Abstract
Biplanar open wedge high tibial osteotomy (OWHTO) has become common since the introduction of OWHTO-specific plates. However, the management of soft tissues, including skin, the pes anserinus, and the superficial medial collateral ligament (sMCL) release vary among surgeons. We introduce an OWHTO methodology that avoids pes incision and repair, uses bone substitute insertion into the opening gap and includes management of soft tissues to minimize complications. We adopted a reversed curved oblique incision to reduce the risk of saphenous nerve injury. We avoided pes incision, taking advantage of its posterior component force to allow it to function as a compressor of the ascending osteotomy site. The proximal component force of the pes provides compression between the bone substitute insertions and the proximal/distal cortices. This allows postoperative weight bearing to be distributed to the substitute, which may reduce the risk of implant failure. The sMCL is detached from the distal tibial attachment without cutting, enabling its return to its original position underneath the pes and to be repaired. This sMCL release with complete pes preservation may reduce the risk of deep infection or medial laxity during total knee arthroplasty conversion, and further reduce the risks of OWHTO.
Technique Video
This video shows the technique used for open-wedge high tibial osteotomy using the TriS plate, with preservation of the pes anserinus and insertion of bone substitutes. One of the authors has a consultancy agreement with Olympus Terumo Biomaterials, which produces the TriS plate. Herein, we demonstrate the surgical procedure on the left knee. Before starting surgery, two bone substitute wedges, posterior and anterior wedges, are cut from a block. Our routine exposure using a reversed curved oblique incision starts from the extension of the anteromedial portal. The torn medial meniscus is arthroscopically resected through an anterolateral portal and an anteromedial portal. After the reversed curved oblique incision is created, the pes anserinus is elevated using forceps, and its proximal border is incised. The pes anserinus is retracted, and the superficial medial collateral ligament is then completely detached from its tibial insertion. If the exposure is inadequate, the curved incision is extended to the portal to provide good visualization of the surgical field. The medial border of the patellar tendon is cut with an electrosurgical knife, and the ascending osteotomy line is drawn. A Cobb elevator is used to detach the popliteal muscle from the tibial posterior aspect to enable the safe insertion of a posterior radiolucent retractor. The oblique osteotomy is started at 4 cm from the joint line. The first K-wire is inserted from the point of intersection of the ascending and oblique osteotomy lines to just above the hinge. The hinge point is confirmed on the internally rotated tangential view to the proximal tibiofibular joint. One or two K-wires are added parallel to the first K-wire. The ascending osteotomy is cut with a micro-oscillating saw and a chisel. The medial cortex is cut with a micro-oscillating saw, and a chisel is inserted into the hinge. The posteromedial cortex is cut with a micro-reciprocating saw, and the posterior cortex is cut with a standard reciprocating saw. The posterior cortical cut is completed with a dedicated chisel. After stepwise opening using 3-5 chisels, the first spreader is inserted into the posterior gap and opened. A small pillow is put under the heel to achieve full knee extension. The anterior spreader is inserted, and the posterior wedge with the planned opening height is inserted to replace the first spreader. The anterior wedge is inserted, and the reflected medial collateral ligament is then returned to its original position beneath the pes anserinus and repaired. The plate is temporarily fixed with a K-wire to enable the confirmation of the appropriate plate position. The locking screws are inserted in sequence using the cannulation technique. A 2-cm incision is added for the insertion of the distal two monocortical screws, which are inserted and locked. This is the final fluoroscopic anteroposterior view.
Introduction
A biplanar version of open-wedge high tibial osteotomy (OWHTO) has become common since the introduction of some OWHTO-specific locking plates, such as TomoFix (TomoFix Medial High Tibial Plate; Synthes; Solothurn, Switzerland).1 Methods of management of soft tissues, including the skin incision, handling of the pes anserinus, and the need for release of the superficial medial collateral ligament (sMCL) remain controversial.
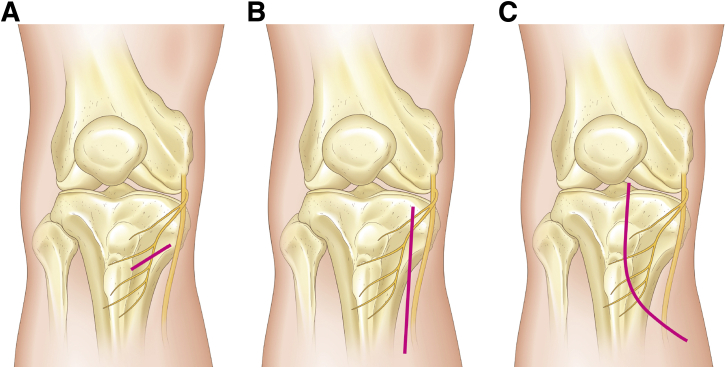
Although the original skin incision for the TomoFix plate1 was a small oblique incision (Fig 1A), Reischl et al.2 reported a higher rate of postoperative infection with an oblique incision compared with a longitudinal incision (Fig 1B), suggesting that a longitudinal incision may reduce the complications induced by excessive skin tension during surgical exposure, although it may increase the risk of saphenous nerve injury given its proximity to the proximal part of the nerve (Fig 1B). Modifications to the oblique or longitudinal incision would be required to avoid these complications.
Fig 1.
Skin incision. (A) A small oblique incision made parallel to the pes anserinus. Even with a nerve-sparing incision, increased skin tension during surgical exposure due to the limited view may increase the risk of skin necrosis or postoperative infection. (B) Longitudinal incision. Although adequate exposure is easily obtained, the more proximal aspect of the saphenous nerve is at risk for injury, especially when the incision is made on the more medial side. (C) Reversed curved oblique incision. Both the anterior and posterior parts of the osteotomy line are clearly visible. The risk of damage to the proximal saphenous nerve is reduced because only the peripheral nerve branches are vulnerable.
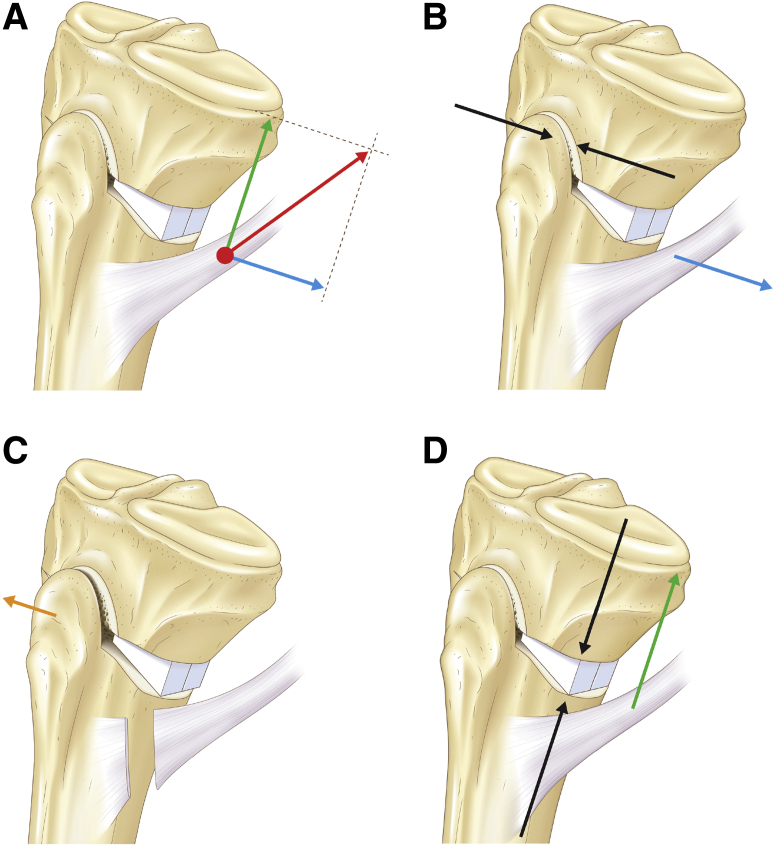
The pes anserinus, which is composed of the combined tendinous insertions of the sartorius, gracilis, and semitendinosus muscles, stabilizes the medial side of the knee.3 Accordingly, a pes-preserving OWHTO1,4,5 may have superior medial stability compared with OWHTO, which involves initial pes incision followed by repair. While some surgeons6, 7, 8, 9 prefer to incise the pes to provide better visualization of the osteotomy, the long-term effects of an incised-and-repaired pes on the OWHTO’s structure and/or biomechanics have not been clarified, making a better understanding of the role of the pes in OWHTO (Fig 2) critical.
Fig 2.
The possible function of the pes anserinus in open-wedge high tibial osteotomy. (A) The traction force of the pes anserinus (red arrow) can be separated into the two component forces: the posterior component (blue arrow) and the proximal component (green arrow). The ascending osteotomy is created as long as possible, with thickness of the basal portion ≥ 15 mm. (B) The posterior component force (blue arrow) compresses the ascending osteotomy site (black arrows), which can increase stability and promote bone union. (C) When the pes anserinus is cut during surgical exposure, in addition to the decreased compressive force, it can result in externally rotated displacement of the distal part of the osteotomy (orange arrow). (D) The proximal component force (green arrow) compresses and stabilizes the bone substitute-proximal/distal cortical interface (black arrows).
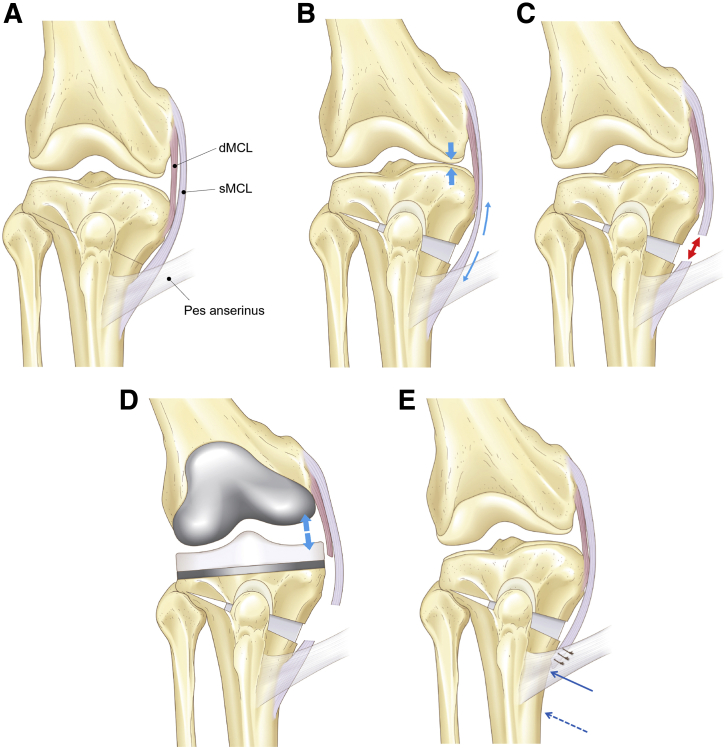
As the osteotomy line lies between the deep MCL (dMCL) and the sMCL, the opening procedure may potentially create increased tension of the sMCL (Fig 3, A and B), which may prevent the principal objective of OWHTO, i.e., decompression of the medial compartment. Agneskirchner et al.10 recommended the complete release of the sMCL to allow sufficient decompression (Fig 3C). Sato et al.11 reported that complete release of the sMCL did not cause postoperative valgus laxity after OWHTO, although a consensus is still lacking.
Fig 3.
The possible function of the medial collateral ligament (MCL) in open wedge high tibial osteotomy. (A) The relationship between the deep/superficial MCL (dMCL/sMCL), pes anserinus, and the osteotomy line (black line). The sMCL attaches 6–7 cm distal to the joint line across the osteotomy line and underneath the pes anserinus. (B) When the open-wedge high tibial osteotomy is performed without releasing the pes anserinus, the MCL is tightened (blue arrows), which can cause insufficient decompression of the medial compartment (blue bold arrows). (C) When the sMCL is dissected proximal to the pes, it cannot be repaired (red double-pointed arrow) despite adequate decompression. (D) As dMCL release is mandatory in total knee arthroplasty conversion, both the dMCL and sMCL lose their distal attachments when sMCL healing is incomplete. This situation induces medial laxity (blue bold arrows). (E) When the sMCL is released from its distal attachment, it can be repaired in a side-to-side manner underneath the pes anserinus. The distal end of the sMCL after the opening moves proximal (blue arrow) to its original attachment (dashed blue arrow).
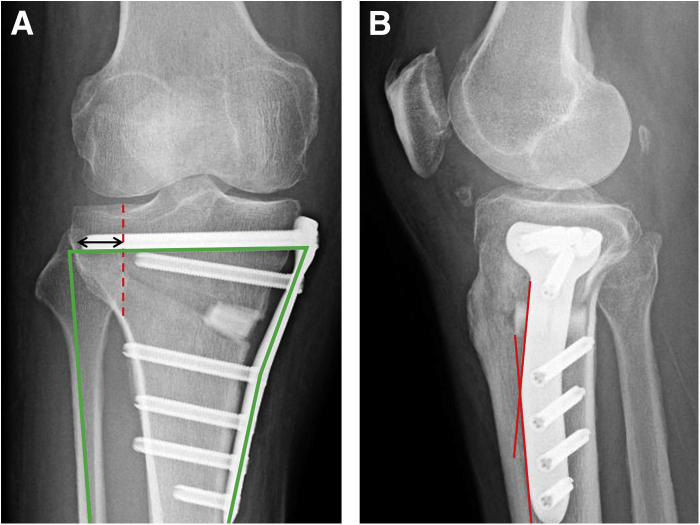
We have developed an OWHTO procedure that 1) addresses the skin tension and saphenous nerve vulnerability involved in making an incision, 2) avoids incision and repair of the pes, and 3) addresses the sMCL tension issues. We describe the pes-preserving OWHTO with bone substitute insertion using the TriS medial HTO plate (Olympus Terumo Biomaterials, Tokyo, Japan), which is placed in a more posteromedial position than the TomoFix (Fig 4).12 The pearls and pitfalls of this procedure are shown in Table 1.
Fig 4.
Characteristics of the TriS medial high tibial osteotomy (HTO) plate. (A) Anteroposterior postoperative radiograph of a 66-year-old male patient who underwent open wedge high tibial osteotomy (OWHTO) with a TriS medial HTO plate in his right knee. The anatomical plate design, which fits the posteromedial portion of the tibia after OWHTO, allows a sufficiently long screw while avoiding plate-head irritation. When the screw tip(s) can be inserted beyond the medial margin of the proximal tibiofibular joint (red dashed line and black double headed arrow), the arch comprising the locking plate, locking screws, and fibula (green outline) promotes the structural strength of the OWHTO. (B) Lateral view. The more posterior plate-head installation can accommodate the 15° shaft angle (red lines).
Table 1.
Pearls and Pitfalls of this Procedure
| Pearls |
| 1. Reversed curved oblique incision |
| - Both the anterior and posterior parts of the osteotomy line are clearly visible. |
| - This reduces the risk of the saphenous nerve injury. |
| 2. Pes preservation |
| - The posterior component force of the pes can increase stability and promote bone union. |
| - The compressive force between the bone substitute and the proximal/distal cortices can be applied by the proximal component of the contractile strength of the intact pes. |
| - The externally rotated displacement of the distal part of the osteotomy can be avoided in cases with an unstable lateral hinge fracture. |
| 3. Complete release of the sMCL from the distal attachment of the tibia |
| - The medial compartment can be adequately decompressed. |
| - The sMCL can be appropriately repaired by returning it to the original position underneath the pes. |
| Pitfalls |
| - There might be a risk of ischemia in cases with thin skin. |
| - It is relatively more difficult to gain a sufficient view with this osteotomy compared to the pes-incision technique. |
| - The possibility of medial laxity during total knee arthroplasty conversion may remain. |
sMCL, superficial medial collateral ligament.
Surgical Procedure (with Video Illustration)
Preoperative Planning and Preparation (Video 1)
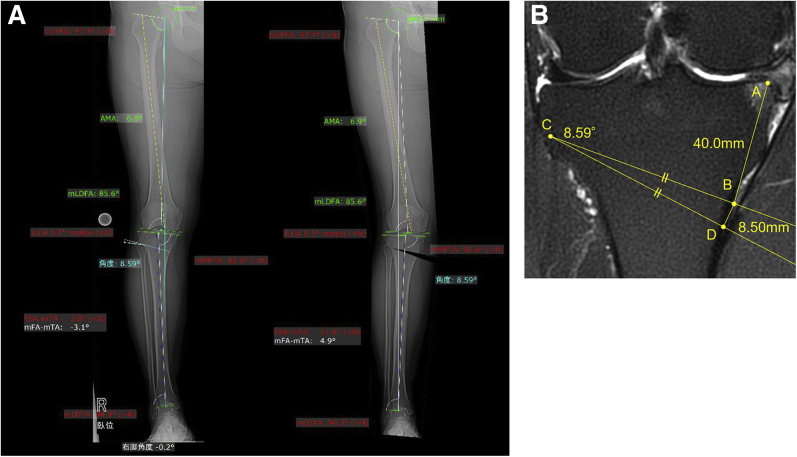
We aim the target postoperative weight-bearing line (WBL) to be 60%–70% in the WBL percentage.7 The correction angle is measured using the method of Miniaci et al.13 using supine frontal lower-extremity X-rays,14 with a digital surgical planning tool (mediCAD®, Hectec, Germany) (Fig 5A) for reference.15 The postoperative medial proximal tibial angle (MPTA)16 is estimated from the sum of the original MPTA and the correction angle. The correction angle is then transferred to the coronal MRI section at the tibia’s widest diameter (Fig 5B) to fine-tune the opening distance. We also need to account for the bone loss generated by the saw blade, a potential cause of undercorrection. As the bone loss in our OWHTO procedure using a micro-oscillating saw is approximately 1 mm, 1 mm is added to the opening distance calculated from the MRI measurement (Fig 5B).
Fig 5.
Preoperative planning. (A) Correction angle calculation with a digital planning tool (mediCAD) for a 61-year-old female patient prior to open-wedge high tibial osteotomy of the right knee. (B) The correction angle (8.59°) was transferred to the coronal MRI section at the tibia’s widest diameter. The starting point of the proximal oblique osteotomy (B), which is 40 mm distal to the medial edge of the medial plateau (A) and hinge point (C), is first plotted. An isosceles triangle B-C-D is then drawn with the apex angle equivalent to the correction angle. The bottom length B-D (8.5 mm plus 1 mm to account for the bone loss from the oscillating saw = 9.5 mm) corresponds to the opening distance.
As we use a bone substitute made of β-tricalcium phosphate (OSferion 60, Olympus Terumo Biomaterials, Tokyo, Japan), the posterior and anterior wedges are cut beforehand to fit the target gap. The operation is performed with the patient supine under general anesthesia. The opposite leg is placed lower than the operative leg to allow full visualization of the medial aspect of the knee.
Approach (Video 1)
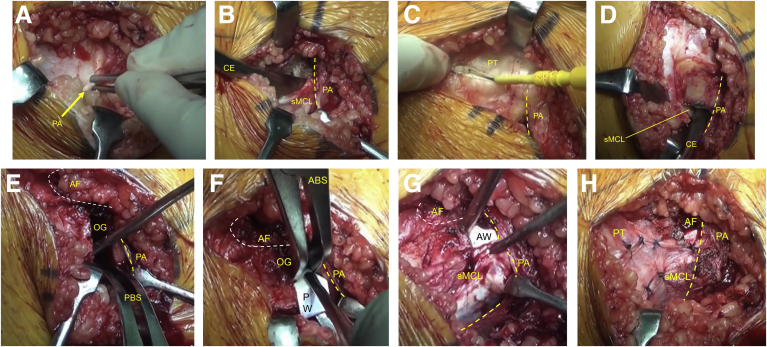
An initial arthroscopy is performed and any intraarticular pathology is addressed through the anterolateral and anteromedial portals. The medial aspect of the proximal tibia is exposed through a reversed curved oblique incision (Fig 1C).17 The pes anserinus is elevated using forceps to detect the proximal border (Fig 6A). Retracting the pes without cutting, the sMCL is then completely detached from its distal tibial insertion (Fig 6B). The medial border of the patellar tendon is cut (Fig 6C) and the ascending osteotomy line for the anterior flange is drawn with an electrosurgical knife. The flange requires a minimum thickness of 15 mm at its base (Fig 2A). We create a flange that is as long as possible to increase the contact area of the coronal plane osteotomy (Fig 2A). The angle between the ascending and oblique osteotomies is set to be approximately 100°. The knee is then flexed, and the popliteal muscle is detached from its tibial posterior aspect18 (Fig 6D), and a radiolucent retractor is inserted.
Fig 6.
Soft tissue management (medial side of the left knee is exposed.) (A) The pes anserinus (PA, yellow arrow) is elevated using forceps to detect the proximal border. (B) Incising the proximal border (yellow dashed line) of the PA without cutting the tendon, it is elevated by a muscle hook. The superficial layer of the medial collateral ligament (sMCL) is then completely detached from its distal tibial insertion using a Cobb elevator (CE). (C) The medial border of the patellar tendon (PT) is cut to prepare the ascending osteotomy. (D) The popliteal muscle is detached from the posterior tibia using the Cobb elevator. (E) After the ascending osteotomy for the anterior flange (AF; white dashed line) and the oblique osteotomy are completed, the PA and the sMCL are retracted distally and posteriorly, respectively. A posterior bone-spreader (PBS) is inserted into the posterior-most opening gap (OG) and opened to 6–7 mm. (F) An anterior bone-spreader (ABS) is then inserted into the anterior gap to maintain the appropriate opening gap (OG). A posterior wedge (PW) made of bone substitute is inserted to replace the first PBS. (G) The ABS is removed and replaced with the anterior wedge (AW), made of bone substitute. The reflected sMCL is then returned to its original position underneath the PA. (H) After the repair of the sMCL in a side-to-side manner, the OG is almost completely covered.
Osteotomy (Video 1)
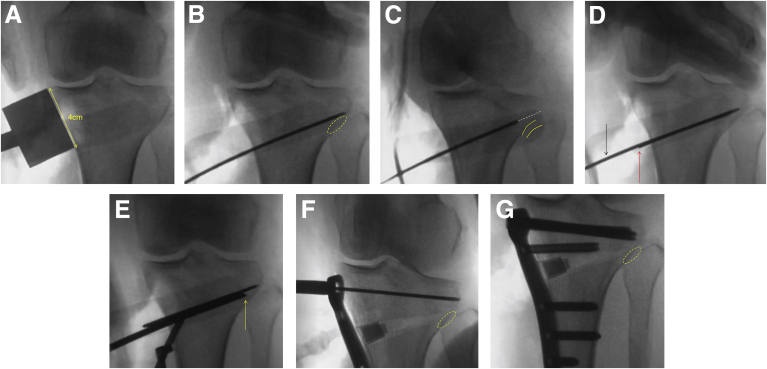
A biplanar OWHTO is performed under Kirschner wire (K-wire) guidance with the knee in extension. A small pillow beneath the knee is used to acquire a fluoroscopic view tangential to the joint surface (Fig 7A).
Fig 7.
Intraoperative fluoroscopic views of the left knee. (A) The entry point of the first K-wire is demonstrated using an original 4-cm gauge (yellow double-headed arrow). (B) The first K-wire is inserted slightly proximal to the level of the proximal tibiofibular joint (PTFJ; yellow dashed circle). (C) The K-wire position is confirmed by a tangential view to the PTFJ (50° internal rotation). A line extending from the K-wire (white dashed line) passes just above the PTFJ (yellow lines). (D) The second K-wire (black arrow) is inserted parallel to the first K-wire (red arrow). (E) The tip of the first chisel (yellow arrow) during the stepwise opening procedure by some chisels terminates at the hinge point, which is located just above the PTFJ and 5 mm medial to the lateral cortex. (F) Temporary fixation of the TriS medial HTO plate. The K-wire(s) for the proximal cannulated screw(s) should be superimposed upon the PTFJ (dashed yellow circle). (G) Final confirmation of the plate installation. The tips of the proximal screws are superimposed on the PTFJ (dashed yellow circle). K-wire, Kirschner wire.
The starting level for the oblique osteotomy is 4 cm distal to the joint line (Fig 7A). At the starting level, the first K-wire is inserted from the point of intersection of the planned ascending and oblique osteotomies up to the hinge point, which is lateral to the medial margin of the proximal tibiofibular joint (PTFJ) and just above the PTFJ (Fig 7B).19 After insertion of the first K-wire, its position is confirmed by a tangential view to the PTFJ (Fig 7C). One or two more K-wires are then added parallel to the first K-wire (Fig 7D). The ascending and oblique osteotomies are performed using a micro-oscillating saw, chisels, a micro-reciprocating saw, and a standard reciprocating saw.
Gap Opening and Plate Fixation (Video 1)
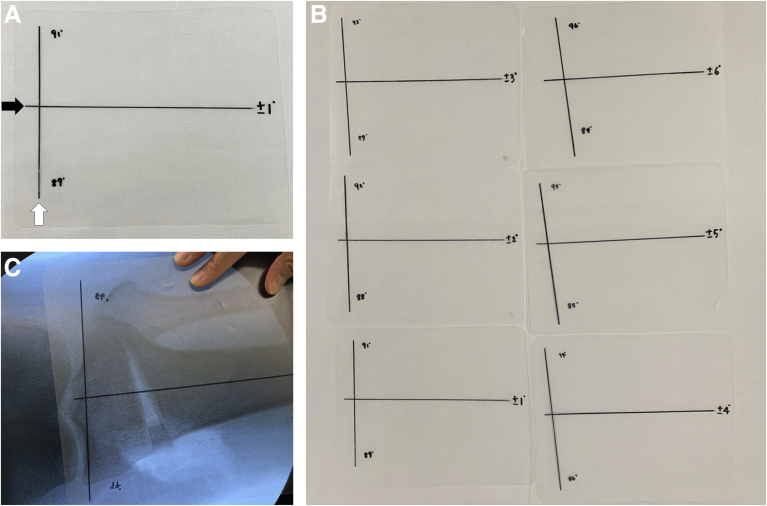
Following the stepwise opening using 3 to 5 chisels (Fig 7E), the K-wires and the retractor are removed. Retracting the pes and the sMCL, the first spreader is inserted into the posterior-most gap and opened to 6 to 7 mm (Fig 6E). The small pillow is then moved under the heel to extend the knee gravitationally. After widening the posterior gap to the desired target distance, the anterior spreader is inserted to maintain the distance (Fig 6F). The posterior bone substitute wedge is inserted to replace the posterior spreader (Fig 6F). Thanks to the tension applied by the pes, the gap will automatically close after the wedge insertion followed by the removal of the anterior spreader. We then confirm that the MPTA has been appropriately corrected using the MPTA-measurement film (Fig 8C). After inserting the anterior bone substitute wedge (Fig 6G), the reflected sMCL is then returned to its original position underneath the pes anserinus (Fig 6G) and repaired (Fig 6H). The TriS medial HTO plate is temporarily fixed with a proximal K-wire through the sleeve, and the correct plate position is confirmed fluoroscopically (Fig 7F). Finally, all screws are inserted and locked (Fig 7G). A general outline of the surgical procedure and the risks and limitations of this technique are described in Tables 2 and 3, respectively.
Fig 8.
Intraoperative confirmation of the correction angle. (A) An original medial proximal tibial angle (MPTA)-measurement film on the monitor. The horizontal axis (black arrow) and vertical axis (white arrow) indicate the tibial shaft axis and joint line, respectively. (B) Films with different MPTA diagrams are prepared for measurement. (C) After inserting the posterior bone substitute wedge, the MPTA-measurement film is placed on the fluoroscopy monitor.
Table 2.
Surgical Procedure
| 1. Preoperative planning and preparation |
| - The target postoperative weight-bearing line lies 60% to 70% from the medial side. |
| - A bone substitute block is cut for the posterior and anterior wedges, according to the surgical plan. |
| - The wedges are dipped into saline including antibiotics (1g cefazolin/100 mL saline) to prevent infection. |
| 2. Approach |
| - The opposite leg is placed lower than the operative leg for good visualization of the medial aspect. |
| - Partial or total meniscectomy/meniscal repair for a torn medial meniscus, if present, is performed. |
| - A reversed curved oblique incision is used. |
| - Pes anserinus elevation is performed without cutting/releasing. |
| - The sMCL is detached from the distal attachment using a Cobb elevator. |
| - The medial border of the patellar tendon is incised, taking care not to injure the infrapatellar fat pad. |
| - An ascending osteotomy line is drawn with an electrosurgical knife, as long as possible to create the anterior flange. |
| - The flange thickness should be approximately 15 mm, and the angle between the ascending and oblique osteotomies is 100°. |
| - The popliteal muscle belly is detached from the posterior aspect of the tibia using a Cobb elevator in knee flexion. |
| A radiolucent retractor is inserted between the popliteal muscle and the tibia. |
| The knee is extended, with a small pillow underneath to achieve the correct tangential view of the joint surface. |
| - Full-extension and mid-flexion positions are recommended for the anterior and posterior exposures, respectively. |
| - The pulsation of the popliteal artery can be easily confirmed if a tourniquet is not applied. |
| 3. Osteotomy |
| - The oblique osteotomy is started 4 cm from the joint line. |
| - The hinge point is set just above the PTFJ, lateral to its medial margin. |
| - The first K-wire is inserted from the intersection of the ascending and oblique osteotomies to just above the hinge point. |
| - An intraoperative X-ray is acquired, tangential to the PTFJ in 50° internal rotation), to confirm the hinge position. |
| -The second and third K-wires are inserted parallel to the first K-wire and the posterior tibial slope. |
| - The ascending osteotomy line is cut using a micro-oscillating saw and a chisel. |
| - The oblique osteotomy is cut using a micro-oscillating saw and chisels leaving the posterior cortex intact. |
| - The oblique osteotomy is completed by cutting the posterior cortex with a micro- or standard-reciprocating saw and a chisel. |
| 4. Gap opening and plate fixation |
| - The gap is opened in a stepwise manner using 3-5 chisels, depending on the target opening distance. |
| - The first spreader is inserted into the posterior-most gap and opened to 6–7 mm after retracting the pes and the sMCL. |
| - A small pillow is placed below the heel to extend the knee. |
| - The posterior gap to the target distance is opened, and the second spreader is inserted into the anterior gap. |
| - Keeping the distance by the second spreader, the first spreader is replaced by the appropriate bone substitute wedge. |
| - The second spreader is replaced by the anterior substitute wedge. |
| - The reflected sMCL is returned to its original position underneath the pes and repaired in a side-to-side manner. |
| - The plate is installed as posteriorly as possible, fixed temporarily with K-wires, and the position is checked fluoroscopically. |
| - The plate is then fixed with locking screws. |
K-wire, Kirschner wire; PTFJ, proximal tibiofibular joint; sMCL, superficial medial collateral ligament.
Table 3.
Risks and Limitations of this Technique
| Risks in Each Surgical Step | Limitations |
|---|---|
1) Reversed curved oblique incision
|
1) The tension of the pes anserinus sometimes disrupts the opening by a spreader in cases with a large opening gap. |
2) Complete release of the sMCL
|
2) In smaller patients, the distance between the joint line and the upper border of the pes anserinus is shorter. It is difficult to make room for osteotomy/bone-substitute insertion/plate installation in such cases. |
3) Double-spreader technique
|
3) The normal bone-ligament interface of the sMCL cannot be reconstructed using side-to-side repair of the sMCL and pes anserinus. |
sMCL, superficial medial collateral ligament.
Postoperative Rehabilitation
Full weight-bearing walking exercise, as well as range of motion exercise, are allowed on the first postoperative day and are advanced gradually, as tolerated.
Discussion
OWHTO surgical exposure maximizes the advantages of the medial biplanar opening technique, while avoiding the risk of complications.
The most important problem in medial knee surgeries is saphenous nerve injury, characterized by hypoesthesia and/or hyperesthesia and/or neuropathic dermatitis that typically appears lateral to the incision site.20 In order to avoid these risks, we adopted the reversed curved oblique incision (Fig 1C), through which both the anterior and posterior parts of the osteotomy line are clearly visible.17
A single-plane osteotomy has little room for plate fixation because of the necessity to cut proximal to the patellar tendon insertion.21 In biplanar OWHTO, in addition to the large contact area at the ascending osteotomy site, the distal osteotomy affords room for plate fixation.21 However, the contact pressure of the ascending osteotomy site cannot be increased by the locking system. An intact pes works as a compressor of the ascending osteotomy owing to the posterior component force (Fig 2, A and B). If the pes is cut, the distal part can be easily rotated externally, especially in cases with an unstable lateral hinge fracture (Fig 2C). The proximal component of the contractile strength of the pes also provides the compressive force between the bone substitute and the proximal/distal cortices (Fig 2, A and D), allowing postoperative weight-bearing to be distributed to the substitute, as well as the plate, which may reduce the risk of implant failure.
Complete sMCL release, which is required for decompression of the medial compartment,10 does not induce medial laxity11 because of the remaining deep MCL (dMCL; Fig 3C). Staubli et al.1 dissect the sMCL proximal to the pes (Fig 3C) and Brosset et al.5 remove it from the posteromedial cortex. However, these unrepairable releases may trigger the risk of deep infection or the possible medial laxity during total knee arthroplasty conversion (Fig 3D).9 Releasing the sMCL from the distal portion using a periosteal elevator6,9 combined with leaving the pes intact can be an effective approach to the repair of these medial stabilizers (Fig 3E).
In conclusion, OWHTO, through a reversed curved oblique incision with pes anserinus preservation, insertion of bone substitutes, and complete distal sMCL release, may prevent multiple complications.
Acknowledgment
The authors would like to thank Howard Colefield, MEDICAL VIEW Co., LTD., and Masaki Amemiya for narrating the video transcript, drawing the figures, and helping to draw the figures, respectively. We also thank Etsuko Tabata and Kaori Matsumoto, who invented the MPTA-measurement film and helped the deformity analysis using the digital surgical planning tool, respectively.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.N. has a consultancy with Olympus Terumo Biomaterials. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video shows the technique used for open-wedge high tibial osteotomy using the TriS plate, with preservation of the pes anserinus and insertion of bone substitutes. One of the authors has a consultancy agreement with Olympus Terumo Biomaterials, which produces the TriS plate. Herein, we demonstrate the surgical procedure on the left knee. Before starting surgery, two bone substitute wedges, posterior and anterior wedges, are cut from a block. Our routine exposure using a reversed curved oblique incision starts from the extension of the anteromedial portal. The torn medial meniscus is arthroscopically resected through an anterolateral portal and an anteromedial portal. After the reversed curved oblique incision is created, the pes anserinus is elevated using forceps, and its proximal border is incised. The pes anserinus is retracted, and the superficial medial collateral ligament is then completely detached from its tibial insertion. If the exposure is inadequate, the curved incision is extended to the portal to provide good visualization of the surgical field. The medial border of the patellar tendon is cut with an electrosurgical knife, and the ascending osteotomy line is drawn. A Cobb elevator is used to detach the popliteal muscle from the tibial posterior aspect to enable the safe insertion of a posterior radiolucent retractor. The oblique osteotomy is started at 4 cm from the joint line. The first K-wire is inserted from the point of intersection of the ascending and oblique osteotomy lines to just above the hinge. The hinge point is confirmed on the internally rotated tangential view to the proximal tibiofibular joint. One or two K-wires are added parallel to the first K-wire. The ascending osteotomy is cut with a micro-oscillating saw and a chisel. The medial cortex is cut with a micro-oscillating saw, and a chisel is inserted into the hinge. The posteromedial cortex is cut with a micro-reciprocating saw, and the posterior cortex is cut with a standard reciprocating saw. The posterior cortical cut is completed with a dedicated chisel. After stepwise opening using 3-5 chisels, the first spreader is inserted into the posterior gap and opened. A small pillow is put under the heel to achieve full knee extension. The anterior spreader is inserted, and the posterior wedge with the planned opening height is inserted to replace the first spreader. The anterior wedge is inserted, and the reflected medial collateral ligament is then returned to its original position beneath the pes anserinus and repaired. The plate is temporarily fixed with a K-wire to enable the confirmation of the appropriate plate position. The locking screws are inserted in sequence using the cannulation technique. A 2-cm incision is added for the insertion of the distal two monocortical screws, which are inserted and locked. This is the final fluoroscopic anteroposterior view.
References
- 1.Staubli A.E., De Simoni C., Babst R., Lobenhoffer P. TomoFix: A new LCP-concept for open wedge osteotomy of the medial proximal tibia—early results in 92 cases. Injury. 2003;34(Suppl 2):B55–B62. doi: 10.1016/j.injury.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 2.Reischl N., Wahl P., Jacobi M., Clerc S., Gautier E., Jakob R.P. Infections after high tibial open wedge osteotomy: a case control study. Arch Orthop Trauma Surg. 2009;129:1483–1487. doi: 10.1007/s00402-008-0773-9. [DOI] [PubMed] [Google Scholar]
- 3.Mochizuki T., Akita K., Muneta T., Sato T. Pes anserinus: Layered supportive structure on the medial side of the knee. Clin Anat. 2004;17:50–54. doi: 10.1002/ca.10142. [DOI] [PubMed] [Google Scholar]
- 4.Lobenhoffer P., Agneskirchner J.D. Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2003;11:132–138. doi: 10.1007/s00167-002-0334-7. [DOI] [PubMed] [Google Scholar]
- 5.Brosset T., Pasquier G., Migaud H., Gougeon F. Opening wedge high tibial osteotomy performed without filling the defect but with locking plate fixation (TomoFix) and early weight-bearing: Prospective evaluation of bone union, precision and maintenance of correction in 51 cases. Orthop Traumatol Surg Res. 2011;97:705–711. doi: 10.1016/j.otsr.2011.06.011. [DOI] [PubMed] [Google Scholar]
- 6.Noyes F.R., Mayfield W., Barber-Westin S.D., Albright J.C., Heckmann T.P. Opening wedge high tibial osteotomy: An operative technique and rehabilitation program to decrease complications and promote early union and function. Am J Sports Med. 2006;34:1262–1273. doi: 10.1177/0363546505286144. [DOI] [PubMed] [Google Scholar]
- 7.Takeuchi R., Ishikawa H., Aratake M., et al. Medial opening wedge high tibial osteotomy with early full weight bearing. Arthroscopy. 2009;25:46–53. doi: 10.1016/j.arthro.2008.08.015. [DOI] [PubMed] [Google Scholar]
- 8.Akiyama T., Okazaki K., Mawatari T., Ikemura S., Nakamura S. Autologous osteophyte grafting for open-wedge high tibial osteotomy. Arthrosc Tech. 2016;5:e989–e995. doi: 10.1016/j.eats.2016.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim H.J., Shin J.Y., Lee H.J., Park K.H., Jung C.H., Kyung H.S. Can medial stability be preserved after open wedge high tibial osteotomy? Knee Surg Relat Res. 2020;32:51. doi: 10.1186/s43019-020-00071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agneskirchner J.D., Hurschler C., Wrann C.D., Lobenhoffer P. The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: A biomechanical study. Arthroscopy. 2007;23:852–861. doi: 10.1016/j.arthro.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 11.Sato D., Kondo E., Yabuuchi K., et al. Assessment of valgus laxity after release of the medial structure in medial open-wedge high tibial osteotomy: An in vivo biomechanical study using quantitative valgus stress radiography. BMC Musculoskelet Disord. 2019;20:481. doi: 10.1186/s12891-019-2859-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Itou J., Itoh M., Maruki C., et al. Deep peroneal nerve has a potential risk of injury during open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2020;28:1372–1379. doi: 10.1007/s00167-019-05445-y. [DOI] [PubMed] [Google Scholar]
- 13.Miniaci A., Ballmer F.T., Ballmer P.M., Jakob R.P. Proximal tibial osteotomy. A new fixation device. Clin Orthop Relat Res. 1989:250–259. [PubMed] [Google Scholar]
- 14.Shin K.H., Jung J.K., Nam J.J., Jang K.M., Han S.B. Preoperative supine radiographs are more accurate than standing radiographs for preoperative planning in medial open-wedge high tibial osteotomy. Arthroscopy. 2020;36:1655–1664. doi: 10.1016/j.arthro.2020.01.057. [DOI] [PubMed] [Google Scholar]
- 15.Schröter S., Ihle C., Mueller J., Lobenhoffer P., Stöckle U., van Heerwaarden R. Digital planning of high tibial osteotomy. Interrater reliability by using two different softwares. Knee Surg Sports Traumatol Arthrosc. 2013;21:189–196. doi: 10.1007/s00167-012-2114-3. [DOI] [PubMed] [Google Scholar]
- 16.Paley D., Herzenberg J.E., Tetsworth K., McKie J., Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25:425–465. [PubMed] [Google Scholar]
- 17.Nakamura R., Komatsu N., Murao T., et al. The validity of the classification for lateral hinge fractures in open wedge high tibial osteotomy. Bone Joint J. 2015;97-B:1226–1231. doi: 10.1302/0301-620X.97B9.34949. [DOI] [PubMed] [Google Scholar]
- 18.Kley K., Bin Abd Razak H.R., Khakha R.S., Wilson A.J., van Heerwaarden R., Ollivier M. Soft-tissue management and neurovascular protection during opening-wedge high tibial osteotomy. Arthrosc Tech. 2021;10:e419–e422. doi: 10.1016/j.eats.2020.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nakamura R., Komatsu N., Fujita K., et al. Appropriate hinge position for prevention of unstable lateral hinge fracture in open wedge high tibial osteotomy. Bone Joint J. 2017;99-B:1313–1318. doi: 10.1302/0301-620X.99B10.BJJ-2017-0103.R1. [DOI] [PubMed] [Google Scholar]
- 20.Nazeer M., Ravindran R., Katragadda B.C., Muhammed E.N., Rema D.T.J., Muhammed M.N. SKINTED: A rare complication after total knee arthroplasty. Arthroplasty Today. 2020;6:1028–1032. doi: 10.1016/j.artd.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Staubli A.E., Jacob H.A. Evolution of open-wedge high-tibial osteotomy: Experience with a special angular stable device for internal fixation without interposition material. Int Orthop. 2010;34:167–172. doi: 10.1007/s00264-009-0902-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video shows the technique used for open-wedge high tibial osteotomy using the TriS plate, with preservation of the pes anserinus and insertion of bone substitutes. One of the authors has a consultancy agreement with Olympus Terumo Biomaterials, which produces the TriS plate. Herein, we demonstrate the surgical procedure on the left knee. Before starting surgery, two bone substitute wedges, posterior and anterior wedges, are cut from a block. Our routine exposure using a reversed curved oblique incision starts from the extension of the anteromedial portal. The torn medial meniscus is arthroscopically resected through an anterolateral portal and an anteromedial portal. After the reversed curved oblique incision is created, the pes anserinus is elevated using forceps, and its proximal border is incised. The pes anserinus is retracted, and the superficial medial collateral ligament is then completely detached from its tibial insertion. If the exposure is inadequate, the curved incision is extended to the portal to provide good visualization of the surgical field. The medial border of the patellar tendon is cut with an electrosurgical knife, and the ascending osteotomy line is drawn. A Cobb elevator is used to detach the popliteal muscle from the tibial posterior aspect to enable the safe insertion of a posterior radiolucent retractor. The oblique osteotomy is started at 4 cm from the joint line. The first K-wire is inserted from the point of intersection of the ascending and oblique osteotomy lines to just above the hinge. The hinge point is confirmed on the internally rotated tangential view to the proximal tibiofibular joint. One or two K-wires are added parallel to the first K-wire. The ascending osteotomy is cut with a micro-oscillating saw and a chisel. The medial cortex is cut with a micro-oscillating saw, and a chisel is inserted into the hinge. The posteromedial cortex is cut with a micro-reciprocating saw, and the posterior cortex is cut with a standard reciprocating saw. The posterior cortical cut is completed with a dedicated chisel. After stepwise opening using 3-5 chisels, the first spreader is inserted into the posterior gap and opened. A small pillow is put under the heel to achieve full knee extension. The anterior spreader is inserted, and the posterior wedge with the planned opening height is inserted to replace the first spreader. The anterior wedge is inserted, and the reflected medial collateral ligament is then returned to its original position beneath the pes anserinus and repaired. The plate is temporarily fixed with a K-wire to enable the confirmation of the appropriate plate position. The locking screws are inserted in sequence using the cannulation technique. A 2-cm incision is added for the insertion of the distal two monocortical screws, which are inserted and locked. This is the final fluoroscopic anteroposterior view.
This video shows the technique used for open-wedge high tibial osteotomy using the TriS plate, with preservation of the pes anserinus and insertion of bone substitutes. One of the authors has a consultancy agreement with Olympus Terumo Biomaterials, which produces the TriS plate. Herein, we demonstrate the surgical procedure on the left knee. Before starting surgery, two bone substitute wedges, posterior and anterior wedges, are cut from a block. Our routine exposure using a reversed curved oblique incision starts from the extension of the anteromedial portal. The torn medial meniscus is arthroscopically resected through an anterolateral portal and an anteromedial portal. After the reversed curved oblique incision is created, the pes anserinus is elevated using forceps, and its proximal border is incised. The pes anserinus is retracted, and the superficial medial collateral ligament is then completely detached from its tibial insertion. If the exposure is inadequate, the curved incision is extended to the portal to provide good visualization of the surgical field. The medial border of the patellar tendon is cut with an electrosurgical knife, and the ascending osteotomy line is drawn. A Cobb elevator is used to detach the popliteal muscle from the tibial posterior aspect to enable the safe insertion of a posterior radiolucent retractor. The oblique osteotomy is started at 4 cm from the joint line. The first K-wire is inserted from the point of intersection of the ascending and oblique osteotomy lines to just above the hinge. The hinge point is confirmed on the internally rotated tangential view to the proximal tibiofibular joint. One or two K-wires are added parallel to the first K-wire. The ascending osteotomy is cut with a micro-oscillating saw and a chisel. The medial cortex is cut with a micro-oscillating saw, and a chisel is inserted into the hinge. The posteromedial cortex is cut with a micro-reciprocating saw, and the posterior cortex is cut with a standard reciprocating saw. The posterior cortical cut is completed with a dedicated chisel. After stepwise opening using 3-5 chisels, the first spreader is inserted into the posterior gap and opened. A small pillow is put under the heel to achieve full knee extension. The anterior spreader is inserted, and the posterior wedge with the planned opening height is inserted to replace the first spreader. The anterior wedge is inserted, and the reflected medial collateral ligament is then returned to its original position beneath the pes anserinus and repaired. The plate is temporarily fixed with a K-wire to enable the confirmation of the appropriate plate position. The locking screws are inserted in sequence using the cannulation technique. A 2-cm incision is added for the insertion of the distal two monocortical screws, which are inserted and locked. This is the final fluoroscopic anteroposterior view.