Abstract
Background
Prevention of child obesity is an international public health priority and believed to be effective when started in early childhood. Caregivers often ask for an early and structured response from health professionals when their child is identified with overweight, yet cost‐effective interventions for children aged 2–6 years and their caregivers in Child Health Services are lacking.
Objectives
To evaluate the effects and cost‐effectiveness of a child‐centered health dialogue in the Child Health Services in Sweden on 4‐year‐old children with normal weight and overweight.
Methods
Thirty‐seven Child Health Centers were randomly assigned to deliver intervention or usual care. The primary outcome was zBMI‐change.
Results
A total of 4598 children with normal weight (zBMI: 0.1 [SD = 0.6] and 490 children with overweight (zBMI: 1.6 [SD = 0.3]) (mean age: 4.1 years [SD = 0.1]; 49% females) were included. At follow‐up, at a mean age of 5.1 years [SD = 0.1], there was no intervention effect on zBMI‐change for children with normal weight. Children with overweight in the control group increased zBMI by 0.01 ± 0.50, while children in the intervention group decreased zBMI by 0.08 ± 0.52. The intervention effect on zBMI‐change for children with overweight was –0.11, with a 95% confidence interval of –0.24 to 0.01 (p = 0.07). The estimated additional costs of the Child‐Centered Health Dialogue for children with overweight were 167 euros per child with overweight and the incremental cost‐effectiveness ratio was 183 euros per 0.1 zBMI unit prevented.
Conclusions
This low‐intensive multicomponent child‐centered intervention for the primary prevention of child obesity did not show statistical significant effects on zBMI, but is suggested to be cost‐effective with the potential to be implemented universally in the Child Health Services. Future studies should investigate the impact of socio‐economic factors in universally implemented obesity prevention programs.
Keywords: child‐centered, child obesity, cost‐effectiveness, family therapy, prevention, primary care
1. INTRODUCTION
Childhood obesity is a worldwide problem and its prevalence has increased noticeably. In 2016, the World Health Organization estimated that worldwide 50 million children under five will have obesity by the year 2030. 1 In Sweden, the prevalence of obesity in 4‐year‐old children, born in 2014, was 2.2%, while 9.2% had overweight using the International Obesity Task Force (IOTF) definitions. 2 , 3 Childhood obesity reduces the child's mental and physical health and well‐being in both the short and the long term and is associated with increasing health care costs. 4 , 5 As child obesity tracks through to adulthood, prevention is an international public health priority. 1 , 6 , 7
Research suggests that the prevention of child obesity and early identification of overweight may be more effective when started in early childhood 1 , 5 and can contribute to the reduction of health inequalities. 4 , 8 A widely accepted indicator for the identification of obesity and overweight is the standardized body‐mass index, zBMI, as it helps to compare results among growing children of different ages and over time. 4 A zBMI reduction in the range of 0.25 is regarded as a suitable threshold of clinical importance in children 2–19 years old. 9
A recent systematic review of 39 randomized controlled trials (RCTs) for preventing obesity, mostly delivered in high‐income countries and at preschools, found that there is moderate evidence that multicomponent trials in children aged from 0 to 5 years reduce zBMI. 4 There are, however, few family‐based interventions involving both caregivers and children in the primary care setting for children aged 2–6 years that show an effect in reducing BMI and report on cost‐effectiveness. 4 , 10 Economic evaluations with a societal perspective, examining both direct costs, such as healthcare costs, and indirect costs, such as caregivers' time costs and productivity losses, are important for decision makers to be able to prioritize among increasingly limited public resources, even when the effect size of an intervention does not reach statistical significance. 5 , 11 , 12
From the family perspective studies show that caregivers want an early and structured response from health professionals when their child is identified with overweight, and they ask for easily understood information based on the needs and literacy level of the family. 13
Family‐based interventions for the management of overweight in young children should be universal, framed around protective factors and engage caregivers for social support to provide structure in favor of healthier eating, activity, and sleep behaviors in the home environment. 14 , 15 , 16
Child Health Services (CHS) during early childhood have great potential to serve as an arena for the promotion of healthy lifestyle and the prevention of obesity, because they reach the whole population and their health professionals have regular contact with children and families over time. 17 , 18 In Sweden, CHS are free of charge and offer a national Child Health Program (CHP) consisting of 18 scheduled universal health visits to Child Health Centers (CHCs) in the primary care setting from birth to the age of six to all children, and extra visits according to need. 19 The 60‐minute universal 4‐years health visit includes surveillance of the child's health and development, a hearing and vision test, a health dialogue on child dietary and physical activity behaviors, and the identification of overweight and obesity calculating BMI. 20 Previous research shows, however, that attention to dietary and physical activity behaviors in children is infrequent at the 4‐years health visit in Swedish CHS and raises concern about the efficacy of prevention efforts against child obesity. 21 Also, the use of the BMI growth chart may be inconsistent and lack quality. 22 Nurses working in CHS lack uniform guidelines for the management of pre‐school children with overweight, which results in a number of consequences that vary from unnecessary extra visits for continuous observations of the child's weight development, to not identifying overweight at all. 23 There is a need for continuous training in the use of structured person‐centered family counseling that empowers families when a child is identified with overweight, yet no evidence‐based model exists for the management of overweight to prevent child obesity in the CHS. 23 , 24
To fill this gap a structured model was developed for the prevention of obesity that can be implemented in routine practices in CHS, the Child‐Centered Health Dialogue (CCHD).
This study aimed to evaluate the effects on zBMI‐change and cost‐effectiveness of this child‐centered intervention for the prevention of obesity in CHS in Sweden in 4‐year‐old children with normal weight and overweight.
We hypothesized that CCHD targeting 4‐year‐old children with normal weight and overweight would reduce zBMI more and that the delivery of this structured intervention would result in fewer unnecessary extra visits and referrals and therefore cost less than usual care.
2. METHODS
2.1. Study design
The study was designed as a cluster RCT, clustered on CHC level with two parallel conditions, (1) usual care and (2) intervention care, and guided by the Medical Research Council framework for development and evaluations of complex interventions. 25 The study registered at ClinicalTrials.gov (2016721LUC3) followed the CONSORT recommendations for RCTs and the CHEERS guidelines for economic evaluations. 26 , 27 The Swedish Ethical Review Authority (721 ⁄2016) approved the study.
2.2. Study settings
The trial took place in the southern county of Sweden, Skåne, where 146 CHC with about 100,000 children aged 0–6 years were registered. 28 In Skåne, the Care Need Index (CNI), a socioeconomic index, is used to allocate CHS resources. The CNI of each CHC is based on sociodemographic information on caregivers listed at the CHC: unemployment, low educational status, single status, children under age 5, high mobility, and born outside Europe. The index value is 1, and higher values are related to increased risk of ill health. 29 Before the start of this study, CNI varied between 0.32 and 2.60 among all CHCs in Skåne (mean 0.93), and the prevalence of overweight among 4‐year‐olds, born 2011, was 9.9% and of obesity 2.3%. 28
2.3. Participants
All CHCs (47) situated in two larger cities with a mean prevalence of overweight of 7.6% and an additional number of 16 CHCs in seven smaller nearby municipalities with a prevalence of overweight of at least 9% were found eligible for the study. 28 Thirty‐seven CHCs, 27 of them in larger cities and 10 in smaller municipalities, agreed to participate, including 92 nurses specialized in CHS. Twenty‐six CHCs comparable in both mean prevalence in overweight (7.8 and 8.6% respectively) and mean CNI (1.1 in both) declined, because of time restraints.
Inclusion criteria were children born between January 2013 and August 2014 that had normal weight or overweight at baseline and participated in the 4‐years health visit. Exclusion criteria were children that did not take part in the 4‐years health visit and those allocated to intervention care that did not receive the intervention, because the nurse was not trained in CCHD. Children whose caregivers actively opted out of the study and children with undocumented BMI at the 4‐years health visit discontinued participation. At baseline, each child's BMI was categorized as underweight, normal weight, overweight and obesity. 3
2.4. Usual care
Children and their caregivers attending CHCs allocated to usual care received the 4‐years health visit according to NCP. 20 They are henceforth described as the control group. The 4‐years health visit includes a health dialogue and identification of overweight using the IOTF definitions. 3 The nurses working in the Swedish CHS are guided in their work by the digital National Handbook for Child Health Services. 19 In spring 2016, the illustrations developed for CCHD 30 , 31 were published in the national handbook and nurses in Skåne received a 30‐minute introduction to the illustrations, but were not trained in the CCHD approach. They also received a traditional 120‐minute lecture on child overweight and the BMI growth chart, without possibility for discussion or reflection.
One questionnaire to describe usual care was distributed before the start of the RCT in May 2016 to all CHCs in Skåne and showed that 55% of nurses did not use a structured health dialogue at the 4‐years health visit and that the majority of the nurses perceived it as difficult to communicate with caregivers about overweight (>90%). 30 Results from the same questionnaire, answered by 171 nurses working at the 63 CHCs eligible for this study, showed that 33% did not offer extra visits to families where a child was identified with overweight, 55% offered one extra visit and 12% two or three extra visits. The nurses responded that 44% always and 42% sometimes referred children identified with overweight to a dietician or to a specialized overweight team.
As CHS is not responsible for treatment of diseases, children with obesity are referred to a multidisciplinary team consisting of a specialized nurse, a dietician and a pediatrician for treatment outside the primary care setting.
2.5. Intervention care
Children and their caregivers attending CHCs allocated to intervention care are henceforth described as the intervention group. According to the study protocol all 4‐year‐old children received CCHD at the 4‐years health visit. Children with overweight were offered the targeted part of CCHD and extra visits or a referral to an overweight team, dietician, or CHS psychologist on the caregiver's request. Children with obesity were referred to specialized care as described under Usual Care.
CCHD is a low‐intensive multicomponent child‐centered intervention based on a Logic model described elsewhere. 30 CCHD builds on a salutogenic family‐therapeutic solution‐focused approach which emphasizes a relationship based on trust and facilitates the family to allocate protective factors and make healthy choices. CCHD is furthermore based on Child Centered Care (CCC), which acknowledges children in their right to take active part in their own health care. 32 CCHD consist of two parts: (1) a universal part directed to all 4‐year‐olds, regardless of their weight, and their families and (2) a targeted part offered to families when the child is identified with overweight.
The universal part encompasses a 10‐minute structured dialogue between the 4‐year‐old, the caregivers, and the nurse using eight animated illustrations based on important healthy choices associated with a long term healthy lifestyle (fruit and vegetable consumption, drinking water, portion size, physical activity, tooth brushing and bedtime routines) 30 , 33 as well as a neutral discussion on the child's growth using the BMI growth chart. 34 Using illustrations and the BMI growth chart strengthens health literacy and enables family members to understand, use, and internalize health information. 35
The 45‐minute targeted part, the Family Guidance (FG), is offered 1 to 3 weeks after the universal health visit to children identified with overweight, their caregivers, and other adults important to the family. FG is inspired by Standardized Obesity Family Therapy (SOFT). 34 SOFT is an evidence‐based treatment model that engages family members through collaborative family support in either identifying already existing protective factors or finding changes in lifestyle that are sustainable. 34 FG is a continuation of the non‐judgmental discussion started during the first part of CCHD and acknowledges the complexity underlying the development of overweight and not blaming caregivers. 36 , 37 The nurse emphasizes concerns about the child's health and clarifies the importance of sustainable weight stabilization instead of weight loss and the advantage of small changes at an early age. 34 , 36 , 37
CCHD builds on trust and partnership to promote child health and offers caregivers the choice to receive additional extra visits or a referral, which is based on the knowledge that compulsory care without choice might not give sustainable healthy behaviors. 38 CCHD was tested for feasibility 30 , and both children 31 and caregivers 33 experienced active participation and supportive guidance in the health dialogue.
Nurses allocated to intervention care received an extra interactive 1‐day training in small groups in October–November 2016. The training, described elsewhere, 39 focused on how to promote child participation and how to apply a family‐therapeutic solution‐focused approach. 30 , 34 The training was followed by four tutorial sessions of one hour, once every two months. These tutorials were used to reflect on how to build trust with the family, how to contextualize and reframe into positive reflections and how to handle the challenges encountered in the early communication about overweight. 13 , 34 A nurse with experience of CHS and active in the development of CCHD was responsible for the training together with a nurse with 15 years' working experience with SOFT, who was also responsible for the tutorial sessions. The first author was present at the workshops, but was not responsible for the training.
2.6. OUTCOMES
2.6.1. Primary outcome
The primary outcome, zBMI‐change, was calculated using weight and height collected at baseline, at the 4‐years health visit, between January 2017 and November 2018 and then followed longitudinally until 12 months after the intervention. The follow‐up was at the 5‐years health visit, between January 2018 and December 2020.
2.6.2. Secondary outcomes
Secondary outcomes were BMI‐change and costs for delivery of care for children identified with overweight. The number of extra visits and the number of referrals to an overweight team, dietician, or CHS psychologist were collected retrospectively by the first author from the child's digital records in June 2020 (Profdoc Medical Office).
Additional data to calculate health costs and effects outside the health‐care sector were also collected from the child's records. Healthcare costs included nurses' time to deliver usual or intervention care as well as costs of the 1‐day training and tutorial sessions offered to the nurses executing CCHD. All costs were translated into monetary units by using average salary rates, including employers' contribution to social and collectively agreed private pensions. Indirect costs were caregivers' time costs and loss of production and were estimated using the number of caregivers present at the 4‐years health visit, ways of transport to the visit and type of leave of absence (Table S1a). Based on this information and the estimated distance between the CHC and the child's home, productivity loss was estimated for the hours the caregivers took part in CHS including estimated time for transport, times the average wage rate (Salary statistics Sweden), multiplied by approximately 1.5 in order to account for payroll taxes.
Development costs for CCHD are displayed in Table 3, but are excluded in the calculation of cost‐effectiveness, along with any other costs associated with research, evaluation or administration of the RCT. 12 Costs are displayed in euros using the average exchange rate from 2017 (1 euro = 9.631 SEK). 40
TABLE 3.
Unit costs and associated sources and assumptions for delivery of care, training in and development of CCHD
| Type of costs | Description | Costs | Sources | Assumption | |
|---|---|---|---|---|---|
| Delivery of care (both Intervention and Usual Care) | |||||
| 4y‐HV per child | |||||
| CHS nurse | 1 h | 34 €/324 SEK | Salary statistics Sweden | Average wage rate* time | |
| One caregiver | 1 h inclusive transport in time | 2.9 €/28 SEK | CCHD database | Wage rate* time | |
| Two caregivers | 1 h inclusive transport in time | 5.5 €/53 SEK | CCHD database | Wage rate* time | |
| Transport costs | 1 or 2 caregivers a | 3.2 €/31 SEK | CCHD database | Calculation invoices | |
| Costs 1 caregiver 4y‐HV | 40 €/383 SEK | ||||
| Costs 2 caregiver 4y‐HV | 42 €/408 SEK | ||||
| Family guidance (FG) (only intervention care) | |||||
| CHS nurse | 45 min | 25 €/243 SEK | Salary statistics Sweden | Average wage rate* time | |
| One caregiver | 45 min inclusive transport in time | 2.8 €/27 SEK | CCHD database | Wage rate* time | |
| Two caregivers | 45 min inclusive transport in time | 5.1 €/49 SEK | CCHD database | Wage rate* time | |
| Transport costs | 1 or 2 caregivers a | 3.2 €/31 SEK | CCHD database | Calculation invoices | |
| Costs 1 caregiver FG | 31 €/301 SEK | ||||
| Costs 2 caregiver FG | 34 €/323 SEK | ||||
| Extra HV (both intervention and usual care) | |||||
| CHS nurse | 30 min | 17 €/162 SEK | Salary statistics Sweden | Average wage rate* time | |
| One caregiver | 30 min inclusive transport in time | 1.9 €/18 SEK | CCHD database | Wage rate* time | |
| Two caregivers | 30 min inclusive transport in time | 3.5 €/34 SEK | CCHD database | Wage rate* time | |
| Transport costs | 1 or 2 caregivers a | 3.2 €/31 SEK | CCHD database | Calculation invoices | |
| Costs 1 caregiver FG | 22 €/211 SEK | ||||
| Costs 2 caregiver FG | 24 €/227 SEK | ||||
| Costs referrals (both intervention and usual care) | |||||
| Costs referral offered | 10 min administration CHS nurse | 5.6 €/54 SEK | Salary statistics Sweden | Average wage rate* time | |
| Overweight team | Unit cost team with physician | 926 €/8904 SEK | Health care pricelist | Average 2017 | |
| Dietician | Unit cost out‐patient dietician | 114 €/1093 SEK | Health care pricelist | Average 2017 | |
| CHS‐psychologist | Unit cost out‐patient psychologist | 116 €/1114 SEK | Health care pricelist | Average 2017 | |
| Workshop (WS) CCHD total costs (6 WS for 53 nurses) | 31 793 €/305 628 SEK | ||||
| CCHD nurse per WS | 8 h and preparation 4 h | 444 €/4270 SEK | CCHD database | Wage rate* time | |
| SOFT nurse per WS | 8 h and preparation 4 h | 416 €/4001 SEK | CCHD database | Wage rate* time | |
| Pediatrician per WS | 8 h and preparation 4 h | 868 €/8344 SEK | CCHD database | Wage rate* time | |
| CHS nurses | 8 h & preparation, 2 h | 338 €/3245 SEK | Salary statistics Sweden | Average wage rate* time | |
| Catering WS | Lunch, coffee/tea, snacks | 624 €/6000 SEK | CCHD database | Calculation based on invoices | |
| Transport nurses WS/TS | Public transport | 500 €/4810 SEK | CCHD database | ||
| Training venue | Hire for one day | 954 €/9175 SEK | CCHD database | ||
| Transport SOFT nurse | Public transport TS at 14 CHCs | 572 €/5500 SEK | CCHD database | ||
| Material pictures | Nutritional pictures used in SOFT | 880 €/8468 SEK | CCHD database | ||
| Tutorial sessions (TS) total costs (49 nurses in 14 TS groups) b | 9 773 €/93 944 SEK | ||||
| Participating CHS‐nurse | 4 TS of 1 h | 135 €/1298 SEK | Salary statistics Sweden | Average wage rate* time | |
| SOFT nurse per TS group | 4 TS of 1 h, transport 2,5 h per TS | 225 €/2167 SEK | CCHD database | Wage rate* time | |
| Totals costs WS and TS | 41 566 €/399 572 SEK | ||||
| Total training costs per nurse (49) | 799 €/7684 SEK | ||||
| Total training costs per child with overweight (238 in IG) | 175 €/1679 SEK | ||||
| Total training costs per child (303 in IG) | 14 €/132 SEK | ||||
| Development CCHD total costs | 18 220 €/175 151 SEK | ||||
| CCHD pictures | Illustrator eight pictures | 10819 €/104 000 SEK | Invoice | ||
| CCHD minibook | Illustrator | 2081 €/20 000 SEK | Invoice | ||
| Nurse (CCHD/SOFT) | Two nurses meeting 12 h | 860 €/8272 SEK | CCHD database | Wage rate* time | |
| Pediatrician | Meeting 3 h | 217 €/2086 SEK | CCHD database | Wage rate* time | |
| Preschool teacher | Meeting 3 h | 83 €/793 SEK | Salary statistics Sweden | Average wage rate* time | |
| Print illustrations | 100 sets of eight illustrations | 728 €/7000 SEK | Invoice | ||
Abbreviations: CCHD, child‐centered health dialogue; CHC, Child Health Centre; FG, Family Guidance; HV, health visit; CHS Child Health Services; SOFT Standardised Obesity Family Therapy.
aWhen two caregivers travelled to the CHC only 1.5% used public transport, therefore no difference in costs if one or two caregivers came to the visit.
bFive small CHC formed two bigger TS groups.
2.7. Sample size
To be able to detect a clinically important difference of 0.25 units in mean zBMI‐change 9 in 4‐year‐old children with overweight at the 12‐months follow‐up, with a power of 0.80 and a significance level of 5%, the sample of children with overweight should contain at least 250 children in each group. Assuming a mean prevalence of children with overweight of 10%, 28 at least 2500 4‐year‐old children were needed in each group. We did not include the expected intra‐cluster correlation coefficient (ICC) when power was calculated, but adjusted the outcomes for cluster effect afterwards.
2.8. Stratification and randomization
The 37 CHCs were first stratified according to CNI. CHCs below the mean CNI in Skåne in 2015 28 formed one stratum (<0.93) and those above formed a second stratum (≥0.93). The CHCs were then divided into groups that had either usual or intervention care (1:1), resulting in 18 CHC (43 nurses) in the control group and 17 CHC (49 nurses) in the intervention group (Figure 1). Random allocation was performed by the third author according to a computer‐generated randomization list. The allocation sequence was revealed to the first author, who contacted all CHCs. Two CHCs declined participation due to time restraints, one in the intervention and one in the control group, both stratified for CNI ≥0.93. As CCHD was delivered as part of routine practice in CHS and as children and their caregivers were informed about the study by an identical poster in the waiting and consultation room at all CHCs, children and caregivers could be considered blind to the allocation of their respective CHC.
FIGURE 1.
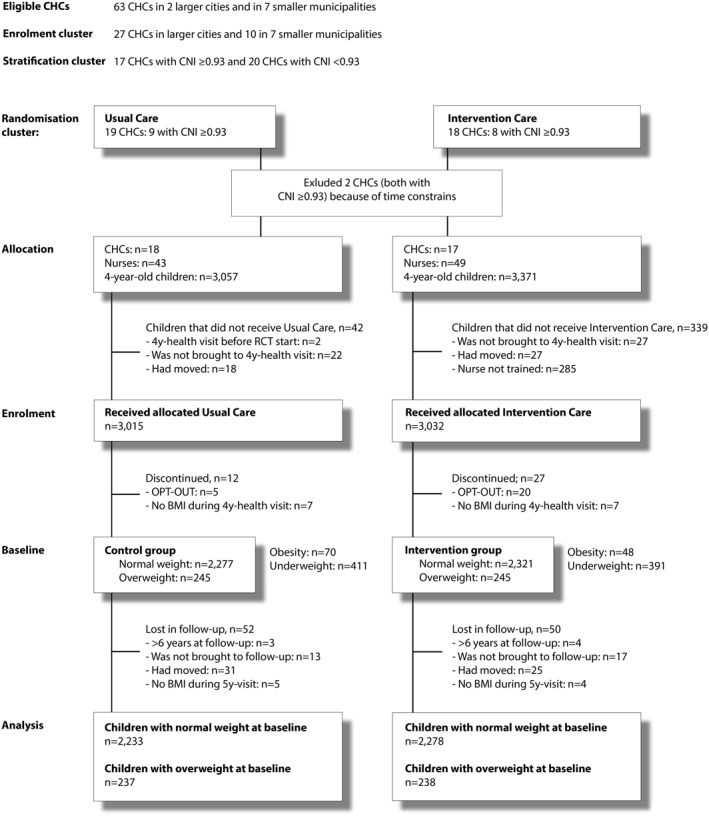
Flow diagram of the trial up to the 12‐months follow‐up
2.9. Statistical and economic analysis
Descriptive statistics were used to describe baseline characteristics. The effect of the intervention on zBMI‐change and BMI‐change for both normal weight children and children with overweight was analyzed using a linear mixed model to be able to adjust for clustering and secondly to adjust for baseline, gender, and CNI, since these were evaluated as possible confounding factors. ICC was calculated (ICC = cluster variance divided by residual plus cluster variance). Additionally, we performed sub‐analyses to demonstrate variations in intervention effects on the primary outcome based on gender and CNI. Analyses were performed in SPSS (IBM, SPSS Statistics, version 26).
As the delivery of care in children identified with overweight is the main difference between the control and intervention group, the economic analysis of the trial was performed in children with overweight at baseline. A wider societal perspective, looking at direct and indirect health care costs, was applied. Two types of effects were used as effectiveness indicators: (a) zBMI‐change and (b) BMI‐change. Incremental costs are the costs for delivery of care plus the costs for training per child with overweight in the intervention group minus the costs for delivery of care per child with overweight in the control group. The incremental cost‐effectiveness ratio (ICER) is the incremental costs divided by the difference in mean zBMI‐change or mean BMI‐change in the intervention and control group and is expressed as costs per 0.1 zBMI and in costs per 1 BMI unit prevented.
3. RESULTS
A flow diagram (Figure 1) describes the flow of participants, the exclusions and losses to follow‐up. Table 1 contains the distribution in weight categories for all 4‐year‐olds and descriptive characteristics at baseline in children with normal weight and overweight in the control group and in the intervention group. The mean age at follow‐up was 5.1 years [SD = 0.1] for children with normal weight and overweight in both the control and the intervention group (Table 2).
TABLE 1.
Characteristics at baseline for all 4‐year‐olds, specifically for children with normal weight and overweight
| All 4‐year‐old children | CG n = 3003 | IG n = 3005 |
|---|---|---|
| zBMI | 0.07 ± 1.02 | 0.07 ± 0.98 |
| BMI (kg/m2) | 15.82 ± 1.42 | 15.83 ± 1.34 |
| Overweight a | 245 (8.2) | 245 (8.2) |
| Normal weight | 2277 (75.8) | 2321 (77.2) |
| Obesity | 47 (1.6) | 30 (1.0) |
| Morbid obesity | 23 (0.8) | 18 (0.6) |
| Underweight grade I | 326 (10.9) | 306 (10.2) |
| Underweight grade II & III | 84 (2.8) | 86 (2.8) |
| All 4‐year‐old children with normal weight | CG n = 2277 | IG n = 2321 |
|---|---|---|
| zBMI | 0.10 ± 0.58 | 0.11 ± 0.59 |
| BMI (kg/m2) | 15.78 ± 0.77 | 15.81 ± 0.78 |
| Age (years) | 4.1 ± 0.11 | 4.0 ± 0.09 |
| Female | 1120 (49.2) | 1099 (47.4) |
| CNI ≥ 0.93 b | 1102 (48.4) | 1004 (43.3) |
| All 4‐year‐old children with overweight | CG n = 245 | IG n = 245 |
|---|---|---|
| zBMI | 1.64 ± 0.27 | 1.62 ± 0.25 |
| BMI (kg/m2) | 18.09 ± 0.48 | 18.05 ± 0.44 |
| Age (years) | 4.1 ± 0.13 | 4.1 ± 0.10 |
| Female | 132 (53.9) | 133 (54.3) |
| CNI ≥ 0.93 b | 131 (53.5) | 126 (51.4) |
| Distance to CHC (km) | 3.9 ± 5.1 | 3.9 ± 5.7 |
Note: Data are presented as mean ± SD values or n (%). The bold signifies that only children with normal weight and overweight are included in the analysis.
Abbreviations: CG, Control Group: IG Intervention Group.
Each child's BMI categorized using IOTF definitions.
CNI ≥ 0.93 is related to risk of ill health.
TABLE 2.
MD in primary (zBMI‐change) and secondary (BMI‐change) outcomes in the control and the intervention group, adjusted for clustering and adjusted for baseline, CNI and gender
| Children with normal weight at baseline | CG | IG | Adjusted for Cluster MD (95% CI) | p | Adjusted for Cluster, baseline, CNI, gender MD (95% CI) | p |
|---|---|---|---|---|---|---|
| (n = 2233) | (n = 2278) | |||||
| zBMI‐change | 0.06 ± 0.48 | 0.04 ± 0.46 | −0.03 (−0.09–0.03) | p = 0.33 a | −0.03 (−0.09–0.03) | p = 0.35 a |
| BMI‐change | −0.11 ± 0.68 | −0.14 ± 0.68 | −0.04 (−0.13–0.04) | p = 0.30 a | −0.04 (−0.12–0.04) | p = 0.33 a |
| zBMI at follow‐up | 0.17 ± 0.72 | 0.16 ± 0.72 | ||||
| BMI at follow‐up | 15.67 ± 1.02 | 15.67 ± 1.01 | ||||
| Age at follow‐up | 5.1 ± 0.11 | 5.1 ± 0.12 |
| Children with overweight at baseline | (n = 237) | (n = 238) | ||||
|---|---|---|---|---|---|---|
| zBMI‐change | 0.01 ± 0.50 | −0.08 ± 0.52 | −0.11 (−0.23–0.008) | p = 0.066 b | −0.11 (−0.24–0.01) | p = 0.069 b |
| BMI‐change | 0.01 ± 1.02 | −0.18 ± 1.01 | −0.22 (−0.45–0.007) | p = 0.057 a | −0.21 (−0.44–0.01) | p = 0.065 b |
| zBMI at follow‐up | 1.66 ± 0.58 | 1.54 ± 0.56 | ||||
| BMI at follow‐up | 18.11 ± 1.18 | 17.87 ± 1.10 | ||||
| Age at follow‐up | 5.1 ± 0.12 | 5.1 ± 0.12 |
Abbreviations: CG Control Group; IG Intervention Group; MD Mean difference.
Intra‐cluster correlation coefficient (ICC) = 0.02.
ICC = 0.03.
3.1. Primary outcome
At follow‐up children with normal weight at baseline had a mean difference (MD) in zBMI‐change adjusted for clustering, baseline, gender and CNI of −0.03 (95% CI: −0.09 to 0.03; p = 0.35). Children with overweight at baseline had a MD in zBMI‐change adjusted for clustering, baseline, gender and CNI of −0.11 (95% CI: −0.24 to 0.01; p = 0.07) (Table 2). Children in the control group with overweight at baseline had slightly increased their zBMI by 0.01 ± 0.50, whereas children with overweight in the intervention group had decreased their zBMI by 0.08 ± 0.52 at follow‐up (Table 2).
3.2. Secondary outcomes
The BMI‐change at follow‐up is presented in Table 2. In the subgroup analysis by gender, the effect on zBMI‐change varied in females compared to males (clustering‐adjusted MD = −0.14, 95% CI: −0.28 to 0.005, p = 0.058 vs. MD = −0.06, 95% CI: −0.16 to 0.11; p = 0.50). Females in the control group increased their zBMI, whereas females in the intervention group decreased their zBMI. Males in the control group did decrease their zBMI, but less than in the intervention group (Table S2). In the subgroup analysis by CNI the effect on zBMI‐change was larger in children visiting CHCs with a CNI < 0.93 (clustering‐adjusted MD = −0.14, 95% CI: −0.31 to 0.03, p = 0.09) than those at CHCs with a CNI ≥ 0.93 (clustering‐adjusted MD = −0.09, 95% CI: −0.30 to 0.12; p = 0.34), but in both subgroups the effects were favorable for the intervention group (Table S2).
3.3. Delivery of care and cost‐effectiveness
3.3.1. Costs for delivery of care for children with overweight at baseline
Costs were calculated separately for the 4‐years health visit, FG, extra health visits and for administration of a referral. Costs were calculated depending on whether one or two caregivers participated (Table 3). Costs for referrals were calculated based on physical units of healthcare obtained from the Swedish southern regional healthcare pricelist for the year 2017 (Table 3).
3.3.2. Cost of training in CCHD
In total, 53 nurses from 17 CHCs received a 1‐day workshop in CCHD. Five workshops were conducted in autumn 2016, four with an average of 10 participants and one for four newly recruited nurses in autumn 2017. After the workshop 49 nurses were offered four tutorial sessions at their workplace. Three smaller CHCs joined another CHC, resulting in only 14 tutorial groups.
The total costs for the training in CCHD were 41,566 euros and 799 euros per nurse. The costs for training per child were 14 euros (total costs divided by all 3032 children that received CCHD). Calculated for 238 children with overweight the cost for training per child with overweight was 175 euros (Table 3).
3.3.3. Delivery of care for children with overweight at baseline according to the child records
In the control group 55 children (23.2%) with overweight according to the IOTF definitions had not been documented in the child records as having overweight and no measures were undertaken, compared to 24 children with overweight (10.1%) in the intervention group. The use of CCHD illustrations was documented in 66 children (32.1%) in the control group compared to 130 (54.6%) in the intervention group and the use of the BMI growth chart in 101 children (42.6%) in the control group compared to 182 (76.5%) in the intervention group (Table 4).
TABLE 4.
Delivery of care according to the study protocol, child records and related estimated costs
| Study protocol | Child records | Cost in euros | |||||
|---|---|---|---|---|---|---|---|
| Universal | CG | IG | CG (n = 237) | IG (n = 238) | 23 011 | 20 700 | |
| All 4y‐olds get 4y‐HV (60 min) | Health dialogue screening overweight using | Structured CCHD with CCHDs approach using | 4y‐HV | 237 | 238 | 9563 | 9616 |
| Present (missing) | 6 (2.5) a | 242 | |||||
| One caregiver | 193 (81.4) | 184 (77.3) | 7 697 | 7 338 | |||
| Two caregivers | 44 (18.6) | 48 (20.2) | 1 866 | 2 036 | |||
| Undocumented overweight | 55 (23.2) | 24 (10.1) | |||||
| CCHD illustrations | Used CCHD illustrations | 76 (32.1) | 130 (54.6) | ||||
| BMI growth chart | Used BMI growth chart | 101 (42.6) | 182 (76.5) | ||||
| Targeted | ‐‐ | Targeted CCHD: FG 1–3 weeks after 4y‐HV (45 min) | Extra visits including FG | 59 (24.9) | 60 (25.1) | 1306 | 1599 |
| FG offered | 61 (25.6) | ||||||
| Declined | 35 (57.4) | ||||||
| Accepted | 26 (42.6) | ||||||
| Present at FG | n = 26 | ||||||
| One caregiver | 12 (46.2) | 376 | |||||
| Two caregivers | 14 (53.8) | 471 | |||||
| 4y‐olds identified with overweight | Extra visit 3–6 months after 4y‐HV (30 min) | Extra visit on caregivers' request (30 min) | Extra HVs | n = 59 | n = 34 (no FG) | ||
| One extra HV | 33 (13.9) | 30 (12.6) | |||||
| Two extra HVs | 10 (4.2) | 2 (0.8) | |||||
| Three extra HVs | 2 (0.8) | ‐‐ | |||||
| Present (missing) | 2 (3.4) a | 4 (11.8) a | 44 | 88 | |||
| One caregiver | 51 (86.4) | 27 (79.4) | 1 120 | 593 | |||
| Two caregivers | 6 (10.2) | 3 (8.8) | 142 | 71 | |||
| Referrals | Referral to overweight team or dietician | Referral on caregivers' request | Referrals | 19 (8.0) | 11 (4.6) | 12142 | 9485 |
| Referral offered | 41 (17.2) | 19 (8.0) | 231 | 107 | |||
| Declined | 22 (53.7) | 8 (42.1) | |||||
| Received care at | 19 (43.6) | 11 (57.9) | |||||
| ‐Overweight team b | 12 (63.2) | 10 (83.3) | 11 115 | 9 262 | |||
| ‐Dietician | 7 (36.8) | ‐ | 796 | ||||
| ‐CHS‐psychologist | 1 (9.1) | 116 | |||||
Abbreviations: CCHD, child‐centered health dialogue; CG, control group; FG, family guidance; HV, health visit; IG, intervention group.
Cost for missing calculated according to ratio one caregiver: two caregivers.
In Skåne the overweight team includes a physician and a specialized nurse or a dietician.
In the control group 33 families (13.9%) received one extra health visit 3–6 months after the 4‐years health visit, 10 families (4.2%) two extra health visits and two families (0.8%) three extra visits. In the intervention group 61 families (25.6%) were offered FG according to the study protocol 1–3 weeks after the child's 4‐years health visit: 26 families (42.6%) accepted and participated in FG, while 37 families (57.4%) declined FG. Thirty families (12.6%) received an extra health visit in the intervention group 3–6 months after the 4‐years health visit, three of them had already participated in FG and five had declined FG in the first place. Two families (0.8%) in the intervention group received two extra visits (Table 4).
Referrals were offered to a larger extent in the control group: 41 referrals (17.2%) compared to 19 (8.0%) in the intervention group. Many families declined the referral offered to them: 22 (53.7%) in the control group compared to eight referrals (42.1%) in the intervention group (Table 4).
The total cost for the delivery of care for children in the control group was 23,011 euros (97 euros per child) and 20,700 euros (87 euros per child) in the intervention group (Table 4).
3.3.4. Incremental cost‐effectiveness ratios
From a societal perspective, the incremental costs of the intervention were estimated at 167 euros per child with overweight. The corresponding ICER for zBMI‐change was 183 euros per 0.1 zBMI unit prevented and for BMI‐change 866 euros per 1 BMI unit prevented.
3.4. Adverse effects
None of the 4‐year‐old children with overweight, whether in the control or in the intervention group, developed underweight. At follow‐up, 14.8% of the children with overweight at baseline in the control group had obesity and 2.1% severe obesity compared to 9.7% and 1.3% respectively in the intervention group.
3.5. Fidelity to the study protocol
Fidelity to the study protocol was monitored through the collection of data from the child's records on delivery of care for children with overweight at baseline and through a digital questionnaire containing 11 questions distributed to all nurses at baseline in May 2016, December 2017, and July 2018. During the RCT 26 nurses stopped working in CHS: 11 nurses in the control group (four replaced and two extra recruited nurses) and 16 nurses in the intervention group (nine replaced). In the intervention group four new recruited nurses were trained in CCHD, while five nurses could not be trained, resulting in the withdrawal of 285 children in the intervention group that met a nurse not trained in CCHD, of whom 31 children had overweight (10.9%). None of the nurses trained in CCHD started working in the control group. In response to the question ‘if they believed they had adequate knowledge of child overweight’, 47.5% of nurses in the control group believed that they had adequate knowledge of child overweight in December 2017 and 50.0% in July 2018 compared to 72.7 and 81.1% respectively of nurses in the intervention group. The baseline questionnaire in May 2016 showed that 55.6% of all eligible nurses believed they had adequate knowledge of child overweight (Table S3a). To the question whether they ‘felt competent in the communication method’ 17.5 and 28.9% of nurses in the control group felt competent compared to 43.2 and 56.8% of nurses in the intervention group and 28.1% at baseline. The question ‘if they felt comfortable in talking about overweight’ was answered comparably: 20 and 34.5% of nurses in the control group compared to 31.8 and 40.5% of nurses in the intervention group and 24.0% at baseline (Table S3a).
4. DISCUSSION
In this cluster RCT of a low‐intensive multicomponent CCHD targeting 4‐year‐old children in the Swedish CHS, we found no intervention effect one year after the intervention on zBMI‐change in children with normal weight at baseline. For children with overweight at baseline, a favorable effect 12 months after the intervention on zBMI‐change was suggested, but the result did not reach statistical significance.
The magnitude of the mean difference in zBMI‐change in children with overweight was in the same range as the mean difference of zBMI‐change of the reported multicomponent child obesity prevention programs targeting children aged 0 to 5 years in the latest Cochrane systematic review. 4
One of reasons for the absence of intervention effect for children with normal weight could be that the differences between the delivery of care in children with normal weight in the intervention and control group were small, which might have decreased the potential to detect an intervention effect. The CCHD illustrations commissioned by the digital national handbook for CHS in Sweden were published before the start of the RCT after a qualitative evaluation that showed that nurses felt the illustrations were helpful during the 4‐years health visit and were therefore used in both the intervention and the control group. 41 However, the nurses in the intervention group received more profound and interactive training in the CCHD approach and were especially trained in the challenges when a child had overweight.
That CCHD can benefit children with overweight was reflected in the larger number of children with overweight in the intervention group that were documented having overweight in the child records and received measures accordingly, compared to the control group. A recent study among nurses working in the Swedish CHS described how nurses sometimes avoided mentioning a child's overweight because they felt unable to communicate about children's weight status and the authors suggested additional communication training. 37 In our study, a larger proportion of nurses in the intervention group believed they had adequate knowledge of child overweight and felt competent in the communication method. A qualitative study describing nurses' experiences of CCHD showed that CCHD encouraged nurses to mention their concern about the child's health in relation to their weight, which is an important step in the prevention of child obesity. 36 , 37 , 39 Nurses trained in CCHD felt that they had been provided with a toolbox that facilitated a more professional way of performing a dialogue with caregivers and children with overweight. 39
The low number of FG in children identified with overweight in the intervention group might be another reason for the absence of intervention effect in children with overweight. Only a quarter of the families were offered FG according to the child records. Another observation is that several caregivers declined the FG offered in the intervention group, which is in line with another study that offered an additional visit for children identified with overweight in CHS. 42 One explanation might be that caregivers experienced the dialogue about the BMI growth chart during the first part of CCHD and the accompanying concerns for the child's health as sufficient motivation to establish changes in lifestyle and did not need extra support. This is corroborated by a study where caregivers after a single conversation about the child's overweight increased motivation to engage in healthy lifestyle. 43 Another explanation might be that caregivers experienced an emotional response when the BMI growth chart was used to identify overweight and did not accept additional care. 13 , 37 , 42 Several studies showed that health professionals felt uncomfortable introducing the topic of overweight and found health dialogues with families about overweight challenging. 23 , 37 , 39 Likewise, in our study nurses in both groups answered that they felt uncomfortable communicating about overweight. The qualitative study of nurses' experiences of CCHD, however, found that the tutorial sessions did increase their self‐esteem in starting the conversation about weight and lifestyle already in early childhood and demonstrated the need for continuous training with room for reflection. 37 , 39 A qualitative interview study exploring caregivers' experiences of CCHD when overweight is identified is ongoing.
Future research should focus on how best to communicate and engage children and families in weight related topics. Although evidence‐based practices are still lacking, a recent study suggested regular conversations about growth and health as early as possible. 44 Even CCHD could be adapted and started earlier. By introducing the BMI growth chart at an early age and gradually building a trusting relationship over multiple visits, the family might increase acceptance for additional support when BMI is rising. 14 , 15 , 44
CCHD did not appear to increase health inequalities regarding gender and socioeconomic status, as the reduction in zBMI in children with overweight was larger in both females and males and in children from families with a higher (CNI < 0.93) and lower socio‐economic status (CNI ≥ 0.93) in the intervention group compared to the control group. The subgroup analyses on gender and CNI suggested that the effect of the intervention was more favorable in females and more beneficial in children from families with a higher socio‐economic status. This is important knowledge to inform the design of future interventions targeting children with overweight from families with a lower socio‐economic status, who perhaps need more prolonged support than the low‐intensive CCHD to enhance larger beneficial effects. 45
The economic evaluation showed that the costs for delivery of care in the intervention were lower than the costs for delivery of care in the control group. CCHD resulted in more extra visits with two caregivers present, which is seen as a promoting factor for a healthy lifestyle, 13 , 36 but led to a lower proportion of two or three extra health visits and fewer referrals. This was expected as we hypothesized that the nurses, already known and trusted by the caregivers and trained in providing care for children with overweight did not offer unnecessary extra visits and referrals.
The ICER in our study is difficult to compare to other studies as the limited economic evaluations of interventions for children aged 0–5 years vary in terms of intervention intensity, age of the children and settings. 5 , 46 , 47 The incremental costs can, however, be compared to an Australian study which estimated the health care cost savings of reductions in zBMI of children aged 2–5 years 48 They suggested that with an intervention effect of the estimated difference of −0.13 zBMI, comparable to our MD in zBMI in children with overweight at baseline, the significant health care cost savings would result in approximately 301 million Australian dollars (189 million euros), if the intervention effect was maintained over the lifetime. 48 The authors demonstrated that effective interventions could cost up to a range from $1,866 (1175 euros) to $326 (205 euros) per child of the Australian population aged 2–5 years, depending on various assumptions in health impact modeling, and still be considered cost‐effective. The incremental costs of our intervention estimated at 167 euros per child identified with overweight, was lower than the lowest threshold in the Australian study, 48 and hence CCHD is likely to be cost‐effective in Sweden.
This present study did not describe changes in the child's dietary intake and physical activity, nor caregivers' feeding practices and self‐efficacy for promoting healthy lifestyle, which is a limitation. Such findings are important in understanding the mechanisms by which family based interventions for obesity prevention influence the child's lifestyle and parental practices. 49 One could discuss whether the setting of the study in a real‐world clinical setting is a limitation, because of the great turnover of nurses in both the control and the intervention group or a strength as it gives valuable information for the future development of family‐based prevention programs. The information collected from the child records gave an objective view of the actual delivery of care of children with overweight in CHS. Other strengths of the study were the long‐term follow‐up of one year after the intervention, the large number of participants, a low number of children lost to follow‐up and the account of health inequalities and adverse events. Another strength is that this study included a detailed description of costs and cost‐effectiveness, which can be used for policymakers and researchers for comparison in future studies. That CCHD is theoretically based on CCC 32 is important as we believe that the engagement of the child in the health dialogue contributes to an awareness of health issues and changes in lifestyle that might improve their health later in life.
5. CONCLUSION
This low‐intensive multicomponent child‐centered obesity prevention intervention, with the potential to be implemented universally in the child health services, is suggested to be cost‐effective with a decreasing effect on zBMI in children with overweight, albeit without statistical significance. Obesity results in a substantial long‐term economic burden on society. Thus, even fairly small average effects from interventions implemented in early childhood can be important from a public health perspective. 50 The economic evaluation showed that the delivery of care in the intervention for children with overweight, assessed from the societal perspective, cost less than delivery of care in the control group. A possible explanation might be that nurses in the intervention group felt more knowledgeable in child overweight and more competent in the communication method. Additional research is needed to ensure that even children and their families from lower socioeconomic backgrounds have equal outcomes in universally implemented obesity prevention programs. Future research should focus on interventions in which CHS works together with childcare settings and other communities to build an overall healthier environment and effectively address childhood overweight on a societal level.
CONFLICT OF INTERESTS
The authors declare no conflicts of interest.
Supporting information
Table S1
Table S2
Table S3
ACKNOWLEDGMENTS
Mariette Derwig carried out the trial and analyzed data with support of JB and AWT. All authors were involved in writing the paper and had final approval of the submitted and published versions.Special thanks to the children and caregivers who participated in the study and the nurses executing CCHD and usual care. Thanks to Linda Håkansson for training in CCHD and to Ami Stenberg for supporting the nurses in the tutorial sessions.This project was funded by the Swedish Research Council for Health, Working Life and Welfare (FORTE), Föreningen Mjölkdroppen Helsingborg, and Region Skåne.
Derwig M, Tiberg I, Björk J, Welander Tärneberg A, Hallström IK. A child‐centered health dialogue for the prevention of obesity in child health services in Sweden – A randomized controlled trial including an economic evaluation. Obes Sci Pract. 2022;8(1):77‐90. 10.1002/osp4.547
REFERENCES
- 1. World Health Organisation . Consideration of the Evidence on Childhood Obesity for the Commission on Ending Childhood Obesity: Report of the Ad Hoc Working Group on Science and Evidence for Ending Childhood Obesity. Geneva, Switzerland: World Health Organisation; 2016. [Google Scholar]
- 2. Spong E, Miregård J, Nylander C. Overweight and obesity among 4‐year‐old children in Sweden 2018. Poster In Swedish. Accessed January 8, 2021. https://samverkan.regionsormland.se/for‐vardgivare/halsoval/barnhalsovard/rapporter‐fran‐barnhalsovarden‐sormland/
- 3. Cole TJ, Bellizzi MC, Flegal KF, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;7244:1240‐1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brown T, Moore TH, Hooper L, et al. Interventions for preventing obesity in children. Cochrane database Syst Rev. 2019;7:CD001871. 10.1002/14651858.CD001871.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Frew E. Economic evaluation of childhood obesity interventions: reflections and suggestions. Pharmacoeconomics. 2016;34(8):733‐740. 10.1007/s40273-016-0398-8 [DOI] [PubMed] [Google Scholar]
- 6. Pulgarón ER. Childhood obesity: a review of increased risk for physical and psychological comorbidities. Clin Ther. 2013;35(1):A18‐A32. 10.1016/j.clinthera.2012.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJM. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev : off J Int Assoc Study Obes. 2008;9(5):474‐488. 10.1111/j.1467-789X.2008.00475.x [DOI] [PubMed] [Google Scholar]
- 8. Marmot M, Bell R. Fair Society. Healthy lives. Publ Health. 2012;126(Supplement 1):S4‐S10. 10.1016/j.puhe.2012.05.014 [DOI] [PubMed] [Google Scholar]
- 9. Grossman DC, Bibbins‐Domingo K, Curry SJ, et al. Screening for obesity in children and adolescents: US preventive services task Force recommendation statement. J Am Med Assoc. 2017;317(23):2417‐2426. 10.1001/jama.2017.6803 [DOI] [PubMed] [Google Scholar]
- 10. Landgren K, Quaye AA, Hallström E, Tiberg I. Family‐based prevention of overweight and obesity in children aged 2–6 years: a systematic review and narrative analysis of randomized controlled trials. Child Adolesc Obes (2574254X). 2020;3(1):57‐104. 10.1080/2574254X.2020.1752596 [DOI] [Google Scholar]
- 11. Döring N, Mayer S, Rasmussen F, Sonntag D. Economic evaluation of obesity prevention in early childhood: methods, limitations and recommendations. Int J Environ Res Public Health. 2016;13(9):911. 10.3390/ijerph13090911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Fourth edition. Oxford: Oxford University Press; 2015. [Google Scholar]
- 13. Ames H, Mosdøl A, Blaasvær N, Nøkleby H, Berg RC, Langøien LJ. Communication of children’s weight status: what is effective and what are the children's and parents’ experiences and preferences? A mixed methods systematic review. BMC Publ Health. 2020;20(1):1‐22. 10.1186/s12889-020-08682-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bohnert AM, Loren DM, Miller AL. Examining childhood obesity through the lens of developmental psychopathology: framing the issues to guide best practices in research and intervention. The American Psychologist. 2020;75(2):163‐177. https://doi‐org.ludwig.lub.lu.se/10.1037/amp0000581 [DOI] [PubMed] [Google Scholar]
- 15. Summary of the clinical practice guideline for multicomponent behavioral treatment of obesity and overweight in children and adolescents. Am Psychol. 2020;75(2):178‐188. https://doi‐org.ludwig.lub.lu.se/10.1037/amp0000530 [DOI] [PubMed] [Google Scholar]
- 16. Hart CN, Jelalian E, Raynor HA. Behavioral and social routines and biological rhythms in prevention and treatment of pediatric obesity. Am Psychol. 2020;75(2):152‐162. https://doi‐org.ludwig.lub.lu.se/10.1037/amp0000599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Oberklaid F, Drever K. Is my child normal? Milestones and red flags for referral. Aust Fam Physician. 2011;40(9):666‐670. [PubMed] [Google Scholar]
- 18. Messito MJ, Mendelsohn AL, Katzow MW, Scott MA, Vandyousefi S, Gross RS. Gross RS prenatal and pediatric primary care–based child obesity prevention program: a randomized trial. Pediatrics. 2020;146(4):1‐11. 10.1542/peds.2020-0709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. The National Handbook for Child Health Services . The National Child Health Programme. Accessed 8 January 2021. https://www.rikshandboken‐bhv.se/metoder‐‐riktlinjer/barnhalsovardens‐nationella‐program/. In Swedish. Last revision February 22, 2018. [Google Scholar]
- 20. The National Handbook for Child Health Services . The 4‐year Health Visit. Accessed 8 January 2021. https://www.rikshandboken‐bhv.se/halsobesok/4‐ar/. In Swedish. Last revision January 31, 2017. [Google Scholar]
- 21. Bohman B, Eriksson M, Lind M, Ghaderi A, Forsberg L, Rasmussen F. Infrequent attention to dietary and physical activity behaviours in conversations in Swedish child health services. Acta Paediatr. 2013;102(5):520‐524. 10.1111/apa.12176 [DOI] [PubMed] [Google Scholar]
- 22. Regber S, Marild S, Johansson Hanse J. Barriers to and facilitators of nurse parent interaction intended to promote healthy weight gain and prevent childhood obesity at Swedish child health centers. BMC Nurs. 2013;12:1–11. 10.1186/1472-6955-12-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Isma GE, Bramhagen AC, Ahlstrom G, Östman M, Dykes AK. Obstacles to the prevention of overweight and obesity in the context of child health care in Sweden. BMC Fam Pract. 2013;14(1):1–10. doi: org.ludwig.lub.lu.se/. 10.1186/1471-2296-14-143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Flodmark C‐E. Prevention models of childhood obesity in Sweden. Obesity Facts. 2018;11(3):257‐262. 10.1159/000482009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. Int J Nurs Stud. 2013;50(5):587‐592. 10.1016/j.ijnurstu.2012.09.010 [DOI] [PubMed] [Google Scholar]
- 26. Consort . Checklist 2010. Accessed January 8, 2021. http://www.consort‐statement.org/checklists/view/32‐‐consort‐2010/78‐interventions [Google Scholar]
- 27. Husereau D, Drummond M, Petrou S, et al. Consolidated health economic evaluation reporting standards (CHEERS) statement. Eur J Health Econ. 2013;14:367‐372. 10.1007/s10198-013-0471-6 [DOI] [PubMed] [Google Scholar]
- 28. County of Scania . Region Skåne, Annual Report Child Health Services County of Scania 2015. 2016. In Swedish. Accessed January 8, 2021. https://vardgivare.skane.se/siteassets/3.‐kompetens‐och‐utveckling/sakkunniggrupper/bhv/arsrapport/barnhalsovard‐arsrapport‐2015.pdf [Google Scholar]
- 29. Sundquist K, Malmstrom M, Johansson SE, Sundquist J. Care need index, a useful tool for the distribution of primary health care resources. J Epidemiol Community Health. 2003;57(5):347‐352. 10.1136/jech.57.5.347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Derwig M, Tiberg I, Björk J, Hallström I. Child‐Centred health dialogue for primary prevention of obesity in child health services – a feasibility study. Scand J Public Health. 2021;49(4):384‐392. 10.1177/1403494819891025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Derwig M, Tiberg I, Hallström I. Elucidating the child's perspective in health promotion: children's experiences of child‐centred health dialogue in Sweden. Health Promot Int. 2021;36(2):363‐373. 10.1093/heapro/daaa060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Coyne I, Hallström I, Söderback M. Reframing the focus from a family‐centred to a child‐centred care approach for children's healthcare. J Child Health Care. 2016;20(4):494‐502. 10.1177/1367493516642744 [DOI] [PubMed] [Google Scholar]
- 33. Håkansson L, Derwig M, Olander E. Parents’ experiences of a health dialogue in the child health services: a qualitative study. BMC Health Serv Res. 2019;19(1):774. 10.1186/s12913-019-4550-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Nowicka P, Flodmark C‐E. Family therapy as a model for treating childhood obesity: useful tools for clinicians. Clin Child Psychol Psychiatry. 2011;16(1):129‐145. 10.1177/1359104509355020 [DOI] [PubMed] [Google Scholar]
- 35. Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000;15(3):259‐267. 10.1093/heapro/15.3.259 [DOI] [Google Scholar]
- 36. Brown CL, Perrin EM. Obesity prevention and treatment in primary care. Academic Pediatrics. 2018;18(7):736‐745. 10.1016/j.acap.2018.05.004 [DOI] [PubMed] [Google Scholar]
- 37. Sjunnestrand M, Nordin K, Eli K, Nowicka P, Ek A. Planting a seed – child health care nurses’ perceptions of speaking to parents about overweight and obesity: a qualitative study within the STOP project. BMC Publ Health. 2019;19:1–11. 10.1186/s12889-019-7852-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Carr KA, Epstein LH. Choice is relative: reinforcing value of food and activity in obesity treatment. Am Psychol. 2020;75(2):139‐151. 10.1037/amp0000521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Castor C, Derwig M, Borg SJ, Ollhage ME, Tiberg I. A challenging balancing act to engage children and their families in a healthy lifestyle – nurses’ experiences of child‐centred health dialogue in child health services in Sweden. J Clin Nurs. 2021;30(5/6):819‐829. 10.1111/jocn.15622 [DOI] [PubMed] [Google Scholar]
- 40. Riksbank. Annual Average Exchange Rates. Accessed January 8, 2021. https://www.riksbank.se/sv/statistik/sok‐rantor‐‐valutakurser/arsgenomsnitt‐valutakurser/?y=2017&m=12&s=Dot&f=y [Google Scholar]
- 41. Håkansson L. Nurses Experiences on the Health Dialogue Concerning Healthy Eating in Child Health Service. Master's thesis. Mittuniversitetet. In Swedish. 2015. Accessed January 8, 2021. http://miun.diva‐portal.org/smash/get/diva2:867420/FULLTEXT01.pdf [Google Scholar]
- 42. Van Grieken A, Veldhuis L, Renders CM, et al. Population‐based childhood overweight prevention: outcomes of the ‘Be active, eat right’ study. PLoS One. 2013;8(5):e65376. 10.1371/journal.pone.0065376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Dawson AM, Brown DA, Cox A, et al. Using motivational interviewing for weight feedback to parents of young children. J Paediatr Child Health. 2014;50(6):461‐470. https://doi‐org.ludwig.lub.lu.se/10.1111/jpc.12518 [DOI] [PubMed] [Google Scholar]
- 44. McPherson AC, Hamilton J, Kingsnorth S, et al. Communicating with children and families about obesity and weight‐related topics: a scoping review of best practices. Obes Rev. 2017;18:164‐182. 10.1111/obr.12485 [DOI] [PubMed] [Google Scholar]
- 45. Ek A, Lewis Chamberlain K, Sorjonen K, et al. A parent treatment program for preschoolers with obesity: a randomized controlled trial. Pediatrics. 2019;144(2):e20183457. 10.1542/peds.2018-3457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Döring N, Zethraeus N, Tynelius P, de Munter J, Sonntag D, Rasmussen F. Economic evaluation of primrose – a trial‐based analysis of an early childhood intervention to prevent obesity. Front Endocrinol. 2018;9(3):1–8. 10.3389/fendo.2018.00104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Brown V, Tan EJ, Hayes A, et al. Cost comparison of five Australasian obesity prevention interventions for children aged from birth to two years. Pediatric obesity. 2020;15(12):e12684. 10.1111/ijpo.12684 [DOI] [PubMed] [Google Scholar]
- 48. Brown V, Ananthapavan J, Sonntag D, Tan EJ, Hayes A, Moodie M. The potential for long‐term cost‐effectiveness of obesity prevention interventions in the early years of life. Pediatric Obesity. 2019;14(8):e12517. 10.1111/ijpo.12517 [DOI] [PubMed] [Google Scholar]
- 49. Enright G, Allman‐Farinelli M, Redfern J. Effectiveness of family‐based behavior change interventions on obesity‐related behavior change in children: a realist synthesis. Int J Environ Res Public Health. 2020;17(4099):4099. https://doi‐org.ludwig.lub.lu.se/10.3390/ijerph17114099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Smith JD, Fu E, Kobayashi MA. Prevention and management of childhood obesity and its psychological and health comorbidities. Annu Rev Clin Psychol. 2020;16:351‐378. 10.1146/annurev-clinpsy-100219-060201 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1
Table S2
Table S3


