Abstract
Objective:
To evaluate the impact of psychological traits on patients' choice of orthodontic appliances and their adjustability to orthodontic treatment.
Materials and Methods:
The sample consisted of 68 adult patients divided into three groups (28 buccal, 19 lingual, and 21 clear aligners). Prior to treatment participants filled out the Brief Symptom Inventory to assess symptoms of mental distress and the Narcissistic Vulnerability Scale to assess narcissistic personality traits. During the first week after appliance delivery and on day 14, patients completed a Health-Related Quality of Life questionnaire to assess their perception of pain and four areas of dysfunction. The correlation between personality traits and patients' reaction to treatment was evaluated.
Results:
Somatization was the only trait that affected the choice of lingual and clear aligner appliance. Reduced self-esteem regulation was associated with increased pain in all patients, while exploitation was associated with pain in lingual patients. Narcissistic vulnerability slightly influenced patients' adaptability to orthodontic appliances. Although adjustability to lingual appliances was the most difficult, only two parameters were affected by personality features. In the buccal group, adjustability was affected by numerous parameters. Adaptation to the clear aligner appliance was relatively uneventful and least affected by psychological features.
Conclusion:
Anxious individuals tend to prefer lingual and clear aligner appliances. The selection of lingual and clear aligner appliances governs the patient's response and recovery process, leaving little room for the effect of psychological features. On the other hand, the buccal appliance allows for greater impact of personality traits on adjustability.
Keywords: Adult, Orthodontic appliance, Personality, Psychological, Adjustability
INTRODUCTION
Adult patients seek orthodontic treatment mainly for esthetic reasons and, to a lesser extent, for functional reasons. Consequently, while the traditional labial appliance (buccal) remains the predominant appliance used, it is not surprising that the more esthetic treatment options of lingual1–3 and clear aligner appliances4 are gaining popularity.
Females under 40 years of age select lingual appliances as a result of esthetic and professional considerations.5,6 A similar profile is found for the clear aligner appliance: 20–30-year-old females prefer this appliance over the buccal appliance for esthetic reasons and over the lingual appliance for functional reasons.7,8
Several studies have assessed patient adaptation to orthodontic appliances, comparing buccal and lingual appliances,6,7,9,10 and clear aligner and buccal appliances.11 In a recent study12 we compared adult patients' adjustability to the three available appliances. Lingual appliances were associated with more severe pain and higher analgesic consumption, the greatest oral and general dysfunction, and the most difficult and longest recovery. The clear aligner patients complained of relatively high levels of pain in the first days after insertion; however, this group was characterized by the lowest level of oral symptoms and by a similar level of general activity disturbance and oral dysfunction when compared to the buccal appliance.12
A patient's choice of appliance may reflect personality traits or psychological status. These in turn may affect the patient's adaptation and adjustability with regard to the appliances. Al-Omiri and Abu Alhaija13 found an association between personality traits and satisfaction after orthodontic treatment: neurotic personality traits were associated with greater dissatisfaction. However, Abu Alhaija et al.14 studied the relationships between personality traits and pain perception during orthodontic treatment and did not find a significant correlation.
The objectives of this study were (1) to determine the psychological features associated with adult patients' appliance selection and (2) to evaluate adjustability to the available orthodontic techniques (buccal, lingual, and clear aligners). We hypothesized that stressed patients would have difficulty with adaptation to the appliance. In addition, we assessed the specific trait of narcissistic vulnerability under the assumption that narcissistic features would affect appliance selection and would also hinder the adaptation process.
MATERIALS AND METHODS
The sample included 68 adult patients (45 females and 23 male), who comprised three groups according to the type of orthodontic appliance used: 28 patients chose treatment with buccal appliances, 19 with lingual appliances, and 21 with clear aligners. Consecutive patients were recruited prospectively from the orthodontic clinic in the Hebrew University–Hadassah School of Dental Medicine and from two private clinics. Patients were treated by the same two senior clinicians in both facilities. Inclusion criteria were the following: consecutive adult patients applying for comprehensive orthodontic treatment who were fluent in Hebrew. The study was approved by the Hadassah Medical Center Ethics Committee for Clinical Trials, and informed consent was obtained from all participants after an explanation of the study was provided.
The three groups were not entirely balanced with respect to size and gender. The buccal group was the largest group (N = 28), consisting of an identical number of men and women. The clear aligners group (N = 21) comprised five men and 16 women. Finally, the smallest group was the lingual group (N = 19), with four men and 15 women. Although the male/female balance was different for the buccal compared to the other groups, this difference did not reach statistical significance. Ages ranged from 19 to 47 years (except for one subject in the clear aligners group who was 60 years old). In the buccal group the mean age was 29.3 years (range = 20–45 years; standard deviation [SD] = 8.1 years); in the lingual group the mean age was 34 years (range = 25–47 years; SD = 9.1 years); and in the clear aligners group the mean age was 29.4 years (range = 19–60 years; SD = 13.9 years). The age differences were not statistically significant.
The buccal appliance was a straight wire appliance (0.022 × 0.028–inch slots) manufactured by GAC and Ormco. The lingual appliance was Incognito™. The initial wire was 0.014-inch Nitinol wire for all buccal and lingual patients. The clear aligner appliance was Invisalign®.
Prior to initiation of treatment all participants filled out the following questionnaires.
1. The Brief Symptom Inventory
The Brief Symptom Inventory (BSI) is designed to assess psychological status and symptoms of mental distress. It consists of 53 self-report, symptom-inventory questions arranged in nine dimensions, as follows: “Somatization” reflects distress arising from perception of bodily dysfunction; “Obsessive-compulsive” measures unwanted thoughts, impulses, or actions that are unremitting and irresistible; “Interpersonal sensitivity” centers on feelings of personal inadequacy and inferiority; “Depression” reflects symptoms indicating clinical depression; “Anxiety” composes symptoms associated with anxiety; “Hostility” indicates thoughts, feelings, or actions that characterize a negative-affect state of anger; “Phobic anxiety” is defined as persistent and irrational fear response to a person, place, object, or situation that leads to avoidance; “Paranoid ideation” represents a paranoid disorder of thought or behavior; and “Psychoticism” indicates a withdrawn, isolated, or schizoid lifestyle or first-rank symptoms of schizophrenia. Answers are rated on a five-point scale from 0 (“not at all”) to 4 (“extremely”).
The BSI has high internal consistency (Cronbach's alpha: 0.71–0.85); test-retest reliability; and convergent, discriminant, and construct validity.15 The questionnaire has a Global Severity Index (GSI) defined as the total sum of all items. Canetti et al.16 studied BSI norms in Israeli adolescents and reported high levels of internal consistency and good concurrent validity in the Hebrew version (Cronbach's alpha for GSI = .95). In the present study the internal consistency was also very high (Cronbach alpha = .95).
2. The Glasgow Health Status Inventory
The Glasgow Health Status Inventory (GHSI) is a questionnaire designed to measure the effect of a health problem on the quality of life. It allows cross-comparison between many health conditions, between different health interventions, and between demographic and cultural subgroups. Originally developed for oto-rhino-laryngological surgery, the questionnaire was adapted to orthodontic intervention. It consists of 18 questions, each one addressing an aspect of health-related quality of life. The response to each question is based on a five-point Likert scale ranging from “high” health status to “low” health status. The GHSI presents a total score and three subscales; a general subscale (12 questions), a social support subscale (three questions), and a physical health subscale (three questions). The questionnaire was found to be valid and had high levels of internal consistency (Cronbach's alpha = 0.87).17 The questionnaire was translated to Hebrew, and in the present study this version had good levels of internal consistency (Cronbach's alpha = 0.80).
3. Narcissistic Vulnerability Scale
The Narcissistic Vulnerability Scale (NVS) is a questionnaire developed in order to assess personality traits related to the existence of narcissistic personality disorder. The questionnaire consists of 48 questions: 10 for grandiosity, 11 for exploitation, and 14 for self-esteem regulation. Thirteen additional items do not relate to the concept of narcissism and are interspersed among the items to prevent a response set. Participants were asked to rate the adherence to each item on a five-point Likert scale. Grandiosity measures to what extent the individual has a grandiose sense of self-importance and requires constant admiration. Exploitation measures to what extent the individual has a sense of entitlement and to what extent he takes advantage of others to achieve his own goals. Self-esteem regulation measures to what extent the individual feels vulnerable and is unable to regulate his self-esteem in the face of narcissistic blows. This questionnaire was developed in Hebrew for the purpose of a previous study on post-trauma and narcissism in the Israeli population. The instrument had good concurrent validity with other scales of narcissism and high internal consistency (Cronbach's alpha = .88).18 In the present study the internal consistency was also high (Cronbach's alpha = .85).
4. Health-Related Quality of Life
After appliance insertion, patients completed a daily Health-Related Quality of Life (HRQOL) questionnaire during the first week and again on day 14. This questionnaire was based on previously used HRQOL instruments19–21 adapted for the present study. The questionnaire assessed the patients' perception of pain severity and dysfunction in four areas. The four areas of dysfunction examined were (1) Oral dysfunction—assessing difficulties in speaking, swallowing, or opening the mouth; (2) Disturbance in eating—examining eating difficulties, reduced enjoyment of food, and change in taste; (3) General activity disturbance—focusing on sleeping, the ability to participate in routine daily activities, and school/work attendance; and (4) Oral symptoms, including sores on the tongue, cheeks, or lip; bad taste/smell; and food accumulation in the mouth. Each parameter was assessed on a five-point scale, as follows: 1 = no instances, 2 = few instances (less than three), 3 = some instances (three to five), 4 = several instances (six to 10), and 5 = numerous instances (more than 10).
In order to perform statistical analyses of the four areas of dysfunction, a mean score of the items in each area was obtained. In the present study the internal consistency of the test was high (Cronbach's alpha = .86 to .91 for all items, .80 to .88 for oral dysfunction, .87 to .92 for disturbance in eating, and .81 to .88 for general activity measures; only for oral symptoms was the reliability lower, at .50 to .60).
5. Visual Analogue Scale
The degree of pain was assessed using the Visual Analogue Scale with scores ranging from 1 to 10, with scores of 1–3 representing mild pain, scores of 4–7 representing moderate pain, and scores of 8–10 representing severe pain.
6. Analgesic Consumption
Analgesic consumption was based on patient self-report.
Recovery time, defined as the number of days needed to achieve mild symptoms or no symptoms, was calculated and compared among the three groups.19–21
Statistical Analyses
Analysis of variance (ANOVA) and post hoc tests were used to compare between groups for the quantitative interval variables, and chi-square tests were used to compare between groups for categorical variables. Pearson correlations were computed to assess relationships between interval variables. A P value <.05 was taken as the minimum criterion of significance.
RESULTS
Appliance Selection
Narcissistic vulnerability, as assessed by the NVS questionnaire, was similar among all patients and was not a factor in the selection of a specific orthodontic appliance. A statistically significant difference was found in only one out of nine categories of the BSI. Patients selecting lingual and clear aligner appliances tended to express more somatization symptoms compared to buccal patients (P = .025). The lingual group also showed more obsessive-compulsive symptoms compared to the two other groups; however, this difference did not reach statistical significance (P = .073).
The effect of the initial patients' orthodontic problems on their quality of life was assessed using the GHSI questionnaire (Figure 1). It was only in the physical health subscale that a significant difference was found between the lingual and clear aligner groups (P = .017), with clear aligner patients expressing the lowest perceived physical health. No differences were found in the general or the social support subscales among the three appliance groups.
Figure 1. .
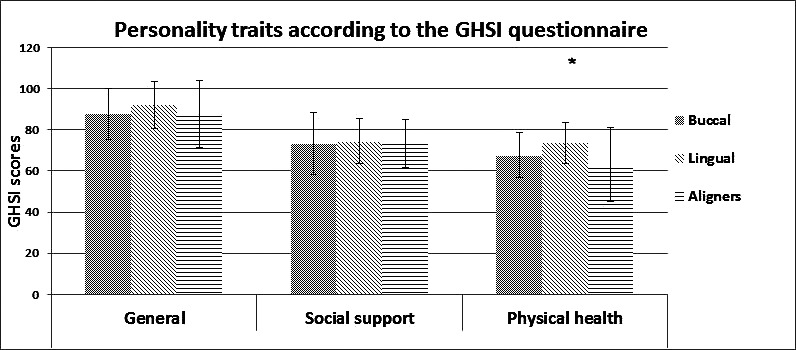
Quality of life as a function of appliance selection. * P < .05.
Pain levels, analgesic consumption, adjustability, and recovery are discussed in detail in a previous study.12
Pain Severity and its Association with Narcissistic Features
The relationship between severity of pain (severe/non-severe) and the three main categories of narcissism was examined over the first 3 days of treatment. We examined the first 3 days since severe pain was mainly reported in this period.12 Two-way ANOVAs were performed for the factors of pain severity (severe/non-severe) and appliance (buccal/lingual/clear aligner). With regard to self-esteem regulation, although on the first 2 days there were no differences, on the third day a relationship was found between self-esteem regulation and the severity of pain in all treatment groups. Patients who reported higher levels of pain had reduced self-esteem regulation (P = .031; Figure 2). Similarly, on the third day, a relationship was found between exploitation and pain levels for lingual patients. Patients reporting higher levels of pain had more narcissistic features (P = .005; Figure 3). No relationship was found between the severity of pain and grandiosity.
Figure 2. .

Self-esteem regulation as a function of pain severity and appliance. * P < .05.
Figure 3. .
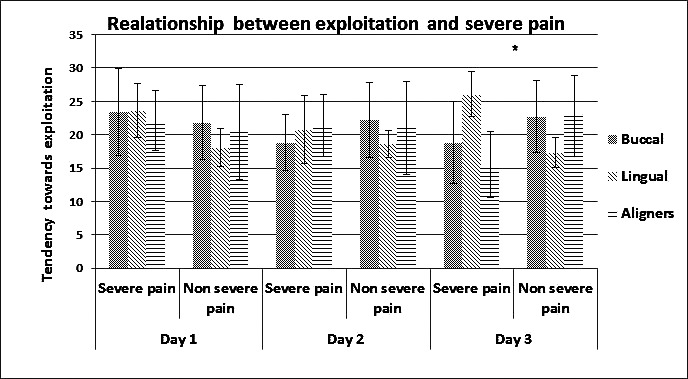
Exploitation as a function of pain severity and appliance. * P < .05.
The Impact of Personality Traits and Psychological Features on Recovery
Personality traits had a significant impact on recovery, mainly in the buccal group. In this group somatization extensively affected recovery in most symptom categories (Table 1). Obsessive-compulsive traits, grandiosity, and hostility affected recovery for general activities and oral dysfunction, while paranoid ideation affected general activities and oral symptoms. Recovery from pain was significantly influenced by somatization and hostility traits.
Table 1. .
The Impact of Psychological Features on Recovery Time in Different Orthodontic Appliances (Only Appliances That Produced Statistically Significant Results Are Presented)
In the lingual group recovery time for only two symptoms, disturbances in eating and oral symptoms, was significantly affected by psychological features such as grandiosity, exploitation, depression, and hostility. In the clear aligners group recovery time for general activities was affected by exploitation.
DISCUSSION
Many patients who opt to use lingual or clear aligner appliances are young women, and this choice is made mainly for reasons of esthetics, profession, or function.5–8,22,23 What determines response, adjustability, and recovery in orthodontic treatment? Are there significant psychological factors involved in the choice of the orthodontic appliance and in patients' perceptions of quality of life after appliance insertion? Little research has been done on this subject, and to our knowledge this study represents the first time that the relationship between appliance selection and psychological features has been investigated.
We examined personality traits and psychological features that could explain patients' preference in the selection of orthodontic appliances. Among the various psychological factors assessed with the BSI questionnaire only somatization had a clear effect, favoring the lingual appliance and clear aligners over the buccal appliance. Obsessive-compulsive symptoms had a slight effect, favoring lingual over buccal appliances. Anxiety is the common denominator of these two dimensions in the BSI. In somatization anxiety is directed toward bodily functions, and obsessive-compulsive symptoms are considered anxious by nature. These findings indicate that patients with a variety of anxious features, especially those with bodily concern, tend to shy away from the more obvious buccal appliance and prefer the concealed lingual or clear aligner appliances. This may illustrate the idiom “out of sight, out of mind.”
Narcissistic traits were found to have no effect on appliance selection. This is in contrast to the expectation that more narcissistic-vulnerable individuals would prefer less conspicuous appliances.
The meaning of the greater physical health concern found in the lingual patients remains unclear to us.
Although narcissistic personality traits did not affect appliance selection, they had an impact on coping with pain. Individuals with reduced self-esteem regulation reported more pain across all three orthodontic appliances. Lingual patients were also higher on the exploitation dimension. As hypothesized, the present results suggest an association between narcissistic vulnerability and adaptability to orthodontic appliance. Our findings are not in line with those of Abu Alhaija et al.,14 who found no significant correlation between personality traits and pain perception during orthodontic treatment.
After appliance selection it is mainly in the buccal group that we see a substantial effect of psychological features on adjustability and recovery. For buccal patients, personality traits and psychological features had a significant impact on adaptability.
Our findings in the lingual appliance group were extremely different from those associated with the buccal group. In our previous study12 lingual patients were found to have a significantly more difficult adaptation across the many areas of dysfunction. In the current study, only two areas of adaptation were found to be affected by psychological features: disturbance in eating and oral symptoms. We suggest that adaptation to the lingual appliance is, in itself, demanding for most patients, shadowing the expression of individual psychological elements on adaptation.
Finally, the clear aligner appliance group seems to behave differently. Adaptation to the clear aligner appliance is relatively uneventful in most areas.12 We suggest that as a result of the general ease of adaptation, psychological features have little effect on the adaptation process.
Our study is a first attempt to address the topic of appliance selection from a psychological viewpoint, and in this regard it is a pilot study.
CONCLUSIONS
Anxious individuals tend to prefer lingual and clear aligner appliances.
The selection of lingual and clear aligner appliances governs the patient's response and recovery process, leaving little room for the effect of psychological features.
On the other hand, buccal appliances allow for greater impact of personality traits on adjustability.
Acknowledgments
The authors wish to thank Professor Adrian Becker, Doctor Tom Weinberger, and Professor Ilana Brin for their constructive comments.
REFERENCES
- 1.Fujita K. Development of lingual bracket technique: aesthetic and hygiene approach to orthodontic treatment. Jpn Res Soc Dent Mater Appliances. 1978;46:81–86. [PubMed] [Google Scholar]
- 2.Sinclair PM, Cannito MF, Goates LJ, Solomos LF, Alexander CM. Patient responses to lingual appliances. J Clin Orthod. 1986;20:396–404. [PubMed] [Google Scholar]
- 3.Creekmore TD. Lingual orthodontics—its renaissance. Am J Orthod Dentofacial Orthop. 1989;96:120–137. doi: 10.1016/0889-5406(89)90253-9. [DOI] [PubMed] [Google Scholar]
- 4.Wong BH. Invisalign A to Z. Am J Orthod Dentofacial Orthop. 2002;121:540–541. doi: 10.1067/mod.2002.123036. [DOI] [PubMed] [Google Scholar]
- 5.Hohoff A, Wiechmann D, Fillion D, Stamm T, Lippold C, Ehmer U. Evaluation of the parameters underlying the decision by adult patients to opt for lingual therapy: an international comparison. J Orofac Orthop. 2003;64:135–144. doi: 10.1007/s00056-003-0217-7. [DOI] [PubMed] [Google Scholar]
- 6.Fritz U, Diedrich P, Wiechmann D. Lingual technique—patients' characteristics, motivation and acceptance. J Orofac Orthop. 2002;63:227–233. doi: 10.1007/s00056-002-0124-3. [DOI] [PubMed] [Google Scholar]
- 7.Nedwed V, Miethke RR. Motivation, acceptance and problems of Invisalign patients. J Orofac Orthop. 2005;66:162–173. doi: 10.1007/s00056-005-0429-0. [DOI] [PubMed] [Google Scholar]
- 8.Miethka RR, Wiemer KB, Meier B. Invisalign—patient profiling. Analysis of a prospective survey. J Orofac Orthop. 2003;64:352–358. doi: 10.1007/s00056-003-0301-z. [DOI] [PubMed] [Google Scholar]
- 9.Caniklioglu C, Oztürk Y. Patient Discomfort: A comparison between lingual and labial fixed appliances. Angle Orthod. 2005;75:86–91. doi: 10.1043/0003-3219(2005)075<0086:PDACBL>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Wu AK, McGrath C, Wong RW, Wiechmann D, Rabie AB. A comparison of pain experienced by patients treated with labial and lingual orthodontic appliances. Eur J Orthod. 2010;32:403–407. doi: 10.1093/ejo/cjp117. [DOI] [PubMed] [Google Scholar]
- 11.Miller KB, McGorray SP, Womack R, Quintero JC, Perelmuter M, Gibson J, Dolan TA, Wheeler TT. A comparison of treatment impacts between Invisalign aligner and fixed appliance therapy during the first week of treatment. Am J Orthod Dentofacial Orthop. 2007;131:302.e1–302.e9. doi: 10.1016/j.ajodo.2006.05.031. [DOI] [PubMed] [Google Scholar]
- 12.Shalish M, Cooper-Kazaz R, Ivgi I, Canetti L, Tsur B, Bachar E, Chaushu S. Adult patients' adjustability to orthodontic appliances. Part I: a comparison between labial, lingual, and Invisalign. Eur J Orthod. 2011 July 12 doi: 10.1093/ejo/cjr086. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 13.Al-Omiri MK, Abu Alhaija ES. Factors affecting patient satisfaction after orthodontic treatment. Angle Orthod. 2006;76:422–431. doi: 10.1043/0003-3219(2006)076[0422:FAPSAO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Abu Alhaija ES, Aldaikki A, Al-Omairi MK, Al-Khateeb SN. The relationship between personality traits, pain perception and attitude toward orthodontic treatment. Angle Orthod. 2010;80:1141–1149. doi: 10.2319/012710-59.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13:595–605. [PubMed] [Google Scholar]
- 16.Canetti L, Shalev AY, De-Nour AK. Israeli adolescents' norms of the Brief Symptom Inventory (BSI) Isr J Psychiatr Relat Sci. 1994;31:13–18. [PubMed] [Google Scholar]
- 17.Hawthorne G, Hogan A. Measuring disability-specific patient benefit in cochlear implant programs: developing a short form of the Glasgow Health Status Inventory, the Hearing Participation Scale. Int J Audiol. 2002;41:535–544. doi: 10.3109/14992020209056074. [DOI] [PubMed] [Google Scholar]
- 18.Bachar E, Hadar H, Shalev AY. Narcissistic vulnerability and the development of PTSD: a prospective study. J Nerv Ment Dis. 2005;193:762–765. doi: 10.1097/01.nmd.0000185874.31672.a5. [DOI] [PubMed] [Google Scholar]
- 19.Chaushu S, Becker A, Zeltser R, Vasker N, Chaushu G. Patients' perception of recovery after surgical exposure of impacted maxillary teeth treated with an open-eruption surgical-orthodontic technique. Eur J Orthod. 2004;26:591–596. doi: 10.1093/ejo/26.6.591. [DOI] [PubMed] [Google Scholar]
- 20.Chaushu S, Becker A, Zeltser R, Branski S, Vasker N, Chaushu G. Patients' perception of recovery after exposure of impacted teeth: a comparison of closed- versus open-eruption techniques. J Oral Maxillofac Surg. 2005;63:323–329. doi: 10.1016/j.joms.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 21.Chaushu G, Becker A, Zeltser R, Vasker N, Branski S, Chaushu S. Patients′ perceptions of recovery after routine extraction of healthy premolars. Am J Orthod Dentofacial Orthop. 2007;131:170–175. doi: 10.1016/j.ajodo.2005.06.024. [DOI] [PubMed] [Google Scholar]
- 22.Miethke RR, Brauner K. A comparison of the periodontal health of patients during treatment with the Invisalign system and with fixed lingual appliances. J Orofac Orthop. 2007;68:223–231. doi: 10.1007/s00056-007-0655-8. [DOI] [PubMed] [Google Scholar]
- 23.Kravitz ND, Kusnoto B, BeGole E, Obrez A, Agran B. How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. Am J Orthod Dentofacial Orthop. 2009;135:27–35. doi: 10.1016/j.ajodo.2007.05.018. [DOI] [PubMed] [Google Scholar]



