Abstract
A 12-year-old male with nonverbal autism and morbid obesity was referred to a pediatric sleep center during the SARS-CoV-2 pandemic for complaints of snoring with tonsillar hypertrophy and difficulty falling asleep. Due to social challenges, the family had not sought in-person care in the past. Through telemedicine consultation and home sleep apnea testing, the patient was diagnosed with obstructive sleep apnea as well as an irregular sleep-wake disorder. This unique utilization of the health care system in the care of a complex patient with multiple sleep disorders demonstrates the utility of remote care and testing. There is a great benefit to continuing to provide pediatric sleep care in this way beyond the pandemic.
Keywords: autism, sleep apnea, insomnia, telemedicine, children, sleep, home sleep apnea testing
CASE
A 12-year-old boy with a history of nonverbal autism, behavioral difficulties, attention-deficit hyperactivity disorder, asthma, and morbid obesity was referred to sleep medicine for snoring in the setting of tonsillar hypertrophy as well as difficulties with sleep onset. The patient was cared for by a single parent who also had obligations to work and home and was caring for her ill mother. The family had limited time and social support, resulting in multiple missed appointments over the years, including sleep medicine.
His mother’s primary sleep concern involved an unpredictable sleep schedule. Before the pandemic, the patient would miss school or his afterschool therapies (eg, speech, occupational, psychology) due to unpredictable sleep patterns. The patient was discharged from some of these therapies due to frequent absences. During the pandemic, the patient was unable to engage in remote learning and his delayed sleep-wake phase morphed into more of an irregular sleep-wake phase. The situation left his mother sleep-deprived as well.
In addition, he had snoring and witnessed apneas with new-onset nocturnal enuresis. The mother reported that she was told he had tonsillar hypertrophy but felt strongly that the patient’s weight (BMI 44.46 kg/m2, z score 3.57) was an important contributor to his sleep-disordered breathing. No prior polysomnography had been performed as the mother worried her son would be unable to fall asleep during the allotted study time.
QUESTION: Given the patient’s presenting complaints and underlying developmental disabilities, what nontraditional platforms for consultation and testing might a practitioner utilize?
ANSWER: Telemedicine and home sleep apnea testing
DISCUSSION
The ability of a parent to manage a child’s behavior in the clinic is an important determinant of whether a practitioner can provide optimal care. When already-limited clinical time is spent calming, distracting, or redirecting a child in the office, the thoroughness of history-taking, physical exam performance, and discussion of recommendations is compromised. With a virtual encounter from home, a parent can offer the child familiar toys and activities, as well as allow them to step away. In this case, the patient slept for much of the telemedicine encounter, waking briefly for a very limited physical exam and then returning to his room. This afforded the physician and parent ample stress-free time to review the complex history and develop a plan of care.
While oropharyngeal exams can be successfully performed during virtual visits with an engaged and cooperative patient,1 this part of the physical exam was unfortunately not feasible, given the patient’s behavioral challenges.
The patient’s nontraditional and unpredictable sleep-wake timing and developmental and behavioral challenges made it unlikely that in-laboratory polysomnography would capture the data required to determine the next steps of care, without significant time and effort put toward desensitization. A home sleep apnea test (HSAT) was ordered instead. The American Academy of Sleep Medicine does not currently recommend the use of HSAT for the diagnosis of obstructive sleep apnea in individuals under 18 years of age.2 While technically feasible, there is a concern for the successful placement of sensors as well as a child’s ability to keep them on throughout the night. There is also a concern for underestimation of the severity of sleep-disordered breathing, given the inability either to score respiratory events based on arousals or collect any CO2 data to assess for hypoventilation.2 However, studies that followed the publication of this guideline demonstrated minimal artifact and good sensitivity and specificity when evaluating moderate/severe sleep-disordered breathing,3 particularly in older children.4,5 More research is needed to explore this technology in children.
Additionally, the American Academy of Otolaryngology—Head and Neck Surgery6 and the American Academy of Pediatrics7 both consider alternative sleep testing as appropriate means to evaluate sleep-disordered breathing to guide adenotonsillectomy. In this case, HSAT was used as a tool for guiding surgical decision-making, given the patient’s reported tonsillar hypertrophy and clinically reported sleep-disordered breathing.
During the pandemic, HSAT was performed with single-use belts and pulse oximeters provided to patients (Table 1 and Figure 1). Sanitized recording devices were picked up and then dropped off at the sleep laboratory during daytime hours. This patient’s device was programmed for 48 hours and his mother was instructed to place the monitoring equipment on the patient during all sleep opportunities. A sleep log was also given to track the patient’s sleep on the study night and onwards to better assess his sleep schedule. Close follow-up via telemedicine was scheduled to go over the results. The mother was also instructed to take a photo of the sleep log and send it through the patient portal application for review.
Table 1.
HSAT results.
| Recording Time | 12:00 pm to 6:00 pm and 3:00 am to 7:00 am |
|---|---|
| Respiratory event index | 41.1 events/h |
| Average SpO2 | 94.1% |
| SpO2 nadir | 78% |
| Recording time with SpO2 < 90% | 55 min |
The mother applied the HSAT equipment to the patient from 12:00 pm to 6:00 pm and again from 3:00 am to 7:00 am, reflecting his irregular sleep-wake pattern. HSAT = home sleep apnea testing, SpO2 = oxygen saturation.
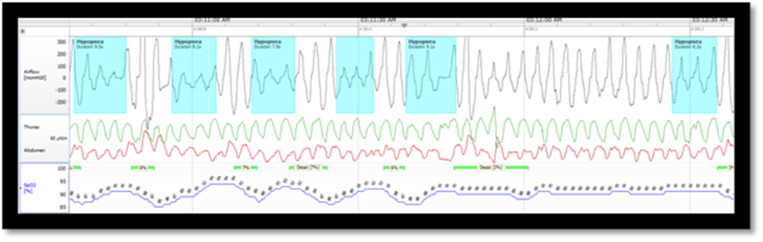
Figure 1. A 2-minute screenshot from the patient’s HSAT recording.
Airflow, thorax and abdominal effort, and pulse oximetry are shown. Despite the patient’s developmental challenges and nonverbal status, the recording from all channels was intact. HSAT = home sleep apnea testing.
The child was diagnosed with obstructive sleep apnea and underwent tonsillectomy without complications. Another HSAT was planned for 10–12 weeks postoperative to reevaluate the patient’s sleep-disordered breathing.
At follow-up, the mother reported that the patient was unable to tolerate wearing the HSAT device for more than 15 minutes and was awake for the entire time. This limited the ability to objectively consider the obstructive sleep apnea resolved. Insufficient collection of data is a risk with HSAT in adults and children, and in-lab polysomnography would be the next step to formally reassess the patient’s postoperative sleep-disordered breathing. This would also allow for an assessment of the patient’s CO2 to rule out any obstructive or obesity hypoventilation.
On a positive note, the mother reported that the patient was no longer snoring, mouth-breathing, or having any witnessed apneas. Likely due to the improved quality of nocturnal sleep, the patient was now sleeping in a consolidated but delayed sleep-wake phase pattern (5 am to 3 pm). The visit was spent formulating a plan for entrainment of the patient’s circadian rhythm, with telehealth making close follow-up a possibility for the family.
While the patient described had a complex presentation, every family has its own challenges. Abnormal sleep-wake schedules, difficult social situations, comorbid neuropsychiatric illnesses, the unfamiliar environment of the clinic and sleep laboratory, and school and activity schedules can all limit the ability of a family to access clinical care for sleep disorders, even in neurotypical children. In adapting to the limitations imposed by the SARS-CoV-2 pandemic, pediatric sleep practitioners may have found a way to address these pre-existing access issues.8
Children with autism spectrum disorder are at even greater risk for sleep challenges.9 Their families have increased barriers to accessing and utilizing sleep resources mainly targeted at children without developmental disabilities.9 By providing more accessible sleep consultation and testing for this population through telehealth, pediatric sleep health practitioners can support the already tremendous efforts of multidisciplinary teams caring for patients with autism spectrum disorder.4
The successful initial use of HSAT in this patient, another adaptation put in place due to the pandemic, highlights its utility as a feasible alternative to polysomnography,3–5 particularly in children with atypical neurodevelopment who already struggle with sleep.9–11 The failed postoperative HSAT demonstrates the difficulties with utilizing this technology in children. However, the next step is to embrace these challenges as opportunities to make remote sleep testing in children more comfortable and reliable, while also developing pediatric patient–centered algorithms that include home testing for diagnosis of sleep-disordered breathing.
Home-based sleep consultation and testing are not always possible and come with their own challenges and limitations. However, this case demonstrates how this approach can enhance patient- and family-centered care during a pandemic and beyond.
SLEEP MEDICINE PEARLS
1. Home-based care can enhance a family’s access to sleep providers, reduce missed school/work/therapeutic time, and allow for evaluation in a more comfortable environment for families.
2. Telemedicine allows flexibility for patients with social and/or developmental challenges to obtain care for sleep disorders.
3. Home sleep apnea testing provides an opportunity to evaluate for sleep-disordered breathing in children with neurodevelopmental challenges.
Citation: Donskoy I, Loghmanee D, Fields BG, Troester M, Martin W. Telemedicine-based sleep services for a complex child: optimizing care during a pandemic and beyond. J Clin Sleep Med. 2022;18(1):325–327.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. Institution where work was performed: Advocate Children's Hospital. The authors report no conflicts of interest.
REFERENCES
- 1. Paruthi S. Telemedicine in pediatric sleep. Sleep Med Clin. 2020; 15( 3S): e1– e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kirk V, Baughn J, D’Andrea L, et al. American Academy of Sleep Medicine position paper for the use of a home sleep apnea test for the diagnosis of OSA in children. J Clin Sleep Med. 2017; 13( 10): 1199– 1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Alonso-Álvarez ML, Terán-Santos J, Ordax Carbajo E, et al. Reliability of home respiratory polygraphy for the diagnosis of sleep apnea in children. Chest. 2015; 147( 4): 1020– 1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Scalzitti N, Hansen S, Maturo S, Lospinoso J, O’Connor P. Comparison of home sleep apnea testing versus laboratory polysomnography for the diagnosis of obstructive sleep apnea in children. Int J Pediatr Otorhinolaryngol. 2017; 100: 44– 51. [DOI] [PubMed] [Google Scholar]
- 5.Chiner E, Cánovas C, Molina V, et al. Home respiratory polygraphy is useful in the diagnosis of childhood obstructive sleep apnea syndrome. J Clin Med. 2020;9(7):2067. [DOI] [PMC free article] [PubMed]
- 6. Roland PS, Rosenfeld RM, Brooks LJ, et al. American Academy of Otolaryngology—Head and Neck Surgery Foundation. Clinical practice guideline: polysomnography for sleep-disordered breathing prior to tonsillectomy in children. Otolaryngol Head Neck Surg. 2011; 145( 1 Suppl): S1– S15. [DOI] [PubMed] [Google Scholar]
- 7. Marcus CL, Brooks LJ, Draper KA, et al. American Academy of Pediatrics. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012; 130( 3): 576– 584. [DOI] [PubMed] [Google Scholar]
- 8. Türkoğlu S, Uçar HN, Çetin FH, Güler HA, Tezcan ME. The relationship between chronotype, sleep, and autism symptom severity in children with ASD in COVID-19 home confinement period. Chronobiol Int. 2020; 37( 8): 1207– 1213. [DOI] [PubMed] [Google Scholar]
- 9. Cortesi F, Giannotti F, Ivanenko A, Johnson K. Sleep in children with autistic spectrum disorder. Sleep Med. 2010; 11( 7): 659– 664. [DOI] [PubMed] [Google Scholar]
- 10. Shahidullah JD, Azad G, Mezher KR, McClain MB, McIntyre LL. Linking the medical and educational home to support children with autism spectrum disorder: practice recommendations. Clin Pediatr (Phila). 2018; 57( 13): 1496– 1505. [DOI] [PubMed] [Google Scholar]
- 11. Primeau M, Gershon A, Talbot L, et al. Individuals with autism spectrum disorders have equal success rate but require longer periods of systematic desensitization than control patients to complete ambulatory polysomnography. J Clin Sleep Med. 2016; 12( 3): 357– 362. [DOI] [PMC free article] [PubMed] [Google Scholar]