Abstract
Background
The purpose of this study was to evaluate the predictive values of lipid level, inflammatory biomarkers, and echocardiographic parameters in late NVAF (nonvalvular atrial fibrillation) recurrence after RFA (radiofrequency ablation).
Material/Methods
This retrospective single-center study enrolled 263 patients with paroxysmal or persistent NVAF who underwent initial RFA from Jan 2017 to Jan 2019. The patients were divided into a Recurrent group (n=70) and a Nonrecurrent group (n=193). Univariate and multivariate logistic regression analyses were used for evaluating the predictive factors of late NVAF recurrence. Receiver operating characteristic (ROC) curves were constructed to assess the predictive performance and the optimum cut-off level of variables.
Results
Late NVAF recurrence occurred in 70 patients (26.6%) after initial RFA within 12-month follow-up. Patients in the Recurrent group had significant higher NLR (neutrophil-to-lymphocyte ratio), hs-CRP (high-sensitivity C-reactive protein), LVEDD (left ventricular end-diastolic dimension), LVESD (left ventricular end-systolic dimension), and LAD (left atrial diameter) than those in the Nonrecurrent group (P<0.05). In multivariate analysis, increased NLR (HR=1.438, 95% CI: 1.036–1.995, P<0.05), hs-CRP (HR=1.137, 95% CI: 1.029–1.257, P<0.05) and LAD (HR=1.089, 95% CI: 1.036–1.146, P<0.05) were independent predictors of NVAF recurrence. The area under the curve (AUC) of NLR and hs-CRP was 0.603 (95% CI 0.525–0.681) and 0.584 (95% CI 0.501–0.666), respectively. The combination of NLR, hs-CRP, and LAD revealed an AUC of 0.684 (95% CI 0.611–0.757), with cut-off values of 2.33, 2.025 ng/L, and 44.5 mm, respectively.
Conclusions
The combination of preoperative NLR, hs-CRP, and LAD can predict late NVAF recurrence.
Keywords: Atrial Fibrillation, C-Reactive Protein (164-173), Recurrence
Background
Atrial fibrillation (AF) is an increasingly prevalent arrhythmia which affects nearly 33 million people worldwide, and its prevalence increases with age [1–3]. Due to the heterogeneity of AF, mechanisms of AF vary among individuals and change with time [4]. Previous studies showed early AF recurrence (within 3 months) and late recurrence (within 1 year) in 20%–50% of patients after ablation [5]. Preventing NVAF recurrences is a challenging aspect of controlling NVAF incidence, and it is crucial to predict late NVAF recurrences in these patients.
Various myocardial injury markers are released to circulation in AF patients on account of the ablation. Nonetheless, elevated cardiac biomarkers showed no association with AF recurrence [6]. Lipid levels are partially modulated by inflammatory pathways and can change cell membrane fluidity, which facilitates the arrhythmias [7]. Recently, inflammatory biomarkers such as NLR have received increased attention due to the crucial role of inflammation in the progression of cardiovascular disease [8]. These epidemiological data highlight the importance of predictive factors for late NVAF recurrence. However, the prognostic performance of preoperative laboratory measurements, echocardiographic parameters (eg, LVEDD, LVESD, LAD, and LVEF), lymphocyte-to-monocyte ratio (LMR), and platelet-to-lymphocyte ratio (PLR) in predicting late NVAF recurrence has been unclear.
In this study, we aimed to evaluate the association between lipid levels, inflammatory biomarkers combined echocardiographic parameters, and late NVAF recurrence in persistent AF and paroxysmal AF patients undergoing initial RFA, providing a simple, comprehensive, and non-invasive approach to assess the risk of NVAF recurrence.
Material and Methods
Study Participants
Medical data of 278 NVAF patients admitted to the First Affiliated Hospital of Soochow University were retrospectively analyzed from Jan 2017 to Jan 2019. A total of 263 consecutive patients who underwent initial RFA were enrolled. The diagnosis and pattern of NVAF was according to the 2016 European Society of Cardiology (ESC) guidelines [9]. Persistent AF was defined as AF lasting ≥7 days and paroxysmal AF was defined as AF lasting <7 days. We excluded 10 cases with structural heart disease (2 cases), hyperthyroidism (3 cases), chronic obstructive pulmonary disease (2 cases), severe hepatic (2 cases), and renal dysfunction (1 case). Five patients were excluded because of the incomplete clinical records on parameters. This study was approved by the Ethics Committee of the First Affiliated Hospital of Soochow University. The requirement of written consent was waived because of the study’s retrospective nature. Independent variables, including major characteristics (sex, age, course of disease, body mass index [BMI]), comorbidities (hypertension, diabetes mellitus, cerebral infarction), CHA2DS2-VASc score, and medication were evaluated. Echocardiographic parameters, including LVEDD, LVESD, LAD, and LVEF, were assessed by transthoracic echocardiography. Preoperative laboratory test parameters, including blood and urinary biomarkers, were collected, and NLR, PLR, and LMR were calculated as previously described [10].
Procedure Details
Pre-procedural evaluation and testing, including trans-esophageal echo, transthoracic echocardiography, and enhanced CT scan, was performed. Patients were treated with warfarin or new oral anticoagulants (NOACs) to maintain INR between 2.0 and 3.0 for at least 3 weeks. All patients had local anesthesia prior to ablation. Under the positioning of CARTO®3 (Biosense Webster, Diamond Bar, CA, USA) and EnSite NavX™ (St. Jude Medical, Inc., St. Paul, MN, USA) three-dimensional mapping system, the radiofrequency ablation electrode was sent into the sheath tube to construct a left atrium three-dimensional model. The ablation was performed at energy of 30–35 W, flow rate of 17 ml/min, and temperature 42°C. Wide circumferential left and right pulmonary vein isolation was performed along the ablation line. Other linear ablations, such as left roof, top and bottom, mitral isthmus, and tricuspid isthmus, were conducted after pulmonary vein isolation. If atrial fibrillation still existed after ablation, two-way wave synchronous defibrillation apparatus was used to achieve electrocardioversion.
Post-Procedure Treatment and Follow-Up
All patients were given oral anticoagulation for at least 3 months after the procedure. After discharge from the hospital, follow-up visits at 1 month, 3 months, 6 months, 9 months, and 12 months were conducted. Routine 12-lead 24-h dynamic electrocardiography was performed at each visit. Late NVAF recurrence was identified by 24-h Holter monitoring (at 3, 6, 9, and 12 months) after 3 months following the RFA procedure. Recurrent NVAF was characterized as arrhythmia ≥30 s duration.
Statistical Analysis
All continuous data are presented as mean±standard deviation or median. All data were analyzed using SPSS statistical software (SPSS, Inc., version 17, Chicago, IL, USA) and the MedCalc analysis program (MedCalc Software, version 15, Ostend, Belgium). Categorical data are presented as counts and percentages. Continuous variables were compared using the t test or Mann-Whitney U test, as appropriate. Categorical data were compared by chi-squared test. Multivariate analysis was calculated on all variables with a P value <0.10 in univariate analysis. Univariate and multivariate logistic regression analyses were used for evaluating the predictive factors of late NVAF recurrence. Receiver operating characteristic (ROC) curve analysis was performed to determine the optimum cut-off level, sensitivity, and specificity of variables. The cut-off value was evaluated by Youden index. The comparison of AUC was performed using the Z-test. DeLong’s test was used to analyze the predictive value of different indexes. A P<0.05 was considered statistically significant.
Results
Baseline Characteristics
We included 263 patients after a follow-up of 12 months, with median age 62 years (age range 53–69 years, 41.83% females, 74.14% had paroxysmal AF). Baseline characteristics of study population are summarized in Table 1. Overall, the Nonrecurrent group and Recurrent group were well balanced, except for the AF type.
Table 1.
Baseline characteristics of study population.
| Variable | Nonrecurrent group (n=193) | Recurrent group (n=70) | P value |
|---|---|---|---|
| Female [n (%)] | 77 (40) | 33 (47) | 0.292 |
| Age (year) | 62 (53, 69) | 62 (57, 67) | 0.694 |
| Course of disease (months) | 24.0 (3.0, 54.5) | 24.0 (6.0, 48.0) | 0.513 |
| BMI (kg/m2) | 25.31±3.30 | 25.22±2.75 | 0.839 |
| Hypertension | 123 (64) | 43 (61) | 0.732 |
| Diabetes mellitus | 24 (12) | 10 (14) | 0.693 |
| Cerebral infarction | 11 (6) | 5 (7) | 0.888 |
| Smoking | 33 (17) | 9 (13) | 0.407 |
| Alcohol | 22 (11) | 8 (11) | 0.995 |
| CHA2DS2-VASc score | 0.469 | ||
| 0 | 30 (16) | 12 (17) | |
| 1 | 47 (24) | 18 (26) | |
| 2 | 57 (30) | 14 (20) | |
| ≥3 | 59 (30) | 26 (37) | |
| AF type | 0.002* | ||
| Paroxysmal AF | 153 (79) | 42 (60) | |
| Persistent AF | 40 (21) | 28 (40) | |
| Previous medication | |||
| ACEI/ARB | 62 (32) | 19 (27) | 0.439 |
| β-blockers | 92 (48) | 33 (47) | 0.940 |
| CCB | 67 (35) | 20 (29) | 0.349 |
| Amiodarone | 33 (17) | 9 (13) | 0.407 |
| Propafenone | 17 (9) | 6 (9) | 0.952 0.809 |
| Preoperative anticoagulants | |||
| Low molecular heparin | 126 (66) | 48 (69) | |
| Warfarin | 33 (17) | 12 (17) | |
| NOAC | 34 (17) | 10 (14) |
ACEI – angiotensin-converting enzyme inhibitor; ARBs – AT1 blockers; BMI – body mass index; CCB – calcium channel blockers.
P<0.01.
Laboratory and Echocardiographic Parameters
Table 2 presents a comparison of laboratory and echocardiographic parameters of patients. When compared to the Nonrecurrent group, patients in the Recurrent group had significantly lower TC, lower LDL-C, lower lymphocyte counts, lower LVEF, higher NLR, higher hs-CRP, higher PT, higher INR, higher LVEDD, higher LVESD, and higher LAD. No significant difference was found between other parameters.
Table 2.
Laboratory and echocardiographic parameters of study population.
| Variable | Nonrecurrent group (n=193) | Recurrent group (n=70) | P value |
|---|---|---|---|
| Glucose(mmol/L) | 5.11 (4.61, 5.61) | 5.06 (4.65, 5.79) | 0.862 |
| Scr(umol/L) | 72.67±17.12 | 73.52±17.60 | 0.724 |
| UA (umol/L) | 348.79±84.50 | 354.29±92.49 | 0.649 |
| TC (mmol/L) | 4.34 (3.86, 5.10) | 4.21 (3.55, 4.67) | 0.027* |
| LDL-C(mmol/L) | 2.48 (2.06, 3.14) | 2.31 (1.87, 2.71) | 0.046* |
| HDL-C(mmol/L) | 1.15 (0.99, 1.36) | 1.10 (0.94, 1.27) | 0.096 |
| TG (mmol/L) | 1.47 (1.06, 2.04) | 1.46 (1.01, 2.16) | 0.673 |
| Lymphocyte count, ×109/L | 1.93 (1.54, 2.38) | 1.85 (1.23, 2.21) | 0.047* |
| Monocyte count, ×109/L | 0.46 (0.38, 0.53) | 0.44 (0.33, 0.58) | 0.619 |
| Neutrophil count, ×109/L | 3.13 (2.50, 3.90) | 3.16 (2.54, 4.05) | 0.373 |
| Platelet count, ×109/L | 188.28±50.19 | 191.09±65.59 | 0.713 |
| NLR | 1.61 (1.27, 2.12) | 1.85 (1.42, 2.49) | 0.011* |
| PLR | 98.52 (76.19, 118.17) | 101.41 (80.76, 135.57) | 0.112 |
| LMR | 4.21 (3.44, 5.32) | 4.10 (2.98, 5.19) | 0.172 |
| hs-CRP, mg/L | 1.06 (0.65, 1.86) | 1.16 (0.76, 3.48) | 0.038* |
| Albumin, g/L | 42.90±3.52 | 42.44±3.66 | 0.354 |
| PT | 11.70 (11.00, 12.70) | 12.40 (11.68, 14.10) | 0.000*** |
| APTT | 29.35 (25.83, 34.28) | 30.25 (26.83, 35.45) | 0.479 |
| INR | 1.02 (0.95, 1.11) | 1.08 (1.02, 1.23) | 0.001** |
| LVEDD, mm | 49 (46, 52) | 51 (47, 53) | 0.023* |
| LVESD, mm | 32 (30, 35) | 34 (31, 36) | 0.027* |
| LAD, mm | 41.58±5.88 | 44.79±5.71 | 0.000*** |
| LVEF, % | 0.63 (0.58, 0.67) | 0.61 (0.57, 0.64) | 0.036* |
APTT – activated partial thromboplastin time; HDL-C – high-density lipoprotein cholesterol; INR – international prothrombin time standardized ratio; LDL-C – low-density lipoprotein cholesterin; LMR – lymphocyte-to-monocyte ratio; LAD – left atrial diameter; LVEDD – left ventricular end-diastolic dimension; LVESD – left ventricular end-systolic dimension; LVEF – left ventricular ejection fraction; PLR – platelet-to-lymphocyte ratio; PT – prothrombin time; Scr – serum creatinine; TC – total cholesterol; TG – triglyceride; UA – uric acid;
P<0.05,
P<0.01,
P<0.001.
Logistic Regression Analysis
Univariate analysis showed that persistent AF (HR: 2.550, 95% CI 1.411–4.607), TC (HR: 0.699, 95% CI 0.517–0.945), LDL-C (HR: 0.692, 95% CI 0.482–0.995), NLR (HR: 1.573, 95% CI 1.147–2.158), hs-CRP (HR: 1.164, 95% CI 1.061–1.277), LVEDD (HR: 1.077, 95% CI 1.017–1.142), LVESD (HR: 1.062, 95% CI 1.008–1.120), LAD (HR: 1.101, 95% CI 1.147–2.158) and LVEF (HR: 0.010, 95% CI 0.000–0.649) were factors significantly associated with NVAF recurrence (Table 3). On multivariable analysis, higher NLR (HR: 1.438, 95% CI 1.036–1.995), hs-CRP (HR: 1.137, 95% CI 1.029–1.257) and LAD (HR: 1.089, 95% CI 1.036–1.146) were independent predictors of NVAF recurrence (Table 4).
Table 3.
Univariate logistic regression for clinical factors.
| Variable | B | SE | Wald χ2 | HR | 95% CI | P value |
|---|---|---|---|---|---|---|
| Persistent AF | 0.936 | 0.302 | 9.623 | 2.550 | 1.411–4.607 | 0.002** |
| TC | −0.358 | 0.154 | 5.420 | 0.699 | 0.517–0.945 | 0.020* |
| LDL-C | −0.368 | 0.185 | 3.946 | 0.692 | 0.482–0.995 | 0.047* |
| NLR | 0.453 | 0.161 | 7.901 | 1.573 | 1.147–2.158 | 0.005** |
| hs-CRP | 0.152 | 0.047 | 10.267 | 1.164 | 1.061–1.277 | 0.001** |
| LVEDD | 0.075 | 0.030 | 6.347 | 1.077 | 1.017–1.142 | 0.012* |
| LVESD | 0.060 | 0.027 | 5.037 | 1.062 | 1.008–1.120 | 0.025* |
| LAD | 0.096 | 0.026 | 13.971 | 1.101 | 1.147–2.158 | 0.000*** |
| LVEF | −4.604 | 2.129 | 4.678 | 0.010 | 0.000–0.649 | 0.031* |
B – regression coefficient; HR – hazard ratio; SE – standard error; 95% CI – 95% confidence interval.
P<0.05,
P<0.01,
P<0.001.
Table 4.
Multivariate analysis of predictors in correlation with late NVAF recurrence.
| Variable | B | SE | Wald χ2 | HR | 95% CI | P value |
|---|---|---|---|---|---|---|
| NLR | 0.363 | 0.167 | 4.721 | 1.438 | 1.036–1.995 | 0.030* |
| hs-CRP | 0.129 | 0.051 | 6.344 | 1.137 | 1.029–1.257 | 0.012* |
| LAD | 0.086 | 0.026 | 11.166 | 1.089 | 1.036–1.146 | 0.001** |
P<0.05,
P<0.01,
P<0.001.
ROC Curve Analysis of NLR, hs-CRP, and LAD
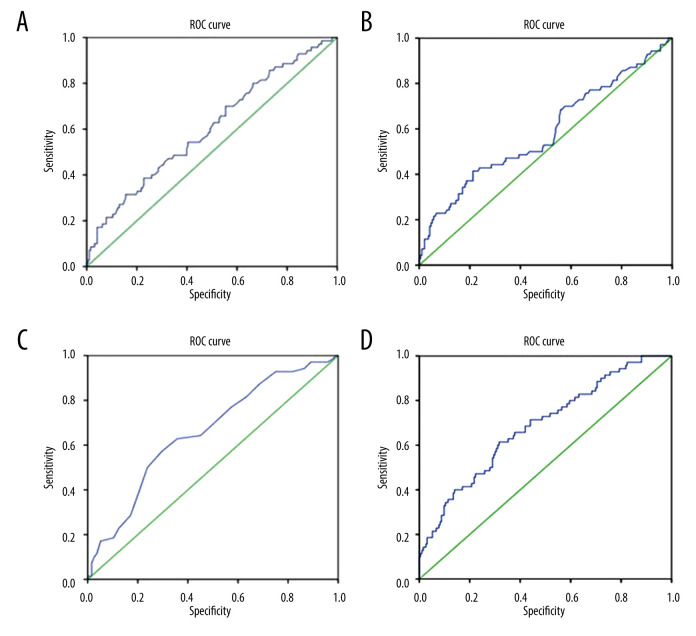
Figure 1 depicts the AUC for NLR, hs-CRP, and LAD was 0.603 (95% CI 0.525–0.681), 0.584 (95% CI 0.501–0.666), and 0.658 (95% CI 0.585–0.732), respectively (Figure 1A–1C). The cut-off value of NLR, hs-CRP, and LA was 2.33 (sensitivity 31.4%, specificity 84.5%), 2.025 ng/L (sensitivity 41.4%, specificity 78.8%), and 44.5 mm (sensitivity 57.1%, specificity 70.5%). The AUC of combination of NLR and hs-CRP was 0.632 (95% CI 0.551–0.712) with sensitivity of 51.4% and specificity of 73.6%. The AUC of combination of NLR, hs-CRP, and LAD was 0.684 (95% CI 0.611–0.757) with sensitivity of 61.4% and specificity of 68.4% (Figure 1D). DeLong’s test indicated that the combination of the NLR, hs-CRP, and LAD is more effective than NLR (P=0.0427) and hs-CRP alone (P=0.0122) but not LAD alone (P=0.2911) in predicting NVAF recurrence.
Figure 1.
Determination of the predictive value of NLR, hs-CRP, and LAD in NVAF. recurrence using SPSS software (SPSS Inc., version 17, Chicago, IL, USA). (A) The AUC=0.603 for NLR, P=0.011; (B) AUC=0.584 for hs-CRP, P=0.038; (C) AUC=0.658 for LAD, P=0.000; (D) AUC=0.684 for combination of NLR, hs-CRP and LAD combined, P=0.000.
Discussion
The current study demonstrated that NLR, hs-CRP, and LAD were associated with late NVAF recurrence. In addition, the combination of NLR, hs-CRP, and LAD has the potential to serve as a simple, comprehensive, and non-invasive approach to assess the risk of NVAF recurrence.
Relapse is common in patients with paroxysmal and persistent atrial fibrillation, but has improved with advances in ablation therapy. Our 78.46% success rate in paroxysmal AF and 58.82% in persistent AF at a follow-up time of 12 months is similar to that of previous reports [11,12]. In this single-center retrospective study, we found persistent AF patients had higher recurrence rates than in patients with paroxysmal AF. Interestingly, we observed early recurrence is not an effective predictor of late recurrence (data not shown). In contrast to the present results, previous studies found that early recurrence was an independent predictor of late relapse in patients who underwent cryoballoon ablation [13]. Lower serum TC is an indicator of poor nutrition status. LDL-C is a known risk factor for ischemic stroke in patients with AF [14]. In this study, patients in the Recurrence group had significantly lower lipid levels, such as serum preoperative TC and LDL-C. However, we found that lower serum TC and LDL-C levels did not predict NVAF recurrence. These findings suggest decreased serum TC and LDL-C can reduce the success rate of RFA in both sexes.
The use of biomarkers to predict relapse has been reported in previous studies, including myocardial injury biomarker, brain-type natriuretic peptides, CRP, oxidative stress markers, and galectin-3 [15,16]. Evidence revealed that accumulated immune cells triggered inflammatory cascades in arrhythmogenesis and structural remodeling during the progression of AF. Moreover, thermal necrosis produced by RFA leads to local or adjacent inflammatory reactions. Many studies have found a strong association of inflammatory marker with risk of AF [17,18], but there is no consensus about the predictive role of hs-CRP and NLR in AF recurrence. Yano et al showed NLR was only useful for predicting late AF recurrence in paroxysmal AF [19]. In the present study, we found that higher hs-CRP and NLR predicted NVAF recurrence 12 months after RFA, regardless of existence of persistent AF and paroxysmal AF.
Enlarged LVEDD and LVESD reflects the deterioration of left ventricular systolic function, which can occur during AF [20]. It is known that LA size, including LA diameter and volume, is a valuable predictor of new-onset AF [21,22]. However, studies about the predictive role of LVEDD, LVESD, LAD, and LVEF in AF recurrence are contradictory [23–25]. In our work, we assessed echocardiographic characteristics and found persistent AF and paroxysmal AF patients in the Recurrent group had enlarged LVEDD, LVESD, and LAD and impaired LVEF, which was congruent with other observations. In line with previous studies, we found LAD was a significant predictor of late AF recurrence.
In addition, we evaluated NLR >2.025 ng/L, hs-CRP>2.33, and LAD >44.5 mm as suitable cut-off values. Zhang and Yuan revealed LAD ≥44.17 mm predicted the risk of left atrial/left atrial appendage thrombosis [26]. Kornej et al found LAD >43 mm could predict AF recurrence [27]. Our results from ROC curve analysis showed that the combination of NLR, hs-CRP, and LAD was superior to NLR and hs-CRP alone in the prediction of AF relapse. Our data emphasize the importance of monitoring pre-ablation NLR, hs-CRP, and LAD. NLR and hs-CRP levels are affected in many diseases, such as malignant tumor, autoimmune diseases, and atherosclerosis. Interestingly, we found that the combination of inflammatory biomarkers and structural factors can enhance the prediction of NVAF recurrence.
The present study is the first to show the following results: i) AF recurrence developed frequently in patients with persistent AF; ii) patients who experienced AF recurrence had lower lipid level, higher levels of NLR, hs-CRP, LVEDD, LVESD, and LAD, and lower LVEF; iii) pre-procedural NLR, hs-CRP, and LAD can be used as independent predictors; iiii) the combination of NLR, hs-CRP, and LAD was the most precise method for prediction. The major limitation of this study is its retrospective single-center design and short follow-up.
Conclusions
In conclusion, the combination of preoperative NLR, hs-CRP, and LAD can predict late NVAF recurrence and may be helpful to risk-stratify patients undergoing initial RFA.
Footnotes
Conflict of interest: None declared
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors, who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Financial support: Funded by the Jiangsu Provincial Key Medical Center (YXZXA2016002) and the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD)
References
- 1.Bhatt HV, Fischer GW. Atrial fibrillation: Pathophysiology and therapeutic options. J Cardiothorac Vasc Anesth. 2015;29(5):1333–40. doi: 10.1053/j.jvca.2015.05.058. [DOI] [PubMed] [Google Scholar]
- 2.Rahman F, Kwan GF, Benjamin EJ. Global epidemiology of atrial fibrillation. Nat Rev Cardiol. 2014;11(11):639–54. doi: 10.1038/nrcardio.2014.118. [DOI] [PubMed] [Google Scholar]
- 3.Zhou Z, Hu D. An epidemiological study on the prevalence of atrial fibrillation in the Chinese population of mainland China. J Epidemiol. 2008;18(5):209–16. doi: 10.2188/jea.JE2008021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wijesurendra RS, Casadei B. Mechanisms of atrial fibrillation. Heart. 2019;105(24):1860–67. doi: 10.1136/heartjnl-2018-314267. [DOI] [PubMed] [Google Scholar]
- 5.Margulescu AD, Mont L. Persistent atrial fibrillation vs paroxysmal atrial fibrillation: Differences in management. Expert Rev Cardiovasc Ther. 2017;15(8):601–18. doi: 10.1080/14779072.2017.1355237. [DOI] [PubMed] [Google Scholar]
- 6.Kızılırmak F, Gokdeniz T, Gunes HM, et al. Myocardial injury biomarkers after radiofrequency catheter and cryoballoon ablation for atrial fibrillation and their impact on recurrence. Kardiol Pol. 2017;75(2):126–34. doi: 10.5603/KP.a2016.0089. [DOI] [PubMed] [Google Scholar]
- 7.Harrison SL, Lane DA, Banach M, et al. Lipid levels, atrial fibrillation and the impact of age: Results from the LIPIDOGRAM2015 study. Atherosclerosis. 2020;312:16–22. doi: 10.1016/j.atherosclerosis.2020.08.026. [DOI] [PubMed] [Google Scholar]
- 8.Farah R, Samra N. Mean platelets volume and neutrophil to lymphocyte ratio as predictors of stroke. J Clin Lab Anal. 2018;32(1):e22189. doi: 10.1002/jcla.22189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893–962. doi: 10.1093/eurheartj/ehw210. [DOI] [PubMed] [Google Scholar]
- 10.Trinh H, Dzul SP, Hyder J, et al. Prognostic value of changes in neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR) and lymphocyte-to-monocyte ratio (LMR) for patients with cervical cancer undergoing definitive chemoradiotherapy (dCRT) Clin Chim Acta. 2020;510:711–16. doi: 10.1016/j.cca.2020.09.008. [DOI] [PubMed] [Google Scholar]
- 11.Morillo CA, Verma A, Connolly SJ, et al. Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of paroxysmal atrial fibrillation (RAAFT-2): A randomized trial [published correction appears in JAMA. 2014;311(22):2337] JAMA. 2014;311(7):692–700. doi: 10.1001/jama.2014.467. [DOI] [PubMed] [Google Scholar]
- 12.Cao H, Xue Y, Zhou Q, et al. Late outcome of surgical radiofrequency ablation for persistent valvular atrial fibrillation in China: A single-center study. J Cardiothorac Surg. 2017;12(1):63. doi: 10.1186/s13019-017-0627-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Quan D, Huang H, Kong B, et al. Predictors of late atrial fibrillation recurrence after cryoballoon-based pulmonary vein isolation: A meta-analysis. Kardiol Pol. 2017;75(4):376–85. doi: 10.5603/KP.a2016.0186. [DOI] [PubMed] [Google Scholar]
- 14.Omelchenko A, Hornik-Lurie T, Gabay H, et al. LDL Cholesterol and ischemic stroke in patients with nonvalvular atrial fibrillation. Am J Med. 2021;134(4):507–13. doi: 10.1016/j.amjmed.2020.08.035. [DOI] [PubMed] [Google Scholar]
- 15.Tsiachris D, Giannopoulos G, Deftereos S, et al. Biomarkers determining prognosis of atrial fibrillation ablation. Curr Med Chem. 2019;26(5):925–37. doi: 10.2174/0929867325666180320122930. [DOI] [PubMed] [Google Scholar]
- 16.Hu YF, Chen YJ, Lin YJ, et al. Inflammation and the pathogenesis of atrial fibrillation. Nat Rev Cardiol. 2015;12(4):230–43. doi: 10.1038/nrcardio.2015.2. [DOI] [PubMed] [Google Scholar]
- 17.Georgakopoulos C, Vlachopoulos C, Lazaros G, et al. Biomarkers of atrial fibrillation in metabolic syndrome. Curr Med Chem. 2019;26(5):898–908. doi: 10.2174/0929867324666171012105528. [DOI] [PubMed] [Google Scholar]
- 18.Berkovitch A, Younis A, Grossman Y, et al. Relation of neutrophil to lymphocyte ratio to risk of incident atrial fibrillation. Am J Cardiol. 2019;123(3):396–401. doi: 10.1016/j.amjcard.2018.10.036. [DOI] [PubMed] [Google Scholar]
- 19.Yano M, Egami Y, Ukita K, et al. Atrial fibrillation type modulates the clinical predictive value of neutrophil-to-lymphocyte ratio for atrial fibrillation recurrence after catheter ablation. Int J Cardiol Heart Vasc. 2020;31:100664. doi: 10.1016/j.ijcha.2020.100664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mele D, Luisi GA, Ferrari R. Evaluation of left ventricular systolic function during atrial fibrillation: Is it reliable? Int J Cardiol. 2018;263:63–64. doi: 10.1016/j.ijcard.2018.03.118. [DOI] [PubMed] [Google Scholar]
- 21.Soeki T, Matsuura T, Tobiume T, et al. Clinical, electrocardiographic, and echocardiographic parameter combination predicts the onset of atrial fibrillation. Circ J. 2018;82(9):2253–58. doi: 10.1253/circj.CJ-17-0758. [DOI] [PubMed] [Google Scholar]
- 22.Debonnaire P, Joyce E, Hiemstra Y, et al. Left atrial size and function in hypertrophic cardiomyopathy patients and risk of new-onset atrial fibrillation. Circ Arrhythm Electrophysiol. 2017;10(2):e004052. doi: 10.1161/CIRCEP.116.004052. [DOI] [PubMed] [Google Scholar]
- 23.Njoku A, Kannabhiran M, Arora R, et al. Left atrial volume predicts atrial fibrillation recurrence after radiofrequency ablation: A meta-analysis. Europace. 2018;20(1):33–42. doi: 10.1093/europace/eux013. [DOI] [PubMed] [Google Scholar]
- 24.Kranert M, Shchetynska-Marinova T, Liebe V, et al. Recurrence of atrial fibrillation in dependence of left atrial volume index. In Vivo. 2020;34(2):889–96. doi: 10.21873/invivo.11854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mulukutla S, Althouse AD, Jain SK, et al. Increased left atrial size is associated with higher atrial fibrillation recurrence in patients treated with antiarrhythmic medications. Clin Cardiol. 2018;41(6):825–29. doi: 10.1002/clc.22964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang Y, Yuan YQ. Value of left atrial diameter with CHA2DS2-VASc score in predicting left atrial/left atrial appendage thrombosis in non-valvular atrial fibrillation. Arq Bras Cardiol. 2021;116(2):325–31. doi: 10.36660/abc.20190492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kornej J, Hindricks G, Shoemaker MB, et al. The APPLE score: a novel and simple score for the prediction of rhythm outcomes after catheter ablation of atrial fibrillation. Clin Res Cardiol. 2015;104(10):871–76. doi: 10.1007/s00392-015-0856-x. [DOI] [PMC free article] [PubMed] [Google Scholar]