Abstract
Background
Cholangiocarcinomas (CCAs) are a rare group of malignancies characterized by dismal prognosis. There are currently no standardized guidelines for multidisciplinary teams (MDTs) in CCAs.
Material and methods
An online survey was built with the aim of defining the current practice of MDTs in CCAs and identifying possible areas of improvement, providing minimum standards of practice for an ideal CCA MDT. Analysis of the replies regarding current and ideal MDT practice was carried out by calculating weighted average (WA) of likelihood of every item. The survey was shared with members of the European Network for the Study of Cholangiocarcinoma and other medical centers with expertise in biliary tract cancer part of the EURO-CHOLANGIO-NET (European Cholangiocarcinoma Network: https://eurocholangionet.eu/) COST Action CA18122 initiative.
Results
The role of the MDT coordinator was a recognized priority in an ideal well-functioning MDT (WA 3.31/4), together with providing minimum clinical information before the meeting to secure adequate case preparation (WA 3.54/4). Optimal frequency of MDT meetings was weekly according to 76.92% of the participants; 73.06% believed that ideally all newly diagnosed patients and each new treatment should be discussed, although that happened only in less than half of the MDTs (46.15%) in current practice. Most participants stated that they always (46.15%) or often (50.00%) used guidelines, mainly international (61.00%) (European and American), followed by national/local (39.00%). We defined the ideal setup of a CCA MDT, identifying specialists whose presence is mandatory with WA >3.0 (oncologist, clinician responsible for patient’s care, surgeon, diagnostic and interventional radiologist, hepatologist, pathologist, endoscopist and gastroenterologist) and those whose presence would be recommended with a WA <3.0 (palliative care, nurse, dietitian, basic researcher, psychologist and social worker).
Conclusions
Our identified minimum requirements should be taken into account at the time of CCA MDT setup and quality assessment.
Key words: multidisciplinary team, cholangiocarcinoma, survey, current practice, Europe
Highlights
-
•
This is the first international effort to establish the basis of adequate MDT dedicated to CCA.
-
•
Patients’ supportive care needs and preference should be discussed collectively.
-
•
Presence of the endoscopist should be area of review in individual MDTs.
Introduction
Cholangiocarcinomas (CCAs) are a group of malignancies characterized by dismal prognosis. According to anatomical location, they can be classified as intrahepatic (iCCA), perihilar (pCCA) and distal CCAs (dCCA).1 CCA is the second most common primary liver cancer, after hepatocellular carcinoma, and represents 3% of deaths related to cancer.2 In Western countries, its incidence is 0.3-3.4 per 100 000 inhabitants per year with significant geographical variation.3 A steady increase in the number of deaths associated to this condition has been observed over the past 20 years.4,5 Today, surgery is considered the only potential curative treatment. However, most patients are not suitable for surgery, because of locally advanced or metastatic disease at the time of diagnosis due to insidious clinical presentation and lack of effective screening tests. In this patient setting, the main therapeutic alternative is palliative chemotherapy, with the combination of cisplatin and gemcitabine as the first-line treatment.6 Especially in patients with pCCAs, malignant strictures may require placement of endoscopic and percutaneous biliary drainages, both in pre-operative and palliative settings. Given the complexity of imaging and the interventional nature of some diagnostic and therapeutic procedures with related complications, a multidisciplinary approach is increasingly used to guarantee to every patient best assessment and right timely treatment.
A multidisciplinary team (MDT) is defined as a group of professionals from different specialties who regularly meet to discuss patients’ diagnosis and treatment plan. The first MDTs date back to the 1980s when it was observed that the combination of chemo-/radiotherapy and the collaboration between oncologists, radiologists and surgeons led to improved survival.7 The contribution of MDTs to improvement in clinical outcomes is still not totally clear although it has been proven that patients discussed at MDT meetings are more likely to receive more accurate staging and more frequently neoadjuvant/adjuvant chemotherapy.8 Today, the MDT is considered ‘best practice’ in cancer care, also on a legal perspective. Unfortunately, there are no standardized guidelines for MDT practice in CCAs. Given the rarity of the disease, we believe that recommendations for a well-functioning MDT would be useful to secure best patient care and for making collaboration between specialists and clinical practice more efficient.
The European Network for the Study of Cholangiocarcinoma (ENS-CCA: www.enscca.org/) is a multidisciplinary network of professionals with expertise in CCA, constituting research groups with interest in basic, translational and clinical CCA research. The aim of the network is to promote research studies on CCAs to understand the complexity of these rare malignancies better and to develop new diagnostic and therapeutic strategies that might help to improve patient outcomes. On this purpose, ENS-CCA recently provided an expert consensus statement with a detailed critical overview of the current knowledge in this field and proposing expert recommendations (4). Under the auspices of ENS-CCA, the EURO-CHOLANGIO-NET (European Cholangiocarcinoma Network: https://eurocholangionet.eu/) COST Action CA18122 aims to set up a pan-European-wide interdisciplinary cooperative network and advance the understanding of CCA to translate basic research and preclinical findings into clinical practice.
For this purpose, the aim of this survey was to define the current practice of MDTs in CCAs and identify possible areas of improvement and define minimum standards of practice.
Materials and methods
An online survey was built and shared with members of ENS-CCA and other medical centers with expertise in biliary tract cancer (BTC) part of the EURO-CHOLANGIO-NET COST Action CA18122 initiative. Questions regarding both the current practice of MDTs for CCAs (i.e. referral, frequency of meeting, different specialties involved) and the ideal vision of each participant were included. The primary aim of the survey was to define the current practice of MDTs dedicated to such a rare disease, to identify any possible areas of improvement and to define agreed minimum standards of practice.
The survey evaluated current and ideal practice in terms of the presence of each specialist in the meeting, the process of diagnostic/therapeutic decision making and the use of guidelines. At the time of assessing current practice, participants were asked to determine how likely a variety of items would currently apply in their MDT; replies were collected in numbers ranging between 1 (very rarely) and 4 (always). Participants were also asked to determine the importance of each of these factors in an ideal practice, collecting replies in numbers ranging between 1 (unnecessary) and 4 (mandatory). Analysis of the replies regarding current and ideal MDT practice was carried out by calculating weighted average (WA) of likelihood of every item.
Those items scoring a WA of 3 or more in an ideal MDT scenario were considered to be key and mandatory in a well-functioning CCA MDT and therefore included as part of the recommended minimum standards of practice; if weighted mean was <3, the aspect was considered recommended but not mandatory.
Comparing WA for each item for both current practice and ideal MDT scenario allowed current practice and practice in an ideal MDT scenario to be compared. For doing so, WA differences (denoted as ΔWA for the purpose of this article) between ideal practice and current practice were calculated for each item, in order to identify areas of improvement. If WA differences (ΔWA) were ≤0.1, the aspect was considered to be already consolidated in clinical practice; if the difference was between 0.11 and 0.4 and between 0.41 and 0.9, the aspect was considered well established and borderline established, respectively. A difference ≥0.9 identified the aspects to which urgent attention should be paid.
Results
Responses were collected between 12 February 2021 and 01 May 2021 from 34 institutions and most were public medical and academic centers (85.29%); of these, 8 (23.53%) were from Italy, 6 (17.65%) from Spain and 4 (11.76%) from Germany (Supplementary Table S1 and Figure S1, available at https://doi.org/10.1016/j.esmoop.2021.100377). A good representation of specialties was observed: most participants were surgeons (26.48%), hepatologists (20.59%) and medical oncologists (17.65%).
Current and ideal MDT setup
The first part of the survey aimed to define the current practice and the setup of MDTs (Table 1). Participants were first asked about the presence and importance of a coordinator in their MDT: 84.62% of the participants had a coordinator, of which 42.31% thought having an MDT coordinator should be mandatory, while 46.15% thought it was important but not mandatory. The role of the MDT coordinator was a recognized priority in an ideal well-functioning MDT (WA 3.31/4). Almost all of the participants (92.31%) supported the availability of minimum information before MDT discussion to allow the radiologist to prepare the MDT in advance; only two sites (7.69%) stated that there was no need to refer patients in advance before discussion. In an ideal MDT scenario, 57.69% of responders believed that this should be mandatory, with 38.46% of responders stating this to be important but not mandatory (WA 3.54/4). Out of all responders, referrals to MDT were mainly in electronic form [online platform (34.62%) or email (30.77%)], with minority of telephone referrals (15.38%) or other (11.54% including one center with regional referral system, one center with both online and telephone agreement); for 7.69% of responders prior referral was not completed. Meeting frequency was mostly weekly (65.38%) and to a lesser extent two-weekly (15.38%). When queried regarding the ideal MDT frequency, 76.92% of the participants believed that MDTs should be held weekly.
Table 1.
Current and ideal MDT setup
| Current |
Ideal |
||||
|---|---|---|---|---|---|
| N | % | N | % | WA | |
| MDT coordinator | |||||
| Yes | 22 | 84.62 | Mandatory (11); important (12) | Mandatory (42.31); important (46.15) | 3.31/4 |
| No | 4 | 15.38 | Not important (3); unnecessary (0) | Not important (11.54); unnecessary (0) | |
| Preliminary information | |||||
| Yes | 24 | 92.31 | Mandatory (15); important (10) | Mandatory (57.69); important (38.46) | 3.54/4 |
| No | 2 | 7.69 | Not important (1); unnecessary (0) | Not important (3.85); unnecessary (0) | |
| Frequency | |||||
| Weekly | 17 | 65.38 | 20 | 76.92 | n/a |
| Two-weekly | 4 | 15.38 | 5 | 19.23 | |
| Monthly | 2 | 7.69 | 0 | 0 | |
| Othera | |||||
| Criteria for patient referral | |||||
| All new patients and discussion of every new treatment | 12 | 46.15 | 17 | 73.08 | n/a |
| All new patients and discussion of some new treatment | 10 | 38.46 | 7 | 26.92 | |
| All new patients only, with no discussion after first treatment decision is made | 2 | 7.69 | 0 | 0 | |
| Discussion of selected scenarios only | 2 | 7.69 | 0 | 0 | |
| Number of CCAs discussed per week | |||||
| Number of total CCAs discussed per week, mean (range) | 3.27 (1-10) | n/a | n/a | n/a | |
| Number of new CCAs discussed per week, mean (range) | 1.72 (0.5-4+) | n/a | n/a | n/a | |
| Cancer type discussed in MDT | |||||
| Only CCA | 0 | 0 | n/a | n/a | n/a |
| Liver cancer | 17 | 65.38 | n/a | n/a | |
| Other GI cancer | 4 | 30.76 | n/a | n/a | |
| Other GI and not cancers also | 1 | 3.85 | n/a | n/a | |
The questions regarding the MDT setup in current practice and their comparison in the ideal MDT scenario are presented in the table.
CCA, cholangiocarcinoma; dCCA, distal cholangiocarcinoma; GI, gastrointestinal; iCCA, intrahepatic cholangiocarcinoma; MDT, multidisciplinary team; N, number; n/a, not applicable; pCCA, perihilar cholangiocarcinoma; WA, weighted average.
Others included in current practice (‘three different MDTs: one for pre-operative dCCA, one for pre-operative iCCA, pCCA and gallbladder carcinoma, one for any post-operative CCA’. ‘When needed’) and in an ideal MDT scenario: (‘weekly and twice a week for undrained pCCA’).
When asked about patient’s referral criteria to the MDT, 73.06% of the participants believed that ideally all newly diagnosed patients and each new treatment should be discussed, although that happened in less than half of the MDTs (46.15%) in current practice; in 38.46% of cases, patients were discussed at first diagnosis (new CCA) and only for some new treatment consideration. The median number of total CCA cases discussed per week was 3.00 with a range of 1-10. The median number of new CCA cases discussed per week was 1.75 with a range of 0.5-4. A total of 65.38% of responders were part of MDTs dedicated to liver cancers; 30.76% also included other gastrointestinal cancers. None of the responders were part of a dedicated CCA-only MDT.
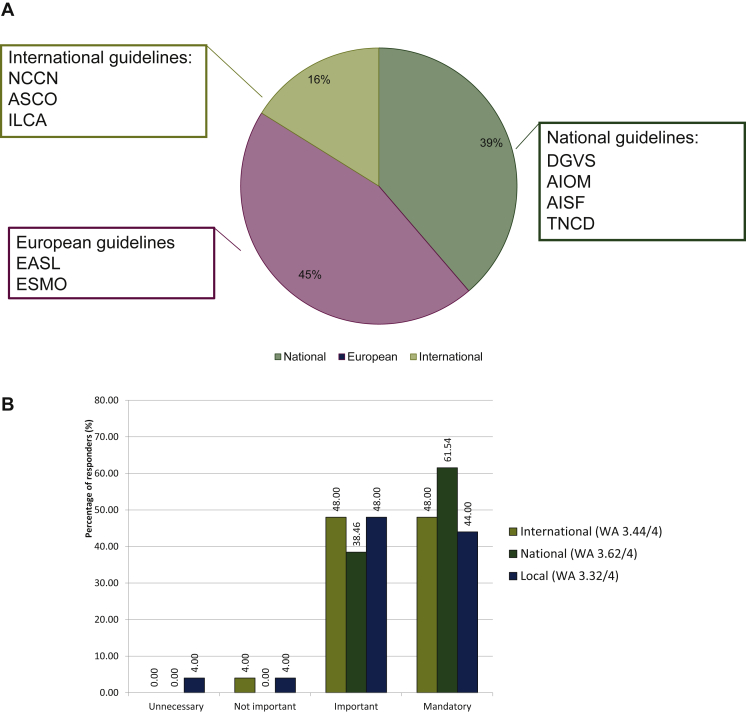
Decision-making process during MDT
Regarding the decision-making process, most participants stated that they always (46.15%) or often (50.00%) used guidelines; only one responder (3.85%) stated that guidelines were rarely used. The most frequently used guidelines were mainly international (61.00%) {European [European Society for Medical Oncology (ESMO) and European Association for the Study of the Liver; 45.00%] and American [National Comprehensive Cancer Network, American Society of Clinical Oncology; 16.00%]}, followed by national/local guidelines (39.00%) (Figure 1A). Interestingly, when participants were asked which guidelines should be used in the ideal scenario (Figure 1B), there was a slight preference in favor of national (ideal MDT WA 3.62/4) over international (ideal MDT WA 3.44/4) and local (ideal MDT WA 3.32/4) guidelines. When the main management aspects to be discussed in current and ideal CCA MDT were assessed, we identified that the collective discussion of diagnostic and treatment decisions was considered to be mandatory (ideal MDT WA 3.42/4 and 3.65/4, respectively) and already well-established practice (ΔWA 0.23 and 0.27, respectively). Discussion of patients’ preferences and supportive care was also considered mandatory (ideal MDT WA 3.25/4 and 3.04/4, respectively), although it was only borderline established in current practice (ΔWA 0.65 and 0.81, respectively) (Supplementary Figure S2, available at https://doi.org/10.1016/j.esmoop.2021.100377; full details provided in Supplementary Table S2, available at https://doi.org/10.1016/j.esmoop.2021.100377).
Figure 1.
Use of guidelines.
(A) Use of guidelines in cholangiocarcinoma (CCA) multidisciplinary teams (MDTs). Summary of the main guidelines used in the MDTs. European guidelines were the most frequently used. (B) Weighted average (WA) of local, national and international guidelines in an ideal scenario.
AIOM, Associazione Italiana Di Oncologia Medica; ASCO, American Society of Clinical Oncology; AISF, Associazione Italiana Per Lo Studio Del Fegato; DGVS, Deutsche Gesellschaft für Gastroenterologie, Verdauungs- und Stoffwechselkrankheiten; EASL, European Association for the Study of the Liver; ESMO, European Society for Medical Oncology; ILCA, The International Liver Cancer Association; NCCN, The National Comprehensive Cancer Network; TNCD, Thesaurus National De Cancerologie Digestive.
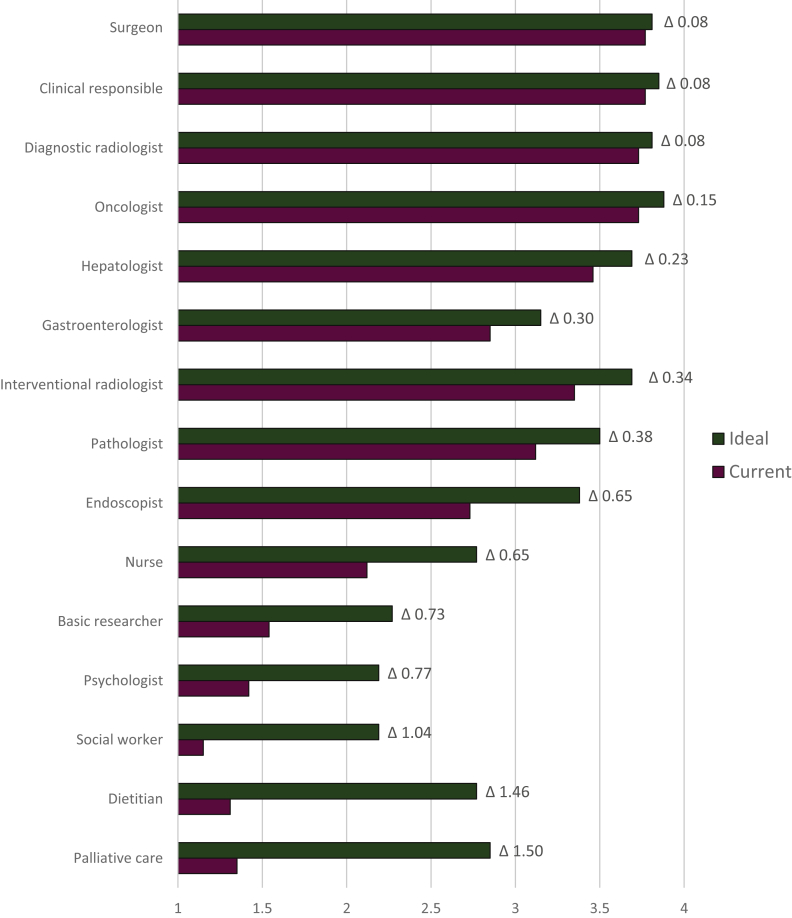
Presence of individual specialists in current and ideal MDTs
Through the ideal MDT WA assessment, we identified the specialists whose presence is considered mandatory (Figure 2; full details provided in Supplementary Table S2, available at https://doi.org/10.1016/j.esmoop.2021.100377) in a well-functioning ideal CCA MDT. These were: the oncologist (ideal MDT WA 3.88/4), the clinician responsible for the patient’s care (ideal MDT WA 3.85/4), surgeon (ideal MDT WA 3.81/4), diagnostic (ideal MDT WA 3.81/4) and interventional (ideal MDT WA 3.69/4) radiologist, hepatologist (ideal MDT WA 3.69/4), pathologist (ideal MDT WA 3.5/4), endoscopist (ideal MDT WA 3.38/4) and gastroenterologist (ideal MDT WA 3.15/4). By exploring the ΔWA, we identified mandatory presence to be already consolidated (ΔWA ≤0.1) for the clinician responsible for the patient’s care, diagnostic radiologist and surgeon and well established (ΔWA 0.11-0.4) for interventional radiologist, oncologist, hepatologist, gastroenterologist and pathologist. In contrast, the presence of the endoscopist was only borderline established and should be area of review in individual MDTs (ΔWA 0.65). We also identified the presence of other specialists such as palliative care (ideal MDT WA 2.8/4), nurse and dietitian (ideal MDT WA 2.77/4), basic researcher (ideal MDT WA 2.27/4), psychologist and social worker (ideal MDT WA 2.19/4) as recommended (not mandatory). Of these, the presence of some specialists such as psychologists (ΔWA 0.77), basic researchers (ΔWA 0.73) and nurses (ΔWA 0.65) seemed to be only borderline established in current practice. In addition, urgent attention should be paid to the under-representation of palliative care (ΔWA 1.5), dietitians (ΔWA 1.46) and social workers (ΔWA 1.04).
Figure 2.
Current and ideal representation of different specialties in cholangiocarcinoma (CCA) multidisciplinary team (MDT).
The presence of some specialist was considered mandatory and well established [ideal weighted average (WA) >3; ΔWA between 0.11 and 0.4] in current practice of CCA MDTs (i.e., clinician responsible, oncologist, hepatologist, gastroenterologist, surgeon and radiologist). The presence of some specialists (i.e., endoscopist, psychologist and pathologist) seemed to be only acceptably established in current practice (ΔWA between 0.41 and 0.9). The presence of palliative care, dietitian and social workers should be considered areas for improvement and in need of urgent attention (ΔWA >0.9).
Open question
The last area of the survey was dedicated to open questions. Participants were asked what the strength of their MDT was; main strengths included expertise of the specialists and collaboration between participants. In terms of identified weaknesses, these were low frequency of meetings, low number of patients referred to MDT and absence of some relevant specialists. Participants were finally asked how their MDT could improve; the main answers related to this were the need of a standardize MDT setup, auditing of results and greater participation of all specialists.
Discussion
To our knowledge, prior to this work, there was no consensus on how an MDT for CCA should look like. ENS-CCA created and shared this survey with medical centers with expertise in BTC with the aim of defining the current and ideal practice of the MDT dedicated to patients with CCA and to provide minimal recommendations for a well-functioning CCA MDT in an area with no standardized practice. Good representation of all specialists was observed in participants from 34 European and international institutions. Our results identified the desirable setup for a well-functioning MDT, the criteria for patient referral and the decision-making process. We also outlined the ideal assessment of the MDT and the use of guidelines. Finally, the survey highlighted some aspects to which attention should be paid, which, although recognized as important, are still only borderline established in current practice. According to our findings, we have provided in Table 2 the list of ENS-CCA recommendations for CCA MDT. Within these minimum recommendations, some areas for improvement were highlighted in Figure 3. MDT meetings are deeply rooted in clinical practice, especially in cancer care, and quality criteria for an effective MDT meeting have already been developed.9 A considerable amount of time and resources are required for all the specialists involved to organize the meetings regularly. MDT meetings also represent a significant financial commitment for the center. However, in a previous national survey, ∼80% of members of an MDT found job satisfaction working in a well-functioning MDT.10 According to our results, the presence of an MDT coordinator who conducts meetings and facilitates collaboration between specialists should be considered mandatory.
Table 2.
ENS-CCA recommendations for CCA MDT
| Recommendations | |
|---|---|
| MDT coordinator | Presence of MDT coordinator should be mandatory for a well-functioning MDT |
| Frequency | The MDT should meet weekly. In escenarios of worsening obstructive jaundice or hospitalization in need of urgent review and discussion, an Ad hoc same-day multidisciplinary discussion should be considered for staging, determining resectability and the corresponding segments that require urgent drainage. |
| Referral | Patients should be referred online to the MDT discussion via standard platform or email |
| Patient information | Information should be provided before the discussion in order to allow radiologists to prepare properly the case and the images |
| Discussion criteria | Each new patient and each new treatment should be discussed |
| Type of MDT | Patients with CCA should be discussed in MDTs dedicated to liver cancers only. Whenever possible, centralisation of care/MDTs within a region is recomended to secure adequate experienzed decision making. |
| Guidelines | Guidelines should be used for diagnosis and treatment decision making. Our preference is to use national guidelines, more aware of locally accessible treatment options |
| Mandatory aspects to be discussed | Collective discussion of diagnostic decision and treatment, patients’ preferences and supportive care needs should be mandatory |
| Mandatory specialists | Presence of the oncologist, clinician responsible for the patient’s care, surgeon, diagnostic and interventional radiologist, hepatologist, pathologist, endoscopist and gastroenterologist should be mandatory in a well-functioning MDT |
| Desirable specialists | Presence of palliative, nurse and dietitian, basic researcher, psychologist and social worker should be recommended |
CCA, cholangiocarcinoma; ENS-CCA, European Network for the Study of Cholangiocarcinoma; MDT, multidisciplinary team.
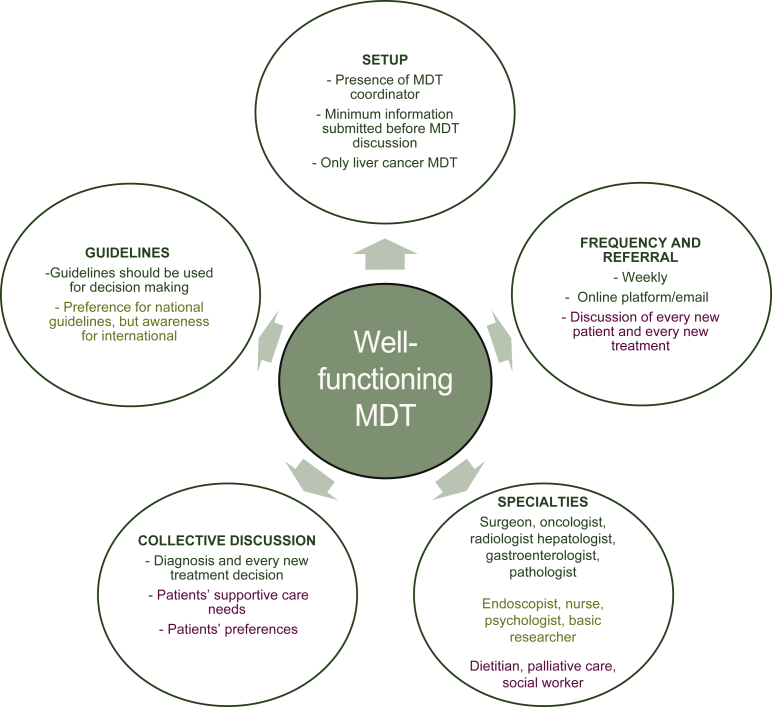
Figure 3.
Take home messages.
Summary of the European Network for the Study of Cholangiocarcinoma (ENS-CCA) recommendations for a well-functioning multidisciplinary team (MDT). Items already consolidated in current practice are shown in green, those only acceptably set in olive green and items to which attention should be paid in burgundy.
The vast majority of our participants (92%) agreed that clinical information needed to be provided before discussion, especially to the radiologists. Indeed, it has been estimated that radiologists take about 2 hours to prepare and review the images needed for an hour of meeting.11 Some exceptions may apply as in the case of patients with pCCA and worsening obstructive jaundice or hospitalization in need of urgent review and discussion. For these selected patients, short in-hospital stay with an Ad hoc same-day multidisciplinary discussion should be considered for staging, determining resectability and the corresponding segments that require urgent drainage. Except for these particular scenarios, patients should be referred before the discussion to allow radiologists and pathologists to prepare the discussion. The most recommended referral method is online: email or online platform, thus being able to standardize the information necessary for an adequate discussion. Furthermore, due to the recent pandemic, many digital options have been implemented globally. These options ensure that centralization of care can be facilitated to lower the threshold to discuss patients in MDTs of CCA centers. In participating MDTs, median of new CCAs discussed per week was 1.75 while median of total CCAs per week was 3.00. Clearly, these numbers refer to specialized tertiary care centers, but they underline the importance of meeting with adequate frequency. Indeed, according to 80% of participants, the optimal frequency of meetings should be weekly. From our survey, it emerges that, ideally, every new patient and every new treatment should be discussed. In clinical practice, however, this only occurs in less than half of the cases. Attention must be paid to this aspect because it is already established that the cancer patients discussed in MDT have access to more timely and appropriate treatments.12,13 None of the participating MDTs were dedicated solely to CCA. Given the rarity of the disease and the small number of CCAs to be discussed per week, an effort should be made to increase the centralization of care or at least the centralization of MDTs. This would increase the experience of MDT specialists and chances to select patients for clinical trials and to be a feasible site for multicenter clinical trials. Also, the development of CCA-specific MDT should be encouraged for the same reasons. If not feasible, it is preferable to discuss CCA cases in MDT with high expertise in liver cancer. It has already been observed that multidisciplinary discussion can improve the management of hepatocellular carcinoma.14 CCA often occurs in patients with liver cirrhosis or other underlying diseases and the presence of specialists with extensive experience in the field is crucial at the time of discussion; joining the CCA patients’ discussion in MDT dedicated to other gastrointestinal cancers is not to be considered best clinical practice to avoid losing focus. We then identified the aspects considered mandatory to be discussed collectively (Supplementary Figure S2, available at https://doi.org/10.1016/j.esmoop.2021.100377), by comparing ΔWA between ideal and current practice of each item. Particularly, the discussion of diagnostic and treatment decision, considered mandatory by almost all the participants, is already consolidated in current practice. Discussion of patient preferences and supportive care needs was also considered mandatory but is only borderline established in the current practice. According to our findings, attention must be paid to this aspect because it could potentially affect the clinical outcome. Indeed, it has been noted that patients usually receive more conservative treatments than originally planned because their preferences and psychological and social issues have not been taken into account previously.15 In terms of decision-making process, the vast majority of participants preferred the use of guidelines (Figure 1). Using the guidelines/group consensus for diagnosis and treatment decision was already a consolidated practice in MDTs. Previous studies have already shown that multidisciplinary care improved adherence to guidelines,16 ensuring the patient the best expected care. Interestingly, our participants expressed a slight preference for using national guidelines in an ideal MDT over international ones. Our recommendation is that the guidelines should be used for diagnostic and treatment decision making. It may be preferable to use national guidelines since these are more likely to be aware of the locally available treatment options. Still, it is important to be aware of international guidelines in order to offer the proper treatment in another specialized center if in the best interest of the patient. As illustrated in Figure 2, we identified specialists whose presence is considered mandatory in a well-functioning CCA MDT. By exploring the ΔWA, we identified mandatory presence to be already consolidated for clinician responsible of patient care, diagnostic radiologist and surgeon and well established for interventional radiologist, oncologist, hepatologist, gastroenterologist and pathologist. Interestingly, the presence of the endoscopist at the MDT was only borderline established. In pCCA/dCCA, biliary decompression is usually carried out by endoscopic retrograde cholangiopancreatography (ERCP), especially in pre-operative settings.17 The presence of such a specialist should therefore be area of review in individual MDTs. A peculiar feature of the clinical management of pCCA/dCCA is the need to obtain final microscopic diagnosis in conditions of jaundice or cholangitis which implicates a rapid conclusion of the diagnostic process ideally before biliary stenting. The presence of endoscopic specialists is going to be even more relevant in consideration of their involvement in the management, often promptly required and of technical advances, e.g. cholangioscopy or confocal endomicroscopy, and emerging evidences, e.g. the role of endoscopic ultrasonography-fine needle aspiration/biopsy (EUS-FNA/B) versus ERCP in the diagnosis of pCCA/dCCA.18 Indeed, EUS-FNA/B nowadays has a consolidate role as the first approach to obtain a definitive diagnosis of pCCA.19 Other than ERCP with sampling, cholangioscopy-guided biopsy of a target lesion is an accurate technique for a final diagnosis of pCCA, although with a low quality of evidence.19 Furthermore, the presence of psychologists, basic researchers and nurses is recommended but it seemed to be only borderline established in current practice. Given the rarity of the disease, for research purposes, it would be good practice to implement the involvement of a basic researcher. Also, the role of genetic advice unit should be considered because it is particularly relevant for molecular profiling and target therapies. As noted in previous studies, the nurse seems in most cases not to play an active role in the MDT discussion,20 although often more aware of patients’ performance status and preferences. They are mostly identified as advocates for the patient,21 but it is worth highlighting that the role of nurses varies greatly across countries. Regarding the presence of the psychologist, our results agree with previous studies22 and still only a few MDTs refer the patient to psychosocial services. Finally, urgent attention should be paid to specialists like palliative care, dietitians and social workers whose presence is considered extremely deficient. An important consideration is the patient’s involvement in the clinical decision-making process in the CCA MDT, on which there is still no consensus. One of the reasons the patient is usually not allowed to attend the discussion is that hearing explicitly discussing about prognosis and procedural risks can lead to significant emotional distress.23 On the other hand, a survey conducted by the UK’s Cholangiocarcinoma Charity (AMMF) has highlighted that, from the patient’s perspective, the main issues are the poor communication with the MDT specialists, the lack of representation in the meetings and the perception that multidisciplinary discussion can lengthen the treatment decision-making time.24 In order to assist and inform cancer patients, the European Cancer Organization has produced the European Code of Cancer Practice, a patient-centered manifesto that informs the patients about what to expect from their health system, in order for them to achieve the best possible outcomes.25 With a similar aim, ESMO provided a guide for BTC patients, their relatives and caregivers to better understand the nature of these malignancies and evaluate the best available treatment choices.26 Standardizing how to relate to patients and inform them of the outcomes of the consultation should therefore be a future challenge for CCA MDTs. It may be also argued that MDTs in CCA are the sole way to ensure the most appropriate health risk management and prevention in consideration of the high risk of procedural complications or adverse effects, e.g. sepsis after ERCP or percutaneous transhepatic cholangiography and post-ERCP pancreatitis.
Some limitations of this work are worth mentioning. Although the survey took place within the specialist centers of the European network, inclusion of countries outside Europe was limited. Therefore, these recommendations may not be easily applicable to non-European countries. Another limitation is the limited number of responders (n = 34). Finally, the responders mainly belonged to public academic institution and it is possible that the results are not applicable to different care delivery models.
Conclusion
In summary, our results provided an overview of current CCA MDT practice and provided minimum recommendations on how a CCA MDT should be set up in the coming future. In particular, having an MDT coordinator should be mandatory together with providing minimum clinical information before the meeting to secure adequate case preparation. Optimal frequency of MDT meetings should be weekly and ideally all newly diagnosed patients and each new treatment should be discussed, taking into account patients’ preferences and supportive care needs. Guidelines should be used for diagnosis and treatment decision-making process. We also defined the desirable setup of a CCA MDT, identifying specialists whose presence should be mandatory or only recommended. Interestingly, despite being considered mandatory, the presence of the endoscopist appeared to be only acceptably established in clinical practice and this should be highlighted as an area for improvement. Finally, urgent attention should be paid to the under-presence of palliative care, dietitians and social workers.
Acknowledgements
MC participated as mentee to the Euro-Cholangio-Net Mentorship Program of EURO-CHOLANGIO-NET COST Action CA18122, as a medical resident of gastroenterology in Sapienza University of Rome. AL received funding from The Christie Charity and the European Union’s Horizon 2020 Research and Innovation Programme [grant number 825510, ESCALON]; this article/publication is based upon work from COST Action European Cholangiocarcinoma Network, supported by COST (European Cooperation in Science and Technology; www.cost.eu), a funding agency for research and innovation networks. JB was funded by Spanish Carlos III Health Institute (ISCIII) [Miguel Servet Program grant numbers CON14/00129 and CPII19/00008]; CIBERehd (ISCIII); Department of Health of the Basque Country [grant number 2017111010]; BIOEF (Basque Foundation for Innovation and Health Research: EiTB Maratoia BIO15/CA/016/BD); ‘Fundación Científica de la Asociación Española Contra el Cáncer’ (AECC Scientific Foundation); and the European Union’s Horizon 2020 Research and Innovation Program [grant number 825510, ESCALON].
Funding
This research was funded by EURO-CHOLANGIO-NET (European Cholangiocarcinoma Network: https://eurocholangionet.eu/) COST Action (CA18122).
Disclosure
AL declares travel and educational support from Ipsen, Pfizer, Bayer, AAA, SirtEx, Novartis, Mylan and Delcath; speaker honoraria from Merck, Pfizer, Ipsen, Incyte, AAA and QED; advisory honoraria from EISAI, Nutricia Ipsen, QED and Roche; and she is a member of the Knowledge Network and NETConnect Initiatives funded by Ipsen, all outside the scope of this work. JWV reports personal fees from Agios, AstraZeneca, Baxter, Genoscience Pharma, Hutchison Medipharma, Imaging Equipment Ltd (AAA), Incyte, Ipsen, Mundipharma EDO, Mylan, QED, Servier, Sirtex and Zymeworks; and grants, personal fees and non-financial support from NuCana, outside the submitted work. JMB declares research grants from Incyte; personal fees for lecturer from Bayer and Intercept; and consulting role for QED Therapeutics, Albireo Pharma and OWL Metabolomics. The remaining authors have declared no conflicts of interest.
Supplementary data
References
- 1.Banales J.M., Cardinale V., Carpino G., et al. Expert consensus document: cholangiocarcinoma: current knowledge and future perspectives consensus statement from the European Network for the Study of Cholangiocarcinoma (ENS-CCA) Nat Rev Gastroenterol Hepatol. 2016;13(5):261–280. doi: 10.1038/nrgastro.2016.51. [DOI] [PubMed] [Google Scholar]
- 2.Fitzmaurice C., Dicker D., Pain A., et al. Global Burden of Disease Cancer Collaboration. The global burden of cancer 2013. JAMA Oncol. 2015;1:505–527. doi: 10.1001/jamaoncol.2015.0735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khan S.A., Tavolari S., Brandi G. Cholangiocarcinoma: epidemiology and risk factors. Liver Int. 2019;39:19–31. doi: 10.1111/liv.14095. [DOI] [PubMed] [Google Scholar]
- 4.Banales J.M., Marin J.J., Lamarca A., et al. Cholangiocarcinoma 2020: the next horizon in mechanisms and management. Nat Rev Gastroenterol Hepatol. 2020;17(9):557–588. doi: 10.1038/s41575-020-0310-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DeOliveira M.L., Cunningham S.C., Cameron J.L., et al. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg. 2007;245(5):755–762. doi: 10.1097/01.sla.0000251366.62632.d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Valle J., Wasan H., Palmer D.H., et al. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med. 2010;362(14):1273–1281. doi: 10.1056/NEJMoa0908721. [DOI] [PubMed] [Google Scholar]
- 7.Taberna M., Moncayo F.G., Jané-Salas E., et al. The multidisciplinary team (MDT) approach and quality of care. Front Oncol. 2020;10:85. doi: 10.3389/fonc.2020.00085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pillay B., Wootten A.C., Crowe H., et al. The impact of multidisciplinary team meetings on patient assessment, management and outcomes in oncology settings: a systematic review of the literature. Cancer Treat Rev. 2016;42:56–72. doi: 10.1016/j.ctrv.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 9.Ottevanger N., Hilbink M., Weenk M., et al. Oncologic multidisciplinary team meetings: evaluation of quality criteria. J Eval Clin Pract. 2013;19(6):1035–1043. doi: 10.1111/jep.12022. [DOI] [PubMed] [Google Scholar]
- 10.Taylor C., Ramirez A.J. 2009. Multidisciplinary team members’ views about MDT working: results from a survey commissioned by the National Cancer Action Team. Lond NHS Natl Cancer Action Team. [Google Scholar]
- 11.Kane B., Luz S., O’Briain D.S., McDermott R. Multidisciplinary team meetings and their impact on workflow in radiology and pathology departments. BMC Med. 2007;5(1):1–10. doi: 10.1186/1741-7015-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang J.H., Vines E., Bertsch H., et al. The impact of a multidisciplinary breast cancer center on recommendations for patient management: the University of Pennsylvania experience. Cancer. 2001;91(7):1231–1237. doi: 10.1002/1097-0142(20010401)91:7<1231::aid-cncr1123>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 13.Licitra L., Keilholz U., Tahara M., et al. Evaluation of the benefit and use of multidisciplinary teams in the treatment of head and neck cancer. Oral Oncol. 2016;59:73–79. doi: 10.1016/j.oraloncology.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Sherman M., Burak K., Maroun J., et al. Multidisciplinary Canadian consensus recommendations for the management and treatment of hepatocellular carcinoma. Curr Oncol. 2011;18(5):228–240. doi: 10.3747/co.v18i5.952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taylor C., Munro A.J., Glynne-Jones R., et al. Multidisciplinary team working in cancer: what is the evidence? Br Med J. 2010;340:c951. doi: 10.1136/bmj.c951. [DOI] [PubMed] [Google Scholar]
- 16.Kelly S.L., Jackson J.E., Hickey B.E., Szallasi F.G., Bond C.A. Multidisciplinary clinic care improves adherence to best practice in head and neck cancer. Am J Otolaryngol. 2013;34(1):57–60. doi: 10.1016/j.amjoto.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 17.Kennedy T.J., Yopp A., Qin Y., et al. Role of preoperative biliary drainage of liver remnant prior to extended liver resection for hilar cholangiocarcinoma. HPB. 2009;11(5):445–451. doi: 10.1111/j.1477-2574.2009.00090.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Valle J.W., Borbath I., Khan S.A., Huguet F., Gruenberger T., Arnold D. Biliary cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27:v28–v37. doi: 10.1093/annonc/mdw324. [DOI] [PubMed] [Google Scholar]
- 19.Alvaro D., Hassan C., Cardinale V., et al. Italian Clinical Practice Guidelines on Cholangiocarcinoma – Part I: classification, diagnosis and staging. Dig Liver Dis. 2020;52(11):1282–1293. doi: 10.1016/j.dld.2020.06.045. [DOI] [PubMed] [Google Scholar]
- 20.Lamb B., Brown K., Nagpal K., Vincent C., Green J.S.A., Sevdalis N. Team decision making by cancer care multidisciplinary teams: a systematic review. Ann Surg Oncol. 2011;18(8):2116–2125. doi: 10.1245/s10434-011-1675-6. [DOI] [PubMed] [Google Scholar]
- 21.Rankin N.M., Lai M., Miller D., et al. Cancer multidisciplinary team meetings in practice: results from a multi-institutional quantitative survey and implications for policy change. Asia Pac J Clin Oncol. 2018;14(1):74–83. doi: 10.1111/ajco.12765. [DOI] [PubMed] [Google Scholar]
- 22.Kidger J., Murdoch J., Donovan J.L., Blazeby J.M. Clinical decision-making in a multidisciplinary gynaecological cancer team: a qualitative study. BJOG. 2009;116(4):511–517. doi: 10.1111/j.1471-0528.2008.02066.x. [DOI] [PubMed] [Google Scholar]
- 23.Butow P., Harrison J.D., Choy E.T., Young J.M., Spillane A., Evans A. Health professional and consumer views on involving breast cancer patients in the multidisciplinary discussion of their disease and treatment plan. Cancer. 2007;110(9):1937–1944. doi: 10.1002/cncr.23007. [DOI] [PubMed] [Google Scholar]
- 24.Morement H., Harrison R., Taylor-Robinson S.D. The multidisciplinary team meeting in the UK from the patients’ perspective: comments and observations from cholangiocarcinoma patients and their families. Int J Gen Med. 2017;10:305–310. doi: 10.2147/IJGM.S145029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lawler M., Oliver K., Gijssels S., et al. The European Code of Cancer Practice. J Cancer Policy. 2021;28:100282. doi: 10.1016/j.jcpo.2021.100282. [DOI] [PubMed] [Google Scholar]
- 26.ESMO What is Biliary Tract Cancer∗? https://www.esmo.org/content/download/266801/5310983/1/EN-Biliary-Tract-Cancer-Guide-for-Patients.pdf Available at.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.