Abstract
INTRODUCTION
Pityrosporum folliculitis (PF) is a common skin condition that can be easily misdiagnosed, especially by non-dermatologists. While the initial diagnosis is often made clinically, skin microscopy may help to confirm the same. However, there is scant literature regarding the clinical epidemiology of PF. To our knowledge, in Singapore, only one prior epidemiological study was performed in 1987. Through the present study, we aimed to provide an update regarding the epidemiology, diagnosis and treatment of patients with PF in Singapore.
METHODS
We performed a retrospective review of patients with clinical presentations compatible with PF who presented to the dermatology clinic at the National University Hospital, Singapore, between 1 January 2011 and 31 December 2015. The medical records of patients identified as having clinical presentations that resembled PF were reviewed via written and electronic databases. Information regarding the demographics and clinical presentation of the patients was collected.
RESULTS
Of the 375 patients identified, 214 (57.1%) were confirmed as having PF based on Gram-stain microscopy. Most (35.0%) of these 214 patients were aged between 21 and 30 years, with a male-to-female ratio of 3:1. The lesions predominantly occurred on the trunk and the back. The majority of patients presented with symptoms that lasted more than one month. 128 (59.8%) patients received oral antifungal treatment, whereas 82 (38.3%) patients were treated with topical antifungal treatment alone.
CONCLUSION
A typical Singapore patient with PF is a young man aged 21–30 years, with erythematous follicular papules or pustules over the trunk and the back.
Keywords: Malassezia folliculitis, pityrosporum folliculitis
INTRODUCTION
Pityrosporum folliculitis (PF) is a common skin condition that can be easily misdiagnosed, especially by non-dermatologists. The characteristic clinical findings of PF include an acneiform eruption over the seborrhoeic areas, including the upper back, shoulders, upper chest and sides of the back, secondary to Malassezia furfur. While the diagnosis is often made clinically, it can be confirmed by skin microscopy. Limited literature exists on the clinical epidemiology of PF. In Singapore, to our knowledge, only one epidemiological study on PF was performed in 1987.(1) However, it is likely that the associated health-seeking behaviour of patients, diagnostic methods and treatments may have since evolved. Through this study, we aimed to provide an update regarding the epidemiology, diagnosis and treatment of patients with PF in Singapore.
METHODS
A retrospective review was performed of patients with clinical presentations compatible with PF who presented to the dermatology clinic at the National University Hospital, Singapore, between 1 January 2011 and 31 December 2015. The medical records of patients identified as having clinical presentations resembling those of PF were reviewed via the hospital’s written and electronic databases. A total of 375 patients with a presumptive diagnosis of PF were screened. Patients with a positive skin scrape for PF on Gram-stain microscopy were confirmed as having PF, and information regarding their age, ethnicity, gender, body mass index, physical distribution of lesions and duration of symptoms was collected.
RESULTS
Of the 375 patients identified, 214 (57.1%) were confirmed as having PF based on the presence of yeast-like organisms on Gram-stain microscopy of skin scrapings. The remaining 161 (42.9%) patients had negative fungal smears.
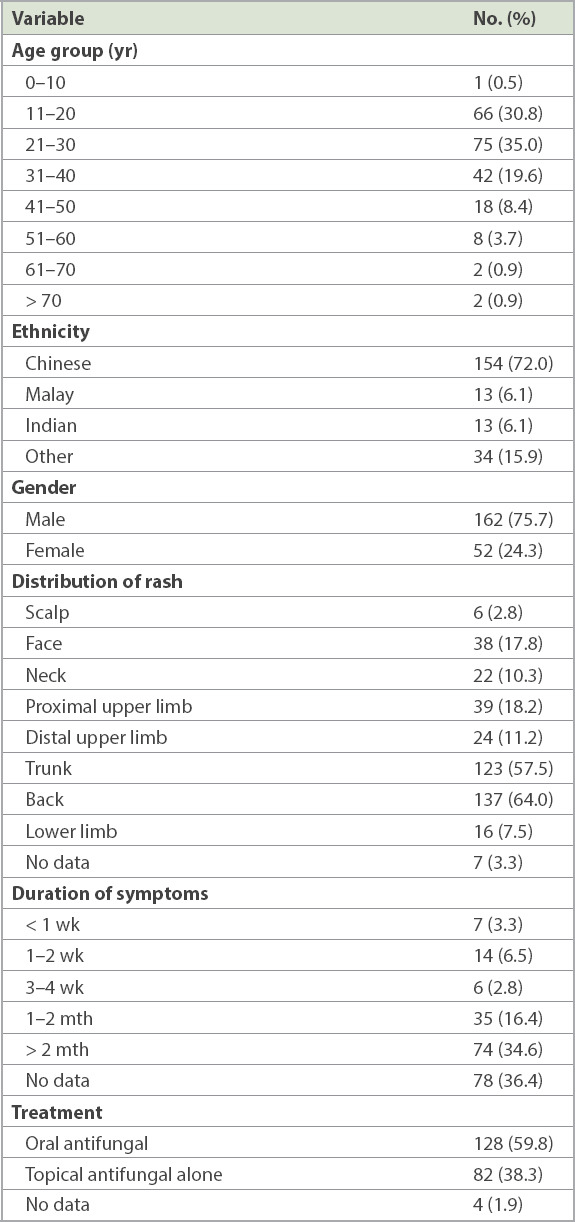
The epidemiologic and clinical features of patients confirmed as having PF were analysed, and the significant findings are summarised in Table I. Most (35.0%) patients with PF in our study were aged between 21 and 30 years. Thus, in general, the study population was young, with a majority of patients in the age groups of 11–20 years (30.8%) and 21–30 years. There were 162 male and 52 female patients, yielding a male-to-female ratio of 3:1. Ethnically, 154 (72.0%) patients were Chinese, 13 (6.1%) were Malay, 13 (6.1%) were Indian and 34 (15.9%) were of other ethnicities. The lesions predominantly occurred on the trunk and back areas, with 123 (57.5%) patients presenting with lesions on the trunk and 137 (64.0%) patients presenting with lesions on their back. A majority of patients presented with symptom duration of more than one month (n = 109, 50.9%).
Table I.
Epidemiologic and clinical features of patients confirmed as having pityrosporum folliculitis (n = 214).
128 (59.8%) patients received oral antifungal treatment, whereas 82 (38.3%) patients were treated with topical antifungal treatment alone. Topical antifungal therapy comprised clotrimazole cream, ketoconazole cream and wash, terbinafine cream, selenium sulfide shampoo, sulfur/resorcinol cream and propylene glycol solution. Oral antifungals prescribed included itraconazole, fluconazole and ketoconazole tablets. Topical antifungals were prescribed until the next follow-up, which was conducted after an average duration of two months. Oral antifungal therapy was generally administered for 2–4 weeks.
In our study, 26 (12.1%) patients experienced relapse, and 88.8% of patients were successfully treated with either topical or systemic antifungals for PF. Among patients with relapse, 10 (38.5%) received oral antifungal therapy and 16 (61.5%) received only topical antifungal therapy without oral antifungal agents. A treatment success rate of 92.2% was observed among patients receiving oral antifungal agents, compared to a rate of 80.5% among patients receiving topical antifungal monotherapy.
DISCUSSION
We observed that PF affected younger patients, with a predilection among those aged 11–40 years (n = 183, 85.5%). The most common age group affected in our analysis was 21–30 years. The demographics of our patients mostly reflected the ethnic composition of Singapore, with a slight over-representation of patients of other ethnicities. Rash distribution predominantly affected the trunk and back areas, with over 50% of patients presenting with rashes in either regions.
Patients predominantly presented after two months of symptoms. This was expected for a tertiary care dermatological centre, as most patients would have been managed in the primary care setting, and only the more recalcitrant ones would have been referred for tertiary medical care. As most of our patients were expected to be recalcitrant in nature, there was a slight preference for the use of oral antifungal agents as treatment, with 59.8% of patients receiving oral antifungal treatment in our study. The positive skin scrape on Gram-stain microscopy shown by 214 of our patients would likely have prompted the treating dermatologists to use oral antifungals.
The first impediment when diagnosing PF is arriving at an accurate diagnosis. PF mimics other diagnoses such as truncal acne vulgaris or other forms of folliculitis. However, certain distinguishing features may be useful in its clinical diagnosis. Firstly, truncal acne presents with comedones, and lesions may be polymorphic, ranging from papules to pustules, nodules and cysts. By contrast, lesions of PF do not include comedones, and tend to comprise monomorphic papules and/or pustules. These features may prompt a clinician to perform microscopic analysis of the skin scrapings.
In our study, although we identified 375 potential patients, only 214 patients ultimately had a positive skin scrape, which represented 57.1% of the sample size. The high proportion of patients who were found to not have PF, as initially thought, was likely attributable to misdiagnoses of PF rather than subsequent false-negative skin microscopy findings, given the high sensitivity and specificity of skin microscopy. A study conducted in 2017(2) regarding the utility of skin scrape with Gram staining for the diagnosis of PF in a group of 32 patients reported a sensitivity and specificity of 84.6% and 100%, respectively. The previous study concluded that Gram staining was a rapid, non-invasive, sensitive and specific method for the diagnosis of PF. These findings, including those of our present study, suggest that it would be prudent for clinicians to consider Gram staining for an accurate diagnosis of PF in suspected patients.
With regard to the distribution of lesions, a previous study(3) that compared the clinical presentations of PF and non-Malassezia folliculitis found that PF showed major involvement of the trunk and low involvement of the face and legs. A retrospective review in 2018(4) also concluded that PF mainly presented with monomorphic, pruritic papules and pustules along the hairline and on the upper portion of the back. This was similar to our findings, where lesions mainly targeted the trunk and back rather than the extremities.
A previous study concluded that PF treated with itraconazole yielded superior results to a placebo.(5) However, a study conducted in 2016 on 44 patients concluded that beneficial results could be safely obtained with topical antifungal therapy alone, although with a slightly longer time to resolution.(6) In our study, clinicians preferentially used oral antifungal treatment instead of topical antifungal treatment alone, possibly owing to the usually recalcitrant nature of PF observed at our tertiary care dermatology centre.
Our findings were similar to those of a previous study conducted in 1987(1) on the epidemiology of PF in Singapore. The mean age of the patients in that study was 22.2 (range 15–31) years. In addition, PF predominantly presented in male patients, with a male-to-female ratio of 11:1, and lesion distribution was predominant in the upper back, shoulders, upper chest and sides of back. Patients presented with a mean symptom duration of 10.9 months (range one month to seven years). Despite a sample size of 48 patients, the epidemiology and clinical features of the patients in the previous study were similar to those in our study. However, the previous study did not delineate a breakdown of the treatments received by patients. It only mentioned that a variety of treatments were prescribed, including both topical and oral antifungal options.
In conclusion, our study updates the local epidemiology, diagnosis and treatment of patients with PF in Singapore. We found that the typical patient with PF from Singapore was a young man aged 21–30 years, with erythematous follicular papules or pustules over his trunk and back. Owing to the recalcitrant and persistent nature of the condition despite topical therapy, the use of oral antifungal agents may be considered as first-line treatment if lesions are extensive and symptomatic. With the high prevalence of PF in temperate climates, such as the one in Singapore, early recognition and diagnosis as well as prompt optimal management of PF are of paramount importance.
About the First Author

Dr Adeline Yong is presently an Associate Consultant in the Division of Dermatology at the Department of Medicine, National University Hospital, Singapore. She attained the OCBC Undergraduate Scholarship and received her Bachelors of Medicine and Surgery from the Yong Loo Lin School of Medicine, National University of Singapore. Subsequently, she did her training in Internal Medicine under the National University Health System Internal Medicine Residency Programme. She obtained membership of the Royal College of Physicians (MRCP UK) in 2016. Thereafter, she did her Senior Residency Training under the National Healthcare Group Dermatology Residency Programme and attained specialist accreditation in dermatology. Having a strong inclination towards research, Dr Yong was also trained under the NUHS Research Residency Programme (RRP), where she was awarded the RRP Research Award (Merit) in 2020. Dr Yong has a keen interest in dermatologic surgery and skin cancer. She is also the Dermatology Undergraduate Director for the Yong Loo Lin School of Medicine, National University of Singapore.
REFERENCES
- 1.Lim KB, Giam YC, Tan T. The epidemiology of malassezia (pityrosporon) folliculitis in Singapore. Int J Dermatol. 1987;26:438–41. doi: 10.1111/j.1365-4362.1987.tb00586.x. [DOI] [PubMed] [Google Scholar]
- 2.Tu WT, Chin SY, Chou CL, et al. Utility of gram staining for diagnosis of malassezia folliculitis. J Dermatol. 2017;45:228–31. doi: 10.1111/1346-8138.14120. [DOI] [PubMed] [Google Scholar]
- 3.Song HS, Kim SK, Kim YC. Comparison between Malassezia Folliculitis and non-Malassezia Folliculitis. Ann Dermatol. 2014;26:598–602. doi: 10.5021/ad.2014.26.5.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prindaville B, Belazarian L, Levin NA, Wiss K. Pityrosporum folliculitis:A retrospective review of 110 cases. J Am Acad Dermatol. 2018;78:511–4. doi: 10.1016/j.jaad.2017.11.022. [DOI] [PubMed] [Google Scholar]
- 5.Parsad D, Saini R, Negi KS. Short term treatment of pityrosporum folliculitis with itraconazole. Indian J Dermatol Venereol Leprol. 1999;65:122–3. [PubMed] [Google Scholar]
- 6.Suzuki C, Hase M, Shimoyama H, Sei Y. Treatment Outcomes for Malassezia Folliculitis in the Dermatology department of a University Hospital in Japan. Med Mycol J. 2016;57:E63–6. doi: 10.3314/mmj.16-00003. [DOI] [PubMed] [Google Scholar]


