Abstract
Objective:
To evaluate the maxillary alveolar buccal bone levels after expansion with banded and bonded expanders, using cone-beam computed tomography (CBCT).
Materials and Methods:
The population sample consisted of 22 patients who required expansion during their comprehensive treatment; 10 patients (five males and five females) with a mean age of 13.5 years (CVMS 3) had bonded hygienic expanders, and 12 (six males and six females) with a mean age of 12.6 years (CVMS 3) had banded hyrax expanders. CBCT was taken both before (T1) and 6 months after last activation (T2). Measurements were made for buccal bone thickness (BT), buccal marginal bone level (MBL), and bone thickness level (BTL) at the right first molar (MRt), left first molar (MLft), right first premolar (PMRt), and left first premolar (PMLft). A mixed-design analysis of variance assessed differences between and within the groups. Post hoc t-tests were completed on significant analysis of variance results to determine where differences occurred.
Results:
Analysis of variance revealed no significant differences between or within the two groups. BT significantly decreased horizontally following rapid maxillary expansion. The amount of bone lost was −0.59 mm MRt, −0.72 mm PMRt, −0.50 mm MLft, and −0.57 mm PMLft (P < .003).
Conclusions:
There was no significant difference between or within the two groups. Buccal bone loss in the vertical dimension (MBL) only showed significance in the banded group for MRt (0.63 mm) and PMLFt (0.37 mm) as evidenced by the paired t-test (P < .05).
Keywords: Expansion, Buccal bone changes, Bonded expanders, Banded expanders, CBCT measurements
INTRODUCTION
Maxillary palatal expansion is a common orthodontic procedure used to correct posterior crossbites, increase maxillary width, or enlarge arch perimeter. It was first described by Angell in 1860 and then later in early dental and orthodontic literature, from Black in 1893 to Hawley in 1912.1 Rapid maxillary expansion (RME) is accomplished by opening the skeletal sutures of the maxilla rather than moving the teeth out of the bone.1–4 Not only is the maxillary palatal suture opened, but the nasal, maxillary-zygomatic, and zygomatico-temporal sutures are affected during RME, with the nasal suture having the most cellular activity.5 Furthermore, RME is an efficient method for correcting arch length discrepancies caused by maxillary constriction.
The majority of the research conducted on RME stability and side effects is limited to the analysis of dental casts and two-dimensional radiographs (lateral and anterior-posterior cephalograms).6–11 The use of 3-dimensional imaging for orthodontic records yields insight into the effects and stability of RME.12–14 Recent research has begun to assess the skeletal effects of the maxilla after RME with the use of cone-beam technology.15–17 Additional studies evaluated the buccal bone changes of the maxillary posterior teeth and assessed the periodontal effects of different types of expanders.18,19 The purpose of this study was to evaluate the maxillary alveolar buccal bone levels after expansion with banded and bonded expanders, using cone-beam computed tomography (CBCT).
MATERIALS AND METHODS
This prospective study evaluated 22 patients treated with palatal expanders for the correction of maxillary palatal constriction. The Power analysis indicated that a sample size of 12 patients was needed to detect a difference of 1 mm or less in response to an alpha of .003 and a power of 80%. Approval of this study was received from the University of Detroit Mercy Institutional Review Board.
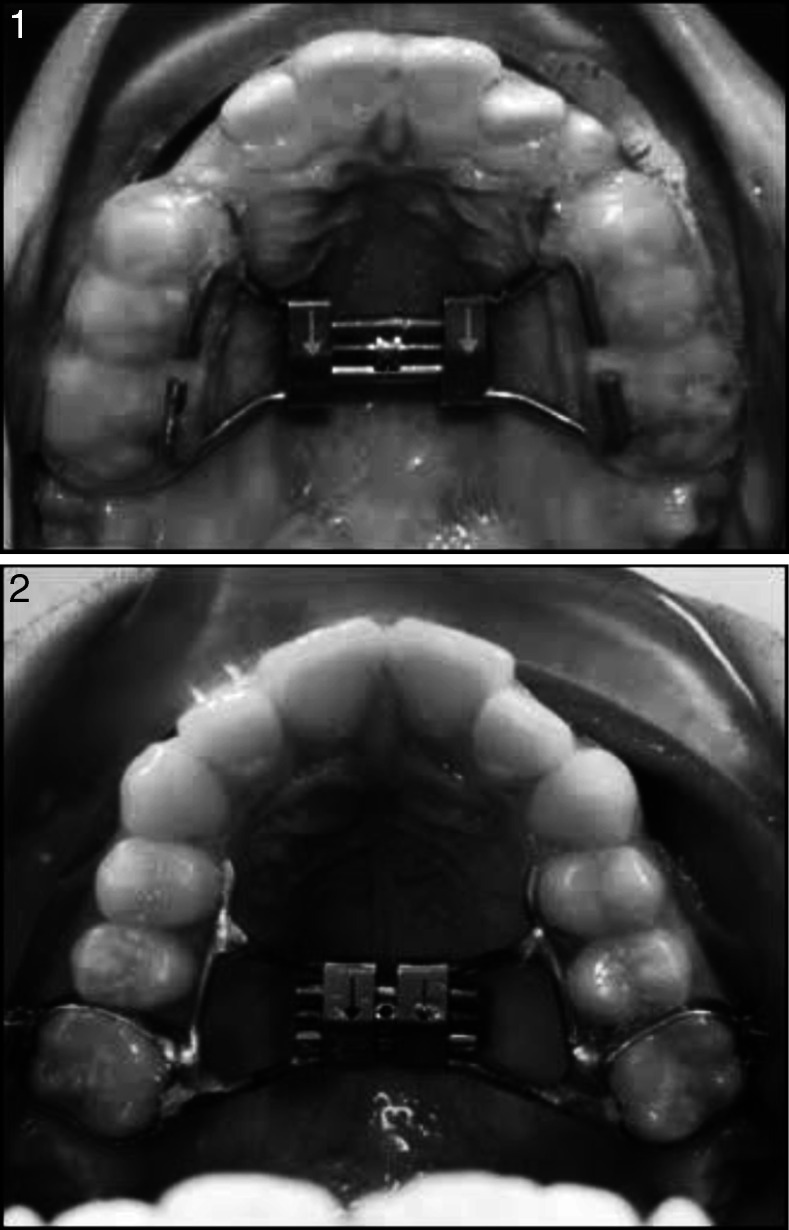
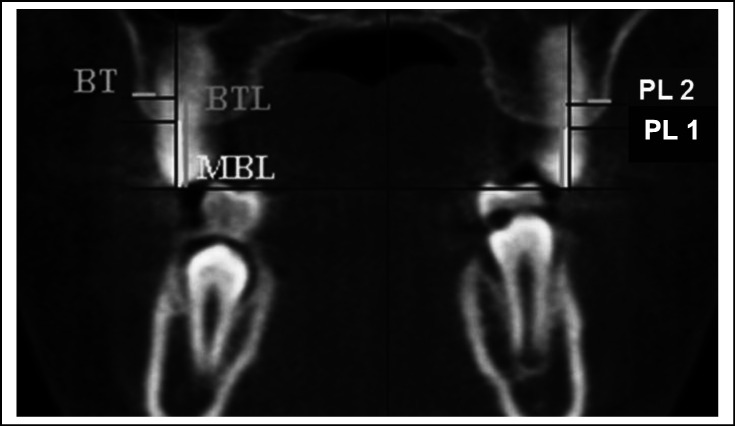
Ten patients (five males and five females) with a mean age of 13.5 ± 2.1 years had bonded hygienic expanders, and 12 patients (six males and six females) with a mean age of 12.5 ± 1.6 years had banded hyrax expanders (Figures 1 and 2). The mean cervical vertebra maturation in both groups was stage 3.
Figure 1. .
Bonded Expander.
Figure 2. Banded Expander.
The expanders were activated one turn a day for 4–6 weeks, with total expansion ranging from 6 to 10 mm. Patients with a dolichocephalic growth pattern received bonded expanders, while patients with a mesocephalic or brachycephalic growth pattern received banded expanders. CBCT was taken both before expansion (T1) and 6 months after the last activation of the expander, which coincided with appliance removal (T2). Measurements were made for buccal bone thickness (BT), buccal marginal bone level (MBL), and bone thickness level (BTL) at the right and left first molars (MRt, MLft) and the right and left first premolars (PMRt, PMLft). The second premolar was not included due to consistent findings of less bone loss in comparison to the adjacent teeth.16,18 All CBCT images were acquired with the I-CAT imaging scanner (Imaging Sciences International, Hatfield, Penn). The radiologic parameters used were 120 kVp, 18.54 mAs, 8.9-second scan time, and 0.3-mm voxel size. Each patient's image data were stored as DICOM (digital imaging and communications in medicine) data files and were assessed using Dolphin3D (version 11.5; Dolphin Imaging and Management Solutions, Chatsworth, Calif).
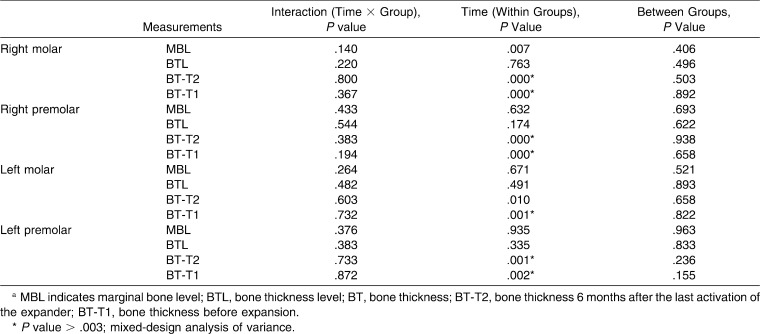
The measurement techniques for BT, MBL, and BTL were similar to those described by Rungcharassaeng et al.18 MBL and BT were measured as follows: from an axial cut of the T1 images at the root levels of the first premolars and molars, an open polygon cut was made buccal-lingual so it bisected the roots bilaterally. On the coronal image derived from the open-polygon cut, reference lines were constructed from the buccal cusp tips to the buccal root tips bilaterally. Only the mesio-buccal roots of the first molars (M) were evaluated due to their greater prominence over the disto-buccal root. A perpendicular line (PL1) to the reference line was made at the most coronal point where the bone meets tooth, and MBL was measured from the cusp tip to PL1. A second perpendicular line (PL2) was made at the level of buccal bone deflection. BTL was defined as the distance from the cusp tip to the PL2 on the reference line. On PL2, the BT was measured from the root surface to the most buccal bone surface (Figure 3). The procedures for T2 measurements were repeated; however, the BT was additionally measured at the BTL determined at T1 to maintain consistency of measurement height.
Figure 3. .
Molar coronal measurements derived from open polygon cut. BT indicates bone thickness; BTL, bone thickness level; MBL, marginal bone level; PL 1, perpendicular line 1; PL 2: perpendicular line 2.
Statistical Analysis
A mixed-model analysis of variance determined differences of BT, MBL, and BTL, with time (T1 vs. T2) as a repeated (or within subjects) effect and expander group as an independent effect. The significance level for each analysis of variance was set at .003 in order to keep the experiment-wide α level at .05. For those analysis of variance results that achieved significance, post hoc t-tests identified specific differences. Since the omnibus analysis of variance tests were adjusted for experiment-wide α, post-hoc tests were conducted with a P value of .05. Intra-rater reliability was assessed by test-retest reliability; measurements for 10 patients selected at random were repeated 1 month after initial readings were taken. Intra-rater reliability was high, ranging from 0.87 to 0.99 for most measures, the only exceptions being BT PMLft (r = .76) and MBL for the right molar (r = .81).
RESULTS
Comparison of Starting Sample
No statistically significant differences were found in either the banded or bonded groups at T1 for the 16 measurements studied.
Comparison of Expansion Effects
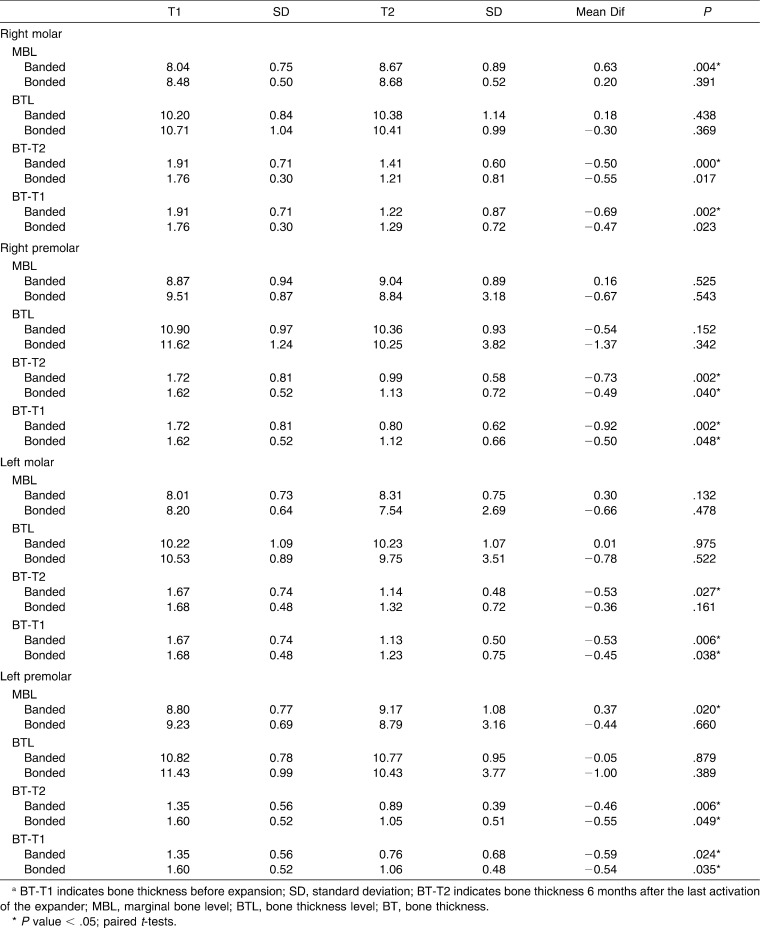
Mixed design analyses of variance indicated no significant interactions within the groups or between the groups. However, both groups changed similarly, and significantly, over time (Table 1).
Table 1. .
Overall Changes Within and Between the Banded and Bonded Hyrax Groups over Timea
Table 2. .
Changes Between the Banded and Bonded Hyrax Groups over Timea
Change in Buccal Bone
Buccal bone loss in the vertical dimension, as depicted by the MBL, only showed significance in the banded group for MRt (0.63 mm) and PMLft (0.37 mm) according to the paired t-test (P < .05). However, a tendency toward more vertical bone loss was observed in the banded group. BTL did not change significantly within and between groups over time for any of the teeth measured.
Statistically significant loss of horizontal buccal bone occurred at right and left first molars and premolars when measured after expansion at BTL-T1. Between T1 and T2, BT of MRt went from a mean value of 1.84 mm to 1.25 mm, for a horizontal buccal bone loss of 0.59 mm (F1,21 = 23.40, P = .000); BT of PMRt went from a mean value of 1.67 mm to 0.95 mm, for a horizontal buccal bone loss of 0.72 mm (F1,21 = 20.82, P = .000); BT of MLft went from a mean value of 1.67 mm to 1.18 mm, for a horizontal buccal bone loss of 0.50 mm (F1,21 = 16.77, P = .001); BT of PMLft went from a mean value of 1.46 mm to 0.90 mm, for a horizontal buccal bone loss of 0.57 mm (F1,21 = 16.77, P = .001) (Table 2).
DISCUSSION
Horizontal buccal bone (BT) was lost in all the teeth analyzed in both expansion groups. Over 0.50 mm of BT loss occurred with both types of expanders. These findings were similar to those of Garib et al.16 and Rungcharassaeng et al.18 Garib et al.,16 using Hass and four banded expander, found BT loss of 0.6 mm at the first premolars and 0.7 mm at the first molars, while Rungcharassaeng et al.18 found 1.14 mm at the first premolar and −1.24 at the first molar. Garib et al.16,19 also showed a decrease in MBL. However, the present study showed a significant vertical bone decrease only in the banded group on the MRt and PMLft. A decrease in vertical MBL is indicative of bone dehiscence.
Buccal tooth movement and bone dehiscence have been linked in animal investigations, where buccal tooth movement with mild forces increased the distance between the cementoenamel junction and the alveolar crest.20–24 Vanardsdall,7 Watson,25 and Greenbaum and Zarchrisson26 made clinical observations of attachment loss and gingival recession on the buccal surface of maxillary posterior teeth following expansion. Nonetheless, due to the lack of better diagnostic instrumentation, they could only suggest that RME could cause bone dehiscence.
The inconsistencies between our findings and those of previous studies highlight the difficulty in determining dehiscence of the buccal plate covering maxillary posterior teeth. The MBL at T2 may be similar to the T1 level, suggesting no loss of bone in the vertical dimension; however, fenestrations could be present at a more apical level. Garib et al.16 analyzed the maximum and minimum changes in MBL and determined that individual variations could be extensive, ranging from 0 to 10.5 mm. They further concluded that patients with initially thin bone plates had larger reductions of alveolar crest levels after expansion. Using the same sample as in the present study, Pangrazio-Kulbersh et al.17 determined that molar tipping was more significant in the banded group; this could possibly explain the vertical decrease of buccal bone in some teeth.
Periodontal stability of patients following expansion is a major concern for clinicians. Therefore, determining clinical significance of buccal bone loss is imperative. Our patients showed no signs of gingival recessions after expansion and at the 6 month retention period. It would be interesting to evaluate this sample long term to determine the effect of BT and vertical marginal bone reduction on the gingival levels.
Research by Steiner et al.21, Thilander et al.22, and Wennstrom et al.23 revealed that loss of connective tissue attachment and migration of junctional epithelium did not follow the buccal alveolar crest unless inflammation was present. Greenbaum and Zarchrisson26 studied the long term periodontal effects in younger patients receiving rapid (tissue-borne) or slow (quad-helix) expansion. At 3 years posttreatment, they compared the two expansion groups to a control group and found, on average, good periodontal conditions in all groups. Individual variations within the group were evident; most patients with attachment loss at the first molar were in the RME group.
Vanardsdall7 assessed the periodontal stability of young patients receiving orthodontic treatment with and without RME. After 8–10 years, gingival recession was present in 20% of the expansion patients and only in 6% of the nonexpansion patients. Recession has many contributing and predisposing factors, such as thin biotype, buccally positioned teeth, bone dehiscence, plaque-induced inflammation, and mechanical trauma from tooth brushing.27–30 Periodontal concerns are heightened when using RME in the late permanent dentition. Buccal bone loss in the horizontal and vertical dimensions is more likely to occur by buccal translation of the posterior teeth within the alveolar bone due to lack of sutural response. Therefore, early treatment of transverse maxillary skeletal discrepancy is essential to achieve an orthopedic effect.31,32
Three-dimensional CBCT imaging has improved the ability to assess the buccal bone of the maxillary posterior teeth. The accuracy of this method has been validated by Ising et al.33 However, the measuring technique is still limited to two-dimensional viewing of data. An initial attempt to quantitatively and qualitatively assess the buccal plate in three dimensions led us to realize that available software is incapable of performing this assessment. The main difficulty is that the nature of the buccal bone is relatively thin and less dense than the surrounding structures. CBCT evaluation of bone levels prior to maxillary expansion could be helpful to determine those patients in whom RME therapy should be chosen with caution to prevent detrimental effects on the periodontal tissues.
CONCLUSIONS
Banded and bonded hygienic expanders had similar effects on the buccal bone of the maxillary posterior teeth.
Horizontal buccal bone (BT) was reduced on MRt, MLft, PMRt, and PMLFt in both the banded and bonded groups following RME.
A tendency for vertical buccal bone loss (MBL) was observed; however, statistical significance was found only in the banded group on the MRt and PMLft following RME.
The CBCT is a reliable method for assessing changes in the buccal bone following RME.
REFERENCES
- 1.Haas AJ. The treatment of maxillary deficiency by opening the midpalatal suture. Angle Orthod. 1965;65:200–217. doi: 10.1043/0003-3219(1965)035<0200:TTOMDB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Haas AJ. Rapid expansion of the maxillary dental arch and nasal cavity by opening the midpalatal suture. Angle Orthod. 1961;31:73–89. [Google Scholar]
- 3.Haas AJ. Long-term post-treatment evaluation of rapid palatal expansion. Angle Orthod. 1965;50:189–217. doi: 10.1043/0003-3219(1980)050<0189:LPEORP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Wertz RA. Skeletal and dental changes accompanying rapid midpalatal suture opening. Am J Orthod. 1970:41–66. doi: 10.1016/0002-9416(70)90127-2. [DOI] [PubMed] [Google Scholar]
- 5.Starnbach H, Bayne D, Cleall J, Subtenly JD. Facioskeletal and dental changes resulting from rapid maxillary expansion. Angle Orthod. 1966;36:152–164. doi: 10.1043/0003-3219(1966)036<0152:FADCRF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Handelman CS, Wang L, BeGole EA, Haas A. Nonsurgical rapid maxillary expansion in adults: report on 47 cases using the haas expander. Angle Orthod. 1999;70:129–144. doi: 10.1043/0003-3219(2000)070<0129:NRMEIA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Vanardsdall RL. Periodontal/orthodontic interrelationships. In: Graber TM, Vanardsdall RL, editors. Orthodontics Current Principles and Techniques 2nd ed. St Louis, Mo : Mosby; 1994. pp. 712–749. [Google Scholar]
- 8.Betts NJ, Vanardsdall RL, Barber HD, Higgin-Barber K, Fonseca RJ. Diagnosis and treatment of transverse maxillary deficiency. Int J Adult Orthod Orthognat Surg. 1995;10:75–96. [PubMed] [Google Scholar]
- 9.McNamara JA, Jr, Baccetti T, Franchi L, Herberger TA. Rapid maxillary expansion followed by fixed appliances: a long term evaluation of changes in arch dimensions. Angle Orthod. 2003;73:344–353. doi: 10.1043/0003-3219(2003)073<0344:RMEFBF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Baccetti T, Franchi L, Cameron CG, McNamara JA., Jr Treatment timing for rapid maxillary expansion. Angle Orthod. 2001;71:343–350. doi: 10.1043/0003-3219(2001)071<0343:TTFRME>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Lagravere MO, Major PW, Flores-Mir C. Long-term dental arch changes after rapid maxillary expansion treatment: a systematic review. Angle Orthod. 2004;75:155–161. doi: 10.1043/0003-3219(2005)075<0151:LDACAR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Scarfe WC, Farman AG, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc. 2006;72:75. [PubMed] [Google Scholar]
- 13.Habersack K, Karoglan A, Sommer B, Benner K. High-resolution multislice computerized tomography with multiplanar and 3-dimensional reformation imaging in rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2007;131:776–781. doi: 10.1016/j.ajodo.2005.09.030. [DOI] [PubMed] [Google Scholar]
- 14.Kau CH, Richmond S, Palomo JM, Hans MG. Three-dimensional cone beam computerized tomography in orthodontics. J Orthod. 2005;32:282–293. doi: 10.1179/146531205225021285. [DOI] [PubMed] [Google Scholar]
- 15.Garrett BJ, Caruso JM, Rungcharassaeng K, Farrage JR, Kim JS, Taylor GD. Skeletal effects of the maxilla after rapid maxillary expansion assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2008;134(1):8.e1–8.e11. doi: 10.1016/j.ajodo.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 16.Garib DC, Henriques JFC, Janson G, Freitas MR, Coelho RA. Rapid maxillary expansion-tooth tissue-borne versus tooth-borne expanders. A computed tomography evaluation of dentoskeletal effects. Angle Orthod. 2005;75:548–557. doi: 10.1043/0003-3219(2005)75[548:RMETVT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Pangrazio-Kulbersh V, Wine P, Haughey M, Pajtas B, Kaczynski R. Cone beam computed tomography evaluation of changes in the naso-maxillary complex associated with two types of maxillary expanders. Angle Orthod. 2012;82:448–457. doi: 10.2319/072211-464.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rungcharassaeng K, Caruso J, Kan JY, Kim J, Taylor G. Factors affecting buccal bone changes of maxillary posterior teeth after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2007;132:428.e1–428.e8. doi: 10.1016/j.ajodo.2007.02.052. [DOI] [PubMed] [Google Scholar]
- 19.Garib DG, Henriques JFC, Janson G, Freitas MR, Fernandes AY. Periodontal effect of rapid maxillary expansion with tooth-tissue-borne and tooth-borne expanders: a computed tomography evaluation. Am J Orthod Dentofacial Orthop. 2006;129:749–758. doi: 10.1016/j.ajodo.2006.02.021. [DOI] [PubMed] [Google Scholar]
- 20.Berger JL, Pangrazio-Kulbersh V, Borgula T, Kaczynski R. Photographic analysis of facial changes associated with maxillary expansion. Am J Orthod Dentofacial Orthop. 1999;116:563–571. doi: 10.1016/s0889-5406(99)70190-3. [DOI] [PubMed] [Google Scholar]
- 21.Steiner GG, Pearson JK, Ainamo J. Changes of the marginal periodontium as a result of labial tooth movement in monkeys. J Periodontol. 1981;52:314–320. doi: 10.1902/jop.1981.52.6.314. [DOI] [PubMed] [Google Scholar]
- 22.Thilander B, Nyman S, Karring T, Magnusson I. Bone regeneration in alveolar bone dehiscences related to orthodontic tooth movements. Eur J Orthod. 1983;5:105–114. doi: 10.1093/ejo/5.2.105. [DOI] [PubMed] [Google Scholar]
- 23.Wennstrom JL, Lindhe J, Sinclair F, Thilander B. Some periodontal tissue reactions to orthodontic tooth movements in monkeys. J Clin Periodontol. 1987;14:121–129. doi: 10.1111/j.1600-051x.1987.tb00954.x. [DOI] [PubMed] [Google Scholar]
- 24.Engelking G, Zachrisson BU. Effects of incisor repositioning on monkey periodontium after expansion through the cortical plate. Am J Orthod. 1982;82:23–32. doi: 10.1016/0002-9416(82)90542-5. [DOI] [PubMed] [Google Scholar]
- 25.Watson WG. Expansion and fenestration or dehiscence. Am J Orthod. 1982;82:330–332. doi: 10.1016/0002-9416(80)90086-x. [DOI] [PubMed] [Google Scholar]
- 26.Greenbaum KR, Zarchrisson BU. The effect of palatal expansion therapy on the periodontal supporting tissues. Am J Orthod. 1982;81:12–21. doi: 10.1016/0002-9416(82)90283-4. [DOI] [PubMed] [Google Scholar]
- 27.Saunders NL. Evidence-based care in orthodontics and periodontics: a review of the literature. J Am Dent Assoc. 1999;130:521–527. doi: 10.14219/jada.archive.1999.0246. [DOI] [PubMed] [Google Scholar]
- 28.Andlin-Sobocki A, Bodin L. Dimensional alterations of the gingiva related to changes of facial/lingual tooth position in permanent anterior teeth of children. A 2-year longitudinal study. J Clin Periodontol. 1993;20:219–224. doi: 10.1111/j.1600-051x.1993.tb00347.x. [DOI] [PubMed] [Google Scholar]
- 29.Artun J, Groberty D. Periodontal status of mandibular incisors after pronounced orthodontic advancement during adolescence: a follow-up evaluation. Am J Orthod Dentofacial Orthop. 2001;119:2–10. doi: 10.1067/mod.2001.111403. [DOI] [PubMed] [Google Scholar]
- 30.Ruf S, Hansen K, Pancherz H. Does orthodontic proclination of lower incisors in children and adolescents cause gingival recession. Am J Orthod Dentofacial Orthop. 1998;114:100–106. doi: 10.1016/s0889-5406(98)70244-6. [DOI] [PubMed] [Google Scholar]
- 31.Silva Filho OG, Montes LA, Torelly LF. Rapid maxillary expansion in the deciduous and mixed dentition evaluated through posteroanterior cephalometric anlaysis. Am J Orthod Dentofacial Orthop. 1995;107:268–275. doi: 10.1016/s0889-5406(95)70142-7. [DOI] [PubMed] [Google Scholar]
- 32.Krebs A. Rapid expansion of the midpalatal suture by fixed appliance: an implant study over a seven year period. Trans Euro Orthod Soc. 1964;10:131–142. [PubMed] [Google Scholar]
- 33.Ising N, Kim KB, Araujo E, Buschang P. Evaluation of dehiscences using cone beam computed tomography. Angle Orthod. 2012;82:122–130. doi: 10.2319/020911-95.1. [DOI] [PMC free article] [PubMed] [Google Scholar]