Abstract
Study Objectives:
To evaluate the impact of the coronavirus disease 2019 (COVID-19) pandemic on insomnia and other sleep disturbances in health care professionals.
Methods:
A survey was distributed using social media and organizational emails to Brazilian active health care professionals during the COVID-19 outbreak. We explored potential associated factors including age, sex, occupation, workplace, work hours, income, previous infection with COVID-19, recent/current contact with COVID-19 patients, regional number of incident deaths, anxiety, and burnout. We evaluated new-onset/previous insomnia worsening episodes (primary outcome), new pharmacological treatments, sleep quality, duration, nightmares, and snoring (secondary outcomes).
Results:
A total of 4,384 health professionals from all regions of the country were included in the analysis (44 ± 12 years, 76% females, 53.8% physicians). Overall, 55.7% were assisting patients with COVID-19, and 9.2% had a previous COVID-19 infection. The primary outcome occurred in 32.9% of respondents in parallel to 13% new pharmacological treatments for insomnia. The sleep quality worsened for 61.4%, while 43.5% and 22.8% reported ≥ 1-hour sleep duration reduction and worsening or new-onset nightmares, respectively. Multivariate analyses showed that age (odds ratio [OR]: 1.008; 95% confidence interval [CI] 1.001–1.015), females (OR: 1.590; 95% CI 1.335–1.900), weight change (decrease: OR: 1.772; 95% CI 1.453–2.161; increase: OR: 1.468; 95% CI 1.249–1.728), prevalent anxiety (OR: 3.414; 95% CI 2.954–3.948), new-onset burnout (OR: 1.761; 95% CI 1.489–2.083), family income reduction > 30% (OR: 1.288; 95% CI 1.069–1.553), and assisting patients with COVID-19 (OR: 1.275; 95% CI 1.081–1.506) were independently associated with new-onset or worsening of previous insomnia episodes.
Conclusions:
We observed a huge burden of insomnia episodes and other sleep disturbances in health care professionals during the COVID-19 pandemic.
Citation:
Drager LF, Pachito DV, Moreno CRC, et al. Insomnia episodes, new-onset pharmacological treatments, and other sleep disturbances during the COVID-19 pandemic: a nationwide cross-sectional study in Brazilian health care professionals. J Clin Sleep Med. 2022;18(2):373–382.
Keywords: sleep, insomnia, health care professionals, anxiety, burnout, COVID-19, pandemic
BRIEF SUMMARY
Current Knowledge/Study Rationale: The stressful routine and risk of infection by COVID-19 may predispose health care professionals to sleep disturbances. This nationwide cross-sectional study comprising several occupational categories explored the burden of several sleep disturbances, new-onset pharmacological treatments for insomnia, and their related independent predictors.
Study Impact: We observed a worrisome scenario of new-onset/worsening preexisting insomnia episodes (which contributed to new pharmacological treatments for insomnia), impaired sleep quality, duration, nightmare, and snoring. Age, females, weight change, anxiety, burnout, income reduction, and assisting patients with COVID-19 were independently associated with the primary outcome. Considering the impact of sleep disorders on work performance/health care decisions, this study underscores the need for dedicated sleep and mental health programs for health care professionals.
INTRODUCTION
The adverse impact of the coronavirus disease 2019 (COVID-19) pandemic on sleep quality and anxiety levels in the global population reinforces the need for urgent attention to sleep disorders and mental health globally.1–4 The lack of effective pharmacological treatments, low availability of vaccines, the rapid dissemination of the virus, social distancing, decreased physical activity, the negative economic impact, and even the alarming fake news are contributing to this scenario.5–7
Health care professionals are particularly exposed to higher levels of stress and work demand.8 In addition, health care professionals have a higher risk of contamination when compared to the general population.9 Several reports10–18 have discussed the potential impact of COVID-19 pandemic on sleep in health care professionals. Limitations of previous studies include one or more factors including small sample sizes, analysis of specific health care occupations, the lack of comparisons with the period before COVID-19, and lack of assessment of several variables associated with insomnia.
In this large survey we aimed to explore the potential impact of the COVID-19 pandemic on sleep, anxiety levels, and burnout symptoms in a large sample of health care professionals from Brazil. Our country has continental dimensions and is experiencing a high overall incidence of COVID-19, but with significant differences among each region. We assessed independent predictors of new-onset or worsening of preexisting insomnia (primary outcome) as well as new-onset pharmacological treatments for insomnia, sleep quality, sleep duration, nightmares, and snoring (secondary outcomes) among these professionals. We made the hypothesis that insomnia among health care professionals will worsen during the pandemic as compared to the prepandemic period. As a consequence, health care professionals will report increased use of hypnotics during the pandemic as compared to the prepandemic period.
METHODS
This study is a joint initiative effort from the Brazilian Association of Sleep (ABS) and the Brazilian Association of Sleep Medicine (ABMS). This cross-sectional study was reviewed and approved by the Hospital das Clínicas Institutional Review Board (CAAE: 31750920.9.0000.0068) and was exempted from a consent form. No participant identifier was required or recorded, preserving the anonymity of responders. The study report aimed at covering all items of the Strobe checklist for cross-sectional studies).19
Sample population
Health care professionals (including physicians, nurses, nurse technicians, physical therapists, psychologists, nutritionists, occupational therapists, pharmacists, physical educators, dentists, biologists, and administrative officers) were invited to participate through the WhatsApp digital platform. Invitations were also sent by email using organizational mailing lists of health care professional associations. The survey was distributed and managed using REDCap electronic data capture tools hosted at the Hospital das Clínicas.20 The survey remained active from May 28, 2020 to June 28, 2020. Participants had to be active health care professionals. Subjects were excluded if their answers to the main outcome questions (insomnia) were left blank. No further exclusion criteria were applied.
The survey was developed by sleep medicine specialists and included information on occupation, age, sex, and workplace environment (intensive care unit, ward, operating room, pharmacy, administrative area, outpatient clinic, etc.) and the postal code of the home address (supplemental material). Participants were also asked to describe current and previous weekly work hours, whether they were involved in the care of COVID-19 patients, and whether they had been diagnosed with COVID-19. Three domains addressing anxiety levels, sleep characteristics, and burnout symptoms were included. The anxiety domain included generalized anxiety disorder 2-item21 to assess the presence of anxiety symptoms and a question asking the participant to compare his (her) current anxiety symptoms to those before the COVID-19 pandemic. The domain related to sleep characteristics included questions regarding current and previous sleep quality, sleep duration, sleepiness assessed by the Stanford Sleepiness Scale,22 insomnia symptoms, nightmares, and snoring. Participants were asked if they had insomnia and whether insomnia worsened during the pandemic. In addition, participants were asked the frequency of insomnia episodes and if they used to take or started taking medications for insomnia. New-onset insomnia was considered when difficult in initiating or maintaining sleep that occurred at least twice a week during the pandemic. Worsening of preexisting insomnia was considered when the participant had a previous insomnia history but it was impaired by at least two additional episodes per week during the pandemic. The burnout domain included questions addressing current and previous burnout symptoms.23 The burnout questionnaire was scored from 1 (no burnout symptoms) to 5 (severe burnout symptoms). New-onset burnout was considered when participants scored 1 or 2 before the pandemic and 3–5 during the pandemic. In addition, participants were asked to declare changes in weight and family income compared to the prepandemic period.
Data on the regional incidence of death due to COVID-19 (per 10,000 inhabitants) was collected from the Brazilian Ministry of Health website in the same period of this survey.24 Since the goal of the present study was to obtain the highest number of responses possible, the sample size calculation was not conducted. A post hoc power calculation based on our main findings is presented in the Results section.
Statistical analysis
All analyses were conducted using the software R 3.6.0. Graphs were built with the ggplot2 package. For comparisons of categorical variables, the χ2 test was performed. Normally distributed continuous variables were compared by using unpaired Student’s t test or one-way analysis of variance and presented as the means and standard deviation. Kruskal-Wallis tests were used to compare skewed variables and are presented as medians and interquartile ranges. We performed a logistic regression analysis to assess the influence of independent variables on the combination of new onset of insomnia and worsening of preexisting insomnia episodes. Logistic regression was also used to determine the independent predictors of new-onset pharmacological treatments, sleep quality, and sleep duration. Adjusted estimates (odds ratio) and their precision (95% confidence interval) are presented. The following variables were entered in the model: age, sex, health category, workplace, previous diagnosis of COVID-19, previous or current care of patients with COVID-19, regional death incidence of COVID-19 according to the epidemiological week in the individual’s municipality, change in working hours, change in weight (no change, decrease, or increase), the proportion of change in family income (no change, increase, decrease > 0 but < 30%, and decrease > 30%), prevalent anxiety, and change in burnout severity. For the secondary outcomes, insomnia was included in the regression model. For all statistical tests, a significance level of 5% was adopted. Incomplete responses were excluded preventing the need for imputation of missing values.
RESULTS
After the completion of study recruitment we obtained 4,939 responses, of which 4,384 were completed for the outcomes of interest (88.8% of the total). Methods applied for disseminating the link to the survey precluded the calculation of response rates.
The distribution of responders across the Brazilian territory is shown on a heat map (Figure S1 in the supplemental material), representing all geographic regions. Around half of the responders were physicians, followed by physiotherapists and nurses (Figure S2 in the supplemental material).
The characteristics of the studied population are shown in Table 1. Overall, our sample comprised middle-aged women. On average, participants reported a reduction of weekly working hours during the pandemic compared to the prepandemic period. Figure S3 in the supplemental material reports work hours changes (per week) by health professional category. A significant proportion of participants reported they were predominantly working from home. More than half of the interviewed professionals were assisting or had previously assisted patients with COVID-19. Almost 10% had a previous COVID-19 infection. The frequencies of professional groups by occupation that were assisting patients with COVID-19 or had a previous diagnosis of COVID-19 are reported in Figure S4 and Figure S5 in the supplemental material, respectively. We observed a substantial proportion of health care professionals with prevalent anxiety (Figure S6 in the supplemental material), burnout (Figure S7 in the supplemental material), reporting worsening sleep quality and duration during the pandemic (Table 1), or reporting family income reduction (Figure S8 in the supplemental material).
Table 1.
Characteristics of the studied population of health care professionals in Brazil.
| Variable | Values |
|---|---|
| Age, mean ± SD, y | 44 ± 12 |
| Females, n (%) | 3333 (76.0%) |
| Weekly work hours (before), mean ± SD | 41.4 ± 15.2 |
| Weekly work hours (current), mean ± SD | 34.6 ± 18.5 |
| Home office, n (%) | 1,742/4,379 (39.8%) |
| Recent or current care of patients with COVID-19, n (%) | 2,442 (55.7%) |
| Previous diagnosis of COVID-19, n (%) | 403 (9.2%) |
| Prevalent anxiety, n (%) | 1,939 (44.2%) |
| New-onset burnout, n (%) | 882 (20.1%) |
| Stanford Sleepiness Scale | 2.5 ± 1.4 |
| Current sleep quality (in comparison to prepandemic) | |
| Worse | 2,691/4,381 (61.4%) |
| Similar | 1,492/4,381 (34.1%) |
| Better | 198/4,381 (4.5%) |
| Current sleep duration (in comparison to prepandemic) | |
| Decreased | 2,135/4,377 (48.8%) |
| Similar | 1,552/4,377 (35.5%) |
| Increased | 690/4,377 (15.8%) |
| Prepandemic subjective sleep duration, h | 6.8 ± 1.2 (n = 4,325) |
| Current subjective sleep duration, h | 6.4 ± 1.6 (n = 4,328) |
COVID-19 = coronavirus disease 2019, SD = standard deviation.
Main outcome: insomnia episodes
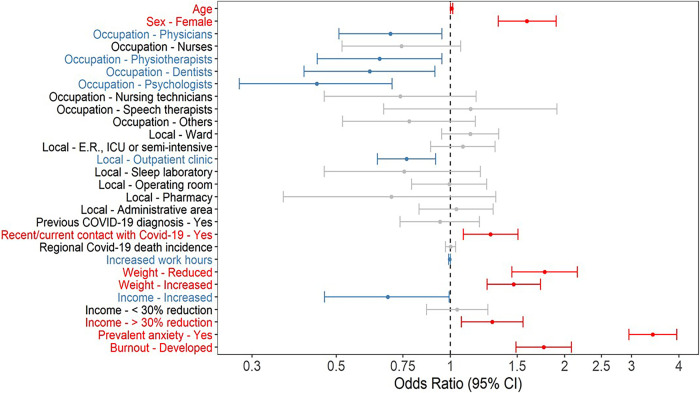
Our survey showed that 1,444 out of 4,384 (32.9%) health care professionals presented new-onset insomnia during the pandemic or worsening of preexisting insomnia episodes. Considering the proportion of the main outcome, this sample size allowed 95% significance level with a margin of error of just 1.46%. The characteristics of health care professionals with no insomnia, no change in previous insomnia, and new insomnia/insomnia impairment during the pandemic of COVID-19 are shown in Table 2. Figure S9 in the supplemental material details the rate of new-onset or worsening insomnia episodes according to the occupation category. In the logistic regression analysis, age (each 1-year increase), female sex, significant weight change (decrease or increase), prevalent anxiety, new-onset burnout, family income reduction > 30%, and previous/current care of patients with COVID-19 were independently associated with new onset of insomnia or worsening of preexisting insomnia episodes (Figure 1). In contrast, physicians, psychologists, physiotherapists, and dentists (administrative officers as the reference group), increased family income, working in the outpatient clinic, and (unexpectedly) increased work hours were associated with a lower chance of new-onset or worsening of preexisting insomnia episodes (Figure 1). Detailed data on insomnia episodes outcomes are presented in Table S1 in the supplemental material.
Table 2.
Characteristics of health care professionals who do not have insomnia episodes, no change in previous insomnia, and new-onset/worsening insomnia episodes during the pandemic of COVID-19.
| Insomnia | P | |||
|---|---|---|---|---|
| No (n = 1,683) |
Yes, but No Significant Change (n = 1,244) |
New Onset/Worsening of Insomnia Episodes (n = 1,444) | ||
| Age, mean ± SD, y | 43.6 ± 11.9 (n = 1,683) |
45.9 ± 11.9 (n = 1,224) |
43.1 ± 11.1 (n = 1,444) |
.001 |
| Female, n (%) | 1,209/1,683 (71.8%) | 898/1,224 (73.4%) | 1,195/1,444 (82.8%) | <.001 |
| Health professional categories, n (%) | <.001 | |||
| Administrative officers | 98/1,683 (5.8%) | 84/1,224 (6.9%) | 131/1,444 (9.1%) | |
| Dentists | 114/1,683 (6.8%) | 116/1,224 (9.5%) | 91/1,444 (6.3%) | |
| Nurses | 101/1,683 (6.0%) | 94/1,224 (7.7%) | 139/1,444 (9.6%) | |
| Nursing assistants | 41/1,683 (2.4%) | 46/1,224 (3.8%) | 62/1,444 (4.3%) | |
| Physicians | 965/1,683 (57.3%) | 650/1,224 (53.1%) | 740/1,444 (51.2%) | |
| Physiotherapists | 155/1,683 (9.2%) | 70/1,224 (5.7%) | 122/1,444 (8.4%) | |
| Speech therapists | 36/1,683 (2.1%) | 24/1,224 (2.0%) | 43/1,444 (3.0%) | |
| Psychologists | 95/1,683 (5.6%) | 74/1,224 (6.0%) | 40/1,444 (2.8%) | |
| Others | 78/1,683 (4.6%) | 66/1,224 (5.4%) | 76/1,444 (5.3%) | |
| Worksite, n (%) | ||||
| Administrative area | 246/1,683 (14.6%) | 190/1,224 (15.5%) | 249/1,444 (17.2%) | .128 |
| Emergency room/ intensive care unit/semi-intensive care unit | 331/1,683 (19.7%) | 222/1,224 (18.1%) | 339/1,444 (23.5%) | .002 |
| Outpatient clinic | 1079/1,683 (64.1%) | 754/1,224 (61.6%) | 766/1,444 (53.0%) | <.001 |
| Pharmacy | 17/1,683 (1.0%) | 21/1,224 (1.7%) | 19/1,444 (1.3%) | .255 |
| Sleep laboratory | 41/1,683 (2.4%) | 35/1,224 (2.9%) | 29/1,444 (2.0%) | .360 |
| Operating room | 226/1,683 (13.4%) | 147/1,224 (12.0%) | 158/1,444 (10.9%) | .103 |
| Ward | 361/1,683 (21.4%) | 233/1,224 (19.0%) | 375/1,444 (26.0%) | <.001 |
| Previous diagnosis of COVID-19, n (%) | 148/1,683 (8.8%) | 109/1,224 (8.9%) | 142/1,444 (9.8%) | .562 |
| Recent/current care of patients with COVID-19, n (%) | 907/1,683 (53.9%) | 629/1,224 (51.4%) | 884/1,444 (61.2%) | <.001 |
| Death rate (per 10,000 inhabitants in the epidemiological week, mean ± SD | 2.9 ± 2.4 (n = 1,683) |
2.8 ± 2.3 (n = 1,224) |
3.0 ± 2.3 (n = 1,444) |
.011 |
| Change in weekly working hours, mean ± SD | −7.5 ± 15.4 (n = 1,683) |
−6.5 ± 14.5 (n = 1,224) |
−6.4 ± 15.2 (n = 1,444) |
.001 |
| Body weight | <.001 | |||
| Decreased | 296/1,683 (17.6%) | 232/1,224 (19.0%) | 334/1,444 (23.1%) | |
| Increased | 735/1,683 (43.7%) | 562/1,224 (45.9%) | 763/1,444 (52.8%) | |
| No change | 652/1,683 (38.7%) | 430/1,224 (35.1%) | 347/1,444 (24.0%) | |
| Income, n (%) | <.001 | |||
| Decreased < 30% | 554/1,683 (32.9%) | 353/1,224 (28.8%) | 391/1,444 (27.1%) | |
| Decreased > 30% | 573/1,683 (34.0%) | 433/1,224 (35.4%) | 564/1,444 (39.1%) | |
| Increased, | 88/1,683 (5.2%) | 44/1,224 (3.6%) | 51/1,444 (3.5%) | |
| No change | 468/1,683 (27.8%) | 394/1,224 (32.2%) | 438/1,444 (30.3%) | |
| Prevalent anxiety, n (%) | 470/1,683 (27.9%) | 477/1,224 (39.0%) | 965/1,444 (66.8%) | <.001 |
| New-onset burnout, n (%) | 237/1,683 (14.1%) | 183/1,224 (15.0%) | 457/1,444 (31.6%) | <.001 |
COVID-19 = coronavirus disease 2019, SD = standard deviation.
Figure 1. Independent predictors of new-onset and worsening insomnia frequency.
Data are presented as OR and 95% CI. Variables reported in blue and red mean significant lower and higher association with new-onset and worsening insomnia frequency, respectively. CI = confidence interval, COVID-19 = coronavirus disease 2019, E.R. = emergency room, ICU = intensive care unit, OR = odds ratio.
Secondary outcomes: new-onset pharmacological treatments for insomnia, sleep quality, sleep duration, nightmares, and snoring
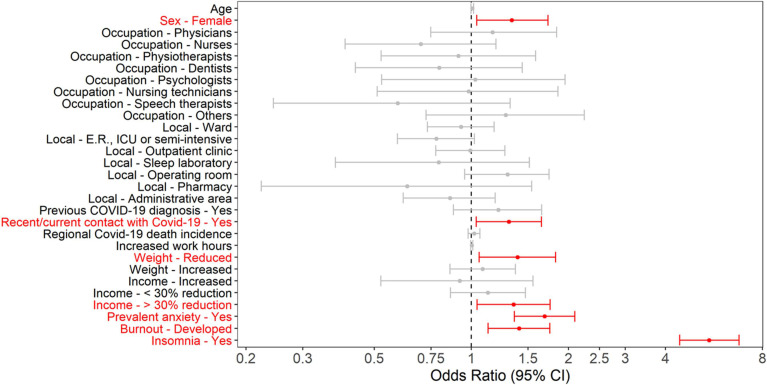
Previous hypnotic use was reported by 9% and new use was reported by 13% of the participants (n = 572) during the pandemic. Nursing technicians and physicians were the most prevalent health care professionals reporting the need for new pharmacological treatment for insomnia (Figure S10 in the supplemental material). The independent predictors of new-onset pharmacological treatments for insomnia included females, previous/current care of patients with COVID-19, reduced weight, prevalent anxiety, new-onset burnout, family income reduction > 30%, and (expected to be the most important factor) insomnia episodes (Figure 2). Detailed data on pharmacological treatment outcome are presented in Table S2 in the supplemental material.
Figure 2. Independent predictors of new-onset pharmacological treatments for insomnia.
Data are presented as ORs and 95% CIs. Variables reported in red mean significant higher association with new-onset pharmacological treatments for insomnia. CI = confidence interval, COVID-19 = coronavirus disease 2019, E.R. = emergency room, ICU = intensive care unit, OR = odds ratio.
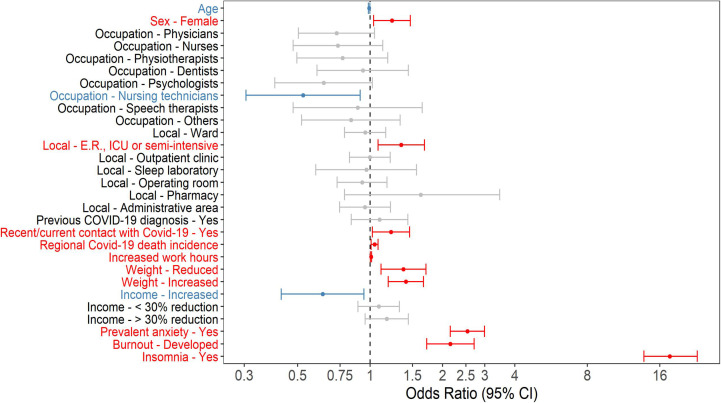
The majority of participants (61.4%) described that their sleep quality worsened during the pandemic. In the logistic regression analysis, females, working in emergency room/intensive care, recent/current care of patients with COVID-19, COVID-19 regional cumulative number of deaths per 10,000 inhabitants, increase in weekly work hours, change in weight (gain or loss), prevalent anxiety, new onset of burnout, and new-onset/worsening preexisting insomnia episodes were independent predictors of impaired sleep quality during the pandemic. In contrast, age, nurse technicians (administrative group as a reference), and increased family income were independently associated with sleep quality improvement (Figure 3). Detailed data on sleep quality outcomes are presented in Table S3 in the supplemental material.
Figure 3. Independent predictors of sleep quality impairment.
Data are presented as ORs and 95% CIs. Variables reported in blue and red mean significant lower and higher association with sleep quality impairment, respectively. CI = confidence interval, COVID-19 = coronavirus disease 2019, E.R. = emergency room, ICU = intensive care unit, OR = odds ratio.
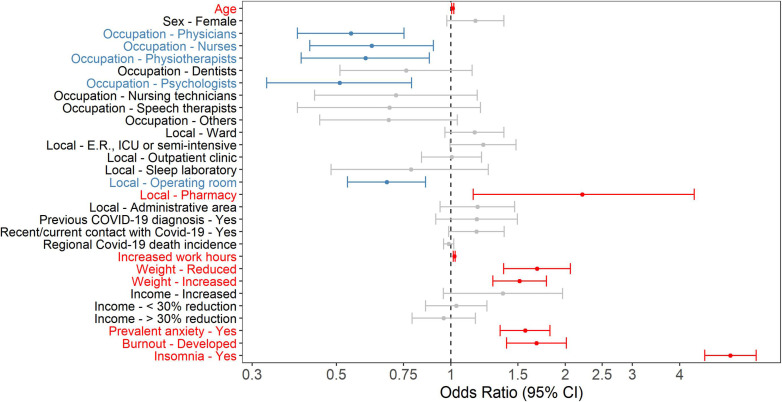
The reduction of at least 1 hour of sleep was reported by 43.5% of the participants. In the logistic regression analysis, age, working at pharmacy, increase in weekly work hours, change in weight (increase or decrease), prevalent anxiety, new-onset burnout, and new-onset/worsening of insomnia episodes were independently associated with an increased chance for reduction at least 1 hour of self-reported sleep duration. In contrast, specific occupational categories (physicians, nurses, physiotherapists, and psychologists) and working in the operating room were independently associated with less chance of having a reduction at least 1 hour in the self-reported sleep duration (Figure 4). Detailed data on sleep quantity outcomes are presented in Table S4 in the supplemental material.
Figure 4. Independent predictors of self-reported sleep duration reduction.
Data are presented as ORs and 95% CIs. Variables reported in blue and red mean significant lower and higher association with self-reported sleep duration reduction, respectively. CI = confidence interval, COVID-19 = coronavirus disease 2019, E.R. = emergency room, ICU = intensive care unit, OR = odds ratio.
Regarding nightmares, 1,001 participants (22.8%) reported worsening or new-onset nightmares. Compared to participants with no nightmares or those with previous nightmare but no change during the pandemic, new onset or worsening of preexisting nightmares episodes were younger, had a higher frequency of females, higher frequency of recent/current contact with patients with COVID-19, had more impact on the income, gained more weight, and had a frequency of anxiety, burnout, and insomnia. In the logistic regression analysis (Figure S11 in the supplemental material), females, recent/current contact with patients with COVID-19, income reduction, weight gain, anxiety, burnout, and insomnia were independently associated with new onset or worsening of preexisting nightmares episodes in health professionals.
New-onset or worsening snoring were reported by 390 participants (8.9%). Independent factors associated with the snoring outcome included being nursing technician, recent/current contact with patients with COVID-19, increased working hours, increased weight, significant reduction in income, anxiety, and insomnia (Figure S12 in the supplemental material).
DISCUSSION
To our knowledge, this is one of the largest investigations addressing sleep disturbances and their predictors among health care professionals during the COVID-19 pandemic. This nationwide cross-sectional study comprising several occupational categories and multiple related factors revealed the following results. Supporting our hypothesis, 32.9% of the health care professionals developed new-onset or worsening preexisting insomnia episodes, which contributed to the initiation of pharmacological treatment for insomnia in 13% of the responders. Sleep quality, duration, nightmare, and snoring were also severely impaired by the pandemic. Our multivariate analyses showed that age, female sex, significant weight change (decrease or increase), prevalent anxiety, new-onset burnout, family income reduction > 30%, and previous/current care of patients with COVID-19 were independently associated with new-onset or worsening preexisting insomnia episodes. A recent survey study of 7,208 Dutch health care workers showed that health care workers who are in direct contact with COVID-19 patients report more sleep problems and are more physically exhausted than those who are not in direct contact with COVID-19 patients.25 Contrary to our hypothesis, we did not find associations with regional COVID-19 death incidence regarding insomnia outcome. Also, increased work hours were associated with less chance of having new-onset insomnia or exacerbation of preexisting insomnia episodes, but the magnitude of the odds ratio and 95% confidence interval suggest that its impact may not have clinical relevance. Increased work hours, change in weight, prevalent anxiety, new-onset burnout, and new-onset/worsening preexisting insomnia episodes have a significant impact on sleep quality and quantity. Taken together, we observed a huge burden of insomnia and other sleep disturbances in Brazilian health care professionals during the pandemic.
Our main results revealed a worrisome scenario. Almost a third of health care professionals, particular nurse technicians and nurses, presented new onset or worsening of preexisting insomnia during the pandemic. A previous study reported a prevalence of insomnia of 34% among health care workers during the pandemic.11 In the present study, a high prevalence of insomnia episodes contributed to a significant increase of new pharmacological treatments for insomnia in a short period. Moreover, 44.2% of all surveyed participants and 66.8% of those with new-onset or worsening insomnia reported anxiety during the pandemic. Anxiety is a well-known risk factor for insomnia and has been described in up to 44.7% of health care workers during the COVID-19 pandemic.26,27 New-onset burnout was also an independent predictor of new-onset or worsening preexisting insomnia in our study. Burnout was reported by 20.1% of the participants and by 31.6% of those complaining of insomnia episodes. Consistently, a high prevalence of burnout during the pandemic (21.8%) has been previously reported among otolaryngologists and residents.28 Female sex was also an independent predictor of new-onset or worsening insomnia episodes in the present study. The majority of our survey participants were women (76%), which is in line with a recent report of the World Health Organization that estimated that women comprise 67% of the world health care workforce.29 Among all participants reporting new-onset or worsening insomnia episodes, 82.8% were women. Potential explanations for the increased burden of insomnia among women may be associated with multifactorial variables, including the common role of caretaker, work–family conflicts, and economic inequality.30 Taken together, new onset and worsening of insomnia episodes is frequent among health care workers during the COVID-19 pandemic. Preventing and treating anxiety and burnout may help mitigate insomnia burden and long-term adverse consequences, especially among women. In this scenario, our study underscores the need for active interventions such as cognitive behavior therapy for insomnia for the susceptible health care population who are presenting insomnia. Cognitive behavior therapy for insomnia is considered the gold-standard treatment for insomnia,31 even when associated with medical, neurological, and psychiatric comorbidities.32
Our secondary outcomes also revealed relevant findings. The new-onset pharmacological treatment for insomnia occurred in 13% of our study population. This result is impressive considering the short period of observation. The predictors related to this outcome are consistent with the primary one. The majority of participants in our survey reported worse sleep quality during the pandemic (61.4%). Recent/current care of patients with COVID-19, COVID-19 regional cumulative number of deaths per 10,000 inhabitants, increase in weekly work hours, change in weight (gain or loss), prevalent anxiety, new onset of burnout, and new-onset/worsening preexisting insomnia were independently associated with worsening sleep quality. Many reports described impaired sleep quality during the pandemic,33–35 but these studies were limited to one or more of the following reasons: (1) no comparisons with the prepandemic period, (2) small sample sizes, and (3) analysis limited to one specific health care professional category or to combined analysis. Regarding the reduction in self-reported sleep duration, to the best of our knowledge this is the first study addressing the potential impact of the pandemic on this sleep quantity outcome in a large sample of health care professionals. Sleep reduction of at least 1 hour was reported by 43.5% of participants. Younger age, working at hospital wards, increase in weekly work hours, change in weight (increase or decrease), prevalent anxiety, new-onset burnout, and new onset/worsening of insomnia were associated with increased odds of reduction at least 1 hour of sleep duration. While several characteristics have plausibility for expecting a reduction in self-reported sleep duration during the pandemic, the precise reason for the independent association of working in the hospital wards, instead of working in the emergency room or in intensive care units, is unclear.
The present investigation has limitations mainly related to the pragmatic approach for participant selection and participation to be addressed. First, the absence of probabilistic samples and the voluntary nature for participation may have introduced bias related to the severity of sleep disturbances, since individuals with more severe sleep disturbances may have felt more motivated to provide answers to the survey. However, we may argue that a significant proportion of participants did not report the main outcomes or initiate medical treatments for insomnia. The survey’s succinct nature (approximately 4 minutes to be completed) prevented low adherence in a scenario of busy work schedules but failed to provide detailed analysis of some sleep complaints. Second, following the same principle described above, we did not use a standard questionnaire to evaluate insomnia. Even the criterion of ≥ 2 episodes per week used to report insomnia is debatable and the reported insomnia prevalence might be overestimated. However, our results were consistent with those of Lai et al.11 Using the insomnia severity index, the authors reported a similar prevalence of insomnia (34%) in 1,257 health care professionals. Of note, the aforementioned study had a prevalence of women similar to ours (76.7 vs 76%), a well-established factor linked to insomnia. In addition, the relevance of the new-onset pharmacological treatments for insomnia and similar predictors provided supportive validation for our primary outcome. Third, a recall bias may have occurred in the questions asking to recall a specific symptom before the pandemic. Fourth, the burnout questionnaire used in this study was validated to assess prevalent burnout. We applied the questionnaire in a somewhat different perspective, asking about previous and current burnout symptoms. Although a recall bias may have occurred, our results show that the pandemic resulted in the development of burnout in a significant proportion of responders. Fifth, although it was clearly stated that the survey was directed to health care professionals, irrespectively of their occupation, it is not possible to refute the possibility of having obtained responses from different occupational groups. The large sample size and the consistency observed in the above-mentioned previous investigations may mitigate the importance of this limitation. Sixth, we did not assess the influence of other factors in the proposed outcomes including information regarding number of offspring of each participant. Finally, our study did not investigate possible differences between health care workers in public or private sectors. The high number of responses collected in such a short period represents one of the strengths of this study. Complete responses were obtained from all regions in Brazil, including responses from participants that work in health care in small, medium, and large municipalities.
In conclusion, this nationwide survey comprising over 4,000 health care professionals in Brazil showed a high prevalence of new-onset or worsening previous insomnia episodes that directly contributed to the initiation of pharmacological treatment for insomnia in a significant number of responders. The unique contribution of this survey was the ability to examine several predictors of emerging or exacerbation of sleep difficulties during the pandemic. Variables such as age, sex (females), significant family income reduction during the pandemic, weight change (decrease or increase), prevalent anxiety, burnout development, and previous or current care of patients with COVID-19 were independently associated with the combined insomnia endpoints. Considering that insomnia may impact not only quality of life but also work performance, future investigations addressing the impact of treating insomnia and its comorbidities in health care professionals will be necessary.36
DISCLOSURE STATEMENT
Funding support for the statistical analysis was provided by Associação Brasileira do Sono (ABS) and Associação Brasileira de Medicina do Sono (ABMS). The authors report no conflicts of interest.
ACKNOWLEDGMENTS
The authors thank all health care professionals that anonymously contributed to this survey and Tiago Mendonça, Stat, for his careful statistical analysis. Author contributions: L.F.D. and P.R.G. are the guarantors of the content of the manuscript. L.F.D., D.V.P., C.R.C.M., A.R.T., S.G.C., M.A., D.A.S., G.A.M., A.B., and P.R.G. contributed substantially to the study design, data analysis and interpretation, and the writing of the manuscript.
ABBREVIATIONS
- CI
confidence interval
- COVID-19
coronavirus disease 2019
- OR
odds ratio
REFERENCES
- 1. Guo J , Feng XL , Wang XH , van Ijzendoorn MH . Coping with COVID-19: exposure to COVID-19 and negative impact on livelihood predict elevated mental health problems in Chinese adults . Int J Environ Res Public Health. 2020. ; 17 ( 11 ): 3857 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brooks SK , Webster RK , Smith LE , et al . The psychological impact of quarantine and how to reduce it: rapid review of the evidence . Lancet. 2020. ; 395 ( 10227 ): 912 – 920 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zhao X , Lan M , Li H , Yang J . Perceived stress and sleep quality among the non-diseased general public in China during the 2019 coronavirus disease: a moderated mediation model . Sleep Med. 2020. ; 77 : 339 – 345 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Vindegaard N , Benros ME . COVID-19 pandemic and mental health consequences: systematic review of the current evidence . Brain Behav Immun. 2020. ; 89 : 531 – 542 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hartley S , Colas des Francs C , Aussert F , et al . [The effects of quarantine for SARS-CoV-2 on sleep: an online survey] . Encephale. 2020. ; 46 ( 3s ): S53 – S59 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cellini N , Canale N , Mioni G , Costa S . Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy . J Sleep Res. 2020. ; 29 ( 4 ): e13074 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wang S , Xie L , Xu Y , Yu S , Yao B , Xiang D . Sleep disturbances among medical workers during the outbreak of COVID-2019 . Occup Med (Lond). 2020. ; 70 ( 5 ): 364 – 369 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Liu Q , Luo D , Haase JE , et al . The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study . Lancet Glob Health. 2020. ; 8 ( 6 ): e790 – e798 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Suárez-García I , Martínez de Aramayona López MJ , Sáez Vicente A , Lobo Abascal P . SARS-CoV-2 infection among healthcare workers in a hospital in Madrid, Spain . J Hosp Infect. 2020. ; 106 ( 2 ): 357 – 363 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Badahdah AM , Khamis F , Al Mahyijari N . Sleep quality among health care workers during the COVID-19 pandemic . J Clin Sleep Med. 2020. ; 16 ( 9 ): 1635 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lai J , Ma S , Wang Y , et al . Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019 . JAMA Netw Open. 2020. ; 3 ( 3 ): e203976 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Morgantini LA , Naha U , Wang H , et al . Factors contributing to healthcare professional burnout during the COVID-19 pandemic: a rapid turnaround global survey. medRxiv. Preprint posted online May 22, 2020. . https://www.medrxiv.org/content/10.1101/2020.05.17.20101915v1 . [DOI] [PMC free article] [PubMed]
- 13. Barello S , Palamenghi L , Graffigna G . Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic . Psychiatry Res. 2020. ; 290 : 113129 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wu W , Zhang Y , Wang P , et al . Psychological stress of medical staffs during outbreak of COVID-19 and adjustment strategy . J Med Virol. 2020. ; 92 ( 10 ): 1962 – 1970 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wu Y , Wang J , Luo C , et al . A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China . J Pain Symptom Manage. 2020. ; 60 ( 1 ): e60 – e65 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. El-Hage W , Hingray C , Lemogne C , et al . [Health professionals facing the coronavirus disease 2019 (COVID-19) pandemic: what are the mental health risks?] Encephale. 2020. ; 46 ( 3s ): S73 – S80 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Qi J , Xu J , Li BZ , et al . The evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19 . Sleep Med. 2020. ; 72 : 1 – 4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pappa S , Ntella V , Giannakas T , Giannakoulis VG , Papoutsi E , Katsaounou P . Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis . Brain Behav Immun. 2020. ; 88 : 901 – 907 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. STROBE . STROBE checklists. https://www.strobe-statement.org/index.php?id=available-checklists . Accessed March 22, 2021.
- 20. Harris PA , Taylor R , Thielke R , Payne J , Gonzalez N , Conde JG . Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support . J Biomed Inform. 2009. ; 42 ( 2 ): 377 – 381 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Plummer F , Manea L , Trepel D , McMillan D . Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis . Gen Hosp Psychiatry. 2016. ; 39 : 24 – 31 . [DOI] [PubMed] [Google Scholar]
- 22. MacLean AW , Fekken GC , Saskin P , Knowles JB . Psychometric evaluation of the Stanford Sleepiness Scale . J Sleep Res. 1992. ; 1 ( 1 ): 35 – 39 . [DOI] [PubMed] [Google Scholar]
- 23. Dolan ED , Mohr D , Lempa M , et al . Using a single item to measure burnout in primary care staff: a psychometric evaluation . J Gen Intern Med. 2015. ; 30 ( 5 ): 582 – 587 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ministry of Health . Panel of coronavirus disease cases 2019 (COVID-19) in Brazil by the Ministry of Health. https://covid.saude.gov.br . Accessed June 15, 2020.
- 25. van Roekel H , van der Fels IMJ , Bakker AB , Tummers LG . Healthcare workers who work with COVID-19 patients are more physically exhausted and have more sleep problems . Front Psychol. 2021. ; 11 : 625626 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Huang Y , Zhao N . Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey . Psychiatry Res. 2020. ; 288 : 112954 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Zhang C , Yang L , Liu S , et al . Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak . Front Psychiatry. 2020. ; 11 : 306 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Civantos AM , Byrnes Y , Chang C , et al . Mental health among otolaryngology resident and attending physicians during the COVID-19 pandemic: national study . Head Neck. 2020. ; 42 ( 7 ): 1597 – 1609 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Boniol M , McIsaac M , Xu L , Wuliji T , Diallo K , Campbell J . Gender equity in the health workforce: analysis of 104 countries. Health Workforce Working Paper No. 1; 2019.
- 30. López-Atanes M , Recio-Barbero M , Sáenz-Herrero M . Are women still “the other”? Gendered mental health interventions for health care workers in Spain during COVID-19 . Psychol Trauma. 2020. ; 12 ( S1 ): S243 – S244 . [DOI] [PubMed] [Google Scholar]
- 31. Trauer JM , Qian MY , Doyle JS , Rajaratnam SM , Cunnington D . Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis . Ann Intern Med. 2015. ; 163 ( 3 ): 191 – 204 . [DOI] [PubMed] [Google Scholar]
- 32. Ashworth DK , Sletten TL , Junge M , et al . A randomized controlled trial of cognitive behavioral therapy for insomnia: an effective treatment for comorbid insomnia and depression . J Couns Psychol. 2015. ; 62 ( 2 ): 115 – 123 . [DOI] [PubMed] [Google Scholar]
- 33. Tu ZH , He JW , Zhou N . Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: a cross-sectional study . Medicine (Baltimore). 2020. ; 99 ( 26 ): e20769 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wu K , Wei X . Analysis of psychological and sleep status and exercise rehabilitation of front-line clinical staff in the fight against COVID-19 in China . Med Sci Monit Basic Res. 2020. ; 26 : e924085 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zhou Y , Yang Y , Shi T , et al . Prevalence and demographic correlates of poor sleep quality among frontline health professionals in Liaoning Province, China during the COVID-19 outbreak . Front Psychiatry. 2020. ; 11 : 520 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Weiner L , Berna F , Nourry N , Severac F , Vidailhet P , Mengin AC . Efficacy of an online cognitive behavioral therapy program developed for healthcare workers during the COVID-19 pandemic: the REduction of STress (REST) study protocol for a randomized controlled trial . Trials. 2020. ; 21 ( 1 ): 870 . [DOI] [PMC free article] [PubMed] [Google Scholar]