Abstract
Introduction and importance
Gossypiboma is defined as developing an exudative inflammatory process around retained foreign bodies (RFBs). This problem may be asymptomatic or present with severe systemic or regional symptoms. Traditionally, every RFB must be removed with a surgical procedure. In the era of minimally invasive surgery, laparoscopic removal is a good choice for these problems.
Case presentation
A young woman was referred to us with intermittent vague abdominal pain and a history of open cholecystectomy. After initial imaging, we found a twisted string-like object in epigastrium. Considering clinical findings and imaging, the patient was taken to the operating room with a diagnosis of RFB. After an explorative laparoscopy, we found an encapsulated fibrotic mass around a surgical sponge with pus-like secretions.
Conclusion
After diagnosing either RFB or gossypiboma, surgical intervention is mandatory, even in asymptomatic patients. Laparoscopy can help the surgeon to remove the retained item safely. Also, decreased length of stay and postoperative pain are significant advantages of laparoscopic removal.
Keywords: Gossypiboma, Laparoscopy, Surgical sponges, Foreign bodies, Case report
Highlights
-
•
A young woman presented to us complaining of vague abdominal pain without any specific signs and symptoms.
-
•
After initial imaging, a twisted string-like radiopaque object was seen in the epigastrium.
-
•
The patient was operated with the aid of laparoscopy, and the retained sponge removed successfully.
1. Introduction
Gossypiboma is a rare but remarkable condition less reported because of various factors. By definition, gossypiboma is a retained foreign body with exudative inflammation in surrounding areas. Retained foreign bodies (RFB) often remain limited and asymptomatic for years but sometimes lead to gossypiboma [1]. Sponges may be retained in the body incidentally during annual checkups or other reasons. If exudative inflammation develops, the patient will present systemic or regional symptoms. Although all the retained sponges must be removed, the inflammatory signs may convince the surgeon to hurry.
Traditionally, every intra-abdominal RFB is extracted with open surgery. However, in the era of minimally invasive surgeries, the concept of doing every surgery in this manner is extending more and more. The formation of pseudocopula and intra-abdominal adhesions may complicate the laparoscopic approach. For this reason, preoperatively diagnosed cases treated with the laparoscopic approach are less reported in the literature [1].
We present a patient with vague abdominal pain and a subhepatic mass. After initial imaging, we found a foreign body inside the abdomen, which was extracted laparoscopically. The work is reported in line with the SCARE criteria [2].
2. Case presentation
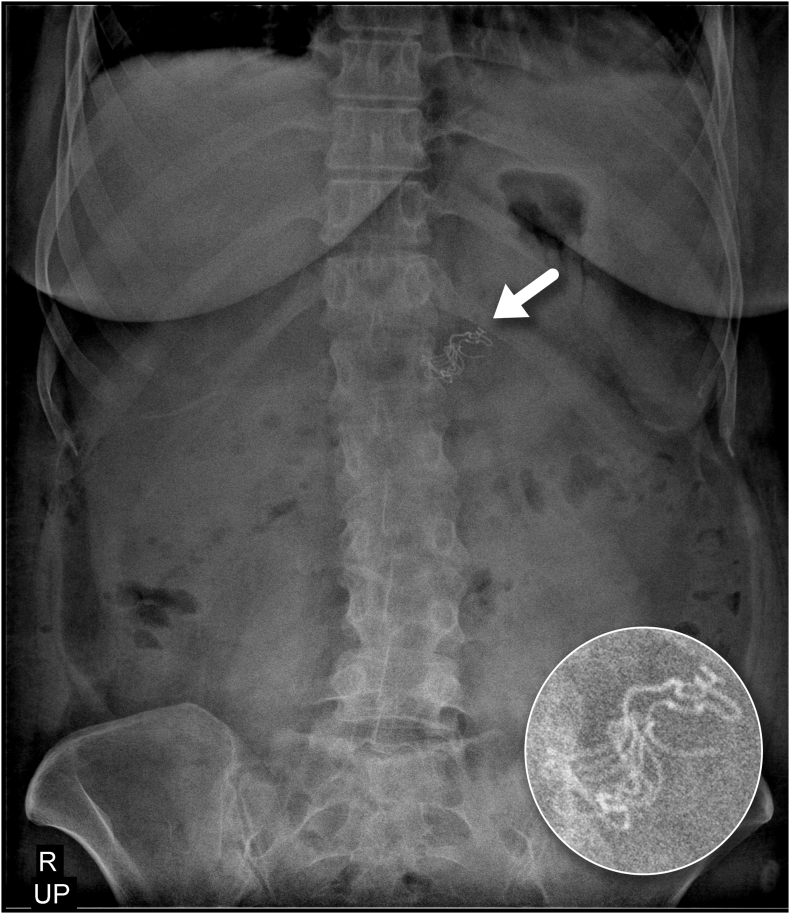
A 37-year-old woman was referred to us with cramping abdominal pain and intermittent anorexia. She had no history of fever, nausea, vomiting, or bowel discomfort. Her vital signs were within normal limits. She had a right subcostal scar on abdominal examination, but no bulging or tenderness was detected. She had undergone an open cholecystectomy two years previously with a diagnosis of the gangrenous gallbladder. Also, she had a history of epilepsy and suffered some episodes of seizures due to chronic subdural hematomas, and was on antiepileptic medication. Her laboratory data showed mild leukocytosis (WBC:11 × 103, neutrophil: 80%) and mild normochromic normocytic anemia. Based on our experience in managing vague abdominal discomforts, we did a plain abdominal X-ray. The film revealed a radio-opaque string-like object in the epigastrium (Fig. 1). This finding, alongside the history of open abdominal surgery, convinced us that the string-like object was probably a retained surgical sponge. Because of the patient's previous experience of pain from open surgery, she insisted on laparoscopy.
Fig. 1.
Plain abdominal upright x-ray shows a convoluted string-like object in epigastrium (this region is also magnified).
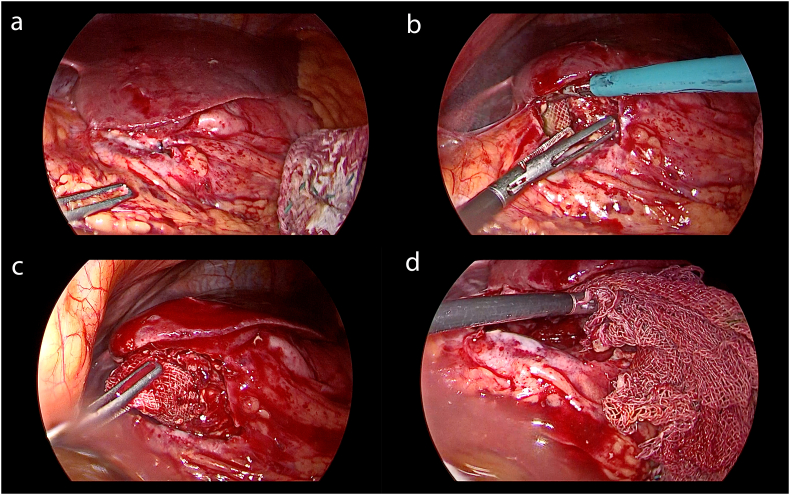
After neurologic consultation and determining the risk of surgery, she was prepared for an explorative laparoscopy. Under general anesthesia, the patient was placed in the reverse Trendelenburg position with both legs split. Because we anticipated adhesions in the upper abdomen, we entered the abdominal cavity via a 10 mm infraumbilical incision using the Hasson technique. Two additional 5 mm ports were also inserted. The subhepatic area was explored, there was a sizeable inflamed mass (7 cm × 5 cm) covered with greater omentum and had multiple adhesions to adjacent structures. The adhesions were carefully released using the LigaSure ™ electrocautery device. After liberating the adhesion bands, we saw an encapsulated surgical sponge in the subhepatic space. Meticulous dissection of the mass was performed using both sharp and blunt dissection. Unfortunately, we ruptured the encapsulated area, and a pus-like grayish fluid erupted into the field. Then, the subhepatic space was washed thoroughly using a suction-irrigation device. No signs of abscess formation and infection were found, and the gossypiboma was removed with an Endobag. The whole abdomen was scrutinized to find any remained pus or potential iatrogenic damage (Fig. 2, Fig. 3). The postoperative follow-up was uneventful and her abdominal symptoms were going through the recovery phase.
Fig. 2.
Four consecutive snapshots from the surgery.
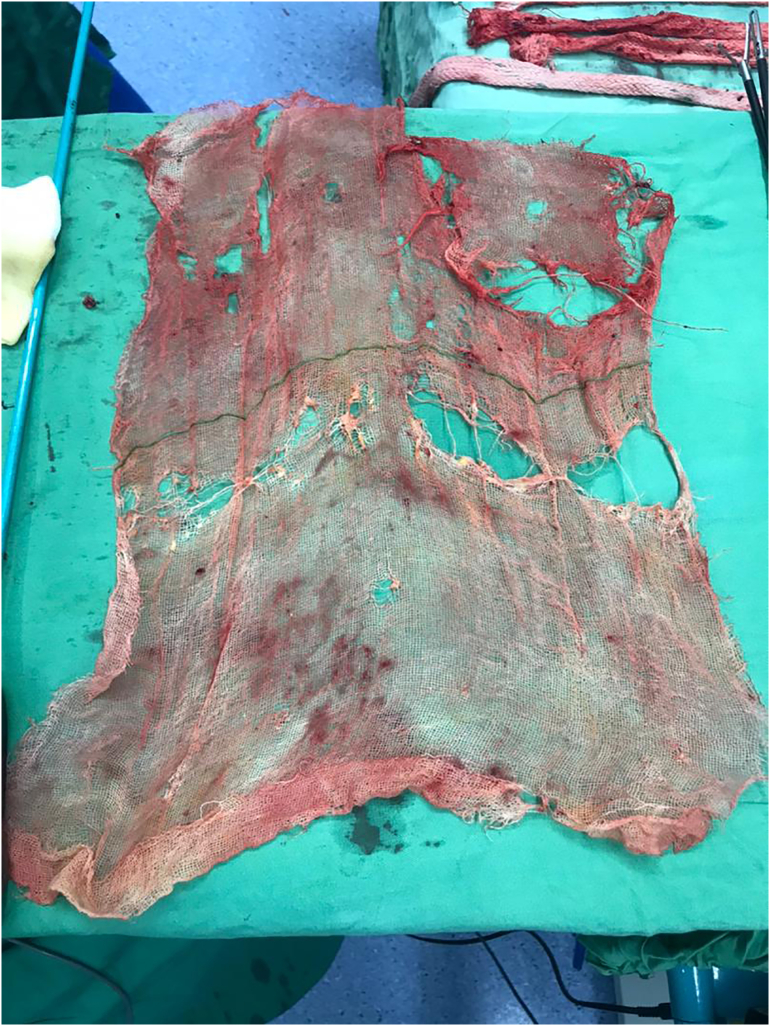
Fig. 3.
The removed 10 cm × 10 cm surgical sponge spread on the table.
3. Discussion
Gossypiboma (originated from Latin and Swahili words “Gossypium” and “boma” meaning cotton and hidden place, respectively), is used to describe the condition of retained surgical sponges or laparotomy pads in cavities of the body [3]. Although every retained sponge in the abdominal cavity is called “retained foreign body,” few cases of RFBs may progress to gossypiboma which specifically refers to the presence of chronic progressive inflammatory processes around the retained sponge. Retained surgical foreign bodies are among preventable but complex surgical events which can cause severe distress to patients and carry serious consequences for the surgical team [4]. Unintended retention of a foreign object in a patient after a surgical procedure is considered a surgical “never event” and is consequently relatively less reported possibly due to potential legal issues or the surgeon's fear of reputation damage. As a result, there is no reliable statistics regarding the incidence of gossypiboma, however, there are some reports on RFBs. In a descriptive study conducted in 2003 in the U.S, the incidence was found to be from 1 in 8801 to 1 in 18,760 [5]. Although there are reports regarding the gender distribution of this condition, it seems that gender is not a determining factor in the development of this condition [7].
Three well-known risk factors for gossypibomas are emergency operations, unplanned change in the operation plan, and the patient's body mass index [5]. Even though emergency operations are associated with only 30% of RFBs, about 70% of them occur following elective surgical procedures [4]. However, our case had undergone an emergency surgery.
Gossypiboma can cause pain, fever, intraabdominal sepsis, abscess formation, gastrointestinal bleeding, fistulas, and even bowel obstruction [1]. Furthermore, in some cases, the inflammatory mass may be mistaken with neoplasms, tumor recurrence or act as a leading point for bowel invagination [6]. This wide range of signs and symptoms is nonspecific; Therefore this diagnosis should be kept in mind in every patient with a history of previous surgery.
Diagnosing RFBs can be a diagnostic dilemma. There are no unique tests, and clinical, imaging, and intraoperative data should be matched. For this reason, taking advantage of an imaging method such as computed tomography (CT), as the most accurate diagnostic modality for RFBs, is almost always recommended as a necessary step after clinical suspicion of RFB [6]. However, in most cases, the plain abdominal x-ray will show an opaque artifact. But plain radiograms may be misleading due to bowel gas patterns, the presence of gallbladder or kidney stones, or the particular position of RFB. Therefore, when we have a strong clinical doubt, it is necessary to do a CT [7]. Also, when a conventional CT cannot help us, a 3D CT with real-time localization could be helpful [8].
After ensuring a correct diagnosis, the main objective would be to remove the object, done either with open or laparoscopic surgery. An Open procedure is easier, faster, and the surgeon can explore and palpate the whole abdomen. On the other hand, an open surgery is associated with excessive pain, large scars, and an increased risk of hernia. For this reason, the laparoscopic approach could be a reasonable choice in selected cases; But it should be noted that laparoscopic removal may cause longer operation times and technical difficulties for the surgical team. Furthermore, in subjects with severe intraabdominal adhesions, the risk of bowel injury is probable. Altogether, it seems that laparoscopic surgeries are more acceptable by the patients, especially when the case may pursue a lawsuit because of a previous bad surgical experience [9].
As we mentioned, although RFBs may cause clinically dangerous consequences, they are entirely preventable, being called by clinicians as “Never events” or “Sentinel events” for this reason. In the modern era, there are a lot of global and regional restrict protocols to enable the prevention of these events in the form of patient safety measures like briefing, debriefing, checklists, and double-counting sponges [10].
In general, RFBs are sometimes unavoidable yet preventable events in every operation. A correct surgical checklist and accurate counts for sponges and instruments are highly advisable [11].This is the responsibility of the whole surgical team including surgeons, scrub and circulating nurses, residents, and even medical students who attend in surgeries as their clerkship due or observership. Counting sponges at three levels is necessary: at the beginning, while closing peritoneum, and after dressing the wound [12].
Considering that there are recommendations regarding the use of routine X-rays after high risk patients or prolonged surgeries, it is worth being investigated in a prospective study with an acceptable number of patients [13].
4. Conclusion
It is recommended to consider RFB as a potential diagnosis in nearly every patient who presents with abdominal pain and a history of previous surgery. Surgical removal is the one and only solution for this problem, even in asymptomatic patients. Laparoscopic extraction of gossypibomas is more complex but has its benefits like less post-operative pain, faster recovery, and smaller incisions. As a “never event”, preventive measures are of paramount importance for the management of RFB.
Sources of funding
The authors didn't receive any financial support for this report.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors' contributions
MS: The main surgeon. RSA: Study design and assisting in the operation. MK: Case presentation and writing the manuscript. AZ: Data gathering and reviewing the manuscript. ME: Image processing and reviewing the manuscript.
All authors read and approved the final manuscript.
Registration of research studies
Not applicable.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Guarantor
Dr. Manoochehr Ebrahimian.
Declaration of competing interest
The authors declared no potential conflict of interests with respect to the research, authorship, and/or publication of this article.
Acknowledgments
None.
References
- 1.Sankpal J., et al. Oh, My Gauze!!!-a rare case report of laparoscopic removal of an incidentally discovered gossypiboma during laparoscopic cholecystectomy. Int. J. Surg. Case Rep. 2020;72:643–646. doi: 10.1016/j.ijscr.2020.04.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agha R.A., et al. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 3.Srivastava K., Agarwal A. Gossypiboma posing as a diagnostic dilemma: a case report and review of the literature. Case Rep. Surg. 2014;2014 doi: 10.1155/2014/713428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stawicki S., et al. Retained surgical foreign bodies: a comprehensive review of risks and preventive strategies. Scand. J. Surg. 2009;98(1):8–17. doi: 10.1177/145749690909800103. [DOI] [PubMed] [Google Scholar]
- 5.Gawande A.A., et al. The cost of health care—highlights from a discussion about economics and reform. N. Engl. J. Med. 2009;361(15):1421–1423. doi: 10.1056/NEJMp0907810. [DOI] [PubMed] [Google Scholar]
- 6.Târcoveanu E., et al. Laparoscopic retrieval of gossypibomas—short series and review of literature. Acta Chir. Belg. 2011;111(6):366–369. doi: 10.1080/00015458.2011.11680774. [DOI] [PubMed] [Google Scholar]
- 7.Campbell E.A., Wilbert C.D. StatPearls [Internet]; 2021. Foreign Body Imaging. [PubMed] [Google Scholar]
- 8.Ariz C., Horton K.M., Fishman E.K. 3D CT evaluation of retained foreign bodies. Emerg. Radiol. 2004;11(2):95–99. doi: 10.1007/s10140-004-0373-0. [DOI] [PubMed] [Google Scholar]
- 9.Sankpal J., et al. Oh, My Gauze !!!- a rare case report of laparoscopic removal of an incidentally discovered gossypiboma during laparoscopic cholecystectomy. Int. J. Surg. Case Rep. 2020;72:643–646. doi: 10.1016/j.ijscr.2020.04.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hempel S., et al. Wrong-site surgery, retained surgical items, and surgical fires: a systematic review of surgical never events. JAMA Surg. 2015;150(8):796–805. doi: 10.1001/jamasurg.2015.0301. [DOI] [PubMed] [Google Scholar]
- 11.Slim K., et al. Annales de radiologie (Paris) 1990. Les corps étrangers textiles oubliés dans l'abdomen. [PubMed] [Google Scholar]
- 12.Le Neel J.-C., et al. Textilomes: à propos de 25 cas et revue de la littérature. Discussion. Chirurgie (Paris) 1994;120(5):272–277. [PubMed] [Google Scholar]
- 13.Teixeira P.G., et al. Retained foreign bodies after emergent trauma surgery: incidence after 2526 cavitary explorations. Am. Surg. 2007;73(10):1031–1034. [PubMed] [Google Scholar]