Abstract
INTRODUCTION
Few studies have investigated the factors that affect the relationship between body image dissatisfaction and disordered eating locally. Our study aimed to investigate the moderating effects of depression and anxiety levels on the body dissatisfaction-disordered eating link in Singapore.
METHODS
A total of 329 participants completed a set of questionnaires that included various scales pertaining to eating behaviours, body image, psychological distress and quality of life.
RESULTS
Participants were diagnosed with schizophrenia (47.4%), depression (46.8%) and substance use disorders (5.8%). Moderation analyses revealed that depression (F [9, 251] = 18.50, p < 0.001, R2 change = 0.021) and anxiety levels (F [9, 268] = 19.54, p < 0.001, R2 change = 0.014) were significant moderators of the relationship between body dissatisfaction and disordered eating scores. Subsequent multivariate linear logistic regression analyses showed that high disordered eating scores were significantly associated with lower physical (F [8, 273] = 9.59, R2 = 0.22, p < 0.001, β = −0.27, p < 0.001), psychological (F [8, 273] = 10.51, R2 = 0.49, p < 0.001, β = −0.27, p < 0.001), social (F [8, 256] = 6.78, R2 = 0.18, p < 0.001, β = −0.18, p = 0.004) and environment (F [8, 273] = 5.29, R2 = 0.13, p < 0.001, β = −0.19, p = 0.001) quality of life scores after controlling for sociodemographic covariates.
CONCLUSION
Greater effort should be dedicated to the screening of disordered eating behaviours in psychiatric outpatients presenting with greater psychological distress.
Keywords: body image dissatisfaction, disordered eating, multi-ethnic, negative affect, non-Western
INTRODUCTION
Disordered eating (DE) refers to a range of unhealthy patterns of eating behaviours, ranging from restrictive dieting and regular skipping of meals to binge eating.(1) While DE behaviours are common and generally benign, individuals who have DE may reflect subclinical eating behaviours; for example, they may present with some but not all the symptoms required to meet the criteria of a recognised and diagnosable eating disorder, such as anorexia nervosa, bulimia nervosa or binge eating disorder.(2,3) Previous studies suggest that the incidence of DE is higher than that of diagnosable eating disorders,(2) although they are generally less noticeable than the more severe presentation of recognised eating disorders.(4) Thus, individuals with DE rarely seek and receive clinical help. However, if left undetected and untreated, DE can have a negative impact on the individual’s physical, emotional and mental well-being, especially in the presence of a comorbid mental illness.(5)
In understanding the formation of DE behaviours, Striegel-Moore and Cachelin posited a theoretical model suggesting that these behaviours stem from the ‘restraint’ pathway involving the internalisation of societal ideals regarding body shape and thinness.(6) Hence, discrepancies between an individual’s actual body weight and the society-perceived ideal weight, reinforced by interpersonal, sociocultural and media-related factors, lead to patterns of unhealthy eating such as restrictive dieting.(6,7) Additional evidence suggests that body image dissatisfaction (BID), defined as a negative subjective evaluation of the weight and shape of one’s own body,(8) is associated with negative psychological outcomes of self-esteem, depression and anxiety.(9,10) Individuals with higher levels of BID engage in behaviours such as DE to alleviate the negative feelings associated with BID.(11) This was reflected in a study on non-help-seeking populations that suggested that feelings of anxiety and depression were potential moderators of the relationship between DE behaviours and BID.(12) Another model of DE identified early adverse experiences as a significant factor that predisposed participants to patterns of BID and DE behaviours in non-help-seeking settings.(13)
Among help-seeking populations, the prevalence of DE in patients with mental illness ranged between 4.1% and 43%.(14,15) One study suggested that girls presenting with depressive and anxiety disorders demonstrated behaviours within subclinical anorexia (restrictive eating) that were associated with higher levels of weight concerns.(5) BID among patients diagnosed with schizophrenia spectrum disorders underlies negative cognitions concerning body image, such as dullness in movement, powerlessness, lifelessness and fragility.(16) Despite the high prevalence of DE behaviours and BID in patients with mental illness, few studies have identified the relevant cognitions and factors that could potentially affect the relationship between these presentations.
It was previously assumed that Asian populations demonstrate lower levels of BID and DE behaviours than Western populations.(17) However, a proportionate reduction in this gap was observed with a country’s increasing levels of economic growth, industrialisation and urbanisation.(18) Therefore, this study aimed to explore the potential moderating effect of depression and anxiety levels on the relationship between BID and DE in patients with mental illness within a tertiary care psychiatric hospital in Singapore, specifically among those with schizophrenia spectrum disorders and depressive disorders, who typically constitute a large proportion of patients seen in this setting. Based on past research in a predominantly Western non-psychiatric sample population,(12) we hypothesised that depression and anxiety levels would moderate the association between BID and DE. This study also elucidated the association between DE and quality of life (QOL), as well as emotional and physical well-being.
METHODS
The sample included English-speaking outpatients aged 18–40 years who were diagnosed as having schizophrenia spectrum disorders, or depressive and substance use disorders (based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition) at the Institute of Mental Health (IMH), a tertiary care psychiatric hospital in Singapore. Patients who were unable to read and write in English and those diagnosed as having intellectual disability were excluded. As Singapore has a high literacy rate of English among younger populations, the patients recruited in this study were all English-speaking. The patients’ disorders were confirmed through medical records and were based on the clinician’s diagnosis.
The sample size for the study was estimated to be approximately 300, based on previous literature that established a 21% prevalence of DE in outpatients with severe and persistent mental illness, at a 95% confidence interval, while assuming 5% precision levels.(4)
A single-phase cross-sectional design was used to establish the presence of DE. After obtaining written informed consent from the participants, their height and weight were measured using a body mass index (BMI) measuring machine (Model B1000; Avamech, Singapore). All patients seen at the outpatient clinic have their BMI measured using this machine as a standard practice. Subsequently, the participants completed a questionnaire that included various scales pertaining to eating behaviours, body image, physical activity, smoking and alcohol behaviours, psychological distress (depression and anxiety) and QOL.
All study procedures and materials were approved by the relevant ethics and institutional review boards, namely the National Health Group Domain Specific Review Board and the IMH Clinical Research Committee. Participants aged 21 years and above provided written informed consent, whereas for those aged below 21 years, consent was obtained from a parent/legal representative.
Various tests were used to measure the various parameters in our study. The Eating Attitudes Test (EAT-26)(19) is a 26-item questionnaire that assesses a participant’s scores in three main domains: dieting, bulimia and food preoccupation, and oral control scales. A summation of scores across the three main domains gives the total score, and higher scores indicate higher levels of DE. The EAT-26 does not diagnose an individual with an eating disorder. However, those with high scores are advised to further consult a qualified healthcare professional. The EAT-26 has high internal consistency (a = 0.90)(19) and a Cronbach’s alpha of 0.86.(20) In our study, the Cronbach’s alpha for our sample was 0.88. Scores ≥ 20 were used as cut-offs, indicating at-risk eating behaviours.(19)
The Body Shape Questionnaire (BSQ8C)(21,22) is an eight-item questionnaire based on preoccupations of body shape and weight as well as their association with self-esteem and BID. The BSQ8C has high sensitivity and an internal consistency of 0.91.(23) Cronbach’s alpha was 0.93 for our sample.
Beck’s Anxiety Inventory (BAI)(24) is a 21-item questionnaire that measures the severity of anxiety in adults and adolescents on a four-point scale. The BAI focuses on the emotional, physiological and cognitive symptoms of anxiety. A total score was calculated for all 21 items, ranging between 0 (no anxiety) and 63 (severe anxiety). The BAI has high internal consistency (a = 0.92) and test-retest reliability (r = 0.75), and good concurrent and discriminant validities.(23) The Cronbach’s alpha for our study was 0.95.
Beck’s Depression Inventory (BDI)(25) is a 21-item questionnaire that assesses depression through attitudes and characteristics. A total score was calculated for all 21 items, ranging between 0 (no depression) and 63 (severe depression). The BDI has high internal reliability (a = 0.91) and convergent validity.(26) The Cronbach’s alpha for our study was 0.95.
Items on the sociodemographic questionnaire pertained to age, gender, ethnicity, educational level, marital status, employment status and personal/household income. The World Health Organization’s Quality of Life-BREF instrument (WHOQOL-BREF)(27) is a 26-item questionnaire that measures four domains of QOL, namely physical health, psychological health, social relationships and environment QOL. Previous studies have reported acceptable internal consistencies ranging from 0.66 to 0.80 between the subdomains, as well as good content and construct validities.(28) Cronbach’s alpha between the subdomains for the current sample ranged from 0.71 to 0.88.
Individuals with substance use disorders and depression were grouped as a single category prior to the main analysis, as an initial analysis of variance indicated that the BDI and BAI scores did not significantly differ between these two groups but differed significantly from those of participants with schizophrenia. At a descriptive level, t-tests were conducted between those with and without DE and between participants with schizophrenia and depression/substance use disorders to investigate whether they differed significantly in DE symptomatology, BID scores, depression, anxiety levels and QOL. Correlational analyses were conducted to understand the direction and strength of association between age, BMI, and the BDI, BAI, BSQ8C and EAT-26 scores. Subsequently, a PROCESS module version 3.3 by Hayes(29) was used to conduct multiple simple moderation analyses (Model 1) using SPSS to investigate whether BDI and/or BAI were significant moderators of the relationship between BSQ and EAT-26 scores. Owing to the exploratory nature of this study, BDI and BAI scores were analysed as continuous variables, whereby the minimum and maximum values of each moderator were PROCESS-defined and not based on predefined cut-off scores. Using the PROCESS module, the mean centres for all interaction terms were automatically created to account for possible multicollinearity.(30) Finally, multivariate linear logistic regression analysis was conducted to investigate the association between EAT-26 and the domains of QOL. Sociodemographic covariates of age, BMI, gender, marital status, educational level, ethnicity and diagnosis categories were controlled for moderation and multivariate linear logistic regression analysis. Associations and interactions were considered significant if the p-value was less than 0.05. All analyses were conducted in IBM SPSS version 23.0 (IBM Corp, Armonk, NY, USA). Missing data was deleted list-wise.
RESULTS
A total of 329 participants were recruited. The majority of participants were diagnosed with schizophrenia (47.4%), followed by depression (46.8%) and substance use disorders (5.8%). The mean age of the participants was approximately 28 (range 18–40) years. 83.3% of the participants were never married. 51.7% of the participants were male, with a mean BMI of 25.5 ± 5.5 kg/m2. The remaining 48.3% of participants, who were female, had a mean BMI of 25 ± 6.5 kg/m2. The majority of participants (68.4%) were of Chinese ethnicity; the rest were of Malay (17.0%), Indian (10.3%) and other (4.3%) ethnicities. With regard to the educational level, 1.8% of participants had primary or no education, 30.7% had secondary school-level education, 27.1% had pre-university education (i.e. A-levels, diploma and advanced diploma), 14.3% had vocational training and 20.1% had university or postgraduate degrees.
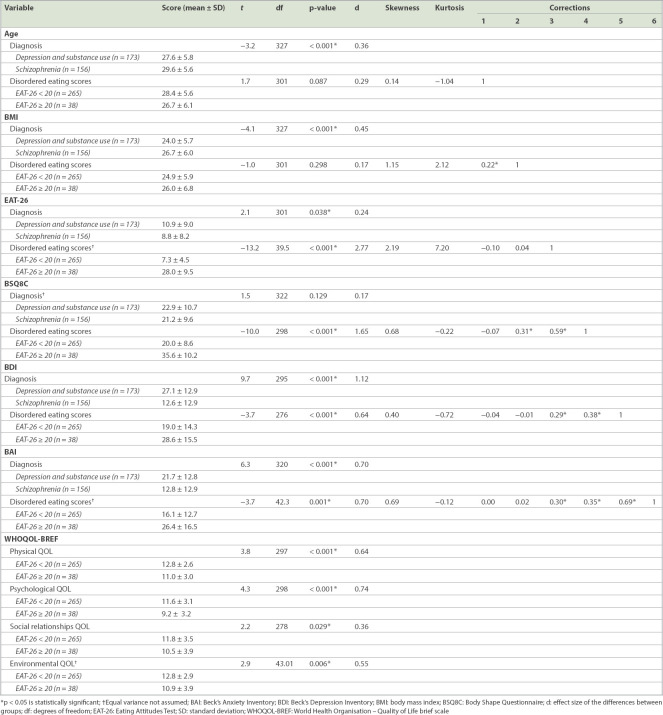
The results of the descriptive analysis and t-tests are summarised in Table I. Kurtosis and skewness statistics showed that all variables except for EAT-26 were normally distributed. Multiple t-tests showed that there were significant differences between depression/substance use disorders and schizophrenia with regard to EAT-26, BDI and BAI scores but not for BSQ8C scores. The mean EAT-26 score of the entire sample was 9.93 ± 8.70. Participants with DE (n = 38, EAT-26 score ≥ 20) had an average score of 27.90 ± 9.49, whereas those without DE (n = 265, EAT-26 score < 20) had an average score of 7.34 ± 4.53. Subsequent t-tests revealed that the EAT-26, BDI, BAI and BSQ8C scores were significantly greater for participants with DE (EAT-26 ≥ 20) than for those without DE (EAT-26 < 20). These differences had moderate-to-large effect sizes (d > 0.60). Participants with DE also had significantly lower levels of QOL scores in the psychological, social relationships and environment domains.
Table I.
Descriptive analysis of participants with and without disordered eating, and in different diagnostic categories.
Initial bivariate correlations indicated that EAT-26 scores were significantly and positively associated with BSQ8C, BDI and BAI scores, but not with BMI or age. Moderation analyses revealed that depression levels (BDI: F [9, 251] = 18.50, p < 0.001, R2 change = 0.021) and anxiety levels (BAI: F [9, 268] = 19.54, p < 0.001, R2 change = 0.014) were significant moderators of the relationship between BID scores (on BSQ8C) and DE (on EAT-26). The low and high levels were characterised at the 16th and 84th percentile levels, respectively, rather than as one standard deviation below and above the mean, as the former was less affected by the normality and shape of distribution.(29) The BSQ and EAT-26 association was found to be stronger at the low (16th percentile BDI: β = 0.31, standard error [SE] = 0.08, p = 0.0002, 95% confidence interval [CI] [0.15–0.47]; BAI: β = 0.37, SE = 0.07, p < 0.001, 95% CI [0.23–0.51]), mean (50th percentile BDI: β = 0.44, SE = 0.05, p < 0.001, 95% CI [0.34–0.55]; BAI: β = 0.46, SE = 0.051, p < 0.001, 95% CI [0.35–0.56]) and high (84th percentile BDI: β = 0.60, SE = 0.06, p < 0.001, 95% CI [0.48–0.73]; BAI: β = 0.56, SE = 0.06, p < 0.001, 95% CI [0.45–0.67]) percentiles of BDI or BAI levels.
As shown in Figs. 1 and 2, at the 16th, 50th and 84th percentile levels, BSQ8C and BDI/BAI together had a strengthening effect on DE, such that high BSQ8C and BDI/BAI levels were associated with higher DE. Upon inspection of these charts, the moderating effect of BDI appeared stronger than that of BAI, as indicated by the wider differences between each interpolation line. A stronger moderating effect of BDI could be attributable to sample characteristics, as this study recruited participants diagnosed with depression, and they may have presented with greater depression levels than anxiety levels at the point of the survey.
Fig. 1.
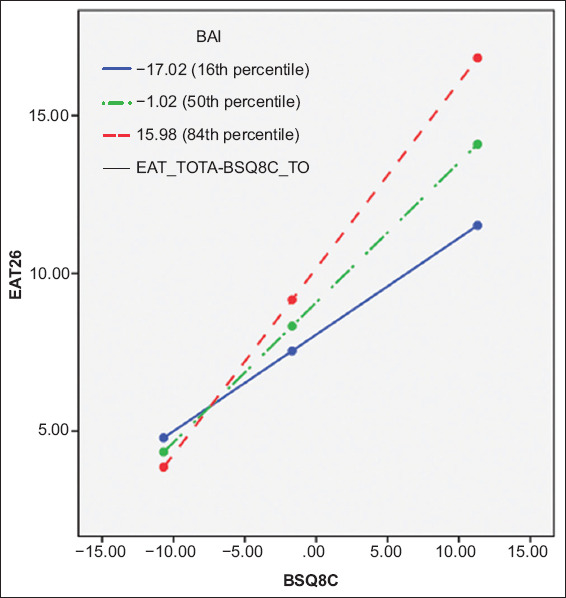
Graph shows interaction of body dissatisfaction (BSQ8C) and depression (BDI) levels. Disordered eating was measured using EAT-26. BDI: Beck’s Depression Inventory; BSQ8C: Body Shape Questionnaire; EAT-26: Eating Attitudes Test
Fig. 2.
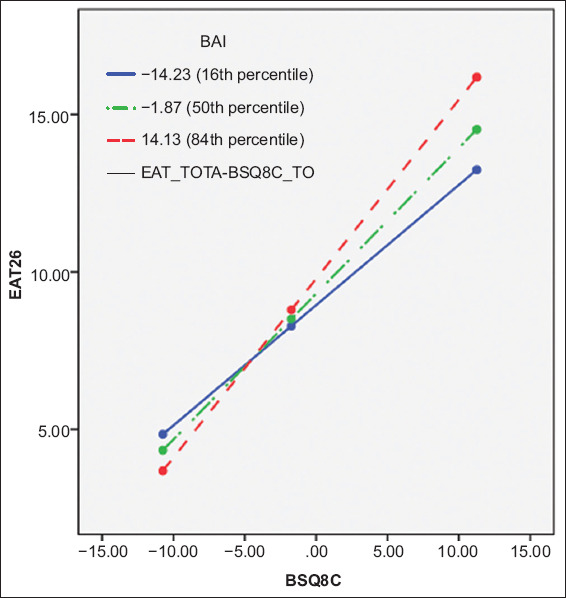
Graph shows interaction of body dissatisfaction (BSQ8C) and anxiety (BAI) levels. Disordered eating was measured using EAT-26. BAI: Beck’s Anxiety Inventory; BSQ8C: Body Shape Questionnaire; EAT-26: Eating Attitudes Test
Multivariate linear logistic regression analyses showed that high EAT-26 scores were significantly associated with lower physical QOL scores (F [8, 273] = 9.59, R2 = 0.22, p < 0.001, β = −0.27, p < 0.001), psychological QOL score (F [8, 273] = 10.51, R2 = 0.49, p < 0.001, β = −0.27, p < 0.001), social relationships QOL score (F [8, 256] = 6.78, R2 = 0.18, p < 0.001, β = −0.18, p = 0.004) and environment QOL score (F [8, 273]) = 5.29, R2 = 0.13, p < 0.001, β = −0.19, p = 0.001) after controlling for participant characteristics and sociodemographic covariates.
DISCUSSION
To the best of our knowledge, past studies were more commonly conducted in non-psychiatric, healthy and Western (predominantly Caucasian) populations(12,31) than in psychiatric non-Western populations. Our study aimed to replicate and extend past findings by exploring the potential moderating effects of depression and anxiety levels (negative affect) on the relationship between BID and DE in psychiatric outpatients residing in a multi-ethnic Asian setting.
Despite the clinical nature of our sample, our participants experienced levels of DE similar to those of a non-clinical and majority Caucasian student sample (mean EAT-26 score: 9.93 vs. 9.88).(32) DE scores were, on average, lower than those reported earlier in a majority Caucasian psychiatric sample (mean EAT-26 score: 9.93 vs. 12.2).(4) Despite multiple dissimilarities in sample characteristics with regard to the previously studied non-clinical and majority Caucasian populations, the patterns of associations between the variables in our study were similar to a great extent. For instance, in our study, participants with DE experienced significantly greater depression, anxiety levels and BID than those without DE did. There were no significant differences in BMI between the groups, which was also a finding similar to previous studies.(12)
The results of our study were consistent with past research conducted in the community, which reported that pre-existing levels of dissatisfaction with the body, in the presence of psychological distress, have a heightened effect on DE.(12,33) When depression or anxiety levels rise, BID will have a greater effect on DE. Conversely, when depression or anxiety level falls, the adverse effects of BID on DE will decrease. In addition to our findings, a recent qualitative study reported that BID was linked to sadness in women diagnosed with anorexia nervosa, which was coped with through restrictive eating and purging.(34) Rumination, a thought process that is intensified during negative mood and affect, has also been found to interact with BID, reinforcing and increasing binge eating behaviour among undergraduate students.(35) Consistent with cognitive behavioural theories of eating disorders, individuals feel compelled to engage in maladaptive behaviours such as DE to deal with aversive experiences that occur in the presence of negative affect and body schemas such as BID.(33)
DE and eating disorders in individuals with mental illness are under-recognised owing to a lack of specific screening.(36-38) Help-seeking individuals generally present more pressing issues at admission, and DE becomes a secondary concern.(4,37) However, when these concerns go unnoticed, the symptoms may become more chronic, which can negatively impact the efficacy of future treatment.(39-41) The importance of early screening is further supported by our finding that, locally, individuals with psychiatric disorders who also have DE (EAT-26 score ≥ 20) have significantly poorer QOL even after accounting for extraneous variables. Thus, our results emphasise the need to screen for eating attitudes in help-seeking individuals who experience high levels of depression or anxiety, as they may have a greater tendency to manifest DE attitudes, behaviours and, possibly, disorders. A previous study showed that individuals receiving treatment in a college counselling centre and counsellors were more likely to discuss DE when they were primed for it through the administration of the EAT-26 scale.(42) Further, this resulted in an increase in the diagnosis of eating disorders within the same period.(42)
This study relied heavily on self-reporting, which may be subject to unintended response bias, leading to an over- or underestimation of results. To recruit a large sample, we utilised self-reporting, as it reduces the labour of administration and is, therefore, more cost-effective. With this cost-effective method of self-reporting, we were firstly able to successfully recruit the large sample size required to achieve sufficient power to detect significance. Second, as our study was largely exploratory in nature, we focused only on simple moderating effects. Future research could extend our findings by investigating both the mediating and moderating roles of negative affect concurrently in DE and BID to further elucidate the complex roles assumed by them.
As previous studies were commonly conducted in the West and predominantly among the Caucasian population, the findings of earlier studies might not be generalisable to non-Western populations. To the best of our knowledge, this is the first study to explore the moderating effects of negative affect on the association between DE and BID in a large sample of psychiatric outpatients in a multicultural Asian setting. Consistent with expectations, levels of depression and anxiety each significantly moderated the BID and DE link. Further, participants with DE also had significantly lower QOL scores. Taken together, the findings of this study imply a need to screen for DE in psychiatric outpatients, especially those who experience high levels of negative affect, as they may have a tendency to experience DE during assessment as well.
ACKNOWLEDGEMENTS
This study was funded by the National Medical Research Council, Singapore, under Centre Grant Seed Funding. The authors declare no conflicts of interest.
REFERENCES
- 1.Eating Disorders Victoria. Disordered eating and dieting. [Accessed May 26, 2019]. Available at: https://www.eatingdisorders.org.au/eating-disorders-a-z/disordered-eating-and-dieting/
- 2.National Eating Disorders Collaboration. Disordered eating and dieting. [Accessed May 26, 2019]. Available at: https://www.nedc.com.au/eating-disorders/eating-disorders-explained/disordered-eating-and-dieting .
- 3.Solmi F, Hatch SL, Hotopf M, Treasure J, Micali N. Prevalence and correlates of disordered eating in a general population sample:the South East London Community Health (SELCoH) study. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1335–46. doi: 10.1007/s00127-014-0822-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Srebnik D, Comtois K, Stevenson J, et al. Eating disorder symptoms among adults with severe and persistent mental illness. Eat Disord. 2003;11:27–38. doi: 10.1080/10640260390167465. [DOI] [PubMed] [Google Scholar]
- 5.Touchette E, Henegar A, Godart NT, et al. Subclinical eating disorders and their comorbidity with mood and anxiety disorders in adolescent girls. Psychiatry Res. 2011;185:185–92. doi: 10.1016/j.psychres.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 6.Striegel-Moore RH, Cachelin FM. Body image concerns and disordered eating in adolescent girls:risk and protective factors. In: Johnson NG, Roberts MC, Worell J, editors. Beyond appearance:a new look at adolescent girls. Washington, DC: American Psychological Association; 1999. pp. 85–108. [Google Scholar]
- 7.Derenne JL, Beresin EV. Body image, media, and eating disorders. Acad Psychiatry. 2006;30:257–61. doi: 10.1176/appi.ap.30.3.257. [DOI] [PubMed] [Google Scholar]
- 8.Xu X, Mellor D, Kiehne M, et al. Body dissatisfaction, engagement in body change behaviors and sociocultural influences on body image among Chinese adolescents. Body Image. 2010;7:156–64. doi: 10.1016/j.bodyim.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 9.Steg L, Keizer K, Buunk AP, Rothengatter T, editors. Applied Social Psychology:Understanding and Managing Social Problems. Cambridge University Press; 2017. [Google Scholar]
- 10.Tiggemann M, Kuring JK. The role of body objectification in disordered eating and depressed mood. Br J Clin Psychol. 2004;43(Pt 3):299–311. doi: 10.1348/0144665031752925. [DOI] [PubMed] [Google Scholar]
- 11.Timko CA, Juarascio AS, Martin LM, Faherty A, Kalodner C. Body image avoidance:an under-explored yet important factor in the relationship between body image dissatisfaction and disordered eating. J Contextual Behav Sci. 2014;3:203–11. [Google Scholar]
- 12.Juarascio AS, Perone J, Timko CA. Moderators of the relationship between body image dissatisfaction and disordered eating. Eat Disord. 2011;19:346–54. doi: 10.1080/10640266.2011.584811. [DOI] [PubMed] [Google Scholar]
- 13.Vartanian LR, Smyth JM, Zawadzki MJ, Heron KE, Coleman SR. Early adversity, personal resources, body dissatisfaction, and disordered eating. Int J Eat Disord. 2014;47:620–9. doi: 10.1002/eat.22313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meng X, D'Arcy C. Comorbidity between lifetime eating problems and mood and anxiety disorders:results from the Canadian Community Health Survey of Mental Health and Well-being. Eur Eat Disord Rev. 2015;23:156–62. doi: 10.1002/erv.2347. [DOI] [PubMed] [Google Scholar]
- 15.Coker E, Telfer J, Abraham S. Perceived body weight, eating and exercise problems of different groups of women. Australas Psychiatry. 2012;20:390–6. doi: 10.1177/1039856212458982. [DOI] [PubMed] [Google Scholar]
- 16.Koide R, Iizuka S, Fujihara K, Morita N. Body image, symptoms and insight in chronic schizophrenia. Psychiatry Clin Neurosci. 2002;56:9–15. doi: 10.1046/j.1440-1819.2002.00925.x. [DOI] [PubMed] [Google Scholar]
- 17.Holmqvist K, Frisén A. Body dissatisfaction across cultures:findings and research problems. Eur Eat Disord Rev. 2010;18:133–46. doi: 10.1002/erv.965. [DOI] [PubMed] [Google Scholar]
- 18.Pike KM, Dunne PE. The rise of eating disorders in Asia:a review. J Eat Disord. 2015;3:33. doi: 10.1186/s40337-015-0070-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garner DM, Olmsted MP, Bohr Y, Garfinkel PE. The eating attitudes test:psychometric features and clinical correlates. Psychol Med. 1982;12:871–8. doi: 10.1017/s0033291700049163. [DOI] [PubMed] [Google Scholar]
- 20.Gleaves DH, Pearson CA, Ambwani S, Morey LC. Measuring eating disorder attitudes and behaviors:a reliability generalization study. J Eat Disord. 2014;2:6. doi: 10.1186/2050-2974-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Evans C, Dolan B. Body Shape Questionnaire:derivation of shortened “alternate forms”. Int J Eat Disord. 1993;13:315–21. doi: 10.1002/1098-108x(199304)13:3<315::aid-eat2260130310>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 22.Cooper PJ, Taylor MJ, Cooper Z, Fairbum CG. The development and validation of the body shape questionnaire. Int J Eat Disord. 1987;6:485–94. [Google Scholar]
- 23.Pook M, Tuschen-Caffier B, Brähler E. Evaluation and comparison of different versions of the Body Shape Questionnaire. Psychiatry Res. 2008;158:67–73. doi: 10.1016/j.psychres.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 24.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety:psychometric properties. J Consult Clin Psychol. 1988;56:893–7. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 25.Beck AT, Beck RW. Screening depressed patients in family practice. A rapid technic. Postgrad Med. 1972;52:81–5. doi: 10.1080/00325481.1972.11713319. [DOI] [PubMed] [Google Scholar]
- 26.Dozois DJA, Dobson KS, Ahnberg JL. A psychometric evaluation of the Beck Depression Inventory–II. Psychol Assess. 1998;10:83–9. [Google Scholar]
- 27.World Health Organization. WHOQOL-BREF Introduction, Administration, Scoring and Generic Version of the Assessment. Field Trial Version, December 1996. [Accessed May 26, 2019]. Available at: http://www.who.int/mental_health/media/en/76.pdf .
- 28.Trompenaars FJ, Masthoff ED, Van Heck GL, Hodiamont PP, De Vries J. Content validity, construct validity, and reliability of the WHOQOL-Bref in a population of Dutch adult psychiatric outpatients. Qual Life Res. 2005;14:151–60. doi: 10.1007/s11136-004-0787-x. [DOI] [PubMed] [Google Scholar]
- 29.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis:A Regression-Based Approach. 2nd ed. The Guilford Press; 2017. [Google Scholar]
- 30.Aiken LS, West SG. Multiple regression:testing and interpreting interactions. Thousand Oaks, CA: Sage Publications Inc; 1991. [Google Scholar]
- 31.Brannan ME, Petrie TA. Moderators of the body dissatisfaction-eating disorder symptomatology relationship:replication and extension. J Couns Psychol. 2008;55:263–75. [Google Scholar]
- 32.Tylka TL. The relation between body dissatisfaction and eating disorder symptomatology:an analysis of moderating variables. J Couns Psychol. 2004;51:178–91. [Google Scholar]
- 33.Williamson DA, White MA, York-Crowe E, Stewart TM. Cognitive-behavioral theories of eating disorders. Behav Modif. 2004;28:711–38. doi: 10.1177/0145445503259853. [DOI] [PubMed] [Google Scholar]
- 34.Espeset EM, Gulliksen KS, Nordbø RH, Skårderud F, Holte A. The link between negative emotions and eating disorder behaviour in patients with anorexia nervosa. Eur Eat Disord Rev. 2012;20:451–60. doi: 10.1002/erv.2183. [DOI] [PubMed] [Google Scholar]
- 35.Gordon KH, Holm-Denoma JM, Troop-Gordon W, Sand E. Rumination and body dissatisfaction interact to predict concurrent binge eating. Body Image. 2012;9:352–7. doi: 10.1016/j.bodyim.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 36.Mintz LB, O'Halloran MS. The Eating Attitudes Test:validation with DSM-IV eating disorder criteria. J Pers Assess. 2000;74:489–503. doi: 10.1207/S15327752JPA7403_11. [DOI] [PubMed] [Google Scholar]
- 37.Buckner ET. Do you have patients with anorexia or bulimia?Understanding is the first step in helping. Postgrad Med. 1991;89:209–12. doi: 10.1080/00325481.1991.11700874. 215. [DOI] [PubMed] [Google Scholar]
- 38.Striegel-Moore RH, DeBar L, Wilson GT, et al. Health services use in eating disorders. Psychol Med. 2008;38:1465–74. doi: 10.1017/S0033291707001833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reas DL, Williamson DA, Martin CK, Zucker NL. Duration of illness predicts outcome for bulimia nervosa:a long-term follow-up study. Int J Eat Disord. 2000;27:428–34. doi: 10.1002/(sici)1098-108x(200005)27:4<428::aid-eat7>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 40.Fichter MM, Quadflieg N, Hedlund S. Twelve-year course and outcome predictors of anorexia nervosa. Int J Eat Disord. 2006;39:87–100. doi: 10.1002/eat.20215. [DOI] [PubMed] [Google Scholar]
- 41.Vall E, Wade TD. Predictors of treatment outcome in individuals with eating disorders:a systematic review and meta-analysis. Int J Eat Disord. 2015;48:946–71. doi: 10.1002/eat.22411. [DOI] [PubMed] [Google Scholar]
- 42.Hoyt WD, Ross SD. Clinical and subclinical eating disorders in counseling center clients:a prevalence study. J College Stud Psychother. 2003;17:39–54. [Google Scholar]