit L, et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 29 juin 2020;291:113264. [DOI] [PMC free article] [PubMed]
- 65.Infographic: Coping with stress during the 2019-nCoV outbreak - PAHO/WHO | Pan American Health Organization [Internet]. [cité 7 Sept 2020]. Disponible sur: http://www.paho.org/en/documents/infographic-coping-stress-during-2019-ncov-outbreak.
- 66.Jiao WY, Wang LN, Liu J, Fang SF, Jiao FY, Pettoello-Mantovani M, et al. Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. J Pediatr. juin. 2020;221:264–6.e1. doi: 10.1016/j.jpeds.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Becker SP, Gregory AM. Editorial Perspective: Perils and promise for child and adolescent sleep and associated psychopathology during the COVID-19 pandemic. J Child Psychol Psychiatry. 2020;61(7):757‑9. [DOI] [PMC free article] [PubMed]
- 68.Nagata JM, Abdel Magid HS, Pettee Gabriel K. Screen Time for Children and Adolescents During the Coronavirus Disease 2019 Pandemic. Obesity. 2020;28(9):1582‑3. [DOI] [PMC free article] [PubMed]
- 69.Ko C-H, Yen J-Y. Impact of COVID-19 on gaming disorder: Monitoring and prevention. J Behav Addict. 6 juin 2020;9(2):187–9. [DOI] [PMC free article] [PubMed]
- 70.Cobham VE, McDermott B, Haslam D, Sanders MR. The Role of Parents, Parenting and the Family Environment in Children’s Post-Disaster Mental Health. Curr Psychiatry Rep. 16 avr 2016;18(6):53. [DOI] [PubMed]
- 71.Narzisi A. Handle the Autism Spectrum Condition during Coronavirus (COVID-19) Stay at Home Period: Ten Tips for Helping Parents and Caregivers of Young Children. Brain Sci. avr. 2020;10(4):207. doi: 10.3390/brainsci10040207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chevance A, Gourion D, Hoertel N, Llorca P-M, Thomas P, Bocher R, et al. Assurer les soins aux patients souffrant de troubles psychiques en France pendant l’épidémie à SARS-CoV-2. L’Encéphale. 1 juin 2020;46(3, Supplement):S3‑13. [DOI] [PMC free article] [PubMed]
- 73.Fegert JM, Schulze UME. COVID-19 and its impact on child and adolescent psychiatry – a German and personal perspective. Ir J Psychol Med. undefined/ed;1–3. [DOI] [PMC free article] [PubMed]
- 74.Chen S. An online solution focused brief therapy for adolescent anxiety during the novel coronavirus disease (COVID-19) pandemic: a structured summary of a study protocol for a randomised controlled trial. Trials. 13 mai 2020;21(1):402. [DOI] [PMC free article] [PubMed]
- 75.Wade M, Prime H, Browne DT. Why we need longitudinal mental health research with children and youth during (and after) the COVID-19 pandemic. Psychiatry Res. 2020;290:113143. [DOI] [PMC free article] [PubMed]