Abstract
Purpose of Review
Nonalcoholic fatty liver disease (NAFLD) and type 2 diabetes mellitus (T2DM) are strongly associated. Both also associate with an increased risk of cardiovascular disease (CVD).
Recent Findings
Several studies have provided evidence that NAFLD could be an independent CVD risk factor. Given the strong association between NAFLD and T2DM, assessing the independent CV effect of these two conditions remains challenging. However, patients with T2DM and NAFLD exhibit higher risk of CVD compared with T2DM without NAFLD suggesting a potential synergistic increase of CV risk in patients with both T2DM and NAFLD supported by several shared pathophysiological pathways. Several anti-diabetic therapies have shown beneficial effect on both NAFLD and CVD.
Summary
Patients with T2DM and NAFLD should be considered at high risk of CVD and could benefit from more intensive CV prevention. Additional long-term follow-up is needed to demonstrate that the treatment of NAFLD effectively reduces the risk of CVD.
Keywords: Nonalcoholic fatty liver disease, Nonalcoholic steatohepatitis, Type 2 diabetes, Fibrosis, Cirrhosis, Cardiovascular disease, Insulin resistance, Metabolic syndrome
Introduction
Nonalcoholic fatty liver disease (NAFLD) has become a major public health concern, affecting approximately 30% of the adult population worldwide [1]. NAFLD encompasses a large spectrum of condition from simple hepatic steatosis (NAFL) to nonalcoholic steatohepatitis (NASH), which may progress towards liver fibrosis, cirrhosis, and increased risk of liver-related complications including end-stage liver disease, hepatocellular carcinoma, liver transplantation requirement, and liver-related mortality [2••]. Strong evidence indicates that the global burden of NAFLD expands beyond liver-related complications as it increases the risk of developing extra-hepatic complications such as cardio-metabolic diseases including type 2 diabetes mellitus (T2DM), dyslipidemia, metabolic syndrome, and cardiovascular diseases (CVD) [2–5]. Indeed, it is now established that the leading cause of death among patients with NAFLD is CVD [6].
CVDs such as ischemic heart disease and stroke are also major public health burdens as they are the leading causes of death globally. CVDs are responsible for approximately 17.9 million deaths annually, which represent 31% of all global deaths [7]. Hence, CV prevention and early detection and management of established cardiovascular risk factors (CVRF) including dyslipidemia, T2DM, and hypertension are crucial in public health policy.
T2DM has long been recognized as an independent CVRF and is a frequent finding in NAFLD. Approximately 60% of patients with T2DM have NAFLD [8, 9]. Indeed, macrovascular complications constitute the leading cause of death in patients with T2DM [10–12], and intensive glycemic control interventions have been demonstrated to reduce the risk of macrovascular complications compared with a less intensive strategy [13, 14]. Several studies have highlighted the strong interaction between NAFLD and T2DM and describe a complex bidirectional relationship. Indeed, the coexistence of these two conditions pejoratively affect the course and prognoses of both diseases, and T2DM is associated with higher risk of hepatocellular carcinoma [15–18]. Furthermore, patients with T2DM and NAFLD had higher risk of CVD compared with patients with T2DM alone. This suggests a potential synergistic increase of CV risk in patients affected by both conditions [19, 20].
In the current manuscript, we will review the evidence for the association between NAFLD and increased risk of CVD with a specific focus on patients with T2DM. The potential pathophysiological mechanisms linking NAFLD, T2DM, and CVD will be discussed. Finally, we will summarize the current knowledge regarding the effect of glucose-lowering therapies on both NAFLD and risk of CVD.
Increased Risk of CVD in Patients with NAFLD
Several studies have linked NAFLD with an increased risk of either subclinical atherosclerosis or CVD in different populations [21, 22]. A strong association between NAFLD and subclinical atherosclerosis, assessed using four surrogate markers including carotid artery intima-media thickness/plaques, arterial stiffness, coronary artery calcification, and endothelial dysfunction, has been reported by the meta-analysis performed by Zhou et al. In this systematic review and meta-analysis, which included 26 observational studies with a total of 85,395 participants and 29,493 NAFLD cases, subjects with NAFLD exhibited a significant independent association with subclinical atherosclerosis compared with the non-NAFLD group (odds ratio (OR), 1.60; 95% confidence interval, 1.45–1.78).
The meta-analysis performed by Targher et al., based upon 16 observational studies including 34,043 individuals and a median follow-up of 6.9 years, confirmed the strong association between NAFLD and incidence of CVD events [22]. This meta-analysis showed that the presence of NAFLD, as determined by liver biopsy or imaging, conferred an increased odds of fatal and/or non-fatal CVD events (random effects OR: 1.64, 95% CI 1.26 to 2.13).
Further studies, including patients with biopsy-proven NAFLD, showed that the severity of NAFLD, especially the stage of fibrosis, is associated with the incidence of CVD and CV mortality [23]. Interestingly, in a multinational cohort study of 458 patients with biopsy-confirmed advanced fibrosis (stage F3 and F4), patients with bridging fibrosis (F3) had predominantly non-hepatic cancers and vascular events, whereas patients with compensated cirrhosis had predominantly liver-related events over a mean follow-up of 5.5 years [24]. Likewise, Henson et al. reported in a smaller cohort of 286 patients with biopsy-proven NAFLD that advanced fibrosis on biopsy was a significant and independent predictor of incident CVD, even after considering traditional risk factors and CV risk scores [25]. Further support for a link between NAFLD and CVD comes from a large case-control study that had a longer follow-up of 18.6 years and included 603 biopsy-proven NAFLD patients who were free of CVD at baseline and were age-, sex-, and geographic area-matched with controls from Sweden. In this study, cases with NAFLD had an increased risk of CVD. However, individual histological parameters such as NASH or fibrosis stage were not associated with the risk of CVD in this study [26]. Another recent population-based case-control study, based upon records from European primary care databases, failed to identify a significant association with the incidence of stroke or acute myocardial infarction in cases with NAFLD [27]. However, the findings of this large retrospective study have been called into question due to potential bias including high risk of misclassification as NAFLD remains largely asymptomatic and underdiagnosed in the general population [28]. Hence, additional larger studies with well-characterized subjects with and without NAFLD and long-term follow-up are warranted to determine the precise impact of NAFLD and its histological features on CV risk.
Finally, Paik et al. have recently reported an increase in NAFLD-related deaths in the USA based upon data from the National Vital Statistics System between 2007 and 2016. Interestingly, CVD was the second leading specific cause of death among subjects with NAFLD [29].
Cardiovascular Risk in Patients with T2DM and NAFLD
T2DM patients are considered at higher risk for both the presence of NAFLD and more severe forms of NAFLD independent of other risk factors for advanced fibrosis such as age, hypertension, dyslipidemia, and familial history of NAFLD-related cirrhosis [2, 30]. Given the strong association between T2DM and both CVD and NAFLD, the question of whether the presence of NAFLD in patients with T2DM confers an additional risk of CVD is of high clinical relevance [31].
Most of the aforementioned studies highlighting the association between NAFLD and CVD included patients with NAFLD with and without T2DM. Statistical adjustment for the presence of T2DM and other CVRF performed in some studies suggests an independent association between NAFLD and CVD [25]. However, to properly and specifically assess the risk of CVD in patients with T2DM and NAFLD compared with those without NAFLD, dedicated studies performed in the T2DM population are needed.
Most studies that assess the association between CVD and NAFLD in T2DM patients implement a cross-sectional design and use imaging modalities such as abdominal ultrasound for the diagnosis of NAFLD [32–38]. These studies report conflicting findings regarding the association between NAFLD and CVD in patients with T2DM. In addition, a few cohort studies that included patients with diabetes have been reported. In a study of 337 subjects with a mean follow-up of 10.9 (± 5.2) years, Adams et al. reported an increased risk of death (hazard ratio 1.7, 95% confidence interval 1.04–2.7) in patients with T2DM and NAFLD. The most common cause of death among T2DM with NAFLD was malignancy followed by liver complications and heart disease as second leading causes of death, which each accounted for 19% of all deaths in patients with diabetes and NAFLD [39]. Another prospective case-control study performed by Targher et al. included 2103 patients with T2DM without CVD at baseline with a 5-year follow-up. In this study, NAFLD associated with a significantly increased risk of CVD after adjustment for other CVR, including age, sex, smoking history, diabetes duration, HbA1c, LDL-cholesterol, liver enzymes, and use of medications [40]. In line with these findings, a retrospective cohort study from a diabetes registry in Scotland, which included a large cohort of 134,368 patients with T2DM, showed that hospital records of patients with NAFLD were independently associated with an increased risk of incident CVD events and mortality over a mean follow-up of nearly 4.5 years [41]. Finally, the association between NAFLD and CVD in patients with diabetes was further confirmed by a meta-analysis of 11 studies that had enrolled a total of 8346 patients with diabetes. Within this pool, 3766 subjects had NAFLD diagnosed primarily by abdominal ultrasound, and 4580 were in the non-NAFLD group. Analysis of the pooled effects estimate showed that patients with diabetes and NAFLD had a doubled risk of CVD compared with patients with diabetes but without NAFLD [19].
All of these studies point toward an additional effect of NAFLD in patients with T2DM in long-term risk of CVD. However, whether advanced stages of NAFLD also associate with an increased risk of CVD in patients with T2DM needs to be determined. A preliminary cross-sectional study has shown that liver stiffness assessed using magnetic resonance elastography associates with surrogate markers of CVD such as coronary artery calcium score in patients with T2DM [42] and correlates with epicardial fat volume [43]. Additional cohort population studies are needed to confirm these findings.
The Potential Pathophysiological Mechanisms Linking NAFLD, T2DM, and CVD
Several shared pathophysiological pathways link NAFLD and T2DM to increased cardiovascular risk including pro-atherogenic lipid alteration, increase in thrombosis factors, insulin resistance, low-grade inflammation, and microbiome alteration (Fig. 1).
Fig. 1.
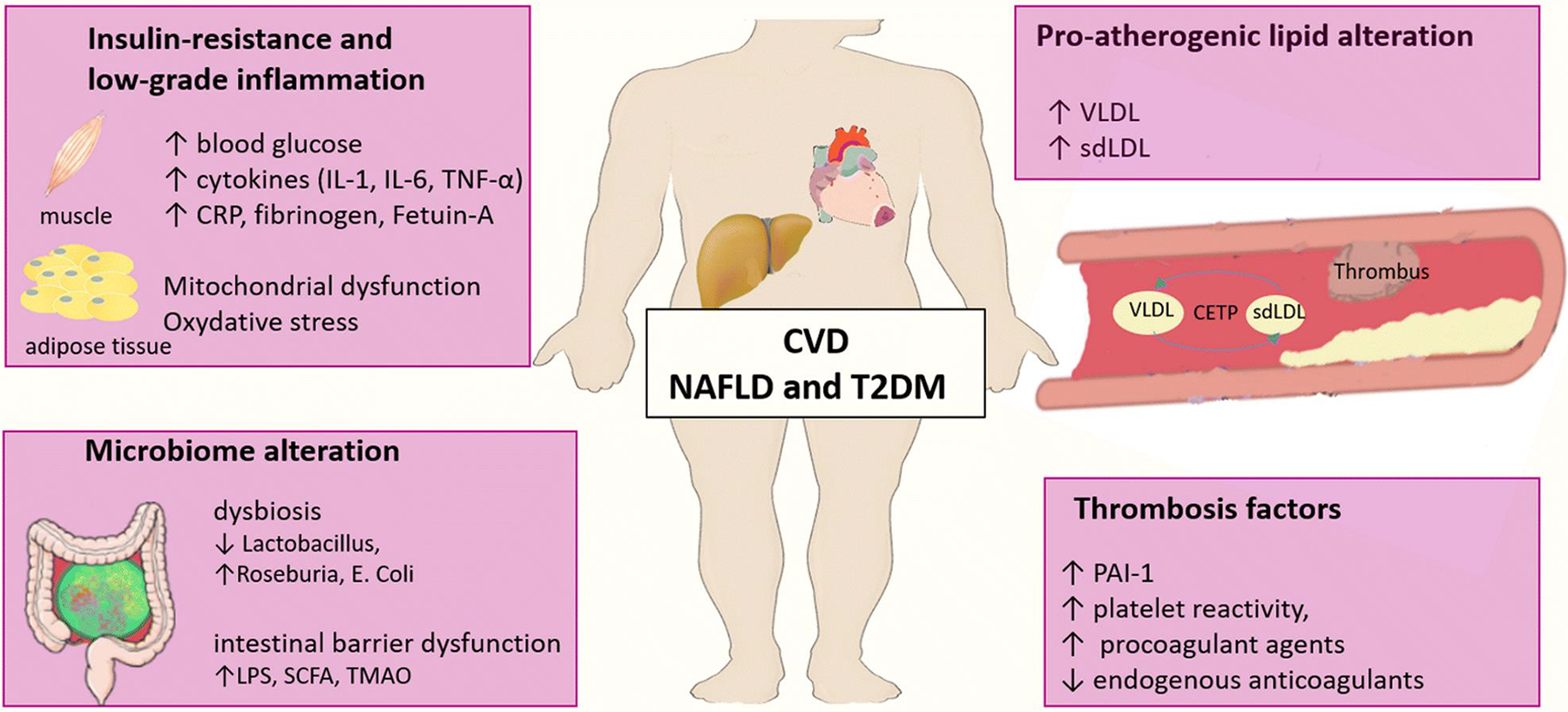
Potential pathophysiological mechanisms linking NAFLD, T2DM, and CVD. Several shared pathophysiological pathways link NAFLD and T2DM to an increased cardiovascular risk including pro-atherogenic lipid alteration, increase in thrombosis factors, insulin resistance, low-grade inflammation, and microbiome alteration.
Abbreviations: CRP: C-reactive protein, IL: interleukin, LPS: lipopolysaccharide, PAI-1: plasminogen activator inhibitor type 1, SCFA: short chain fatty acids, sdLDL: small dense low-densitylipoprotein, TMAO: trimethylamine N-oxide, TNF-α: tumor necrosis factor-α, VLDL: very low density lipoprotein
Pro-atherogenic Lipid Alteration
Dyslipidemia is a common risk factor for atherosclerosis. Individuals with NAFLD exhibit a specific lipid profile that is often associated with metabolic syndrome, insulin resistance, and T2DM, including elevated triglyceride-rich lipoproteins, low HDL-cholesterol, and increased proportion of circulating small-dense particles of LDL-cholesterol [44•]. Hepatic fat accumulation and insulin resistance lead to an increased production of triglyceride-rich particles such as very low density lipoproteins (VLDL). This increased level of plasma VLDL induces an increase in cholesteryl ester transfer protein (CETP) activity. The CETP is a key enzyme that mediates the reciprocal exchange between triacylglycerols from VLDL particles and cholesteryl esters from LDL and HDL particles in circulation. This will lead to an increase in triacylglycerol content of HDL and LDL particles. These triacylglycerols will be further hydrolyzed by hepatic lipase resulting in small and dense HDL and LDL particles [45]. Small dense LDL particles have been long identified as highly atherogenic [46], whereas epidemiological genetic studies have demonstrated that the level of plasma triacylglycerols causally contributes to the risk of CVD, especially coronary artery disease [47].
Thrombosis Factors
The rupture of unstable atherosclerotic plaques and subsequent thrombosis is responsible for acute ischemic events. The liver is a key organ for production of coagulation and fibrinolytic factors such as plasminogen activator inhibitor type 1 (PAI-1), an inhibitor of the fibrinolytic pathway involved in the resolution of thrombus. Elevated PAI-1 is associated with thrombosis and atherosclerosis [48]. In addition, PAI-1 levels, which are mainly determined by the liver, are increased in the presence of NAFLD and thus may contribute to pro-thrombotic processes involved in CVD [49]. Likewise, T2DM is also a pro-thrombotic condition due to increased platelet reactivity, higher levels of procoagulant agents, and lower concentrations of endogenous anticoagulants. Hence, these alterations may confer additional risk for thrombosis in patient with both T2DM and NAFLD [50].
Insulin Resistance and Hyperglycemia
The accumulation of intrahepatic steatosis is associated with the accumulation of intrahepatic ceramides and diacylglycerols, which have been shown to inhibit insulin signaling and thus favoring hepatic insulin resistance [17]. Due to the increase of hepatic insulin resistance, the presence of NAFLD has a pejorative effect on glycemic control in patients with T2DM. Indeed, patients with T2DM and NAFLD usually require intensive anti-diabetic therapies in order to achieve an optimal glycemic control compared with patients with T2DM without NAFLD [51]. Suboptimal glycemic control could account for the increased risk of CVD in patients with T2DM and NAFLD. The causal role of hyperglycemia in the development of coronary artery disease in T2DM has been questioned as randomized control trials with significant plasma glucose lowering have reported mixed effects on cardiovascular protection. This could be due to short follow-up periods, lack of statistical power, or heterogeneous populations with T2DM. More recently, data from randomized clinical trials using anti-diabetic agents with longer follow-up or designed specifically to assess CV outcomes have reported CV benefits [13, 14, 52]. Conversely, epidemiological studies using Mendelian randomization have reported that a genetic predisposition to hyperglycemia is associated with an increased risk of coronary artery disease, suggesting a causal effect of [53]. Hyperglycemia may influence coronary artery disease through a direct effect on the structure of the arterial wall via promotion of monocyte/macrophage adhesion to the endothelium, enhancement of vascular smooth muscle cell proliferation, or induction of endothelial dysfunction and inflammatory macrophages [54].
Low-Grade Inflammation
NAFLD and T2DM are both associated with a systemic, low-grade inflammatory state that may promote atherosclerosis by secreting multiple cytokines (e.g., interleukin (IL)-1, IL-6, tumor necrosis factor-α (TNF-α), and acute phase proteins (C-reactive protein, fibrinogen, Fetuin-A) [55]. Indeed, hepatic fat accumulation induces endoplasmic reticulum stress, which activates multiple pro-inflammatory pathways such as the nuclear factor-kB (NF-kB) pathway and the mitogen-activated protein kinase (MAPK) pathway. In addition, hepatic steatosis induces mitochondrial dysfunction and subsequently oxidative stress. The precise role of this inflammatory status on the development of CVD is not clearly elucidated. Interestingly, the causal role of IL-1 in the pathogenesis of CVD was recently reported in a clinical trial. Indeed, the inhibition of IL-1β using a monoclonal antibody was associated with a reduction of recurrent CVD events independent of lipid lowering [56].
Microbiome Alteration
Over the last decade, gut dysbiosis has been repeatedly observed in metabolic diseases such as T2DM and NAFLD. Alterations in the gut microbiome have been reported across the whole spectrum of NAFLD [57–61]. Specific gut-microbiome signatures in NAFLD have been demonstrated to accurately detect the presence of advanced fibrosis or cirrhosis [59, 62, 63]. Interestingly, obesity, T2DM, and NAFLD share common gut-microbiome alterations such as a decrease in the abundance of Lactobacillus, increased abundance of Roseburia and E. Coli in both NAFLD and T2DM [60]. Finally, dysbiosis is also associated with CVD. Intestinal barrier dysfunction and gut-microbiome derived mediators could play potential roles in increasing the risk of CVD, as reviewed in reference [64]. Briefly, the potential pathophysiological mechanism involves increased intestinal permeability leading to circulating lipopolysaccharide (LPS). This in turn favors the release of pro-inflammatory cytokines and metabolites such as short chain fatty acids (SCFA) and trimethylamine N-oxide (TMAO) [65, 66]. The increase in TMAO may induce an endoplasmic reticulum stress or pro-inflammatory pathways, but its precise mechanism of action is not fully elucidated. Nevertheless, gut-microbiome derived metabolites including TMAO, SCFA, and LPS are potential important factors associated with CVD NAFLD and T2DM.
Anti-diabetic Drugs, Cardiovascular Benefit, and Potential Effect on NAFLD
Given the strong association between CVD and T2DM, anti-diabetic drugs are required to be at least neutral on CVD events. Hence, over the last decade, many glucose-lowering agents have been tested for their safety and/or efficacy on CV outcomes in T2DM. These CV outcome trials have highlighted the beneficial effect of several medications on CV events beyond glycemic control and led to significant modifications of treatment strategy for patients with T2DM [67]. In addition, T2DM and NAFLD share common pathophysiological mechanisms, including insulin resistance. Thus, the effects of anti-diabetic treatments on insulin resistance have logically been studied in patients with NAFLD with or without T2DM for the treatment of NAFLD. Here, we provide an overview of the main anti-diabetic agents that improve insulin resistance and their effects on CV outcomes in patients with T2DM as well as their potential effects on NAFLD (Table 1).
Table 1.
Potential effect of anti-diabetic agents on NAFLD and cardiovascular outcomes
| Glucose-lowering agent | NAFLD | CV outcomes | ||
|---|---|---|---|---|
| Hepatic steatosis | NASH | Liver fibrosis | ||
| Metformin | Neutral | Neutral | Neutral | Reduction/neutral |
| Meta-analysis [68, 69] | Several RCTs [70,71,72,73] | Meta-analyses [68, 69] | -UKPDS [14, 74]: ↓MI Design: metformin vs conventional dietary measures Population: newly diagnosed T2DM and overweight -HOME TRIAL [75]: ↓ macrovascular events Design: metformin vs placebo Population: T2DM patients with insulin -SPREAD-DIMCAD [76]: ↓ recurrent CV events Design: metformin vs glipizide Population: T2DM with CAD -Meta-analysis [77, 78]: neutral * * ↑ CV risk when metformin is combined with sulfonylurea |
|
| DPP-4 inhibitors | Neutral/improved | Unknown | Unknown | Neutral |
|
- Neutral [79]: MRI-PDFF Design: RCT Sitagliptin vs placebo Population: Pre-T2DM or T2DM with NAFLD - Improved [80]: ↓MRI-PDFF Design: RCT vildaglitin vs placebo Population: T2DM with NAFLD |
-SAVOR-TIMI 53 [81]: neutral* Design: RCT saxagliptin vs placebo Population: T2DM with high CV risk * ↑ Hospitalizations for HF in patients with history of HF -TECOS [82]: neutral Design: RCT sitagliptin vs placebo Population: T2DM with CVD -EXAMINE [83]: neutral* Design: RCT alogliptin vs placebo Population: T2DM with CVD * ↑ HF incidence in patients already symptomatic at baseline [84] -CARMELINA [85]: neutral Design: RCT linagliptin vs placebo Population: T2DM with high CV risk -Meta-analyses [86, 87]: neutral |
|||
| Pioglitazone | Improved | Improved | Neutral/improved | Reduction/THF |
| Several RCTs and meta-analysis [68] | Several RCTs and meta-analysis [88] | -Neutral Several RCTs and Meta-analysis [68] -Improved* in patients with advanced fibrosis (F3F4) Meta-analysis [88] |
- PROactive [89]: neutral * Design: RCT pioglitazone vs placebo Population: T2DM with high CV risk * ↓ all-cause mortality, nonfatal MI, and stroke (secondary endpoint) -IRIS trial 2016 [90]: ↓strokes or MI Design: RCT pioglitazone vs placebo Population: non-diabetic with history of stroke or TIA - Meta-analyses: ↓MACE [91], ↑ HF incidence ↓ MACE and MI* [87], ↑ HF incidence ↓ All-cause mortality, MI or stroke [92] |
|
| GLP-1 receptor agonist | Improved | Improved | Neutral | Reduction |
|
LEAN trial: ↓hepatic steatosis in liver biopsy [93], Design: RCT liraglutide vs placebo Population: overweight patients with NASH with or without T2DM |
- LEAN trial: resolution of definite NASH with no worsening of fibrosis [93] Design: RCT liraglutide vs placebo Population: overweight patients with NASH with or without T2DM - resolution of definite NASH with no worsening of fibrosis [94] Design: semaglutide vs placebo Population: patient with NASH and fibrosis F1, F2 or F3 with or without T2DM |
Neutral: [94] Design: semaglutide vs placebo Population: patient with NASH and fibrosis F1, F2 or F3 with or without T2DM |
-LEADER [95]: ↓ 3-point MACE Design: RCT liraglutide vs placebo Population: T2DM high CV risk -SUSTAIN6 [96]: neutral* Design: RCT semaglutide vs placebo Population: T2DM with high CV risk *↓composite endpoint (CV death , nonfatal MI, stroke) -REWIND [97]: ↓composite endpoint (non fatal MI, non fatal stroke, CV death) Design: RCT dulaglutide vs placebo Population: T2DM at high CV risk -ELIXA [98]: neutral MACE Design: RCT lixisenatide versus placebo Population: T2DM with CVD -EXSCEL [99]: neutral MACE Design: RCT exenatide vs placebo Population: T2DM with or without CVD -HARMONY [100]: ↓ 3-point MACE Design: RCT albiglutide vs placebo Population: T2DM and CVD -Meta-analyses: ↓MACE in secondary CV prevention [101•: ↓ MACE , ↓ HF [87] |
|
| SGLT2 inhibitors | Neutral/improved | Unknown | Unknown | Reduction |
|
-Improved [102]: ↓MRI-PDFF Design: RCT empaglifozin vs standard of care. Population: T2DM with NAFLD -Improved [103]: ↓ MRI-PDFF Design: RCT dapagliflozin vs placebo Population: T2DM -Neutral [104]: proton-magnetic resonance spectroscopy Design: RCT canagliflozin vs placebo Population: uncontrolled T2DM |
-EMPA-REG OUTCOME [105] ↓ MACE empagliflozin vs placebo T2DM patients at high CV risk -CANVAS [106]: ↓ composite endpoint (CV death, non-fatal MI, non-fatal stroke) canagliflozin vs placebo T2DM and high CV risk -DECLARE-TMI 58 [107]: ↓CV death and HF hospitalization Dapagliflozin vs placebo T2DM with and without CVD -DAPA HF [108]: ↓composite endpoint (CV death/hospitalization or urgent visit for HF) dapagliflozin 10 mg/d vs placebo T2DM and non-diabetic patients, with HFrEF -Meta-analyses [87, 101•, 109] ↓ MACE in patients with CVD ↓ hospitalization for HF |
|||
MACE major adverse cardiac events, CAD coronary artery disease, CVD cardiovascular disease, HF heart failure, HFrEF heart failure and reduced ejection fraction, MI myocardial infarction, MRI-PDFF magnetic resonance imaging proton-density fat fraction, RCT randomized control trial, TIA transient ischemic attack, T2DM type 2 diabetes mellitus
Metformin
Metformin is considered the first-line drug for the treatment of T2DM, because it effectively reduces HbA1c, is well-tolerated with a modest beneficial effect on body weight, and is highly cost-effective [67].
Effect on NAFLD
Several RCTs have investigated the effect of metformin on NAFLD. Overall, these RTCs failed to demonstrate significant improvement in hepatic steatosis, NASH, or liver fibrosis. Hence, metformin is not recommended for the treatment of patients with NAFLD [2, 3].
Effect on CVD
The beneficial effect of metformin in CV prevention remains debatable. The protective CV effect of metformin has been reported by the UK Prospective Diabetes Study (UKPDS) trial [74]. In this large RCT of 3867 newly diagnosed patients with T2DM, a subgroup of overweight patients with T2DM in the intensive therapy arm with metformin (n = 342) exhibited a 39% reduction in the risk of nonfatal myocardial infarction compared with a subgroup that underwent conventional dietary intervention (n = 411) [74]. The protective CV effect of metformin was further confirmed in the 10-year follow-up study [14]. Another RCT with shorter duration of follow-up (4.3 years) compared CV outcomes in metformin versus placebo in 390 patients with T2DM treated with insulin. Metformin was not associated with improvement of the primary endpoint (a composite endpoint of microvascular, macrovascular outcomes, and mortality) but showed a reduction in the risk of macrovascular events [75]. Although several observational studies have suggested a reduction of CV risk under metformin either in monotherapy or in combination with other oral anti-diabetic drugs, two meta-analyses failed to confirm the protective effect of metformin and raised concerns about an increased risk of CVD when metformin is added to sulfonylurea [77, 78]. The SPREAD-DIMCAD trial, which included 304 patients with T2DM and CAD, confirmed the protective CV effect of metformin. Patients treated with metformin exhibited a 46% risk reduction (p = 0.026) of recurrent cardiovascular events compared with patients treated with the sulfonylurea glipizide [76].
DPP-4 Inhibitors
Dipeptidyl peptidase-4 (DPP-4) degrades endogenous glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic peptide (GIP). DPP4 inhibitors indirectly promote GLP-1 and GIP action through a longer half-life, thus leading to insulin secretion from beta-cells and decreased secretion of glucagon from alpha-cells.
Effect on NAFLD
Few RCTs have investigated the effect of DPP-4 inhibitors mainly on hepatic steatosis. A study performed by Cui et al. demonstrated that sitagliptin was safe but was not better than placebo in reducing liver fat in patients with pre-diabetes or diabetes and NAFLD [79]. Macauley et al. have reported a significant decrease in hepatic steatosis in patients with T2DM treated with vildagliptin compared with placebo in a 6-month RCT [80]. However, whether DPP-4 inhibitors improve NASH or liver fibrosis is unknown.
Effect on CVD
Four RCTs have assessed CV safety using different DPP-4 inhibitors (saxagliptin [81], sitagliptin [82], alogliptin [83], and linagliptin [85]). All of these studies demonstrated a neutral effect on CV outcomes. Some concerns were raised about the risk of heart failure (HF) with saxagliptin in patients with history of congestive symptoms in the SAVOR-TIMI trial. However, post hoc analysis showed that this effect occurred in patients with pre-existing HF [110]. The neutral effect of DPP-4 inhibitor on CV outcomes was further confirmed by two meta-analyses [86, 87].
Pioglitazone
Pioglitazone is a peroxisome proliferator-activated receptors (PPAR)-gamma agonist. Pioglitazone decreases insulin resistance and lipotoxicity, especially in the liver, and increases lipid storage in subcutaneous adipose tissue.
Effect on NAFLD
Several RCTs have tested pioglitazone versus placebo in patients with biopsy-proven NASH and shown an improvement on both hepatic steatosis and NASH. This beneficial effect on NAFLD and NASH was confirmed in a meta-analysis performed by Musso et al. [68]. However, the effect of pioglitazone on liver fibrosis improvement is less clear, as contradictory results have been reported from RCTs [111]. Recently, a meta-analysis that included 8 RCTs showed that pioglitazone improved advanced liver fibrosis in patients with and without T2DM [88•]. Pioglitazone may be considered for use in patients with pre-diabetes and T2DM and with biopsy-proven NASH, according to American Association for the Study of Liver Diseases (AASLD) [2••] and European Association for the Study of Liver (EASL) [3] guidelines. However, the benefit-risk ratio needs to be considered, as pioglitazone is associated with weight gain, fluid retention, and increased risk of bone fracture.
Effect on CVD
The first CV outcome trial to assess pioglitazone versus placebo was the PROactive trial, which included patients with T2DM at high risk of CVD. Although the trial failed to demonstrate a beneficial effect of pioglitazone on the primary composite endpoint, it showed that the drug has a protective effect on secondary endpoints (all-cause mortality, nonfatal MI, and stroke): HR 0.84; 0.72–0.98, p = 0.027 [89]. Several additional RCTs showed a decrease in MI and stroke using pioglitazone, even in patients without diabetes [90]. A comprehensive meta-analysis performed by Zhu et al. also reported that pioglitazone decreased the risk of MACE and MI [87••]. However, several studies, including meta-analyses, also reported that pioglitazone increases the risk of HF [91, 92].
GLP-1 Receptor Agonist
GLP-1 is an incretin hormone secreted by intestinal L-cells at the post-prandial phase. GLP-1 receptor agonists (GLP-1-RA) target GLP-1 receptors expressed in various organs including pancreas, intestine, adipose tissue, and brain. GLP-1 regulates plasma glucose levels by stimulating glucose-dependent insulin secretion and inhibiting glucagon secretion. In addition, GLP-1 induces weight loss by reducing gastric-emptying time while enhancing satiety by activation of GLP-1 receptors in the hypothalamus.
Effect on NAFLD
The efficacy of GLP-1-RA in reducing serum liver enzymes and improving hepatic steatosis using imaging modalities has been reported in several studies [112•]. The LEAN trial further demonstrated a significant histological resolution of NASH without worsening of fibrosis in patients treated with liraglutide 1.8 mg daily versus placebo [93]. Very recently, Newsome and colleagues conducted a large randomized, placebo-controlled trial in patients with biopsy-proven NASH and stage 1–3 fibrosis. They randomized patients to 3 doses of subcutaneous semaglutide versus placebo and treated them for 72 weeks. The highest dose semaglutide group (0.4 mg sq daily) achieved a statistically significant reduction in NASH resolution rate versus placebo (59% versus 17%, p value <0.001). However, despite significant weight loss, no significant improvement in fibrosis was observed in the semaglutide arm versus placebo [94]. Combinatorial therapy approaches are being tried to examine the role of combinations of other drugs with semaglutide in inducing improvement in fibrosis [113].
Effect on CVD
GLP1-RAs are associated with significant reduction of CV risk. Indeed, several trials have demonstrated a beneficial effect on CV outcomes using different GLP1-RAs including liraglutide [95], semaglutide [96], liraglutide [97], and albiglutide [100]. The GLP1-RA class effect on the reduction of CV outcomes was also confirmed by 2 meta-analyses [87, 101]. These strong evidences of CV protection led to a modification in the consensus recommendation for glucose-lowering medications such that GLP1-RA are currently recommended in patients with T2DM and established CVD, regardless of their level of HbA1c [67].
SGLT2 Inhibitors
This class of anti-diabetic agents exert their glucose-lowering effects by inhibition of the sodium/glucose transport protein 2 (SGLT2) that accounts for about 90% of the glucose reabsorbed by the kidney.
Effect on NAFLD
Clinical studies have reported a reduction in plasma ALT levels driven by weight loss and glycemic control [112•]. A few RCT trials including small number of participants have reported a decrease in hepatic fat content using empagliflozin [102], dapagliflozin [103] but not with canagliflozin [104]. The effects on NASH or liver fibrosis remain unknown, as there are no RCTs investigating the effect of SGLT2 inhibitors in patients with biopsy-proven NAFLD.
Effect on CVD
SGLT2 inhibitors have consistently demonstrated a reduction in cardiovascular events in patients with T2DM in large randomized clinical trials using empagliflozin [105], canagliflozin [106], or dapagliflozin [107] versus placebo. Meta-analyses assessing the effect of SGLT2 inhibitors on CV outcomes suggest a class effect on the reduction of MACE and hospitalization for HF in patients with CVD but report no effect on MACE in patients without established atherosclerotic vascular disease [101•] [87••].
Conclusion
The data presented in the current review provide strong evidence of the association between NAFLD and an increased risk of CVD. Given the strong association between CVD, T2DM, and NAFLD, assessments of the individual impacts of T2DM and NAFLD and its advanced stages on the risk of CVD remain challenging. Longitudinal studies specifically designed to address this issue are warranted in the future. However, studies performed in patients with T2DM have shown that the coexistence of both diseases tend to increase the risk of CVD. Several common pathophysiological pathways support the potential synergistic effect of T2DM and NAFLD on CVD. This suggests that patients with both T2DM and NAFLD should be considered at high risk for CVD and could benefit from more intensive CV prevention efforts. Furthermore, several anti-diabetic therapies have shown beneficial effect on either or both NAFLD and CVD. These benefits need to be considered in the individualized management of patients with T2DM. Finally, studies with long-term follow-up are needed to demonstrate that the treatment of NAFLD effectively reduces the risk of CVD.
Funding
RL receives funding support from NIEHS (P42ES010337), NCATS (UL1TR001442), NIDDK (U01DK061734, R01DK106419, P30DK120515, R01DK121378, R01DK124318), NHLBI (P01HL147835), NIAAA (U01AA029019), and DOD PRCRP (W81XWH-18-2-0026).
Conflict of Interest
C.C received consultant fees from Gilead, NovoNordisk, AstraZeneca, received grant support from Gilead. A.A declares no conflict of interest. R.L serves as a consultant for Anylam/Regeneron, Amgen, Arrowhead Pharmaceuticals, AstraZeneca, Bristol-Myer Squibb, CohBar, Eli Lilly, Galmed, Gilead, Glympse bio, Inipharm, Intercept, Ionis, Janssen Inc., Madrigal, Metacrine, Inc., NGM Biopharmaceuticals, Novartis, Novo Nordisk, Pfizer, Sagimet, 89 bio, and Viking Therapeutics. In addition, his institution has received grant support from Allergan, Astrazeneca, Boehringer-Ingelheim, Bristol-Myers Squibb, Eli Lilly, Galectin Therapeutics, Galmed Pharmaceuticals, Genfit, Gilead, Intercept, Inventiva, Janssen, Madrigal Pharmaceuticals, Merck, NGM Biopharmaceuticals, Pfizer and Siemens. He is also co-founder of Liponexus, Inc.
Footnotes
This article is part of the Topical Collection on Macrovascular Complications in Diabetes
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 2.••.Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328–57. 10.1002/hep.29367 [DOI] [PubMed] [Google Scholar]; Most recent practice guideline for the management of NAFLD from AASLD.
- 3.••.European Association for the Study of the Liver. Electronic address eee, European Association for the Study of D, European Association for the Study of O. EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64(6):1388–402. 10.1016/j.jhep.2015.11.004 [DOI] [PubMed] [Google Scholar]; Most recent European practice guideline for the management of NAFLD.
- 4.Loomba R, Wong R, Fraysse J, Shreay S, Li S, Harrison S, et al. Nonalcoholic fatty liver disease progression rates to cirrhosis and progression of cirrhosis to decompensation and mortality: a real world analysis of Medicare data. Aliment Pharmacol Ther. 2020;51(11):1149–59. 10.1111/apt.15679. [DOI] [PubMed] [Google Scholar]
- 5.Long MT, Zhang X, Xu H, Liu CT, Corey KE, Chung RT, et al. Hepatic fibrosis associates with multiple cardiometabolic disease risk factors: the Framingham Heart Study. Hepatology. 2020. 10.1002/hep.31608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anstee QM, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol. 2013;10(6):330–44. 10.1038/nrgastro.2013.41. [DOI] [PubMed] [Google Scholar]
- 7.Collaborators GBDCoD. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736–88. 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Younossi ZM, Golabi P, de Avila L, Paik JM, Srishord M, Fukui N, et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: a systematic review and meta-analysis. J Hepatol. 2019;71(4):793–801. 10.1016/j.jhep.2019.06.021. [DOI] [PubMed] [Google Scholar]
- 9.Doycheva I, Cui J, Nguyen P, Costa EA, Hooker J, Hofflich H, et al. Non-invasive screening of diabetics in primary care for NAFLD and advanced fibrosis by MRI and MRE. Aliment Pharmacol Ther. 2016;43(1):83–95. 10.1111/apt.13405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Webster MWI, Scott RS. What cardiologists need to know about diabetes. Lancet. 1997;350:S23–S8. 10.1016/S0140-6736(97)90025-8. [DOI] [PubMed] [Google Scholar]
- 11.Kosiborod M, Gomes MB, Nicolucci A, Pocock S, Rathmann W, Shestakova MV, et al. Vascular complications in patients with type 2 diabetes: prevalence and associated factors in 38 countries (the DISCOVER study program). Cardiovasc Diabetol. 2018;17(1):150. 10.1186/s12933-018-0787-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rydén L, Grant PJ, Anker SD, Berne C, Cosentino F, Danchin N, et al. ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2013;34(39):3035–87. 10.1093/eurheartj/eht108. [DOI] [PubMed] [Google Scholar]
- 13.Hayward RA, Reaven PD, Wiitala WL, Bahn GD, Reda DJ, Ge L, et al. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;372(23):2197–206. 10.1056/NEJMoa1414266. [DOI] [PubMed] [Google Scholar]
- 14.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577–89. 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 15.McPherson S, Hardy T, Henderson E, Burt AD, Day CP, Anstee QM. Evidence of NAFLD progression from steatosis to fibrosingsteatohepatitis using paired biopsies: implications for prognosis and clinical management. J Hepatol. 2015;62(5):1148–55. 10.1016/j.jhep.2014.11.034. [DOI] [PubMed] [Google Scholar]
- 16.Wang P, Kang D, Cao W, Wang Y, Liu Z. Diabetes mellitus and risk of hepatocellular carcinoma: a systematic review and meta-analysis. Diabetes Metab Res Rev. 2012;28(2):109–22. 10.1002/dmrr.1291. [DOI] [PubMed] [Google Scholar]
- 17.Birkenfeld AL, Shulman GI. Nonalcoholic fatty liver disease, hepatic insulin resistance, and type 2 diabetes. Hepatology. 2014;59(2):713–23. 10.1002/hep.26672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Watt GP, De La Cerda I, Pan JJ, Fallon MB, Beretta L, Loomba R, et al. Elevated glycated hemoglobin is associated with liver fibrosis, as assessed by elastography, in a population-based study of Mexican Americans. Hepatol Commun. 2020;4(12):1793–801. 10.1002/hep4.1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhou YY, Zhou XD, Wu SJ, Hu XQ, Tang B, Poucke SV, et al. Synergistic increase in cardiovascular risk in diabetes mellitus with nonalcoholic fatty liver disease: a meta-analysis. Eur J Gastroenterol Hepatol. 2018;30(6):631–6. 10.1097/MEG.0000000000001075. [DOI] [PubMed] [Google Scholar]
- 20.•.Targher G, Lonardo A, Byrne CD. Nonalcoholic fatty liver disease and chronic vascular complications of diabetes mellitus. Nat Rev Endocrinol. 2018;14(2):99–114. 10.1038/nrendo.2017.173 [DOI] [PubMed] [Google Scholar]; Meta-analysis underlying the increase risk of CVD in T2DM patient with NAFLD compared to T2DM without NAFLD.
- 21.Zhou YY, Zhou XD, Wu SJ, Fan DH, Van Poucke S, Chen YP, et al. Nonalcoholic fatty liver disease contributes to subclinical atherosclerosis: a systematic review and meta-analysis. Hepatol Commun. 2018;2(4):376–92. 10.1002/hep4.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Targher G, Byrne CD, Lonardo A, Zoppini G, Barbui C. Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: a meta-analysis. J Hepatol. 2016;65(3):589–600. 10.1016/j.jhep.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 23.Taylor RS, Taylor RJ, Bayliss S, Hagstrom H, Nasr P, Schattenberg JM, et al. Association between fibrosis stage and outcomes of patients with nonalcoholic fatty liver disease: a systematic review and meta-analysis. Gastroenterology. 2020;158(6):1611–25 e12. 10.1053/j.gastro.2020.01.043. [DOI] [PubMed] [Google Scholar]
- 24.Vilar-Gomez E, Calzadilla-Bertot L, Wai-Sun Wong V, Castellanos M, Aller-de la Fuente R, Metwally M, et al. Fibrosis severity as a determinant of cause-specific mortality in patients with advanced nonalcoholic fatty liver disease: a multi-national cohort study. Gastroenterology. 2018;155(2):443–57 e17. 10.1053/j.gastro.2018.04.034. [DOI] [PubMed] [Google Scholar]
- 25.Henson JB, Simon TG, Kaplan A, Osganian S, Masia R, Corey KE. Advanced fibrosis is associated with incident cardiovascular disease in patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2020;51(7):728–36. 10.1111/apt.15660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hagstrom H, Nasr P, Ekstedt M, Hammar U, Stal P, Askling J, et al. Cardiovascular risk factors in non-alcoholic fatty liver disease. Liver Int. 2019;39(1):197–204. 10.1111/liv.13973. [DOI] [PubMed] [Google Scholar]
- 27.Alexander M, Loomis AK, van der Lei J, Duarte-Salles T, Prieto-Alhambra D, Ansell D, et al. Non-alcoholic fatty liver disease and risk of incident acute myocardial infarction and stroke: findings from matched cohort study of 18 million European adults. BMJ. 2019;367:l5367. 10.1136/bmj.l5367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Henson JB, Roden M, Targher G, Corey KE. Is nonalcoholic fatty liver disease not a risk factor for cardiovascular disease: not yet time for a change of heart. Hepatology. 2020;71(5):1867–9. 10.1002/hep.31156. [DOI] [PubMed] [Google Scholar]
- 29.Paik JM, Golabi P, Biswas R, Alqahtani S, Venkatesan C, Younossi ZM. Nonalcoholic fatty liver disease and alcoholic liver disease are major drivers of liver mortality in the United States. Hepatol Commun. 2020;4(6):890–903. 10.1002/hep4.1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Caussy C, Soni M, Cui J, Bettencourt R, Schork N, Chen CH, et al. Nonalcoholic fatty liver disease with cirrhosis increases familial risk for advanced fibrosis. J Clin Invest. 2017;127(7):2697–704. 10.1172/JCI93465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bazick J, Donithan M, Neuschwander-Tetri BA, Kleiner D, Brunt EM, Wilson L, et al. Clinical model for NASH and advanced fibrosis in adult patients with diabetes and NAFLD: guidelines for referral in NAFLD. Diabetes Care. 2015;38(7):1347–55. 10.2337/dc14-1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Agarwal AK, Jain V, Singla S, Baruah BP, Arya V, Yadav R, et al. Prevalence of non-alcoholic fatty liver disease and its correlation with coronary risk factors in patients with type 2 diabetes. J Assoc Physicians India. 2011;59:351–4. [PubMed] [Google Scholar]
- 33.Chan WK, Tan AT, Vethakkan SR, Tah PC, Vijayananthan A, Goh KL. Ultrasonography-diagnosed non-alcoholic fatty liver disease is not associated with prevalent ischemic heart disease among diabetics in a multiracial Asian hospital clinic population. Clin Res Hepatol Gastroenterol. 2014;38(3):284–91. 10.1016/j.clinre.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 34.Takeuchi Y, Ito H, Komatsu Y, Oshikiri K, Antoku S, Abe M, et al. Non-alcoholic fatty liver disease is an independent predictor for macroangiopathy in Japanese type 2 diabetic patients: a cross-sectional study. Intern Med. 2012;51(13):1667–75. 10.2169/internalmedicine.51.7307. [DOI] [PubMed] [Google Scholar]
- 35.Targher G, Bertolini L, Padovani R, Poli F, Scala L, Tessari R, et al. Increased prevalence of cardiovascular disease in Type 2 diabetic patients with non-alcoholic fatty liver disease. Diabet Med. 2006;23(4):403–9. 10.1111/j.1464-5491.2006.01817.x. [DOI] [PubMed] [Google Scholar]
- 36.Targher G, Bertolini L, Rodella S, Tessari R, Zenari L, Lippi G, et al. Nonalcoholic fatty liver disease is independently associated with an increased incidence of cardiovascular events in type 2 diabetic patients. Diabetes Care. 2007;30(8):2119–21. 10.2337/dc07-0349. [DOI] [PubMed] [Google Scholar]
- 37.Idilman IS, Akata D, Hazirolan T, Doganay Erdogan B, Aytemir K, Karcaaltincaba M. Nonalcoholic fatty liver disease is associated with significant coronary artery disease in type 2 diabetic patients: a computed tomography angiography study 2. J Diabetes. 2015;7(2):279–86. 10.1111/1753-0407.12172. [DOI] [PubMed] [Google Scholar]
- 38.Lu H, Zeng L, Liang B, Shu X, Xie D. High prevalence of coronary heart disease in type 2 diabetic patients with non-alcoholic fatty liver disease. Arch Med Res. 2009;40(7):571–5. 10.1016/j.arcmed.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 39.Adams LA, Harmsen S, St Sauver JL, Charatcharoenwitthaya P, Enders FB, Therneau T, et al. Nonalcoholic fatty liver disease increases risk of death among patients with diabetes: a community-based cohort study. Am J Gastroenterol. 2010;105(7):1567–73. 10.1038/ajg.2010.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Targher G, Bertolini L, Poli F, Rodella S, Scala L, Tessari R, et al. Nonalcoholic fatty liver disease and risk of future cardiovascular events among type 2 diabetic patients. Diabetes. 2005;54(12): 3541–6. 10.2337/diabetes.54.12.3541. [DOI] [PubMed] [Google Scholar]
- 41.Wild SH, Walker JJ, Morling JR, McAllister DA, Colhoun HM, Farran B, et al. Cardiovascular disease, cancer, and mortality among people with type 2 diabetes and alcoholic or nonalcoholic fatty liver disease hospital admission. Diabetes Care. 2018;41(2): 341–7. 10.2337/dc17-1590. [DOI] [PubMed] [Google Scholar]
- 42.Mangla N, Ajmera VH, Caussy C, Sirlin C, Brouha S, Bajwa-Dulai S, et al. Liver stiffness severity is associated with increased cardiovascular risk in patients with type 2 diabetes. Clin Gastroenterol Hepatol. 2020;18(3):744–6 e1. 10.1016/j.cgh.2019.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brouha SS, Nguyen P, Bettencourt R, Sirlin CB, Loomba R. Increased severity of liver fat content and liver fibrosis in non-alcoholic fatty liver disease correlate with epicardial fat volume in type 2 diabetes: a prospective study. Eur Radiol. 2018;28(4): 1345–55. 10.1007/s00330-017-5075-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.•.Brouwers M, Simons N, Stehouwer CDA, Isaacs A. Non-alcoholic fatty liver disease and cardiovascular disease: assessing the evidence for causality. Diabetologia. 2020;63(2):253–60. 10.1007/s00125-019-05024-3 [DOI] [PMC free article] [PubMed] [Google Scholar]; Recent review article of the pathophysiological link between NAFLD and CVD.
- 45.Adiels M, Olofsson SO, Taskinen MR, Boren J. Overproduction of very low-density lipoproteins is the hallmark of the dyslipidemia in the metabolic syndrome. Arterioscler Thromb Vasc Biol. 2008;28(7):1225–36. 10.1161/ATVBAHA.107.160192. [DOI] [PubMed] [Google Scholar]
- 46.Chapman MJ, Guerin M, Bruckert E. Atherogenic, dense low-density lipoproteins. Pathophysiology and new therapeutic approaches. Eur Heart J. 1998;19(Suppl A):A24–30. [PubMed] [Google Scholar]
- 47.Do R, Willer CJ, Schmidt EM, Sengupta S, Gao C, Peloso GM, et al. Common variants associated with plasma triglycerides and risk for coronary artery disease. Nat Genet. 2013;45(11):1345–52. 10.1038/ng.2795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vaughan DE. PAI-1 and atherothrombosis. J Thromb Haemost. 2005;3(8):1879–83. 10.1111/j.1538-7836.2005.01420.x. [DOI] [PubMed] [Google Scholar]
- 49.Alessi MC, Bastelica D, Mavri A, Morange P, Berthet B, Grino M, et al. Plasma PAI-1 levels are more strongly related to liver steatosis than to adipose tissue accumulation. Arterioscler Thromb Vasc Biol. 2003;23(7):1262–8. 10.1161/01.ATV.0000077401.36885.BB. [DOI] [PubMed] [Google Scholar]
- 50.Biondi-Zoccai GG, Abbate A, Liuzzo G, Biasucci LM. Atherothrombosis, inflammation, and diabetes. J Am Coll Cardiol. 2003;41(7):1071–7. 10.1016/s0735-1097(03)00088-3. [DOI] [PubMed] [Google Scholar]
- 51.Cusi K Treatment of patients with type 2 diabetes and non-alcoholic fatty liver disease: current approaches and future directions. Diabetologia. 2016;59(6):1112–20. 10.1007/s00125-016-3952-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gerstein HC, Miller ME, Ismail-Beigi F, Largay J, McDonald C, Lochnan HA, et al. Effects of intensive glycaemic control on ischaemic heart disease: analysis of data from the randomised, controlled ACCORD trial. Lancet. 2014;384(9958):1936–41. 10.1016/S0140-6736(14)60611-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Merino J, Leong A, Posner DC, Porneala B, Masana L, Dupuis J, et al. Genetically driven hyperglycemia increases risk of coronary artery disease separately from type 2 diabetes. Diabetes Care. 2017;40(5):687–93. 10.2337/dc16-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bornfeldt KE, Tabas I. Insulin resistance, hyperglycemia, and atherosclerosis. Cell Metab. 2011;14(5):575–85. 10.1016/j.cmet.2011.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Santos RD, Valenti L, Romeo S. Does nonalcoholic fatty liver disease cause cardiovascular disease? Current knowledge and gaps. Atherosclerosis. 2019;282:110–20. 10.1016/j.atherosclerosis.2019.01.029. [DOI] [PubMed] [Google Scholar]
- 56.Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377(12):1119–31. 10.1056/NEJMoa1707914. [DOI] [PubMed] [Google Scholar]
- 57.Betrapally NS, Gillevet PM, Bajaj JS. Changes in the intestinal microbiome and alcoholic and nonalcoholic liver diseases: causes or effects? Gastroenterology. 2016;150(8):1745–55 e3. 10.1053/j.gastro.2016.02.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Henao-Mejia J, Elinav E, Jin C, Hao L, Mehal WZ, Strowig T, et al. Inflammasome-mediated dysbiosis regulates progression of NAFLD and obesity. Nature. 2012;482(7384):179–85. 10.1038/nature10809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Loomba R, Seguritan V, Li W, Long T, Klitgord N, Bhatt A, et al. Gut microbiome-based metagenomic signature for non-invasive detection of advanced fibrosis in human nonalcoholic fatty liver disease. Cell Metab. 2017;25(5):1054–62 e5. 10.1016/j.cmet.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Aron-Wisnewsky J, Vigliotti C, Witjes J, Le P, Holleboom AG, Verheij J, et al. Gut microbiota and human NAFLD: disentangling microbial signatures from metabolic disorders. Nat Rev Gastroenterol Hepatol. 2020;17(5):279–97. 10.1038/s41575-020-0269-9. [DOI] [PubMed] [Google Scholar]
- 61.Aron-Wisnewsky J, Clement K. The gut microbiome, diet, and links to cardiometabolic and chronic disorders. Nat Rev Nephrol. 2016;12(3):169–81. 10.1038/nrneph.2015.191. [DOI] [PubMed] [Google Scholar]
- 62.Caussy C, Tripathi A, Humphrey G, Bassirian S, Singh S, Faulkner C, et al. A gut microbiome signature for cirrhosis due to nonalcoholic fatty liver disease. Nat Commun. 2019;10(1): 1406. 10.1038/s41467-019-09455-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Oh TG, Kim SM, Caussy C, Fu T, Guo J, Bassirian S, et al. A universal gut-microbiome-derived signature predicts cirrhosis. Cell Metab. 2020;32(5):901. 10.1016/j.cmet.2020.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tang WHW, Backhed F, Landmesser U, Hazen SL. Intestinal microbiota in cardiovascular health and disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019;73(16):2089–105. 10.1016/j.jacc.2019.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schiattarella GG, Sannino A, Toscano E, Giugliano G, Gargiulo G, Franzone A, et al. Gut microbe-generated metabolite trimethylamine-N-oxide as cardiovascular risk biomarker: a systematic review and dose-response meta-analysis. Eur Heart J. 2017;38(39):2948–56. 10.1093/eurheartj/ehx342. [DOI] [PubMed] [Google Scholar]
- 66.Qi J, You T, Li J, Pan T, Xiang L, Han Y, et al. Circulating trimethylamine N-oxide and the risk of cardiovascular diseases: a systematic review and meta-analysis of 11 prospective cohort studies. J Cell Mol Med. 2018;22(1):185–94. 10.1111/jcmm.13307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Buse JB, Wexler DJ, Tsapas A, Rossing P, Mingrone G, Mathieu C, et al. 2019 Update to: Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2020;43(2):487–93. 10.2337/dci19-0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Musso G, Cassader M, Rosina F Gambino R. Impact of current treatments on liver disease, glucose metabolism and cardiovascular risk in non-alcoholic fatty liver disease (NAFLD): a systematic review and meta-analysis of randomised trials. Diabetologia. 2012;55(4):885–904. 10.1007/s00125-011-2446-4. [DOI] [PubMed] [Google Scholar]
- 69.Li Y, Liu L, Wang B, Wang J, Chen D. Metformin in non-alcoholic fatty liver disease: a systematic review and meta-analysis. Biomed Rep. 2013;1(1):57–64. 10.3892/br.2012.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Uygun A, Kadayifci A, Isik AT, Ozgurtas T, Deveci S, Tuzun A, et al. Metformin in the treatment of patients with non-alcoholic steatohepatitis. Aliment Pharmacol Ther. 2004;19(5):537–44. 10.1111/j.1365-2036.2004.01888.x. [DOI] [PubMed] [Google Scholar]
- 71.Shields WW, Thompson KE, Grice GA, Harrison SA, Coyle WJ. The effect of metformin and standard therapy versus standard therapy alone in nondiabetic patients with insulin resistance and nonalcoholic steatohepatitis (NASH): a pilot trial. Ther Adv Gastroenterol. 2009;2(3):157–63. 10.1177/1756283X09105462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Haukeland JW, Konopski Z, Eggesbo HB, von Volkmann HL, Raschpichler G, Bjoro K, et al. Metformin in patients with non-alcoholic fatty liver disease: a randomized, controlled trial. Scand J Gastroenterol. 2009;44(7):853–60. 10.1080/00365520902845268. [DOI] [PubMed] [Google Scholar]
- 73.Lavine JE, Schwimmer JB, Van Natta ML, Molleston JP, Murray KF, Rosenthal P, et al. Effect of vitamin E or metformin for treatment of nonalcoholic fatty liver disease in children and adolescents: the TONIC randomized controlled trial. JAMA. 2011;305(16):1659–68. 10.1001/jama.2011.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.UK prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998;352(9131):854–65. [PubMed] [Google Scholar]
- 75.Kooy A, de Jager J, Lehert P, Bets D, Wulffele MG, Donker AJ, et al. Long-term effects of metformin on metabolism and micro-vascular and macrovascular disease in patients with type 2 diabetes mellitus. Arch Intern Med. 2009;169(6):616–25. 10.1001/archinternmed.2009.20. [DOI] [PubMed] [Google Scholar]
- 76.Hong J, Zhang Y, Lai S, Lv A, Su Q, Dong Y, et al. Effects of metformin versus glipizide on cardiovascular outcomes in patients with type 2 diabetes and coronary artery disease. Diabetes Care. 2013;36(5):1304–11. 10.2337/dc12-0719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Boussageon R, Supper I, Bejan-Angoulvant T, Kellou N, Cucherat M, Boissel JP, et al. Reappraisal of metformin efficacy in the treatment of type 2 diabetes: a meta-analysis of randomised controlled trials. PLoS Med. 2012;9(4):e1001204. 10.1371/journal.pmed.1001204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lamanna C, Monami M, Marchionni N, Mannucci E. Effect of metformin on cardiovascular events and mortality: a meta-analysis of randomized clinical trials. Diabetes Obes Metab. 2011;13(3): 221–8. 10.1111/j.1463-1326.2010.01349.x. [DOI] [PubMed] [Google Scholar]
- 79.Cui J, Philo L, Nguyen P, Hofflich H, Hernandez C, Bettencourt R, et al. Sitagliptin vs. placebo for non-alcoholic fatty liver disease: a randomized controlled trial. J Hepatol. 2016;65(2):369–76. 10.1016/j.jhep.2016.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Macauley M, Hollingsworth KG, Smith FE, Thelwall PE, Al-Mrabeh A, Schweizer A, et al. Effect of vildagliptin on hepatic steatosis. J Clin Endocrinol Metab. 2015;100(4):1578–85. 10.1210/jc.2014-3794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Scirica BM, Bhatt DL, Braunwald E, Steg PG, Davidson J, Hirshberg B, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013;369(14): 1317–26. 10.1056/NEJMoa1307684. [DOI] [PubMed] [Google Scholar]
- 82.Green JB, Bethel MA, Armstrong PW, Buse JB, Engel SS, Garg J, et al. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;373(3):232–42. 10.1056/NEJMoa1501352. [DOI] [PubMed] [Google Scholar]
- 83.Zannad F, Cannon CP, Cushman WC, Bakris GL, Menon V, Perez AT, et al. Heart failure and mortality outcomes in patients with type 2 diabetes taking alogliptin versus placebo in EXAMINE: a multicentre, randomised, double-blind trial. Lancet. 2015;385(9982):2067–76. 10.1016/S0140-6736(14)62225-X. [DOI] [PubMed] [Google Scholar]
- 84.Standl E, Schnell O. DPP-4 inhibitors and risk of heart failure EXAMINEd. Lancet. 2015;385(9982):2022–4. 10.1016/S0140-6736(15)60037-X. [DOI] [PubMed] [Google Scholar]
- 85.Rosenstock J, Perkovic V, Johansen OE, Cooper ME, Kahn SE, Marx N, et al. Effect of linagliptin vs placebo on major cardiovascular events in adults with type 2 diabetes and high cardiovascular and renal risk: the CARMELINA Randomized Clinical Trial. JAMA. 2019;321(1):69–79. 10.1001/jama.2018.18269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rehman MB, Tudrej BV, Soustre J, Buisson M, Archambault P, Pouchain D, et al. Efficacy and safety of DPP-4 inhibitors in patients with type 2 diabetes: meta-analysis of placebo-controlled randomized clinical trials. Diabetes Metab. 2017;43(1):48–58. 10.1016/j.diabet.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 87.••.Zhu J, Yu X, Zheng Y, Li J, Wang Y, Lin Y, et al. Association of glucose-lowering medications with cardiovascular outcomes: an umbrella review and evidence map. Lancet Diabetes Endocrinol. 2020;8(3):192–205. 10.1016/S2213-8587(19)30422-X [DOI] [PubMed] [Google Scholar]; Recent systematic review and meta-analysis of the anti-diabetic drugs and CV outcomes.
- 88.•.Musso G, Cassader M, Paschetta E, Gambino R. Thiazolidinediones and advanced liver fibrosis in nonalcoholic steatohepatitis: a meta-analysis. JAMA Intern Med. 2017;177(5): 633–40. 10.1001/jamainternmed.2016.9607 [DOI] [PMC free article] [PubMed] [Google Scholar]; Recent meta-analysis of the effect of thiazolidinediones on NASH-related advanced fibrosis.
- 89.Dormandy JA, Charbonnel B, Eckland DJ, Erdmann E, Massi-Benedetti M, Moules IK, et al. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet. 2005;366(9493):1279–89. 10.1016/S0140-6736(05)67528-9. [DOI] [PubMed] [Google Scholar]
- 90.Kernan WN, Viscoli CM, Furie KL, Young LH, Inzucchi SE, Gorman M, et al. Pioglitazone after ischemic stroke or transient ischemic attack. N Engl J Med. 2016;374(14):1321–31. 10.1056/NEJMoa1506930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Liao HW, Saver JL, Wu YL, Chen TH, Lee M, Ovbiagele B. Pioglitazone and cardiovascular outcomes in patients with insulin resistance, pre-diabetes and type 2 diabetes: a systematic review and meta-analysis. BMJ Open. 2017;7(1):e013927. 10.1136/bmjopen-2016-013927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lincoff AM, Wolski K, Nicholls SJ, Nissen SE. Pioglitazone and risk of cardiovascular events in patients with type 2 diabetes mellitus: a meta-analysis of randomized trials. JAMA. 2007;298(10):1180–8. 10.1001/jama.298.10.1180. [DOI] [PubMed] [Google Scholar]
- 93.Armstrong MJ, Gaunt P, Aithal GP, Barton D, Hull D, Parker R, et al. Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet. 2016;387(10019):679–90. 10.1016/S0140-6736(15)00803-X. [DOI] [PubMed] [Google Scholar]
- 94.Newsome PN, Buchholtz K, Cusi K, Linder M, Okanoue T, Ratziu V, et al. A placebo-controlled trial of subcutaneous semaglutide in nonalcoholic steatohepatitis. N Engl J Med. 2020. 10.1056/NEJMoa2028395. [DOI] [PubMed] [Google Scholar]
- 95.Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):311–22. 10.1056/NEJMoa1603827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jodar E, Leiter LA, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375(19):1834–44. 10.1056/NEJMoa1607141. [DOI] [PubMed] [Google Scholar]
- 97.Gerstein HC, Colhoun HM, Dagenais GR, Diaz R, Lakshmanan M, Pais P, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet. 2019;394(10193):121–30. 10.1016/S0140-6736(19)31149-3. [DOI] [PubMed] [Google Scholar]
- 98.Pfeffer MA, Claggett B, Diaz R, Dickstein K, Gerstein HC, Kober LV, et al. Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med. 2015;373(23):2247–57. 10.1056/NEJMoa1509225. [DOI] [PubMed] [Google Scholar]
- 99.Holman RR, Bethel MA, Hernandez AF. Once-weekly exenatide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2017;377(25):2502. 10.1056/NEJMc1714163. [DOI] [PubMed] [Google Scholar]
- 100.Hernandez AF, Green JB, Janmohamed S, D’Agostino RB Sr, Granger CB, Jones NP, et al. Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (Harmony Outcomes): a double-blind, randomised placebo-controlled trial. Lancet. 2018;392(10157):1519–29. 10.1016/S0140-6736(18)32261-X. [DOI] [PubMed] [Google Scholar]
- 101.•.Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Furtado RHM, et al. Comparison of the effects of glucagon-like peptide receptor agonists and sodium-glucose cotransporter 2 inhibitors for prevention of major adverse cardiovascular and renal outcomes in type 2 diabetes mellitus. Circulation. 2019;139(17):2022–31. 10.1161/CIRCULATIONAHA.118.038868 [DOI] [PubMed] [Google Scholar]; Recent meta-analysis of the CV outcomes of GLP-1-RA and SGLT2 inhibitors.
- 102.Kuchay MS, Krishan S, Mishra SK, Farooqui KJ, Singh MK, Wasir JS, et al. Effect of empagliflozin on liver fat in patients with type 2 diabetes and nonalcoholic fatty liver disease: a randomized controlled trial (E-LIFT Trial). Diabetes Care. 2018;41(8):1801–8. 10.2337/dc18-0165. [DOI] [PubMed] [Google Scholar]
- 103.Latva-Rasku A, Honka MJ, Kullberg J, Mononen N, Lehtimaki T, Saltevo J, et al. The SGLT2 Inhibitor dapagliflozin reduces liver fat but does not affect tissue insulin sensitivity: a randomized, double-blind, placebo-controlled study with 8-week treatment in type 2 diabetes patients. Diabetes Care. 2019;42(5):931–7. 10.2337/dc18-1569. [DOI] [PubMed] [Google Scholar]
- 104.Cusi K, Bril F, Barb D, Polidori D, Sha S, Ghosh A, et al. Effect of canagliflozin treatment on hepatic triglyceride content and glucose metabolism in patients with type 2 diabetes. Diabetes Obes Metab. 2019;21(4):812–21. 10.1111/dom.13584. [DOI] [PubMed] [Google Scholar]
- 105.Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28. 10.1056/NEJMoa1504720. [DOI] [PubMed] [Google Scholar]
- 106.Neal B, Perkovic V, Matthews DR. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(21):2099. 10.1056/NEJMc1712572. [DOI] [PubMed] [Google Scholar]
- 107.Wiviott SD, Raz I, Sabatine MS. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. Reply N Engl J Med. 2019;380(19): 1881–2. 10.1056/NEJMc1902837. [DOI] [PubMed] [Google Scholar]
- 108.McMurray JJV, Solomon SD, Inzucchi SE, Kober L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381(21): 1995–2008. 10.1056/NEJMoa1911303. [DOI] [PubMed] [Google Scholar]
- 109.Saad M, Mahmoud AN, Elgendy IY, Abuzaid A, Barakat AF, Elgendy AY, et al. Cardiovascular outcomes with sodium-glucose cotransporter-2 inhibitors in patients with type II diabetes mellitus: a meta-analysis of placebo-controlled randomized trials. Int J Cardiol. 2017;228:352–8. 10.1016/j.ijcard.2016.11.181. [DOI] [PubMed] [Google Scholar]
- 110.McGuire DK, Van de Werf F, Armstrong PW, Standl E, Koglin J, Green JB, et al. Association between sitagliptin use and heart failure hospitalization and related outcomes in type 2 diabetes mellitus: secondary analysis of a randomized clinical trial. JAMA Cardiol. 2016;1(2):126–35. 10.1001/jamacardio.2016.0103. [DOI] [PubMed] [Google Scholar]
- 111.Boettcher E, Csako G, Pucino F, Wesley R, Loomba R. Meta-analysis: pioglitazone improves liver histology and fibrosis in patients with non-alcoholic steatohepatitis. Aliment Pharmacol Ther. 2012;35(1):66–75. 10.1111/j.1365-2036.2011.04912.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.•.Mantovani A, Byrne CD, Scorletti E, Mantzoros CS, Targher G. Efficacy and safety of anti-hyperglycaemic drugs in patients with non-alcoholic fatty liver disease with or without diabetes: an updated systematic review of randomized controlled trials. Diabetes Metab. 2020;46(6):427–41. 10.1016/j.diabet.2019.12.007 [DOI] [PubMed] [Google Scholar]; Recent systematic review of the effect of anti-diabetic drug on NAFLD.
- 113.Dufour JF, Caussy C, Loomba R. Combination therapy for non-alcoholic steatohepatitis: rationale, opportunities and challenges. Gut. 2020;69(10):1877–84. 10.1136/gutjnl-2019-319104. [DOI] [PMC free article] [PubMed] [Google Scholar]


