Abstract
Study Objectives:
This study evaluated the effect on infant sleep of a novel intervention (Play2Sleep) that combined infant sleep information with self-modeled video feedback on parent-infant interactions.
Methods:
An explanatory sequential mixed-methods design consisting of a randomized controlled trial with 63 mother-father-infant triads randomized to Play2Sleep or comparison home visit interventions was used. We used repeated measures analysis of covariance to detect changes in infant night wakings, nocturnal wakefulness, and sleep durations and Wilcoxon signed rank test to evaluate changes in perception of infant sleep problems. Family interviews (n = 20) were used to explain the quantitative findings and analyzed qualitatively using thematic analysis.
Results:
Play2Sleep was effective in reducing maternal-reported infant wakefulness, F(1,55) = 5.33, P = .03, partial η2 = .09, and the number of paternal-reported naps, F(1,58) = 4.90, P = .03, partial η2 = .08. Parents in the Play2Sleep group reported significant improvements in problematic infant sleep that were not observed in the comparison group; however, Play2Sleep was not effective in reducing the number of parent-reported night wakings. Information overwhelm, learning infant cues, and working together with a subtheme of father involvement were key qualitative themes developed to explain the quantitative results. Unplanned exploratory analyses revealed a significant improvement in maternal depression symptoms in the Play2Sleep group.
Conclusions:
This study suggests Play2Sleep could improve infant sleep by promoting parental awareness of infant cues and father involvement and improving maternal depression. Additional research is needed to determine the optimal number and timing of sessions.
Clinical Trial Registration:
Registry: ClinicalTrials.gov; Name: Play2Sleep: Using Play to Improve Sleep; URL: https://clinicaltrials.gov/ct2/show/NCT02742155; Identifier: NCT02742155.
Citation:
Keys EM, Benzies KM, Kirk VG, Duffett-Leger L. Effect of Play2Sleep on mother-reported and father-reported infant sleep: a sequential explanatory mixed-methods study of a randomized controlled trial. J Clin Sleep Med. 2022;18(2):439–452.
Keywords: infants, mothers, fathers, parenting, sleep, wakefulness, parent-child interaction
BRIEF SUMMARY
Current Knowledge/Study Rationale: Parent-child interactions are crucial in child development and may be associated with parent-reported difficulties in infant sleep. Previous studies have examined how supporting parent-child interactions may improve infant sleep; however, this strategy has not yet been experimentally tested. This sequential explanatory mixed-methods study examines the effect of parental education on infant sleep with a novel self-modeled video-feedback parent-child interaction home visit intervention on parent-reported infant sleep.
Study Impact: In families experiencing infant sleep problems, a brief home intervention with education on infant sleep and parent-child interaction for mothers and fathers may improve infant sleep and maternal depression, enhance parental awareness of infant cues, and assist parents to work together by facilitating father involvement.
INTRODUCTION
Infant sleep problems are associated with poorer outcomes, including cognitive and behavioral developmental difficulties.1,2 Parental behaviors, such as rocking or feeding to sleep, often promote the development of infant sleep problems. Likely, a combination of parent, infant, and environmental factors converge to promote the use of more involved “hands on” sleep-related parent practices and/or an infant’s responsiveness to these parenting practices.3,4 Although effective,5 concerns about implementing certain behavioral-based extinction-interventions (such as graduated extinction) in infants less than age 6 months have been expressed.6 Parents also report reservations and practical challenges when implementing these interventions.7 Interventions that consider only infant sleep behaviors may artificially isolate this common challenge from the broader parenting experience and not translate to broader and longer-term improvements in parental capacity to manage future sleep difficulties. Infant sleep interventions that integrate broad parenting skills may help to improve infant sleep while also building parental capacity to address and manage other aspects of parenting.
Previous research suggests a relationship between parent-child interactions and infant sleep; however, this research is often focused on maternal sensitivity.8–12 While modifiable, focusing only on maternal sensitivity underestimates the role of the infant in eliciting parental responses and artificially isolates mother-infant interactions from the family context. For example, infants have been reported to send clearer social cues and be more responsive during interactions with fathers than mothers.13 While studies that have included fathers have generally been limited by small numbers of father participants, Bordeleau et al8 did measure father parent-child interactions and concluded that both high quality mother-infant and father-infant interactions between ages 12 and 18 months predicted larger percentages of night time sleep at 4 years of age. The apparent link between infant sleep and parent-child interactions supports the premise that sleep problems may represent underlying difficulties in parent-child relationships.4 As such, improving parental capacity in both mothers and fathers for high quality parent-child interactions may be a mechanism for preventing or improving infant sleep difficulties.
In clinical samples, programs that aim to improve parent-child interactions and parental understanding of infant sleep and social cues have demonstrated promise in improving maternal perception of infant sleep difficulties.14–16 In addition, improving maternal-infant interactions in preterm infants was associated with fewer sleep difficulties at age 3 months.17 For infants born with very low birth weight, participants in the home-based version of a 12-month maternal-infant intervention had fewer maternal reports of sleep difficulties at age 24 months.18 Such studies suggest that promoting high-quality parent-child interactions in families could prevent or reduce subsequent infant sleep problems. However, this body of research is limited by a lack of experimental designs and an isolated focus on the mother-infant dyad. Research using stronger research designs shows promise for using a relational approach for improving sleep in higher risk populations.
Building on a relational approach in a coparenting paradigm, we developed Play2Sleep, a brief home-visit intervention that combines individualized sleep education with personalized self-modeled video feedback of structured parent-infant play sessions for both mothers and fathers to improve infant sleep. Play2Sleep was designed to address the broader parenting difficulties that may underlie infant sleep difficulties by using personalized coaching to enhance parental ability to identify and respond appropriately to their infant’s sleep-related and broader social cues. The aim of this mixed-methods study was to evaluate the effectiveness of Play2Sleep in a community sample of mothers and fathers who considered their 5-month-old infant’s sleep to be problematic. As such, the quantitative research question was: Does 1 dose of Play2Sleep delivered during home visits with mothers and fathers of 5-month-old infants with infant sleep disturbances reduce the number of night wakings at age 7 months? The qualitative research question was: What are parental perceptions of family experiences, processes, and contexts related to Play2Sleep and infant sleep disturbances? The mixed-methods research question was: How do parental perceptions of family experiences, processes, and contexts related to infant sleep explain the effectiveness of Play2Sleep?
The theoretical foundation of this study was a proposed nursing theory for infant sleep and development,3 which combines Bronfenbrenner’s Bioecological Theory of Human Development19 with the Barnard Model of parent-child interactions.20 This theory postulates that parent-child interactions are powerful influencers of both infant sleep patterns and child development. Because infant sleep disturbances occur during a critical time of brain development and may cause parent distress that leads to strained parent-child interactions, it may be advantageous for infant sleep interventions to contextualize parent education on infant sleep within a relational context that supports sensitive and responsive caregiving.
METHODS
Study design
In a large Canadian urban center, we used an explanatory sequential mixed-methods design comprised of a parallel randomized controlled trial with follow-up family interviews.21 We used this design to increase understanding related to the contexts within which parent-child interactions influence infant sleep and to provide insight into the processes that do, or do not, contribute to the effectiveness of Play2Sleep.
Participants
Between December 2016 to July 2018, we recruited families through social media and advertisement at all 8 community health centers in a large urban center. These centers offer universal well-child clinic appointments and immunizations by public health nurses to families of children aged 2 months and older. Interested families contacted the study team directly or provided their contact information to their public health nurse and were later contacted by the first author (E.M.K.). The University of Calgary Conjoint Health Research Ethics Board (REB15-2652) approved this study, which was registered with ClinicalTrials.gov (NCT02742155). We followed the Consolidated Standards of Reporting Trials (CONSORT) guidelines (Table S1 in the supplemental material).22
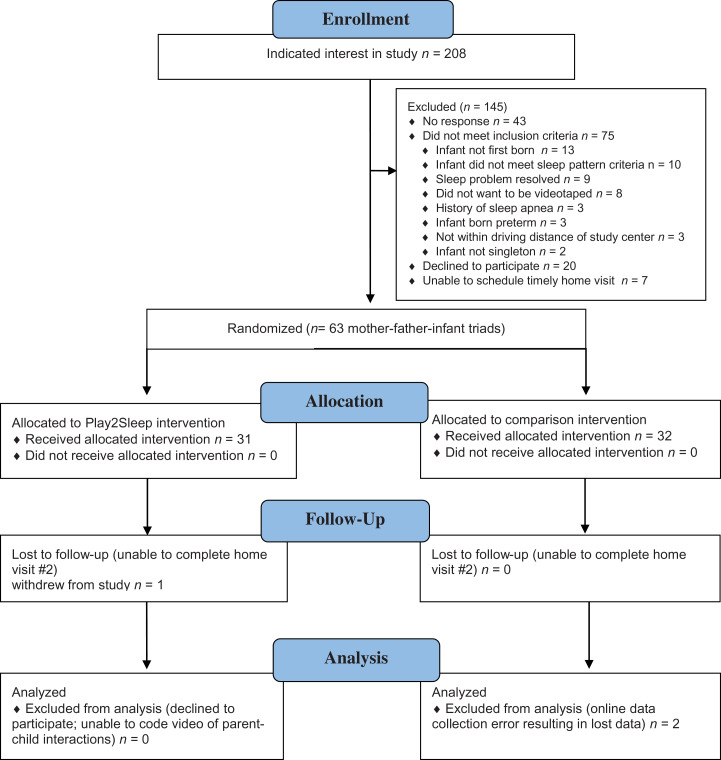
We included cohabiting mothers and fathers if 1) they perceived their first-born, full-term, healthy singleton, 4-month old infant was experiencing sleeping difficulties; 2) parents agreed to a home visit where they would be video-recorded playing with their baby; and 3) their infant’s sleep pattern met 1 of 3 specified criteria (> 3 wakings/night, > 60 minutes awake during the night, and/or < 9 hours of sleep in 24 hours). These criteria were derived using Sadeh’s23 designation of characteristics that constituted a “poor sleeper”. Due to requirements of the intervention and measurement, we included only parents who could read, write, and speak English. According to Statistics Canada (www.statcan.gc.ca) over 95% of the region of Canada in which the study was conducted speaks English, 85.5% of households are married or common-law couples, and 99% of these are opposite sex. From 2001 to 2011, the median income of couple families with 1 child in the region was $122,740 CAN. Eighty-eight percent of mothers in Canada take maternity and/or parental leave, which, at the time of the study, was up to 50 weeks. We excluded families if either parent or infant had a known or suspected medical or physiological cause of sleep problems. To detect an effect size comparable to those of other brief infant sleep interventions, .44 to .64,24,25 a sample of 60 families (30 in each group) was needed to detect an effect size of .32 with a power of .80 at a .05 level of significance. We contacted 208 families and enrolled 63 (recruitment rate of 30.3%). Of the 63 families, 1 family withdrew, citing scheduling difficulties for the outcome home visit, and data for 2 families were lost due to difficulties with the online data collection platform. See Figure 1 for the CONSORT flow diagram.
Figure 1. CONSORT (Consolidated Standards of Reporting Trials) flow diagram.
Trial arms
Play2Sleep intervention
In the Play2Sleep intervention, each parent individually received immediate verbal feedback on their video-recorded parent-child interaction, in addition to parental educational about infant sleep. For the structured video recording, parents were asked to select from a list of play activities a task (ie, squeak a toy, scribble on a piece of paper) that was novel to their infant. The parent was then instructed to teach their infant to complete the play activity. This structured play session was video recorded. Upon completing the structured play session, the home visitor (a specially trained registered nurse; EK) reviewed the video recording with the parent and provided tailored feedback on 2–3 parental behaviors that contributed to positive parent-child interactions and 1–2 suggestions for growth. Feedback included comments on parental behaviors relating to sensitivity (eg, how the parent was [or was not] allowing enough time for the infant to respond), response to infant disengagement (eg, rearranging the infant’s position in response to infant disengagement), social-emotional growth (eg, supporting social interaction by smiling and being positioned face-to-face), and/or cognitive growth (eg, using descriptive words and/or modeling to demonstrate the play task to the infant).
In addition, the home visitor used the video to point out examples of the infant’s engagement and disengagement cues, as described by Parent-Child Relationship Programs.20 This included how infants signaled engagement or disengagement during social interactions, as well as how the infant may cluster more subtle (less obvious) cues (eg, hand-to-ear, joining hands, head lowering, gaze aversion, yawning) and/or potent (more obvious) disengagement cues (eg, back arching, maximal lateral gaze aversion, fussing, crying) to indicate the need for a momentary (eg, pause, change in activity) or a more significant break (eg, sleep). Mothers and fathers completed these feedback sessions separately and each lasted between 10 and 20 minutes. Following the separate feedback sessions, the home visitor reviewed public health handouts on infant seep with mothers and fathers together (approximately 30–40 minutes). These handouts contained information on typical infant sleep patterns, as well as sleep cues, sleep associations, and routines. Each Play2Sleep home visit took approximately 90 minutes. No additional Play2Sleep home visits occurred.
Comparison intervention
The comparison intervention included only the parental educational component on infant sleep. While the comparison mothers and fathers completed the same individual video-recorded structured play sessions with their infant (as a measure of their interaction quality), the home visitor did not review the video recording or provide personalized feedback on parent-child interactions. Instead, parents were immediately brought back together to review of public health infant sleep handouts as the Play2Sleep group. Each comparison home visit took approximately 60 minutes. No additional comparison intervention home visits occurred.
Blinding
Due to the nature of the intervention and single home visitor for all home visits, the home visitor could not be blinded to group. Participants were blinded by being told that the study was examining 2 different types of information related to infant sleep to see if one was more effective. Video recording parents in both groups minimized procedural differences, helping to maintain blinding. Given the minimal procedural differences in home visits, rate of recruitment, and large urban population from which the sample was drawn, it was unlikely that study families met and/or exchanged details of the intervention. Although we did not assess whether participants could distinguish between groups; had parents been able to do so, the individualized nature of the information provided would mitigate expectation or contamination bias. Parent-child interaction outcome assessors were blinded to group assignment during coding and data analysis. There were no circumstances or adverse events that necessitated unblinding.
Measures
Because interventions for infant sleep are generally initiated based on parental perceptions of problematic sleep patterns, parental-report (subjective) measures were used to assess the impact of the intervention from the family’s perspective. Parental report of infant sleep was captured using the Brief Infant Sleep Questionnaire23,26 from both mothers and fathers. The number of night wakings as reported in the expanded version of the Brief Infant Sleep Questionnaire26 was chosen as the primary infant sleep outcome measure, as this aspect of infant sleep has been most strongly associated with parental perception of the presence of more serious infant sleep problems.23,26 Nocturnal wakefulness (wake after sleep onset), sleep latency (the time it takes to fall asleep), and the longest consolidated sleep episode were also assessed, as these have also been linked to parental perception of problematic infant sleep.23,26 We also assessed sleep duration, number of naps, and parental perception of problematic infant sleep using the Brief Infant Sleep Questionnaire.26 We measured parent-child interactions using the Parent-Child Interaction Teaching Scale to assess for the effect of the intervention in improving parent-child interactions. Based on our theoretical framework,3 we included maternal and paternal measures of potential covariates: 1) symptoms of depression,27 2) parental cognitions about infant sleep,28 3) perceptions of infant temperament,29 marital satisfaction,30 parental sense of competence,31 4) demographics, and 5) investigator-designed single items about infant feeding, use of parenting and/or sleep resources and strategies, and perceptions of effectiveness. Detailed descriptions of these measures are available in the published protocol21 and Table S2.
Procedures
In the week before the initial home visit when the infant was aged 5 months (± 2 weeks), mothers and fathers were emailed separate links to the online study questionnaire. Immediately prior to the initial home visit, the first author (E.M.K.) used an online automated simple randomization service (Sealed Envelope Ltd. London, UK) to allocate families to the intervention or comparison group using a 1:1 allocation ratio. After obtaining written consent, mothers and fathers were each video recorded with their infant in a 3- to 5-minute novel play activity, as per the Parent-Child Interaction Teaching Scale protocol.20 The family then received the Play2Sleep intervention or the comparison intervention.
At age 7 months (± 2 weeks), mothers and fathers were again emailed a separate link to the outcome study questionnaire. Only 1 family was unable to schedule their follow-up visit within the designated timeframe and completed their follow-up visit when their infant was aged 8 months. As at baseline, each parent was video recorded engaging in a structured play session with their infant.
Upon completion of the 7-month outcome home visit, we selected families (10 from each group) for interviews based on maximum variation in the change of night wakings. Using a semistructured interview guide (available upon request), EK explored parental experiences and perceptions of infant sleep and participating in the study. Interviews lasted approximately 60 minutes, were audio recorded, and transcribed verbatim. Families received a $10 gift card after each home visit.
Statistical analysis
We replaced missing values (< 1.5%) on scales with the group mean. Except for positive skewness, data met assumptions for statistical tests. We compared group differences at baseline using chi-square and independent samples t-tests and assessed for correlations between variables. We selected covariates based on significant correlation with the dependent variable at P < .01 level (2-tailed). We used a paired t-test to assess within-group differences for night wakings over time. Controlling for covariates, we used a repeated measures analysis of covariance to test whether group had an effect over time on the number of infant night wakings. We also used repeated measures analysis of covariance to test if Play2Sleep improved secondary infant sleep variables (nighttime wakefulness, daytime, nighttime, and total 24-hour sleep duration, longest self-regulated sleep period, number of naps). We applied a Bonferroni correction in SPSS using SPSS statistical software package (IBM SPSS Statistics, Version 24; Chicago, IL) to account for multiple tests. We conducted Wilcoxon signed rank test to determine the effect of the intervention on parental perception of problematic infant sleep and sleep latency. We compared Parent-Child Interactive Teaching Scale scores to normed (mothers) and reference (fathers) values using independent samples t-tests.
Qualitative analysis
E.M.K. used inductive thematic analysis32 to develop themes, which were reviewed for credibility, confirmability, and transferability by a second, more experienced coder (KB). A compare-and-contrast method was used to compare themes and supporting codes between groups (Play2Sleep or comparison). Themes and supporting codes were also contrasted between families with the least and most improvements in infant sleep, as measured by maternal and/or paternal report of decreases in infant night wakings. For context, interviewed mothers in Play2Sleep and comparison families with the most improvements reported a mean decrease of 3.4 and 2.0 night wakings, respectively. In contrast, mothers in Play2Sleep and comparison families with the least improvements reported a mean decrease of 0.2 and 0.6, respectively. To increase transferability and authenticity, preliminary code clusters, broad themes, relationships between themes, and codes were discussed with the research team, as well as local clinical experts.
RESULTS
Quantitative findings
See Table 1 for sample characteristics by group. Twelve (40%) infants in the Play2Sleep group were female and 11 (37%) infants in the comparison group were female. Mothers in the comparison group were significantly more likely to have a postgraduate degree and speak mostly English at home. Table 2 shows means and standard deviations of scale scores for mothers and fathers, by group. At baseline, mothers in Play2Sleep scored significantly higher on the Maternal Cognitions about Infant Sleep Questionnaire Anger subscale, t(1, 58) = 2.65, P = .01, and significantly lower on relationship satisfaction (brief version of the Dyadic Adjustment Scale), t(1, 49.79) = −1.96, P = .005. We found no other group differences at baseline. Sleep variables reported by mothers and fathers at baseline and outcome by group are reported in Table 3 and Table 4.
Table 1.
Participant demographic characteristics with group differences at baseline.
| Mothers (n = 60) | Fathers (n = 60) | |||||||
|---|---|---|---|---|---|---|---|---|
| Play2Sleep (n = 30) | Comparison (n = 30) | χ2 | P | Play2Sleep (n = 30) | Comparison (n = 30) | χ2 | P | |
| Parental age (years) | 5.55* | .18 | 1.38* | .98 | ||||
| < 30 | 7 (23) | 3 (10) | 3 (10) | 4 (13) | ||||
| 30–34 | 16 (53) | 21 (70) | 16 (53) | 14 (47) | ||||
| 35–39 | 7 (23) | 5 (17) | 8 (27) | 8 (27) | ||||
| ≥ 40 | 0 (0) | 1 (3) | 3 (10) | 4 (13) | ||||
| Employment | 3.41* | .70 | 2.02* | 1.00 | ||||
| Employed full-time (>30 h/wk) | 1 (3) | 2 7) | 26 (87) | 25 (83) | ||||
| Employed part-time (<30 h/wk) | 0 (0) | 2 (7) | 1 (3) | 2 (7) | ||||
| Parental leave or at-home parent | 28 (93) | 26 (87) | 0 (0) | 0 (0) | ||||
| Other (eg, student, unemployed) | 1 (3) | 0 (0) | 3 (10) | 3 (10) | ||||
| Education | 9.07* | .02 | 5.49* | .18 | ||||
| High school diploma | 0 (0) | 1 (3) | 1 (3) | 1 (3) | ||||
| Certificate or diploma after high school | 7 (23) | 2 (7) | 4 (13) | 10 (33) | ||||
| College or university degree | 19 (63) | 14 (47) | 17 (57) | 10 (33) | ||||
| Postgraduate degree | 4 (13) | 13 (43) | 8 (27) | 8 (27) | ||||
| Prefer not to answer | 0 (0) | 0 (0) | 0 (0) | 1(3) | ||||
| Ethnicity | 8.07* | .27 | 6.51* | .49 | ||||
| White (Caucasian) | 17 (57) | 22 (73) | 24 (80) | 22 (73) | ||||
| Native (eg, First Nations, Inuit, or Metis) | 1 (3) | 0 (0) | 0 (0) | 1 (3) | ||||
| Chinese | 2 (7) | 1 (3) | 2 (7) | 2 (7) | ||||
| South Asian (eg, East Indian, Pakistani, Sri Lankan) | 2 (7) | 4 (13) | 1 (3) | 3 (10) | ||||
| Latin American | 3 (10) | 0 (0) | 2 (7) | 0 (0) | ||||
| Southeast Asian (eg, Vietnamese, Cambodian, Malaysian) | 0 (0) | 1 (3) | 0 (0) | 1 (3) | ||||
| West Asian (eg, Iranian, Afghan) | 2 (7) | 0 (0) | 1 (3) | 0 (0) | ||||
| Other | 3 (10) | 2 (7) | 0 (0) | 1 (3) | ||||
| Language most spoken at home | – | .02* | – | .24 | ||||
| English | 24 (8) | 30 (100) | 27 (90) | 30 (100) | ||||
| Other | 6 (20) | 0 (0) | 3 (10) | 0 (0) | ||||
| Household income | 2.79* | 1.00 | 5.78* | .21 | ||||
| < $60,000 | 2 (7) | 1 (3) | 0 (0) | 2 (7) | ||||
| $60,000–$79,000 | 1 (3) | 1 (3) | 4 (13) | 0 (0) | ||||
| More than $80,000 | 26 (7) | 25 (83) | 24 (80) | 26 (87) | ||||
| Don't know/prefer not to answer | 1 (3) | 3 (10) | 2 (7) | 2 (7) | ||||
Values are presented as n (%). Asterisk (*) indicates that cell counts were less than 5 and Fisher’s test was used if 2 × 2. For crosstabs greater than 2 × 2, Fisher-Freeman-Halton Test is reported.
Table 2.
Maternal and paternal scale scores by group at baseline (5 months) and outcome (7 months).
| Mothers (n = 60) | Fathers (n = 60) | |||||||
|---|---|---|---|---|---|---|---|---|
| Play2Sleep (n = 30) | Comparison (n = 30) | Play2Sleep (n = 30) | Comparison (n = 30) | |||||
| Baseline | Outcome | Baseline | Outcome | Baseline | Outcome | Baseline | Outcome | |
| EPDS | 8.93 (5.10) | 5.57 (3.17) | 8.00 (4.26) | 7.60 (5.14) | 5.60 (3.44) | 5.74 (3.33) | 5.67 (4.1) | 5.60 (4.09) |
| MCISQ (total) | 45.00 (14.66) | 34.97 (16.08) | 43.00 (15.59) | 34.70 (12.45) | 34.80 (13.64) | 28.13 (12.8) | 34.87 (12.39) | 27.80 (10.64) |
| MCISQ Limits | 15.60 (4.02) | 12.77 (5.71) | 16.50 (5.89) | 13.77 (5.62) | 12.47 (5.23) | 11.07 (5.29) | 13.47 (4.75) | 10.23 (4.50) |
| MCISQ Anger | 8.00 (3.95) | 6.87 (4.57) | 5.40 (3.65) | 4.73 (2.83) | 7.70 (3.77) | 6.40 (3.74) | 6.30 (3.22) | 5.13 (2.86) |
| MCISQ Doubt | 9.33 (5.18) | 6.47 (4.56) | 8.73 (4.84) | 5.93 (3.82) | 6.63 (4.58) | 4.53 (3.77) | 6.53 (4.17) | 4.40 (3.01) |
| MCISQ Feeding | 8.40 (3.13) | 6.47 (3.34) | 8.53 (3.61) | 7.77 (3.51) | 6.10 (3.28) | 4.73 (3.23) | 6.70 (3.45) | 6.03 (3.40) |
| MCISQ Safety | 3.67 (2.54) | 2.40 (1.89) | 3.83 (2.79) | 2.50 (2.66) | 1.90 (1.83) | 1.40 (1.61) | 1.87 (1.91) | 2.00 (2.05) |
| IBQ-R-VSF | ||||||||
| Surgency | 4.21 (0.90) | 4.86 (0.69) | 4.33 (0.75) | 4.86 (0.65) | 4.33 (0.77) | 4.78 (0.81) | 4.35 (0.60) | 4.90 (0.59) |
| Negative emotionality | 4.09 (0.61) | 4.14 (0.57) | 3.98 (0.82) | 3.96 (0.84) | 3.88 (0.43) | 3.95 (0.89) | 3.95 (0.92) | 3.85 (0.98) |
| Orienting/regulatory capacity | 5.10 (0.56) | 5.07 (0.67) | 5.00 (0.58) | 5.11 (0.63) | 4.98 (0.49) | 4.91 (0.71) | 4.96 (0.73) | 4.97 (0.72) |
| DAS Total | 9.17 (1.51) | 9.30 (1.88) | 10.67 (2.32) | 9.70 (2.41) | 9.80 (2.12) | 10.23 (2.84) | 9.43 (2.57) | 9.83 (2.41) |
| PSOC Total | 70.20 (10.72) | 73.37 (12.45) | 68.83 (8.94) | 73.20 (10.38) | 69.70 (10.56) | 72.57 (12.74) | 71.63 (11.56) | 75.03 (12.41) |
| PSOC Satisfaction | 33.30 (5.98) | 35.73 (6.07) | 31.93 (4.87) | 35.40 (5.86) | 32.03 (4.99) | 33.90 (5.11) | 33.27 (5.15) | 34.77 (6.04) |
| PSOC Self Efficacy | 36.90 (6.12) | 37.63 (7.99) | 36.90 (5.71) | 37.80 (6.00) | 37.67 (7.22) | 38.67 (8.86) | 38.37 (7.89) | 40.27 (7.72) |
| Parent-child interaction | ||||||||
| Total | 53.63 (5.76) | 51.67 (5.52) | 52.03 (7.66) | 51.97 (6.66) | 51.60 (7.90) | 52.30 (6.22) | 53.70 (7.20) | 50.40 (6.02) |
| Parent Total | 37.73 (4.43) | 36.97 (4.00) | 36.43 (5.28) | 37.23 (4.81) | 35.77 (5.69) | 36.37 (5.51) | 37.70 (5.10) | 35.80 (4.33) |
| Infant Total | 15.90 (2.99) | 14.70 (3.19) | 15.60 (3.19) | 14.73 (3.41) | 15.83 (3.19) | 15.93 (2.35) | 16.00 (3.32) | 14.60 (3.08) |
| Contingency Parent | 13.50 (2.64) | 12.87 (3.41) | 12.67 (3.32) | 13.87 (2.91) | 13.13 (3.54) | 12.83 (3.51) | 13.70 (3.65) | 12.90 (3.13) |
| Contingency Infant | 7.47 (2.00) | 6.57 (1.92) | 7.20 (1.77) | 6.50 (2.08) | 7.33 (2.01) | 7.03 (1.59) | 7.47 (2.11) | 6.30 (1.84) |
Values are presented as mean (standard deviation). DAS = Brief version of the Dyadic Adjustment Scale, EPDS = Edinburgh Postnatal Depression Scale, IBQ-R-VSF = Infant Behavior Questionnaire—Revised, very short form, MCISQ = Maternal Cognitions about Infant Sleep Questionnaire, PSOC = Parental Sense of Competence Scale.
Table 3.
Maternal- and paternal-reported infant sleep characteristics at baseline (5 months) and outcome (7 months) by group.
| Mothers (n = 60) | Fathers (n = 60) | |||||||
|---|---|---|---|---|---|---|---|---|
| Play2Sleep (n = 30) | Comparison (n = 30) | Play2Sleep (n = 30) | Comparison (n = 30) | |||||
| Baseline | Outcome | Baseline | Outcome | Baseline | Outcome | Baseline | Outcome | |
| Number of night wakings | 4.20 (2.11) | 2.80 (1.69) | 3.50 (1.53) | 2.57 (1.47) | 3.33 (1.63) | 2.69 (1.66) | 3.10 (1.24) | 2.53 (1.43) |
| Nocturnal wakefulness (minutes) | 82.67 (37.85)* | 41.40 (36.39)* | 70.33 (55.10)* | 67.17 (87.02)* | 78.62 (50.65) | 50.00 (32.77) | 62.00 (30.05) | 43.62 (34.28) |
| Longest self-regulated sleep period (minutes) | 235.86 (87.27) | 309.66 (147.78) | 253.17 (106.82) | 324.57 (183.70) | 262.93 (111.98) | 303.10 (144.91) | 259.50 (83.85) | 294.66 (153.66) |
| Nighttime sleep duration (minutes) | 588.00 (64.17) | 636.93 (80.94) | 575.37 (83.00) | 625.50 (80.07) | 538.97 (118.30) | 591.72 (111.67) | 553.50 (94.73) | 606.21 (66.56) |
| Daytime sleep duration (minutes) | 164.50 (67.25) | 145.00 (45.14) | 161.50 (80.03) | 156.50 (44.16) | 147.68 (65.92) | 151.03 (82.81) | 148.83 (76.01) | 167.50 (61.04) |
| Number of naps | 3.03 (0.56) | 2.62 (0.49) | 3.02 (1.74) | 2.65 (0.59) | 3.07 (0.75)* | 2.57 (0.50)* | 2.80 (0.92)* | 2.78 (0.72)* |
| Mean nap duration (minutes) | 55.32 (24.12) | 57.31 (20.62) | 61.50 (29.19) | 60.43 (17.73) | 50.05 (21.49) | 55.30 (20.66) | 54.22 (22.98) | 61.60 (20.92) |
| Total 24-hour sleep time (minutes) | 752.50 (95.85) | 781.93 (95.39) | 736.87 (97.23) | 782.00 (103.23) | 693.04 (139.34) | 742.76 (158.09) | 702.33 (137.50) | 773.28 (77.55) |
| Length of bedtime routine (minutes) | 49.17 (25.70) | 37.67 (15.13) | 65.50 (48.00) | 49.83 (39.88) | 45.34 (24.67) | 43.33 (15.94) | 54.67 (28.86) | 38.50 (31.93) |
Values are presented as mean (standard deviation). Bold values indicate statistically significant group differences over time. Asterisk (*) indicates that cell counts were less than 5 and Fisher’s test was used if 2 × 2. For crosstabs greater than 2 × 2, Fisher-Freeman-Halton Test is reported.
Table 4.
Maternal- and paternal-reported perceptions of infant sleep at baseline (5 months) and outcome (7 months) by group.
| Mothers (n = 60) | Fathers (n = 60) | |||||||
|---|---|---|---|---|---|---|---|---|
| Play2Sleep (n = 30) | Comparison n = 30 | Play2Sleep (n = 30) | Comparison (n = 30) | |||||
| Baseline | Outcome | Baseline | Outcome | Baseline | Outcome | Baseline | Outcome | |
| Typically, how difficult is bedtime for your child, for example, fussing, crying, protesting? | ||||||||
| Very easy | 0 | 0 | 2 (7) | 2 (7) | 0 | 0 | 0 | 1 (3) |
| Somewhat easy | 9 (30) | 17 (57) | 5 (17) | 10 (33) | 4 (13) | 6 (20) | 8 (27) | 5 (17) |
| Neither easy nor difficult | 3 (10) | 4 (13) | 8 (27) | 5 (17) | 6 (20) | 14 (47) | 2 (7) | 13 (43) |
| Somewhat difficult | 13 (43) | 8 (27) | 7 (23) | 10 (33) | 16 (53) | 7 (23) | 12 (40) | 9 (30) |
| Very difficult | 5 (17) | 1 (3) | 8 (27) | 3 (10 | 4 (13) | 3 (10) | 8 (27) | 2 (7) |
| How long does it typically take your child to fall asleep at night? | ||||||||
| Less than 5 minutes | 1 (3) | 4 (13) | 2 (7) | 1 (3) | 0 | 2 (7) | 2 (7) | 0 |
| 5–15 minutes | 11 (37) | 16 (53) | 9 (30) | 18 (60) | 7 (23) | 16 (53) | 7 (23) | 16 (53) |
| 16–30 minutes | 9 (30) | 6 (20) | 6 (20) | 5 (17) | 15 (50) | 9 (30) | 10 (33) | 11 (37) |
| 31–60 minutes | 6 (20) | 2 (7) | 8 (27) | 5 (17) | 7 (23) | 3 (10) | 8 (27) | 2 (7) |
| More than 1 hour | 3 (10) | 2 (7) | 5 (17) | 1 (3) | 1 (3) | 0 | 3 (10) | 1 (3) |
| Rate how well your child usually sleeps at night | ||||||||
| Very well | 0 | 3 (10) | 0 | 2 (7) | 1 (3) | 3 (10) | 0 | 0 |
| Well | 2 (7) | 7 (23) | 0 | 4 (13) | 1 (3) | 5 (17) | 3 (10) | 6 (20) |
| Fairly well | 10 (33) | 12 (40) | 19 (63) | 16 (53) | 16 (53) | 12 (40) | 19 (63) | 17 (57) |
| Fairly poorly | 12 (40) | 4 (13) | 5 (17) | 4 (13) | 7 (23) | 9 (30) | 7 (23) | 3 (10) |
| Poorly | 5 (17) | 2 (7) | 6 (20) | 3 (10) | 3 (10) | 0 | 1 (3) | 4 (13) |
| Very poorly | 1 (3) | 2 (7) | 0 | 1 (3) | 2 (7) | 1 (3) | 0 | 0 |
| Do you consider your child’s sleep as a problem? | ||||||||
| A very serious problem | 14 (47) | 6 (20) | 7 (23) | 6 (20) | 8 (27) | 4 (13) | 6 (20) | 4 (13) |
| A small problem | 16 (53) | 18 (60) | 23 (77) | 20 (67) | 22 (73) | 17 (57) | 20 (67) | 20 (67) |
| Not a problem | 0 | 6 (20) | 0 | 4 (13) | 0 | 9 (30) | 4 (13) | 6 (20) |
Values are presented as n (%).
After adjusting for covariates (child sleep location, bed sharing after waking, and attendance at a general parenting class), mothers in Play2Sleep reported significantly more reductions in nocturnal wakefulness (minutes) over time than those in the comparison group, F(1,55) = 5.33, P = .025, partial η2 = .09. Compared to fathers in the comparison group, fathers in Play2Sleep reported a significant decrease over time in the number of infant naps, F(1,58) = 4.90, P = .03, partial η2 = .08 (no covariates). We found significant improvements over time in parental rating of problematic infant sleep for both mothers and fathers in the Play2Sleep (based on negative ranks, Z = −2.82, P = .005; based on positive ranks, Z = −3.19, P = .001), whereas no such improvements over time were observed in the comparison group (Table 4).
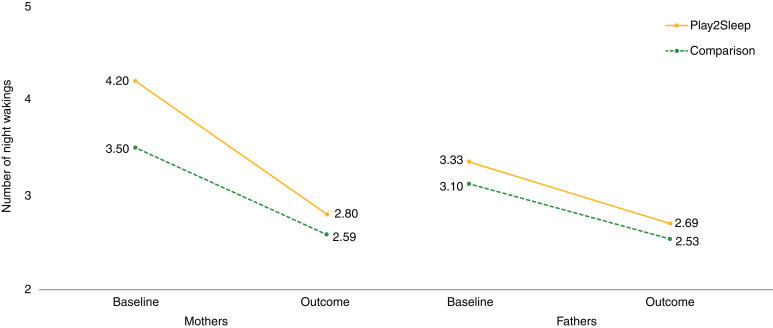
There were significant within-group decreases in the number of night wakings over time in both the Play2Sleep group (as reported by mothers, t(29) = 3.58, P = .001; as reported by fathers, t(29) = 2.29, P = .03) and the comparison group (as reported by mothers t(29) = 3.92, P < .001; as reported by fathers, t(29) = 2.43, P = .02). After adjusting for covariates (child sleep location, child falling asleep by self in own crib/bed, ethnicity, English spoken at home, and Maternal Cognitions about Infant Sleep Questionnaire total score), we found no significant differences between groups over time in the number of night wakings reported by mothers, F(1,53) = 1.59, P = .21, partial η2 = .03 (Figure 2). Similarly, after adjusting for covariates (father Maternal Cognitions about Infant Sleep Questionnaire Limits subscale score, infant sleep surface, and child falling asleep by self in own crib/bed), we found no significant differences between groups over time in the number of night wakings reported by fathers, F(1,55) = 0.36, P = .85, partial η2 = .001 (Figure 2).
Figure 2. Parent-reported night wakings by group at baseline and outcome.
(Left) Maternal-reported number of night wakings by group at baseline and outcome (covariates = child sleep location, child falling asleep by self in own crib/bed, ethnicity, English spoken at home, and MCISQ total score). (Right) Paternal-reported number of night wakings by group at baseline and outcome (covariates = father MCISQ Limits, infant sleep surface, child falling asleep by self in own crib/bed). MCISQ = Maternal Cognitions about Infant Sleep Questionnaire.
We found no other significant group differences for any of the remaining infant sleep variables. However, the prevalence of mothers considered high risk for postpartum depression (>12; 28.3%) was more than 9 times than the 3% reported for a Canadian cohort sample within the same setting33 and nearly double the typical 10–15% prevalence rate.34 As such, we conducted unplanned post hoc exploratory analyses to assess the effect of Play2Sleep on parental depression. Using a repeated measure analysis of variance we found that there was a significant effect for mother’s depression symptoms, F(1,58) = 8.5, P = .005, partial η2 = .13.
Compared to normed reference Parent-Child Interaction Teaching Scale scores,20 mothers in the present study had significantly lower baseline scores on the total score and parent domain score, as well as lower scores in all parent domain subscales (Table S2). Compared to reference values,13 fathers in the present study had significantly lower scores on the total score, parent domain, and infant domain total scores, as well as the social emotional growth fostering, both infant subscales (clarity of cues and responsiveness to caregiver), and contingency subscales for both the father and infant.
Qualitative themes
To explain the quantitative findings, 3 qualitative themes were developed, including 1) information overwhelm, 2) learning infant cues, and 3) working together with a subtheme of father involvement (Table 5).
Table 5.
Inductively developed themes to explain effectiveness of Play2Sleep.
| Information Overwhelm |
| Mother: [W]e’ve just recognized that there’s a lot of information out there. A lot of expectations, the social expectations that are imposed on us especially from others. You know, you kind of have to just disregard a lot of it.” (Play2Sleep most improved) |
| Father: [T]here is a lot of contradicting information on the web too. The problem is you gotta take it with a very large grain of salt. For everything you read you’ll find something else that contradicts it. It’s hard to figure out which ones are valid.” (Play2Sleep least improved) |
| Mother: [B]ecause there’s just so much overwhelming and conflicting information that it was really hard to figure out.…We knew that we didn’t want him to nurse to sleep but then didn’t really know how to fix it. I found it really overwhelming with the sleep stuff because there’s so many books and not one of them says like the same thing as the other one…. But it’s hard if they haven’t met your baby and you can’t ask specific questions like we could with [home visitor]. (Comparison most improved) |
| Learning About Infant Cues |
| Mother: I had a really hard time figuring out what those [early cues] were before watching the video. So, I’ve found that’s really helped me cuz I’m really visual, be really aware of what those cues are. I think that’s why we’ve been successful the majority of the time putting him down for a nap and him just going straight down because of that….understanding cues ahead of time is really, really important and something we immediately started applying.…I think there is this misinformation when you are having a child that, like, you’re gonna get to know your child so well that you know, every cry they make or every motion they make you’re gonna know what it means. I feel like that’s a bit of a fallacy. Like there’s so much that’s thrown at you. You try your best but there’s only so much you can figure out by yourself.” (Play2Sleep most improved) |
|
Mother: I think I remember the, I think we covered pulling the ears at one point in one of the visits. Cuz I vaguely remember that from somewhere. I can’t remember if it was the book, or one of the visits…. Father: I read it and was trying to do stuff but you [to mother] were just so exhausted at that point the reception was just not there (Play2Sleep least improved) |
| Mother: For so long we were waiting for her to cue us in when she was hungry, when she was sleepy, um, but now it’s the time of day. If it’s this time of day, we feed her. So, I know what I need to be doing, making food or getting her bath ready or anything like that. So, it’s made our lives a little bit easier. She’s reacted ok to that. The sleep thing is during the day she’s amazing but as soon as you try and get her to that long sleep she turns into a monster. (Comparison least improved) |
| Working Together |
| Mother: I would get up with her and [father] would sleep in the night. I think there was one time or two times that I woke you [to father] up because I was like really frustrated but mostly it was just me and her. So, it was really helpful once you were on, not that you weren’t on board before but once we decided we were doing this together, to have that support. To have both of us doing it at the same time.…When he was home, I could go for sleeps. We’ve always had a good relationship, never, like we were resentful or anything. But I would say yeah in the last few weeks it does feel like we’re more of a team. (Play2Sleep most improvement) |
|
Mother: [T]hat was really taking a toll I found, at least I found on our relationship because I was getting super frustrated because it was always me that had to put him down obviously cuz [father] would try to shush him or whatever but it just didn’t work…. Father: Different philosophies to putting the baby down. (Play2Sleep least improved) |
|
Father: She’s not getting any sleep and it’s affecting her day, and then she’s screaming at night and it kind of led to, you know, some arguments about what I felt is right and what she felt is right…. Mother: Yes, of course you wanna be on the same page but if you have completely different viewpoints how do you get, while still managing the day to day, how do you get to the same page, or how do you come to an agreement that this is how you’re going to move forward? (Comparison least improved) |
| Father Involvement |
|
Father: If I get to do the routine, we get more time together and it means he’s more used to me putting him to sleep so [mother] doesn’t have to do it every night…. when I put him to bed when we were on holidays, he seemed to sleep a little better and I kind of was like “Oh I’m actually not terrible at this at all”. I can actually do it quite well.…I really felt I hit my stride when we were when I was doing it every other night and stuff. We’re trying to do that now, I do it a couple of times a week if possible, here. It’s really part of my routine as well, putting him to bed. It’s, I’m annoyed at myself for not doing it earlier cuz “Oh this is great, I got some quality time with my son”.…It’s nice that he lets me put him to sleep so I’m happy with that.… Mother: [A]nd then helping put him to bed. Um, that was nice because it shared, it lifted some of the burden off me and then I could you know, get a drink or eat myself. So, I think that was nice when you were able to start doing that. I think that was my proud moment of being proud of [father] for being, you know, taking the initiative as well to do it. It wasn’t like me asking, he would just be like “C’mon then let’s go up to bed” …. Father: I know his tells. That’s something that I’m actually very happy, kind of proud about, I, I feel like I know him a bit better now and I know what cues to look for. (Play2Sleep most improved) |
| Father: By the time I was getting home baby was almost already going to bed. Like there were nights …. when I was getting home at like 6 o’clock so then baby, I get home just in time to wrap up baby and put her to bed. Then I’d be postcall, so I’d be sleeping all day.…when I was here it was just for like a very brief moment when she was still awake. (Play2Sleep least improved) |
|
Mother: You got her down twice, on your own without me. Father: I’ve done more than twice actually. Mother: Well not at that time, I’m proud of that because it’s always me. I always have to get her down, it has to be me, and he did it twice I remember. Father: I did it more than twice. Mother: Those two times stood out for me because it was over an hour long. The first time was like an hour and then the next time was 45 minutes. So, the fact that he was able to get her down…. I think he tried this morning without me and she was sort of getting sleepy? No? She was quiet though. Father: I got her to be quiet. (Play2Sleep least improved) |
| Mother: I think I always rushed in and said, “No it’s my job, it’s my job, give her to me”. That wasn’t fair to either of us so now I try to take a little bit more time to kind of say like, No grandma’s here, [father] is here, whoever is here they can deal with it until such a point that I feel like I can’t deal with it anymore. So, we’re trying to redefine the roles and the responsibilities in the relationship and try to get it as 50/50 as we can. Sleep ultimately you can’t do it to a certain degree because of the approach that we’re taking and because of the hours he works. But everything else we try. (Comparison least improved) |
Information overwhelm
Nearly all parents, regardless of group allocation (ie, Play2Sleep or comparison) or changes in infant night wakings (ie, the most vs least improvements in infant night wakings) described experiences and frustrations with an overwhelming number of potential information sources (external to the study) on infant sleep (eg, books, blogs, providers, friends/family). The breadth of accessible infant sleep information, particularly that found on the internet, was described as overwhelming, contradictory, and often subjective (being based in personal opinions, philosophies, or social expectations). Parents reported that finding credible sources (such as the home visitor or trusted friends who were experienced parents) was helpful in improving their infant’s sleep. Conflicting information hindered parental ability to improve infant sleep, while information provided by sources perceived as credible facilitated infant sleep improvements. Despite the overwhelming amount of information parents received external to the study, Play2Sleep parents who reported the greatest improvements in infant night wakings described the video feedback process as an effective strategy to gain new knowledge about their infant’s cues. Play2Sleep parents with least improvements had minimal recollections of the infant cue information and more often recollected broader parenting suggestions related to daytime play activities instead.
Learning infant cues
While parents from both allocation groups commented on learning to respond to their infant, Play2Sleep parents with the greatest improvements described how they were immediately able to implement learning about infant cues. These parents described how they were immediately able to recognize more subtle cues, and this translated to improved ability in helping their infant with state regulation (not just sleep) and success in timing and anticipating sleep need (particularly with naps). These parents gained new appreciation about their infant’s capacity to communicate and reflected they may have previously misinterpreted infant disengagement cues as feeding cues. Parents were proud of their enhanced ability better to understand and interpret their infant’s cues and described how this skill helped them get to know their baby better. In contrast, Play2Sleep parents with least improvements did not remember (to the same intensity) discussing their infant’s cues. These parents did not typically generalize information beyond daytime (awake) periods and appeared more likely to retain information related to pacing activities or play-specific interactions. They did not report this information translating into a feeling of knowing their baby better. In addition to infant cues, these parents used the time of day to determine sleep-related activities. In the comparison group, parents with the most improvements described that they learned how to interpret their infant’s cues (cries) more accurately as they became more experienced parents and their infant got older, whereas parents reporting the least improvements described using the time of day to judge when to put their infant to bed.
Working together
Parents with the most improvements in infant sleep from the Play2Sleep and comparison groups described the importance of working together in a process of “getting on the same page” or becoming more of a team in their efforts to improve their infant’s sleep. In contrast, this theme was absent when parents reported less improvements in infant night wakings. Parents with more improvements appeared more likely to agree with each other’s parenting practices and philosophies, whereas parents with least improvements would more often describe how their parenting approaches and philosophies were different. A key component of working together was the subtheme father involvement.
Father involvement
Regardless of group allocation, parents with the greatest improvements in infant sleep discussed the experience and value of fathers becoming more involved in sleep-related parenting practices and decisions. This involvement facilitated and reinforced the ability of parents to be working together. These parents described how fathers started taking a more active role in bedtime routines, either by taking turns or taking over bedtime routines entirely, and that their infant responded differently to fathers’ efforts to put them down to sleep due to differing expectations from their infant, mainly relating to breastfeeding. Both mothers and fathers reporting greater improvements in infant sleep described feeling more confident in fathers’ abilities. For Play2Sleep parents, learning infant cues was helpful in building fathers’ infant care skills and facilitated confidence in fathers’ abilities. In contrast, fathers reporting less improvement in infant night wakings describe being less involved in their infant’s sleep and bedtime routines, often due to work schedules, strong infant feeding-to-sleep associations, and/or deferral to the mother as the primary caregiver. These fathers had erratic or irregular success in helping their infant fall asleep and there was less emphasis of how fathers’ abilities had improved and little descriptions of how either mothers or fathers had increased confidence in the father’s ability to put the infant to sleep.
DISCUSSION
To our knowledge, this is the first attempt to experimentally manipulate parent-child interactions to evaluate the effect of these interactions on infant sleep difficulties. This mixed-methods study demonstrated Play2Sleep was effective in reducing maternal-reported duration of infant nocturnal wakefulness and the number of paternal-reported infant naps. While the number of parent-reported night wakings significantly decreased in both groups over time, the rate of this decrease over time was not significantly greater in the Play2Sleep group. There were significant improvements in the parental rating of problematic infant sleep in the Play2Sleep group that were not reported in the comparison group. Qualitative themes of information overwhelm, learning infant cues, and working together explain the quantitative results.
Too much, too little, and too late
Parents from the Play2Sleep group who experienced the greatest improvements in their infant’s sleep qualitatively reported that the individualized video feedback on infant cues increased their confidence and ability to read their infant’s sleep and social cues more accurately. However, no statistically significant improvements in parent-child interactions were achieved. This contrast suggests that while the dose of the Play2Sleep intervention may have been adequate to increase parental knowledge, it was too small to achieve quantifiable changes in actual parent-child interaction behavior. The finding that Play2Sleep significantly reduced maternal-reported nocturnal wakefulness is promising, as infant nocturnal wakefulness is associated with cognitive growth trajectories.35 However, it is possible that Play2Sleep may have only helped mothers more accurately identify what infant behavioral cues were indicative of a waking state, rather than change the actual duration of infant wakefulness. This inference would be consistent with the idea that the single dose of Play2Sleep was enough to influence parental knowledge, albeit not strong enough improve everyday parent-child interactions and subsequent changes in infant sleep. Up to four doses of similar interventions have been required to influence parent-child interactions in fathers of infants born preterm.36 As there were no group differences with other maternal-reported infant sleep variables (night wakings, sleep duration and latency), additional research to find the appropriate dose of Play2Sleep will require use of measures that assess parental knowledge of infant states and interaction, as well as objective infant sleep measures (ie, actigraphy).
The ability to translate information into measurable changes in parent-child interaction may have been hindered by “information overwhelm”, as well as the breadth of information presented during the single Play2Sleep home visit and additional parent factors, such as parental sleep disruption, fatigue, and/or mental health concerns. Although we did not measure parental sleep or fatigue, we did assess parental mental health, which is known to influence parental perspectives of infant behavior.37 The relationship between infant sleep and maternal depression is well-established, and it was not unexpected to have high rates of postpartum depression symptoms in a sample experiencing infant sleep difficulties. Over 50% of mothers presenting to an inpatient service for sleep difficulties had postpartum depression.14 It is possible that the improvements in nocturnal wakefulness and/or parental perception of problematic infant sleep may be attributed to improvements in maternal depression symptoms, rather than actual changes in infant sleep. Although improved postpartum depression symptoms could be both a result of and contributor to improved infant sleep,4 accurate parental assessment of infant wakefulness and distress may be an intermediary step to improving parent-child interactions and preventing sleep disturbances during the early postpartum period.38 This explanation suggests that families experiencing infant sleep problems need more than a brief intervention approach to improve parent-child interactions. Information may be more effectively delivered in a series of sessions, as has been used to improve parent-child interaction in more high risk and vulnerable populations.39 Interventions may be further strengthened by incorporating additional active strategies into parental education components, such as supervised practice with return demonstration of parent-child interaction skills, which has been identified as a key component of early intervention programs for parents of infants born preterm.40
Our findings demonstrated that families who are experiencing infant sleep difficulties may already be at risk of lower overall quality parent-child interactions at age 5 months. This speaks to the need for early intervention to support families who express concerns with sleep-specific parenting practices or parent-child interactions. In the present study, mean maternal-infant dyad scores were lower across multiple parent, but not infant, domains of interaction. In contrast, mean paternal-infant scores were lower for only 1 parent domain (social-emotional growth fostering) but both infant domains (clarity of cues and responsiveness to caregiver). Further research is needed to determine if these results are consistent in more diverse groups and whether interventions should focus on specific aspects of parent-child interactions (ie, sensitivity to cues, social emotional growth fostering) and whether these targets should differ between mothers and fathers. Given that the current sample had relatively few risk factors for poorer quality parent-child interaction (eg, relatively high levels of education, infants born full term), we would expect lower scores on parent-child interaction quality in families with additional risk factors (eg, lower levels of parental education, infants born preterm).
The timing of the Play2Sleep intervention may have been delivered too late for families to capitalize on the effects of improving parent-child interactions on sleep. Given that infant sleep duration may moderate how infants differentially respond to sensitive maternal caregiving,41 patterns of interaction may have been so well-established that the single dose of Play2Sleep at age 5 months was insufficient to overcome these interaction patterns. Delivering interventions to improve parent-child interactions earlier may also enhance parental emotional availability at bedtime, which has been linked to infant sleep.12,42,43 These interventions could be delivered as early as the newborn period. For instance, mothers of preterm infants who received intensive (7 sessions over approximately 2 weeks) training in infant cues, states, and interaction reported improved mother-infant interactions and fewer sleep problems at age 3 months.17 Accordingly, future research could explore prevention approaches that incorporate elements of parent-child interaction training into prenatal education and/or in the early perinatal period.
Working together to improve infant sleep
Families with more infant sleep improvements tended to describe experiences of working together and that the father was able to take a more active role in sleep-related parenting practices (ie, taking over the bedtime routine). In Play2Sleep families, learning infant cues may have helped to foster father involvement, helping parents to work together. This supports other literature describing how broader father involvement in daytime caregiving predicts improved sleep for both mothers and infants.44,45 Given that there were no statistically significant changes in father-reported mean nap duration or total daytime sleep duration, it is possible that the father-reported decrease in the number of naps may represent improved nap consolidation. That is, increased father involvement could have led to fewer, but longer, infant naps. However, it is also possible that this difference represents more accurate reporting of the number of infant naps by fathers, which could also have been facilitated by increased father involvement. Given that the majority of mothers in this study were on parental leave (90%), which is offered up to 50 weeks postpartum in Canada, and none of the families reported starting formal paid childcare, it is possible that increased father involvement may have also reduced maternal stress associated with daytime caregiving.
For fathers in this study to become more actively involved in sleep-related practices, it appeared that both parents needed to have some degree of confidence in the father’s ability to soothe and settle his infant. Such a finding is consistent with literature that describes how maternal beliefs about father’s roles46 and maternal encouragement47 may moderate the level of paternal involvement. Our study highlights the importance of building positive paternal caregiving experiences, as success in putting their infant to sleep reinforced their confidence and involvement, while unsuccessful attempts diminished confidence and overall involvement. As confidence in paternal abilities diminish, families may develop a pattern whereby mothers engage in gatekeeping and fathers become less involved.48 Future infant sleep interventions should integrate purposeful strategies to enhance coparenting as a means of promoting fathers’ abilities and confidence related to general and sleep-related parenting behaviors.
Limitations
Although the study was adequately powered, it was limited by a relatively small sample size whereby random allocation resulted in baseline group differences. We did not assess if participants knew each other or could distinguish between the 2 groups and cannot exclude potential expectation or contamination bias. With masking (ie, similar procedures with each group), recruitment in a large center, and phased recruitment, it is unlikely that this occurred. The use of parental report tends to underestimate nocturnal wakefulness compared to objective sleep measures,49 and our findings are limited to parental perception of infant sleep. While such parent-reported outcomes are helpful in understanding impact of interventions and treatments on individual and family health-related quality of life,50 future research should include objective measures of infant sleep, such as actigraphy, to assess the effects of Play2Sleep. In light of the findings related to the decreases in maternal depression associate with Play2Sleep, it would have been helpful to determine whether either parent had started treatment for mental health concerns; however, we did not collect this information. Although no parents identified any developmental delays, we did not conduct developmental screening or assessment. Future research should consider assessment of developmental delays. Lastly, this study was limited to first-born term infants of cohabiting heterosexual couples and our convenience sample likely contributed to a selection bias that resulted in a sample of parents with relatively high income and education levels. Although these inclusion criteria limited potential confounders, such as parenting experience, these limitations reduce the generalizability of the results. These findings may be best generalized to other first-time parents and additional research could explore the effect of Play2Sleep in parents who have had additional infant caregiving experience with prior children. Future research should also include more diverse parent groups. While these findings indicate that Play2Sleep may hold promise as an intervention, additional refinement and testing is needed.
CONCLUSIONS
The Play2Sleep intervention shows promise to reduce infant sleep disturbances, and parents valued learning how to accurately identify and respond to their infant’s sleep and social disengagement cues. Adaptations in the dose, delivery, and timing of Play2Sleep may increase the effectiveness in improving additional infant sleep characteristics.
DISCLOSURE STATEMENT
All authors have seen and approved this manuscript. Work for this study was performed at University of Calgary. E.M.K. was supported by a Pre-Doctoral Canadian Child Health Clinician Scientist Program Award, Alberta Children’s Hospital Research Institute—Canadian Institute for Health Research Training Program, Alberta Children’s Hospital Foundation, and an Alberta Innovates—Health Solutions Clinician Fellowship (#201504). The authors report no conflicts of interest.
ACKNOWLEDGMENTS
The authors gratefully acknowledge the families who participated in the Play2Sleep Study and express their gratitude to the community health center nurses and staff who assisted with recruitment and Jana Kurilova for her technical assistance in the quantitative data analysis. Author contributions: Dr. Keys conceptualized and designed the study, collected and analyzed data, drafted the initial manuscript. Dr. Benzies conceptualized and designed the study, supervised all data collection and analyses. Drs. Kirk and Duffett-Leger critically reviewed the study design, and data analyses. All authors reviewed and approved the final version of the submitted manuscript.
REFERENCES
- 1. Sadeh A , De Marcas G , Guri Y , Berger A , Tikotzky L , Bar-Haim Y . Infant sleep predicts attention regulation and behavior problems at 3-4 years of age . Dev Neuropsychol. 2015. ; 40 ( 3 ): 122 – 137 . [DOI] [PubMed] [Google Scholar]
- 2. Sun W , Li SX , Jiang Y , et al . A community-based study of sleep and cognitive development in infants and toddlers . J Clin Sleep Med. 2018. ; 14 ( 6 ): 977 – 984 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Keys EM , Benzies KM . A proposed nursing theory: Infant sleep and development . Nurs Sci Q. 2018. ; 31 ( 3 ): 279 – 286 . [DOI] [PubMed] [Google Scholar]
- 4. Sadeh A , Tikotzky L , Scher A . Parenting and infant sleep . Sleep Med Rev. 2010. ; 14 ( 2 ): 89 – 96 . [DOI] [PubMed] [Google Scholar]
- 5. Meltzer LJ , Mindell JA . Systematic review and meta-analysis of behavioral interventions for pediatric insomnia . J Pediatr Psychol. 2014. ; 39 ( 8 ): 932 – 948 . [DOI] [PubMed] [Google Scholar]
- 6. Douglas PS , Hill PS . Behavioral sleep interventions in the first six months of life do not improve outcomes for mothers or infants: a systematic review . J Dev Behav Pediatr. 2013. ; 34 ( 7 ): 497 – 507 . [DOI] [PubMed] [Google Scholar]
- 7. Tse L , Hall W . A qualitative study of parents’ perceptions of a behavioural sleep intervention . Child Care Health Dev. 2008. ; 34 ( 2 ): 162 – 172 . [DOI] [PubMed] [Google Scholar]
- 8. Bordeleau S , Bernier A , Carrier J . Longitudinal associations between the quality of parent-child interactions and children’s sleep at preschool age . J Fam Psychol. 2012. ; 26 ( 2 ): 254 – 262 . [DOI] [PubMed] [Google Scholar]
- 9. Beijers R , Jansen J , Riksen-Walraven M , de Weerth C . Attachment and infant night waking: a longitudinal study from birth through the first year of life . J Dev Behav Pediatr. 2011. ; 32 ( 9 ): 635 – 643 . [DOI] [PubMed] [Google Scholar]
- 10. Higley E , Dozier M . Nighttime maternal responsiveness and infant attachment at one year . Attach Hum Dev. 2009. ; 11 ( 4 ): 347 – 363 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Priddis LE . Tuned in parenting and infant sleep patterns . Early Child Dev Care. 2009. ; 179 ( 3 ): 259 – 269 . [Google Scholar]
- 12. Teti DM , Kim BR , Mayer G , Countermine M . Maternal emotional availability at bedtime predicts infant sleep quality . J Fam Psychol. 2010. ; 24 ( 3 ): 307 – 315 . [DOI] [PubMed] [Google Scholar]
- 13. Harrison MJ , Magill-Evans J , Benzies K . Fathers’ scores on the Nursing Child Assessment Teaching Scale: are they different from those of mothers? J Pediatr Nurs. 1999. ; 14 ( 4 ): 248 – 254 . [DOI] [PubMed] [Google Scholar]
- 14. Črnčec R , Cooper E , Matthey S . Treating infant sleep disturbance: does maternal mood impact upon effectiveness? J Paediatr Child Health. 2010. ; 46 ( 1-2 ): 29 – 34 . [DOI] [PubMed] [Google Scholar]
- 15. Matthey S , Speyer J . Changes in unsettled infant sleep and maternal mood following admission to a parentcraft residential unit . Early Hum Dev. 2008. ; 84 ( 9 ): 623 – 629 . [DOI] [PubMed] [Google Scholar]
- 16. Treyvaud K , Rogers S , Matthews J , Allen B . Outcomes following an early parenting center residential parenting program . J Fam Nurs. 2009. ; 15 ( 4 ): 486 – 501 . [DOI] [PubMed] [Google Scholar]
- 17. Newnham CA , Milgrom J , Skouteris H . Effectiveness of a modified Mother-Infant Transaction Program on outcomes for preterm infants from 3 to 24 months of age . Infant Behav Dev. 2009. ; 32 ( 1 ): 17 – 26 . [DOI] [PubMed] [Google Scholar]
- 18. Wu Y-C , Leng C-H , Hsieh W-S , et al . A randomized controlled trial of clinic-based and home-based interventions in comparison with usual care for preterm infants: effects and mediators . Res Dev Disabil. 2014. ; 35 ( 10 ): 2384 – 2393 . [DOI] [PubMed] [Google Scholar]
- 19. Bronfenbrenner U , editor. Making Human Beings Human: Bioecological Perspectives on Human Development. Thousand Oaks, CA: : Sage; ; 2005. . [Google Scholar]
- 20. Oxford ML , Findlay DM . NCAST Caregiver/Parent-Child Interaction Teaching Manual. Seattle, WA: : NCAST Progams, University of Washington, School of Nursing; ; 2013. . [Google Scholar]
- 21. Keys E , Benzies K , Kirk V , Duffett-Leger L . Using play to improve infant sleep: A mixed methods protocol to evaluate the effectiveness of the Play2Sleep intervention . Front Psychiatry. 2018. ; 9 : 109 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schulz KF , Altman DG , Moher D ; CONSORT Group . CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials . Trials. 2010. ; 11 ( 1 ): 32 . [PMC free article] [PubMed] [Google Scholar]
- 23. Sadeh A . A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample . Pediatrics. 2004. ; 113 ( 6 ): e570 – e577 . [DOI] [PubMed] [Google Scholar]
- 24. Hall WA , Clauson M , Carty EM , Janssen PA , Saunders RA . Effects on parents of an intervention to resolve infant behavioral sleep problems . Pediatr Nurs. 2006. ; 32 ( 3 ): 243 – 250 . [PubMed] [Google Scholar]
- 25. Mindell JA , Du Mond CE , Sadeh A , Telofski LS , Kulkarni N , Gunn E . Efficacy of an internet-based intervention for infant and toddler sleep disturbances . Sleep. 2011. ; 34 ( 4 ): 451 – 458 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sadeh A , Mindell JA , Luedtke K , Wiegand B . Sleep and sleep ecology in the first 3 years: a web-based study . J Sleep Res. 2009. ; 18 ( 1 ): 60 – 73 . [DOI] [PubMed] [Google Scholar]
- 27. Cox JL , Holden JM , Sagovsky R . Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale . Br J Psychiatry. 1987. ; 150 ( 6 ): 782 – 786 . [DOI] [PubMed] [Google Scholar]
- 28. Morrell JM . The role of maternal cognitions in infant sleep problems as assessed by a new instrument, the maternal cognitions about infant sleep questionnaire . J Child Psychol Psychiatry. 1999. ; 40 ( 2 ): 247 – 258 . [PubMed] [Google Scholar]
- 29. Putnam SP , Helbig AL , Gartstein MA , Rothbart MK , Leerkes E . Development and assessment of short and very short forms of the infant behavior questionnaire—revised . J Pers Assess. 2014. ; 96 ( 4 ): 445 – 458 . [DOI] [PubMed] [Google Scholar]
- 30. Sabourin S , Valois P , Lussier Y . Development and validation of a brief version of the dyadic adjustment scale with a nonparametric item analysis model . Psychol Assess. 2005. ; 17 ( 1 ): 15 – 27 . [DOI] [PubMed] [Google Scholar]
- 31. Johnston C , Mash EJ . A measure of parenting satisfaction and efficacy . J Clin Child Psychol. 1989. ; 18 ( 2 ): 167 – 175 . [Google Scholar]
- 32. Braun V , Clarke V . Thematic Analysis . In: Cooper H , Camic PM , Long DL , Panter AT , Rindskopf D , Sher KJ , eds. APA Handbook of Research Methods in Psychology, Vol 2: Research Designs: Quantitative, Qualitative, Neuropsychological, and Biological. Washington, DC: : American Psychological Association; ; 2012. : 57 – 71 . [Google Scholar]
- 33. Premji S , McDonald SW , Metcalfe A , et al . Examining postpartum depression screening effectiveness in well child clinics in Alberta, Canada: a study using the All Our Families cohort and administrative data . Prev Med Rep. 2019. ; 14 : 100888 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. O’Hara MW , Swain AM . Rates and risk of postpartum depression—a meta-analysis . Int Rev Psychiatry. 1996. ; 8 ( 1 ): 37 – 54 . [Google Scholar]
- 35. Pisch M , Wiesemann F , Karmiloff-Smith A . Infant wake after sleep onset serves as a marker for different trajectories in cognitive development . J Child Psychol Psychiatry. 2019. ; 60 ( 2 ): 189 – 198 . [DOI] [PubMed] [Google Scholar]
- 36. Benzies K , Magill-Evans J , Kurilova J , Nettel-Aguirre A , Blahitka L , Lacaze-Masmonteil T . Effects of video-modeling on the interaction skills of first-time fathers of late preterm infants . Infants Young Child. 2013. ; 26 ( 4 ): 333 – 348 . [Google Scholar]
- 37. Tikotzky L , Chambers AS , Gaylor E , Manber R . Maternal sleep and depressive symptoms: links with infant Negative Affectivity . Infant Behav Dev. 2010. ; 33 ( 4 ): 605 – 612 . [DOI] [PubMed] [Google Scholar]
- 38. Voltaire ST , Teti DM . Early nighttime parental interventions and infant sleep regulation across the first year . Sleep Med. 2018. ; 52 : 107 – 115 . [DOI] [PubMed] [Google Scholar]
- 39. Anis L , Letourneau NL , Benzies K , Ewashen C , Hart MJ . Effect of the attachment and child health parent training program on parent–child interaction quality and child development . Can J Nurs Res. 2020. ; 52 ( 2 ): 157 – 168 . [DOI] [PubMed] [Google Scholar]
- 40. Benzies KM , Magill-Evans JE , Hayden KA , Ballantyne M . Key components of early intervention programs for preterm infants and their parents: a systematic review and meta-analysis . BMC Pregnancy Childbirth. 2013. ; 13 ( Suppl 1 ): S10 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bernier A , Bélanger ME , Tarabulsy GM , Simard V , Carrier J . My mother is sensitive, but I am too tired to know: infant sleep as a moderator of prospective relations between maternal sensitivity and infant outcomes . Infant Behav Dev. 2014. ; 37 ( 4 ): 682 – 694 . [DOI] [PubMed] [Google Scholar]
- 42. Philbrook LE , Teti DM . Bidirectional associations between bedtime parenting and infant sleep: Parenting quality, parenting practices, and their interaction . J Fam Psychol. 2016. ; 30 ( 4 ): 431 – 441 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Jian N , Teti DM . Emotional availability at bedtime, infant temperament, and infant sleep development from one to six months . Sleep Med. 2016. ; 23 ( Suppl C ): 49 – 58 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Tikotzky L , Sadeh A , Volkovich E , Manber R , Meiri G , Shahar G . Infant sleep development from 3 to 6 months postpartum: links with maternal sleep and paternal involvement . Monogr Soc Res Child Dev. 2015. ; 80 ( 1 ): 107 – 124 . [DOI] [PubMed] [Google Scholar]
- 45. Tikotzky L , Sadeh A , Glickman-Gavrieli T . Infant sleep and paternal involvement in infant caregiving during the first 6 months of life . J Pediatr Psychol. 2011. ; 36 ( 1 ): 36 – 46 . [DOI] [PubMed] [Google Scholar]
- 46. McBride BA , Brown GL , Bost KK , Shin N , Vaughn B , Korth B . Paternal identity, maternal gatekeeping, and father involvement . Fam Relat. 2005. ; 54 ( 3 ): 360 – 372 . [Google Scholar]
- 47. Schoppe-Sullivan SJ , Brown GL , Cannon EA , Mangelsdorf SC , Sokolowski MS . Maternal gatekeeping, coparenting quality, and fathering behavior in families with infants . J Fam Psychol. 2008. ; 22 ( 3 ): 389 – 398 . [DOI] [PubMed] [Google Scholar]
- 48. Fagan J , Barnett M . The relationship between maternal gatekeeping, paternal competence, mothers’ attitudes about the father role, and father involvement . J Fam Issues. 2003. ; 24 ( 8 ): 1020 – 1043 . [Google Scholar]
- 49. Tikotzky L , Volkovich E . Infant nocturnal wakefulness: a longitudinal study comparing three sleep assessment methods . Sleep. 2019. ; 42 ( 1 ):1–12. [DOI] [PubMed] [Google Scholar]
- 50. Deshpande PR , Rajan S , Sudeepthi BL , Abdul Nazir CP . Patient-reported outcomes: a new era in clinical research . Perspect Clin Res. 2011. ; 2 ( 4 ): 137 – 144 . [DOI] [PMC free article] [PubMed] [Google Scholar]