Abstract
Aim and objective
To report the incidence of late-onset endophthalmitis following XEN45® stent implantation.
Background
Long-term safety profile and efficacy in relation to the so-called microinvasive glaucoma surgery (MIGS) techniques are still under evaluation. The XEN45® gel stent entails a bleb formation and often requires postoperative conjunctival management, differing from the current reviewed concept of minimally invasive procedures. Endophthalmitis has been described among the complications, triggered in the majority of cases by tube extrusion.
Cases description
From our chart of 293 eyes operated on between November 2016 and November 2019, five (1.7%) patients developed endophthalmitis, which took place in the months 3, 4, 5, 11, and 14 after surgery, respectively. Sixty percent had undergone previous needling procedures. All of them showed a previous flat bleb and developed perforation of the conjunctiva caused by the distal portion of the tube. One patient was early eviscerated due to a fateful course. Treatment consisted of intravitreal, oral, and topical antibiotics, as well as topical corticosteroids. Eighty percent underwent device withdrawal, conjunctival gap suturing, anterior chamber washout, aqueous humor (AH) tab extraction (one positive for S. epidermidis and one for Streptococcus agalactiae), and pars plana vitrectomy. A second patient was eviscerated due to phthisis bulbi. Out of three remaining patients, one underwent vitrectomy for retinal detachment, while two patients required glaucoma surgery for intraocular pressure control. The final VA was ≤20/125 in all patients.
Conclusion
The XEN45® device appears to trigger endophthalmitis by extruding the stent or unnoticed leakage through conjunctival defects. Special attention should be paid to flat and avascular blebs.
Clinical significance
This series shows a higher rate of endophthalmitis (1.7%) compared with previous studies with a significant sample size (0.4–1.4%).
How to cite this article
Burggraaf-Sánchez de las Matas R, Such-Irusta L, Alfonso-Muñoz EA, et al. Late-onset Endophthalmitis after XEN45® Implantation: A Retrospective Case Series and Literature Review. J Curr Glaucoma Pract 2021;15(3):153–160.
Keywords: Endophthalmitis, Microinvasive glaucoma surgery, Minimally penetrating glaucoma surgery, Needling, Retrospective case series, Safety-profile, XEN45® gel stent
Background
A large variety of new microinvasive glaucoma surgery (MIGS) techniques have been applied to glaucoma during the last two decades, aiming to decrease the comorbidity associated with classic filtering surgery. The concept of MIGS has included: procedures performed via ab interno, which provide effectiveness with a high safety profile, supposing minimal trauma to ocular tissues and rapid recovery.1 According to these statements, MIGS have been classified into four groups based on their mechanism of intraocular pressure (IOP) reduction: procedures increasing aqueous humor (AH) trabecular outflow, devices increasing suprachoroidal outflow, those entailing bleb formation for subconjunctival drainage, and procedures decreasing AH production.2,3
The XEN45® stent (Allergan, Dublin, Ireland) was approved by the FDA in 2016, consisting of a gel tube implanted from the anterior chamber into the subconjunctival space, creating a bleb. As part of the procedure, 0.1 mL of mitomycin-C (MMC) at 0.1–0.2 mg/mL or 0.1 mL of 5-fluorouracil (5-FU) at 25 mg/mL4–6 are usually injected with a 30-gauge needle under the conjunctiva.3 Postsurgical needling revision rates have been reported in up to 71%,7 but most studies have notified numbers ranging between 30% and 45%.5,8–18
The mentioned characteristics distance the XEN45® stent from the concept of MIGS. Some authors already proposed in 2018 to better classify it as an example of minimally penetrating glaucoma surgery.19 The recently published European Glaucoma Society Guidelines (5th edition) have delimitated the term MIGS to only ab interno, bleb-less forming procedures, excluding suprachoroidal and subconjunctival devices.20
As a relatively recent device, the long-term safety profile is still under evaluation. After XEN gel stent implantation, the reported intraoperative complications include intraoperative conjunctival or intraocular bleeding, need for stent relocation, or stent reimplantation. Postsurgical reported complications comprise hypotony, choroidal detachment, cyclodialysis cleft, hyphema, fibrin reaction in the anterior chamber, aqueous misdirection, IOP spikes, stent obstruction, extrusion or malposition, tube rupture, macular edema, hypotonous maculopathy, retinal detachment, central retinal vein occlusion, and endophthalmitis.4–6
XEN-related endophthalmitis has been described in single or case series reports, most of them caused by stent extrusion through the conjunctiva.21–28 This article aims to review the mechanisms, rates, bleb characteristics, the association to previous needling procedure, causative microorganisms, and management, considering our experience and the so-far previously reported cases.
Cases Description
We describe an endophthalmitis case series from a chart of 293 eyes who underwent Xen implantation between November 2016 and November 2019.
All procedures followed the principles of the Declaration of Helsinki, and we certify that informed consent was obtained from all the subjects before the surgery. Data were collected retrospectively from medical records. Patients’ data are summarized in Table 1.
Table 1.
Case series’ data
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | |
|---|---|---|---|---|---|
| Demographics | |||||
| Sex | Female | Female | Male | Male | Male |
| Age | 89 | 81 | 85 | 82 | 49 |
| Eye | Left | Left | Left | Right | Left |
| Ocular history | POAG | POAG | POAG | POAG | POAG |
| Recurrent conjunctivitis + Dacryocystitis DCR surgery | Allergic to sulfonamides | Allergic to Penicillin | RD surgery | ||
| Presurgical status | |||||
| IOP | 20 | 19 | 18 | 19 | 20 |
| VA | 20/32 | 20/40 | 20/30 | 20/25 | 20/63 |
| Previous topical hypotensive drugs | 4 drugs | 4 drugs | 2 drugs | 3 drugs | 3 drugs |
| Type of surgery | XEN45® alone | XEN45® + Phacoemulsification | XEN45® + Phacoemulsification | XEN45® alone | XEN45® + Phacoemulsification |
| Complications during surgery | Intrasurgical extrusion | Not reported | Not reported | Not reported | Not reported |
| Previous needling | Twice | Twice | Not performed | Not performed | Once |
| Months from surgery to endophthalmitis presentation | 5 | 4 | 3 | 14 | 11 |
| Mechanism | Conjunctival perforation | Conjunctival perforation | Conjunctival perforation | Conjunctival perforation | Conjunctival perforation |
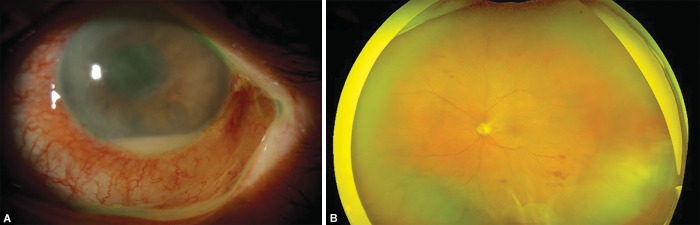
| Clinical findings | >½ AC hypopyon | Dense fibrin component | <1/3 AC hypopyon (Fig. 1A) | <1/3 AC hypopyon | Dense fibrin component |
| Culture | S. epidermidis | Negative | Negative | S. agalactiae | Negative |
| Treatment | |||||
| AB | Topical fortified | Topical | Topical | Topical | Topical |
| Intravitreal | Intravitreal | Intravitreal | Intravitreal | Intravitreal | |
| Oral | Oral | Oral | Oral | Oral | |
| CS | Topical | Topical | Topical | Topical | Topical |
| PPV | Not performed | Performed | Performed | Performed | Performed |
| Final status | |||||
| Second procedure | Eviscerated | Ahmed valve | Retinal detachment surgery (Fig. 1B) | Phthisis bulbi eviscerated | NPDS |
| AV | 20/400 | 20/400 | 20/125 | ||
| IOP | 20 | 12 | 14 | ||
| Hypotensive drugs | 2 | 2 | 0 | ||
| Mean follow-up Time (months) | 6 | 23 | 17 | 29 | 25 |
POAG, primary open angle glaucoma; DCR, dacryocystorhinostomy; RD, retinal detachment; AC, anterior chamber; MMC, mitomycin C; AB, antibiotics; CS, corticosteroids; PPV, Pars plana vitrectomy; HM, hand motion; NPDS, non-penetrating deep sclerectomy; VA, visual Acuity
Sample Description
Five eyes suffered endophthalmitis in the months 3, 4, 5, 11, and 14 after surgery. The patient's age ranged from 49 to 89 years. The indication for surgery was mild to moderate primary open-angle glaucoma (POAG), not responding and/or not tolerating topical drugs. Previous ocular history included recurring conjunctivitis and dacryocystorhinostomy in patient 1, and retinal detachment surgery in patient 5.
Ocular History
The mean preoperative IOP was 19 ± 3 mm Hg on 3 ± 1 drugs. Two different surgeons performed the procedures, taking place in July 2018, October 2018, January 2019, February 2019, and June 2019.
Isolated XEN45® implantation was performed in patients 1 and 4. The remaining patients underwent combined XEN45® implantation and phacoemulsification with intraocular lens implantation. A 0.1-mL injection of subconjunctival mitomycin-C (0.02%) was utilized as an anti-fibrotic agent. An intraoperative device extrusion was recorded in patient 1, who underwent second device implantation and suturing of the conjunctiva in the same surgical act. A second device was implanted in patient 5 in the same sitting, who showed a highly scarred conjunctiva due to previous retinal detachment surgery, and there was no bleb formation observed in the first attempt.
One hundred sixty-four (60%) eyes required needling during follow-up due to surgical failure before the endophthalmitis developed. The needling procedure was carried out with mitomycin-C (0.01%). All these patients had a previous flat bleb.
Endophthalmitis Findings
At the time of presentation, the clinical findings were perforation of the conjunctiva caused by the distal portion of the tube in all the patients. Two patients exhibited clear cornea, anterior chamber cells with a dense fibrin reaction, while three presented corneal edema, hypopyon (Fig. 1A), and flare. Only patient 1 presented signs of blebitis, visualizing purulent secretion around the conjunctival gap.
Figs 1A and B.
Findings corresponding to patient 3. (A) Anterior segment photography shows corneal edema and 1.2 mm hypopyon at day 1 of presentation; (B) Ultra-widefield retinography demonstrates several retinal hemorrhages and inferior retinal detachment after the first PPV procedure
Management
Antibiotic therapy was initiated with hourly drops of fortified ceftazidime (5%) and vancomycin (5%) for patient 1, presenting with signs of blebitis, while the others received moxifloxacin (0.5%) hourly. Intravitreal injections of vancomycin (1 mg/0.1 mL) and ceftazidime (2 mg/0.1 mL) were given to all patients, except for patient 4, who received amikacin (0.5 mg/0.1 mL) instead of ceftazidime due to a penicillin allergy. Oral linezolid (600 mg every 12 hours) was administered to all patients. The corticosteroid therapy consisted of topical dexamethasone 0.1% drops four times a day for all patients.
A control visit after 48 hours revealed no improvement with a fateful course in patient 1, presenting VA of no light perception (LP), pancorneal epithelial ulcer, and stromal thinning with severe pain. This patient underwent evisceration after 1 week post-infection. The rest of the patients received scheduled surgery for AH tap extraction, device withdrawal, anterior chamber washout, and central core pars plana vitrectomy (PPV).
Aqueous humor samples were introduced in a thioglycollate medium and sent to the Microbiology Department to obtain the causative agent. Positive results were obtained in two patients: S. epidermidis (penicillin-resistant but sensible to tobramycin and vancomycin) in patient 1 and Streptococcus agalactiae (sensible to vancomycin) in patient 4.
Final Status and Further Surgeries
The follow-up time from surgery ranged from 6 to 29 months (mean follow-up time of 20 months).
Apart from patient 1, patient 4 also required evisceration in due course due to phthisis bulbi. Patients 2 and 5 developed raised IOP in the postoperative period and underwent second glaucoma surgery. Patient 2 underwent Ahmed valve implant while patient 5 underwent non-penetrating deep sclerotomy. Patient 3 suffered a retinal detachment (Fig. 1B) and underwent a second PPV. The final VA in these three patients was ≤20/125, and the mean was IOP 16.5 ± 2.5 mm Hg.
Patients 2 and 3 required two further hypotensive topical drugs (patient 2 even after Ahmed valve implantation).
Discussion
Taking classic surgery as a frame of reference, the incidence of endophthalmitis after a trabeculectomy appears to vary in previous studies between 0.17 and 13.2%. This may be due to differences in sample sizes, surgical techniques, and follow-up period. The US study found a 5-year cumulative incidence ranging from 0.45 to 1.3% in 1,461 glaucoma filtering surgeries.29 With the introduction of antimetabolites in the 1990s, an increase in infections was observed. However, new studies have proven that the incidence has been reduced due to improved surgical techniques.30,31
Regarding glaucoma drainage devices (GDDs), the rate of endophthalmitis ranges from 0.5 to 5%.32 The tube vs trabeculectomy study showed a higher rate of infection in the trabeculectomy group, but the sample size limited it, and the results could not be reported as statistically significant.33
Being a recently introduced device, literature is scarce regarding endophthalmitis episodes after XEN45® implantation. Reported endophthalmitis rates vary from 0.4 to 3%,5,6,15,34–36 after a maximum follow-up of 35.8 months. The superior boundary of this range corresponds to the calculated rate in a retrospective study performed by Başer and Seymenoğlu, including only 29 eyes to evaluate the effectiveness and safety of 5-fluorouracil as an anti-fibrotic agent.36 If we consider larger sample sizes, the highest rate would be 1.4%, as reported by Ibáñez-Muñoz et al. in a retrospective study comprising 74 eyes.35
The mechanism behind infectious complications in glaucoma surgery varies according to the procedure. After trabeculectomy, the infection is usually produced due to the thinning of the bleb and leakage. GDD-associated episodes are produced due to the tube's exposure after the erosion of the overlying Tenon's fascia and conjunctiva. The tube serves as a conduit by which host flora may pass from the ocular surface into the eye.37
The gel stent can trigger both mechanisms, which could explain the higher rate of endophthalmitis in a shorter period. Concerning trabeculectomy, the meantime from the procedure to the diagnosis of endophthalmitis was 33 months in the US study,29 while infections in our case series appeared after a mean time of 7.4 months. Regarding GDD, Al-Torbak et al.38 observed a median interval of 206 days (range 63–330 days) between Ahmed valve implant surgery and diagnosis of endophthalmitis, while we found infection after a median interval of 150 days.
To evaluate specific characteristics of endophthalmitis associated with the XEN device, we reviewed the cases published so far in the PubMed database (Patients’ data are summed up in Table 2). Infections took place ranging from 3 to 24 months postoperatively. The first case was reported by Lim and Lim in February 2018, describing stent extrusion through a conjunctival gap.21 Most authors have suggested conjunctival erosion and/or tube extrusion as the triggering mechanism of infection, often related to flat blebs.22–28 Only three cases cited no visible conjunctival epithelial defect nor leakage: one corresponding to an avascular bleb,27 one reporting impossibility to evaluate the bleb area due to intense inflammation during the presentation,39 and the one remaining to visualize a necrotic scleral patch under the stent position.25 Then, the second mechanism would entail susceptible thin avascular blebs, in which leakage defects may go unnoticed.
Table 2.
Characteristics of previously reported endophthalmitis associated with XEN45®
| Authors | Number of cases | Months following surgery | Previous needling procedure | Bleb | Mechanism | Culture | Initial medical treatment | PPV | Final result |
|---|---|---|---|---|---|---|---|---|---|
| Lim and Lim (2018)21 | 1 | 11 | NM` | NM | Extrusion | NM | NS | No | NM |
| Karri et al. (2018)22 | 1 | 4 | No | Shallow bleb | Extrusion | Enterococcus faecalis | IV vancomycin and ciprofloxacin | Performed | VA = 20/125 |
| Topical chloramphenicol | IOP = 21 | ||||||||
| Oral ciprofloxacin | HD = 0 | ||||||||
| Topical prednisolone | |||||||||
| Lapira et al. (2018)23 | 1 | 3.5 | No | Shallow bleb | Extrusion | Negative | IV vancomycin and ceftazidime | Performed | VA = 20/50 |
| Topical moxifloxacin | IOP = 20 | ||||||||
| Oral moxifloxacin | HD* = 3 | ||||||||
| Oral prednisolone | |||||||||
| Colás-Tomás and Pérez-Trigo (2018)39 | 1 | 8 | Performed with MMC | Flat bleb | No conjunctival erosion visualized | Streptococcus oralis | IV vancomycin and ceftazidime | Not performed | Enucleated |
| Scleral necrosis | Oral ciprofloxacin | ||||||||
| Olgun et al. (2018)27 | 2 | 5 | No | Avascular bleb | No conjunctival erosion visualized | Negative | IV vancomycin and ceftazidime | Performed | VA = HM |
| Topical vancomycin and ceftazidime | IOP = 15 | ||||||||
| Oral ciprofloxacin | HD = 0 | ||||||||
| 4 | No | Flat bleb | Extrusion | Negative | NM | Performed | VA = 20/400 | ||
| IOP = 20 | |||||||||
| HD = 0 | |||||||||
| Kerr et al. (2018)25 | 3 | 8 | No | Avascular bleb | Extrusion | Staphylococcus aureus | Topical moxifloxacin | Not performed | VA = 20/32 |
| Signs of blebitis | Oral moxifloxacin | IOP = 18 | |||||||
| Topical dexamethasone | HD = 2 | ||||||||
| 7 | No | NM | No conjunctival erosion visualized | Moraxella nonliquefaciens | Topical moxifloxacin | Performed | VA = 20/40 | ||
| XEN exposure 4 months earlier | Oral moxifloxacin | IOP = 19 | |||||||
| Topical dexamethasone | HD = 2 | ||||||||
| 24 | No | Avascular bleb | Conjunctival erosion | Negative | IV vancomycin and amikacin | Performed | VA = 20/63 | ||
| Topical moxifloxacin | IOP = 10 | ||||||||
| Oral moxifloxacin | HD = 0 | ||||||||
| Topical and IV dexamethasone | |||||||||
| Oral prednisolone | |||||||||
| Napoli et al. (2019)24 | 1 | 3 | Performed with 5-FU | Flat bleb | Extrusion | Sphingobacterium spiritivorum | IV vancomycin and amikacin | Performed | VA = 20/200 |
| History of trauma with a vegetable twig | Topical fortified ceftazidime | IOP = 15 | |||||||
| Intravenous meropenem | HD = 0 | ||||||||
| Oral cotrimoxazole | |||||||||
| Buffault et al. (2020)26 | 1 | 21 | No | Avascular | Extrusion | Streptococcus pneumoniae | IV vancomycin and ceftazidime | Not performed | Eviscerated |
| Flat bleb | Topical fortified vancomycin, piperacillin, and gentamicin | ||||||||
| Imipenem | |||||||||
| Oral levofloxacin | |||||||||
| Intravenous methylprednisolone | |||||||||
| Moussaoui et al. (2020)28 | 1 | 3 | No | Flat bleb | Extrusion | Abiotrophia | IV vancomycin and ceftazidime | Performed | VA = 20/50 |
| Defective | Topical moxifloxacin | IOP = 16 | |||||||
| (Nutritionally variant streptococci) | Intravenous vancomycin and ceftazidime | HD = 2 | |||||||
| IV dexamethasone |
PPV, pars plana vitrectomy; NM, not mentioned; NS, not specified; IV, intravitreal; VA, visual acuity; HD, hypotensive drugs; MMC, mitomycin-C, HM, hand motion; 5-FU, 5-fluorouracil
Needling procedure was performed in two out of twelve (17%) of the previously reported patients, as opposed to three out of five patients (60%) in our series. Due to this variability, we cannot establish a direct association between needling and a higher threat of posterior stent extrusion. Despite that, we attribute a higher risk of endophthalmitis to flat blebs, which are most likely to require needling procedures.40 It should be kept in mind that the use of anti-fibrotic agents for bleb revision would also increase the rates of vulnerable avascular blebs.
Lenzhofer et al., who have reported the highest rate of needling post-XEN to date, studied the relationship between stent position and final IOP. They postulate that a deeper location of the stent would avoid bleb leaks and bleb-related endophthalmitis and suggest that a correct intrasurgical hydrodissection of the conjunctiva and Tenon layers from deeper structures would facilitate better tube positioning.7
Considering causative agents, the Streptococcus species were identified as the most common pathogens in BRE after filtering surgery. Yamamoto et al. analyzed prospectively 170 bleb-related infections between 2005 and 2010 in Japan, reporting 54.7% of positive cultures among the intraocular tapping samples: 51.7% for Streptococcus, 13.7% for Staphylococcus, 10.3% for Enterococcus, and 6.9% for the Haemophilus species.41 Jin Kwon et al. reviewed 67 cases of BRE between 1997 and 2015 in Australia. The rate of positive cultures was 71.6%: 43.8% of them were Streptococcus, 20.8% Moraxella, 14.6% Staphylococcus, 10.4% Haemophilus, and 6.3% of the Enterococcus species,32 although we have to consider that 22% of the positive results were obtained from conjunctival swabs.
Regarding the previous XEN-related reported cases (Table 2), 58.3% exhibited a positive culture. Of them, 57.1% were gram-positive [Staphylococcus aureus, Streptococcus oralis, Streptococcus pneumoniae, and Abiotrophia defective (nutritionally variant streptococci)]. In comparison, the other 42.9% were gram-negative bacteria (Enterococcus faecalis, Sphingobacterium spiritivorum, and Moraxella nonliquefaciens). In our series, we obtained 40% of positive cultures, all of them corresponding to gram-positive bacteria, one for S. agalactiae and another for S. aureus (Table 1). Combining our results with the previously published reports, the Streptococcus species appears as the most frequent pathogen (44.4% of the whole positive cultures) among the XEN-related endophthalmitis.
The decision to perform immediate PPV to manage endophthalmitis has been properly studied relating to acute episodes following cataract surgery. The prospective, randomized, multicenter Endophthalmitis Vitrectomy Study (EVS) was recommended in 1995 to perform core vitrectomy in cases presenting decreased VA to LP.42 Several years later, Kuhn and Gini proposed complete PPV in patients suffering from acute postphacoemulsification endophthalmitis, presenting abnormal reflex or not responding to initial medical therapy within the first 24 hours, based on consecutive series of 47 patients in which 91% resulted in a VA of 20/40 or better after the intervention.43
There is no definite consensus regarding BRE. Episodes following glaucoma surgery use tend to be late-onset endophthalmitis, and little literature for decision-making is found. In the study performed by Al-Turki et al. in 2010, 32% received initial PPV. Poorer final visual outcomes were found among non-vitrectomized patients (25.5% presenting final VA of no LP) vs vitrectomized patients (16.7% presenting VA of no LP), but these percentages were not statistically significant.44 In 2015, Ohtomo et al. reported a median value for VA of 20/125 after PPV in 11 patients suffering endophthalmitis following trabeculectomy, but there was no comparative group.45 A more recent retrospective series published by Negretti et al. reported the results after performing early PPV in several kinds of endophthalmitis. From the patients included, five cases followed glaucoma surgery: one after XEN implant, three after trabeculectomy, and one associated with the drainage tube. The visual outcomes in this specific group improved by 80% after PPV, but the results were not statistically significant.46 Therefore, clear indications and protocols are still to be determined.
Nevertheless, let us analyze XEN-related cases from our series (patient 1–Table 1) and the previously published reports (Table 2). We observe that the final visual outcomes are quite variable. Still, as a remarkable fact, 100% of the non-vitrectomized cases were early eviscerated or enucleated,26,39 suggesting a clear benefit of performing early PPV on such patients.
As a specific forethought in our series, we considered our episodes not to be surgeon-dependent, and we dismissed association to any device defect, given that the endophthalmitis developed at different periods postoperatively and that the surgeries were performed in different months between July 2018 and June 2019.
Limitations of this review include the retrospective analysis of our cases and the heterogeneity of clinical data among the other reviewed reports. We cannot yet estimate a mean incidence, considering that only our series report a percentage, while the literature is limited to descriptive reports, and other authors have not indicated the rates of endophthalmitis about XEN.
Conclusion
Endophthalmitis about the subconjunctival device XEN45® exhibits the typical characteristics of bleb-related infections: it can debut at any moment after the initial surgery, and thinner blebs are more vulnerable. In addition, the stent remains as a foreign body under the conjunctiva, associating the threat of tube extrusion similarly to drainage devices. Consequently, the safety profile in terms of infection resembles the one previously reported in non-MIGS procedures but developing earlier during follow-up. A careful XEN position surveillance should be carried out, especially in those cases presenting flat or avascular blebs, which have the highest risk of presenting endophthalmitis.
Clinical Significance
The calculated rate of endophthalmitis in our chart of 293 operated eyes reaches 1.7%, which is higher than numbers reported in previous studies with a significant sample size (0.4–1.4%). This case series highlights the necessity of bleb supervision in patients undergoing XEN45® stent implantation.
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Achiron A, Sharif N, Achiron RNO, et al. Micro-invasive glaucoma surgery. Harefuah. 2014;153(10):625–685. [PubMed] [Google Scholar]
- 2.Richter GM, Coleman AL. Minimally invasive glaucoma surgery: Current status and future prospects. Clin Ophthalmol. 2016;10:189–206. doi: 10.2147/OPTH.S80490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nichani P, Popovic MM, Schlenker MB, et al. Microinvasive glaucoma surgery: a review of 3476 eyes. Surv Ophthalmol. 2021;66(5):714–742. doi: 10.1016/j.survophthal.2020.09.005. [DOI] [PubMed] [Google Scholar]
- 4.Fea AM, Durr GM, Marolo P, et al. Xen® gel stent: a comprehensive review on its use as a treatment option for refractory glaucoma. Clin Ophthalmol. 2020;14:1805–1832. doi: 10.2147/OPTH.S178348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karimi A, Lindfield D, Turnbull A, et al. A multi-centre interventional case series of 259 ab-interno Xen gel implants for glaucoma, with and without combined cataract surgery. Eye. 2019;33(3):469–477. doi: 10.1038/s41433-018-0243-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heidinger A, Schwab C, Lindner E, et al. A retrospective study of 199 Xen45 stent implantations from 2014 to 2016. J Glaucoma. 2019;28(1):75–79. doi: 10.1097/IJG.0000000000001122. [DOI] [PubMed] [Google Scholar]
- 7.Lenzhofer M, Strohmaier C, Sperl P, et al. Effect of the outer stent position on efficacy after minimally invasive transscleral glaucoma gel stent implantation. Acta Ophthalmol. 2019;97(8):e1105–e1111. doi: 10.1111/aos.14167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galal A, Bilgic A, Eltanamly R, et al. XEN glaucoma implant with mitomycin C 1-year follow-up: result and complications. J Ophthalmol. 2017:545–546. doi: 10.1155/2017/5457246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schlenker MB, Gulamhusein H, Conrad-Hengerer I, et al. Efficacy, safety, and risk factors for failure of standalone ab interno gelatin microstent implantation versus standalone trabeculectomy. Ophthalmology. 2017;124(11):1579–1588. doi: 10.1016/j.ophtha.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 10.Grover DS, Flynn WJ, Bashford KP, et al. Performance and safety of a new ab interno gelatin stent in refractory glaucoma at 12 months. Am J Ophthalmol. 2017;183:25–36. doi: 10.1016/j.ajo.2017.07.023. [DOI] [PubMed] [Google Scholar]
- 11.Widder RA, Dietlein TS, Dinslage S, et al. The XEN45 gel stent as a minimally invasive procedure in glaucoma surgery: success rates, risk profile, and rates of re-surgery after 261 surgeries. Graefe's Arch Clin Exp Ophthalmol. 2018;256(4):765–771. doi: 10.1007/s00417-018-3899-7. [DOI] [PubMed] [Google Scholar]
- 12.Mansouri K, Guidotti J, Rao HL, et al. Prospective evaluation of standalone XEN gel implant and combined phacoemulsification-XEN gel implant surgery: 1-year results. J Glaucoma. 2018;27(2):140–147. doi: 10.1097/IJG.0000000000000858. [DOI] [PubMed] [Google Scholar]
- 13.Kalenak JW. Performance and safety of a new ab interno gelatin stent in refractory glaucoma at 12 months. Am J Ophthalmol. 2018;188:185–186. doi: 10.1016/j.ajo.2018.01.031. [DOI] [PubMed] [Google Scholar]
- 14.De Gregorio A, Pedrotti E, Stevan G, et al. XEN glaucoma treatment system in the management of refractory glaucomas: a short review on trial data and potential role in clinical practice. Clin Ophthalmol. 2018;12:773–782. doi: 10.2147/OPTH.S146919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reitsamer H, Sng C, Vera V, et al. Two-year results of a multicenter study of the ab interno gelatin implant in medically uncontrolled primary open-angle glaucoma. Graefe's Arch Clin Exp Ophthalmol. 2019;257(5):983–996. doi: 10.1007/s00417-019-04251-z. [DOI] [PubMed] [Google Scholar]
- 16.Smith M, Charles R, Abdel-Hay A, et al. Performance and safety of a new ab interno gelatin stent in refractory glaucoma at 12 months. J Glaucoma. 2019;33(5):983–996. [Google Scholar]
- 17.Gillmann K, Bravetti GE, Mermoud A, et al. XEN gel stent in pseudoexfoliative glaucoma: 2-year results of a prospective evaluation. J Glaucoma. 2019;28(8):676–684. doi: 10.1097/IJG.0000000000001295. [DOI] [PubMed] [Google Scholar]
- 18.Smith M, Charles R, Abdel-Hay A, et al. 1-year outcomes of the Xen45 glaucoma implant. Eye. 2019;33(5):761–766. doi: 10.1038/s41433-018-0310-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.García-Feijóo J, Larrosa JM, Martínez-de-la-Casa JM, et al. Redefiniendo la cirugía de glaucoma mínimamente invasiva. Cirugía mínimamente penetrante. Arch Soc Esp Oftalmol. 2018;93(4):157–159. doi: 10.1016/j.oftal.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 20.European Glaucoma Society Terminology and Guidelines for Glaucoma, 5th ed., Chapter 3: Treatment principles and options Supported by the EGS Foundation. 2020. [DOI] [PMC free article] [PubMed]
- 21.Lim R, Lim KS. XEN implant-related endophthalmitis. Ophthalmology. 2018;125(2):209. doi: 10.1016/j.ophtha.2017.10.019. [DOI] [PubMed] [Google Scholar]
- 22.Karri B, Gupta C, Mathews D. Endophthalmitis following XEN stent exposure. J Glaucoma. 2018;27(10):931–933. doi: 10.1097/IJG.0000000000001012. [DOI] [PubMed] [Google Scholar]
- 23.Lapira M, Cronbach N, Shaikh A. Extrusion and breakage of XEN gel stent resulting in endophthalmitis. J Glaucoma. 2018;27(10):934–935. doi: 10.1097/IJG.0000000000001058. [DOI] [PubMed] [Google Scholar]
- 24.Napoli L, Riva I, Oddone F, et al. A rare case of endophthalmitis after bleb needle revision for glaucoma Xen® gel stent. Eur J Ophthalmol. 2019:2–5. doi: 10.1177/1120672119878016. [DOI] [PubMed] [Google Scholar]
- 25.Kerr NM, Wang J, Sandhu A, et al. Ab interno gel implant–associated bleb-related infection. Am J Ophthalmol. 2018;189:96–101. doi: 10.1016/j.ajo.2018.02.014. [DOI] [PubMed] [Google Scholar]
- 26.Buffault J, Baudouin C, Labbé A. Is the Xen® gel stent really minimally invasive? Am J Ophthalmol Case Rep. 2020;19:100850. doi: 10.1016/j.ajoc.2020.100850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Olgun A, Imamoğlu S, Karapapak M, et al. Endophthalmitis after XEN gel stent implantation: 2 cases. J Glaucoma. 2018;27(12):E191–E194. doi: 10.1097/IJG.0000000000001076. [DOI] [PubMed] [Google Scholar]
- 28.Moussaoui LE, Djalali-Talab Y, Walter P, et al. Endophthalmitis nach bindehautperforation eines glaukom-gelstentimplantates [endophthalmitis after perforation of the conjunctiva by a glaucoma gel-stent implant]. Ophthalmologe. 2020;117(12):1229–1233. doi: 10.1007/s00347-020-01077-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vaziri K, Kishor K, Schwartz SG, et al. Incidence of bleb-associated endophthalmitis in the United States. Clin Ophthalmol. 2015;9:317–322. doi: 10.2147/OPTH.S75286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Greenfield DS, Suñer IJ, Miller MP, et al. Endophthalmitis after filtering surgery with mitomycin. Arch Ophthalmol. 1996;114(8):943–949. doi: 10.1001/archopht.1996.01100140151007. [DOI] [PubMed] [Google Scholar]
- 31.Rai P, Kotecha A, Kaltsos K, et al. Changing trends in the incidence of bleb-related infection in trabeculectomy. Br J Ophthalmol. 2012;96(7):971–975. doi: 10.1136/bjophthalmol-2011-300926. [DOI] [PubMed] [Google Scholar]
- 32.Kwon HJ, Kumar H, Green CM, et al. Bleb-associated endophthalmitis: proportion, presentation, management and outcomes in Victoria, Australia. Clin Exp Ophthalmol. 2019;47(5):588–597. doi: 10.1111/ceo.13477. [DOI] [PubMed] [Google Scholar]
- 33.Gedde SJ, Herndon LW, Brandt JD, et al. Postoperative complications in the tube versus trabeculectomy (TVT) study during five years of follow-up. Am J Ophthalmol. 2012;153(5):804–814. doi: 10.1016/j.ajo.2011.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Linton E, Au L. Technique of Xen implant revision surgery and the surgical outcomes: a retrospective interventional case series. Ophthalmol Ther. 2020;9(1):149–157. doi: 10.1007/s40123-020-00234-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ibáñez-Muñoz A, Soto-Biforcos VS, Rodríguez-Vicente L, et al. XEN implant in primary and secondary open-angle glaucoma: a 12-month retrospective study. Eur J Ophthalmol. 2020;30(5):1034–1041. doi: 10.1177/1120672119845226. [DOI] [PubMed] [Google Scholar]
- 36.Başer EF, Seymenoğlu RG. Results of fluorouracil-augmented Xen45 implantation in primary open-angle and pseudoexfoliation glaucoma. Int Ophthalmol. 2021;41(3):945–955. doi: 10.1007/s10792-020-01650-8. [DOI] [PubMed] [Google Scholar]
- 37.Gedde SJ, Scott IU, Tabandeh H, et al. Late endophthalmitis associated with glaucoma drainage implants. Ophthalmology. 2001;108(7):1323–1327. doi: 10.1016/s0161-6420(01)00598-x. [DOI] [PubMed] [Google Scholar]
- 38.Al-Torbak AA, Al-Shahwan S, Al-Jadaan I, et al. Endophthalmitis associated with the Ahmed glaucoma valve implant. Br J Ophthalmol. 2005;89(4):454–458. doi: 10.1136/bjo.2004.049015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Colás-Tomás T, Pérez-Trigo S. Delayed-onset endophthalmitis following implantation of a XEN45 glaucoma device: a case report. J Glaucoma. 2018;27(10):936–938. doi: 10.1097/IJG.0000000000001064. [DOI] [PubMed] [Google Scholar]
- 40.Vera V, Sheybani A, Lindfield D, et al. Recommendations for the management of elevated intraocular pressure due to bleb fibrosis after XEN gel stent implantation. Clin Ophthalmol. 2019;13:679–684. doi: 10.2147/OPTH.S195457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yamamoto T, Kuwayama Y, Kano K, et al. Clinical features of bleb-related infection: a 5-year survey in Japan. Acta Ophthalmol. 2013;91(7):619–624. doi: 10.1111/j.1755-3768.2012.02480.x. [DOI] [PubMed] [Google Scholar]
- 42.Results of the Endophthalmitis Vitrectomy Study. A randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Endophthalmitis vitrectomy study group. Arch Ophthalmol. 1995;113(12):1479–1496. doi: 10.1001/archopht.1995.01100120009001. [DOI] [PubMed] [Google Scholar]
- 43.Kuhn F, Gini G. In: Vitreo-retinal surgery. Essentials in ophthalmology. 1st ed., Kirchhof B, Wong D, et al., editors. Berlin, Heidelberg: Springer; 2007. Complete and early vitrectomy for endophthalmitis (CEVE) as today's alternative to the endophthalmitis vitrectomy study. pp. 53–68. [Google Scholar]
- 44.Al-Turki TA, Al-Shahwan S, Al-Mezaine HS, et al. Microbiology and visual outcome of bleb-associated endophthalmitis. Ocul Immunol Inflamm. 2010;18(2):121–126. doi: 10.3109/09273940903370730. [DOI] [PubMed] [Google Scholar]
- 45.Ohtomo K, Mayama C, Ueta T, et al. Outcomes of late-onset bleb-related endophthalmitis treated with pars plana vitrectomy. J Ophthalmol. 2015;2015:923857. doi: 10.1155/2015/923857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Negretti GS, Chan W, Pavesio C, et al. Vitrectomy for endophthalmitis: 5-year study of outcomes and complications. BMJ Open Ophthalmol. 2020;5(1):1–8. doi: 10.1136/bmjophth-2019-000423. [DOI] [PMC free article] [PubMed] [Google Scholar]