Abstract
South America comprises of heterogeneous topographies, populations, and health care systems. Therefore, it is not surprising to see differences among the countries regarding expertise, education, and practices of ophthalmic genetics for patients with rare eye diseases. Nevertheless, common challenges such as limited genetics training in medical schools and among ophthalmologists, scarcity of diagnostic tools for phenotyping, and expensive genetic testing not covered by the public healthcare systems, are seen in all of them. Here, we provide a detailed report of the current status of ophthalmic genetics, described by the personal views of local ophthalmologists from Brazil, Colombia, Argentina, and Chile. By reporting our strengths and weaknesses as a region, we intend to highlight the need for guidelines on how to manage these patients aligned with public health policies. Our region contributes to research worldwide, with thousands of well diagnosed patients from a number of unique and genetically diverse populations. The constant expansion of ophthalmic genetics and molecular diagnostics requires us to join forces to collaborate across South America and with other countries to improve access to next-generation diagnostics and ultimately improve patient care.
Keywords: development, genetics, ophthalmology, ophthalmic genetics, South America
1 |. INTRODUCTION
South America is a region that comprises 13 sovereign states: Brazil, Colombia, Argentina, Peru, Venezuela, Chile, Ecuador, Bolivia, Paraguay, Uruguay, Guyana, Surinam, and French Guiana, listed here from the most populated to the least (Figure 1) (United Nations Department of Economic and Social Affairs, 2019). It involves all of the subequatorial Americas and it is divided from Central America around Panama’s Isthmus. South America’s first inhabitants arrived possibly from Northeast Asia around 14,000 years ago, and developed civilizations throughout the continent (Moya, 2018). Migratory currents from Europe, mainly Portugal, Spain, France and the Netherlands started arriving on the 18th century, prompted by the gold, silver, and diamonds in our region. European migrants also brought West Africans to work as slaves in the mines. Around one quarter of the colonizers were women, enabling the perpetuation of their culture locally as well as the development of a new race, derived from their mating with indigenous people (Armus & Denis, 2011). The official language in Brazil is Portuguese; in French Guiana, French; and in the rest of the countries, Spanish. Many native dialects however, such as Quechua and Guarani remain in use in certain regions (mainly Peru and Paraguay, respectively). Between the mid-19th century and the 1930s world depression, South America received the largest population inflow of its history, from Europe (Moya, 2014). The majority were Italian, followed by Spanish and Portuguese. Around half of them went to Argentina, one third to Brazil and the remaining to the rest of the region’s countries (Moya, 1998). Several Jewish migrants arrived as well, due to their diaspora during World War II and more recently, Japanese and Chinese. Brazil, specially São Paulo, has the largest Japanese community outside Japan and the largest Syrian Lebanese colony overseas.
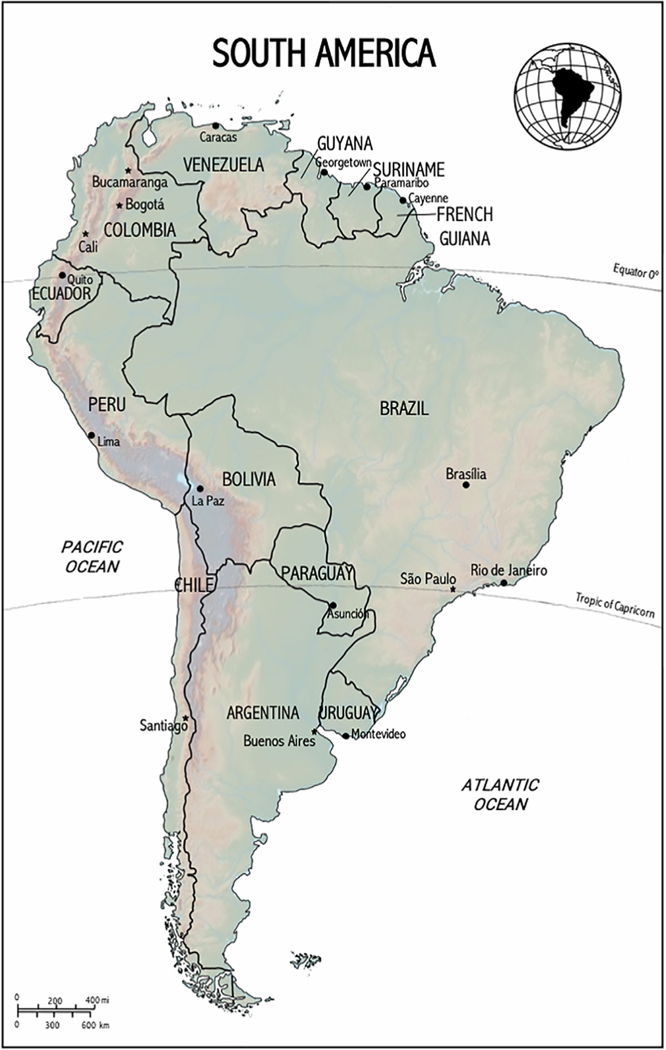
FIGURE 1.
Map of South America. The cities marked with starts represent those mentioned in this report. Those with dots correspond to capital and big cities within the region
Mao and colleagues described the Latino population as the result of a two-way admixture between Native Americans and Europeans, or a three-way admixture of Native American, European, and West African populations (Mao et al., 2007). Homburger et al. used genome-wide single nucleotide polymorphism (SNP) data to calculate the genetic ancestry of a few South American countries and concluded that European ancestry was the most important one in Argentina (67%), Colombia (62%), and Chile (57%), whereas in Ecuador and Peru, Native American was the most prevalent one (50 and 68%, respectively) (Homburger et al., 2015). West African and East Asian genes were present in up to 9 and 2.5%, in Colombia and Peru respectively. Adhikari et al. reported 79% European ancestry in Brazil (combined with 12% Native American and 9% African), and an even contribution of European and Native American in Chile (46 and 49%, respectively) (Adhikari, Mendoza-Revilla, Chacón-Duque, Fuentes-Guajardo, & Ruiz-Linares, 2016).
Medical genetics has been officially recognized as a subspecialty in many countries of the region for over 30 years. The first Newborn Screening (NBS) approach in South America was in Brazil in 1976 and the first NBS programs started in Argentina in 1985 and in Chile in 1992 (Belló & Becerril-Montekio, 2011; Borrajo, 2007). NBS programs have become a tool to assess how developed the genetics field is within a country, as well as the awareness of rare diseases and the effort toward their diagnosis through a public health program (District of Columbia Department of Health, 2010; Hoehn et al., 2013). But the importance of NBS reflecting the country’s development relays on how it is kept up to speed with the expansion of genetics and genomics worldwide. In this area, Brazil has shown the most interest in NBS within the region, adding new conditions to screen and expanding their coverage (Therrell & Padilla, 2018). NBS in Argentina, Colombia, and Brazil includes an ophthalmologic evaluation with the main objective of ruling out gross defects such as congenital cataracts.
Four professionals won a Nobel Prize in Science in South America. Dr. Bernardo Houssay, from Argentina, won in 1947 for his discovery of the part played by the hormone of the anterior pituitary lobe in the metabolism of sugar. Dr. Baruj Benacerraf, Venezuelan, won the Nobel Prize in Physiology or Medicine in 1980 for his discoveries concerning genetically determined structures on the cell surface that regulate immunological reactions. Dr. César Milstein, Argentinian, won the Nobel Prize in Physiology or Medicine in 1984 for theories concerning the specificity in development and control of the immune system and the discovery of the principle for production of monoclonal antibodies. And Dr. Luis Federico Leloir, from Argentina, won the Nobel Prize in Chemistry in 1987 for his discovery of sugar nucleotides and their role in the biosynthesis of carbohydrates (https://www.nobelprize.org/).
There are several Pan-American ophthalmology associations within our region, such as the Pan-American Association of Ophthalmology, Latin American Strabismus Council, Pan-American Retinopathy of Prematurity Society, and South American Pediatric Ophthalmology Society. There is also the Latin American Network of Human Genetics. However, ophthalmic genetics remains poorly developed in the region, with no officially recognized societies or consortiums.
In this article we address the current situation that our countries face while diagnosing and monitoring a patient with an inherited ocular condition. We also describe the challenges we deal with as interventional clinical trials for these patients continue to expand, with the aim of improving the collaboration between ophthalmology and medical genetics locally.
1.1 |. Brazil
Brazil is the largest country of the region (sixth worldwide, 8.515.770 km2) and has a population of 209.5 million inhabitants (Central Intelligence Agency, 2020). Within this country, 47.5% of the inhabitants consider their race or color to be white, 43.1% brown, 7.61% black, and the remaining yellow or indigenous (Instituto Brasileiro de Geografía e Estadística, 2015). There is a higher concentration of European ancestry on the Southern region and of African in the Northern.
The Brazilian public health system is called Unified Health System (Portuguese abbreviation, SUS) and it provides universal and free healthcare to all the inhabitants. Around 50 million people are also beneficiaries of private health plans. The SUS only provides genetic testing for ocular genetic disorders when they are a part of a syndrome, or under research basis.
The Brazilian Society of Medical Genetics and Genomics (consisting of around 100 Board certified geneticists) has established certain guidelines (Diretrizes) for some genetic conditions, but those for ocular genetics are still under development [Sociedade Brasileira de Genética Médica e Genômica (SBGM), 2020]. Brazil also launched the Rare Disease Policy in 2014, to promote research on rare diseases and their treatments. Infectious diseases during pregnancy however, are still a frequent cause of congenital malformations in Brazil (Ministério da Saúde, 2018).
As per genetic testing, Sanger sequencing became accessible in 1986, for research purposes only. Around 2006, commercial use DNA tests became available by sending the samples abroad, with few genes sequenced per disease (e.g., retinitis pigmentosa panel had only four genes) and high cost. In 2009, DNA Array made genetic testing more affordable and around 2011, next generation sequencing (NGS) allowed to test many genes simultaneously, which decreased the costs more and raised the yield of conclusive tests. A few years later, NGS became available in Brazil. This led to better pricing, reports written in the native language and a lab setting nearby in case a patient needed additional testing. Over the past 10 years, more than 15 commercial genetic labs were established in Brazil, with local management of the samples. Some of these labs developed their own bioinformatic analysis program as well as specific panels for inherited retinopathies (https://www.mendelics.com.br/en/oftalmologia/), including Brazilian variants. These are contained in ABraOM—Brazilian genomic variants (http://abraom.ib.usp.br/)—, a repository for local genomic variants.
Currently, clinical molecular diagnostic testing remains expensive but has become feasible for some private or insured patients. Individuals that relay in the public healthcare though, do not have access to genetic testing for ocular diseases and insurance companies are still not covering them. The development of genetics has transformed the diagnostic workflow and will soon change the management as well. Also, the price of genetic testing continues to decrease, costing now around the same as the rest of the workup these patients go through (fundus photography, autofluorescence, visual field, electrophysiology, and optic coherence tomography). The latter are even repeated to monitor disease’s progression, while molecular diagnosis is usually done once if the first test comes conclusive.
Brazilian ophthalmologists are well prepared to diagnose, manage and treat congenital cataract and glaucoma, subluxated lenses in people with Marfan syndrome and homocystinuria, and retinoschisis with retinal detachment in individuals with Stickler. The healthcare system however, makes the patient’s journey longer due to scarce specialized clinics concentrated in metropolitan areas, causing long waiting lists. Also, there are only 11 residency programs in Medical Genetics in this country, with 25 medical residency vacancies total, causing a shortage in these specialists.
The patients’ association Retina Brazil has 7,000 registered patients, among which 15% have been genotyped. Networks of ophthalmologists work as advisory boards within different regional patients’ associations, providing specialized inherited retinal degenerations (IRD) care. As of 2018, approximately 45% of the patients seen at the retinal dystrophy clinic of Federal University of São Paulo—UNIFESP—and Instituto de Genética Ocular had genetic testing, and 32% had a molecular diagnosis (Motta, Martin, Filippelli-Silva, Vallim Salles, & Sallum, 2018). The latter corresponds mainly to individuals with Leber’s Congenital Amaurosis (LCA), Stargardt disease and Choroideremia. For those with negative results, further analysis is pursued with collaborators. At the moment, there are some ongoing clinical trials for inherited retinal dystrophies at UNIFESP clinic. Brazil also collaborates in many multinational initiatives, providing molecularly diagnosed, deep phenotyped patients (Khan et al., 2020) and contributed to the discovery of NMNAT1 as a causative gene for a subset of individuals with LCA (Chiang et al., 2012).
The query “ophthalmic genetics Brazil” currently gives 80 results, which represents the largest number of the region (https://pubmed.ncbi.nlm.nih.gov/?term=ophthalmic+genetics+Brazil, queried on June 2020). These articles address syndromes, corneal and retinal dystrophies, congenital eye malformations and electrophysiology. Genetics training in medicine courses in Brazil is still not enough, but there is a continuing effort to teach students, ophthalmology residents and fellows and clinical geneticists, and create awareness about Ocular Genetics. Recently, the Brazilian Counsel of Ophthalmology published the first virtual textbook on Ocular Genetics, which will be used for teaching purposes throughout the country (Sallum, Abalem, Melo, & Finzi, 2019). This effort involved ophthalmologists from different fields of ocular genetics (anterior segment, glaucoma, retina), basic science, bioinformatics, and oncology.
1.2 |. Colombia
Colombia is the second most populated country in South America with 49.084.841 inhabitants, and the third biggest one with a total area of 1,138,910 km2 (Central Intelligence Agency, 2020). The population is ethnically diverse: 49% identify themselves as mestizo (mixed European and Native American ancestry), 37% as of European ancestry, 10% African ancestry, and 3.4% as Native American (Departamento Administrativo Nacional de Estadística, 2005). There is also a high prevalence of consanguinity in rural areas (Tapiero-Rodriguez et al., 2018). Access to healthcare services is provided by the universal general social security system under two modalities: contributing and subsidized. The contributing population pays a percentage of its income to subscribe to the health plan and the subsidized population access this system through the National State (Vargas-Zea, Castro, Rodríguez-Páez, Téllez, & Salazar-Arias, 2012). The basic health plan allows anyone in need to access medical genetic evaluation and genetic testing, after being referred by a local general practitioner. The challenge is that many providers are not familiar with clinical genetics as a specialty.
Rare diseases are recognized by the Colombian law as of special interest by the Ministry of Health. The National System of Surveillance in Public Health (Spanish abbreviation, SIVIGILA) requires mandatory notification of rare diseases (Ministerio de Salud, 2017). This law facilitates access to genetic testing for individuals with rare diseases, given government’s interest to guarantee opportune diagnosis and management of these disorders. Several registries have been developed to monitor diagnosis and incidence of rare diseases in the country (Mateus, Pérez, & Mesa, 2017). There are many barriers to this system yet, such as access, complexity for users, and high costs (Vargas-Zea et al., 2012). Congenital birth defects are also monitored by the Colombian government and Universities and Institutes in Bogotá, Pereira, and Cali have implemented surveillance programs (Pachajoa, Villota, & Cruz, 2015; Porras-Hurtado, León-Castañeda, & Molano-Hurtado, 2016; Zarante, Sarmiento, & Mallarino, 2016). These are part of the Latin American Collaborative Study of Congenital Malformations (Spanish abbreviation, ECLAMC) (Castilla & Orioli, 2004). These efforts have improved access to healthcare by patients with genetic diseases and awareness in the general population.
Clinical genetics training in medical schools in Colombia is limited. Most programs have genetics training during basic science semesters without direct clinical correlation. No clinical rotations are available to students. There are only two medical genetics residency programs in the country, and shortage of genetics professionals across the country. The estimated ratio of geneticists to inhabitants is 1 medical genetics doctor per every 1 million inhabitants. They work in medical genetics specialized centers that are typically located only in major cities of the country, limiting the access of patients located in less populated areas.
Individuals with genetic eye disorders are typically evaluated by an ophthalmologist who will then make a referral to a geneticist for a systemic evaluation and family history assessment. Genetic testing ordered by geneticists is then evaluated by the insurance company to determine medical necessity. The majority of clinical genetic studies are performed abroad, given the high costs of equipment, chemicals, and lack of trained personnel to operate new sequencing technologies locally. Recently however, due to insurance companies asking for less expensive testing, Universities, local laboratories and international genetic testing companies are collaborating towards establishing local testing capabilities.
A PubMed search of “ophthalmic genetics Colombia” provides the following peer-reviewed articles (n = 11). A study reports the prevalence of congenital eye defects in Colombia at 2.46 per 10,000 live births (Manotas & Sarmiento, 2019). The most common congenital eye defect in this study was microphthalmia-anophthalmia. Another article is a multination effort to understand retinoblastoma’s presentation by national income level, which found that patients with retinoblastoma in lower-income countries are more likely to present with a more advanced disease at the time of diagnosis, and poor prognosis. Colombia is classified as an upper-middle income country, and this study found that genetic tests are available in 42.4% of patients for this group, compared with 96.4% in high-income countries (Global Retinoblastoma Study Group, Fabian, & Abdallah, 2020). A novel genetic disorder related to TAF1 mutations was described in a Colombian family with a new recognizable hereditary syndrome (O’Rawe, Wu, & Dörfel, 2015), and other manuscripts report cases of oculocutaneous albinism, X-linked retinoschisis, gelatinous drop-like corneal dystrophy, and Fabry disease (Mendoza-Londono, Hiriyanna, & Bingham, 1999; Morantes et al., 2016; Rothstein et al., 2019; Sanabria, Groot, Guzmán, & Lattig, 2012). A case report describes findings in a Colombian family with 9 of 22 members affected by Criswick-Schepens syndrome (Nicholson & Galvis, 1984). Lastly, the results of two screening programs were published, identifying 95 individuals with Waardenburg syndrome among 1,763 deaf persons and reporting the prevalence of Usher syndrome to be 3.2:100,000 individuals within Colombian population (Tamayo et al., 1991; Tamayo et al., 2008).
1.3 |. Argentina
Argentina is the third most populated country in South America, with around 45 million inhabitants, and the second one in area (2,780,400 km2) (Central Intelligence Agency, 2020). There is no race category in the Argentinian census, therefore it is difficult to assess the ethnic groups’ percentages within the Nation. An interesting point to underscore though is the Argentinian genetic heterogeneity, where around 76% of the population of City of Buenos Aires has European ancestry whereas this represents 33% in the north of the country (Avena et al., 2012). Argentina’s healthcare system has three sectors: public, social security and private. The public one assists around 14 million people a year through public hospitals and primary health care units, financed with taxes and payments made by social security beneficiaries that use these facilities. Social security’s sector covers every legal worker and their families (18 million individuals a year), usually with their own clinics and funded by the employer and a percentage of the employees’ salaries. The private sector corresponds to private insurance companies and is financed by individual payments, providing service to around 3 million people yearly (Belló & Becerril-Montekio, 2011). Genetic testing for individuals with ophthalmic genetics’ disorders is not covered regularly by any sector of the healthcare system.
The National Center of Medical Genetics (CENAGEM) reports that up to August 2017 there were 51 genetic laboratories and 45 consult services available through public institutions throughout Argentina (Centro Nacional de Genética Médica, 2017a). The genetic tests performed in these centers include cytogenetics, Fluorescence in situ hybridization (FISH), and NGS (Centro Nacional de Genética Médica, 2017b). There are around 20 NGS devices in the country and sequencing is performed both locally and outsourced to other countries such as Brazil and Spain (Vishnopolska, 2018). Array-CGH was introduced by CENAGEM in 2014 and is currently being incorporated by other institutions as well (Cotignola, 2019). The National Administration of Health Laboratories and Institutions (ANLIS) states that 76 genetic disorders can be diagnosed through the public health system of our country (Centro Nacional de Genética Médica, 2017c). Of these, only one is purely eye related: retinoblastoma, and a few have ophthalmic manifestations as part of a systemic condition (i.e., X-linked adrenoleukodystrophy, congenital disorders of glycosylation, and lysosomal storage disorders). Argentina has an Argentinian Genetics Society founded in 1969, a public repository of anonymized genomic and epidemiological information of patients within the Argentine Hereditary Cancer Network (SITHER, http://www.inc.gob.ar/sither/docs/), and a National Registry of Congenital Anomalies (RENAC, http://www.msal.gov.ar/congenitas/renac-el-registro-nacional-de-anomalias-congenitas/). There is also a well-developed retinoblastoma program, led by ocular oncologists and several pioneers in the area of medicine and chemistry.
Genetics-related didactics is scarce in the curriculum of local Medical Schools and there are only a few locations with a handful of slots to get formal postgraduate training in Medical Genetics (Ministerio de Salud, 2020). There are 1.3 genetics institutions, 1.7 medical genetics doctors, and 3.6 laboratory technicians every 1 million inhabitants, across the country (Centro Nacional de Genética Médica y Administración Nacional de Laboratorios e Institutos de Salud, 2004). Although this is expanding at a fast pace, short staffed institutions lead to long waiting lists and contribute to many patients remaining undiagnosed (Penchaszadeh, 2015). Also, few ophthalmologists are well trained to diagnose and manage ophthalmic genetics patients, and there are no guidelines to follow.
A current PubMed query of “ophthalmic genetics Argentina” provides 18 results (https://pubmed.ncbi.nlm.nih.gov/?term=ophthalmic+genetics+Argentina, queried on June 2020). Eight of these are about retinoblastoma, two about infectious diseases, two about glaucoma, two about systemic conditions with ophthalmic manifestations, one about corneal dystrophy, one about age-related macular degeneration, one is preclinical, and one is part of a multinational approach of Stargardt disease, where Argentina contributed with 27 patients, and Brazil with 9 (Khan et al., 2020). The only one report addressing IRD is possibly due to the difficulties ophthalmologists face diagnosing these conditions. There is a severe shortage in diagnostic tools such as ultrawide-field color and autofluorescence imaging, and electrophysiology devices. Also, there are a handful of experts who know how to perform studies following International Society for Clinical Electrophysiology of Vision (ISCEV) standards across the county (McCulloch et al., 2015). The knowledge of inherited eye conditions is poor among ophthalmologists, even retina specialists and, although the cost of genetic testing continues to drop, it remains unaffordable for most individuals or health systems. This leads to inequalities, poor access, and a low percentage of patients being tested and properly counseled. Argentina’s Retinitis Pigmentosa’s Foundation has around 5,000 registered patients, 8% of which have a molecular diagnosis. This scenario, with poor collaboration between medical genetics and ophthalmologists, leads to late diagnosis and mismanagement.
1.4 |. Chile
Chile is a country with 17.5 million inhabitants and 756,102 km2 of territory, by the Pacific Ocean (Central Intelligence Agency, 2020). Their National healthcare system is based in two sectors: public and private. The public is called FONASA and is funded by mandatory contributions. It assists approximately 80% of the population, including the lower income segments. The private system, called ISAPRES, is represented by insurers and funded both by mandatory and voluntary contributions, covering approximately 15% of the population (Cid, Herrera, & Prieto, 2016; Vásquez, Paraje, & Estay, 2013). Neither the National healthcare system nor insurances cover genetic testing and no legal or financial aid are provided for patients with IRD (Encina et al., 2019; Pinilla-Roncancio, 2018).
Throughout the country, over 15 clinical cytogenetic laboratories offer karyotype and FISH, and three laboratories provide molecular genetic tests such as multiplex ligation-dependent probe amplification (MLPA), microarrays, Sanger sequencing, and comparative genomic hybridization (CGH). NGS is available overseas only, at a high cost (Vásquez et al., 2013). There are currently 33 clinical geneticists in the country, 1 medical genetics residency program, and 3 ophthalmologists with formal training in ocular genetics (Clouet-Huerta, González, & Correa, 2017; Taucher, 2003).
On 2015, Hospital del Salvador in Santiago (the Capital city) opened a public Ocular Genetics clinic for patients from all over the country with emphasis in IRD. At present, 700 patients visit this clinic on a regular basis where they are studied with a multi-imaging approach including SD-OCT, visual field, wide-field color, and autofluorescence retinal imaging and electrophysiology. Every case is analyzed in a single visit and patients, along with their relatives, are provided with genetic counseling at the same appointment. Details regarding ongoing clinical trials are also discussed (Margarit, Alvarado, Alvarez, & Lay-Son, 2013). Molecular diagnosis is the main limitation for the ocular genetics’ clinic, due to its high cost. Currently only 21% of the patients have molecular diagnoses, most of them as part of collaborative research projects. In Chile there is no national registry of genetic or rare diseases, therefore the Ocular Genetics clinic’s records are the closest to that. The Ocular genetics’ clinic also provides training for ophthalmology residents from University of Chile (included on their yearly schedule), for retina fellows and soon, for medical genetics residents. Furthermore, the clinic collaborates with the Foundation Fighting Retinitis Pigmentosa (FUNDALURP), allowing patients access to low vision rehabilitation and aids, as well as psychologists.
The query “ophthalmic genetics Chile” in PubMed gives sixteen results: two about the prevalence of ophthalmic conditions within the country, one about genetic testing in IRD, one about retinoblastoma, two about corneal dystrophy, one about nail-patella syndrome associated with glaucoma, two about infectious diseases, two preclinical, one about Alstrom syndrome, one about Knobloch syndrome, one about epidermolysis bullosa, two about retinal degenerations, and one about retinal vein occlusion (https://pubmed.ncbi.nlm.nih.gov/?term=ophthalmic+genetics+Chile, queried on June 2020).
There are numerous challenges that Chile faces such as: increasing the knowledge of genetics among ophthalmologists and other health professionals, promoting international partnerships for research and clinical collaboration, increasing training opportunities abroad, participation in multicenter projects and, of course, strengthen public health policies towards better genomic medicine (Encina et al., 2019).
1.5 |. Patients’ organizations and support groups
There are several patient organization groups in the region with differing visibility and level of activity (Fundación Argentina de Retinosis Pigmentaria, n.d.; Asociación de Padres de Niños con Enfermedad de Stargardt, n.d.; Fundación Lucha contra Retinitis Pigmentosa, n.d.; Retinosis Pigmentaria Colombia, n.d.; Retina Brasil, n.d.). Most of them have websites with basic information for patients and links to regional and global organizations. Many patients seek online information after their diagnosis, and the top search results correspond to these groups, where they can register for email updates and information. These institutions manage a low budget since it is not as common in South America to donate to organizations, such as it is in other parts of the world (e.g., United States of America).
For several patients this support is the only way to complete their path to a correct diagnosis and management. The journey from onset of symptoms to molecular diagnosis is treacherous and time consuming for most patients and families. The abundance of incorrect information, miracle cures offered, lack of retina specialists with experience managing IRD, few or no guidelines from medical societies, and inexistence of official programs or public institutions support, lead to many patients abandoning the search for a correct diagnosis and, currently, a possible treatment. Sometimes, patients’ associations in their honest will to better guide the patients, end up themselves promoting therapies, tests, and specialists’ recommendations that are inadvertently not in the best interest for the patients.
2 |. DISCUSSION
Ophthalmic genetics is a relatively new subspecialty. Despite the rapid pace in which the field continues to evolve, difficulties regarding genetic testing and insurance coverage are present even in countries with successful universal healthcare systems (Lai & Wu, 2017) or high-income (Lowery, Dehnel, Schaefer, & Uwaydat, 2020).
South America is a heterogenous, big region that includes countries with different healthcare situations. As a whole, however, we struggle with similar challenges:
Ophthalmologists and healthcare professionals in general are not trained enough in genetics and inherited eye diseases, due to poor training in medical schools and from then on.
Tools to diagnose retinal degenerations are scarce and focused in large cities.
Adequate genetic testing is generally not covered by the public healthcare system and it is expensive.
This leads to low access to proper care, undiagnosed patients, absent genetic counseling, and inability to participate in clinical trials.
As the common saying states, you cannot diagnose a disease that you do not even know exists. In order to see an important change in ophthalmic genetics in South America, education is key. Medical schools’ curricula need to be updated and include clinical practice, with more credits dedicated to genetics. Ophthalmology postgraduate courses also have to include more content on how to manage patients with IRD and how to communicate with geneticists. Patients with inherited eye conditions require a large team of well-trained professionals within ophthalmology (i.e., general ophthalmologists, pediatric ophthalmologists, retina specialists, technicians, electrophysiology specialists) and other fields (geneticists, primary care doctors, among others). The Federal University of São Paulo is the only institution in South America that provides a postgraduate course in Ocular Genetics. The rest of the professionals in the region that wish to pursue a career in ophthalmic genetics needs to get training abroad, despite having good development of medical genetics locally. As the knowledge of genetics increases, more training opportunities should accompany this effort, providing further specialization for those interested in the topic.
Ophthalmology societies across the region should provide clear guidelines for the optimal diagnosis and management of individuals with IRD and other inherited eye diseases. These should be available for general ophthalmologists as well as for other colleagues such as primary care doctors, audiologists, and pediatricians. National programs need to be set up in order to help patients suspected of having an inherited eye disease to afford the costs of the referral to large ophthalmology centers in capital cities. Necessary equipment should be arranged in specialized centers, along with trained professionals. Also, collaboration with patients’ organizations will reduce the spread of unproven therapies and confusing information. Most patients do not have proper warning signs to timely consult and the bureaucracy of health systems tend to tire them out, therefore having adequate knowledge and tools is key for us to make full use of every consult.
Moreover, to benefit from the results of tested patients, we need to collaborate with each other and create repositories of genomic, clinical, and epidemiological information. This will generate knowledge about the specifics of the Latin American cohort, contributing with the worldwide efforts towards managing these conditions.
The international struggle to include genetic testing in insurance plans needs to change urgently, as new treatment options for preventing, slowing progression, or even reverse it are now in development for inherited retinal diseases. There is already one FDA approved gene therapy (Luxturna) and the field is actively working in including more conditions to treat (Russell et al., 2017). Therefore, what before was a diagnostic tool not considered relevant enough to be included in any Mandatory Medical Program will soon have to be added. The cost will continue to decrease but its inclusion should also take into account the valuable information that it adds to patient care. Furthermore, several conditions in the field of ocular genetics have systemic involvement. Genetic testing provides precise diagnoses with direct implications on the quality of care, pointing out other organs to be screened for sometimes treatable conditions, if diagnosed early enough (i.e., Bardet-Biedl syndrome, Senior Loken, Fabry disease). Early molecular diagnosis becomes then more efficient and less expensive in the long run and can be used for family planning as well.
Lacking the final step of molecular diagnosis, the patients cannot meet the inclusion criteria for interventional clinical trials. This not only represents a loss for the patient, being the main management and treatment opportunity that currently exists, but for the field. As a developing subspecialty, information on novel damaging variants and genes helps us improve our knowledge of these rare conditions, ameliorating the overall management of these patients.
As a summary, our region should work towards:
Updating the genetics curriculum on medical schools and ophthalmology residency programs.
Creating an Ophthalmic Genetics Society within South America, which will enable us to join efforts towards organizing local training opportunities for professionals, creating guidelines and genetic repositories.
Setting up telemedicine services among the few local professionals that are acquainted with IRD, to assist colleagues in remote areas.
Collaborating with local geneticists and researchers, in order to achieve a better insurance coverage for genetic testing, increasing the percentage of patients molecularly diagnosed, and eligible for clinical trials.
Ophthalmic genetics’ situation in our region sheds light on larger problems: incomplete curriculum in medical schools and residency programs, and tight budget for public health. Patients with rare and ultra-rare genetic conditions are a minority whose needs are barely attended. South America can contribute with research with thousands of well-diagnosed patients and a genetically unique population, in need of proper management and treatment opportunities. Research set ups and collaborations must be created, with grants and with researchers’ employment possibilities. We need to team up as a region and as a subspecialty to create consensus on how to manage these patients and how to improve healthcare systems, delivering better-quality care.
Acknowledgments
Funding information
NEI Intramural Funds
REFERENCES
- Adhikari K, Mendoza-Revilla J, Chacón-Duque J, Fuentes-Guajardo M, & Ruiz-Linares A. (2016). Admixture in Latin America. Current Opinion in Genetics & Development, 41, 106–114. 10.1016/j.gde.2016.09.003 [DOI] [PubMed] [Google Scholar]
- Armus D, & Denis A. (2011). Disease, medicine, and health). In Moya J. (Ed.), The Oxford handbook of Latin American history. New York, NY: Oxford University Press. [Google Scholar]
- Asociación de Padres de Niños con Enfermedad de Stargardt. n.d.. Retrieved from www.stargardt.com.ar
- Avena S, Via M, Ziv E, Pérez-Stable EJ, Gignoux CR, & Dejean C. (2012). Heterogeneity in genetic admixture across different regions of Argentina. PLoS One, 7(4), e34695. 10.1371/journal.pone.0034695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belló M, & Becerril-Montekio V. (2011). The health system of Argentina. Salud Pública de México, 53(Suppl. 2), s96–s108. [PubMed] [Google Scholar]
- Borrajo G. (2007). Newborn screening in Latin America at the beginning of the 21st century. Journal of Inherited Metabolic Disease, 30(4), 466–481. 10.1007/s10545-007-0669-9 [DOI] [PubMed] [Google Scholar]
- Castilla E, & Orioli I. (2004). ECLAMC: The Latin-American collaborative study of congenital malformations. Community Genetics, 7, 76–94. [DOI] [PubMed] [Google Scholar]
- Central Intelligence Agency. (2020). The World Factbook. Retrieved from https://www.cia.gov/library/publications/the-world-factbook/rankorder/2147rank.html
- Centro Nacional de Genética Médica. (2017a). National census of public resources for diagnosis of genetic diseases. Retrieved from http://www.anlis.gov.ar/cenagem/?page_id=119
- Centro Nacional de Genética Médica. (2017b). Administración Nacional de Laboratorios e Institutos de salud. Retrieved from Laboratories List: http://www.anlis.gov.ar/cenagem/wp-content/uploads/2017/11/Laboratorios-Argentina-2017-1.pdf
- Centro Nacional de Genética Médica. (2017c). Administración Nacional de Laboratorios e Institutos de salud. Retrieved from pathologies with molecular diagnosis and molecular cytogenetics available in the public sphere: http://www.anlis.gov.ar/cenagem/wp-content/uploads/2017/10/Patologías-1017.pdf
- Centro Nacional de Genética Médica y Administración Nacional de Laboratorios e Institutos de Salud. (2004). Census of resources in medical genetics in Argentina and promotion of a National Network carried out by the Center for Epidemiological Research (ANLIS). [Google Scholar]
- Chiang P, Wang J, Chen Y, Fu Q, Zhong J, Chen Y, … Qi M. (2012). Exome sequencing identifies NMNAT1 mutations as a cause of Leber congenital amaurosis. Nature Genetics, 44(9), 972–974. 10.1038/ng.2370 [DOI] [PubMed] [Google Scholar]
- Cid C, Herrera CA, & Prieto L. (2016). Hospital performance in a segmented and unequal health system: Chile 2001–2010. Salud Publica de Mexico, 58(5), 553–560. 10.21149/spm.v58i5.7972 [DOI] [PubMed] [Google Scholar]
- Clouet-Huerta D, González B, & Correa K. (2017). Medical specialization in Chile: Types, mechanisms and application requirements. An update on processes for general practitioners. Revista Médica de Chile, 145(11), 1454–1462. 10.4067/s0034-98872017001101454 [DOI] [PubMed] [Google Scholar]
- Cotignola JR (2019). Genetics and genomic medicine in Argentina. Molecular Genetics & Genomic Medicine, 7(4), e00571. 10.1002/mgg3.571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Departamento Administrativo Nacional de Estadística. (2005). General census. Retrieved from https://www.dane.gov.co/index.php/estadisticaspor-tema/demografia-y-poblacion/censo-general-2005-1
- District of Columbia Department of Health. (2010). Understanding genetics: A District of Columbia guide for patients and health professionals (Chapter 4, Newborn screening). Genetic Alliance. Retrieved from: Washington (DC). https://www.ncbi.nlm.nih.gov/books/NBK132148/ [PubMed] [Google Scholar]
- Encina G, Castillo-Laborde C, Lecaros J, Dubois-Camacho K, Calderón J, Aguilera X, … Reppetto GM (2019). Rare diseases in Chile: Challenges and recommendations in universal health coverage context. Orphanet Journal of Rare Diseases, 14, 289. 10.1186/s13023-019-1261-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fundación Argentina de Retinosis Pigmentaria. n.d. Retrieved from www.retinosis.org
- Fundación Lucha contra Retinitis Pigmentosa. n.d. Retrieved from www.fundalurp.cl
- Global Retinoblastoma Study Group, Fabian ID, & Abdallah E. (2020). Global retinoblastoma presentation and analysis by National Income Level. JAMA Oncology, 6, 685. 10.1001/jamaoncol.2019.6716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoehn T, Lukacs Z, Stehn M, Mayatepek E, Philavanh K, & Bounnack S. (2013). Establishment of the first newborn screening program in the People’s Democratic Republic of Laos. Journal of Tropical Pediatrics, 59(2), 95–99. 10.1093/tropej/fms057 [DOI] [PubMed] [Google Scholar]
- Homburger JR, Moreno-Estrada A, Gignoux CR, Nelson D, Sanchez E, Ortiz-Tello P, … Acevedo-Vasquez EM-R (2015). Genomic insights into the ancestry and demographic history of South America. PLoS Genetics, 11(12), e1005602. 10.1371/journal.pgen.1005602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Instituto Brasileiro de Geografía e Estadística. (2015). Sistema IBGE de Recuperaçao Automática - SIDRA. Retrieved from National Household Sample Survey: https://sidra.ibge.gov.br/Tabela/262
- Khan M, Cornelis SS, Pozo-Valero MD, Whelan L, Runhart EH, Mishra K, … AlTalbishi AD-Y (2020). Resolving the dark matter of ABCA4 for 1054 Stargardt disease probands through integrated genomics and transcriptomics. Genetics in Medicine, 22, 1235–1246. [DOI] [PubMed] [Google Scholar]
- Lai YH, & Wu KY (2017). Ocular genetics in Taiwan. Current Opinion in Ophthalmology, 28(5), 430–435. 10.1097/ICU.0000000000000398 [DOI] [PubMed] [Google Scholar]
- Lowery R, Dehnel J, Schaefer G, & Uwaydat S. (2020). Rates of diagnostic genetic testing in a tertiary ocular genetics clinic. Ophthalmic Genetics, 41, 1–4. 10.1080/13816810.2020.1759107 [DOI] [PubMed] [Google Scholar]
- Manotas M, & Sarmiento K. (2019). Risk factors associated with congenital defects that alter hearing or vision in children born in the city of Bogotá between 2002 and 2016. International Journal of Pediatric Otorhinolaryngology, 126, 109594. [DOI] [PubMed] [Google Scholar]
- Mao X, Bigham A, Mei R, Gutierrez G, Weiss K, Brutsaert T, … P M. (2007). A genomewide admixture mapping panel for Hispanic/Latino populations. American Journal of Human Genetics, 80(6), 1171–1178. 10.1086/518564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margarit SB, Alvarado M, Alvarez K, & Lay-Son G. (2013). Medical genetics and genetic counseling in Chile. Journal of Genetic Counseling, 22(6), 869–874. 10.1007/s10897-013-9607-1 [DOI] [PubMed] [Google Scholar]
- Mateus H, Pérez A, & Mesa M. (2017). A first description of the Colombian national registry for rare diseases. BMC Research Notes, 10(1), 514. 10.1186/s13104-017-2840-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCulloch DL, Marmor MF, Brigell MG, Hamilton R, Holder GE, Tzekov R, & Bach M. (2015). ISCEV standard for full-field clinical electroretinography (2015 update) documenta ophthalmologica. Advances in Ophthalmology, 130(1), 1–12. 10.1007/s10633-014-9473-7 [DOI] [PubMed] [Google Scholar]
- Mendoza-Londono R, Hiriyanna K, & Bingham E. (1999). A Colombian family with X-linked juvenile retinoschisis with three affected females finding of a frameshift mutation. Ophthalmic Genetics, 20(1), 37–43. 10.1076/opge.20.1.37.2299 [DOI] [PubMed] [Google Scholar]
- Ministério da Saúde. (2018). Programa nacional de triagem neonatal. Retrieved from https://www.saude.gov.br/acoes-e-programas/programa-nacionalda-triagem-neonatal [Google Scholar]
- Ministerio de Salud. (2017). Current situation of orphan diseases in Colombia 2017. In M. Pareja, Revista CES Derecho. [Google Scholar]
- Ministerio de Salud. (2020). General information examination of residences. Retrieved from https://www.argentina.gob.ar/salud/residencias/ingresoresidencias/examen-unico/informacion-general
- Morantes S, Evans C, Valencia A, Davidson A, Hardcastle A, Ruiz Linares A, … Cuevas M. (2016, Aug). Spectrum of clinical signs and genetic characterization of gelatinous drop-like corneal dystrophy in a Colombian family. Cornea, 35(8), 1141–1146. 10.1097/ICO.0000000000000895 [DOI] [PubMed] [Google Scholar]
- Motta F, Martin R, Filippelli-Silva R, Vallim Salles M, & Sallum FJM (2018). Relative frequency of inherited retinal dystrophies in Brazil. Scientific Reports, 8(1), 1–9. 10.1038/s41598-01834380-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moya J. (1998). Cousins and strangers: Spanish immigrants in Buenos Aires (pp. 1850–1930). Berkeley, CA: University of California Press. [Google Scholar]
- Moya J. (2014). Latin America and transatlantic flows: A historical category from a global perspective. In Azcue CN (Ed.), Vaivenes del destino: inmigrantes europeos y latinoamericanos en los espacios atlánticos (pp. 21–38). Madrid: Ediciones Polifemo. [Google Scholar]
- Moya J. (2018). Migration and the historical formation of Latin America in a global perspective. Sociologias, 20(49), 24–68. 10.1590/15174522-02004902 [DOI] [Google Scholar]
- Nicholson D, & Galvis V. (1984, Oct). Criswick-Schepens syndrome (familial exudative vitreoretinopathy). Study of a Colombian kindred. Archives of Ophthalmology, 102(10), 1519–1522. [DOI] [PubMed] [Google Scholar]
- O’Rawe J, Wu Y, & Dörfel M. (2015). TAF1 variants are associated with dysmorphic features, intellectual disability, and neurological manifestations. American Journal of Human Genetics, 97(6), 922–932. 10.1016/j.ajhg.2015.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachajoa H, Villota V, & Cruz L. (2015). Prevalence of birth defects diagnosed at birth in two hospitals of different levels of complexity. Biomédica, 35(2), 227–234. 10.1590/S012041572015000200011 [DOI] [PubMed] [Google Scholar]
- Penchaszadeh V. (2015). Ethical issues in genetics and public health in Latin America with a focus on Argentina. Journal of Community Genetics, 6(3), 223–230. 10.1007/s12687-015-0217-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinilla-Roncancio M. (2018). The reality of disability: Multidimensional poverty of people with disability and their families in Latin America. Disability and Health Journal, 11(3), 398–404. 10.1016/j.dhjo.2017.12.007 [DOI] [PubMed] [Google Scholar]
- Porras-Hurtado G, León-Castañeda O, & Molano-Hurtado J. (2016). Prevalence of birth defects in Risaralda, 2010–2013. Biomedica, 36(4), 556–563. 10.7705/biomedica.v36i4.2771 [DOI] [PubMed] [Google Scholar]
- Retina Brasil. n.d.. Retrieved from www.retinabrasil.org.br
- Retinosis Pigmentaria Colombia. n.d.. Retrieved from https://www.facebook.com/geneticarp/
- Rothstein K, Gálvez J, Gutiérrez A, Rico L, Criollo E, & De-la-Torre A. (2019). Ocular findings in Fabry disease in Colombian patients. Biomedica, 39(3), 434–439. 10.7705/biomedica.3841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell S, Bennett J, Wellman JA, Chung DC, Yu ZF, Tillman A, … Cross DM (2017). Efficacy and safety of voretigene neparvovec (AAV2-hRPE65v2) in patients with RPE65-mediated inherited retinal dystrophy: A randomised, controlled, open-label, phase 3 trial. Lancet, 390(10097), 849–860. 10.1016/S0140-6736(17)31868-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallum J, Abalem M, Melo M, & Finzi S. (2019). Série oftalmologia brasileira genética ocular. Rio de Janeiro: Cultura Médica. [Google Scholar]
- Sanabria D, Groot H, Guzmán J, & Lattig M. (2012). An overview of oculocutaneous albinism: TYR gene mutations in five Colombian individuals. Biomédica, 32(2), 269–276. 10.1590/S012041572012000300015 [DOI] [PubMed] [Google Scholar]
- Sociedade Brasileira de Genética Médica e Genômica (SBGM). (2020). Retrieved from https://www.sbgm.org.br/
- Tamayo M, Bernal J, Tamayo G, Frias J, Alvira G, Vergara O, … Silva J. (1991). Usher syndrome: Results of a screening program in Colombia. Clinical Genetics, 40(4), 304–311. [DOI] [PubMed] [Google Scholar]
- Tamayo M, Gelvez N, Rodriguez M, Florez S, Varon C, Medina D, & Bernal J. (2008). Screening program for Waardenburg syndrome in Colombia: clinical definition and phenotypic variability. American Journal of Medical Genetics A, 146A(8), 1026–1031. 10.1002/ajmg.a.32189 [DOI] [PubMed] [Google Scholar]
- Tapiero-Rodriguez S, Acosta Guio J, Porras-Hurtado G, García N, Solano M, Pachajoa H, & Velasco H. (2018). Determination of genotypic and clinical characteristics of Colombian patients with mucopolysaccharidosis IVA. The Application of Clinical Genetics, 11, 45–57. 10.2147/TACG.S141881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taucher S. (2003). Genetic services in Chile. Community Genetics, 7(2–3), 121–125. 10.1159/000080781 [DOI] [PubMed] [Google Scholar]
- Therrell BL, & Padilla CD (2018). Newborn screening in the developing countries. Current Opinion in Pediatrics, 30(6), 734–739. 10.1097/MOP.0000000000000683 [DOI] [PubMed] [Google Scholar]
- United Nations Department of Economic and Social Affairs (2019). World population prospects, total population - both sexes. Retrieved from https://population.un.org/wpp/Download/Standard/Population/
- Vargas-Zea N, Castro H, Rodríguez-Páez F, Téllez D, & Salazar-Arias R. (2012). Colombian health system on its way to improve allocation efficiency—Transition from a health sector reform to the settlement of an HTA agency. Value in Health Regional Issues, 1, 218–222. [DOI] [PubMed] [Google Scholar]
- Vásquez F, Paraje G, & Estay M. (2013). Income-related inequality in health and health care utilization in Chile, 2000–2009. Pan American Journal of Public Health, 33(2), 98–106. 10.1590/s1020-49892013000200004 [DOI] [PubMed] [Google Scholar]
- Vishnopolska SA (2018). Genetics and genomic medicine in Argentina. Molecular Genetics & Genomic Medicine, 6(4), 481–491. 10.1002/mgg3.455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarante I, Sarmiento K, & Mallarino C. (2016). Description of Bogotá birth defects surveillance and follow-up program. Journal of Registry Management, 41(3), 116–121. [PubMed] [Google Scholar]