Abstract
Our aim was to reduce the frequency of unnecessary testing used by pediatric cardiologists in the evaluation of pediatric patients with syncope or pre-syncopal symptoms without negatively affecting patient outcomes. Guidelines for cardiac testing in pediatric patients with syncope were developed and disseminated to members of our pediatric cardiology division. Educational brochures and water bottles labeled with tips on preventing syncope were made available to families and providers in our clinics. Compliance to the guidelines was tracked and shared with providers. Segmented regression analysis was used to model cardiac testing utilization and guideline compliance by provider over time before and after the implementation of the guidelines. A pre-intervention cohort of 237 patients (June 2014–May 2015) was compared to 880 post-intervention patients (August 2015–June 2019). There was a significant decrease in the utilization of unnecessary tests [odds ratio (OR) 0.3; 95% confidence interval (CI) 0.14, 0.65; p = 0.002] after the intervention. Charges associated with patient evaluation were significantly lower in the post-intervention cohort (interquartile range $0, $1378 vs $0, $213; p = 0.005). Post-intervention visits to emergency departments within our system were significantly decreased, with no change in the incidence of cardiac arrest, hospitalization for syncope, or referral to pediatric electrophysiologists. We demonstrated a significant reduction in the use of unnecessary testing and associated charges by developing guidelines related to the evaluation of pediatric patients with syncope or pre-syncopal symptoms. There was no demonstrable negative impact on patient outcomes.
Keywords: Pediatric, Syncope, Cardiac disease, Quality improvement, Diagnostic test
Introduction
Syncope is a common problem in children, with an incidence ranging from 15 to 35% in the pediatric population [1, 2]. Determining the etiology of dizziness and syncope can be costly and time-consuming, often leading to referral to a pediatric cardiologist to rule out possible life-threatening cardiac etiologies. However, the majority of evaluations lead to a diagnosis of vasovagal syncope (VVS). Only about 0.4–3% of pediatric syncope is secondary to underlying cardiac disease, with the most common causes including arrhythmias, hypertrophic cardiomyopathy, inherited cardiomyopathies, or coronary artery anomalies [3–6].
Physical examination, along with careful review of the patient’s history, are key to evaluating these patients [7, 8], but beyond an electrocardiogram (ECG), more extensive testing, including echocardiograms, exercise tests, and event monitors, is often costly with a low diagnostic yield [9–11]. In order to safely manage patients presenting with lightheadedness or syncope without over-testing, a number of care pathways have been developed for identifying low-risk patients [4, 12, 13].
We evaluated how individual providers in our academic pediatric cardiology division approached patients with pre-syncope or syncope and found significant variability in testing utilized. Even though the majority of patients had a clinical history consistent with a vasovagal etiology, many patients underwent additional cardiac testing in the absence of identified risk factors for an underlying cardiac etiology. We identified this variability as a source of unnecessary testing and expense.
Therefore, the aim of this quality improvement project was to develop syncope testing guidelines and promote a standardized approach to the evaluation of children and adolescents referred to our pediatric cardiology clinics for the evaluation and treatment of pre-syncope and syncope. Additionally, we sought to assess the impact of our guidelines on associated patient charges and outcomes.
Materials and Methods
Guidelines and Supplemental Materials
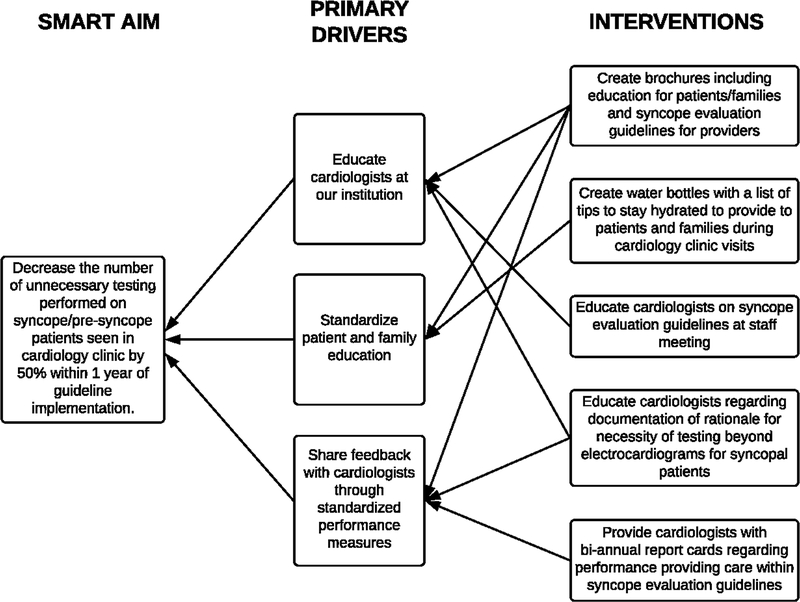
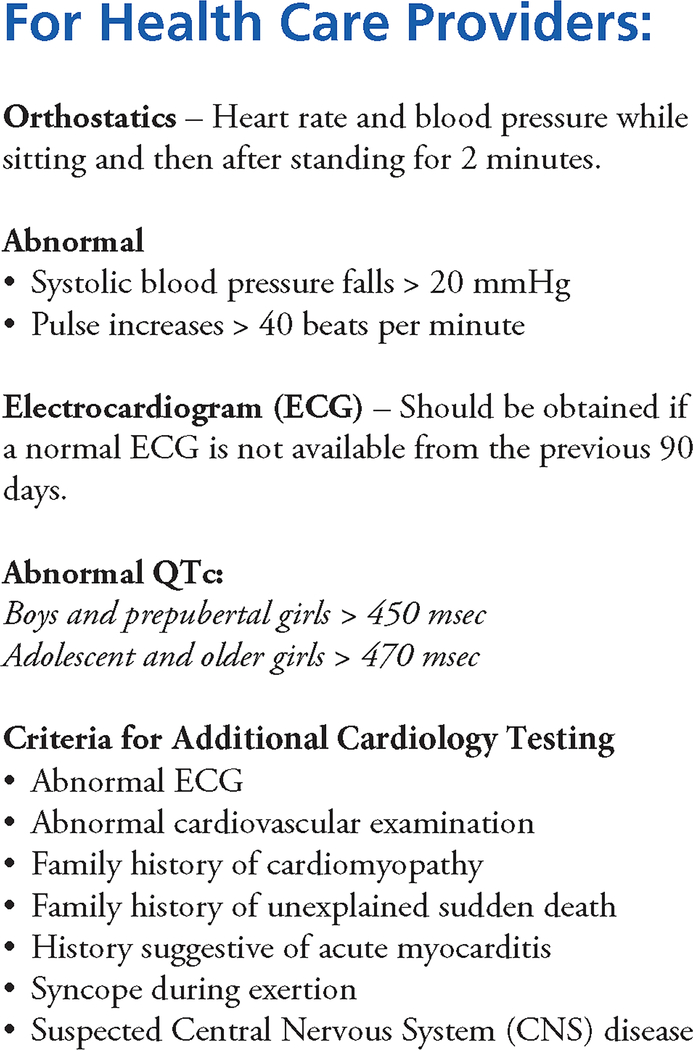
After we identified the need for standardization of care, a key driver diagram was created (Fig. 1). Clinical care guidelines for the evaluation of children and adolescents seen with a chief complaint of dizziness, light-headedness, pre-syncope, or syncope were developed from the current literature and by soliciting input from our providers. A current (within 90 days of the clinic visit) ECG was established as the only uniformly indicated cardiac test. The guidelines clarify the indications for additional testing (Fig. 2). Once a patient has met criteria for additional testing, the modality of testing chosen is left to the discretion of the provider based upon individual clinical presentation. Obtaining a repeat ECG during the clinic visit was considered acceptable even if another ECG from the past 90 days was available. Pediatric cardiologists were asked to explain the rationale for cardiac testing beyond an ECG and to make note of this in the patient’s chart.
Fig. 1.
Syncope evaluation initiative key driver diagram
Fig. 2.
Syncope evaluation guidelines
Supplemental materials were also developed to standardize the approach to these patients and to simplify patient management and education provided by pediatric cardiologists. Brochures describing the etiology, management, and prevention of vasovagal syncope were created and made available in our cardiology clinics. Given the importance of hydration in the management of pre-syncope and syncope, water bottles for patient use were also developed that were labeled with a list of tips for the prevention and management of lightheadedness and fainting on the bottle.
Study of the Intervention
At least every 3 months, patient charts were reviewed to assess for physician compliance to guidelines and adverse outcomes. If criteria were met, including physician compliance to guidelines > 80% and adverse outcomes < 2 events annually, then the guidelines continued unchanged until the next review. Throughout the study period, criteria were met to proceed and no changes were made to the guidelines. Use of the guidelines and supplemental materials was reinforced during quarterly performance evaluations and staff meetings.
Study Population and Setting
The study cohort included patients evaluated in our academic pediatric cardiology clinics, aged 5–18 years, presenting with a chief complaint of dizziness, light-headedness, pre-syncope, or syncope. Only initial cardiology evaluations were included for analysis. A pre-intervention cohort consisted of patients meeting inclusion criteria who were seen in our pediatric cardiology clinics during the 12-month period from June 2014 to May 2015. The formal syncope evaluation guidelines were disseminated to our providers in early June 2015. The post-intervention cohort consisted of patients seen from August 2015 to June 2019, allowing a 2-month washout period following introduction of the guidelines. Patients with a prior diagnosis of congenital heart disease, arrhythmia, pacemaker, or pulmonary hypertension were excluded from analysis. Providers were given quarterly feedback during performance evaluations on their use of the guidelines as a group and individually.
Measures
Data were collected through chart review and included: patient age, gender, cardiology provider, diagnostic cardiac testing completed, diagnoses, and patient outcomes. Major cardiac testing included electrocardiogram (ECG), echocardiogram (echo), rhythm monitoring, chest x-ray (CXR), and exercise testing. Charges for testing were estimated from standardized, approximate values and not based on individual medical bills.
The primary outcome of this study was compliance with the management guidelines, as demonstrated by the number of unnecessary tests utilized in the evaluation of these patients. The secondary outcome was associated cost using standardized, estimated charges of major tests, including testing supported by the guidelines and testing that was deemed unnecessary. Patient outcomes including a diagnosis of significant arrhythmia, cardiac arrest, and physician visit or hospitalization for syncope or other cardiac abnormality were monitored by chart review throughout the study period up to January 2020.
Statistical Analysis
Patient age, gender, diagnosis and testing outcomes were summarized and descriptively stratified by pre- and post-intervention cohorts. Continuous and count variables were summarized as mean (standard deviation (SD)), median (interquartile range (IQR)) and range, and compared using Wilcoxon rank sum tests between cohorts. Categorical variables were summarized as frequency and percentage and compared using chi-squared or Fisher’s exact tests where appropriate.
The effect of the intervention was evaluated using segmented regression, which estimated the immediate intervention effect (pre/post) after the 2-month washout window, the existing time trend prior to the intervention, and the difference between the post-intervention time trend and the pre-intervention time trend. For guideline compliance and unnecessary testing, logistic models were used where the exponentiated coefficients represented odds ratios (ORs). Coefficients, 95% confidence intervals (CIs) and p values were reported from all models. For each outcome, the model was run with and without adjusting for age, gender, and diagnosis. Observed outcomes in the pre- and post-intervention are displayed in statistical process control charts. Analyses were conducted using R 3.5. Statistical significance was assessed at the 0.05 level, and all tests were two-tailed.
Ethical Considerations
This quality improvement study was approved by the University of Utah Institutional Review Board and Primary Children’s Hospital Privacy Board.
Results
Between June 2014 and June 2019, 1174 patients were seen in our pediatric cardiology clinics who met the inclusion criteria. Exclusions included 23 repeat referrals for vasovagal syncope and 34 patients seen during the washout period of June and July 2015. Therefore, 1117 patients were included for analysis, with 237 pre-intervention patients and 880 post-intervention patients. Referral rates averaged 20 patients/month in the pre-intervention cohort and 22 patients/month in the post-intervention cohort.
Patient characteristics are described in Table 1. Age and gender distribution were similar in both cohorts. Final diagnosis as assigned by the patient’s cardiologist, included VVS (87% pre- vs 73% post-intervention), syncope with exertion (8% vs 9%), dizziness (3% vs 12%), postural orthostatic tachycardia syndrome (1% vs 3%), and other (2% vs 3%).
Table 1.
Patient characteristics
| Variable | Pre-implementation cohort n = 240 | Post-implementation cohort n = 897 | p value |
|---|---|---|---|
|
| |||
| Age at clinic visit, years | |||
| Median (IQR) | 14.7 (12.5, 16.2) | 14.6 (12.3, 16.1) | 0.59 |
| Range | 5.7, 17.9 | 5.1, 18.0 | |
| Gender, n(%) | |||
| Male | 83 (35) | 369 (42) | 0.06 |
| Female | 153 (65) | 511 (58) | |
| Diagnosis, n(%) | < 0.001 | ||
| Dizziness | 7 (3) | 108 (12) | |
| POTS | 3 (1) | 24 (3) | |
| SWE | 18 (8) | 79 (9) | |
| VVS | 205 (87) | 639 (73) | |
| Other | 4 (2) | 23 (3) | |
IQR interquartile range, POTS postural orthostatic tachycardia syndrome, SWE syncope with exertion, VVS vasovagal syncope
Outcome variables are described in Table 2, with signifcantly fewer unnecessary echocardiograms (15% vs 3%, p<0.001), rhythm monitors (8% vs 4%, p=0.009), and CXR (3% vs 0%, p<0.001) in the post-intervention cohort. The median number of total tests per patient decreased with the introduction of the guidelines (p = 0.015). The median number of unnecessary tests performed per patient was also significantly lower in the post-intervention cohort (p < 0.001). Guidelines were retroactively applied to the pre-intervention cohort to assess the percentage of patients who received necessary vs unnecessary testing. Upon direct comparison of the two cohorts, there was a significant increase in testing methodology in accordance with the guidelines in the post-intervention cohort (76% vs 93%, p < 0.001). The number of patients that required no additional cardiac testing beyond a current ECG increased from 55 to 66% (p = 0.002). Major cardiac testing charges, including appropriate and unnecessary testing, was significantly lower in the post-intervention cohort (interquartile range (IQR) $0, $1378 vs $0, $213; p = 0.005).
Table 2.
Descriptive outcome summary
| Variable | Pre-implementation cohort n = 237 | Post-implementation cohort n = 880 | p value |
|---|---|---|---|
|
| |||
| Unnecessary testing, n(%) | |||
| Echocardiogram | 35 (15) | 25 (3) | < 0.001 |
| Exercise testing | 4 (2) | 12 (1) | 0.76 |
| Rhythm testing | 18 (8) | 32 (4) | 0.009 |
| Chest X-ray | 8 (3) | 2 (0) | < 0.001 |
| No additional testing | 130 (55) | 580 (66) | 0.002 |
| Total number of unnecessary tests per patient per visit | |||
| Median (IQR) | 0 (0, 0) | 0 (0, 0) | < 0.001 |
| Range | 0, 4 | 0, 2 | |
| Total number of tests per patient per visit | |||
| Median (IQR) | 1 (1, 2) | 1 (1, 2) | 0.015 |
| Range | 0, 7 | 0, 5 | |
| Cardiology testing within guidelines, n(%) | 180 (76) | 821 (93) | < 0.001 |
| Major testing charge per patient per visit (dollars) | |||
| Median (IQR) | 0 (0, 1378) | 0 (0, 213) | 0.004 |
| Range | 0, 2171 | 0, 2044 | |
IQR interquartile range
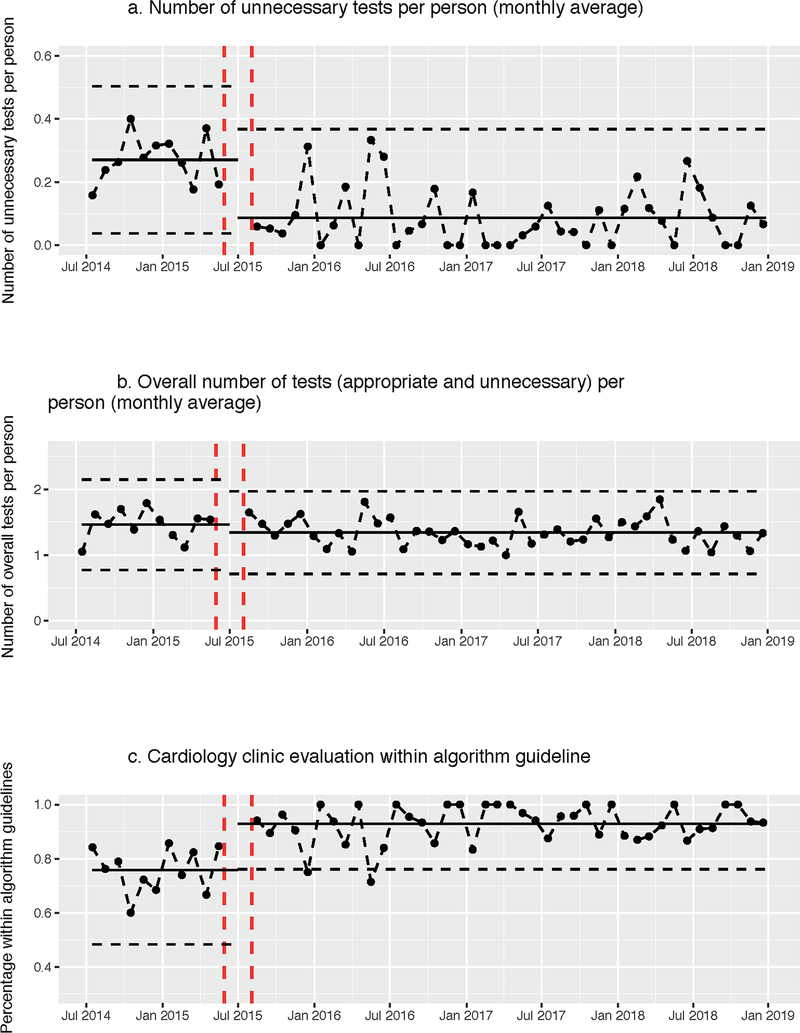
Results from segmented regression analyses are summarized in Table 3, with data displayed in statistical process control charts in Fig. 3. As a result of the intervention there was an immediate significant decrease in unnecessary testing (OR 0.3; 95% CI 0.14, 0.65; p = 0.002; Fig. 3a), after adjusting for age, gender, and diagnosis. In the pre-intervention period, the testing rate was stable (OR 0.82; 95% CI 1.02, 1.11; p = 0.57); after the 70% reduction in the unnecessary testing, the post-intervention testing rate was sustained at the reduced rate over time (OR 0.97; 95% CI 0.89, 1.05; p = 0.41). However, there was no significant change in necessary testing (Fig. 3b). Odds of appropriate use of cardiac testing in accordance with the guidelines increased by 265% (OR 3.65; 95% CI 1.44, 9.17; p = 0.006; Fig. 3c) immediately upon intervention, and results were sustained over time. For all outcomes, models without adjusting for age, gender, and diagnosis gave similar results.
Table 3.
Results from segmented regression
| Variable | ORa (95% CI) | p valuea | ORb (95% CI) | p valueb |
|---|---|---|---|---|
|
| ||||
| Unnecessary echocardiogram testing | ||||
| Immediate intervention effect | 0.32 (0.09,1.12) | 0.07 | 0.30 (0.09,1.09) | 0.07 |
| Baseline trend before intervention | 0.92 (0.82,1.03) | 0.16 | 0.93 (0.83,1.04) | 0.22 |
| Trend after intervention | 1.08 (0.96,1.22) | 0.19 | 1.07 (0.95,1.21) | 0.26 |
| Unnecessary rhythm testing | ||||
| Immediate intervention effect | 0.48 (0.13,1.91) | 0.28 | 0.41 (0.11,1.71) | 0.21 |
| Baseline trend before intervention | 1.03 (0.89,1.21) | 0.67 | 1.05 (0.90,1.24) | 0.50 |
| Trend after intervention | 0.95 (0.81,1.11) | 0.55 | 0.93 (0.79,1.09) | 0.39 |
| Total number of unnecessary tests | ||||
| Study period-post | 0.32 (0.16,0.69) | 0.003 | 0.30 (0.14,0.65) | 0.002 |
| Baseline trend before intervention | 1.01 (0.93,1.09) | 0.82 | 1.02 (0.95,1.11) | 0.57 |
| Trend after intervention | 0.98 (0.91,1.06) | 0.67 | 0.97 (0.89,1.05) | 0.41 |
| Total number of tests by cardiology appointment | ||||
| Study period-Post | 0.93 (0.70,1.23) | 0.60 | 0.97 (0.74,1.30) | 0.86 |
| Baseline trend before intervention | 1.00 (0.97,1.04) | 0.89 | 0.99 (0.96,1.03) | 0.65 |
| Trend after intervention | 1.00 (0.96,1.03) | 0.80 | 1.01 (0.97,1.04) | 0.74 |
| Cardiology evaluation within guidelines | ||||
| Study period-Post | 3.01 (1.23,7.28) | 0.015 | 3.65 (1.44,9.17) | 0.006 |
| Baseline trend before intervention | 1.01 (0.92,1.11) | 0.83 | 0.99 (0.90,1.09) | 0.83 |
| Trend after intervention | 1.01 (0.91,1.11) | 0.90 | 1.03 (0.93,1.14) | 0.57 |
Without adjusting for covariates
Adjusting for age, sex, and diagnosis
Fig. 3.
Statistical process control charts of cardiac testing outcomes during the study period. First vertical dashed lines represent implementation of guidelines and second vertical dashed lines represent the end of the washout period. Solid horizontal line is the overall mean (central line), estimated as the mean of monthly average (dots). Dashed horizontal lines represents the upper and lower control limits, calculated as overall mean ± 3 standard deviations. This is done separately for the pre- and post-intervention period
Balance measures demonstrated no significant difference between cohorts in patients suffering cardiac arrest, needing to be hospitalized for syncope, loop recorder or pacemaker implantation, or patients undergoing invasive electrophysiologic study/intervention after initial evaluation for syncope (Table 4). ED visits after initial cardiology evaluation were significantly decreased in the post-intervention cohort (1–2 ED visits: 8% vs 4%, p = 0.032; 3 + ED visits: 2% vs 0.3%, p = 0.04).
Table 4.
Descriptive summary of balance measures
| Variable | Pre-implementation cohort n = 237 | Post-implementation cohort n = 880 | p value |
|---|---|---|---|
|
| |||
| Cardiac arrest | 1 (0.4%) | 1 (0.1%) | 0.32a |
| Hospitalized for syncope | 3 (1.3%) | 5 (0.6%) | 0.38a |
| Loop recorder implanted | 2 (0.8%) | 5 (0.6%) | 0.64a |
| Pacemaker implanted | 0 (0%) | 1 (0.1%) | 1.00a |
| 1–2 ED visits for syncope | 18 (7.6%) | 37 (4.2%) | 0.032b |
| 3 + ED visits for syncope | 4 (1.7%) | 3 (0.3%) | 0.040a |
| Electrophysiology study/intervention | 1 (0.4%) | 12 (1.4%) | 0.32a |
ED emergency department
Fisher’s exact test
Chi-squared test
Two patients were initially diagnosed with VVS but were subsequently diagnosed with underlying heart disease following cardiac events. Of these two patients, one was from the pre-intervention cohort and received no additional testing following cardiology evaluation for a syncopal event but was subsequently found to have anomalous left coronary artery after cardiac arrest (successfully resuscitated). The other patient was from the post-intervention cohort and initially underwent Holter monitoring, which did not demonstrate any significant arrhythmias; however, the patient subsequently developed ventricular tachycardia with cardiac arrest (successfully resuscitated). Following introduction of these guidelines and based on abnormal exam, history or ECG findings, twelve patients underwent appropriate cardiac testing beyond an ECG and the following cardiac diagnoses were identified or confirmed: atrioventricular node reentrant tachycardia (5 patients), Wolff-Parkinson White syndrome (3), supraventricular tachycardia (2), ventricular tachycardia (1, described above), and myocarditis (1). In the pre-intervention cohort, only one patient was found to have a cardiac diagnosis (anomalous left coronary artery as described above).
Discussion
Patients being evaluated for syncope commonly undergo additional testing before and after referral to a pediatric cardiologist even when their symptoms strongly suggest a vasovagal etiology. This is likely due to fears of missing an underlying, life-threatening, cardiac disorder even when this possibility seems unlikely based upon a reassuring history, physical examination and ECG. The medical literature demonstrates that appropriately screening patients can eliminate the need for a large number of costly and time-consuming diagnostic tests [3, 10, 13, 14]. Our find ings demonstrate that implementation of guidelines for cardiac testing in syncopal patients resulted in a significant decrease in the overall number of unnecessary diagnostic tests without increasing adverse events.
Algorithm-driven evaluation of pediatric patients with syncope has been shown to appropriately identify high-risk patients [3, 4, 13]. Based on protocol-driven testing, twelve patients were diagnosed with underlying cardiac abnormalities. Eleven of these patients underwent electrophysiologic studies with ablations for abnormal rhythms. We can only speculate as to whether the arrhythmias identified and ablated contributed to the syncopal events as none of these patients had rhythm monitoring in place during syncopal events. None of these patients has had subsequent documented episodes of syncope. One patient with myocarditis required no further interventions. Loop recorders were implanted infrequently in both cohorts, and none revealed abnormal findings.
A decrease in testing did not correspond with an increase in adverse events. There were no cardiac-related mortalities in either group. There were two aborted cardiac arrests (1 pre-intervention; 1 post-intervention) and both patients survived. Hospitalizations for syncope were uncommon both before and after the implementation of these guidelines.
Standardized care pathways for management of pediatric diseases have been shown to reduce resource utilization. For example, a standardized clinical assessment and management plan for pediatric chest pain demonstrated a significant reduction in use of resources not recommended by management plans and consequently a substantial impact on the cost of care [15]. However, little information is available on the impact of similar protocols for pediatric syncope on resource utilization. Phelps et al. (2016) found that a clinical practice guideline helped safely manage syncopal patients, but there was no change to cost or resource utilization [4].
Similar to other studies, we found pediatric cardiologists amenable to following syncope testing guidelines with high compliance as demonstrated by additional diagnostic tests meeting high-risk criteria 93% of the time, with compliance sustained over time. Compliance was likely maintained through quarterly reports regarding testing in accordance with the guidelines provided to each pediatric cardiologist within our institution. Our results demonstrate that compliance to the guidelines significantly reduced unnecessary testing and associated charges, constituting an important impact on resource utilization. The percentage of unnecessary testing (echo, exercise testing, rhythm testing, or CXR) between pre- and post-intervention cohorts was lower in all categories, and there was a significant increase in patients undergoing no additional cardiac testing. If pre-intervention testing percentages had remained the same in the post-intervention cohort, an estimated 207 additional unnecessary tests would have been performed, reflecting an estimated $169,700 in patient charges and placing a significant burden on patients and the healthcare system.
Patient and parental education provided by pediatric cardiologists was an important aspect of this quality improvement initiative and likely had an impact on the successful implementation of these guidelines. Parental expectation has been shown to adversely influence provider prescribing practices [16, 17] and undoubtedly affects the decision making for many providers when evaluating children with pre-syncope or syncope. Fortunately, the education of patients and parents has been shown to reduce unnecessary prescription of antibiotics while preserving parental satisfaction [18]. The observed reduction in unnecessary testing in our patient population was likely due in part to providing patients and parents with a customized water bottle and educational brochure.
Similarly, parental education efforts during outpatient visits has likely contributed to a reduction in emergency department visits in children with asthma [19], seizures [20], and non-urgent medical concerns [21]. Focusing on patient and parental education in cardiology clinic visits likewise may have contributed to a significant decrease in ED utilization for syncope in post-intervention patients.
The cost of medical care in the United States results in a significant financial burden for many patients and families. Furthermore, medical expenses in the United States constitute a greater percentage of gross domestic product than any other country in the world. As a result, there is a growing need to reduce the costs of healthcare without sacrificing quality or patient outcomes. Our results demonstrate a significant decrease in the charges resulting from the evaluation of pediatric patients undergoing evaluation for pre-syncope or syncope without an increase in missed diagnoses. Adoption of these guidelines by primary care providers has the potential to decrease referrals to pediatric cardiologists and further reduce the cost associated with evaluating patients with these common symptoms.
Limitations
Limitations inherent to a single-center quality improvement project are present, such as the sequential nature of pre- and post-protocol cohorts and the ability to generalize to other institutions. Follow-up ED visits and events data are limited by utilizing chart review and the potential for patients being lost to follow-up within our system. Concomitant, non-cardiac disorders are not accounted for in this study. The ability to calculate a true decrease in cost is limited by the fact that charge values were applied to tests performed instead of analyzing actual charge data.
Conclusion
We describe the implementation of pediatric syncope testing guidelines used to educate providers and families and to decrease unnecessary testing. We were able to achieve a high level of provider compliance to the guidelines and found a significant decrease in overall unnecessary testing and estimated charges, without an increase in adverse events. Management pathways are beneficial in optimizing resource utilization in this clinical setting.
Acknowledgments
Funding Statistical support through the University of Utah Study Design and Biostatistics Center for this investigation was supported by the University of Utah Population Health Research (PHR) Foundation, with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1TR002538 (formerly 5UL1TR001067-05, 8UL1TR000105 and UL1RR025764).
Abbreviations
- ECG
Electrocardiogram
- CXR
Chest x-ray
- ED
Emergency department
- VVS
Vasovagal syncope
- SD
Standard deviation
- IQR
Interquartile range
- OR
Odds ratio
- CI
Confidence interval
Footnotes
Conflict of interest All the authors declared that they have no conflict of interest.
Data Availability De-identified patient data have been retained to verify all reports within this manuscript.
Compliance with Ethical Standards
Ethical Approval This quality improvement study was approved and provided exempt status by the University of Utah Institutional Review Board (IRB_00126778) and Primary Children’s Hospital Privacy Board.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affliations.
References
- 1.Lewis DA, Dhala A (1999) Syncope in the pediatric patient. The cardiologist’s perspective. Pediatr Clin N Am 46:205–219 [DOI] [PubMed] [Google Scholar]
- 2.Sapin SO (2004) Autonomic syncope in pediatrics: a practice-oriented approach to classification, pathophysiology, diagnosis, and management. Clin Pediatr 43:17–23 [DOI] [PubMed] [Google Scholar]
- 3.Zhang Q, Du J, Wang C et al. (2009) The diagnostic protocol in children and adolescents with syncope: a multi-centre prospective study. Acta Paediatr 98:879–884 [DOI] [PubMed] [Google Scholar]
- 4.Phelps H, Sachdeva R, Mahle W et al. (2016) Syncope best practices: a syncope clinical practice guideline to improve quality. Congenit Heart Dis 11:230–238 [DOI] [PubMed] [Google Scholar]
- 5.Johnson ER, Etheridge SP, Minich LL et al. (2014) Practice variation and resource use in the evaluation of pediatric vasovagal syncope: are pediatric cardiologists over-testing? Pediatr Cardiol 35:753–758 [DOI] [PubMed] [Google Scholar]
- 6.Bagnall RD, Weintraub RG, Ingles J et al. (2016) A prospective study of sudden cardiac death among children and young adults. N Engl J Med 374:2441–2452 [DOI] [PubMed] [Google Scholar]
- 7.Zhang Q, Zhu L, Wang C et al. (2013) Value of history taking in children and adolescents with cardiac syncope. Cardiol Young 23:54–60 [DOI] [PubMed] [Google Scholar]
- 8.Anderson JB, Willis M, Lancaster H et al. (2016) The evaluation and management of pediatric syncope. Pediatr Neurol 55:6–13 [DOI] [PubMed] [Google Scholar]
- 9.Redd C, Thomas C, Willis M et al. (2017) Cost of unnecessary testing in the evaluation of pediatric syncope. Pediatr Cardiol 38:1115–1122 [DOI] [PubMed] [Google Scholar]
- 10.Ritter S, Tani LY, Etheridge SP et al. (2000) What is the yield of screening echocardiography in pediatric syncope? Pediatrics 105:E58. [DOI] [PubMed] [Google Scholar]
- 11.Steinberg LA, Knilans TK (2005) Syncope in children: diagnostic tests have a high cost and low yield. J Pediatr 146:355–358 [DOI] [PubMed] [Google Scholar]
- 12.Kuriachan V, Sheldon RS, Platonov M (2008) Evidence-based treatment for vasovagal syncope. Heart Rhythm 5:1609–1614 [DOI] [PubMed] [Google Scholar]
- 13.Paris Y, Toro-Salazar OH, Gauthier NS et al. (2016) Regional implementation of a pediatric cardiology syncope algorithm using standardized clinical assessment and management plans (SCAMPS) methodology. J Am Heart Assoc 5:e002931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tretter JT, Kavey RE (2013) Distinguishing cardiac syncope from vasovagal syncope in a referral population. J Pediatr 163:1618–1623 [DOI] [PubMed] [Google Scholar]
- 15.Verghese GR, Friedman KG, Rathod RH et al. (2012) Resource utilization reduction for evaluation of chest pain in pediatrics using a novel Standardized Clinical Assessment and Management Plan (SCAMP). J Am Heart Assoc. 10.1161/JAHA.111.000349 [DOI] [PMC free article] [PubMed]
- 16.Magione-Smith R, McGlynn EA, Elliott MN et al. (2001) Parent expectations for antibiotics, physician-parent communication, and satisfaction. Arch Pediatr Adolesc Med 155:800–806 [DOI] [PubMed] [Google Scholar]
- 17.Bauchner H, Pelton SI, Klein JO (1999) Parents, physicians, and antibiotic use. Pediatrics 103:395–401 [DOI] [PubMed] [Google Scholar]
- 18.Mangione-Smith R, Zhou C, Robinson JD et al. (2015) Communication practices and antibiotic use for acute respiratory tract infections in children. Ann Fam Med 13:221–227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coffman JM, Cabana MD, Halpin HA, Yelin EH (2008) Effects of asthma education on children’s use of acute care services: a meta-analysis. Pediatrics 121:575–586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anup D, Patel E (2017) Reduced emergency department utilization by patients with epilepsy using QI methodology. Pediatrics 139:e20152358. [DOI] [PubMed] [Google Scholar]
- 21.Yoffe SJ, Moore RW, Gibson JO et al. (2011) A reduction in emergency department use by children from a parent educational intervention. Fam Med 43:106–111 [PubMed] [Google Scholar]