Abstract
We described two cases of acute pancreatitis secondary to ansa pancreatica. The first patient was diagnosed on MRCP and improved after standard treatment of AP. In the second case, ansa pancreatica was diagnosed on IOP. At the second episode of AP, sphincterotomy of the minor papilla was performed.
Keywords: acute pancreatitis, ansa pancreatica, cholangiography, magnetic resonance cholangiopancreatography, pancreatic ducts
Ansa pancreatica is a rare anatomic variant of the pancreatic duct known as predisposing factor for acute pancreatitis. This abnormality should be considered in the diagnosis and management of subjects with idiopathic recurrent acute pancreatitis.

1. INTRODUCTION
Ansa pancreatica is a rare anatomic variant of the pancreatic duct characterized by the atrophy of the accessory duct, which is replaced with an additional curved communicating duct between the ventral and dorsal ducts forming a loop that terminates at the minor papilla. 1
This condition was first described by Dawson and Langman in 1961. 2 Although it does not have specific clinical manifestations, ansa pancreatica is considered to be a predisposing factor for acute pancreatitis particularly in alcoholic patients. 3 This association is still hypothetical since its physiopathology is not yet well understood. The diagnosis of this rare congenital pancreatic ductal anomaly can be made by magnetic resonance cholangiopancreatography (MRCP) or by endoscopic retrograde cholangiopancreatography (ERCP), which allows endoscopic treatment through sphincterotomy of the minor papilla.
Ansa pancreatica causing acute pancreatitis is an under‐reported disease entity. We herein report two relevant cases to highlight the diagnostic and therapeutic challenge.
2. CASE REPORT 1
A thirty‐two‐year‐old female without past medical history was presented with epigastric abdominal pain evolving for two days. Physical examination showed epigastric tenderness. Laboratory findings revealed a high level of lipase (3280 U/L). Otherwise, liver function tests, serum calcium, and triglycerides were within normal limits. Abdominal ultrasound revealed an empty gallbladder. The diagnosis of acute pancreatitis was then made. The abdominal CT scan objectified an acute pancreatitis stage D of Balthazar. The biliary ducts were not dilated. The patient improved after standard treatment of acute pancreatitis based on bowel rest and adequate intravenous hydration and was then discharged. As part of the etiological assessment, an outpatient MRCP was performed. The latter revealed an acalculous gallbladder. The common bile duct and intrahepatic bile ducts were slightly dilated with no visualized lithiasis. Otherwise, the Wirsung duct was thin and we note the presence of a ductal variant consisting of the termination of a secondary pancreatic duct in an accessory papilla, an aspect according to ansa pancreatica (Figure 1). Then, ansa pancreatica was considered as the main etiology of this episode of acute pancreatitis and no specific management was considered. After one year of follow‐up, the patient is doing well with no recurrence of pancreatitis.
FIGURE 1.
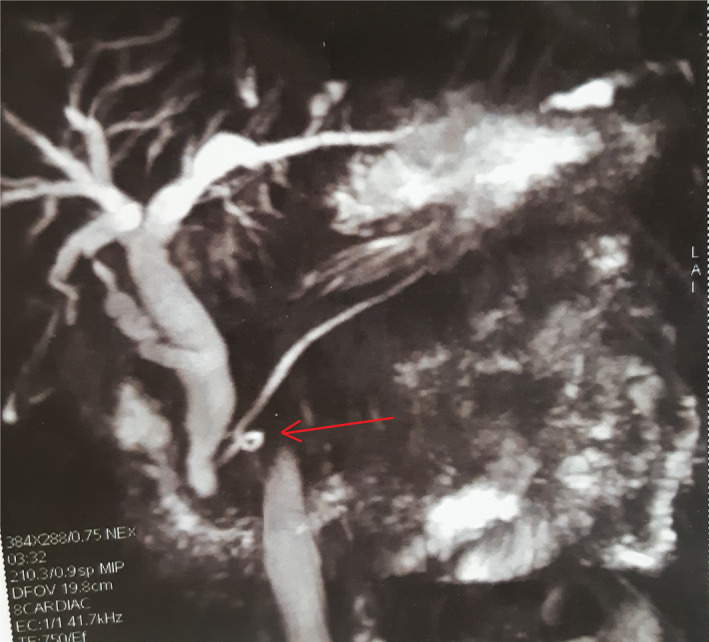
Magnetic resonance cholangiopancreatography showing a looping duct: ansa pancreatica (red arrow)
3. CASE REPORT 2
A fifty‐nine‐year‐old diabetic woman presented to the emergency department with severe pain in the epigastrium, which radiated to the back, evolving for four days. The diagnosis of acute pancreatitis was made based on clinical findings (epigastric wheelbase) and a high level of serum lipase on laboratory workup (1890 U/L). The abdominal CT scan objectified an acute pancreatitis stage C of Balthazar, and abdominal ultrasound showed a gallbladder sludge (the common bile duct had a normal caliber). The biliary origin of the pancreatitis was then retained. The patient was operated on 7 days later. A laparoscopic cholecystectomy was performed and a transcystic tube was posed. The intraoperative cholangiography showed a normal cholangiogram; however, there was an abnormal variation of the pancreatic ducts. A looping branch arises from the main pancreatic duct and terminates near the minor papilla, which corresponds to ansa pancreatica type of ductal anatomy (Figure 2). Gross examination of the resected gallbladder confirmed the absence of gallstones. Consequently, ansa pancreatica is the cause of this acute pancreatitis. The postoperative course was uneventful, and the patient was discharged on the second postoperative day. Four months later, the patient experienced her second episode of acute pancreatitis (stage B of Balthazar on abdominal CT scan). Sphincterotomy of the minor papilla was then performed, and the patient was discharged with complete resolution of symptoms and did not present any additional episodes of pancreatitis for a total follow‐up of two years.
FIGURE 2.

Intraoperative cholangiography: (yellow arrow): ansa pancreatica
4. DISCUSSION
Acute pancreatitis has several known causes. The most common ones are gallstones, alcohol intake, and metabolic disorders (hypercalcemia and hypertriglyceridemia). 4 However, variations in pancreatic duct anatomy such as pancreas divisum, annular pancreas, and ansa pancreatica represent rare causes of acute pancreatitis. 5
Ansa pancreatica is an uncommon anatomic variant of the pancreatic duct in which a branch descends as an extension of the main pancreatic duct, later ascending to form a loop that terminates at the minor papilla. 1 Dawson and Langman (1961) were the first to describe this ductal anomaly, in an anatomical and radiological study of cadaveric subjects. 2
Due to its rarity, the prevalence of ansa pancreatica is not well established in the literature. Based on radiological findings (MRCP and ERCP), some reports have evaluated the occurrence rate of ansa pancreatica in patients with acute pancreatitis and have determined that the rate varies from 0.5% to 0.9%. 6 Moreover, these studies consisted of community‐based cohorts so their results cannot apply to the general population in the world. In our department, only three cases of ansa pancreatica were detected among 569 patients admitted for acute pancreatitis between January 2010 and December 2019, giving an incidence of 0.5%. The first case was published in 2012, 7 and we here report the second and the third cases.
Generally, this anomaly is incidentally discovered since it has no clinical significance. On the other hand, most of the reported cases in the literature propose ansa pancreatica as a predisposing factor for acute pancreatitis. The real mechanism of this association has not been clear yet. Similar to pancreas divisum, it is suggested that in ansa pancreatica the drainage through the minor papilla is inadequate due to its oblique communication with the main duct, leading to recurrent acute pancreatitis. 8
This hypothesis remained unconfirmed for a long time. Among the 23 studies found on our research on PubMed using ansa pancreatica as a search term, only three series studied the correlation between ansa pancreatica and the onset of acute recurrent pancreatitis.
Ishii et al. (1998) 9 reported that approximately 7% of the patients with ansa pancreatica presented with acute pancreatitis. A Turkish series published by Adibelli et al. (2016) 10 reported an ansa pancreatica incidence of 1.2%. This study tried to establish the connection between pancreatic ducts variations and the modified MRCP Cambridge classification system of chronic pancreatitis. In the results, ansa pancreatica was associated with a higher score and, thus, might be considered a relevant factor to the onset of chronic pancreatitis.
But the solid statistically significant evidence was only provided by the case‐control study of Hayashi et al. (2016). 11 It was determined that patients with recurrent pancreatitis had a higher frequency of ansa pancreatica than the general population (11.1% vs 0.85%).
In our case, there seemed to be no other explanation for the patients’ episodes of acute pancreatitis other than the patients having ansa pancreatica. The patient of the second case had complete resolution of symptoms after sphincterotomy of the minor papilla. We can conclude that findings from both of our reported cases are in line with previous studies, and ansa pancreatica can be considered to be the main cause of these patients’ acute pancreatitis or at least the main predisposing factor.
In addition to the standard treatment of acute pancreatitis, ansa pancreatica being the cause of pancreatitis necessitates the decompression of minor duodenal papilla by sphincterotomy, 12 which can be technically challenging as isolated endoscopic cannulation of the minor papilla in patients presenting anatomical variants such as ansa pancreatica increases the technical difficulty.
Based on our experience and current consistent evidence, we would propose that in patients with idiopathic recurrent acute pancreatitis, clinicians should investigate the presence of ductal anomaly such as ansa pancreatica and should consider it in the diagnosis and management of these patients.
A firm knowledge of common and variant anatomy is paramount for surgeons, who often come across anatomic variations that either are asymptomatic or cause pathology. Ansa pancreatica is a bold example of how aberrant anatomy could predispose to certain pathologic conditions.
CONFLICTS OF INTEREST
Authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Dr Ben Ismail Imen: Study concepts and manuscript writing. Dr Rebii Saber: Helped in data interpretation and manuscript evaluation. Dr Zenaidi Hakim: Data acquisition. Dr Zoghlami Ayoub: Critical revision.
ETHICAL APPROVAL
Ethical approval was not required, and patient identifying knowledge was not presented in the report.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGMENTS
This study was not supported by any institution and company.
Ben Ismail I, Rebii S, Zenaidi H, Zoghlami. Acute pancreatitis secondary to ansa pancreatica: Two new cases and review of the literature. Clin Case Rep. 2022;10:e05381. doi: 10.1002/ccr3.5381
Funding information
This research received no specific grant from any funding agency in the public, commercial, or not‐for‐profit sectors
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Delhaye M, Matos C, Deviere J. Acute relapsing pancreatitis. Congenital variants: diagnosis, treatment, outcome. JOP. 2001;2:373‐381. [PubMed] [Google Scholar]
- 2. Dawson W, Langman J. An anatomical‐radiological study on the pancreatic duct pattern in man. Anat Rec. 1961;139:59‐68. [DOI] [PubMed] [Google Scholar]
- 3. Jarrar MS, Khenissi A, Ghrissi R, Hamila F, Letaief R. Ansa pancreatica: an anatomic variation and a rare cause of acute pancreatitis. Surg Radiol Anat. 2013;35:745‐748. [DOI] [PubMed] [Google Scholar]
- 4. Whitcomb DC. Clinical practice. Acute pancreatitis. N Engl J Med. 2006;354:2142‐2150. [DOI] [PubMed] [Google Scholar]
- 5. Ben Ismail I, Zenaidi H, Yahmadi A, Rebii S, Zoghlami A. Surgical management of groove pancreatitis: a case report. Pan African Medical Journal. 2020;36:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kosirog J, Boulay B, Yazici C. Ansa pancreatica, a rare cause of acute pancreatitis: clinical relevance and review of the literature. JOP. 2018;19(6):315‐320. [Google Scholar]
- 7. Ayari H, Rebii S, Ayari M, Hasni R, Zoghlami A. L’ansa pancreatica: une cause rare de pancréatite aigue. Pan Afr Med J. 2012;13:33. [PMC free article] [PubMed] [Google Scholar]
- 8. Bhasin DK, Rana SS, Nanda M, et al. Ansa pancreatica type of ductal anatomy in a patient with idiopathic acute pancreatitis. JOP. 2006;7:315‐320. [PubMed] [Google Scholar]
- 9. Ishii H, Arai K, Fukushima M, et al. Fusion variations of pancreatic ducts in patients with anomalous arrangement of pancreaticobiliary ductal system. J Hepatobiliary Pancreat Surg. 1998;5:327‐332. [DOI] [PubMed] [Google Scholar]
- 10. Adibelli ZH, Adatepe M, Imamoglu C, Esen OS, Erkan N, Yildirim M. Anatomic variations of the pancreatic duct and their relevance with the Cambridge classification system: MRCP findings of 1158 consecutive patients. Radiol Oncol. 2016;50:370‐377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hayashi TY, Gonoi W, Yoshikawa T, Hayashi N, Ohtomo K. Ansa pancreatica as a predisposing factor for recurrent acute pancreatitis. World J Gastroenterol. 2016;22:8940‐8948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Riff PB, Chandrasekhara V. The role of endoscopic retrograde cholangiopancreatography in management of pancreatic diseases. Gastroenterol Clin North Am. 2016;45:45‐65. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


