Abstract
Introduction and importance
Thoracic outlet syndrome (TOS) is a rare syndrome caused by compression of one of the three neurovascular structures in their passage from the cervical area toward the axilla and proximal arm either at the interscalene triangle, the costoclavicular triangle, or the sub coracoid space. The mainstay of management is nonsurgical; however, surgery may be needed when patients persist with symptoms despite conservative management and when vascular structures are involved. Symptoms are non-specific and require high clinical awareness since this pathology tends to affect otherwise healthy young patients.
Case presentation
We present the case of a 45-year-old female without any past medical history. She was active and did plenty of exercises. After a high-intensity routine without any guidance, she presented with acute upper limb swelling with pain. After further examination, a venous thoracic outlet syndrome was identified and treated without complications.
Clinical discussion & conclusion
Venous TOS is a rare pathology associated with high long-term morbidity and disability if left untreated; heightened clinical awareness of the possibility of acute thrombosis obstructing venous return and producing these rare symptoms should lead the medical team to assess the patient further and lead to the appropriate medical and surgical intervention.
Keywords: Thoracic outlet syndrome (TOS), Venous TOS, Subclavian vein thrombosis, Paget-Schroetter syndrome
Highlights
-
•
Venous TOS is a rare pathology associated with morbidity and disability if left untreated.
-
•
Due to its broad spectrum of clinical symptoms, it continues to be a challenge to the medical team
-
•
This disorder can affect the subclavian artery, vein, or brachial plexus, resulting in different syndromes.
1. Introduction
Thoracic outlet syndrome occurs when the neurovascular bundle is structurally compromised between the first rib and collar bone [1], [2]. This disorder can affect the subclavian artery, vein, or brachial plexus resulting in different syndromes with broad clinical presentation [2], [3]. Chronic compression can lead to inflammation, scarring and ultimately thrombosis of the subclavian vein, leading to long-term morbidity and disability if left untreated [4]. Therefore, prevention, well-planned exercise routine, quick diagnosis, and treatment of this rare pathology are essential to prevent these troublesome complications [1], [4].
We present the case of a 45-year-old female who developed venous thoracic outlet syndrome after a non-guided exercise routine. After surgical treatment, the patient completely recovered.
The work has been reported in line with the SCARE criteria [11].
2. Case report
Patient is a healthy 45-year-old female. She did countless exercises throughout her life, and she started a new high-intensity training on her own, gaining over 10-pounds in two years, most of it on her shoulders and arms. Suddenly she noticed acute-onset swelling and mild pain in her right upper extremity during an exercise routine; she stopped training and was evaluated by her primary care physician. She was advised to discontinue exercise and put ice on her upper limb. After 48 h, the symptoms and signs completely subsided, and ten days after this incident, she returned to her conventional routine.
Fifteen days passed, and she appeared to be completely normal. Then abruptly, an identical episode occurred during an exercise routine; this time, the pain was severe; thus, she was brought immediately to the emergency room.
Clinical examination revealed a cyanotic and swollen right arm; she showed paresthesia and general weakness (4/5) of all muscles in the right upper extremity. However, her left extremity appeared normal, and after 48 h, the weakness persisted, but the swelling in her right arm reverted to normal. Wright's hyperabduction test was positive, causing cyanosis and obliteration of the radial pulse in her right arm. Further, examination revealed normal skin sensation and normal deep tendon reflexes for her biceps and triceps, with no symptoms related to her cervical spine. Thoracic outlet syndrome was suspected, but color Doppler sonography was inconclusive, failing to visualize the whole subclavian vein. With these findings, a contrast venogram of her upper right limb revealed a near-complete obstruction at the subclavian vein, venous stenosis, and concomitant thrombosis from the axillary vein to the subclavian vein (Fig. 1A & B). A computed tomography, electromyogram, and a nerve conduction study were completed to rule out concurrent neurogenic thoracic outlet syndrome, but no abnormalities were discovered (Fig. 2).
Fig. 1.
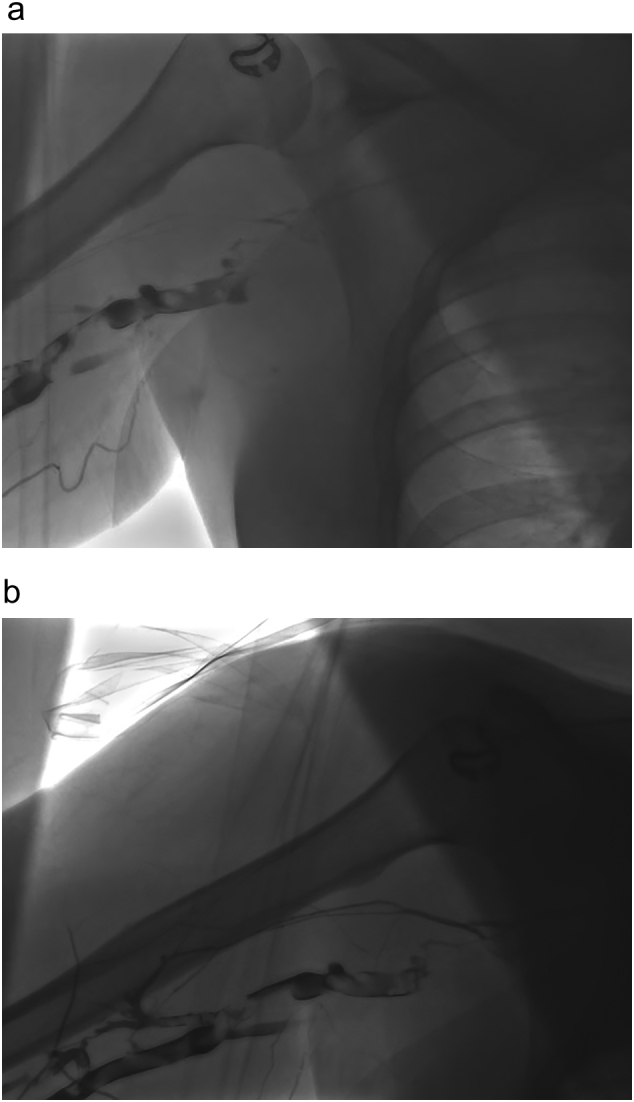
A: Venogram, showing obstruction at the level of the subclavian vein.
B: Venogram, multiple thrombi are seen in the axillary vein and subclavian vein.
Fig. 2.

Contrast enhanced CT, showing near complete obstruction in the subclavian vein.
Venous thoracic outlet syndrome was the final diagnosis, and surgical treatment was decided. Nevertheless, the patient refused any surgical intervention, and she asked to be discharged against medical advice. Seven months passed, and the patient persisted with these symptoms; she couldn't practice any sport and had severe pain.
Thus, the patient underwent subclavicular first rib resection. The first rib was dissected and sectioned to allow complete decompression. Surgical resection of the scalene muscles was also completed allowing the costoclavicular space to be completely free. The rest of the procedure was completed without any complications (Fig. 3).
Fig. 3.

Chest X-ray during postoperative period.
Her postoperative course was uneventful, and she was discharged on her second postoperative day once the pain was controlled. She began a one-week course of low-weight heparin, followed by a one-month warfarin regimen. On follow-ups, the patient is doing well; she resumed her regular training this time with a personal trainer and has not experienced pain or swelling in over two years.
3. Discussion
Thoracic outlet syndrome (TOS), described by Paget in 1857 [1], results from the compression of one of the three neurovascular structures in the interscalene triangle; brachial plexus, subclavian vein, or subclavian artery [1], [2]. Patients present with symptoms depending on the involved anatomical structure [3]. The neurogenic thoracic syndrome is the most common (90–95%), followed by venous (5%) and arterial (1%) [1], [3]. There have been multiple names describing the condition in which vein is compromised, and a thrombus appears, such as Paget-Schroetter or McCleery syndrome; however, it's essential to distinguish them both [4]. Primary effort thrombosis (Paget-Schroetter) appears when a thrombus in the subclavian vein is formed due to its chronic compression [2], [5]. McCleery syndrome occurs due to an intermittent obstruction but without thrombosis [1], [2]. These events happen due to the subclavian vein's repeated compression inside a triangle bordered by the first rib, clavicle, and the subclavius muscle, leading to injury, inflammation, and eventual thrombosis [3].
Venous TOS is rare, with an incidence of 1 every 100,000 adults; it usually affects active middle-aged men, with a predominance of 2:1 over females [1], [6]. The right arm is most often involved due to the worldwide dominance of right-handed people [1]. Athletes are at higher risk because they perform repetitive upper extremity movements, such as swimming or lifting weights [2], [7]. Other causes include congenital bone structures, fibromuscular anomalies, and posture [1], [7]. In our case, our patient was active and started high-intensity training on her own, which may have caused the compression of her subclavian vein.
Patients usually present with a cyanotic and swollen upper extremity after exercise or carrying heavy objects; on occasions, dilated superficial veins over the upper arm, neck, and chest can also be seen [8].
Pain is usually accompanied by numbness, tingling, weakness, or discoloration [2], [7], as our patient experienced.
Diagnosis is made by clinical history, physical examination, and imaging studies, usually a venous duplex ultrasound [2], [4]. Lymphedema, Raynaud disease, vasculitis, Pancoast tumor, or malignancy must be among the differential [1], [6]. Duplex ultrasound has high sensitivity (78%) and specificity (82%), but it is challenging to observe the costoclavicular region [2], [3]. Contrast venography can be used in patients with high clinical suspicion and a negative Duplex test or when an endovascular intervention is planned [2], [5]. An obstruction or more than 50% is an indication for intervention [1].
Other imaging methods like CT or magnetic resonance venogram can also give more anatomic details [9] as it was done in our patient. Treatment is based on anticoagulation and thrombolysis; nonetheless, poor outcomes (29%), including recurrent thrombosis, disability, and persistent symptoms, have made surgical intervention the treatment of choice [1], [3]. Other treatment techniques include catheter-directed thrombolysis or angioplasty [2], [3], [4].
First rib resection and scalenectomy described by Roos et al. in 1965 allow complete decompression of the thoracic outlet [4], [9]. However, some patients may already have a vein defect that, even after surgery, could develop vein injury, fibrosis, and scars [1], [10]. Therefore, venolysis and venoplasty might be offered to a subset number of patients [3].
After surgery, patients regularly need anticoagulation therapy and close follow-up; good outcomes are expected with early recognition and treatment [1], [2]. Misdiagnosis is common as symptoms are non-specific and may overlap with other cervical pathologies [1], [6]. In our case, after surgery, the patient completely recovered and returned to her normal activities, this time with a personal trainer.
4. Conclusions
Venous TOS is a rare pathology associated with high long-term morbidity and disability. Due to its broad spectrum of clinical symptoms, it continues to be a challenge to the medical team. Therefore, prompt diagnosis is vital to prevent troublesome complications.
Patient perspective
At first, the patient was unsure about her treatment, whether it would hurt, and whether she could be “cured”; nonetheless, since surgery was successful, she was grateful to the medical team.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors and has been approved by the ethics committee of our hospital.
Sources of funding
None.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Registration of research studies
N/A.
Guarantor
Santiago A. Endara Hospital Metropolitano, Department of Surgery Division of Cardiothoracic Surgery, Quito, Ecuador.
Declarations
The submission has not been previously published, nor is it with another journal for consideration.
All authors listed on the paper have reviewed and approved the manuscript in its current form and are aware that it has been submitted.
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
SE and GD analyzed and interpreted the patient data and did the surgical treatment. GM was a major contributor in writing the manuscript. AM prepared the figures. CF revised the manuscript and reviewed all the available data. All authors read and approved the final manuscript.
Declaration of competing interest
We have no conflict of interest to declare.
Acknowledgments
None.
References
- 1.Moore R., Lum Y. Venous thoracic outlet syndrome. Vasc. Med. 2015;20(2):182–189. doi: 10.1177/1358863x14568704. [DOI] [PubMed] [Google Scholar]
- 2.Köknel Talu G. Thoracic outlet syndrome. J. Turk. Soc. Algol. 2005;17(2):5–9. [PubMed] [Google Scholar]
- 3.Ozoa G., Alves D., Fish D.E. Thoracic outlet syndrome. Phys. Med. Rehabil. Clin. N. Am. 2011;22(3):473–483. doi: 10.1016/j.pmr.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 4.Peek J., Vos C.G., Ünlü Ç., van de Pavoordt H.D.W.M., van den Akker P.J., de Vries J.-P.P.M. Outcome of surgical treatment for thoracic outlet syndrome: systematic review and meta-analysis. Ann. Vasc. Surg. 2017;40:303–326. doi: 10.1016/j.avsg.2016.07.065. [DOI] [PubMed] [Google Scholar]
- 5.Kuhn J.E., Lebus G.F., Bible J.E. Thoracic outlet syndrome. J. Am. Acad. Orthop. Surg. 2015;23(4):222–232. doi: 10.5435/jaaos-d-13-00215. [DOI] [PubMed] [Google Scholar]
- 6.Hussain M.A., Aljabri B., Al-Omran M. Vascular thoracic outlet syndrome. Semin. Thorac. Cardiovasc. Surg. 2016;28(1):151–157. doi: 10.1053/j.semtcvs.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 7.Svensson A., Brismar T.B., Brehmer K. Computed tomography venography of the upper extremities — using low dose bilateral contrast media injection in a patient with suspected venous thoracic outlet syndrome. Radiol.Case Rep. 2020;15(3):302–305. doi: 10.1016/j.radcr.2019.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Illig K.A., Donahue D., Duncan A., Freischlag J., Gelabert H., Johansen K., Thompson R.… Reporting standards of the Society for Vascular Surgery for thoracic outlet syndrome. J. Vasc. Surg. 2016;64(3):e23–e35. doi: 10.1016/j.jvs.2016.04.039. [DOI] [PubMed] [Google Scholar]
- 9.Nitz A.J., Nitz J.A. Vascular thoracic outlet in a competitive swimmer: a case report. Int.J.Sports Phys.Ther. 2013;8(1):74–79. [PMC free article] [PubMed] [Google Scholar]
- 10.Sul J., Lim J., Kang S.-K., Choi S.-W., Kwon H.-J., Youm J.-Y. Thoracic outlet syndrome induced by huge lipoma: a case report. Korean J.Neurotrauma. 2019;15(1):67. doi: 10.13004/kjnt.2019.15.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]


