Abstract
Determinants of parental HPV vaccine hesitancy, including medical mistrust and exposure to negative vaccine information, are understudied in racial/ethnic minority communities where vaccine uptake is low. We conducted a cross-sectional survey (March 2021) among parents of adolescents, ages 9–17 years, from an academic enrichment program serving low-income, first-generation, underrepresented minority families in Los Angeles to understand determinants of parental HPV vaccine hesitancy. Parents completed self-administered surveys, including a 9-item HPV vaccine hesitancy scale, in either English, Spanish, or Chinese. Logistic regression was used to identify individual and interpersonal factors associated with parental hesitancy and adolescent HPV vaccination. One-fifth of parents (n = 357) reported high HPV vaccine hesitancy and > 50% reported concerns about safety or side effects. High medical mistrust was associated with high parental HPV vaccine hesitancy (adjusted-OR 1.69, 95% CI: 1.13, 2.37). Community-tailored and multilevel strategies to increase vaccine confidence are needed to improve HPV and other adolescent vaccinations.
Keywords: HPV vaccination, Vaccine hesitancy, Health equity, Medical mistrust, Adolescent health
Introduction
Human papillomavirus (HPV) vaccines protecting against high-risk HPV types associated with cervical and other cancers have been approved in the United States (US) since 2006 and are currently recommended for routine use among adolescents ages 11–12 years old (Meites et al., 2016). Positive trends in decreasing high-risk HPV infections and pre-cancerous HPV-related lesions in vaccinated individuals have been observed in recent years (Dehlendorff et al., 2021; Harder et al., 2018; Tabrizi et al., 2012; Xu et al., 2019). However, rates of HPV vaccine uptake among adolescents in the target age group remain suboptimal in the US (Elam-Evans et al., 2020) and well below target goals outlined in Healthy People 2030 (Centers for Disease Control & Prevention, 2020). In addition, substantial missed doses of adolescent vaccines during the COVID-19 pandemic indicate any gains in HPV vaccination rates achieved in recent years may be severely impacted (Patel Murthy et al., 2021). Increased efforts will be needed for catch-up vaccinations going forward, particularly among adolescents in high-risk communities.
Prior to the COVID-19 pandemic, HPV vaccination coverage was highly heterogeneous at both national and local levels (Elam-Evans et al., 2020). Statewide HPV vaccine initiation rates among adolescents aged 13–17 years old in California have exceeded the national average in recent years (Centers for Disease Control & Prevention, 2021). However, pockets of low HPV vaccine coverage persist, including in immigrant and racial/ethnic minority communities in Los Angeles (Los Angeles County Department of Public Health, 2018). Barriers to adolescent HPV vaccination previously identified by racial/ethnic minority parents include perceived high financial cost, limited access to in-language vaccine information and understanding of medical terms, lack of provider recommendation, and low HPV vaccine knowledge (Aragones et al., 2016; Ashing et al., 2017; Glenn et al., 2015a, 2015b; Kornfeld et al., 2013; Roncancio et al., 2017; Victory et al., 2019; Vu et al., 2020; Warner et al., 2015). Less is understood about the role of vaccine hesitancy in racial/ethnicity communities and the impact on HPV vaccine uptake, particularly in recent years when general vaccine confidence has declined overall in the US and internationally.
Vaccine hesitancy was identified as a significant public health challenge by the World Health Organization’s Strategic Advisory Group of Experts on Immunization (WHO SAGE) in 2014 (Hickler et al., 2015; Strategic Advisory Group of Experts on Immunization, 2014). The WHO SAGE defines vaccine hesitancy as a “delay in acceptance or refusal of vaccines despite availability of vaccine services” (Strategic Advisory Group of Experts on Immunization, 2014). While many studies have examined public beliefs about childhood vaccines in general in the US (Gidengil et al., 2019; Kempe et al., 2020), only a few recent studies have specifically focused on parental HPV vaccine hesitancy (Patel & Berenson, 2013; Szilagyi et al., 2020). Reported reasons for vaccine hesitancy include lack of confidence in the effectiveness of the HPV vaccine and perceived risk of side effects and concerns about sexual promiscuity (Hanson et al., 2018; Helmkamp et al., 2021; Karafillakis et al., 2019; Szilagyi et al., 2020), despite the evidence that there is no correlation between HPV vaccines and the age of sexual debut (Madhivanan et al., 2016). Predictors of HPV vaccine hesitancy are multifactorial and complex (Cooper et al., 2019), particularly for racial/ethnic minority and low-resourced communities facing additional logistical barriers to accessing preventive care services. Furthermore, there is a limited understanding of how medical mistrust, experiences with healthcare discrimination and exposure to misinformation contribute to HPV vaccine hesitancy within racial/ethnic minority communities.
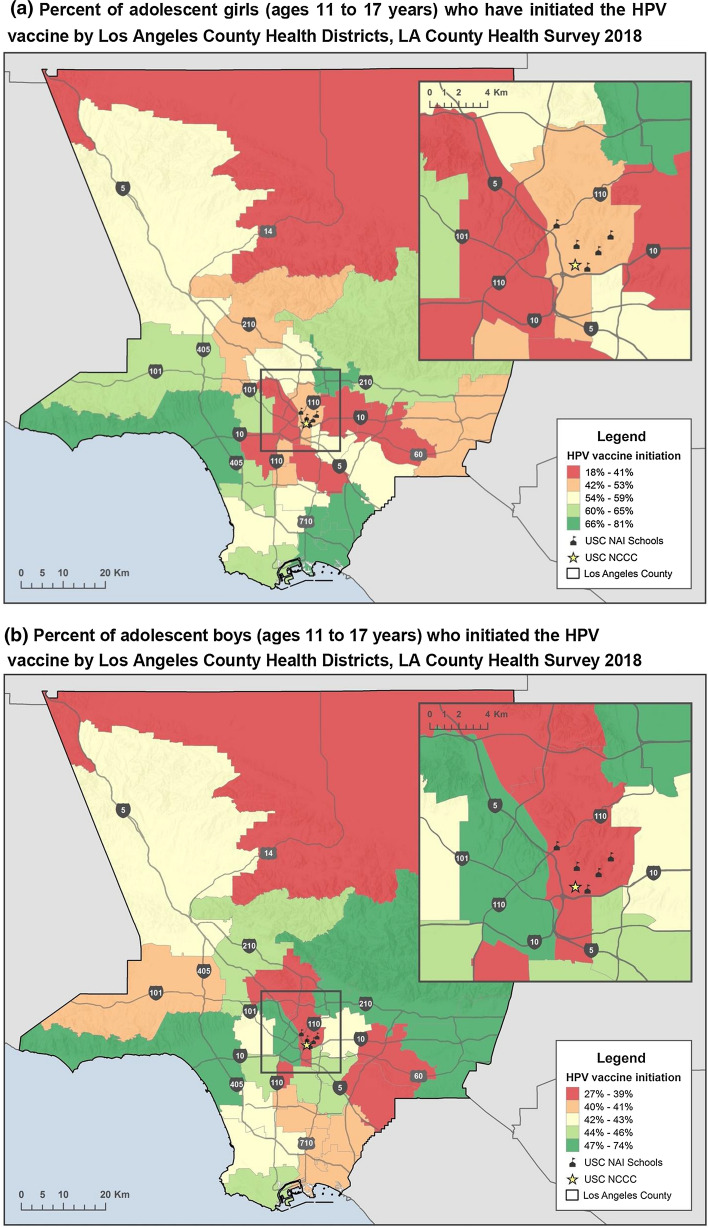
According to the Los Angeles County Health Survey, HPV vaccination is lowest among Hispanic/Latino and Asian adolescent boys and Hispanic/Latina adolescent girls of immigrant parents (Los Angeles County Department of Public Health, 2018). This is particularly concerning because of higher rates of cervical cancer among Hispanic/Latinas compared to NH-white women and the increasing rates of HPV-related oropharyngeal cancer in both genders (Pytynia et al., 2014; Van Dyne et al., 2018).This study examines factors associated with HPV vaccine hesitancy among diverse racial/ethnic parents residing in primarily low-income, low HPV vaccine uptake neighborhoods within Los Angeles to inform parent, provider, and community-level strategies for HPV vaccination improvement. The greater Los Angeles region is the largest geographic metropolitan area in the US and home to several racially/ethnically diverse communities. We hypothesized that limited access to HPV vaccine information among parents, lack of engagement with providers in low uptake areas, and increased medical mistrust contribute to higher parental HPV vaccine hesitancy. Furthermore, we hypothesized that parental HPV vaccine hesitancy differs by survey language, adolescent age, and gender.
Methods
Study setting and sample population
This was a cross-sectional study using self-administered surveys among parents with children ages 9–17 years to understand parental HPV vaccine hesitancy. We recruited parents from The University of Southern California (USC) Leslie and William McMorrow Neighborhood Academic Initiative (NAI), an academic enrichment program for underrepresented minority families in Los Angeles. The vision of NAI is to increase the enrollment and graduation rate of low socioeconomic neighborhood, under-represented students to USC, by serving as a model for a seven-year pre-college enrichment program. The goals of NAI include: increasing the enrollment of under-represented students to enter and successfully complete a Bachelor’s degree by providing a rigorous academic curriculum, providing for the empowerment of parents as mentors and guides for increased student achievement through the provision of meaningful parent educational opportunities through the Family Development Institute, and contributing to the development of student experiences. NAI annually serves 1,000 racial and ethnically diverse, mostly first-generation, low-income middle and high school students in South and East Los Angeles, where adolescent male and female HPV vaccination rates are among the lowest in Los Angeles County (see Fig. 1a, b).
Fig. 1.
a Percent of adolescent girls (ages 11–17 years) who have initiated the HPV vaccine by Los Angeles County Health Districts, LA County Health Survey 2018. b Percent of adolescent boys (ages 11–17 years) who initiated the HPV vaccine by Los Angeles County Health Districts, LA County Health Survey 2018
Participant recruitment and eligibility criteria
In collaboration with NAI, recruitment of middle and high school parents took place over two weekends in March 2021. A core component of the program, in addition to academic enrichment for students, is to provide a Saturday Academy, consisting of morning workshops for parents and students on a variety of topics. During our study period, all parent and student activities in NAI were conducted virtually due to the COVID-19 pandemic. Parents of middle and high school students enrolled in NAI were invited to complete the survey online during two of NAI’s mandatory weekly virtual parent enrichment sessions on Saturday mornings. Study eligibility included being a parent or guardian of a child between ages 9–17 years and the ability to complete the survey in English, Spanish or Chinese. Screening for study eligibility and survey completion were self-administered via REDCap live, in real-time, during virtual parent workshops. Multi-lingual NAI and USC research team members were present during the virtual sessions to answer parent questions and provide support for eligibility screening. Parents received a $25 gift card for survey completion. The study was approved by USC’s Institutional Review Board and found to be exempt from the requirement to obtain written consent from study subjects prior to study participation. However, all participating parents received an in-language study information sheet with details about study procedures, risks and benefits. All Human Subject procedures and Internal Review Board protocols were followed. NAI staff provided feedback and approval of the study’s recruitment strategy and reviewed all study materials.
Survey instrument
The 60-item survey instrument included measures from prior work of our team and others to understand HPV vaccination in multiethnic populations, including previously validated instruments for HPV vaccine hesitancy, medical mistrust, and acculturation (Baezconde-Garbanati et al., 2017; Boyd et al., 2018; Casillas et al., 2011; Glenn et al., 2015a, 2015b; Greenfield et al., 2015; Hirth, 2019; Jeudin et al., 2014; Tsui et al., 2013, 2019). Survey topics included: parental and adolescent demographic characteristics, parental HPV vaccine awareness, HPV vaccine hesitancy (Szilagyi et al., 2020), exposure to negative HPV information, medical mistrust (Thompson et al., 2004), acculturation (Norris et al., 1996), provider recommendation of adolescent HPV vaccine, prior receipt of HPV and other adolescent vaccines, healthcare utilization, and COVID-19 vaccination intent for parents themselves and their adolescents.
The survey was translated from English to Spanish and to Chinese using an external translation service, familiar with and frequently used by health-related research studies. Translated surveys in Spanish and Chinese were then reviewed and back-translated by NAI and USC research staff to ensure appropriateness for the target parent population, including literacy level for the target parent population (approximately 8th grade). Surveys in all three languages were then inputted into the USC Clinical and Translation Science Institute’s REDCap (Research Electronic Data Capture) platform, a free, secure, web-based application designed for rapidly developing databases and surveys for research studies. A link to the REDCap platform to access surveys were made available to NAI parents during the live, virtual parent workshops after the study team introduced the research study. There were 318 unique viewers who joined the first NAI parent webinar and 307 unique viewers who joined the second NAI webinar. All webinar attendees were introduced to the study and survey instructions in the last 30 min of the webinar. Following screening eligibility procedures, parents were asked to select their survey language of preference (English, Spanish, Chinese) and initiate the self-administered survey. Parents who required clarification of any survey items during the live self-administered survey period, which occurred virtually via Zoom (Zoom Video Communications, Inc., San Jose, CA), had the option of asking USC and NAI research staff for assistance in virtual breakout rooms by language. The online survey took approximately 15–25 min to complete.
Measures
Parent and adolescent demographic and access to care characteristics
Respondents were asked to provide information about the following sociodemographic covariates: parental race, age, gender, insurance coverage type, education, income, nativity, adolescent age, gender, and number of siblings. We asked parents to report the usual source of care for their adolescents with the following categories: doctor’s office; emergency room; health department clinic; school clinic; clinic or health center; and no usual source of care. Due to lack in distribution of responses across these categories, usual source of care was re-categorized as yes (any source other than emergency room) and no (no usual source, emergency room, or unknown/missing). Adolescent insurance options included no insurance; parent-employer provided private insurance; parent-purchased private insurance; and Medicaid (Medi-Cal)/Children’s Health Insurance Program (CHIP). Parental and adolescent insurance was dichotomized into public and private insurance; public insurance types included Medi-Cal, Medicare, and My Health LA, and private insurance types included private insurance purchased through an employer and private insurance purchased by the parent or a family member.
HPV vaccine hesitancy
Our primary outcome of interest was HPV vaccine hesitancy. We used the 9-item HPV vaccine hesitancy scale (Szilagyi et al., 2020), previously adapted by Szilagyi and colleagues from the WHO SAGE Vaccine Hesitancy Scale (Larson et al., 2015) and by the literature on assessments of hesitancy in similar populations in the US (Hirth et al., 2019; Moran et al., 2016, 2017; Painter et al., 2019; Victory et al., 2019). The scale contains a series of statements describing attitudes towards HPV vaccination (e.g., “The HPV vaccine is effective”; “The HPV vaccine is important for my adolescent’s health”; and “I am concerned about serious side effects of the HPV vaccine”) and a 4-point Likert scale ranging from strongly agree to strongly disagree (no neutral response option) as answer choices. Similar to Szilagyi and colleagues, we calculated scale scores by averaging the responses to all items (item scores ranged from 1 to 5), with higher values corresponding to higher hesitancy, and used a cutoff score of higher than 3 to define high parental HPV vaccine hesitancy.
Medical mistrust
We used Thompson’s Group-Based Medical Mistrust Scale (Thompson et al., 2004) to assess parental medical mistrust. This 12-item scale asked participants to state their agreement or disagreement with a number of statements that describe experiences of perceived suspicion or hostility by healthcare professionals (e.g., “Doctors and health care workers sometimes hide information from patients who belong to my ethnic group”; “People of my ethnic group cannot trust doctors and health care workers”; “I have personally been treated poorly or unfairly by doctors or health care workers because of my ethnicity”). Response categories consisted of a 5-point Likert scale ranging from strongly agree to strongly disagree. As indicated by Thompson et al., scale scores were summed for all item responses with a possible range of 12–60, where higher scores denoted more medical mistrust. We compared parents with higher medical mistrust, those with scores one deviation or more from the mean to parents with mean medical mistrust scores or lower.
Acculturation
The Brief Acculturation Scale for Hispanics (Norris et al., 1996), previously validated in Hispanic/Latino and Asian populations, was included to assess acculturation among our sample. Answer choices were modified in our survey to be appropriate for non-Hispanic/Latino respondents by replacing the Spanish-specific language choices with “your native language.” A scale score was calculated by averaging all responses, with scores ranging from 1 to 5 with higher scores denoting higher acculturation. Respondents with scores higher than 3.25 were considered to have high acculturation.
Parental exposure to negative HPV vaccine information
We asked parents the following yes/no question: “Have you ever received or heard negative information about HPV vaccines?” Participants who responded yes were prompted to provide details about the negative information they received.
Gender neutral perception of vaccine need
In addition to the 9-item HPV vaccine hesitancy scale we also included an additional item to assess attitudes towards vaccinating adolescent males: “It is important for boys/males to get the HPV vaccine” (strongly agree to strongly disagree).
HPV vaccination and other adolescent vaccination history
For survey items on receipt of physician recommendation, adolescent HPV vaccination history (number of shots, age at first shot), parents were asked to respond with their youngest child in mind if they had more than one child in the eligible age range (9–17 years). Parents were also asked if their youngest child ever received the Tdap vaccine and the influenza vaccine in the past 12 months. Both of these questions were modeled after the NIS-Teen survey items (Centers for Disease Control & Prevention, 2019).
COVID-19 vaccine intent
We included a question asking parents to report the likelihood that they would obtain a COVID-19 vaccine for themselves and their children once it became available. The answer choices were a 4-item Likert scale (very likely, somewhat likely, not too likely, not likely at all), plus an option for having already received the COVID-19 vaccine. At the time of data collection (March 2021), COVID-19 vaccines were only approved for ages 16 and older in the US.
Statistical analyses
Descriptive statistics were used to summarize parental HPV vaccine hesitancy, medical mistrust, acculturation, parent and adolescent demographic characteristics, among other variables in the final analytic sample. Chi-Square and Fisher’s exact test were used to compare HPV vaccine hesitancy items across predictors of interest and survey language (English, Spanish, and Chinese). Comparisons of mean hesitancy and acculturation scores were examined using ANOVA. Of the 497 parents who attended the two NAI weekend workshops and initiated an online survey, 75 surveys were excluded due to incomplete eligibility information. An additional 55 participants were excluded from the analytic dataset due to incomplete surveys or missing data in our variables of interest. Unadjusted logistic regression models were used to assess bivariate relationships between medical mistrust and other independent variables of interest and parental HPV vaccine hesitancy (high versus low hesitancy), while controlling for parent and adolescent demographic characteristics. The final multivariable logistic regression model was determined based on significant bivariate associations (p < 0.05) as well as prior literature on important predictors of parental vaccine hesitancy. All analyses were conducted in SAS statistical software version 9.4 (SAS Institute Inc., Cary, NC).
Results
Sample characteristics
Parent and adolescent sociodemographic characteristics are shown in Table 1 by survey language. Of the 357 parents included in the analytic sample, more than half (54.9%) completed the survey in English, 35.9% in Spanish and 9.2% in Chinese. The majority (88.3%) of survey participants were mothers/female guardians. Almost three quarters (76.7%) of parents self-identified as Hispanic/Latino and another 16.2% identified as Asian/Asian American. Consistent with the target population of families within the NAI program, nearly half of all parents had public insurance coverage (44.5%) and reported an annual household income below $40,000 (49.3%). In addition, the majority of parents were non-US born (73.4%) and had less than a college degree (79.6%). While the total population showed a high acculturation average (85%), this was largely driven by the English survey participants, as Spanish and Chinese respondents were likely to report low acculturation (95.3% and 100%, respectively; χ2 = 114.24, p < 0.01). Some parental sociodemographic factors differed across survey language, including a higher proportion Spanish survey parents reporting having no insurance compared to English and Chinese survey parents (χ2 = 41.33, p < 0.01) and English survey parents reporting higher education (χ2 = 73.53, p < 0.01) and higher income compared to parents who completed the survey in Spanish and Chinese (χ2 = 46.35, p < 0.01).
Table 1.
Sociodemographic characteristics of parents and adolescents by survey language (n = 357)
| Total | English | Spanish | Chinese | P value | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Total | 357 | 100.0 | 196 | 54.9 | 128 | 35.9 | 33 | 9.2 | |
| Parent characteristics | |||||||||
| Race/ethnicity | < 0.01 | ||||||||
| Hispanic/Latinos | 260 | 76.7 | 139 | 73.5 | 121 | 100.0 | 0 | 0.0 | |
| NH-White | 3 | 0.9 | 3 | 1.6 | 0 | 0.0 | 0 | 0.0 | |
| NH-Black | 10 | 3.0 | 10 | 5.3 | 0 | 0.0 | 0 | 0.0 | |
| NH-Asian | 55 | 16.2 | 26 | 13.8 | 0 | 0.0 | 29 | 100.0 | |
| Other/multi-race | 11 | 3.2 | 11 | 5.8 | 0 | 0.0 | 0 | 0.0 | |
| Age | 0.36 | ||||||||
| 30–40 years | 107 | 30.7 | 65 | 33.7 | 35 | 28.2 | 7 | 21.9 | |
| 41- 50 years | 176 | 50.4 | 91 | 47.2 | 64 | 51.6 | 21 | 65.6 | |
| > 50 years | 66 | 18.9 | 37 | 19.2 | 25 | 20.2 | 4 | 12.5 | |
| Gender | 0.04 | ||||||||
| Male | 40 | 11.4 | 22 | 11.3 | 14 | 11.2 | 4 | 12.5 | |
| Female | 310 | 88.3 | 172 | 88.7 | 111 | 88.2 | 27 | 84.4 | |
| Insurance type | < 0.01 | ||||||||
| Private Insurance | 120 | 33.6 | 99 | 50.5 | 18 | 14.1 | 3 | 9.1 | |
| Public Insurance | 159 | 44.5 | 73 | 37.2 | 58 | 45.3 | 25 | 84.9 | |
| Uninsured/Other | 78 | 21.9 | 24 | 12.2 | 52 | 40.6 | 2 | 6.1 | |
| Education | < 0.01 | ||||||||
| Less than High School | 111 | 31.1 | 38 | 19.4 | 65 | 50.8 | 8 | 24.2 | |
| High School graduate | 80 | 22.4 | 38 | 19.4 | 25 | 19.5 | 17 | 51.5 | |
| Higher than High School | 140 | 39.2 | 110 | 56.1 | 25 | 19.5 | 5 | 15.2 | |
| Unknown/Prefer not to answer | 26 | 7.3 | 10 | 5.1 | 13 | 10.2 | 3 | 9.1 | |
| Income ($) | < 0.01 | ||||||||
| 0–39,999 | 176 | 49.3 | 68 | 34.7 | 87 | 68.0 | 21 | 63.6 | |
| 40,000–79,999 | 153 | 42.9 | 101 | 51.5 | 41 | 32.0 | 11 | 33.3 | |
| > 80,000 | 28 | 7.8 | 27 | 13.8 | 0 | 0.0 | 1 | 3.0 | |
| Nativity | < 0.01 | ||||||||
| Us-Born | 87 | 26.2 | 85 | 46.5 | 2 | 1.8 | 0 | 0.0 | |
| Non-US Born | 240 | 73.4 | 98 | 53.6 | 112 | 98.3 | 30 | 100.0 | |
| Acculturation score | < 0.01 | ||||||||
| High (< 3.25–5.0) | 118 | 67.0 | 112 | 57.1 | 6 | 4.7 | 0 | 0.0 | |
| Low (1.0–3.25) | 239 | 33.1 | 84 | 42.9 | 122 | 95.3 | 33 | 100.0 | |
| Medical mistrust (mean, SD) | 28.43 | (9.15) | 24.94 | (9.87) | 28.84 | (8.66) | 29.7 | (6.05) | 0.48 |
| Neg. HPV vaccine info | 0.11 | ||||||||
| Yes | 49 | 13.7 | 32 | 16.3 | 16 | 12.5 | 1 | 3.0 | |
| No | 308 | 86.3 | 164 | 83.7 | 112 | 87.5 | 32 | 97.0 | |
| Adolescent characteristics | |||||||||
| Age | 0.24 | ||||||||
| 9–10 years | 53 | 14.9 | 32 | 16.3 | 15 | 11.7 | 6 | 18.2 | |
| 11–13 years | 104 | 2.1 | 59 | 30.1 | 33 | 25.8 | 12 | 36.4 | |
| 14–17 years | 117 | 32.8 | 68 | 34.7 | 42 | 32.8 | 7 | 21.2 | |
| Unknown | 83 | 23.3 | 37 | 18.9 | 38 | 29.7 | 8 | 24.2 | |
| Gender | 0.64 | ||||||||
| Male | 163 | 46.2 | 92 | 47.2 | 54 | 43.2 | 17 | 51.5 | |
| Female | 190 | 53.8 | 103 | 52.8 | 71 | 56.8 | 16 | 48.5 | |
| Has older sibling | 0.59 | ||||||||
| Yes | 184 | 51.5 | 103 | 52.6 | 62 | 48.4 | 19 | 57.6 | |
| No | 173 | 48.5 | 93 | 47.4 | 66 | 51.6 | 14 | 42.4 | |
| Insurance type | < 0.01 | ||||||||
| Private insurance | 82 | 28.2 | 72 | 41.9 | 8 | 8.9 | 2 | 6.9 | |
| Medicaid/CHIP | 201 | 69.1 | 95 | 55.2 | 79 | 87.8 | 27 | 93.1 | |
| Uninsured/Other | 8 | 2.8 | 5 | 2.9 | 3 | 3.3 | 0 | 0.0 | |
| Usual source of care | < 0.01 | ||||||||
| Yes | 289 | 98.6 | 170 | 98.8 | 28 | 96.6 | 1 | 3.5 | |
| No | 4 | 1.4 | 2 | 1.2 | 1 | 3.5 | 1 | 3.5 | |
| Initiated HPV vaccine | |||||||||
| No | 155 | 53.3 | 92 | 53.8 | 41 | 45.1 | 22 | 75.9 | 0.02 |
| Yes | 136 | 43.7 | 79 | 46.2 | 50 | 55.0 | 7 | 24.1 | |
| Yes—Males | 61 | 44.9 | 35 | 44.3 | 23 | 46.0 | 3 | 42.9 | 0.01 |
| Yes—Females | 75 | 55.2 | 44 | 55.7 | 27 | 54.0 | 4 | 57.1 | |
| Received Tdap Vaccine | |||||||||
| Yes | 219 | 76.6 | 139 | 81.3 | 58 | 67.4 | 22 | 75.9 | 0.05 |
| No | 67 | 23.4 | 32 | 18.7 | 28 | 32.6 | 7 | 24.1 | |
| Received flu vaccine | |||||||||
| Yes | 170 | 58.0 | 98 | 57.0 | 54 | 58.7 | 18 | 62.1 | 0.87 |
| No | 123 | 42.0 | 74 | 43.0 | 38 | 41.3 | 11 | 37.9 | |
| COVID-19 vaccine for child | |||||||||
| Very likely | 168 | 58.3 | 101 | 59.4 | 57 | 63.3 | 10 | 35.7 | 0.01 |
| Somewhat likely | 76 | 26.4 | 39 | 22.9 | 20 | 22.2 | 17 | 60.7 | |
| Not too likely | 31 | 10.8 | 20 | 11.8 | 10 | 11.1 | 1 | 3.6 | |
| Not likely at all | 13 | 4.5 | 10 | 5.9 | 3 | 3.3 | 0 | 0.0 | |
| It is important for boys/males to get the HPV vaccine | < 0.01 | ||||||||
| Strongly disagree | 34 | 9.6 | 18 | 9.2 | 16 | 12.7 | 0 | 0.0 | |
| Somewhat disagree | 41 | 11.6 | 24 | 12.2 | 11 | 8.7 | 6 | 19.5 | |
| Somewhat agree | 138 | 39.1 | 75 | 38.3 | 41 | 32.5 | 22 | 71.0 | |
| Strongly agree | 140 | 39.7 | 79 | 40.3 | 58 | 46.0 | 3 | 9.7 | |
Adolescent age and gender were evenly distributed across categories and were similar across survey language (see Table 1). Nearly half of parents reported their adolescents were ages 9–13 years (44%), female (53.2%) and had an older sibling (51.5%). Relevant to primary care and HPV vaccine access, a higher proportion of English survey parents reported their children were privately insured (χ2 = 40.65, p < 0.01) and went to a doctor’s office for their usual source of care (χ2 = 55.93, p < 0.01) compared to other survey languages. Most parents reported their children had received the Tdap vaccine (76.6%), while fewer reported their children had initiated the HPV vaccine (43.7%) or received a flu shot in the previous year (58.0%). Parents reported significantly higher HPV vaccination uptake in daughters/females (55%) than in sons/males (45%) (χ2 = 6.67, p = 0.0098), a pattern was consistent across survey languages.
HPV vaccine hesitancy
Mean HPV vaccine hesitancy scores were 2.27 in our sample and nearly one-fifth (19.3%) of parental hesitancy scores fell within the high hesitancy category. Mean hesitancy scores and the proportion of parents falling in the high HPV vaccine hesitancy category did not differ significantly by survey language (see Table 2). The distribution across response categories (strongly agree to strongly disagree) for individual HPV vaccine hesitancy items differed significantly by survey language (p < 0.05) for all items except item #9, which stated: “I am concerned about serious side effects of the HPV vaccine” (p = 0.07). Overall, Chinese survey respondents rarely “strongly disagreed” with any hesitancy item while the distribution of English and Spanish survey respondents across hesitancy items were more similar. Notably, 57.4% of all parents across the language groups somewhat/strongly agreed to the statement, “the HPV vaccine has not been around long enough to be sure it’s safe” (p = 0.01). 64.5% of all parents somewhat/strongly agreed to the statement, “I am concerned about serious side effects of the HPV vaccine,” although it was not statistically significant across the groups (p = 0.07).
Table 2.
Parental HPV vaccine hesitancy items by survey language
| Total | English | Spanish | Chinese | P value | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean hesitancy score (SD) | 2.27 (0.92) | 2.23 (0.97) | 2.31 (0.92) | 2.30 (0.41) | 0.72 | ||||||||||||
| HPV vaccine hesitancy | |||||||||||||||||
| High hesitancy | 19.3% | 19.9% | 21.9% | 93.9% | 0.12 | ||||||||||||
| Low hesitancy | 80.7% | 80.1% | 78.1% | 6.1% | |||||||||||||
| % Strongly disagree | % Somewhat disagree | % Somewhat agree | % Strongly agree | % Strongly disagree | % Disagree | % Agree | % Strongly agree | % Strongly disagree | % Disagree | % Agree | % Strongly agree | % Strongly disagree | % Disagree | % Agree | % Strongly agree | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Info received from HCP is reliable and trustworthy | 7.4 | 10.5 | 38.8 | 43.3 | 8.2 | 9.2 | 35.7 | 46.9 | 8.0 | 12.8 | 34.4 | 44.8 | 0.0 | 9.4 | 75.0 | 15.6 | < 0.01 |
| The HPV vaccine is effective | 7.0 | 9.9 | 44.2 | 38.9 | 7.1 | 10.2 | 43.4 | 39.3 | 8.7 | 9.5 | 35.7 | 46.0 | 0.0 | 9.1 | 81.8 | 9.1 | < 0.01 |
| Getting the HPV vaccine is a good way to protect from HPV-related cancers | 9.6 | 6.5 | 35.1 | 48.7 | 8.7 | 6.6 | 34.2 | 50.5 | 13.6 | 7.2 | 26.4 | 52.8 | 0.0 | 3.1 | 75.0 | 21.9 | < 0.01 |
| The HPV vaccine is beneficial for my child/adolescent | 9.0 | 9.0 | 34.8 | 47.2 | 7.7 | 10.2 | 34.2 | 48.0 | 13.4 | 7.9 | 26.0 | 52.8 | 0.0 | 6.1 | 72.7 | 21.2 | < 0.01 |
| Generally, I do what my HCP recommends about HPV vaccines | 8.5 | 10.2 | 37.4 | 43.9 | 9.7 | 10.7 | 37.2 | 42.4 | 8.8 | 11.2 | 30.4 | 49.6 | 0.0 | 3.1 | 65.6 | 31.3 | 0.02 |
| The HPV vaccine is important | 8.8 | 8.2 | 33.7 | 49.3 | 8.7 | 8.2 | 35.2 | 48.0 | 11.2 | 9.6 | 22.4 | 56.8 | 0.0 | 3.1 | 68.8 | 28.1 | < 0.01 |
| Having my child/adolescent get the HPV vaccine is important my community | 10.2 | 9.4 | 37.5 | 42.9 | 8.7 | 9.2 | 40.8 | 41.3 | 15.3 | 11.3 | 21.8 | 51.6 | 0.0 | 3.1 | 78.1 | 18.8 | < 0.0001 |
| The HPV vaccine has not been around long enough to be sure it’s safe | 16.1 | 26.6 | 44.4 | 13.0 | 18.9 | 30.1 | 40.8 | 10.2 | 15.9 | 22.2 | 45.2 | 16.7 | 0.0 | 21.9 | 62.5 | 15.6 | 0.01 |
| I am concerned about serious side effects of the HPV vaccine | 17.2 | 18.3 | 43.9 | 20.6 | 16.8 | 20.9 | 42.4 | 19.9 | 21.4 | 14.3 | 41.3 | 23.0 | 3.0 | 18.2 | 63.6 | 15.2 | 0.07 |
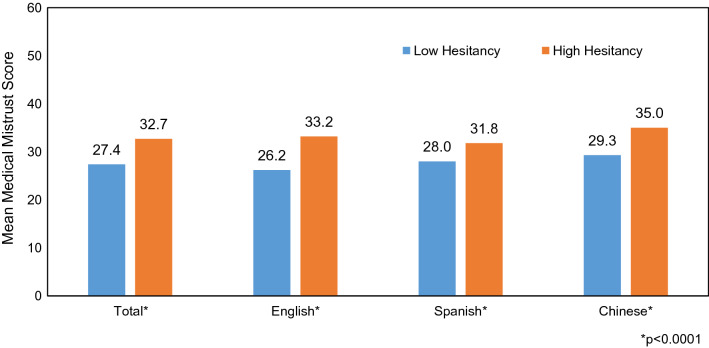
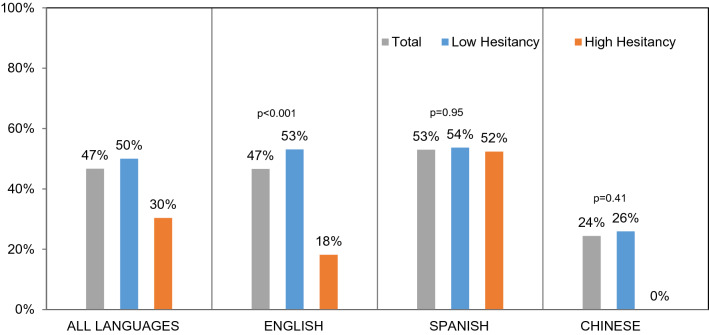
Medical mistrust
The mean medical mistrust score was 28.4 among all parents and did not differ significantly by survey language. We observed higher levels of medical mistrust among parents with high HPV vaccine hesitancy compared to those with low HPV vaccine hesitancy (27.4 vs. 32.6, two-sided paired t test = − 58.83, p < 0.01) (see Fig. 2). We further observed higher HPV vaccine initiation among adolescents of parents reporting low hesitancy compared to those with high hesitancy (50% vs. 30%, χ2 = 0.0076, p < 0.01) (see Fig. 3).
Fig. 2.
Parental medical mistrust by parental HPV vaccine hesitancy
Fig. 3.
HPV vaccine initiation among adolescents by parental HPV vaccine hesitancy
Other HPV vaccine attitudes and exposure to negative information
More than three-fourths (78.8%) of parents either somewhat or strongly agreed that it was “important for males to receive the HPV vaccine.” However, a much higher proportion of Spanish survey parents strongly disagreed with this statement (12.7% vs 9.2% of English and 0% of Chinese groups, p < 0.001). Few parents (13.7%) reported having heard negative information about the HPV vaccine and the likelihood of having heard negative information about the HPV vaccine were significantly different by survey language (p = 0.11). The majority of open text responses on type of negative information parents encountered were related to side effects and the long-term effectiveness of the HPV vaccine.
Bivariate and multivariable models for HPV vaccine hesitancy
In our unadjusted logistic regression analyses (see Table 3), we found significantly higher odds of having high parental HPV vaccine hesitancy among those with higher mean medical mistrust (OR = 1.80, 95% CI: 1.36–2.39) compared to those with average or lower mean medical mistrust score, who had heard negative information about the HPV vaccine (OR = 3.65, 95% CI: 1.91–6.96) compared to those who had not, and parents of children who had not gotten a flu vaccine in the previous year (OR = 2.15, 95% CI: 1.18–3.92). Parents who reported being only somewhat likely (OR = 1.58, 95% CI: 0.75–3.31) or not likely at all (OR = 15.7, 4.45–55.70) to get their children vaccinated against COVID-19 once the vaccine became available also had higher odds of having high HPV vaccine hesitancy. Parental race/ethnicity, age, gender, education, nativity and acculturation as well as adolescent insurance type were not statistically significant in the unadjusted associations with parental HPV vaccine hesitancy and omitted from the multivariable analyses and Table 3.
Table 3.
Bivariate and multivariable logistic regression models for high parental HPV vaccine hesitancy and No HPV vaccine uptake
| High HPV vaccine hesitancy | No HPV vaccine initiation | |||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted model | Adjusted model | Unadjusted model | Adjusted model | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Parent characteristics | ||||||||
| Survey language | ||||||||
| English | REF | REF | REF | REF | REF | REF | REF | REF |
| Chinese | 0.26 | 0.06, 1.13 | 0.32 | 0.07, 1.56 | 2.70 | 1.10, 6.65 | 3.39 | 1.17–9.82 |
| Spanish | 1.13 | 0.65, 1.95 | 1.13 | 0.53, 2.43 | 0.70 | 0.42, 1.17 | 0.50 | 0.28–0.91 |
| Medical mistrust | ||||||||
| 1 SD + versus mean | 1.80 | 1.36, 2.39 | 1.69 | 1.13, 2.37 | 1.15 | 0.92, 1.45 | 1.09 | 0.82, 1.45 |
| HPV negative information | ||||||||
| Yes | 3.65 | 1.91, 6.96 | 2.57 | 1.03, 6.42 | 1.12 | 0.55, 2.31 | 0.89 | 0.37, 2.11 |
| No | REF | REF | REF | REF | REF | REF | ||
| HPV vaccine hesitancy | ||||||||
| Yes [High] | 2.35 | 1.24, 4.45 | 2.78 | 1.27, 6.06 | ||||
| No [Low] | REF | REF | REF | REF | ||||
| Adolescent characteristics | ||||||||
| Age | ||||||||
| 9–10 years | 1.58 | 0.66, 3.80 | 1.24 | 0.42, 3.67 | 3.09 | 1.52, 6.29 | 2.86 | 1.27, 6.46 |
| 11–13 years | 2.15 | 1.06, 4.35 | 2.20 | 0.94, 5.14 | 1.96 | 1.13, 3.38 | 1.94 | 1.03, 3.66 |
| 14–17 years | REF | REF | REF | REF | REF | REF | REF | REF |
| Unknown | 2.02 | 0.96, 4.26 | 1.66 | 0.44, 6.29 | 1.00 | 0.43, 2.29 | 0.49 | 0.18, 1.28 |
| Gender | ||||||||
| Male | 1.05 | 0.62, 1.78 | 1.27 | 0.61, 2.65 | 1.84 | 1.16–2.94 | 2.39 | 1.37, 4.18 |
| Female | REF | REF | REF | REF | REF | REF | REF | REF |
| Usual source of care | ||||||||
| Yes | REF | REF | REF | REF | ||||
| No | 4.56 | 0.63, 33.10 | 0.29 | 0.03, 2.80 | ||||
| Tdap | ||||||||
| Yes | REF | REF | REF | REF | REF | REF | REF | REF |
| No | 1.01 | 0.49, 2.06 | 0.86 | 0.36, 2.06 | 2.53 | 1.41, 4.55 | 3.02 | 1.53, 5.94 |
| Flu | ||||||||
| Yes | REF | REF | REF | REF | REF | REF | REF | REF |
| No | 2.15 | 1.18, 3.92 | 1.85 | 0.91, 3.75 | 1.33 | 0.83, 2.13 | 1.38 | 0.79, 2.41 |
| Has older sibling | ||||||||
| Yes | REF | REF | REF | REF | ||||
| No | 0.73 | 0.43, 1.23 | 0.38 | 0.24, 0.61 | ||||
| COVID-19 vaccine intent-child | ||||||||
| Very likely | REF | REF | REF | REF | REF | REF | REF | REF |
| Somewhat likely | 1.58 | 0.76, 3.31 | 1.56 | 0.67, 3.68 | 1.80 | 1.03, 3.15 | 1.12 | 0.58, 2.15 |
| Not too likely | 2.86 | 1.16, 7.05 | 1.54 | 0.54, 4.40 | 1.07 | 0.45, 2.34 | 0.77 | 0.31, 1.90 |
| Not likely at all | 15.75 | 4.45, 55.71 | 8.65 | 2.07, 38.20 | 3.58 | 0.95, 13.47 | 0.82 | 0.18, 3.82 |
Values are statistically significant at the p < 0.05 level
*Parental race/ethnicity, age, gender, education, nativity and acculturation and adolescent insurance were not significant in the bivariate analyses
In our adjusted multivariable models (see Table 3), we observed that having higher medical mistrust (OR = 1.69, 95% CI: 1.13–2.37), exposure to HPV vaccine negative information (OR = 2.57, 95% CI: 1.03–6.42), and lower intent to get COVID-19 vaccine for the child (OR = 8.65, 95% CI: 2.07–38.20) were significantly associated with higher parental HPV vaccine hesitancy after adjusting for survey language, adolescent age, gender, Tdap vaccination, and influenza vaccination. Our exploratory models consistently showed medical mistrust, exposure to negative HPV information, lower COVID-19 vaccine intent for child to be significantly associated with high parental HPV vaccine hesitancy. These associations did not change in significance or magnitude when we replaced survey language with race/ethnicity or nativity with acculturation in our adjusted models.
Bivariate and multivariable models for HPV vaccine initiation
We observed significant associations between lack of HPV vaccine initiation and high parental HPV vaccine hesitancy in the bivariate analyses (see Table 3). Parents with high HPV vaccine hesitancy had over 2 time the odds of reporting that their child had not received the HPV vaccine compared to parents with low HPV vaccine hesitancy (OR = 2.35, 95% CI: 1.24–4.45). Parents who responded to the survey in Chinese had higher odds of a child who did not initiate the HPV vaccine compared to English survey parents (OR = 2.70, 95% CI: 1.10–6.65). Similar observations were observed between parents with younger children aged 9–10 (OR = 3.09, 95% CI: 1.52–6.29), or 11–13 (OR = 1.96, 95% CI: 1.13–3.38) compared to those with children ages 14–17, parents with sons compared to daughters (OR = 1.84, 95% CI: 1.16–2.94), and those with children who did not receive the Tdap vaccine compared to those who did receive the Tdap vaccine (OR = 2.53, 95% CI: 1.41–4.55) for lack of initiating the HPV vaccine. Parental race/ethnicity, age, gender, education, nativity and acculturation as well as adolescent insurance type were also not statistically significant in the unadjusted associations with HPV vaccine initiation and omitted from the multivariable analyses and Table 3.
After adjusting for survey language, child age and sex, receipt of Tdap and Influenza immunizations and child COVID-19 vaccine intent, the relationship between high HPV vaccine hesitancy and lack of HPV vaccine initiation increased slightly (aOR = 2.78, 95% CI: 1.27–6.06) in the multivariable model. We found that parents who responded to the survey in Spanish where half as likely to have a child who had not received the HPV vaccine compared to those who responded to the survey in English (aOR = 0.50, 95% CI: 0.28–0.91); the direction and significance of the other covariates remained the same. We did not find a statistically significant association between medical mistrust and HPV vaccine initiation in the bivariate or multivariable analyses.
Discussion
Vaccine hesitancy is a key concern in adequately protecting populations from vaccine-preventable diseases, including HPV-associated cancers. Our findings indicate nearly one-fifth of parents are hesitant towards HPV vaccines in our study of primarily low-income, Hispanic/Latino and Asian American, immigrant parents. Reports of parental HPV vaccine hesitancy in our study (20%) were slightly lower compared to two recent studies using nationally representative samples (23–25%) of parents (Helmkamp et al., 2021; Szilagyi et al., 2020). Furthermore, reports of parental HPV vaccine hesitancy in our study were also lower than parental hesitancy for influenza vaccines for adolescents in other studies (25.8% and 26.1%) (Helmkamp et al., 2021; Kempe et al., 2020). Previous studies have noted similar proportions of hesitant parents and rationale behind HPV vaccine and influenza vaccine hesitancy due to parent lack of confidence in the effectiveness of both vaccines and the perception that these vaccines are optional (Helmkamp et al., 2021; Kempe et al., 2020; Szilagyi et al., 2020). The lower proportion of HPV vaccine hesitant parents in our sample may be due to the fact that three-fourths of our sample identified as Hispanic/Latino and prior studies have found lower rates of vaccine hesitancy among Hispanic/Latino parents compared to other racial/ethnic groups (Kempe et al., 2020; Szilagyi et al., 2020).
Parents who reported high levels of medical mistrust were more likely to have high HPV vaccine hesitancy. The COVID-19 pandemic has highlighted the relationship between vaccine hesitancy and medical mistrust across multiple racial/ethnic groups in the US (Khubchandani & Macias, 2021; Nguyen et al., 2021; Thompson et al., 2021). Prior use of the medical mistrust scale has shown a relationship between mistrust and decreased cervical cancer screening among rural white women (Hall et al., 2018), decreased intention to be screened for and negative perceptions about colorectal cancer among African Americans (Purnell et al., 2010), and negative attitudes towards prostate cancer screening among urban Black men (Shelton et al., 2010). Increased availability and exposure to misinformation on vaccines, including for HPV, influenza, and COVID-19, has created an environment that promotes hesitancy, especially among racial/ethnic minorities that may already have mistrust of the system. A legacy of medical mistrust exists among racial/ethnic minorities, due in part to the Tuskegee study, involuntary sterilization of Hispanic/Latino women in Los Angeles, and ongoing experiences of discrimination by the healthcare system. The association between high medical mistrust and high HPV vaccine hesitancy among parents, of whom a great majority identified as Hispanic/Latino, highlights the ongoing health disparities and inequities that are rooted in historical acts of social injustice and discriminatory health policies, educational and social services to “illegal aliens” in California (Stern, 2005). Our findings, where exposure to negative information about the HPV vaccine and general mistrust of the medical system and health care providers remained as important influences on parental hesitancy towards the HPV vaccine, even after controlling for adolescent gender and age, indicate the need to address hesitancy from a multi-level perspective that includes current misinformation and historical contexts within communities.
HPV vaccine initiation among adolescents in our study was alarmingly low compared to the California state average (43.7% vs. 78.7%). Similar to the study conducted by Szilagyi and colleagues, where adolescents of HPV vaccine hesitant parents were less likely to receive the HPV vaccine (Szilagyi et al., 2020), adolescents of parents with high HPV vaccine hesitancy had were less likely to have initiated the HPV vaccine in our study. Newness of the HPV vaccine, a specific item within the hesitancy scale, has been previously identified as a barrier to HPV vaccination (Gidengil et al., 2019; Holman et al., 2014; Szilagyi et al., 2020) and was also indicated by parents as a concern in our study. Although HPV vaccines have been routinely recommended for adolescents in the US for over a decade, low awareness of the vaccine (Amboree & Darkoh, 2020; Wisk et al., 2014), limited exposure to HPV vaccine information, especially in-language materials (Bastani et al., 2011; Jeudin et al., 2014), and lack of strong physician recommendation (Gilkey & McRee, 2016) are likely contributors to parental perception that HPV vaccines are still new. Furthermore, our study was conducted during the initial COVID-19 vaccine rollout for individuals ages 16 and over in the US and prior to the recommended use among adolescents ages 12–15 years. Although our study specifically measured HPV vaccine hesitancy, the observed relationship between parental COVID-19 vaccine intent for adolescents and parental HPV vaccine hesitancy further indicates the need to study both the shared factors contributing to vaccine hesitancy in general and distinct factors related to hesitancy for specific vaccines as efforts to catch-up missed HPV vaccine doses across high-risk communities continue.
Some limitations to this study include the following: First, few African American parents were included in this sample. While recruitment through the USC NAI program allowed us to understand views on HPV vaccines among primarily immigrant, low-income parents from communities where HPV vaccine uptake is low, our sample may not be representative of all medically underserved parents of HPV vaccine-eligible adolescents in Los Angeles. Furthermore, although our study leverages the racial/ethnic diversity among the communities of Los Angeles, our findings may not be generalizable to other geographic areas that are more homogenous in race/ethnicity. Second, to adapt to the confines of participant recruitment and data collection during the COVID-19 pandemic, only parents who were able to attend the virtual NAI parent workshops on Saturdays were introduced to the study and recruited for participation. Although the USC NAI and research team members were available in real-time during the workshops to answer questions about the survey, parents experiencing additional barriers to technology and those not within the NAI program were not part of the study. Third, we did not assess health literacy in our survey instrument. Parents with lower health literacy levels may be less inclined to complete the survey, more likely to have missing data, or have answered inaccurately. However, we worked in close partnership with the NAI Program leadership and staff, who interact with parents on a routine basis over several years on topics including COVID-19, vaccinations, safety, and social and emotional well-being. Our study materials were reviewed thoroughly for the appropriateness for the target parent populations. Fourth, while we captured the relationship between HPV vaccine hesitancy and COVID-19 vaccine intentions, we did not specifically measure COVID-19 vaccine or general vaccine hesitancy, which may limit the applicability of our findings in addressing other vaccine-related hesitancy. Furthermore, our exposure to negative HPV vaccine information item was not validated. Lastly, our study captured parental views on HPV vaccine hesitancy, medical mistrust, and other factors in a cross-sectional snapshot during the COVID-19 pandemic, when the national focus on vaccinations was heightened and may have impacted the parental survey responses differently than if the study were conducted in pre-pandemic times. Nonetheless, the impact of COVID-19 vaccines on parental HPV vaccine hesitancy is likely relevant going forward.
Although evidence has pointed to the need for multi-component strategies for HPV vaccine improvement within communities and healthcare settings, these strategies must now also incorporate factors that contribute to vaccine misinformation and broader historical contexts that impact trust in the health care system and uptake of preventive services. Locally focused, multilevel approaches to comprehensively identify factors associated with HPV vaccine hesitancy in low-uptake communities are necessary to engage and inform stakeholders on how to address HPV vaccine hesitancy. Our findings highlight needed efforts to simultaneously address logistical barriers to accessing routine adolescent preventive care as well as sources of vaccine hesitancy rooted in broader aspects of medical mistrust and exposure to negative vaccine information to optimize HPV vaccine uptake in medically underserved communities.
Acknowledgements
We thank The University of Southern California (USC) Leslie and William McMorrow Neighborhood Academic (NAI) leadership, staff and volunteers for their contributions this study. We are immensely grateful for the NAI parents for their participation. We acknowledge Saira Mayet and Levi Bonnell for their early contributions to survey design and data collection. This study was supported by a National Cancer Institute supplement to USC Norris Comprehensive Cancer Center parent grant P30 CA014089, R01 CA74397, and R25 CA225513 (which supported Alec Allee-Munoz).
Authors' contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Jennifer Tsui, Bibiana Martinez, Ivonne Rodriguez, Jazmin Navarro, Kim R. Thomas-Barrios, W. Martin Kast, and Lourdes Baezconde-Garbanati. The first draft of the manuscript was written by Jennifer Tsui, Bibiana Martinez, Michelle Shin, and Alec Allee-Munoz and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This study was funded by a National Cancer Institute supplement to USC Norris Comprehensive Cancer Center parent grant P30 CA014089. W. Martin Kast was supported by R01 CA74397 and Alec Allee-Munoz was supported by R25 CA225513.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This is an observational study. The University of Southern California Institutional Review Board (IRB) approved this as an exempt study, where written/signed consent was not required, due to the anonymous nature of the survey.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Amboree TL, Darkoh C. Barriers to human papillomavirus vaccine uptake among racial/ethnic minorities: A systematic review. Journal of Racial and Ethnic Health Disparities. 2020 doi: 10.1007/s40615-020-00877-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aragones A, Genoff M, Gonzalez C, Shuk E, Gany F. HPV vaccine and Latino immigrant parents: If they offer it, we will get it. Journal of Immigrant and Minority Health. 2016;18:1060–1065. doi: 10.1007/s10903-015-0225-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashing KT, Carrington A, Ragin C, Roach V. Examining HPV- and HPV vaccine-related cognitions and acceptability among US-born and immigrant Hispanics and US-born and immigrant non-Hispanic blacks: A preliminary catchment area study. Cancer Causes and Control. 2017;28:1341–1347. doi: 10.1007/s10552-017-0973-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baezconde-Garbanati L, Lienemann BA, Robles M, Johnson E, Sanchez K, Singhal R, Steinberg J, Jaque JM, Pentz MA, Gruber S. Implementation of HPV vaccination guidelines in a diverse population in Los Angeles: Results from an environmental scan of local HPV resources and needs. Vaccine. 2017;35:4930–4935. doi: 10.1016/j.vaccine.2017.07.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastani R, Glenn BA, Tsui J, Chang LC, Marchand EJ, Taylor VM, Singhal R. Understanding suboptimal human papillomavirus vaccine uptake among ethnic minority girls. Cancer Epidemiology, Biomarkers & Prevention. 2011;20:1463–1472. doi: 10.1158/1055-9965.EPI-11-0267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd ED, Phillips JM, Schoenberger YM, Simpson T. Barriers and facilitators to HPV vaccination among rural Alabama adolescents and their caregivers. Vaccine. 2018;36:4126–4133. doi: 10.1016/j.vaccine.2018.04.085. [DOI] [PubMed] [Google Scholar]
- Casillas A, Singhal R, Tsui J, Glenn BA, Bastani R, Mangione CM. The impact of social communication on perceived HPV vaccine effectiveness in a low-income, Minority Population. Ethnicity & Disease. 2011;21:495–501. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2019). The 2019 National Immunization Survey: Teen. Retrieved from https://www.cdc.gov/vaccines/imz-managers/nis/datasets-teen.html.
- Centers for Disease Control and Prevention. (2020). Increase the Proportion of Adolescents Who Get Recommended Doses of the HPV Vaccine—IID‑08. In: Healthy People 2030. Retrieved from https://health.gov/healthypeople/objectives-and-data/browse-objectives/vaccination/increase-proportion-adolescents-who-get-recommended-doses-hpv-vaccine-iid-08.
- Centers for Disease Control and Prevention. (2021). HPV Vaccination Coverage among Adolescents Age 13–17 Years, Survey Years 2015–2019, United States, National Immunization Survey—Teen. Retrieved from https://www.cdc.gov/vaccines/imz-managers/coverage/teenvaxview/data-reports/index.html.
- Cooper, S., Schmidt, B. M., Ryan, J., Leon, N., Mavundza, E., Burnett, R., Tanywe, A. C., & Wiysonge, C. S. (2019). Factors that influence acceptance of human papillomavirus (HPV) vaccination for adolescents: A qualitative evidence synthesis. Cochrane Database of Systematic Reviews,9. 10.1002/14651858.CD013430.
- Dehlendorff C, Baandrup L, Kjaer SK. Real-world effectiveness of human papillomavirus vaccination against vulvovaginal high-grade precancerous lesions and cancers. Journal of the National Cancer Institute. 2021;113:869–874. doi: 10.1093/jnci/djaa209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elam-Evans LD, Yankey D, Singleton JA, Sterrett N, Markowitz LE, Williams CL, Fredua B, McNamara L, Stokley S. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2019. MMWR Morbidity and Mortality Weekly Report. 2020;69:1109–1116. doi: 10.15585/mmwr.mm6933a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gidengil C, Chen C, Parker AM, Nowak S, Matthews L. Beliefs around childhood vaccines in the United States: A systematic review. Vaccine. 2019;37:6793–6802. doi: 10.1016/j.vaccine.2019.08.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilkey MB, McRee AL. Provider communication about HPV vaccination: A systematic review. Human Vaccines & Immunotherapeutics. 2016;12:1454–1468. doi: 10.1080/21645515.2015.1129090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn BA, Tsui J, Coronado GD, Fernandez ME, Savas LS, Taylor VM, Bastani R. Understanding HPV vaccination among Latino adolescent girls in three US regions. Journal of Immigrant and Minority Health. 2015;17:96–103. doi: 10.1007/s10903-014-9996-8. [DOI] [PubMed] [Google Scholar]
- Glenn BA, Tsui J, Singhal R, Sanchez L, Nonzee NJ, Chang LC, Taylor VM, Bastani R. Factors associated with HPV awareness among mothers of low-income ethnic minority adolescent girls in Los Angeles. Vaccine. 2015;33:289–293. doi: 10.1016/j.vaccine.2014.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield LS, Page LC, Kay M, Li-Vollmer M, Breuner CC, Duchin JS. Strategies for increasing adolescent immunizations in diverse ethnic communities. Journal of Adolescent Health. 2015;56:S47–53. doi: 10.1016/j.jadohealth.2014.10.274. [DOI] [PubMed] [Google Scholar]
- Hall MB, Vos P, Bess JJ, Reburn KL, Locklear GD, McAlister J, Bell RA. Cervical cancer screening behaviors and perceptions of medical mistrust among rural black and white women. Journal of Health Care for the Poor and Underserved. 2018;29:1368–1385. doi: 10.1353/hpu.2018.0101. [DOI] [PubMed] [Google Scholar]
- Hanson KE, Koch B, Bonner K, Mcree A-L, Basta NE. National trends in parental human papillomavirus vaccination intentions and reasons for hesitancy, 2010–2015. Clinical Infectious Diseases. 2018;67:1018–1026. doi: 10.1093/cid/ciy232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harder T, Wichmann O, Klug SJ, van der Sande MAB, Wiese-Posselt M. Efficacy, effectiveness and safety of vaccination against human papillomavirus in males: A systematic review. BMC Medicine. 2018;16:110. doi: 10.1186/s12916-018-1098-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helmkamp LJ, Szilagyi PG, Zimet G, Saville AW, Gurfinkel D, Albertin C, Breck A, Vangala S, Kempe A. A validated modification of the vaccine hesitancy scale for childhood, influenza and HPV Vaccines. Vaccine. 2021;39:1831–1839. doi: 10.1016/j.vaccine.2021.02.039. [DOI] [PubMed] [Google Scholar]
- Hickler B, Guirguis S, Obregon R. Vaccine special issue on vaccine hesitancy. Vaccine. 2015;33:4155–4156. doi: 10.1016/j.vaccine.2015.04.034. [DOI] [PubMed] [Google Scholar]
- Hirth J. Disparities in HPV vaccination rates and HPV prevalence in the United States: A review of the literature. Human Vaccines & Immunotherapeutics. 2019;15:146–155. doi: 10.1080/21645515.2018.1512453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirth JM, Fuchs EL, Chang M, Fernandez ME, Berenson AB. Variations in reason for intention not to vaccinate across time, region, and by race/ethnicity, NIS-Teen (2008–2016) Vaccine. 2019;37:595–601. doi: 10.1016/j.vaccine.2018.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: A systematic review of the literature. JAMA Pediatrics. 2014;168:76–82. doi: 10.1001/jamapediatrics.2013.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeudin P, Liveright E, Del Carmen MG, Perkins RB. Race, ethnicity, and income factors impacting human papillomavirus vaccination rates. Clinical Therapeutics. 2014;36:24–37. doi: 10.1016/j.clinthera.2013.11.001. [DOI] [PubMed] [Google Scholar]
- Karafillakis E, Simas C, Jarrett C, Verger P, Peretti-Watel P, Dib F, De Angelis S, Takacs J, Ali KA, Pastore Celentano L, Larson H. HPV vaccination in a context of public mistrust and uncertainty: A systematic literature review of determinants of HPV vaccine hesitancy in Europe. Human Vaccines & Immunotherapeutics. 2019;15:1615–1627. doi: 10.1080/21645515.2018.1564436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempe A, Saville AW, Albertin C, Zimet G, Breck A, Helmkamp L, Vangala S, Dickinson LM, Rand C, Humiston S, Szilagyi PG. Parental hesitancy about routine childhood and influenza vaccinations: A national survey. Pediatrics. 2020;146:e20193852. doi: 10.1542/peds.2019-3852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khubchandani J, Macias Y. COVID-19 vaccination hesitancy in Hispanics and African-Americans: A review and recommendations for practice. Brain, Behavior, & Immunity - Health. 2021;15:100277. doi: 10.1016/j.bbih.2021.100277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornfeld J, Byrne MM, Vanderpool R, Shin S, Kobetz E. HPV knowledge and vaccine acceptability among Hispanic fathers. The Journal of Primary Prevention. 2013;34:59–69. doi: 10.1007/s10935-013-0297-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson HJ, Jarrett C, Schulz WS, Chaudhuri M, Zhou Y, Dube E, Schuster M, MacDonald NE, Wilson R. Measuring vaccine hesitancy: the development of a survey tool. Vaccine. 2015;33:4165–4175. doi: 10.1016/j.vaccine.2015.04.037. [DOI] [PubMed] [Google Scholar]
- Los Angeles County Department of Public Health. (2018). Percent of Children (Ages 11 to 17 Years) Who Have Received at Least One Dose of Human Papilloma Virus (HPV). In 2018 LA County Health Survey - Topics & Data.
- Madhivanan P, Pierre-Victor D, Mukherjee S, Bhoite P, Powell B, Jean-Baptiste N, Clarke R, Avent T, Krupp K. Human papillomavirus vaccination and sexual disinhibition in females. American Journal of Preventive Medicine. 2016;51:373–383. doi: 10.1016/j.amepre.2016.03.015. [DOI] [PubMed] [Google Scholar]
- Meites E, Kempe A, Markowitz LE. Use of a 2-Dose schedule for human papillomavirus vaccination—Updated recommendations of the advisory committee on immunization practices. MMWR Morbidity and Mortality Weekly Report. 2016;65:1405–1408. doi: 10.15585/mmwr.mm6549a5. [DOI] [PubMed] [Google Scholar]
- Moran MB, Chatterjee JS, Frank LB, Murphy ST, Zhao N, Chen N, Ball-Rokeach S. Individual, cultural and structural predictors of vaccine safety confidence and influenza vaccination among Hispanic female subgroups. Journal of Immigrant and Minority Health. 2017;19:790–800. doi: 10.1007/s10903-016-0428-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran MB, Frank LB, Chatterjee JS, Murphy ST, Baezconde-Garbanati L. Information scanning and vaccine safety concerns among African American, Mexican American, and non-Hispanic white women. Patient Education and Counseling. 2016;99:147–153. doi: 10.1016/j.pec.2015.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen, L. H., Joshi, A. D., Drew, D. A., Merino, J., Ma, W., Lo, C. H., Kwon, S., Wang, K., Graham, M. S., Polidori, L., Menni, C., Sudre, C. H., Anyane-Yeboa, A., Astley, C. M., Warner, E. T., Hu, C. Y., Selvachandran, S., Davies, R., Nash, D., Franks, P. W., Wolf, J., Ourselin, S., Steves, C. J., Spector, T. D., & Chan, A. T. (2021). Racial and ethnic differences in COVID-19 vaccine hesitancy and uptake. medRxiv. 10.1101/2021.02.25.21252402
- Norris AE, Ford K, Bova CA. Psychometrics of a brief acculturation scale for Hispanics in a probability sample of urban Hispanic adolescents and young adults. Hispanic Journal of Behavioral Sciences. 1996;18:29–38. doi: 10.1177/07399863960181004. [DOI] [Google Scholar]
- Painter JE, de Viana OMS, Jimenez L, Avila AA, Sutter CJ, Sutter R. Vaccine-related attitudes and decision-making among uninsured, Latin American immigrant mothers of adolescent daughters: A qualitative study. Human Vaccines & Immunotherapeutics. 2019;15:121–133. doi: 10.1080/21645515.2018.1514353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel Murthy B, Zell E, Kirtland K, Jones-Jack N, Harris L, Sprague C, Schultz J, Le Q, Bramer CA, Kuramoto S, Cheng I, Woinarowicz M, Robison S, McHugh A, Schauer S, Gibbs-Scharf L. Impact of the COVID-19 pandemic on administration of selected routine childhood and adolescent vaccinations - 10 U.S. Jurisdictions, March-September 2020. MMWR Morbidity and Mortality Weekly Report. 2021;70:840–845. doi: 10.15585/mmwr.mm7023a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel PR, Berenson AB. Sources of HPV vaccine hesitancy in parents. Human Vaccines & Immunotherapeutics. 2013;9:2649–2653. doi: 10.4161/hv.26224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purnell JQ, Katz ML, Andersen BL, Palesh O, Figueroa-Moseley C, Jean-Pierre P, Bennett N. Social and cultural factors are related to perceived colorectal cancer screening benefits and intentions in African Americans. Journal of Behavioral Medicine. 2010;33:24–34. doi: 10.1007/s10865-009-9231-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pytynia KB, Dahlstrom KR, Sturgis EM. Epidemiology of HPV-associated oropharyngeal cancer. Oral Oncology. 2014;50:380–386. doi: 10.1016/j.oraloncology.2013.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roncancio AM, Ward KK, Carmack CC, Muñoz BT, Cribbs FL. Hispanic mothers’ beliefs regarding HPV vaccine series completion in their adolescent daughters. Health Education Research. 2017;32:96–106. doi: 10.1093/her/cyw055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelton RC, Winkel G, Davis SN, Roberts N, Valdimarsdottir H, Hall SJ, Thompson HS. Validation of the group-based medical mistrust scale among urban black men. Journal of General Internal Medicine. 2010;25:549–555. doi: 10.1007/s11606-010-1288-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern AM. STERILIZED in the name of public health. American Journal of Public Health. 2005;95:1128–1138. doi: 10.2105/AJPH.2004.041608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strategic Advisory Group of Experts on Immunization. (2014). Report on the SAGE working group on vaccine hesitancy. Retrieved from https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf.
- Szilagyi PG, Albertin CS, Gurfinkel D, Saville AW, Vangala S, Rice JD, Helmkamp L, Zimet GD, Valderrama R, Breck A, Rand CM, Humiston SG, Kempe A. Prevalence and characteristics of HPV vaccine hesitancy among parents of adolescents across the US. Vaccine. 2020;38:6027–6037. doi: 10.1016/j.vaccine.2020.06.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabrizi SN, Brotherton JML, Kaldor JM, Skinner SR, Cummins E, Liu B, Bateson D, Mcnamee K, Garefalakis M, Garland SM. Fall in human papillomavirus prevalence following a national vaccination program. Journal of Infectious Diseases. 2012;206:1645–1651. doi: 10.1093/infdis/jis590. [DOI] [PubMed] [Google Scholar]
- Thompson HS, Manning M, Mitchell J, Kim S, Harper FWK, Cresswell S, Johns K, Pal S, Dowe B, Tariq M, Sayed N, Saigh LM, Rutledge L, Lipscomb C, Lilly JY, Gustine H, Sanders A, Landry M, Marks B. Factors associated with racial/ethnic group-based medical mistrust and perspectives on COVID-19 vaccine trial participation and vaccine uptake in the US. JAMA Network Open. 2021;4:e2111629. doi: 10.1001/jamanetworkopen.2021.11629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson HS, Valdimarsdottir HB, Winkel G, Jandorf L, Redd W. The group-based medical mistrust scale: psychometric properties and association with breast cancer screening. Preventative Medicine. 2004;38:209–218. doi: 10.1016/j.ypmed.2003.09.041. [DOI] [PubMed] [Google Scholar]
- Tsui J, Gee GC, Rodriguez HP, Kominski GF, Glenn BA, Singhal R, Bastani R. Exploring the role of neighborhood socio-demographic factors on HPV vaccine initiation among low-income, ethnic minority girls. Journal of Immigrant and Minority Health. 2013;15:732–740. doi: 10.1007/s10903-012-9736-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsui, J., Vincent A, Anuforo B, Btoush R, & BF, C. (2019). Physician reported communication strategies for HPV vaccine recommendation: A qualitative study within a large academic hospital system. In Paper presented at the 6th NCI cancer centers HPV vaccination summit, simmons comprehensive cancer center. Dallas, TX.
- Van Dyne EA, Henley SJ, Saraiya M, Thomas CC, Markowitz LE, Benard VB. Trends in human papillomavirus-associated cancers—United States, 1999–2015. MMWR Morbidity and Mortality Weekly Report. 2018;67:918–924. doi: 10.15585/mmwr.mm6733a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victory M, Do TQN, Kuo YF, Rodriguez AM. Parental knowledge gaps and barriers for children receiving human papillomavirus vaccine in the Rio Grande valley of Texas. Human Vaccines & Immunotherapeutics. 2019;15:1678–1687. doi: 10.1080/21645515.2019.1628551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vu M, Berg CJ, Escoffery C, Jang HM, Nguyen TT, Travis L, Bednarczyk RA. A systematic review of practice-, provider-, and patient-level determinants impacting Asian-Americans' human papillomavirus vaccine intention and uptake. Vaccine. 2020;38:6388–6401. doi: 10.1016/j.vaccine.2020.07.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner EL, Lai D, Carbajal-Salisbury S, Garza L, Bodson J, Mooney K, Kepka D. Latino parents’ perceptions of the HPV vaccine for sons and daughters. Journal of Community Health. 2015;40:387–394. doi: 10.1007/s10900-014-9949-0. [DOI] [PubMed] [Google Scholar]
- Wisk LE, Allchin A, Witt WP. Disparities in human papillomavirus vaccine awareness among U.S. Parents of preadolescents and adolescents. Sexually Transmitted Diseases. 2014;41:117–122. doi: 10.1097/olq.0000000000000086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu L, Selk A, Garland SM, Bogliatto F, Kyrgiou M, Weyers S, Arbyn M. Prophylactic vaccination against human papillomaviruses to prevent Vulval and vaginal cancer and their precursors. Expert Review of Vaccines. 2019;18:1157–1166. doi: 10.1080/14760584.2019.1692658. [DOI] [PubMed] [Google Scholar]