Abstract
Objective
To determine the effectiveness of workplace exercise interventions in the treatment of musculoskeletal disorders.
Design
Systematic review of randomised controlled trials (RCTs).
Data sources
The bibliographical databases PubMed, CINAHL Plus, Cochrane, Scopus, ISI WoS and PeDRO were searched, with studies from 1 January 2010 to 31 December 2020 eligible for inclusion.
Eligibility criteria
We included RCTs, reported in English or Spanish, with at least an intervention group performing workplace exercises among office workers with musculoskeletal disorders.
Data extraction and synthesis
Two independent reviewers extracted data and assessed the risk of bias. A narrative synthesis was carried out with a tabular method specifying the study characteristics following the SWiM (Synthesis Without Meta-Analysis) guideline for synthesis without meta-analysis. The revised Cochrane Risk of Bias (RoB-2) tool was used to analyse the risk of bias of the included studies.
Results
Seven studies with a total of 967 participants met the inclusion criteria and were included in this review. Due to heterogeneity in different workplace exercise interventions, outcome measures and statistical analyses, it was not possible to conduct a meta-analysis and a narrative synthesis was performed. The interventions were classified into three categories: multiple body regions, neck and shoulder, and lower back. The seven studies concluded that workplace exercise interventions were effective in reducing musculoskeletal disorders and pain compared with other types of interventions or with control groups with no interventions. The RoB-2 tool found a high risk of bias in six of the seven studies.
Conclusions
The findings of the RCTs on workplace exercise interventions suggest that interventions were effective in treating musculoskeletal disorders among office workers. However, due to the high risk of bias of the included studies, no firm conclusions could be drawn and more high-quality studies are needed.
PROSPERO registration number
CRD42020177462.
Keywords: musculoskeletal disorders, pain management, occupational & industrial medicine, rehabilitation medicine
Strengths and limitations of this study.
The search strategy was developed in collaboration with an expert documentalist and included the following databases: PubMed, CINAHL Plus, Cochrane, Scopus, ISI WoS and PeDRO.
We ensured rigorous and consistent sets of inclusion and exclusion criteria.
This is an innovative review as it focuses only on exercise interventions among employees’ own workplaces, providing specific data on the most effective workplace exercise interventions (volume, intensity, time).
The review is limited by heterogeneity in study methodologies, interventions and outcome measures.
The risk of bias of the studies was high overall, making it difficult to draw firm conclusions.
Introduction
The exponential growth of sedentary lifestyle in the society is due to the great technological advances in recent years, increasing the time spent sitting throughout the day.1 2 Sitting, reclining and lying for a long time are sedentary behaviours with low energy expenditures (<1.5 Metabolic equivalent of tasks [METs]).3 It is important to note that sedentary behaviour and physical inactivity have different meanings,4 with the latter the result of performing an insufficient amount of moderate-intensity (3–6 METs) and vigorous-intensity (>6 METs) activity.3 It is therefore critical for strategies to improve physical activity and reduce sedentary behaviour in order to improve health.
American and Eastern Mediterranean countries have higher rates of physical inactivity, where 43% of the adult population do not reach the recommendations of the WHO physical activity guidelines (at least 150 min of moderate physical activity or 75 min of vigorous physical activity per week)5; the worldwide average is lower but surpasses 30%.6 Moreover, these numbers may be worse due to COVID-19, where home confinement and mobility restrictions are necessary to reduce the spread of the virus, increasing sedentary behaviour.7
Even though the association seems obvious, there is limited evidence that physically active individuals have less prevalence of chronic musculoskeletal complaints.8 More high-quality studies are required to determine the cause/effect of sedentary behaviour and its association with musculoskeletal pain.9 This condition is one of the leading causes of health problems among the global population, resulting in work disability, absenteeism and work presenteeism.10
Because the office workplace is an unfavourable environment in terms of high sedentary behaviour,11 daily exercise is crucial to prevent pathologies caused by lack of movement and poor posture while spending most of the workday in front of the computer.12 13 In a study by Kaliniene et al14 on 513 public service sector computer workers in Lithuania, the participants without rest breaks in their schedules had a higher prevalence (8.1%–13%) of musculoskeletal disorders in the elbow, wrist/hand, and upper and lower back than participants with rest breaks every 2 hours. This higher prevalence of pain is also due to working overtime, high quantitative and cognitive demands, and not taking breaks during work hours, increasing the total time spent in a seated position.14 15
Since productivity seems to be maintained by taking different standing breaks (from 5 min every 30 min of work to bouts of 50 s every 5 min of work) compared with not taking breaks in 1 hour of work,16 performing exercise interventions may help reduce the effect of sickness presenteeism on musculoskeletal complaints and work ability.17
Having a daily schedule for exercise interventions at work might help reduce the time spent sitting and increase the daily physical activity of employees,18 preventing cardiovascular and metabolic illnesses and reducing musculoskeletal disorders of the back.19
Strength and aerobic exercises that focus on reducing the intensity, disability and duration of neck and shoulder pain can be easily performed in work environments because they do not require equipment and can be performed according to the office worker’s own bodyweight.20 With regard to the type of exercises, the most common interventions are stretching and strength training exercises.21 22 Additionally, the practice of disciplines such as yoga23 or qigong24 has been implemented in the workplace, along with home-based sessions, and could be considered a feasible option in the treatment of musculoskeletal disorders related to job demands.
However, to our knowledge, this is the first systematic review to focus exclusively on workplace exercise interventions for treatment of musculoskeletal disorders among symptomatic office workers from any sector who spend most of their time in a seated position.
This review aims to:
Determine the effect of workplace exercise interventions on the treatment of musculoskeletal disorders.
Describe the characteristics of workplace interventions to improve therapeutic exercise programmes for office workers.
Recommend future lines of research to enhance interventions for a more active lifestyle among sedentary workers.
Methods
A systematic review of randomised controlled trials (RCTs) published in English and Spanish between 1 January 2010 and 31 December 2020 was conducted according to the standards of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).25 The study protocol provides more specific details.26
Data sources and search strategy
The search was generated using PubMed Medical Subject Headings (MeSH) terms and keywords related to office workers, musculoskeletal pain and exercise interventions. Subsequently, the search was adapted in the following databases: CINAHL Plus, Cochrane, Scopus, ISI WoS and PeDRO. The full search strategy for all databases is available in online supplemental file 1.
bmjopen-2021-054288supp001.pdf (57.3KB, pdf)
The strategy was reviewed in pairs and followed the criteria of the Peer Review of Electronic Search Strategies (PRESS) tool.27 Two reviewers (RP-P and CT-M) performed a peer review of all the retrieved records by title and abstract and then by full text using the Covidence tool.28
Inclusion criteria and study selection
The selection criteria for the review were as follows:
RCT articles with at least one intervention through exercise at work.
Studies with an entire sample carried out on office workers spending the majority of their working hours sitting.
Evaluation of musculoskeletal disorders or pain in all body regions or specific areas of the body.
Exercise interventions in the workplace, excluding those with exercises prescribed at home or outside the office setting.
Studies where the intervention is by means of ‘Sit-Stand Workstations’ or guidelines of ergonomics and health education without a physical exercise programme have been excluded.
Data extraction
Data extraction was performed by two reviewers (CT-M and CB) based on the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions.29 Data extraction was carried out in a standardised way, following the characteristics of the studies’ methodology, taking into account participants, interventions, outcome measures and the results. Consensus method was used to resolve differences between reviewers, and when differences were not resolved a third reviewer (FR-C) was consulted to reach full consensus.
Risk of bias assessment
The risk of bias of each article was independently assessed by two reviewers (FB, CT-M) using the Cochrane Risk of Bias 2 tool.30 The sections where there was no coincidence between the two reviewers needed a third opinion (FR-C) to reach a consensus.
Data synthesis
It was not possible to conduct a meta-analysis due to the significant heterogeneity in different workplace exercise interventions, the random-effects model of the outcome measures and the statistical analyses. A narrative synthesis was carried out following the Economic and Social Research Council’s guidance on conduct of narrative synthesis31 and the SWiM (Synthesis Without Meta-Analysis) checklist items.32 The results of the included studies were summarised and regrouped into three categories according to body regions. A preliminary synthesis was performed, presented in a common rubric through tabulation.
Patient and public involvement
There was no patient or public involvement.
Results
Results of the search
The search results yielded 276 articles after removing duplicates. After screening by title and abstract, 232 articles were excluded, resulting in a total of 44 full-text studies. The search followed the aforementioned specified inclusion and exclusion criteria. In total, seven studies were included. More detailed information is presented in the adapted PRISMA flow chart (figure 1).
Figure 1.
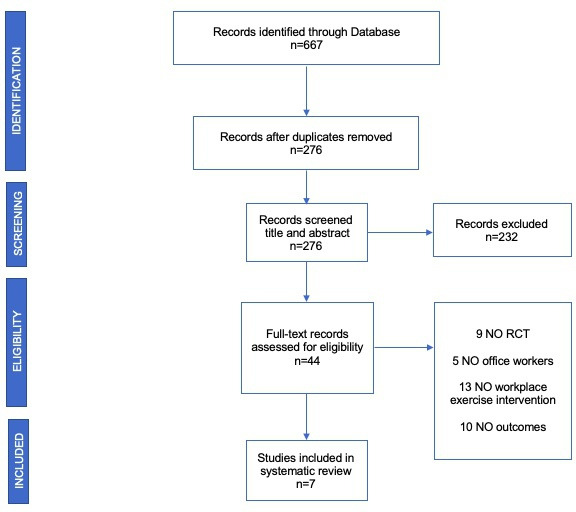
Flow diagram of trial selection, adapted from PRISMA. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; RCT, randomised controlled trial.
Characteristics of the studies
The seven studies that met the inclusion criteria were published from 2010 to 2018: Andersen et al33 and Marangoni34 in 2010, del Pozo-Cruz et al 35 in 2013, Nakphet et al36 and Andersen et al37 in 2014 Kaeding et al38 in 2017, and Shariat et al39 in 2018. A total of 967 participants were included in the seven studies, from the smallest sample of 30 participants36 to the largest sample of 549.33 A summary of the different interventions, the statistical analysis of the relevant outcomes and the results of the different studies are shown in table 1.
Table 1.
Summary of the results of the individual studies
| Authors | Country | Participants | Intervention group vs control | Relevant outcome | Results | Measurement tools | Adverse effect |
| Andersen et al33 | Denmark | n=549 (616 participants in the baseline test; 219 male, age: 45.7; 397 female, age: 44.6). |
|
There were main effects for region (F=3.04, p<0.0005), group (F=2.93, p=0.05) and status (F=905, p<0.0001). In relation to pain intensity, there was greater reduction in neck, low back, right elbow and right hand in the SRT and APE groups (p<0.0001–0.05). Also, APE compared with REF had a preventative effect on the development of pain symptoms in the right shoulder (p<0.05). Neck pain decreased in SRT (−0.73±0.36, p<0.05) and APE (−0.91±0.31, p<0.01). | Both SRT and APE for office workers produced better effects than the REF group in several regions of the upper body and in the number of pain regions in individuals with neck pain specifically. | Nordic Musculoskeletal Questionnaire, intensity of pain of 0–9 lasts 3 months. | No. |
| Andersen et al37 | Denmark | n=47 (10 male, 37 female), age: 44 (12), BMI: 25 (4). |
|
There was significant difference between groups in terms of pain in the neck/shoulder region (p<0.01). Also, PPT in the lower trapezius had an increase of 129 kPa (95% CI 31 to 227 kPa) (p<0.01). In terms of shoulder elevation and protraction strength, SFT showed an increased shoulder elevation strength of 7.7 kg (95% CI 2.2 to 13.3 kg) (p<0.01) more than the CG. | SFT reduces pain intensity and increases shoulder elevation strength in adults with chronic non-specific pain in the neck/shoulder region. | Self-rated pain intensity (0–9), PPT with algometer, maximal muscle strength with dynamometer, adherence. | No. |
| Marangoni34 | USA | n=68 (8 male, 60 female), age: 43 (21–62 years). |
|
There were significant improvements in reduction of pain in the intervention groups (CASP subjects VAS=−73%, PSA=−70%; FLIP subjects VAS=−64%, PSA=−62%) compared with CG, which slightly increased (VAS=1%, PSA=1%). | Positive effect on the reduction in pain in the intervention groups compared with the CG. No significant differences in the type of media used to prompt stretching exercises. | VAS and PSA, created by the author. | No. |
| Kaeding et al38 | Germany | n=41 (13 male, 28 female), age: 45.5 (9.1), BMI: 26.6 (5.2). |
|
There were significant differences regarding RMQ and ODI between groups (p=0.027) (t test p=0.002, ANCOVA p<0.001). Also the SF-36 physical scale (t test p=0.013, ANCOVA p=0.026) and the Freiburg Activity Questionnaire showed significant difference on Wilcoxon test (p=0.022). Sick leave also showed a difference (p=0.008). | WBV training seems to be an effective, safe and suitable intervention for seated working employees with CLBP. | RMQ, ODI, WAI, SF-36, Freiburg Activity Questionnaire, isokinetic performance, sick leave, posturography. | No. |
| del Pozo-Cruz et al35 | Spain | n=90 (24 male, 66 female), age: CG: 45.5 (7.02) and IG: 46.83 (9.13), with diagnosis of subacute Low Back Pain. |
|
In the intervention group, participants were more likely to exhibit improvements in functional disability (ODI clinical change 85%, p=0.001), risk of chronicity (SBST clinical change 75%, p<0.001) and most of the EQ-5D-3L components (VAS 73%, p<0.001; EQ-5D-3L utility score clinical change 78%, p<0.001; mobility 77%, p<0.001; self-care 79%, p=0.003; pain/discomfort 88%, p<0.001; and anxiety/depression 84%, p<0.001). | A web-based occupational intervention in a university administrative office is effective in improving quality of life and reducing the severity of low back pain. | VAS from the EQ-5D-3L, ODI, SBST. | No. |
| Shariat et al39 | Malaysia | n=142 (47 male, 95 female), age Exercise group: 29.41 (1.16); Ergonomic modification group: 28.31 (0.92); Combined group: 29.64 (0.9); and Control group: 28.74 (0.82). |
|
After 6 months, there were significant differences in pain scores for neck, right and left shoulder, and lower back: MD −10.55 (−14.36 to −6.74); MD −12.17 (−16.87 to −7.47); MD −11.1 (−15.1 to −7.09); MD −7.8 (−11.08 to −4.53) between exercise group and control group, and also between the combined group and control group in terms of pain in the neck, right and left shoulder, and lower back: MD −9.99 (−13.63 to −6.36); MD −11.12 (−15.59 to −6.65); MD −10.67 (−14.49 to −6.85); and MD −6.87 (−10 to −3.74). | Exercise modification was more effective in comparison with the ergonomic modification group after 4 months. | CMDQ. | No. |
| Nakphet et al36 | Thailand | n=30 female (18–40 years); Stretching group (SG): 31.4 (5.9); Dynamic contractions group (DCG): 29.6 (5.9); Reference group (RG): 27.6 (3.0). |
|
There was significant time effect on the myoelectric activity of the upper trapezius between three sessions of a 20 min computer typing task: F(1.59, 42.81)=5.35 (p=0.013). However, there were no significant differences between groups. | Positive effect on muscle discomfort in the three groups after the rest break interventions. Rest breaks with a variation in activities did not decrease the level of muscle electrical activity in the neck and shoulder muscles during computer work. |
SEMG, Borg’s Category- Ratio (CR-10) scale (0–10 scale for muscle discomfort); productivity=total number of correct words/overall time of typing. |
No. |
ANCOVA, Analysis of covariance; APE, all-round physical exercise; BMI, Body Mass Index; CASP, Computer Assisted Stretching Program; CG, control group; CLBP, chronic low back pain; CMDQ, Cornell Musculoskeletal Disorders Questionnaire; EQ-5D-3L, EuroQol - Five Dimensions Questionnaire - Three Level Version; FLIP, Facsimile Lesson with Instructional Pictures; IG, Intervention Group; MD, Mean deviation; ODI, Oswestry Disability Index; PPT, pressure pain threshold; PSA, pain spot assessment; REF, reference intervention without physical activity; RMQ, Roland-Morris Disability Questionnaire; SBST, STarT Back Screening Tool; SEMG, surface myoelectric activity; SF-36, Short Form 36; SFT, scapular function training; SRT, specific resistance training; VAS, Visual Analogue Scale; WAI, Work Ability Index Questionnaire; WBV, whole-body vibration training.
Interventions varied in each study, from 10 s to 15 s of stretch exercises every 6 min during work hours,34 to up to 1 hour of strengthening exercises with 2–3 sets of 10–15 repetitions combined with 5 s of static neck exercises once a week.33 A 3 min break intervention in Nakphet et al,36 with a dynamic contraction group and a stretching group, focused on the neck/shoulder region. Andersen et al and Shariat et al37 39 performed a 3-day-a-week intervention: Andersen et al37 with a 10–15 min stretching routine and Shariat et al39 with a 20 min strength routine with scapular training function. While Kaeding et al’s,38 employed whole-body interventions in 2.5 sessions a week of 15 min vibration training, del Pozo-Cruz et al35 performed physical exercise with postural stability strengthening, flexibility, mobility and stretching in 5-day-a-week sessions of 7 min each one.
With regard to the length of the interventions, many studies had medium-term and long-term interventions, except for Nakphet et al,36 where a 1-day intervention was performed to identify the acute effects of two workplace exercise interventions compared with a passive pause, and Marangoni,34 where a 3-week intervention was performed. The rest of the studies lasted from a 10-week intervention in the case of Andersen et al,37 to a 3-month intervention in Kaeding et al,38 to a 6-month intervention in Shariat et al,39 a 9-month intervention in del Pozo-Cruz et al35 and a 1-year intervention in Andersen et al.33
There is great variety in the comparison groups that sort from strategies to increase physical activity levels and to improve health and work conditions in Andersen et al.33 Access to standard care in del Pozo-Cruz et al.35 Ergonomic modifications in Shariat et al.39 A passive pause in Nakphet et al.36 And no-treatment groups in Marangoni et al, Andersen et al, Kaeding et al and Shariat et al.34 37–39
Risk of bias
All studies, except for Andersen et al,33 had a ‘high risk’ of bias in terms of ‘measurement of the outcome’ because the participants and/or the instructors were not blinded. In Andersen et al,33 the participants were blinded through cluster randomisation and replied to internet-based questionnaires.
In Marangoni, Nakphet et al and Shariat et al,34 36 39 we found ‘some concerns’ in the ‘selection of the reported results’ due to lack of a ‘prespecified analysis plan’. Although all studies were randomised, in the study of Nakphet et al,36 the type of randomisation was not specified and the ‘randomisation process’ was considered ‘high risk’. Another section to highlight is evaluating ‘missing the outcome data’. Despite finding five articles with low adherence to the intervention only in Andersen et al and Shariat et al the cause of the dropout was documented.37 39 In Andersen et al,33 there was no information on why the participants dropped out of the study, while Marangoni34 did not specify the number of participants or the reason for dropout, showing a ‘high risk’ of bias in this aspect. A summary of the risk of bias is shown in figures 2 and 3.
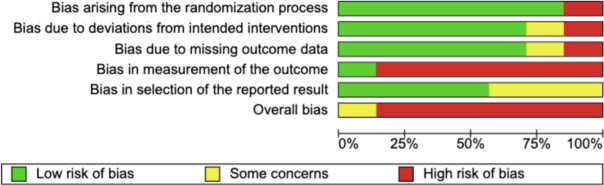
Figure 2.
Risk of bias graph. Review authors’ judgements of the risk of bias items are presented as percentages across the included randomised controlled trials.
Figure 3.
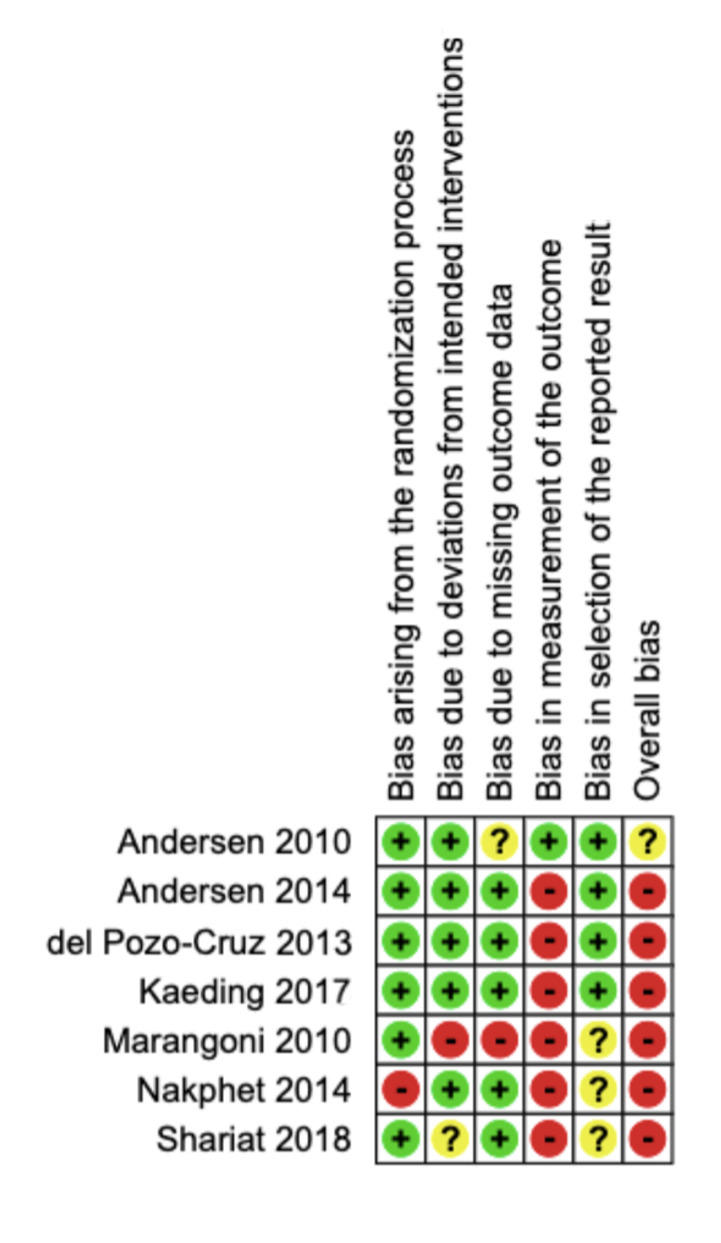
Risk of bias summary: review authors’ judgements of each risk of bias item for each included study. Green: low risk; yellow: some concerns; and red: high risk.
Effectiveness of workplace exercise interventions in reducing musculoskeletal disorders and pain
In Andersen et al, Marangoni and Shariat et al,33 34 39 reduction in musculoskeletal pain among office workers was assessed in multiple body parts. Nakphet et al and Andersen et al36 37 focused on the neck and shoulder area, while del Pozo-Cruz et al and Kaeding et al35 38 assessed workplace interventions in terms of disability caused by lower back pain.
Effectiveness of workplace exercise interventions in reducing musculoskeletal disorders in multiple body regions
As mentioned above, Andersen et al, Marangoni and Shariat et al33 34 39 evaluated the effectiveness of workplace exercise interventions in reducing musculoskeletal pain in more than one specific region. In Andersen et al,33 the Nordic Musculoskeletal Questionnaire was used to measure musculoskeletal symptoms, while the Visual Analogue Scale (VAS) was used to measure participants’ pain perception. Pain intensity was significantly reduced in the neck, lower back, right elbow and right hand in the two interventions with exercise and physical activity compared with the reference group (p<0.0001–0.05) (main effects for region: F=3.04, p<0.0005; group: F=2.93, p=0.05; and status: F=905, p<0.0001). In the feet region, the group where participants were encouraged to perform physical activity on their own showed greater reduction in pain perception than the workplace exercise intervention (p<0.001) and the reference group (p<0.05).
Marangoni’s34 exercise interventions found a positive effect on reducing pain in both intervention groups, Computer Assisted Stretching Program (CASP) and Facsimile Lesson with Instructional Pictures (FLIP) compared with the control group. VAS (CASP subjects=−73%; FLIP subjects=−64%) and a pain spot assessment created by the author (CASP subjects=−70%; FLIP subjects=−62%) were used to measure pain reduction among computer workers. There were no significant differences in pain reduction when using stretching exercises prompted by a software program (p<0.001) or a hard copy paper (p<0.001) when compared with the control group, which had a slight increase in pain of 1%.
The Shariat et al study39 found significant differences in pain reduction after 6 months of intervention using the Cornell Musculoskeletal Disorders Questionnaire in the group with exercise sessions compared with the control group without intervention in the neck (Mean Deviation [MD] −10.55; 95%CI −14.36 to −6.74), right shoulder (MD −12.17; 95%CI −16.87 to −7.47), left shoulder (MD −11.1; 95%CI −15.1 to −7.09) and lower back (MD −7.8; 95%CI −11.08 to −4.53). Additionally, significant differences were found between the combined group with exercises and ergonomic modification compared with the control group in the four regions: neck (MD -9.99; 95%CI −13.63 to −6.36), right shoulder (MD −11.12; 95%CI −15.59 to −6.65), left shoulder (MD −10.67; 95%CI −14.49 to −6.85) and lower back (MD −6.87; 95%CI −10 to −3.74). Measures were taken every 2 months, and the most significant improvement in pain reduction was experienced from months 4 to 6 in the exercise group (p<0.05).
Effectiveness of workplace exercise interventions in reducing musculoskeletal disorders and pain in the neck and shoulder region
Nakphet et al and Andersen et al36 37 carried out interventions where neck and shoulder pain was assessed. In Andersen et al’s study,37 there was a significant reduction in pain in the neck and shoulder region (p<0.01) and an increase in the lower trapezius pressure pain threshold (129 kPa, 95% CI 31 to 227 kPa, p<0.01) in the active pause group compared with the control group, which did not perform any intervention in the neck/shoulder region. No significant differences in the pressure pain threshold in the other body regions were measured.
In Nakphet et al,36 the Borg Scale for pain perception was used to assess pain, showing a reduction in neck discomfort in the three groups after each pause, without significant differences between the active pauses and the passive pauses intervention groups: neck: F(6.16, 83.16)=1.41, p=0.221; right shoulder: F(4.97, 67.11)=1.30, p=0.273; left shoulder: F(6.56, 88.54)=1.15, p=0.342; right elbow: F(6.78, 91.76)=0.91, p=0.500; left elbow: F(5.29, 71.36)=0.73, p=0.613; right wrist and hand: F(5.45, 73.55)=1.14, p=0.347; and left wrist and hand: F(4.86, 65.59)=1.39, p=0.242.
Effectiveness of workplace exercise interventions in reducing musculoskeletal disorders and pain due to disability caused by low back pain
The study of del Pozo-Cruz et al and Kaeding et al involved reducing disability and intensity of lower back pain.35 38 In Kaeding et al,38 using a whole-body vibration machine as the intervention, improvements in reducing lower back disability were reported compared with the control group with no intervention. There was a mean difference between the two groups of 1.8 points (95% CI 0.2 to 3.4, p=0.027) on the Roland-Morris Disability Questionnaire (RMQ), with an improvement in the training group of 1.5 (±2.6) RMQ points and with the control group worsening by an average of 0.3 (±2.6) RMQ points. Additionally, the Oswestry Disability Index and changes at the end of the intervention were significantly higher in the training group, with an improvement of 4.5 (±6.6) compared with a worsening of −1.2± (3.2) in the control group (p=0.002).
There was also a reduction in disability due to lower back pain in the del Pozo-Cruz et al study35 among participants who performed a physical exercise intervention, as measured by the Oswestry Disability Index, with a clinical change of 5.420 (1.707 to 17.216; 85%, p=0.001) compared with the control group. Additionally, there was a reduction in the risk of chronicity (STarT Back Screening Tool clinical change 75%, p<0.001) and in the EuroQol - Five Dimensions Questionnaire - Three Level Version (EQ-5D-3L) pain-related and disability-related components (VAS 73%, p<0.001; mobility 77%, p<0.001; self-care 79%, p=0.003; pain/discomfort 88%, p<0.001). However, the participants in the intervention group did not perceive an improvement in the performance of their daily tasks (p=0.103). Additionally, in the non-physical exercise group, an increase in disability and low back pain episodes was reported at the end of the intervention.
Discussion
Based on the results of the seven RCTs, exercise has significant benefits in treating musculoskeletal disorders of the lower back, neck and general regions of the body. There was a wide variety of exercise routines performed in the different interventions, with supervised or unsupervised programmes, in the different outcome measures, and in the number of participants with musculoskeletal disorders who participated in each study. There has also been found a diversity among control groups with no interventions, other exercise interventions and ergonomic advice. There is also a lack of consistency in the outcomes, which did not allow us to draw firm conclusions with regard to the effectiveness of workplace exercise interventions in treating musculoskeletal disorders.
The risk of bias of the trials was considered high overall, except for Andersen et al,33 which was the only study that blinded the instructor and the participants. The rest of the RCTs did not provide information regarding blinding of their participants or the exercise programme’s instructors, which is the most important aspect of quality assessment that can affect the internal validity of the results, despite being very complicated to implement in exercise interventions.40 With regard to external validity, it should be noted that the interventions were carried out at the workplace, except for the Nakphet et al study,36 where the office setting was simulated in a laboratory to carry out a 1-day intervention to gather data on the surface myoelectric activity of the targeted muscles. This might be a limitation as it is essential to carry out interventions at employees’ workspaces so that the results can be easily extrapolated to the population working in an office setting.41 More significant efforts should be made when carrying out participant recruitment and designing the intervention procedure, considering essential aspects to reduce biases such as blinding and loss to follow-up.42
As previously mentioned, one remarkable point of the review is the significant difference in the interventions that workers carried out in the different studies. The duration of the studies with physical exercise in clinical and non-clinical populations commonly ranged between 1 and 3 months, making the performance of the intervention and the economic costs viable.40
The reviewed studies showed no difference in exercise physiological adaptations between longer sessions with low weekly frequency and shorter sessions with a high weekly frequency; however, further investigation is required to draw firm conclusions. Mainenti et al12 showed that physical activity in a more extended session is not associated with decreased level of sedentarism. Therefore, using brief sessions with increased frequency each week could result in significant improvements among office workers without prolonged interruption in work activity.43
Evidence on workplace exercise interventions in the treatment of musculoskeletal disorders
As the inclusion criteria of the search, one of the key points was that the interventions should be done exclusively at the workplace. It is difficult to determine if the musculoskeletal disorders are work-related or whether there may be other leading causes. However, even in non-work-related musculoskeletal disorders, the implementation of workplace exercise interventions could help reduce symptoms that might worsen by prolonged sitting and working without rest breaks in their schedule.
Three studies that evaluated musculoskeletal pain in multiple body regions33 34 39 concluded that workplace exercise interventions reduced pain compared with the control groups. Rodrigues et al’s systematic review,44 which also included Marangoni’s study,34 found that with regard to the duration of the exercise programme, performing strength exercises in the workplace three times a week for 20 min could reduce musculoskeletal pain in the different regions of the spine and upper limbs. Another systematic review,45 which focused on video display terminal workers with musculoskeletal pain, used a rehabilitation programme with exercises, pain education and ergonomic adjustments and found a significant reduction in pain in different body areas, such as the wrist, shoulder and lower back regions.
However, analysing the best treatment for specific interventions in the neck and shoulder region in Bertozzi et al’s systematic review46 45has been found a significant overall effect supporting exercise therapies alone on the reduction of pain in the short and intermediate term. The two studies analysed in this review that focused on the neck and shoulder region showed benefits in terms of decreasing pain intensity and associated disability. Nakphet et al’s study36 concluded that taking a break during working hours, either with an exercise intervention or a passive pause, resulted in a reduction in pain perception. In Andersen et al,37 with a 10-week intervention, scapular function training with exercise reduced pain intensity in the neck and shoulder region. A previous systematic review20 reported a disparity in the results associated with differences between interventions aimed at treating neck disorders, concluding with strong evidence that interventions with strength and endurance programmes were more effective at reducing neck pain.
When focusing on the treatment of lower back pain among office workers, two studies concluded positive effects in reducing musculoskeletal pain; however, there was disparity between the workplace exercise interventions performed. The del Pozo-Cruz et al study35 consisted of a 9 min daily routine of strength, stretching and mobility exercises in a 9-month intervention, while Kaeding et al38 performed 2.5 sessions a week of whole-body vibration training with 10–15 min sessions during a 3-month intervention. These studies agree with the results of the study by Sipaviciene and Kliziene,47 which showed positive effects of performing stabilisation exercises for the trunk and of performing muscle strength exercise programmes to reduce lower back pain. Additionally, the systematic review by Gordon and Bloxham48 concluded that a general exercise programme with strength, flexibility and aerobic training would be beneficial in treating non-specific, chronic lower back pain in the adult population.
Adherence to the exercises prescribed using compliance terminology was reported in more than 80% of the total interventions performed in three of the seven studies analysed.35 37 38 There is no standardised definition of adherence to therapeutic exercises for musculoskeletal pain due to lack of consistency in the literature, finding other terminologies such as compliance or concordance.49
A standard definition of therapeutic adherence reported in the studies was noted by Bissonnette50: ‘Adherence can be defined as the extent to which patients follow the instructions they are given for prescribed treatments’. It is essential to consider the level of therapeutic adherence of participants with musculoskeletal pain when reporting the results of clinical trials.49 Considering that adherence to exercise is ordinarily low,51 52 strategies to enhance a higher rate of treatment adherence must be considered when designing intervention procedures. The del Pozo-Cruz et al35 web-based intervention used a log-in system with high compliance reported. Implementation of web-based interventions using customised push reminders via email or phone and regularly updating the content, such as in Edney et al’s study,53 is also effective. Additionally, no differences were found in the study of Gram and collaborators,54 where both the intervention groups improved in terms of reduced neck pain and headache with or without instructor supervision. A web-based programme with push reminders is likely a feasible option for future interventions.
Ambrose and Golightly55 conclude that any exercise regimen is better than a sedentary lifestyle as long as there is sustainable progression. Additionally, exercise induces analgesia in healthy people due to the pain inhibition mechanism as a result of endogenous opioids and nociception inhibitory mechanisms. However, in people with chronic pain, these reactions seem to not occur in the same way, and pain relief requires time after the initial increase in pain has been overcome.56 In Bravo et al’s study,57 where therapeutic exercises were performed among participants with fibromyalgia, a significant reduction in pain did not appear until 2 weeks after the intervention.
Hence, it is essential to consider specific items at the methodological level with a multidimensional approach58 59 in order to carry out interventions achieving a low dropout rate. With high compliance with exercise preferences, self-management and pain neuroscience education for treatment of musculoskeletal disorders.60 61
Study limitations
The present study was limited by the small number of RCTs available that performed workplace exercise interventions to treat musculoskeletal disorders. Only studies published in English and Spanish were analysed. Relevant articles published in other languages could be missed.
The great diversity in the methodological aspects of the different interventions performed in the trials could be a limitation. We found significant heterogeneity in the samples, in the type of interventions and in the period in which the studies’ pre/post interventions were carried out. Additionally, heterogeneity was found in the outcomes, which did not allow us to perform a meta-analysis due to the different outcome measures for musculoskeletal disorders and pain used in the studies.
Musculoskeletal conditions are a global concern.62 More studies are needed to draw firm conclusions in developed and developing countries, where different factors can predict musculoskeletal disorders among office workers.63 The studies included in the review were conducted in developed countries with high income33–35 37 38 and in developing countries with middle-upper income.36 39 Differences could be found when extrapolating results to low-income and middle-income countries, with the prevalence of musculoskeletal disorders rising exponentially.62
The review only focused on RCTs, excluding studies with interventions without a control group. There was a disparity in the control groups’ interventions among the analysed studies.
The sample size of the participants was low in the majority of the studies34–38 and some studies used non-validated scales,33 34 36 37 which could be additional limitations of this review.
Conclusions
The results of this systematic review suggest that workplace exercise interventions can effectively reduce musculoskeletal disorders in different body regions, such as the neck and shoulder, lower back, and upper limbs, compared with other groups of ergonomic guidelines or control groups without interventions. However, heterogeneity in the intervention characteristics, in the number of participants and in the outcome measures and the low methodological quality of the included studies restricted our ability to draw firm conclusions.
Improvement in the quality of studies is required to strengthen the current evidence on workplace exercise interventions among office workers. There were significant differences between the workplace programmes, such as in the exercises performed, the duration of the session and the weekly frequency. A consensus is needed to find structured therapeutic exercise programmes by following a proper methodological assessment that can be convenient for office workers and other similar sedentary professions.
Supplementary Material
Acknowledgments
The authors want to acknowledge the Research Group of Health Care (GRECS) - IRBLleida and the University of Lleida.
Footnotes
Contributors: This systematic review was developed and conceived by CT-M, who was involved in the entire process of writing the manuscript. CT-M and RP-P were involved in the review of the manuscript and contributed to the methodological aspects and the search strategy. CT-M, FB and FR-C were involved in the analysis of the Risk of Bias tool, CT-M and CB in data extraction and redaction of the results, and ERA acting as a guarantor of the overall content and involved in the supervision and quality assurance of the systematic review. All authors read and approved the final manuscript.
Funding: Serra Húnter Programme. Generalitat de Catalunya. Predoctoral staff in training Program University of Lleida, Jade Plus and La Caixa Bank Foundation 2019.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available. All data relevant to the study are included in the article or uploaded as online supplementary material.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study does not involve human participants.
References
- 1.Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obes Rev 2012;13:659–80. 10.1111/j.1467-789X.2011.00982.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Proper KI, Singh AS, van Mechelen W, et al. Sedentary behaviors and health outcomes among adults. Am J Prev Med 2011;40:174–82. 10.1016/j.amepre.2010.10.015 [DOI] [PubMed] [Google Scholar]
- 3.Tremblay MS, Aubert S, Barnes JD, et al. Sedentary behavior research network (SBRN) – terminology consensus project process and outcome. Int J Behav Nutr Phys Act 2017;14:1–17. 10.1186/s12966-017-0525-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rhodes RE, Mark RS, Temmel CP. Adult sedentary behavior: a systematic review. Am J Prev Med 2012;42:e3–28. 10.1016/j.amepre.2011.10.020 [DOI] [PubMed] [Google Scholar]
- 5.Bull FC, Al-Ansari SS, Biddle S, et al. World Health organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med 2020;54:1451–62. 10.1136/bjsports-2020-102955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hallal PC, Andersen LB, Bull FC, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012;380:247–57. 10.1016/S0140-6736(12)60646-1 [DOI] [PubMed] [Google Scholar]
- 7.Chandrasekaran B, Ganesan TB. Sedentarism and chronic disease risk in COVID 19 lockdown - a scoping review. Scott Med J 2021;66:3–10. 10.1177/0036933020946336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nilsen TIL, Holtermann A, Mork PJ. Physical exercise, body mass index, and risk of chronic pain in the low back and neck/shoulders: longitudinal data from the Nord-Trondelag health study. Am J Epidemiol 2011;174:267–73. 10.1093/aje/kwr087 [DOI] [PubMed] [Google Scholar]
- 9.Stefansdottir R, Gudmundsdottir SL. Sedentary behavior and musculoskeletal pain: a five-year longitudinal Icelandic study. Public Health 2017;149:71–3. 10.1016/j.puhe.2017.04.019 [DOI] [PubMed] [Google Scholar]
- 10.GBD 2016 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet 2017;390:1211–59. 10.1016/S0140-6736(17)32154-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ryan CG, Dall PM, Granat MH, et al. Sitting patterns at work: objective measurement of adherence to current recommendations. Ergonomics 2011;54:531–8. 10.1080/00140139.2011.570458 [DOI] [Google Scholar]
- 12.Mainenti MRM, Felicio LR, Rodrigues É de C, et al. Pain, work-related characteristics, and psychosocial factors among computer workers at a university center. J Phys Ther Sci 2014;26:567–73. 10.1589/jpts.26.567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Collins RM, Janse Van Rensburg DC, Patricios JS. Common work-related musculoskeletal strains and injuries. South African Family Practice 2011;53:240–6. 10.1080/20786204.2011.10874091 [DOI] [Google Scholar]
- 14.Kaliniene G, Ustinaviciene R, Skemiene L, et al. Associations between musculoskeletal pain and work-related factors among public service sector computer workers in Kaunas County, Lithuania. BMC Musculoskelet Disord 2016;17:1–12. 10.1186/s12891-016-1281-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mahmud N, Bahari SF, Zainudin NF. Psychosocial and ergonomics risk factors related to neck, shoulder and back complaints among Malaysia office workers. IJSSH 2014;4:260–3. 10.7763/IJSSH.2014.V4.359 [DOI] [Google Scholar]
- 16.Sheahan PJ, Diesbourg TL, Fischer SL. The effect of rest break schedule on acute low back pain development in pain and non-pain developers during seated work. Appl Ergon 2016;53 Pt A:64–70. 10.1016/j.apergo.2015.08.013 [DOI] [PubMed] [Google Scholar]
- 17.Gustafsson K, Marklund S. Consequences of sickness presence and sickness absence on health and work ability: a Swedish prospective cohort study. Int J Occup Med Environ Health 2011;24:153–65. 10.2478/s13382-011-0013-3 [DOI] [PubMed] [Google Scholar]
- 18.Parry S, Straker L, Gilson ND, et al. Participatory workplace interventions can reduce sedentary time for office workers--a randomised controlled trial. PLoS One 2013;8:e78957. 10.1371/journal.pone.0078957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kett AR, Sichting F. Sedentary behaviour at work increases muscle stiffness of the back: why roller massage has potential as an active break intervention. Appl Ergon 2020;82:102947. 10.1016/j.apergo.2019.102947 [DOI] [PubMed] [Google Scholar]
- 20.Sihawong R, Janwantanakul P, Sitthipornvorakul E, et al. Exercise therapy for office workers with nonspecific neck pain: a systematic review. J Manipulative Physiol Ther 2011;34:62–71. 10.1016/j.jmpt.2010.11.005 [DOI] [PubMed] [Google Scholar]
- 21.Sihawong R, Janwantanakul P, Jiamjarasrangsi W. A prospective, cluster-randomized controlled trial of exercise program to prevent low back pain in office workers. Eur Spine J 2014;23:786–93. 10.1007/s00586-014-3212-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ma C, Szeto GP, Yan T, et al. Comparing biofeedback with active exercise and passive treatment for the management of work-related neck and shoulder pain: a randomized controlled trial. Arch Phys Med Rehabil 2011;92:849–58. 10.1016/j.apmr.2010.12.037 [DOI] [PubMed] [Google Scholar]
- 23.Joshi VS, Bellad AS. Effect of yogic exercises on symptoms of musculoskeletal disorders of upper limbs among computer users: a randomised controlled trial. Indian J Med Sci 2011;65:424. 10.4103/0019-5359.109256 [DOI] [PubMed] [Google Scholar]
- 24.Phattharasupharerk S, Purepong N, Eksakulkla S, et al. Effects of Qigong practice in office workers with chronic non-specific low back pain: a randomized control trial. J Bodyw Mov Ther 2019;23:375–81. 10.1016/j.jbmt.2018.02.004 [DOI] [PubMed] [Google Scholar]
- 25.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tersa-Miralles C, Pastells-Peiró R, Rubí-Carnacea F, et al. Effectiveness of workplace exercise interventions in the treatment of musculoskeletal disorders in office workers: a protocol of a systematic review. BMJ Open 2020;10:1–5. 10.1136/bmjopen-2020-038854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McGowan J, Sampson M, Salzwedel DM, et al. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J Clin Epidemiol 2016;75:40–6. 10.1016/j.jclinepi.2016.01.021 [DOI] [PubMed] [Google Scholar]
- 28.Covidence . Covidence - Better systematic review management [Internet]. Cochrane, 2019. Available: https://www.covidence.org/home [Accessed 15 Jan 2020].
- 29.Higgins JPT G. Cochrane Handbook for systematic reviews of interventions. Wiley, 2008. [Google Scholar]
- 30.Sterne JAC, Savović J, Page MJ, et al. Rob 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 31.Popay J, Roberts H, Sowden A. Narrative synthesis in systematic reviews: a product from the ESRC methods programme. ESRC Methods Program 2006;2006:93. [Google Scholar]
- 32.Campbell M, McKenzie JE, Sowden A, et al. Synthesis without meta-analysis (swim) in systematic reviews: reporting guideline. BMJ 2020;368:l6890. 10.1136/bmj.l6890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Andersen LL, Christensen KB, Holtermann A, et al. Effect of physical exercise interventions on musculoskeletal pain in all body regions among office workers: a one-year randomized controlled trial. Man Ther 2010;15:100–4. 10.1016/j.math.2009.08.004 [DOI] [PubMed] [Google Scholar]
- 34.Marangoni AH. Effects of intermittent stretching exercises at work on musculoskeletal pain associated with the use of a personal computer and the influence of media on outcomes. Work 2010;36:27–37. 10.3233/WOR-2010-1004 [DOI] [PubMed] [Google Scholar]
- 35.del Pozo-Cruz B, Gusi N, del Pozo-Cruz J, et al. Clinical effects of a nine-month web-based intervention in subacute non-specific low back pain patients: a randomized controlled trial. Clin Rehabil 2013;27:28–39. 10.1177/0269215512444632 [DOI] [PubMed] [Google Scholar]
- 36.Nakphet N, Chaikumarn M, Janwantanakul P. Effect of different types of rest-break interventions on neck and shoulder muscle activity, perceived discomfort and productivity in symptomatic VDU operators: a randomized controlled trial. Int J Occup Saf Ergon 2014;20:339–53. 10.1080/10803548.2014.11077048 [DOI] [PubMed] [Google Scholar]
- 37.Andersen CH, Andersen LL, Zebis MK, et al. Effect of scapular function training on chronic pain in the neck/shoulder region: a randomized controlled trial. J Occup Rehabil 2014;24:316–24. 10.1007/s10926-013-9441-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kaeding TS, Karch A, Schwarz R, et al. Whole-Body vibration training as a workplace-based sports activity for employees with chronic low-back pain. Scand J Med Sci Sports 2017;27:2027–39. 10.1111/sms.12852 [DOI] [PubMed] [Google Scholar]
- 39.Shariat A, Cleland JA, Danaee M, et al. Effects of stretching exercise training and ergonomic modifications on musculoskeletal discomforts of office workers: a randomized controlled trial. Braz J Phys Ther 2018;22:144–53. 10.1016/j.bjpt.2017.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hecksteden A, Faude O, Meyer T, et al. How to construct, conduct and analyze an exercise training study? Front Physiol 2018;9:1007. 10.3389/fphys.2018.01007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hoffmann TC, Maher CG, Briffa T, et al. Prescribing exercise interventions for patients with chronic conditions. CMAJ 2016;188:510–8. 10.1503/cmaj.150684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Falagas ME, Grigori T, Ioannidou E. A systematic review of trends in the methodological quality of randomized controlled trials in various research fields. J Clin Epidemiol 2009;62:227–31. 10.1016/j.jclinepi.2008.07.012 [DOI] [PubMed] [Google Scholar]
- 43.Ting JZR, Chen X, Johnston V. Workplace-Based exercise intervention improves work ability in office workers: a cluster randomised controlled trial. Int J Environ Res Public Health 2019;16:2633. 10.3390/ijerph16152633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rodrigues EV, Gomes ARS, Tanhoffer AIP, et al. Effects of exercise on pain of musculoskeletal disorders: a systematic review. Acta ortop. bras. 2014;22:334–8. 10.1590/1413-78522014220601004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee DH, Kang B, Choi S, et al. Change in musculoskeletal pain in patients with work-related musculoskeletal disorder after tailored rehabilitation education: a one-year follow-up survey. Ann Rehabil Med 2015;39:726. 10.5535/arm.2015.39.5.726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bertozzi L, Gardenghi I, Turoni F, et al. Effect of therapeutic exercise on pain and disability in the management of chronic nonspecific neck pain: systematic review and meta-analysis of randomized trials. Phys Ther 2013;93:1026–36. 10.2522/ptj.20120412 [DOI] [PubMed] [Google Scholar]
- 47.Sipaviciene S, Kliziene I. Effect of different exercise programs on non-specific chronic low back pain and disability in people who perform sedentary work. Clin Biomech 2020;73:17–27. 10.1016/j.clinbiomech.2019.12.028 [DOI] [PubMed] [Google Scholar]
- 48.Gordon R, Bloxham S. A systematic review of the effects of exercise and physical activity on non-specific chronic low back pain. Health Care 2016;4:22. 10.3390/healthcare4020022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bailey DL, Holden MA, Foster NE, et al. Defining adherence to therapeutic exercise for musculoskeletal pain: a systematic review. Br J Sports Med 2020;54:326–31. 10.1136/bjsports-2017-098742 [DOI] [PubMed] [Google Scholar]
- 50.Bissonnette JM. Adherence: a concept analysis. J Adv Nurs 2008;63:634–43. 10.1111/j.1365-2648.2008.04745.x [DOI] [PubMed] [Google Scholar]
- 51.Crandall S, Howlett S, Keysor JJ. Exercise adherence interventions for adults with chronic musculoskeletal pain. Phys Ther 2013;93:17–21. 10.2522/ptj.20110140 [DOI] [PubMed] [Google Scholar]
- 52.Nielsen G, Wikman JM, Jensen CJ, et al. Health promotion: the impact of beliefs of health benefits, social relations and enjoyment on exercise continuation. Scand J Med Sci Sports 2014;24 Suppl 1:66–75. 10.1111/sms.12275 [DOI] [PubMed] [Google Scholar]
- 53.Edney S, Ryan JC, Olds T, et al. User engagement and attrition in an app-based physical activity intervention: secondary analysis of a randomized controlled trial. J Med Internet Res 2019;21:e14645. 10.2196/14645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gram B, Andersen C, Zebis MK, et al. Effect of training supervision on effectiveness of strength training for reducing neck/shoulder pain and headache in office workers: cluster randomized controlled trial. Biomed Res Int 2014;2014:1–9. 10.1155/2014/693013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ambrose KR, Golightly YM. Physical exercise as non-pharmacological treatment of chronic pain: why and when. Best Pract Res Clin Rheumatol 2015;29:120–30. 10.1016/j.berh.2015.04.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nijs J, Kosek E, Van Oosterwijck J, et al. Dysfunctional endogenous analgesia during exercise in patients with chronic pain: to exercise or not to exercise? Pain Physician 2012;15:ES205–13. [PubMed] [Google Scholar]
- 57.Bravo C, Skjaerven LH, Espart A, et al. Basic body awareness therapy in patients suffering from fibromyalgia: a randomized clinical trial. Physiother Theory Pract 2019;35:919–29. 10.1080/09593985.2018.1467520 [DOI] [PubMed] [Google Scholar]
- 58.McPhail SM, Schippers M, Marshall AL, et al. Perceived barriers and facilitators to increasing physical activity among people with musculoskeletal disorders: a qualitative investigation to inform intervention development. Clin Interv Aging 2014;9:2113. 10.2147/CIA.S72731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Meade LB, Bearne LM, Godfrey EL. "It's important to buy in to the new lifestyle": barriers and facilitators of exercise adherence in a population with persistent musculoskeletal pain. Disabil Rehabil 2021;43:468–78. 10.1080/09638288.2019.1629700 [DOI] [PubMed] [Google Scholar]
- 60.Devan H, Hale L, Hempel D, et al. What works and does not work in a self-management intervention for people with chronic pain? qualitative systematic review and meta-synthesis. Phys Ther 2018;98:381–97. 10.1093/ptj/pzy029 [DOI] [PubMed] [Google Scholar]
- 61.Louw A, Zimney K, Puentedura EJ, et al. The efficacy of pain neuroscience education on musculoskeletal pain: a systematic review of the literature. Physiother Theory Pract 2016;32:332–55. 10.1080/09593985.2016.1194646 [DOI] [PubMed] [Google Scholar]
- 62.Blyth FM, Briggs AM, Schneider CH, et al. The global burden of musculoskeletal Pain-Where to from here? Am J Public Health 2019;109:35–40. 10.2105/AJPH.2018.304747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Maakip I, Keegel T, Oakman J. Prevalence and predictors for musculoskeletal discomfort in Malaysian office workers: investigating explanatory factors for a developing country. Appl Ergon 2016;53 Pt A:252–7. 10.1016/j.apergo.2015.10.008 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-054288supp001.pdf (57.3KB, pdf)
Data Availability Statement
No data are available. All data relevant to the study are included in the article or uploaded as online supplementary material.